
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 09 January 2023
Sec. Sleep Disorders
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.1095404
Objective: Interest in sleep disorders among the elderly, especially those in Korea, has increased. We aimed to describe the overall sleep status of the elderly population in Korea using survey data and to determine the risk factors concerning different aspects of sleep status.
Methods: We conducted a cross-sectional survey on 271 respondents aged 65–86 years old. We performed multistage clustered random sampling according to the population and socioeconomic distribution of all Korean territories. The survey questionnaire was used to perform a structural assessment of sociodemographic characteristics; medical comorbidities; psychiatric comorbidities; and sleep status, including sleep duration, sleep quality, presence of insomnia, excessive daytime sleepiness, sleep apnea, and restless legs syndrome.
Results: Approximately 12.5, 22.%, and 51.3% of the elderly population had poor sleep quality, excessive daytime sleepiness, and insomnia, respectively. Hypertension, dyslipidemia, insomnia, anxiety, and depression predicted poor sleep quality. Female sex, insomnia, and sleep apnea predicted excessive daytime sleepiness. Poor sleep quality and depression predicted insomnia.
Conclusion: A substantial proportion of the elderly Korean population have sleep problems, including poor sleep quality, excessive daytime sleepiness, and insomnia. Sleep status is influenced by various factors, including age, sex, and metabolic and psychiatric comorbidities.
South Korea has the fastest-aging population in the world. According to the Korean Statistical Information Service, individuals aged > 65 years comprised only 7.2% of the population in 2000, but >10.2% in 2008 and is expected to exceed 20% by 2025 (1). Despite the growing demand for medical care for the elderly population, medical infrastructure and personnel remain insufficient (2). With increasing numbers of the elderly, an increase in sleep disorders in the elderly population has been noted; however, sleep disorders have not been studied to the extent that chronic neurodegenerative or metabolic diseases have. Among the elderly, poor sleep quality causes deterioration of basic cognitive function, memory, and performance (3, 4). Furthermore, insomnia and inconsistent sleep duration are associated with metabolic syndrome (5, 6). In a recent study of the elderly population aged 65 years or older, there was also a study that self-reported poor sleep quality and self-reported too short or too long sleep duration were associated with an increased risk of falls (7). Although not targeting only the elderly, a nation-wide cohort study in Denmark showed that sleep disorder was associated with a high suicidal rate even after adjusting for other psychiatric comorbidities (8).
The duration of lighter sleep stages increases with aging, with more frequent episodes of nocturnal waking up. Moreover, the total sleep time decreases with age (9). Furthermore, the quality of sleep worsens with aging in combination with anxiety, chronic illness, and lack of social support (10). In addition to these aging-related physiological changes, sleep problems are strongly influenced by sociological factors (11). Sociologic factors affecting sleep quality have been studied in several countries (12–15). Poor sleep quality is prevalent among the rural elderly population (16, 17). Accordingly, in addition to drug and cognitive behavioral therapy, modulating sociodemographic factors in the elderly population is crucial to address sleep disorders (10, 18). Determining the sleep status of elderly individuals is important in choosing an appropriate intervention (19).
Recently, studies have emerged that COVID-19 infection affects sleep. In one study conducted in a group of 300 patients aged 18 years or older, poor sleep quality was observed in 64.8% of the follow-up results 6 months after confirmation (20). In addition, in the group of 1,733 discharged patients followed for about 6 months after diagnosis of COVID-19, the most common symptom was fatigue or muscle weakness followed by sleep difficulties (21). In a French study in which 1,736 participants responded, the incidence of posttraumatic stress disorder after an unprecedented lockdown was 17.5%, and it was found that anxiety, depression, and sleep problems developed high in this group 1 month later (22). Furthermore, there is also a study that psychological distress and anxiety have a high incidence rate in the COVID-19 patient group, and insomnia is a risk factor (23).
Based on these studies, we cannot rule out the possibility that the prevalence of psychiatric and general health comorbidities may have changed in demographic data before and after COVID-19 (20, 24, 25). This pandemic is thought to adversely affect the sleep behavior of the elderly population and increase risks such as falls, but studies on the relationship between the COVID-19 pandemic and sleep in the elderly are lacking (26). However, the data used in this study were collected before 2019, so COVID-19-related content was not included.
Nationwide cross-sectional studies on sleep are being conducted in many countries, and various conclusions have been drawn from each study. A study in China estimated that one in 10 of the population studied had sleep disorders (27). In addition, this study confirmed that sleep quality was correlated with sociodemographic data such as sex, marital status, and education level. According to another recent nationwide cross-sectional study conducted in China, excessive sleep duration rather adversely affects the cognitive function of the elderly population (28). In addition, a US study of 25,962 people with an average age of 48.1 years concluded that sleep duration was independently associated with a high incidence of depression (29). A nationwide cross-sectional study in Indonesia showed that aging is a risk factor for poor sleep quality, which can lead to depression, and stressed that managing such sleep quality is important to lower the incidence of depression in communities (30). As such, since sleep status is closely related to sociodemographic data, studies according to the characteristics of the population in each region are needed.
However, research on the sleep status of the elderly population in Korea is still lacking (31–34). Accordingly, determining the predictive factors for sleep quality, daytime sleepiness, and insomnia could facilitate the integrated management of elderly patients. We aimed to examine the overall sleep status of the elderly population in Korea and the various predictive factors for sleep disorders.
We analyzed data from a nationwide cross-sectional survey of headache and sleep of Korean adult population aged 65–86 years, excluding Jeju-do.
South Korea was geographically divided into 16 administrative division at the time of study, and each administrative division was further divided into basic administrative units (si, gun, or gu). We performed multistage clustered random sampling according to the population and socioeconomic distribution in all Korean territories, except Jeju-do. First, 15 administrative divisions of South Korea (do), except Jeju-do, were designated as primary sampling units, and appropriate sample numbers were assigned to each primary sampling unit according to population distribution. In the second stage, we selected representative basic administrative units (si, gun, and gu) for each primary sampling units, and assigned a target sample number (35). Total 311 respondents were included.
The respondents gave their informed consent for face-to-face interviews using questionnaires regarding sleep status conducted by experienced interviewers hired by Gallup Korea. To minimize potential interest bias, the interviewers were informed that the survey was on a social health issue rather than a sleep issue.
The survey questionnaire was used to perform a structural assessment of sociodemographic characteristics including educational attainment, occupational status, drinking behavior, presence of lack of exercise, obesity, shift work, and taking sleep pill; cardiovascular and metabolic comorbidities, including hypertension, diabetes mellitus, dyslipidemia, and cardiovascular diseases; and psychiatric comorbidities, including depression and anxiety.
Educational attainment was divided into middle school graduation or less and high school graduation or higher. Occupation was considered to be present if the person answered the question asking what the job was. Alcohol consumption was considered to be a risk factor if alcohol was consumed on four or more days per week. Lack of exercise was considered as no exercise day during the week. Obesity was considered when the respondent had a BMI of 25 or higher based on the height and weight written by the respondent. In the questionnaire, respondents were asked if they worked shifts, and if they answered yes, they were defined as shift workers. In addition, it was defined as having a factor in taking sleeping pills if the respondents answered that they took sleeping pills at least once a week through the questionnaire. The presence of hypertension, diabetes, hyperlipidemia, and cardiovascular disease were all based on the respondents' description. Cardiovascular disease referred to coronary heart disease, stroke, peripheral arterial disease, and aortic disease.
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) (36), which is a self-reported scale comprising seven components (subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction). Based on the Korean version of the PSQI, poor sleep quality was indicated by a PSQI score ≥ 9 (37).
The Epworth Sleepiness Scale (ESS) was used to evaluate daytime sleepiness. Excessive daytime sleepiness (EDS) was indicated by an ESS score ≥ 10 (38).
The presence of insomnia was evaluated using the Insomnia Severity Index (ISI), which comprises seven items for diagnosing insomnia scored on a 0–4 scale. Subthreshold insomnia was indicated by an ISI score ≥ 8 (39).
Korean version of depression screening tool (Patient Health Questionnaire-9, PHQ-9) was used as screening tool. The Korean PHQ-9 was known as having 81.1% sensitivity and 89.9% specificity (40). In this study, depression was considered probable if the PHQ-9 score was five or higher (41). Goldberg Anxiety Scale (GAS) questionnaire was used to diagnose anxiety among participants. Participants were regarded as having anxiety according to GAS score ≥ 5, with a sensitivity of 82.0% and specificity of 94.4% (42).
The risk of sleep apnea was assessed using the Berlin Questionnaire (BQ), with a positive score in more than two or more categories indicating a high risk of sleep apnea (43). The presence of restless leg syndrome was assessed using the Cambridge-Hopkins Diagnostic Questionnaire; specifically, we used four essential diagnostic criteria proposed by the International Restless Legs Syndrome Study Group (44). If all four criteria were satisfied, the participant was considered to have restless leg syndrome. This was diagnosed by a neurologist based on a questionnaire.
The study protocol was approved by the Institutional Review Board/Ethics Committee of Hallym University Sacred Heart Hospital in Korea (Approval no. 2011-I077). Written informed consent was obtained before the survey.
The normality of data distribution was assessed using the Kolmogorov–Smirnov test. After confirming normal data distribution, continuous variables were compared using Student's t-test, with an estimation of statistical significance under homogeneity of variances. The chi-square test was used to compare categorical variables. Finally, we performed binary multivariate logistic regression analysis to calculate the odds ratios (ORs) with 95% confidence intervals (CIs) for the occurrence of poor sleep quality, EDS, and insomnia. Multicollinearity between variants was minimized using the backward elimination method. Statistical significance was set at p < 0.05. Statistical analyses were performed using the Statistical Package for Social Sciences (version 26.0; IBM Corp., Armonk, NY, USA). This study was reported according to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist (45).
Among 311 initial participants aged > 65 years, 271 participants [age: 69.9 ± 4.4 years; 139 (51.3%) women] completed the survey. 139 (51.3%) participants were female. A total of 200 (73.8%) participants had an educational level lower than middle school. Moreover, 74 (27.3%) and 17 (6.3%) participants were unemployed and shift workers, respectively. Further, 142 (52.4%), and 72 (26.6%) participants did not exercise at all and were overweight or obese (body mass index > 25), respectively. Only 12 (4.4%) participants reported taking sleeping pills. Additionally, 123 (45.4%), 48 (17.7%), 86 (31.7%), and 15 (5.5%) participants had hypertension, diabetes mellitus, cardiovascular disease, and dyslipidemia, respectively (Table 1).
The average sleep duration during weekdays and the weekend were 7.14 ± 1.38 h and 7.28 ± 1.39 h, respectively. Thirty-four (12.5%) participants had poor sleep quality, based on PSQI scores ≥ 9; 139 (51.3%), 62 (22.9%), 53 (19.6%), 28 (10.3%), 45 (16.6%), and 64 (23.6 %) participants had insomnia, EDS, a high risk of sleep apnea, restless leg syndrome, anxiety, and depression, respectively (Table 1).
Furthermore, we compared sleep-related indicators according to gender. There was no difference in sleep duration according to gender, but PSQI, ISI, and ESS scores were statistically significantly higher in females (5.63 ± 2.71 vs. 4.80 ± 2.83, 10.90 ± 6.75 vs. 8.95 ± 6.69, 6.91 ± 4.30 vs. 5.71 ± 4.15, retrospectively) (Supplementary Table 1).
Compared with participants with good sleep quality, participants with poor sleep quality were older (71.4 ± 3.9 years vs. 69.7 ± 4.4. years, p = 0.04) and had a significantly shorter daily sleep duration on weekdays (5.46 ± 1.55 h vs. 7.38 ± 1.18 h, p = 0.01) and weekends (5.75 ± 1.61 h vs. 7.50 ± 1.21 h, p = 0.01) as well as a higher prevalence of insomnia (97.1 vs. 44.7%, p = 0.01) and sleep apnea (38.2 vs. 16.9%, p = 0.01). Additionally, compared with participants with good sleep quality, participants with poor sleep quality were more likely to have psychiatric comorbidities (anxiety, 52.9 vs. 11.4%; depression, 70.6 vs. 16.9%; both p = 0.01), dyslipidemia (17.6 vs. 3.8%, p = 0.01), and sleeping pill intake (23.5 vs. 1.7%, p = 0.01). Compared to participants with good sleep quality, those with poor sleep quality had a more frequent EDS and restless legs syndrome, but these differences were not statistically significant. Finally, there were no between-group differences in the frequency of sociodemographic risk factors, including low educational attainment, inoccupation, drinking alcohol, smoking, lack of exercise, obesity, and shift work (Table 2).
There was no significant age difference between patients with and without EDS (69.3 ± 4.0 vs. 70.1 ± 4.4 years, p = 0.17). There was a significantly higher proportion of women among participants with EDS than among those without (66.1 vs. 46.9%, p = 0.01).
Respondents with EDS were more likely to have insomnia (66.1 vs. 46.9%, p = 0.01) and depression (33.9 vs. 20.6%, p = 0.03) than those without EDS. More frequent anxiety, poor sleep quality, sleep apnea, restless legs syndrome, and shorter sleep durations on weekdays (6.98 ± 1.52 h vs. 7.19 ± 1.34 h, p = 0.33) and weekends (7.11 ± 1.46 h vs. 7.33 ± 1.37 h, p = 0.27) were also noted among those with excessive daytime sleepiness, but these differences were not statistically significant.
There was no significant between-group difference in educational attainment, occupational status, alcohol drinking, and shift work; however, participants with EDS had a significantly lower frequency of current smoking than those without (3.2 vs. 17.7%, p = 0.01). Finally, there was no significant between-group difference in the use of sleeping pills (Table 3).
There was no significant difference in the mean age according to the presence of insomnia (70.2 ± 4.4 vs. 69.7 ± 4.3, p = 0.48). Compared with participants without insomnia, those with insomnia showed a higher proportion of women (60.4 vs. 41.7%, p = 0.01). Moreover, in the group with insomnia, the rate of lacking exercise was higher (60.4 vs. 43.9%, p = 0.02). There was no significant difference in the frequency of hypertension, diabetes mellitus, and dyslipidemia according to the presence of insomnia; however, participants with insomnia had a higher prevalence of cardiovascular disease (38.1 vs. 25.0%, p = 0.02). While poor sleep quality, anxiety, and depression were more prevalent in the group with insomnia, there was no significant difference in the prevalence of sociodemographic factors (Table 4).
Multivariate logistic regression analysis revealed that hypertension (OR, 2.51; 95% CI, 1.01–6.26; p = 0.05), dyslipidemia (OR, 6.62; 95% CI, 1.56–28.10; p = 0.01), insomnia (OR, 29.90; 95% CI, 3.13–286.10; p = 0.01), anxiety (OR, 4.15; 95% CI, 1.53–11.28; p = 0.01), and depression (OR, 2.93; 95% CI, 1.10–7.83; p = 0.03) were independent risk factors for poor sleep quality (Table 5).
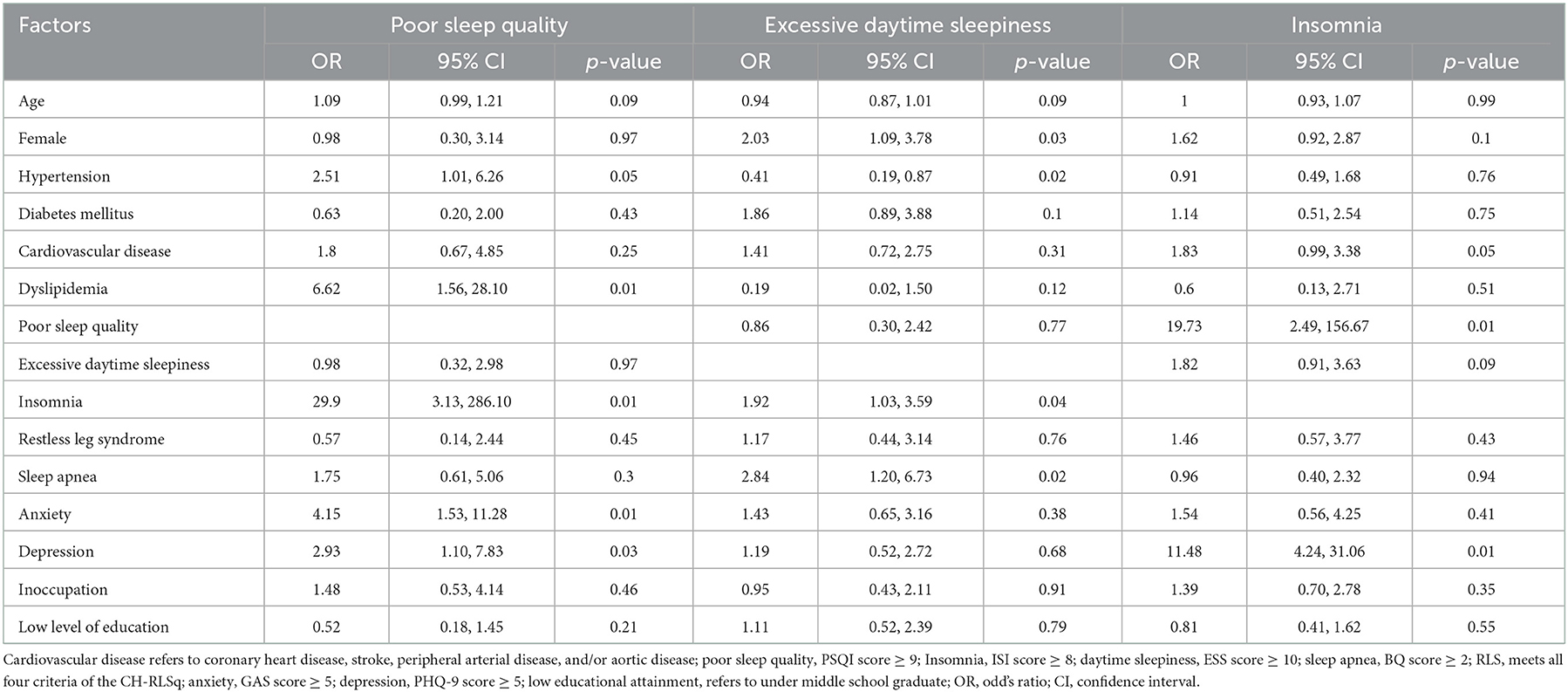
Table 5. Risk factors for poor sleep quality, excessive daytime sleepiness, and insomnia in the elderly population.
Multivariate logistic regression analysis revealed that female sex (OR, 2.03; 95% CI, 1.09–3.78; p = 0.03), insomnia (OR, 2.84; 95% CI, 1.03–3.59; p = 0.04), and sleep apnea (OR, 2.84; 95% CI, 1.20–6.73; p = 0.02) were independent risk factors for EDS; in contrast, the presence of hypertension decreased the risk of EDS (OR, 0.41; 95% CI, 0.19–0.87; p = 0.02) (Table 5).
Multivariate logistic regression analysis revealed that poor sleep quality (OR, 19.73; 95% CI, 2.49–156.67) and depression (OR, 11.48; 95% CI, 4.24–31.06) were independent risk factors for insomnia (Table 5).
In our study, 12.5, 22.9, and 51.3% of the participants had poor sleep quality, EDS, and insomnia, respectively. Further, sleep status in the elderly population was influenced by various factors, including age, sex, and metabolic and psychiatric comorbid diseases.
Comparing sleep indices including PSQI, ISI, and ESS, it was found that female had worse sleeping habits even in the elderly population. Female have shown higher prevalence of insomnia compared to male according to previous studies (46–48). Similar results were also found in this study in the elderly population. According to a study of young adult population, female showed higher prevalence of poor sleep quality, even after adjusting psychiatric and sociodemographic factors (49).
The frequency of arousal during sleep increases with age, which causes difficulty in maintaining sleep, reduced sleep duration and decreased slow-wave sleep (50). Over 50% of individuals aged > 65 years have at least one sleep problem, including trouble falling asleep, waking up, waking up too early, needing to nap, and not feeling rested (51). Since sleep patterns vary according to health status and environment, there are wide variations in the clinical characteristics of sleep disorders in the elderly population (31). Our study performed an overall review of the sleep status in the general, rather than only healthy, elderly population.
The total sleep duration decreases with age (50). The SIESTA database showed that the total sleep time in the adult population decreased by ~8–10 min per 10 years in the adult population; however, physiological sleep changes usually stop at the age of ~60 years (52). Since even older adults without complaints of sleep problems present with significant sleep disturbance upon objective evaluation, it is necessary to properly evaluate sleep quality in the elderly population (53). A survey study on 1,085 individuals aged ≥ 75 years reported poor sleep quality in 16.6% of the participants (54), which is consistent with our finding that 34 (12.5%) participants had poor sleep quality.
Participants with poor sleep quality had shorter sleep duration on both weekdays and weekends, with this difference being higher than that previously reported (53). Among the sleep problems, insomnia is a predictor of poor sleep quality. Specifically, since patients with insomnia have a greater need for good sleep quality, they are more vulnerable to poor sleep quality (55).
We found that underlying metabolic comorbidities, including hypertension and dyslipidemia, as well as psychiatric comorbidities, including anxiety and depression, increased the risk of poor sleep quality in the elderly population. Subjective sleep problems in the elderly population are influenced by comorbidities. Our findings are consistent with previous reports (53). Several environmental factors have been reported to affect sleep status (11, 14); however, we observed no correlation between occupational status and educational attainment with the presence of poor sleep quality.
In our study, 62 (22.9%) participants reported EDS, which is consistent with a previously reported prevalence of 20% among adults aged 65 years (56). The female sex was predominant among participants with EDS and was an independent predictor of EDS in the elderly Korean population. Contrastingly, a Swiss study on individuals aged 35–75 years reported that the male sex was a predictor of EDS (57). However, consistent with this previous study, the presence of insomnia and sleep apnea could predict excessive daytime (57).
Hypertension was a negative predictor of EDS in the elderly population. A previous study reported that total ESS scores decreased with age in hypertensive patients with sleep apnea (58). Furthermore, a 6-year follow-up study reported that EDS was a risk factor for mortality related to cardiovascular diseases, including hypertension, in the elderly population (59). This suggests an inter-relationship between EDS and hypertension; however, further studies are warranted.
EDS worsens physical and functional activity in the elderly population (60). A French study reported that EDS negatively affected cognitive function in the elderly population and that a high EDS score could be an early modifiable risk factor (61). Therefore, it is important to evaluate EDS in the elderly population.
The prevalence of insomnia in our study was 51.3%, which was higher than that in a previous Korean study on adults aged 20–69 years (32). Since previous studies have reported a prevalence of insomnia of 12–20% in the elderly population (62), our reported prevalence was rather high. This could be attributed to our definition of subthreshold insomnia as an ISI score ≥ 8. However, another study has reported that ~ 50% of the older adult population presents with insomnia symptoms, including difficulty initiating or maintaining sleep (63).
In our study, poor sleep quality and depression were independent predictors of insomnia in the elderly population. It is well-known that clinicians should consider psychiatric comorbidities when treating insomnia. Our study shares the same clinical context (64). The correlation between sleep problems and psychiatric problems has been studied in the past (65), and more active research is needed in the area of appropriate treatment in the future.
This study has several limitations. First, we used questionnaires administered by interviewers; it is difficult to determine whether the elderly respondents comprehended the question well and provided proper responses since we did not conduct a baseline assessment of their cognitive function status. Furthermore, questionnaire findings cannot accurately reflect objective sleep quality (66). Accordingly, it is difficult to measure sleep status and quality in the elderly population (66, 67).
Second, chronic diseases including neurological disorders such as history of stroke, neurodegenerative disease, head trauma, primary and secondary headache in the elderly population have been scantily studied. About 93% of the elderly population presents with chronic diseases (68). In the future, when planning a study on sleep in the elderly population, the evaluation of chronic diseases should be thoroughly considered since sleep problems have various causes.
Third, although this was a nationwide study, our sample size was small due to our low cooperation rate (36.2%) (69). Therefore, future large-scale studies are warranted to reliably establish the prevalence and predictors of sleep disorders in the elderly population.
Lastly, since this is a study using data prior to COVID-19, which had a global impact, there are limitations in directly incorporating it into the sleep of the current elderly population. Additional research is needed on the relationship between COVID-19 infection and sleep status in the elderly.
A substantial proportion of elderly individuals experience poor sleep quality, EDS, and insomnia. Factors influencing sleep problems included age, sex, and metabolic and psychiatric comorbidities. It is important to determine the sleep status in the elderly population since it affects overall health, including cognitive and metabolic function.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study protocol was approved by the Institutional Review Board/Ethics Committee of Hallym University Sacred Heart Hospital in Korea (Approval no. 2011-I077). The patients/participants provided their written informed consent to participate in this study.
HH designed the study, analyzed the data, and wrote the article. KK supervised data analysis. C-HY, KY, and MC collected data. W-JK designed the study, analyzed the data, and assisted in writing the article. All authors have reviewed and approved the final version of the manuscript.
We would like to thank Editage (www.editage.co.kr) for assisting with English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1095404/full#supplementary-material
1. Korean Statistical Information Service,. Estimated Population by Major Age Group of Korea. Projected Population by Age Group (Korea) (2021). Available online at: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA003&conn_path=I2&language=en
2. Won CW, Kim S, Swagerty D. Why geriatric medicine is important for korea: lessons learned in the United States. J Kor Med Sci. (2018) 33:e175. doi: 10.3346/jkms.2018.33.e175
3. Sutter C, Zöllig J, Allemand M, Martin M. Sleep quality and cognitive function in healthy old age: the moderating role of subclinical depression. Neuropsychology. (2012) 26:768–75. doi: 10.1037/a0030033
4. Damsgaard L, Janbek J, Laursen TM, Erlangsen A, Spira AP, Waldemar G. Hospital-diagnosed sleep disorders and incident dementia: a nationwide observational cohort study. Eur J Neurol. (2022) 29:3528–36. doi: 10.1111/ene.15517
5. Akbaraly TN, Jaussent I, Besset A, Bertrand M, Barberger-Gateau P, Ritchie K, et al. Sleep complaints and metabolic syndrome in an elderly population: the Three-City Study. Am J Geriatr Psychiatry. (2015) 23:818–28. doi: 10.1016/j.jagp.2014.10.001
6. Xie J, Li Y, Zhang Y, Vgontzas AN, Basta M, Chen B, et al. Sleep duration and metabolic syndrome: an updated systematic review and meta-analysis. Sleep Med Rev. (2021) 59:101451. doi: 10.1016/j.smrv.2021.101451
7. Zhu W, Lin H, Zhang J, Sheng M, Kathleen Y, Zheng P, et al. Real-world association of self-reported sleep duration and quality with falls among older adults: a representative nationwide study of China. Sleep Med. (2022) 100:212–8. doi: 10.1016/j.sleep.2022.08.019
8. Kjær Høier N, Madsen T, Spira AP, Hawton K, Eriksen Benros M, Nordentoft M, et al. Association between hospital-diagnosed sleep disorders and suicide: a nationwide cohort study. Sleep. (2022) 45:zsac069. doi: 10.1093/sleep/zsac069
9. Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. (2018) 18:155–65. doi: 10.1111/psyg.12319
10. Zhu X, Hu Z, Nie Y, Zhu T, Chiwanda Kaminga A, Yu Y, et al. The prevalence of poor sleep quality and associated risk factors among Chinese elderly adults in nursing homes: a cross-sectional study. PLoS One. (2020) 15:e0232834. doi: 10.1371/journal.pone.0232834
11. Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. (2010) 10:475. doi: 10.1186/1471-2458-10-475
12. Lallukka T, Sares-Jäske L, Kronholm E, Sääksjärvi K, Lundqvist A, Partonen T, et al. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health. (2012) 12:565. doi: 10.1186/1471-2458-12-565
13. Stringhini S, Haba-Rubio J, Marques-Vidal P, Waeber G, Preisig M, Guessous I, et al. Association of socioeconomic status with sleep disturbances in the Swiss population-based CoLaus study. Sleep Med. (2015) 16:469–76. doi: 10.1016/j.sleep.2014.12.014
14. Takahashi M, Tsutsumi A, Kurioka S, Inoue A, Shimazu A, Kosugi Y, et al. Occupational and socioeconomic differences in actigraphically measured sleep. J Sleep Res. (2014) 23:458–62. doi: 10.1111/jsr.12136
15. Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. (2011) 34:509–18. doi: 10.1093/sleep/34.4.509
16. Choi YH, Chu MK, Kim W-J. Sleep status among older adults in Korea according to urban or rural area residence. J Sleep Med. (2020) 17:37–43. doi: 10.13078/jsm.190051
17. Wang P, Song L, Wang K, Han X, Cong L, Wang Y, et al. Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: a population-based study. Aging Clin Exp Res. (2020) 32:125–31. doi: 10.1007/s40520-019-01171-0
18. Desjardins S, Lapierre S, Vasiliadis HM, Hudon C. Evaluation of the effects of an intervention intended to optimize the sleep environment among the elderly: an exploratory study. Clin Interv Aging. (2020) 15:2117–27. doi: 10.2147/CIA.S277252
19. Hu CP, Zhao YH, Zhao XD, Zhu BG, Qin HY. Correlation between sleep characteristics and cognitive decline in the elderly people: a cross-sectional study in China. Int J Clin Pract. (2021) 75:e14225. doi: 10.1111/ijcp.14225
20. Ahmed GK, Khedr EM, Hamad DA, Meshref TS, Hashem MM, Aly MM. Long term impact of Covid-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Res. (2021) 305:114243. doi: 10.1016/j.psychres.2021.114243
21. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. (2021) 397:220–32. doi: 10.1016/S0140-6736(20)32656-8
22. Alleaume C, Peretti-Watel P, Beck F, Leger D, Vaiva G, Verger P. Incidence of PTSD in the French population a month after the COVID-19 pandemic-related lockdown: evidence from a national longitudinal survey. BMC Public Health. (2022) 22:1500. doi: 10.1186/s12889-022-13880-9
23. Nahidi M, Mokhber N, Sinichi F, Hatefipour Z, Zohorian Sadr P, Emadzadeh M, et al. Mental health outcomes and sleep status among patients with coronavirus disease 2019. Iran J Psychiatry. (2022) 17:276–83. doi: 10.18502/ijps.v17i3.9727
24. Straburzyński M, Kuca-Warnawin E, Waliszewska-Prosół M. COVID-19-related headache and innate immune response - a narrative review. Neurol Neurochir Pol. (2022). doi: 10.5603/PJNNS.a2022.0049
25. Wieckiewicz M, Danel D, Pondel M, Smardz J, Martynowicz H, Wieczorek T, et al. Identification of risk groups for mental disorders, headache and oral behaviors in adults during the COVID-19 pandemic. Sci Rep. (2021) 11:10964. doi: 10.1038/s41598-021-90566-z
26. Parveen S, George SM, Chand S. Was sleep a problem for the elderly during COVID-19? Sleep Vigil. (2021) 5:197–203. doi: 10.1007/s41782-021-00164-2
27. Zhang Y, Wang J, Lu X, Che B, Yu J. Sleep status and the associated factors: a large cross-sectional study in Shaanxi Province, China. Int J Environ Res Public Health. (2021) 18:1250. doi: 10.3390/ijerph18031250
28. Chen WC, Wang XY. Longitudinal associations between sleep duration and cognitive impairment in Chinese elderly. Front Aging Neurosci. (2022) 14:1037650. doi: 10.3389/fnagi.2022.1037650
29. Dong L, Xie Y, Zou X. Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord. (2022) 296:183–8. doi: 10.1016/j.jad.2021.09.075
30. Amelia VL, Jen HJ, Lee TY, Chang LF, Chung MH. Comparison of the associations between self-reported sleep quality and sleep duration concerning the risk of depression: a nationwide population-based study in Indonesia. Int J Environ Res Public Health. (2022) 19:14273. doi: 10.3390/ijerph192114273
31. Lee JS, Yoo RY, Nam HJ, Kwon YN, Sung MJ, Cho HA, et al. Clinical characteristics of elderly patients aged over 65 years with insomnia symptoms. J Korean Sleep Res Soc. (2013) 10:25–30. doi: 10.13078/jksrs.13005
32. Cho YW, Shin WC, Yun CH, Hong SB, Kim J, Earley CJ. Epidemiology of insomnia in korean adults: prevalence and associated factors. J Clin Neurol. (2009) 5:20–3. doi: 10.3988/jcn.2009.5.1.20
33. Park JH, Yoo MS, Bae SH. Prevalence and predictors of poor sleep quality in Korean older adults. Int J Nurs Pract. (2013) 19:116–23. doi: 10.1111/ijn.12047
34. Kim WJ, Joo WT, Baek J, Sohn SY, Namkoong K, Youm Y, et al. Factors associated with insomnia among the elderly in a Korean rural community. Psychiatry Investig. (2017) 14:400–6. doi: 10.4306/pi.2017.14.4.400
35. Oh K, Cho SJ, Chung YK, Kim JM, Chu MK. Combination of anxiety and depression is associated with an increased headache frequency in migraineurs: a population-based study. BMC Neurol. (2014) 14:238. doi: 10.1186/s12883-014-0238-4
36. Buysse DJ, Reynolds CF. 3rd, Monk TH, Berman SR, Kupfer DJ The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
37. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. (2012) 16:803–12. doi: 10.1007/s11325-011-0579-9
38. Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. (2011) 15:377–84. doi: 10.1007/s11325-010-0343-6
39. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. (2014) 10:210–5. doi: 10.3988/jcn.2014.10.3.210
40. Choi HS, Choi JH, Park KH, Joo KJ, Ga H, Ko HJ, et al. Standardization of the Korean Version of Patient Health Questionnaire-9 as a screening instrument for major depressive disorder. J Korean Acad Fam Med. (2007) 28:114–9.
41. Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. (2008) 49:218–23. doi: 10.1016/j.comppsych.2007.08.006
42. Lim JY, Lee SH, Cha YS, Park HS, Sunwoo S. Reliability and validity of anxiety screening scale. J Korean Acad Fam Med. (2001) 22:1224–32.
43. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. (1999) 131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002
44. Allen RP, Burchell BJ, MacDonald B, Hening WA, Earley CJ. Validation of the self-completed Cambridge-Hopkins questionnaire (CH-RLSq) for ascertainment of restless legs syndrome (RLS) in a population survey. Sleep Med. (2009) 10:1097–100. doi: 10.1016/j.sleep.2008.10.007
45. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. (2008) 61:344–9. doi: 10.1016/j.jclinepi.2007.11.008
46. Zeng LN, Zong QQ, Yang Y, Zhang L, Xiang YF, Ng CH, et al. Gender difference in the prevalence of insomnia: a meta-analysis of observational studies. Front Psychiatry. (2020) 11:577429. doi: 10.3389/fpsyt.2020.577429
47. Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. (2006) 29:85–93. doi: 10.1093/sleep/29.1.85
48. Li RH, Wing YK, Ho SC, Fong SY. Gender differences in insomnia–a study in the Hong Kong Chinese population. J Psychosom Res. (2002) 53:601–9. doi: 10.1016/S0022-3999(02)00437-3
49. Fatima Y, Doi SA, Najman JM, Mamun AA. Exploring gender difference in sleep quality of young adults: findings from a large population study. Clin Med Res. (2016) 14:138–44. doi: 10.3121/cmr.2016.1338
50. Li J, Vitiello MV, Gooneratne NS. Sleep in normal aging. Sleep Med Clin. (2018) 13:1–11. doi: 10.1016/j.jsmc.2017.09.001
51. Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. (1995) 18:425–32. doi: 10.1093/sleep/18.6.425
52. Dorffner G, Vitr M, Anderer P. The effects of aging on sleep architecture in healthy subjects. Adv Exp Med Biol. (2015) 821:93–100. doi: 10.1007/978-3-319-08939-3_13
53. Vitiello MV, Larsen LH, Moe KE. Age-related sleep change: gender and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. (2004) 56:503–10. doi: 10.1016/S0022-3999(04)00023-6
54. Pedraza S, Al Snih S, Ottenbacher KJ, Markides KS, Raji MA. Sleep quality and sleep problems in Mexican Americans aged 75 and older. Aging Clin Exp Res. (2012) 24:391–7. doi: 10.3275/8106
55. Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep. (2008) 31:383–93. doi: 10.1093/sleep/31.3.383
56. Whitney CW, Enright PL, Newman AB, Bonekat W, Foley D, Quan SF. Correlates of daytime sleepiness in 4578 elderly persons: the Cardiovascular Health Study. Sleep. (1998) 21:27–36. doi: 10.1093/sleep/21.1.27
57. Berger M, Hirotsu C, Haba-Rubio J, Betta M, Bernardi G, Siclari F, et al. Risk factors of excessive daytime sleepiness in a prospective population-based cohort. J Sleep Res. (2021) 30:e13069. doi: 10.1111/jsr.13069
58. Martynowicz H, Skomro R, Gać P, Mazur G, Porebska I, Bryłka A, et al. The influence of hypertension on daytime sleepiness in obstructive sleep apnea. J Am Soc Hypertens. (2017) 11:295–302. doi: 10.1016/j.jash.2017.03.004
59. Empana JP, Dauvilliers Y, Dartigues JF, Ritchie K, Gariepy J, Jouven X, et al. Excessive daytime sleepiness is an independent risk indicator for cardiovascular mortality in community-dwelling elderly: the three city study. Stroke. (2009) 40:1219–24. doi: 10.1161/STROKEAHA.108.530824
60. Chasens ER, Sereika SM, Weaver TE, Umlauf MG. Daytime sleepiness, exercise, and physical function in older adults. J Sleep Res. (2007) 16:60–5. doi: 10.1111/j.1365-2869.2007.00576.x
61. Jaussent I, Bouyer J, Ancelin ML, Berr C, Foubert-Samier A, Ritchie K, et al. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep. (2012) 35:1201–7. doi: 10.5665/sleep.2070
62. Roth T, Coulouvrat C, Hajak G, Lakoma MD, Sampson NA, Shahly V, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. (2011) 69:592–600. doi: 10.1016/j.biopsych.2010.10.023
63. Crowley K. Sleep and sleep disorders in older adults. Neuropsychol Rev. (2011) 21:41–53. doi: 10.1007/s11065-010-9154-6
64. Oh CM, Kim HY, Na HK, Cho KH, Chu MK. The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: a population-based study. Front Neurol. (2019) 10:849. doi: 10.3389/fneur.2019.00849
65. Alvaro PK, Roberts RM, Harris JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. (2014) 15:934–41. doi: 10.1016/j.sleep.2014.03.019
66. Luyster FS, Choi J, Yeh CH, Imes CC, Johansson AE, Chasens ER. Screening and evaluation tools for sleep disorders in older adults. Appl Nurs Res. (2015) 28:334–40. doi: 10.1016/j.apnr.2014.12.007
67. Hughes JM, Song Y, Fung CH, Dzierzewski JM, Mitchell MN, Jouldjian S, et al. Measuring sleep in vulnerable older adults: a comparison of subjective and objective sleep measures. Clin Gerontol. (2018) 41:145–57. doi: 10.1080/07317115.2017.1408734
68. Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6,800 persons over three years. Sleep. (1999) 22(Suppl. 2):S366–72.
Keywords: sleep, aging, sleep qualities, daytime sleepiness, insomnia
Citation: Hwang H, Kim KM, Yun C-H, Yang KI, Chu MK and Kim W-J (2023) Sleep state of the elderly population in Korea: Nationwide cross-sectional population-based study. Front. Neurol. 13:1095404. doi: 10.3389/fneur.2022.1095404
Received: 11 November 2022; Accepted: 16 December 2022;
Published: 09 January 2023.
Edited by:
Helena Martynowicz, Wroclaw Medical University, PolandReviewed by:
Mieszko Wieckiewicz, Wroclaw Medical University, PolandCopyright © 2023 Hwang, Kim, Yun, Yang, Chu and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Won-Joo Kim,  a3pvb0B5dWhzLmFj
a3pvb0B5dWhzLmFj
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.