
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 09 December 2022
Sec. Epilepsy
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.1077624
This article is part of the Research TopicThe Mechanism of Sudden Unexpected Death in Epilepsy and the Specific Forensic Diagnostic Indicators in Sudden Death with a Negative AutopsyView all 10 articles
Background and aims: Epilepsy is a common and chronic neurological disorder characterized by seizures that increase the risk of mortality. SUDEP is the most common seizure-related category of death. The study aimed to evaluate the key characteristics between SUDEP and not-SUDEP death cases.
Methods: A retrospective study of forensic autopsy cases from 2002 to 2021, performed by the Academy of Forensic Science (Ministry of Justice, China), identified a total of 31 deaths associated with epilepsy. We compared the different characteristics between individuals who died of SUDEP (SUDEP group) and individuals with epilepsy died suddenly due to unrelated causes (not-SUDEP group).
Results and conclusions: 13 cases met the general accepted definition of SUDEP; and 18 cases were classified as not-SUDEP. The mean age of the not-SUDEP group was significantly higher than that of the SUDEP groups (p < 0.05) and there were more cases without a clear cause of epilepsy in the SUDEP group than in the not-SUDEP group (p < 0.05). Death position differed significantly between the two groups, with more cases dying in the prone position in the SUDEP group (p < 0.05). Complete autopsies were performed in 24 of the 31 cases. There were no significant differences in heart, lungs and brain weights, or in ventricular thickness (p > 0.05) between the SUDEP and not-SUDEP groups. In addition, compared to the not-SUDEP group, the SUDEP group featured a significantly more cases with coronary lesions (grades 1-3, p < 0.05). Neuropathological lesions were identified in 12 of the 13 SUDEP cases (92.3%), cardiac lesions were present in 10 cases (76.9%) and pulmonary edema and pulmonary congestion were present in all cases. The primary cause of death in 13 of the 31 cases was seizure disorder or epilepsy. The primary mechanism of death in SUDEP group was mainly asphyxia while that in the not-SUDEP group was cardiopulmonary failure (p < 0.05). Patients in the prone position had a significantly higher risk of asphyxia than those who were not. Here, we investigated the key characteristics between SUDEP and not-SUDEP death cases, which may help to facilitate forensic diagnosis in presumed SUDEP cases.
Epilepsy is a common neurological disease that represents a serious threat to human health, affecting ~70 million people globally (1). The weighted median of the standardized death ratio (SMR) in patients with epilepsy is 2.3 in high-income countries and 2.6 in low-income countries, thus indicating a significantly higher risk of mortality than that in the general population (2). Leading causes of death in epilepsy include the sudden death of unknown causes, status of epilepsy, accidental injury, and suicide (3).
Sudden unexpected death in epilepsy (SUDEP) is defined as a sudden, unexpected death, witnessed or unwitnessed, of a person with epilepsy, for whom a complete postmortem examination does not reveal a specific cause of death (4). This nomenclature was initially defined in 1997 by Annegers (5) and (6). The definition of SUDEP was unified in 2012. According to this definition, SUDEP is defined as a category of death and can be classified into seven subtypes: (1) definite SUDEP, (2) definite SUDEP plus, (3) probable SUDEP/probable SUDEP plus, (4) possible SUDEP, (5) near-SUDEP/near-SUDEP plus, (6) not-SUDEP, and (7) unclassified (7). The new definition showed the extension and refinement of the understanding of the disease. Deaths caused by SUDEP remain a serious public health concern (8). SUDEP is the leading cause of epilepsy-related premature mortality and accounts for 8–17% of deaths among people with epilepsy (9). The calamity of SUDEP preferentially targets young people (10).
Because the diagnosis of SUDEP is made by exclusion of other causes of death, it requires a clinical history of epilepsy, witness statements, details of the scene and circumstances of death, and complete postmortem examinations including toxicology. Therefore, forensic medicine study has also played an important role in SUDEP research, and it provides many important clues to elucidate the mechanism of SUDEP as well (11). The neuropathology and cardiac pathology findings in SUDEP are the main concerns of the autopsy (12–16). However, there are no specific neuropathological and cardiac alterations that can categorically confirm SUDEP. The postmortem examination of SUDEP in the future will be an integration of clinical, pathological, and molecular genetic investigation conducted by both forensic experts and neuropathologists.
Obtaining insight into its pathophysiological mechanisms is a cardinal step toward the prevention and reduction of the incidence of SUDEP. The exact mechanism of SUDEP is unknown but postictal disturbed cardiac or respiratory physiology is implicated (17). Seizures that arise in the cortical region can spread to involve the subcortical regions of the central autonomic network. The ictal activity of the central autonomic network can disrupt the functional connectivity of this network by inhibiting or activating autonomic areas, causing diverse autonomic manifestations, including respiratory and cardiovascular dysfunction (18). Adverse effects of adenosine signaling may also potentiate a fatal outcome in the form of SUDEP by suppressing breathing and arousal in the postictal period (19).
Clinical studies on death, including SUDEP, are challenging. It can hardly be carried out in a trial, but only through patient history reviews, medical records, or surrogate measures such as cardiac and respiratory abnormalities (20). Furthermore, retrospective research is still complicated by the loss of data. Previous studies have either compared individuals who had died of SUDEP to individuals who were alive and had epilepsy (20), or compared individuals who died of SUDEP to individuals who died suddenly due to some unrelated causes without epilepsy. Therefore, in this study, we analyzed forensic autopsy cases associated with epilepsy and compared the characteristics of individuals who died of SUDEP to individuals with epilepsy who died of other causes.
This study was approved by the Academic Committee of the Academy of Forensic Science (AFS), Ministry of Justice, China. We conducted a retrospective study of all cases investigated by the AFS between 2002 and 2021. The cases, in which the cause of death was listed as a seizure or a clear medical history of epilepsy was confirmed, were sifted out from the AFS autopsy case database. Data for forensic pathological identification, including detailed investigation records, surveillance videos, medical history, and autopsy findings, had been collected by AFS, and all case information was never published in any literature.
Electronic searches revealed 31 cases for analysis. We reviewed investigation reports and autopsy findings for each of these 31 cases. Cases were then classified according to the latest definition of SUDEP (7). The definitions of each classification are described as below: (1) “definite SUDEP”: a sudden, unexpected, witnessed or unwitnessed, non-traumatic and non-drowning death, occurring in benign circumstances, in an individual with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus (seizure duration ≥30 min or seizures without recovery), in which postmortem examination does not reveal a definite cause of death; (2) “SUDEP plus”: satisfying the definition of definite SUDEP, if a concomitant condition other than epilepsy is identified before or after death, if the death may have been due to the combined effect of both conditions, and if autopsy or direct observations/recordings of terminal event did not prove the concomitant condition to be the cause of death; (3) “probable SUDEP”: same as definite SUDEP but without autopsy; (4) “possible SUDEP”: a competing cause of death is present; (5) “near-SUDEP”: a patient with epilepsy survives resuscitation for more than 1 h after a cardiorespiratory arrest that has no structural cause identified after investigation; (6) “not-SUDEP”: a clear cause of death is known; (7) “unclassified”: not possible to classify. The classification results for the 31 cases are shown in Figure 1. The deceased cases were assigned into two groups: (1) those that met the diagnostic criteria for SUDEP (either definite SUDEP or SUDEP plus) or (2) death unrelated to epilepsy (not-SUDEP). Analysis of etiology was based on the Classification of International League against Epilepsy (ILAE) (21).
Data were then analyzed from several different perspectives: (1) demographic data of the subject, such as age and gender; (2) personal information obtained from records of investigation, including medical history and history of drug or alcohol use; (3) information acquired from the evaluation of the scene and the circumstances of death such as the time of death, the location of death, and the position of the deceased when found; and (4) the cause of death and the mechanism of death.
Cases that met any of the following criteria were excluded to ensure comparability of measurements: (1) The case was an external examination only; (2) The decedent was under 14 years old; and (3) The decedent was decomposing to such a degree as to alter normal organ weights. Finally, the exclusion of 7 cases above left 24 autopsies. All of the 24 cases received a complete autopsy, including histopathological examinations and postmortem toxicological analysis (22). In each autopsy, the heart was dissected 1–2 cm above the aorta and pulmonary trunk. The heart mass was determined by weighing the fresh heart on a metric pan scale after blood and clots were removed from the heart. The epicardial fat was left intact for weighing.
The presence of anti-epileptic drugs (AEDs) was detected by gas chromatography/mass spectrometry (GC/MS). Several AEDs were routinely detected, including carbamazepine, lamotrigine, phenytoin, phenobarbitone, valproic acid, levetiracetam, hydroxycarbazepine, and primidone. For the purpose of forensic identification and this study, therapeutic concentrations were considered as follows: carbamazepine, 4–8 mg/L; lamotrigine, 3–14 mg/L; phenytoin, 10–20 mg/L; phenobarbitone, 10–30 mg/L; valproic acid, 50–100 mg/L; levetiracetam, 10–37 mg/L; zonisamide, 20–30 mg/L; topiramate, 3.4–5.2 mg/L; and hydroxycarbazepine, 12–30 mg/L (23, 24).
Statistical analyses were performed using Jamovi 2 (jamovi.org) (25) and ggstatsplot (26). We checked normal distribution with the Shapiro-Wilk test and verified the homogeneity of variances for each set of data. Normally distributed data are presented as means ± standard error, categorical data are presented as numbers (percentages), and the continuity variables that are not normally distributed are represented by M (Q1, Q3). Statistical testing involved Welch's t-test and the Mann-Whitney U-test for continuous variables and the chi-square test and Fisher's exact test for categorical variables. To predict whether death position could have exerted an impact on the mechanism of death, we used binomial logistic regression models. Statistical significance difference was defined as p < 0.05.
A total of 31 cases were classified into three groups according to the latest SUDEP definition; 7 cases (22.6%) met the definition of “definite SUDEP,” 6 cases (19.4%) were classified as “SUDEP plus” group, and the rest 18 cases (58.1%) were defined as “not-SUDEP.” The classification results for the 31 cases are shown in Figure 1.
Of the 31 cases, 22 were men and 9 were women, and the mean age at death was 42.4 ± 16.3 years (range: 17–80 years). Gender ratios did not vary significantly when compared between the SUDEP and not-SUDEP groups (p > 0.05). However, the age of the cases in the not-SUDEP group (50.1 ± 15.9 years) was significantly higher than that of the cases in the SUDEP group (31.7 ± 9.9) (p < 0.01). The age comparison results are shown in Figure 2.
In total, 11 cases were associated with epileptic lesions, including intracranial occupancy in three cases and brain trauma in eight cases. The metabolic causes of epilepsy were brain hypoxia and poisoning in four cases; 16 cases had no significant cause of epilepsy. The distribution of cases with or without definite etiology was significantly different when compared between the two groups and more cases in the SUDEP group did not have a definite etiology (p < 0.05). Table 1 shows that there were more cases (10/13) with undefined etiology of epilepsy in the SUDEP group than that in the not-SUDEP group (6/18).
Investigations indicated that 14 cases (45.2%) died in the hospital or the clinic, while 11 cases (35.5%) died at their residence. Other death locations included a jail cell, a driveway, a massage room, a working place, and in a sewer. The distribution of death locations did not differ significantly when compared between the SUDEP and not-SUDEP groups (p > 0.05), as shown in Table 1. By reviewing the case records, a total of 29 cases clearly stated the time of death; two cases did not specify the time of death. The time of death was classified as day and night (daytime was defined as 8:00 a.m. to 8:00 p.m.). No significant difference was detected in terms of the time of death when compared between the SUDEP and not-SUDEP groups (p > 0.05), as shown in Table 1. Death positions were analyzed according to case investigations and livor mortis distribution, while 28 cases had a determined death position, and 3 cases of the not-SUDEP group could not determine the death position. Results arising from the SUDEP group differed significantly from the not-SUDEP group. More cases died in the prone position in the SUDEP group (7/13) than that in the not-SUDEP group (1/15) (p < 0.05). Details of the death position are shown in Table 1.
Postmortem toxicological analysis revealed that 13 subjects (41.9%) had detectable levels of antiepileptic drugs (AEDs), including valproate (6/13), carbamazepine (6/13), oxcarbazepine (4/13), topiramate (2/13), levetiracetam (1/13), and phenytoin (1/13). Only one case had a supra-therapeutic concentration of carbamazepine; the remaining 12 cases all showed therapeutic concentrations of AEDs. Of the cases taking epilepsy drugs, six took two drugs and seven took one drug. There was no significant difference between the two groups regarding the use of AEDs (p > 0.05), as shown in Table 1. One patient had undergone surgery for epilepsy and one other case received electrotherapy. Alcohol consumption was recorded for one case just before death, and traditional Chinese medicine injections were co-administered in another case.
In total, 24 of the 31 subjects underwent a complete autopsy, including body surface examination, autopsy, and histopathological examinations.
There were no significant differences between the SUDEP and not-SUDEP groups in terms of the weights of the heart, lungs, and brains, or the ventricular thickness (p > 0.05). Further details are shown in Table 2.
Analysis showed that the SUDEP group featured a significantly higher number of cases with coronary lesions (grades 1–3) than that in the not-SUDEP group (p < 0.05); further details are shown in Figure 3.
Next, we analyzed the main pathological findings of the 13 cases in the SUDEP group. Neuropathological findings were present in 12 cases (92.3%), and four typical epileptic lesions are presented in Figure 4; the remaining cases showed no gross or microscopic abnormalities. Ten cases showed cardiac pathological changes (76.9%), most of which involved subpericardial petechiae; the next most common condition was local myocardial fibrosis. Seven cases (53.8%) had coronary artery atherosclerosis with stenosis degrees of stages I to III. All subjects showed pulmonary congestion and edema. Other pulmonary outcomes included hemorrhage and focal inflammation. Nail cyanosis and other pathological findings were also recorded and shown in Table 3.
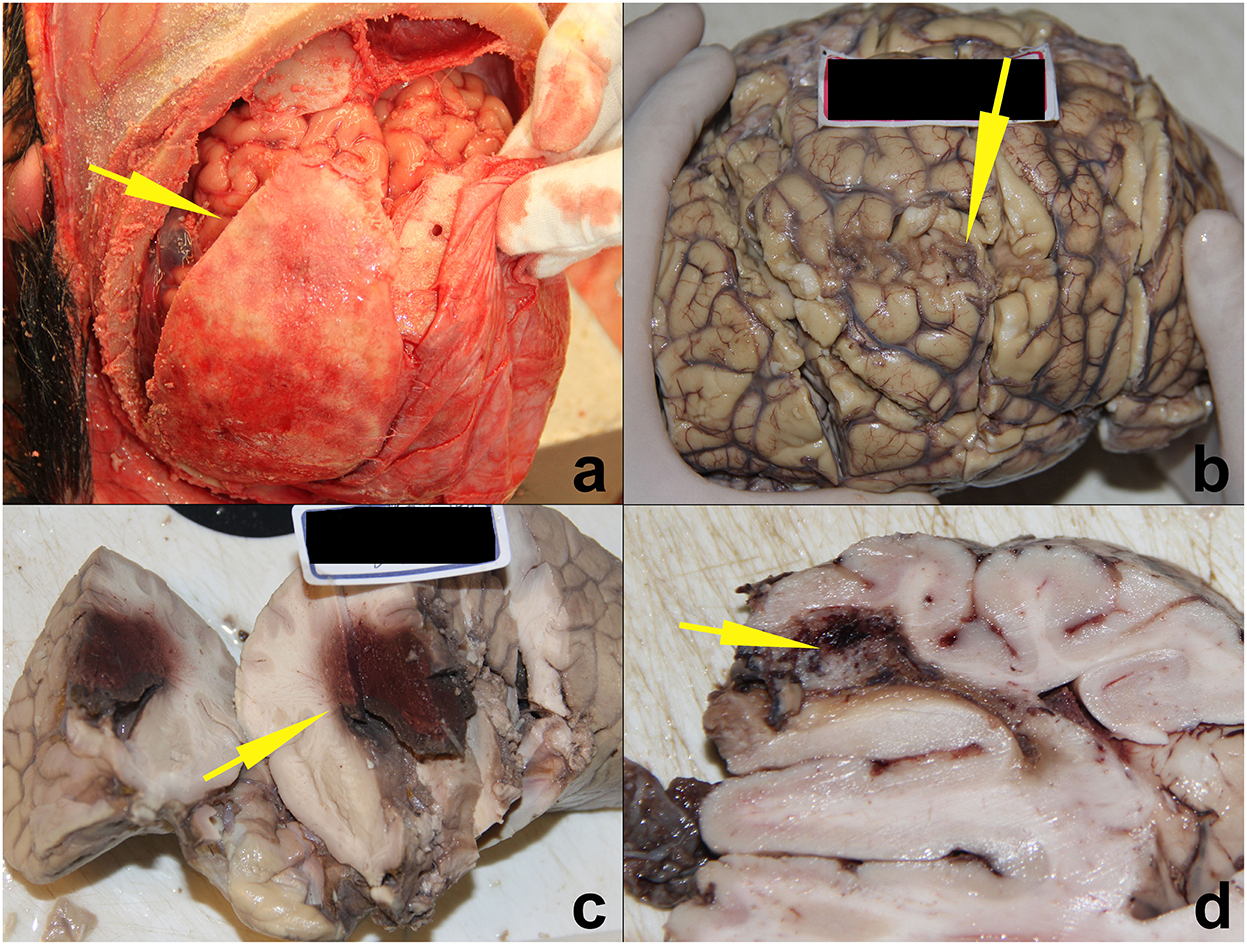
Figure 4. Four SUDEP cases with typical epileptic brain lesions. (a) Epilepsy secondary to chronic subdural hematoma ossification. (b) Epilepsy secondary to old cerebral contusions. (c) Epilepsy secondary to cerebral glioma. (d) Epilepsy secondary to vascular malformation. All lesions are indicated by yellow arrows.
Table 4 shows the causes and mechanisms of death, as identified by forensic pathologists. Of the 31 cases, SUDEP/epileptic state was listed as the primary cause of death in 14 cases. The mechanism of death was classified as cardiopulmonary failure in 15 cases, asphyxia in eight cases, central nervous system dysfunction in five cases, and sudden cardiac death in three cases.
Comparative analysis showed that there was a significant difference between the SUDEP and not-SUDEP groups in terms of the mechanisms of death (p < 0.05). The main mechanism of death in the SUDEP group was asphyxia; in the not-SUDEP group, the predominant mechanism was a cardiopulmonary failure. Comparative analyses of the mechanism of death are shown in Figure 5.
Next, we used logistic regression analyses to investigate the effect of death position on the mechanisms of death in the SUDEP group and found that death position had a significant influence on the mechanism of death by SUDEP. Patients in the prone position had a 57-fold higher risk of asphyxia than those in the non-prone position (95% confidence interval [CI]: 4.36–22.26, p = 0.002). There was a statistical difference (p < 0.05) in the classification of causes of death between the SUDEP and not-SUDEP groups, where the not-SUDEP group died mainly from cardiopulmonary failure (67%), while the SUDEP group died mostly from asphyxia (46%). Further details are shown in Figure 6.
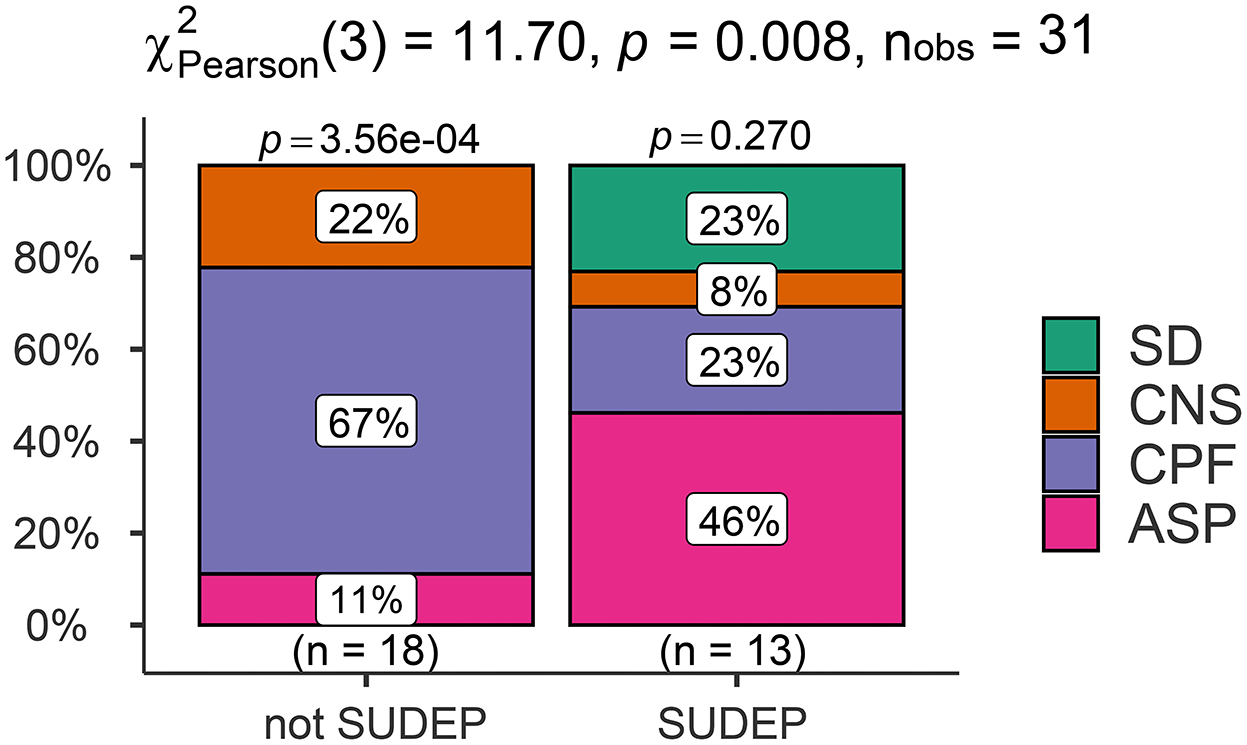
Figure 6. Comparison of the cause of death classification results in the SUDEP and not-SUDEP groups.
Epilepsy is a common and chronic neurological disorder characterized by seizures (27). Epilepsy can cause death or contribute to the circumstances of death in numerous different ways: status epilepticus, complications following seizure such as aspiration pneumonia, injury or drowning, complications of treatment, or suicide (28).
Sudden unexpected death in epilepsy (SUDEP) is defined as a sudden, unexpected death, witnessed or unwitnessed, of a person with epilepsy, where a complete postmortem examination does not reveal a specific cause of death (47). The definition of SUDEP has been revised over recent years; it is now recognized that SUDEP is actually a general term for a range of diseases. Thus, SUDEP was divided into seven groups by Nashef et al.: (1) definite SUDEP, (2) definite SUDEP plus, (3) probable SUDEP/probable SUDEP plus, (4) possible SUDEP, (5) near-SUDEP/near-SUDEP plus, (6) not-SUDEP, and (7) unclassified (7). The refined classification shows the complex presentation of SUDEP cases. The cases described in this study involved only three groups: definite SUDEP, SUDEP plus, and not-SUDEP groups; our analysis did not involve the other five classifications of SUDEP. It is clear that by definition the “probable SUDEP” and “near SUDEP” groups could not be in the forensic autopsy file records. This result may also be related to the relatively small number of cases in this study, while the small sample size of this study is due to the low autopsy rate in China. Since there is no clear conclusion that shows a different mechanism between the definite “SUDEP” and the “SUDEP plus” groups, we considered the two groups together in the experiment, which is called the SUDEP group, while those deaths with a clear cause of death were included in the not-SUDEP group. We performed a comparative analysis of the demographic profiles, death scenes, medical histories, histopathology results, and mechanisms of death between the SUDEP group and the not-SUDEP group, both of which had epilepsy. Such a grouping is significantly different from the previous studies. Previous studies have either compared individuals who had died of SUDEP to individuals who were alive and had epilepsy (20), or compared individuals who died of SUDEP to individuals without epilepsy who died suddenly due to some unrelated causes, and very few cases have directly compared individuals who died of SUDEP to individuals with epilepsy who died due to other certain causes (29). We considered this comparison to be practically valuable, which revealed another perspective for studying the SUDEP. Because all the death cases are combined with epilepsy, it can eliminate the interference of disease background to the fullest extent, and the comparative results are more convincing in terms of death mechanism.
The risk factors of SUDEP include generalized tonic-clonic seizures, the levels of anti-epileptic drugs (AEDs), frequent seizures, sleep, the prone position, reduced heart rate variability (HRV), and concomitant channelopathies (30–33). However, our analyses identified some new aspects to consider.
Previous studies suggested that nocturnal seizures and the prone position can be related to SUDEP (34, 35). There is a strong association between SUDEP and sleep, with ~70% of SUDEP cases identified during sleep (36). Our analysis of death scenes and medical history found that the SUDEP group differed from the not-SUDEP group in terms of the death position, as there were more deaths in the prone position in the SUDEP group. However, there was no significant difference between the two groups in terms of the time of death and the place of death. It should be noted that the time of death does not fully relate to whether a patient is in a state of sleep; this is because in many cases, the process of death is not witnessed. This may contribute to a divergence in the results of trials. Other case-control investigations of SUDEP postmortems also have shown no evidence for diurnal patterns with respect to SUDEP (37).
The effect of taking anti-epileptic medications on the occurrence of SUDEP may be influenced by the presence or absence of generalized tonic-clonic seizures (GTCS) episodes or sub-therapeutic levels of anti-seizure medications l (35, 38). In the present study, we found no significant difference between the SUDEP and not-SUDEP groups regarding the use of medications when considering postmortem toxicological analysis. Furthermore, we did not identify any cases with sub-therapeutic levels of anti-seizure medications; this may also suggest that the effect of AED use on SUDEP is limited without other qualifying conditions (39).
We also found some interesting phenomena when conducting demographic and etiological analyses. First, in terms of the age at death, we found that cases in the not-SUDEP group were significantly older than those in the SUDEP group (p < 0.05). Second, based on medical records, we identified more cases with undefined etiology of epilepsy in the SUDEP group than that in the not-SUDEP group. These findings might suggest that SUDEP may differ from other types of epilepsy in terms of etiology and pathogenesis (40).
A key research focus is whether patients with SUDEP have potentially fatal cardiovascular and cerebral diseases (41). Our statistical analyses found no significant difference in the weights of the heart, lungs, and brains, or the thickness of the ventricles when compared between the SUDEP and not-SUDEP groups (p > 0.05). However, the proportion of cases with coronary lesions in the SUDEP group was significantly higher than that in the not-SUDEP group (p < 0.05). However, no significant pathological changes of myocardial infarction were detected in these cases with coronary lesions, thus indicating that coronary artery disease is not the main cause of death in SUDEP but may be involved in the nosogenesis of SUDEP. Myocardial ischemia due to coronary heart disease may induce abnormal ECG activity rather than myocardial infarction which could then participate in the development of SUDEP. This is potentially supported by the findings that T-wave alternans is considered a potential biomarker for SUDEP (42–44).
Analysis of the mechanism of death is an important aspect of forensic pathology practice and is also the focus of SUDEP (43). The mechanism of SUDEP involves neuropeptidergic, serotonergic, and adenosine systems, as well as alterations of the ventrolateral medulla, amygdala, hippocampus, and central autonomic regions, orchestrating autonomic dysfunction (45). In the present study, pooled analysis of 31 cases of SUDEP identified the mechanisms of death in epileptic patients as asphyxia, cardiopulmonary dysfunction, central nervous system dysfunction, and sudden cardiac death. Our results showed that the mechanisms of death differed between the definite SUDEP and not-SUDEP groups. Most of the cases in the definite SUDEP group showed signs of asphyxia, such as nail cyanosis, hemorrhage in the bulbar conjunctiva, pulmonary pleura, and the sub-epicardium. To explain this phenomenon, we performed regression analysis on the death position most likely to cause asphyxia and found a strong correlation between death position and asphyxia, thus suggesting that the prone position was the main factor associated with asphyxia in patients with SUDEP. Ictal and postical effects on autonomic function and accidental asphyxia are commonly considered potential factors of SUDEP (18). As such, SUDEP may share mechanisms similar to sudden infant death syndrome (31).
However, due to the small number of cases, the conclusions of this study may need to be verified by further studies with larger sample sizes. In addition, due to the lack of background data, and the lack of awareness of SUDEP in many cases during the autopsy, there may be a lack of intensive and detailed pathological examinations, such as immunohistochemistry studies for mild malformations of cortical development (MCD) (46). Thus, more detailed results concerning the mechanisms of death could not be obtained.
Based on the forensic death cases, we conducted a statistical analysis of deaths in patients with epilepsy, focusing specifically on the comparative analysis of individuals who died of SUDEP (SUDEP group) to individuals with epilepsy who died due to other certain causes (not-SUDEP group). Significant differences were founded between the two groups: compared to the not-SUDEP group, the SUDEP group was younger in age; the SUDEP group has more cases with uncertain etiology of epilepsy, prone death position, and coronary lesions. The primary mechanism of death in the SUDEP group was mainly asphyxia while that in the not-SUDEP group was a cardiopulmonary failure. Additionally, asphyxia in the SUDEP group correlates significantly with the prone position. This will provide new ideas and directions for further research and forensic identification on SUDEP.
The raw data supporting the conclusions of this article will be made available by the authors.
The studies involving human participants were reviewed and approved by Academic Committee of the Academy of Forensic Science (AFS), Ministry of Justice, PR China. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
XZ and ZL conceptualized the study. ZL responsible for the methodology. XZ and JZ responsible for the formal analysis. XZ wrote the original draft. DZ supervised the research. JW provided administration services. DZ and ZL acquired the funding. All authors read and agreed to the published version of the manuscript.
This study was financially supported by grants from the National Natural Science Foundation of China (Reference: 82171872), the Natural Science Foundation of Shanghai (Reference: 21ZR1464600), the Shanghai Key Laboratory of Forensic Medicine (Reference: 17DZ2273200), the Shanghai Forensic Service Platform (Reference: 19DZ2290900), and the Central Research Institute Public Project (References: GY2020G-4 and GY2021G-5).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Thijs RD, Surges R, O'Brien TJ, Sander JW. Epilepsy in adults. Lancet. (2019) 393:689–701. doi: 10.1016/S0140-6736(18)32596-0
2. Levira F, Thurman DJ, Sander JW, Hauser WA, Hesdorffer DC, Masanja H, et al. Premature mortality of epilepsy in low- and middle-income countries: ystematic review from the mortality task force of the international league against epilepsy. Epilepsia. (2017) 58:6–16. doi: 10.1111/epi.13603
3. Mbizvo GK, Bennett K, Simpson CR, Duncan SE, Chin R. Epilepsy-related and other causes of mortality in people with epilepsy: a systemc review of systematic reviews. Epilepsy Res. (2019) 157:106192. doi: 10.1016/j.eplepsyres.2019.106192
4. Panelli RJ. SUDEP: a global perspective. Epilepsy Behav. (2020) 103:106417. doi: 10.1016/j.yebeh.2019.07.018
5. Annegers JF. United States perspective on definitions and classifications. Epilia. (1997) 38:S9–12. doi: 10.1111/j.1528-1157.1997.tb06137.x
6. Nashef L. Sudden unexpected death in epilepsy: terminology and definitions. Epilepsia. (1997) 38:S6–8. doi: 10.1111/j.1528-1157.1997.tb06130.x
7. Nashef L, So EL, Ryvlin P Tomson Tnifying the definitions of sudden unexpected death in epilepsy. Epilepsia J Int League Against Epilepsy. (2012) 53:227–33. doi: 10.1111/j.1528-1167.2011.03358.x
8. Shankar R, Donner EJ, Mclean B, Nashef L, Tomson T. Sudden unexpected death in epilepsy (SUDEP): what every neurologist should know. Epileptic Disord Int Epilepsy J Videotape. (2017) 19:1–9. doi: 10.1684/epd.2017.0891
9. Thurman DJ, Logroscino G, Be E, Hauser WA, Hesdorffer DC, Newton CR, et al. The burden of premature mortality of epilepsy in high-income countries: a systematic review from the mortality task force of the internatal league against epilepsy. Epilepsia. (2017) 58:17–26. doi: 10.1111/epi.13604
10. Devinsky O, Hesdorffer DC, Thurman DJ, Lhatoo S, Richerson G. Sudden unexpected death in epilepsy: epidemiology, mechanisms, and prevention. Lancet Neuro. (2016) 15:1075–88. doi: 10.1016/S1474-4422(16)30158-2
11. Thom M, Boldrini M, Bundock E, Sheppard MN, Devinsky O. The past, present and future challenges in epilepsy related and den deaths and biobanking. Neuropathol Appl Neurobiol. (2017) 44:32–55. doi: 10.1111/nan.12453
12. Kawamura Y, Ohashi M, Ihira M, Hashimoto S, Taniguchi K, Yoshikawa T. Nationwide survey of rotavirus-associated encephalopathy and sudden unexpected death in Japan. Brain Dev. (2014) 36:601–7. doi: 10.1016/j.braindev.2013.07.013
13. Thom M, Michalak Z, ght G, Dawson T, Hilton D, Joshi A, et al. Audit of practice in sudden unexpected death in epilepsy (SUDEP) post mortems and neuropathological findings. Neuropathol Appl Neurobiol. (2016) 42:463–76. doi: 10.1111/nan.12265
14. Nascimento FA, Tseng ZH, Palmiere C, Maleszewski JJ, Shiomi T, Mccrillis A, et al. Pulmonary and cardiac pathology in suddenxpected death in epilepsy (SUDEP). Epilepsy Behav. (2017) 73:119–25. doi: 10.1016/j.yebeh.2017.05.013
15. Neff JL, Lin PT. An unexpected finding in SUDEP involving a child: focal myocardial infarct adjacent to bundle of his. J Forensic Sci. (2017) 622–4. doi: 10.1111/1556-4029.13454
16. Ravindran K, Powell KL, Todaro M, O'Brien TJ. The pathophysiology of cardiac dysfunction in epilepsy. Epilepsy Res. (2016) 127:19–29. doi: 10.1016/j.eplepsyres.2016.08.007
17. Bhasin harma S, Ramachandrannair R. Can we prevent sudden unexpected death in epilepsy (SUDEP)? Can J Neurol Sci. (2021) 48:464–8. doi: 10.1017/cjn.2020.221
18. Tam A, Aam B, Hm C, Asm D. Sudden unexpected death in epilepsy: the neurrdio-respiratory connection. Seizure. (2019) 64:65–73. doi: 10.1016/j.seizure.2018.12.007
19. Purnell B, Murugan M, Jani R, Boison D. The good, the bad, and the deadly: adenosinergic mechanisms underlying sudden unexpected death in epilepsy. Front Neurosci. (2021) 15:708304. doi: 10.3389/fnins.2021.708304
20. Pavlova M. Sudden unexpected death in epilepsyAbout SUDEP: assessing the risk factors. Neurology. 20 94:e436–8. doi: 10.1212/WNL.0000000000008928
21. Falco-Walter JJ, Scheffer IE, Fisher RS. The new definition and classification of seizures and epilepsy. lepsy Res. (2018) 139:73–9. doi: 10.1016/j.eplepsyres.2017.11.015
22. Zhuo L, Zhang Y, Zielke HR, Levine B, Zhang X, Lin C, et al. Sudden unexpected death in epilepsy: Evaluation of forensic autopsy cases. Forensic Sci Int. (2012) 223:171–5. doi: 10.1016/j.forsciint.2012.08.024
23. Moffat AC, Osselton MD, Widdop B, Watts J. Clarke's Analysf Drugs and Poisons (Vol. 3). London: Pharmaceutical press (2011).
24. Jones AW. Disposition of Toxic Drugs and Chemicals in Man. Seal Beach, CA, USA: Biomedical Publications. (2011).
25. Alhusseini Sajid MR, Alsheikh HA, Sriwi TH, Odeh NB, Elshaer RE, et al. Evaluation of COVID-19 myths in Saudi Arabia. Saudi Med J. (2021) 42:377–83. doi: 10.15537/smj.2021.42.4.20200706
26. Patil I. Visualizations with statistical details: the ‘ggstatsplot’ approach. J Open Source Softw. (2021) 6:3167. doi: 10.21105/joss.03167
27. Milligan TA. Epilepsy: a clinical overview. Am J Med. (2021) 134:840–7. doi: 10.1016/j.amjmed.2021.01.038
28. Zhang Q, Suller-Marti A, Ding JJ, Deng G, He W, Burneo JG, et al. Epilepsy-associated death in the Southwestern Ontario: A clinicopathological correlation study. Brain Pathol. (2022) e13121. doi: 10.1111/bpa.13121. [Epub ahead of print].
29. Davis GG, Mcgwin G. Comparison of heart mass in seizure patients dying of sudden unexned death in epilepsy to sudden death due to some other cause. Am J Forensic Med Pathol. (2004) 25:23–8. doi: 10.1097/01.paf.0000113930.53578.f8
30. Tomson T, Surges R, Delamont R, Haywood S, Hesdorffer DC. Who to target in sudden unexpected death in epilepsevention and how? Risk factors, biomarkers, and intervention study designs. Epilepsia. (2016) 57:4–16. doi: 10.1111/epi.13234
31. Liebenthal JA, Wu S, Rose S, Ebersole JS, Tao JX. Association of prone position with sudden unexpected death in epilepsy. Neurology. (2015) 84:703–9. doi: 10.1212/WNL.0000000000001260
32. Nicole O, Bateman LM. Sudden unexpected death in epilepsy, peral physiology, and the SUDEP-7 inventory. Epilepsia. (2018) 59:e157–60. doi: 10.1111/epi.14552
33. Bagnall RD, Crompton DE, Petrovski S, Lam L, Cutmore C, Garry SI, et al. Exome-based analysis of cardiac arrhythmia, respiratory control, and epilepsy genn sudden unexpected death in epilepsy. Ann Neurol. (2016) 79:522–34. doi: 10.1002/ana.24596
34. Marije V, Hesdorffer DC, Sander JW, Thijs RD. Nocturnal supervision and SUDEP risk at different epilepsy care settings. Neurology. (2018) 91:e1508 doi: 10.1212/WNL.0000000000006356
35. Eslami V, Molina DK, Szabó CK. Definite SUDEP population in Bexar County, Texas: a 36-year data registry. Epilepsy Behav. (2021) 121:108005. doi: 10.1016/j.yebeh.2021.108005
36. Ali A, Wu S, Issa NP, Rose S, Towle VL, Warnke P, et al. Association of sleep with sudden unexpected death in epilepsy. Epilepshav. (2017) 76:1–6. doi: 10.1016/j.yebeh.2017.08.021
37. Bleasel A. Reader response: temporal trends and autopsy findings of SUDEP based on medicolegal investigations in the United Statesurology. (2021) 97:350–1. doi: 10.1212/WNL.0000000000012433
38. Lee JW. Sometimes, more is more: antiseizure medication polytherapy is associated with decreased SUDEP risk:. Epilepsy Curr. (2021) 21:90–2. doi: 10.1177/1535759720988546
39. Hesdorffer DC, Tomson T, Benn E, Sander JW, Nilsson L, Langan Y, et al. Do antiepileptic drugs or ralized tonic-clonic seizure frequency increase SUDEP risk? A combined analysis. Epilepsia. (2012) 53:249–52. doi: 10.1111/j.1528-1167.2011.03354.x
40. Surges R, Sperling MR, Degiorgio CM. Editorial: sudden unexpected death in epilepsy: bio-markers, mechanisms, risk identification and preven. Front Neurol. (2019) 10: 1277. doi: 10.3389/fneur.2019.01277
41. Akyüz E, Uner AK, Kklü B, Arul A, Shaikh MF. Cardiorespiratory findings in epilepsy: a recent review on outcomes and pathophyogy. J Neurosci Res. (2021) 99:2059–73. doi: 10.1002/jnr.24861
42. Marcantoni I, Cerquetti V, Cotechini V, Lattanzi M, Burattini L. T-wave alternans in partial epileptic patients. in 2018 Computing in Cardiology Conference (CinC), vol. (2019). p. 1–4. doi: 10.22489/CinC.2018.043
43. Cai Y, Ding J, Wang X. Research progress of sudden unexpected death in epilepsy. Chin J Neurol. (2020) 53:631–5. doi: 10.3760/cma.j.cn113694-20191023-00653
44. Strzelczyk, A., Adjei P., Scott C. A., Bauer S., Rose F., Walker M. C., et al. (2011). post-ictal increase in T-wave alternans after generalized tonic-clonic seizures. Epilepsia:2112–7. doi: 10.1111/j.1528-1167.2011.03266.x
45. Patodia S, Somani A, Thom M. Review: neuropathology findings in autonomic brain regions in SUDEP and future research directions. Auteurosci. (2021) 235:102862. doi: 10.1016/j.autneu.2021.102862
46. Liu JY, Ellis M, Brooke-Ball H, De Tisi J, Eriksson SH, Brandner S, et al. High-throughput, automated quantification of white matter neurons in mild malformation of cortical developmen epilepsy. Acta Neuropathol Commun. (2014) 2:1–10. doi: 10.1186/2051-5960-2-72
Keywords: sudden unexpected death in epilepsy (SUDEP), forensic pathology, autopsy, post-mortem findings, cause of death
Citation: Zhang X, Zhang J, Wang J, Zou D and Li Z (2022) Analysis of forensic autopsy cases associated with epilepsy: Comparison between sudden unexpected death in epilepsy (SUDEP) and not-SUDEP groups. Front. Neurol. 13:1077624. doi: 10.3389/fneur.2022.1077624
Received: 23 October 2022; Accepted: 14 November 2022;
Published: 09 December 2022.
Edited by:
Beixu Li, Shanghai University of Political Science and Law, ChinaReviewed by:
Xie Yuquan, Shanghai Jiao Tong University, ChinaCopyright © 2022 Zhang, Zhang, Wang, Zou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianhua Zhang, emhhbmdqaEBzc2ZqZC5jbg==; Donghua Zou, em91ZGhAc3NmamQuY24=; Zhengdong Li, bHpkYWR2QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.