- 1Department of Molecular Medicine and Medical Biotechnology, Federico II University of Naples, Naples, Italy
- 2Multiple Sclerosis Clinical Unit, Federico II University Hospital, Naples, Italy
- 3Occupational Health Unit, Department of Public Health, Federico II University of Naples, Naples, Italy
- 4Department of Public Health, Federico II University of Naples, Naples, Italy
- 5Department of Primary Care and Public Health, Imperial College, London, United Kingdom
- 6Department of Neuroscience, Reproductive Science and Odontostomatology, Federico II University of Naples, Naples, Italy
Introduction: Unemployment can directly affect social status and identity. Assessing and adjusting determinants of early working impairments in a chronic disease can thus reduce its long-term burden. Hereby, we aim to evaluate differences in occupational history and early working impairments between people with multiple sclerosis (MS) and healthy workers.
Methods: This is a cross-sectional study comparing 71 workers with MS [age 41.7 ± 9.4 years; females 59.1%; EDSS 2.0 (1.0–6.0)] and 71 controls (age 42.6 ± 11.9 years; females 33.8%). All participants filled in Work Ability Index (WAI), Work Productivity and Activity Impairment (WPAI), European Questionnaire for Quality of Life (EuroQoL), Beck Depression Inventory II (BDI-II), and Pittsburgh Sleep Quality Index (PSQI). In MS, we further collected expanded disability status scale (EDSS), MS Questionnaire for Job difficulties (MSQ-Job), Fatigue severity scale (FSS), and the Brief International Cognitive Assessment for MS (BICAMS).
Results: Workers with MS were more working disabled (p < 0.01), less exposed to workplace risks (p < 0.01), and more limited in fitness to work (p = 0.01), compared with controls. On linear regression models adjusted by age, sex, education, and type of contract, people with MS had worse WAI (Coeff=−5.47; 95% CI = −7.41, −3.53; p < 0.01), EuroQoL (Coeff = −4.24; 95% CI = −17.85, −6.50; p < 0.01), BDI-II (Coeff = 3.99; 95% CI = 2.37, 7.01; p < 0.01), and PSQI (Coeff = 4.74; 95% CI = 3.13, 7.61; p < 0.01), compared with controls, but no differences in WPAI (p = 0.60). EuroQoL, BDI-II, and PSQI were equally associated with both WAI and WPAI in MS and controls (all p< 0.01). In MS, worse MSQJob was associated with higher EDSS (Coeff = 5.22; 95% CI = 2.24, 7.95; p < 0.01), progressive disease (Coeff = 14.62; 95% CI = 5.56, 23.69; p < 0.01), EuroQoL (Coeff = 4.63; 95% CI = 2.92, 6.35; p < 0.01), FSS (Coeff = 0.55; 95% CI = 0.38, 0.72; p < 0.01), and cognitive impairment (Coeff = 4.42; 95% CI = 0.67, 8.22; p = 0.02).
Discussion: Early factors associated with working difficulties in MS include disability, fatigue, depression, and cognitive dysfunction. Early identification of clinical features potentially causing working difficulties should be considered to enhance job retention, along with targeted prevention and protection measures.
Introduction
Multiple sclerosis (MS) is a chronic and potentially highly-disabling disease of the central nervous system, which can lead to physical and cognitive impairment, including walking difficulties, fatigue, poor balance, bladder and bowel dysfunction, reduced visual acuity, mood changes, and impaired cognition, (1). Symptoms can present in the form of relapses, followed by a recovery period [relapsing-remitting MS (RRMS)], or as gradual progression of disability, either preceded by relapses [secondary progressive MS (SPMS)] or not [primary progressive MS (PPMS)] (2). The MS natural history has changed thanks to the use of disease modifying treatments (DMTs), which primarily target relapses, but also affect disability outcomes in the long term (3).
MS holds significant psychological, physical, financial and social burden on patients, their caregivers, and healthcare services (4–6). The heavy financial burden of MS is related to young age at onset (usually around 30 years of age), variety of chronic symptoms, and subsequently high unemployment rates (7). Indeed, about 50% of workers with MS suffer from reduced working abilities from disease onset (e.g., scaling down from full-time to part-time work), and will eventually lose (or quit) their job (8–11). Exclusion from the workplace is responsible for worsening social status and finances, thus affecting health outcomes in MS (12). The main factors potentially associated with unemployment are progressive disease course, motor disability, fatigue, mood changes, and cognitive impairments (9, 11, 13–17). Nevertheless, data on work ability and occupational difficulties related to MS are rather limited. Also, most studies compared demographic and clinical variables between employed and unemployed people with MS, with potential bias coming from largely different populations (e.g., disease duration, disability) (12). As such, in the present study, we specifically focused on workers with MS to evaluate differences in occupational history and early working impairments (e.g., ability, productivity and activity), when compared with healthy workers as controls, and to define clinical correlates of MS-related perceived working difficulties. Identifying determinants of early working impairments in employed people with MS can direct work retention strategies, ultimately reducing the long-term burden of this chronic disease.
Methods
Study design
This is a cross-sectional study comparing workers with MS and healthy workers as controls. The study was conducted at the MS Unit and at the Occupational Health Unit, of the Federico II University Hospital, Naples, Italy. The study was approved by Ethics Committee, at Federico II University Hospital, Naples, Italy (355/19), and all recruited subjects signed informed consent authorizing the use of anonymized data, in line with data protection regulation (GDPR EU2016/679). The study was performed in accordance with good clinical practice and Declaration of Helsinki.
Study setting and participants
We included people with MS, consecutively recruited from Feb 2021 (until the reaching of the recruitment target, as from power calculation), according to the following inclusion criteria: (1) diagnosis of MS (18); (2) employment age (18–65 years); (3) employment in the previous 6 months; and exclusion criteria: (1) any concomitant condition, disease or treatment potentially affecting employment; (2) relapses in the previous 3 months.
We also recruited consecutively a group of healthy controls within the same age range (with a case:control matching ratio of 1:1), from Feb 2021 (until the reaching of the recruitment target, as from power calculation), while attending the same hospital within the same period for their scheduled visit at the Occupational Health Unit, in accordance with Italian legislation (Legislative Decree n. 81/2008) on the protection of health and safety in the workplace. The Occupational Health Unit regularly sees healthy workers from a number of public and private institutions, thus providing heterogeneous case mix.
Data collection was conducted by MS specialists with the support of Occupational Health specialists and neuropsychologists, as appropriate.
Main variables of interest
To measure work ability and work productivity and activity impairment, people with MS and controls were required to fill in the following questionnaires:
- Work Ability Index questionnaire (WAI) (19), with higher scores indicating better work ability;
- Work Productivity and Activity Impairment Questionnaire: General Health questionnaire (WPAI) (20), with higher scores indicating better work productivity and activity.
To measure MS-related perceived difficulties in work-related tasks, people with MS were required to fill in the following questionnaire:
- MS Questionnaire for Job difficulties (MSQ-Job) (7), with higher percent scores indicating worse perception of difficulties in work-related tasks;
Endpoints in people with MS and controls
We collected demographics (age, sex), education (highest educational attainment), and occupational history, using a structured questionnaire, as from the clinical practice at the Occupational Health Unit, in people with MS and controls. In detail, occupational history included the following variables: formal acknowledgment of working disability status, percent of disability status (with higher scores indicating higher disability), type of contract (e.g., permanent, temporary, self-employed), occupational risk factors (e.g., physical, ergonomic, biological, chemical, etc.), and formal limitations in the fitness to work (depending on both working disability status and exposure to specific occupational risk factors). We also classified working activity using the Italian Institute of Statistics classification (ISTAT – Nomenclatura e classificazione delle Unità Professionali), which includes: (1) law makers, businessmen, and managers; (2) intellectual, scientific and high-specialization work; (3) technical work; (4) office executive work; (5) qualified work in commercial activities and services; (6) craftsmen, skilled workers, and farmers; (7) System operators, workers of fixed and mobile machinery, and vehicle drivers; (8) Unqualified work; (9) armed forces.
Also, people with MS and controls were required to fill in the following questionnaires:
- European Questionnaire for Quality of Life – 5 Domains (EuroQoL) (21), for evaluating impairments in daily activities and percent rating of quality of life (we collected only the latter in controls, who would have had no significant impairments);
- Beck Depression Inventory II (BDI-II) (22), with higher scores indicating worse depression;
- Pittsburgh Sleep Quality Index (PSQI) (23), with higher scores indicating worse sleep quality.
MS specialists, MS nurses, and Occupational Health specialists were available to people with MS and controls while filling in the questionnaires, as needed.
Endpoints in people with MS
In people with MS, we collected disease duration (time from reported disease onset to baseline assessment), expanded disability status scale (EDSS), clinical subtype (RRMS, SPMS and PPMS; for statistical purposes SPMS and PPMS were grouped), and DMTs (grouped into first and second line DMTs). EDSS was categorized into <3.5 and >4.0 to identify people with MS without and with walking impairment. Moreover, workers with MS were also administered the following questionnaire and neuropsychological tests:
- Fatigue severity scale (FSS) (24), with higher scores indicating worse fatigue;
- Brief International Cognitive Assessment for MS(BICAMS) neuropsychological battery, which includes the following tests: the Symbol Digit Modalities Test (SDMT), evaluating attention and information processing speed; the California Verbal Learning Test-II (CVLT-II), evaluating memory and verbal learning; and the Brief Visuospatial Memory Test-Revised (BVMTR), evaluating visuo-spatial learning (25). Results were corrected for age, sex, and education, according to the Italian normative values. We then calculated the corresponding cerebral functional system (FS) score (0 corresponds to normal BICAMS tests, ≥1 corresponds to at least one impaired BICAMS test), as from previous studies (26).
Study size and power analysis
Considering a normal distribution of variables to be analyzed in regression model (including one dependent variable and four covariates), given a 10% minimum detectable effect size, a two-sided tail and a 5% α error, a sample of 142 individuals (71 cases and 71 controls) would be able to achieve 98% power.
Statistical methods
Results are presented as mean (standard deviation), median (range), or number (percent), as appropriate. Differences in demographics and occupational history in people with MS and controls were evaluated using t-test, chi-square test and Fisher's exact test, as appropriate.
Differences between MS cases and controls were evaluated using linear regression models including each scale (WAI, WPAI, EuroQoL, BDI-II, PSQI), in turn, as dependent variable, and disease status as independent variable (people with MS vs. controls). Then, correlates of working ability (WAI), productivity and activity impairment (WPAI) were evaluated using linear regression models including each of these scales (WAI, WPAI), in turn, as dependent variable, and potential correlates (EuroQoL, BDI-II, PSQI), in turn, as independent variable; we also included an interaction term between disease status (people with MS vs. controls) and potential correlates (EuroQoL, BDI-II, PSQI), in turn, to evaluate changes in these associations between people with MS and controls.
Correlates of MS-related perceived difficulties in work-related tasks were evaluated using linear regression models including MSQJob as dependent variable, and each additional clinical variable (disease duration, EDSS, walking impairment on EDSS, clinical subtype, DMT, EuroQoL, FSS, SDMT, CVLT, BVMRT, cerebral functional system), in turn, as independent variable.
Univariate linear regression models were preliminarily run to evaluate associations between main variables of interests and study endpoints, in turn. We selected age, sex, education, and type of contract as covariates, that were included in all statistical models.
Distribution of variables and residuals was checked using both graphical and statistical methods. Results are reported as coefficients (Coeff), 95% confidence intervals (95% CI), and p-values, as appropriate. Statistical analyses were performed using Stata 17.0.
Result
We included 71 people with MS and 71 controls. Demographics and occupational history in subjects with MS and controls are reported in Table 1. MS workers had similar age, when compared with controls (p = 0.61), but were more frequently females (p < 0.01), less educated (p = 0.01), more working disabled (p < 0.01), less exposed to occupational risk factors (p < 0.01), and more limited in fitness to work (p = 0.01) (Table 1).
Working impairment (e.g., ability, productivity and activity) of people with MS and controls, and their associations with clinical features (e.g., quality of life, depression, quality of sleep) are reported in Table 2. People with MS had worse WAI (Coeff = −5.47; 95% CI = −7.41, −3.53; p < 0.01), EuroQoL (Coeff = −4.24; 95% CI = −17.85, −6.50; p < 0.01), BDI-II (Coeff = 3.99; 95% CI = 2.37, 7.01; p < 0.01), and PSQI (Coeff = 4.74; 95% CI = 3.13, 7.61; p < 0.01), compared with controls, while no difference in WPAI was found (Coeff = −1.62; 95% CI = −7.82, 4.57; p = 0.60). EuroQoL, BDI-II, and PSQI were associated with both WAI and WPAI (all p < 0.01); however, when evaluating differences between people with MS and controls in these associations using interaction terms, only the association between EuroQoL and WAI was less strong in people with MS, when compared with controls (p < 0.01) (Table 2).
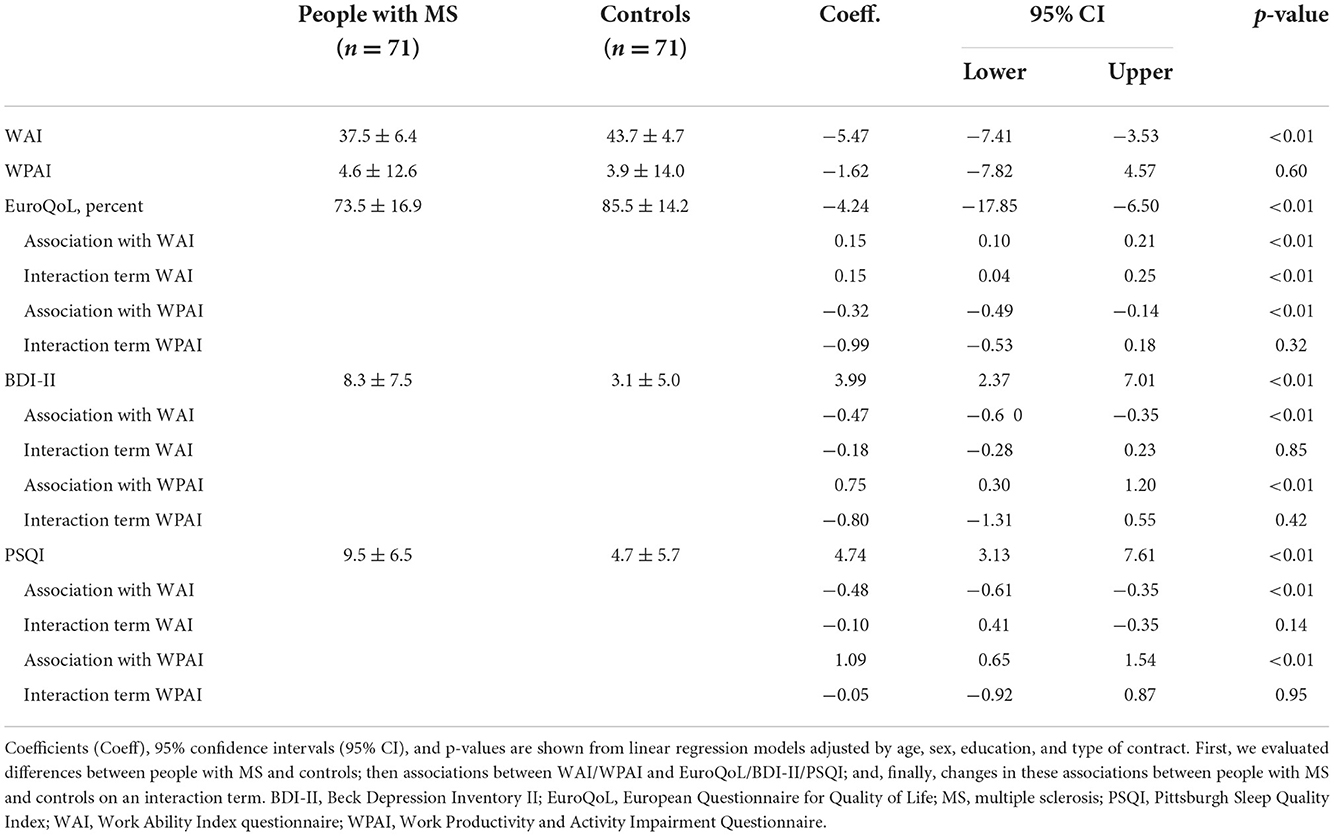
Table 2. Working impairment in people with MS and controls, and their associations with clinical features.
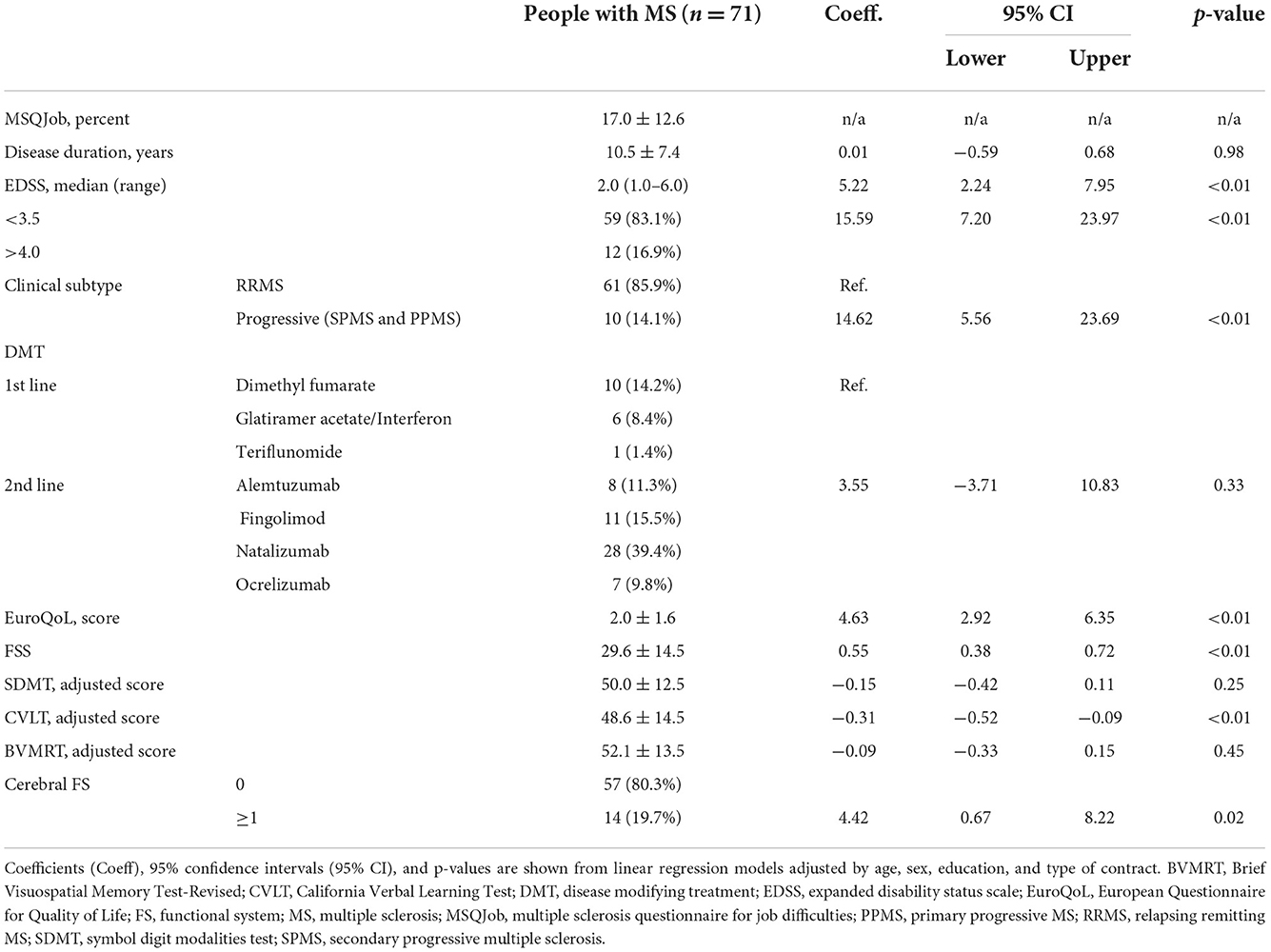
Clinical features of workers with MS, and their associations with perceived work-related difficulties (MSQJob) are reported in Table 3. Worse MSQJob was associated with higher EDSS (Coeff = 5.22; 95% CI = 2.24, 7.95; p < 0.01), walking impairment (EDSS > 4.0) (Coeff = 5.59; 95% CI = 7.20, 23.97; p < 0.01), progressive disease subtype (Coeff = 14.62; 95% CI = 5.56, 23.69; p < 0.01), EuroQoL (Coeff = 4.63; 95% CI = 2.92, 6.35; p < 0.01), FSS (Coeff = 0.55; 95% CI = 0.38, 0.72; p < 0.01), CVLT (Coeff = −0.31; 95% CI = −0.52, −0.09; p < 0.01), and MS-related cerebral functional system involvement (Coeff = 4.42; 95% CI = 0.67, 8.22; p = 0.02) (Table 3).
Discussion
In the present study, we showed that, working ability, productivity and activity impairment are associated with quality of life, depressive symptoms, and sleep quality in both MS and age-matched controls, though overall working ability is lower in people with MS. In particular, determinants of perceived work-related difficulties in MS are disability, walking impairment, progressive symptoms, lower quality of life, fatigue and cognitive dysfunction. Of note, we specifically focused on employed people with MS, rather than on unemployment, and, thus, our work aims at increasing awareness on determinants of early working impairments, and at considering medications, rehabilitation, and specific working adaptations to tackle employability in clinical practice (16). The baseline level of work productivity is associated with work productivity trajectories over time (11), and, thus, variables associated with working difficulties should be identified and targeted as soon as possible during the course of the disease.
We showed that employed people with MS have lower working ability, when compared with controls, but are able to keep up with requested working productivity and activity, possibly thanks to the acknowledgment of working disability and subsequent arrangements (e.g., reduced or modified exposure to selected occupational risk factors). In previous studies, there was poor awareness on the tools to assist people with MS in retaining employment (27), while this does not seem the case in our population. Over the disease course, there is a progressive reduction of occupational activities, with up to 50% patients with MS being unemployed within 10 years from disease onset (8, 9, 27–29). As such, the employability of workers with MS should be preserved by adaptation and prevention of working conditions (e.g., ergonomic and technical aspects of the workplace) based on the individual clinical manifestations of the disease (11). In a recent survey, Italian occupational physicians reported on difficulties in rating fitness to work in people with MS (30), and, thus, we hope that our study will raise awareness on the opportunity to design and implement special and reasonable accommodations for MS workers in order to meet their individual needs, according to their clinical features.
Among the novelties of our study, we included both people with MS and controls, and showed that quality of life, depressive symptoms and quality of sleep were worse in people with MS, when compared with controls, but were equally associated with working activity and capacity (productivity and ability). These results suggest that, though quantitatively different, people with MS and controls share qualitatively similar correlates of working impairment. As such, early identification and clinical management of worsening quality of life, depression and sleep, along with subsequent working adaptations, may contribute to improve productivity and to retain employment in individuals with MS, as well as in otherwise healthy workers (10, 11).
Looking at MS-specific factors, in our study, self-perceived difficulties in work-related tasks were associated with higher disability (especially walking impairment), progressive disease subtype, fatigue and cognitive dysfunction, especially in relation to verbal learning and memory. These results are in line with previous studies showing associations between unemployment and mood changes (11, 13), fatigue (8, 13, 28), motor disability (8, 13, 28, 31, 32), and cognitive dysfunction (32). Intriguingly, we specifically focused on workers with MS, and decided to evaluate determinants of perceived working difficulties, which were ultimately not different from actual correlates of unemployment. In keep with this, previous studies showed associations between work difficulties and mood changes (14, 33, 34), fatigue (11, 14, 34), motor disability (11, 14, 33), and cognitive dysfunction (11, 14, 35). In a previous study also using the BICAMS, attention and processing speed (SDMT) was associated with working ability (35), while we found an association for verbal learning and memory (CVLT). While we acknowledge that the SDMT is a marker of overall cognitive function in MS (36), in our study, we computed the cerebral FS score based on overall BICAMS results, which also reflects cognitive impairment (26), and was associated with working difficulties. Not least, working difficulties can be associated with a variety of cognitive deficits based on the actual tasks. We cannot exclude a similar association in controls as well, but unfortunately did not have availability of cognitive variables.
Our study is limited by the single-center design and the relatively small sample size, though sufficiently powered to show consistently significant associations. Controls were recruited based on the age range, which is a main determinant of employability; however, cases and controls were not balanced in sex and education, which were included as covariates in the statistical models. As such, notwithstanding statistical adjustments, we have to acknowledge the risk of bias coming from sex and education differences. Also, our cross-sectional design does not allow causal inference, nor the evaluation of longitudinal changes in working difficulties, also in relation to treatments (20). Generalizability of our results is definitely limited to countries with similar working retention policies and universal healthcare coverage (e.g., Europe, Canada) (17, 37).
In conclusion, our study encourages the early identification and management of clinical features potentially causing an impairment of working ability in people with MS, along with the implementation of individually targeted prevention and protection measures on the workplace. Based on our results, MS specialists should primarily consider disability, fatigue, depression, and cognitive impairment, and liaise with occupational physicians to identify the most suitable arrangements, counseling programs and strategies to support workers with MS. In the future, multidisciplinary patient/worker management teams, including MS specialists, occupational physicians and other healthcare professionals (38, 39), should be considered to protect the health and the employment of vulnerable people with MS.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Federico II University Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MM and LF contributed to data collection, data analysis and interpretation, manuscript preparation, and revision. VB and II contributed to data interpretation, manuscript revision, and coordination. RP and MT contributed to data analysis and interpretation and manuscript revision. FFa, FFi, MF, RL, and LR contributed to data collection, database preparation, and manuscript revision.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a past co-authorship with the authors VB and MM.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thompson AJ, Baranzini SE, Geurts J, Hemmer B, Ciccarelli O. Multiple sclerosis. Lancet. (2018) 391:1622–36. doi: 10.1016/S0140-6736(18)30481-1
2. Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen PS, Thompson AJ, et al. Defining the clinical course of multiple sclerosis : the 2013 revisions. Neurology. (2014) 83:278–86. doi: 10.1212/WNL.0000000000000560
3. De Angelis F, John NA, Brownlee WJ. Disease-modifying therapies for multiple sclerosis. BMJ. (2018) 363:1–10. doi: 10.1136/bmj.k4674
4. Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. (2011) 21:718–79. doi: 10.1016/j.euroneuro.2011.08.008
5. Moccia M, Palladino R, Lanzillo R, Triassi M, Brescia Morra V. Predictors of the 10-year direct costs for treating multiple sclerosis. Acta Neurol Scand. (2017) 135:522–8. doi: 10.1111/ane.12630
6. Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler. (2017) 23:1123–36. doi: 10.1177/1352458517694432
7. Raggi A, Giovannetti A, Schiavolin S, Confalonieri P, Brambilla L, Brenna G, et al. Development and validation of the multiple sclerosis questionnaire for the evaluation of job difficulties (MSQ-Job). Acta Neurol Scand. (2015) 132:226–34. doi: 10.1111/ane.12387
8. Lunde HMB, Telstad W, Grytten N, Kyte L, Aarseth J, Myhr K-M, et al. Employment among patients with multiple sclerosis-a population study. PLoS ONE. (2014) 9:e103317. doi: 10.1371/journal.pone.0103317
9. Findling O, Baltisberger M, Jung S, Kamm CP, Mattle HP, Sellner J. Variables related to working capability among swiss patients with multiple sclerosis — a cohort study. PLoS ONE. (2015) 10:e0121856. doi: 10.1371/journal.pone.0121856
10. Glanz BI, Dégano IR, Rintell DJ, Chitnis T, Weiner HL, Healy BC. Work productivity in relapsing multiple sclerosis: associations with disability, depression, fatigue, anxiety, cognition, and health-related quality of life. Value Heal. (2012) 15:1029–35. doi: 10.1016/j.jval.2012.07.010
11. Bessing B, Hussain MA, Claflin SB, Chen J, Blizzard L, Van DP, et al. Work productivity trajectories of Australians living with multiple sclerosis : a group-based modelling approach. Mult Scler Relat Disord. (2021) 54:103131. doi: 10.1016/j.msard.2021.103131
12. Dobson R, Rice DR, Marie D, Horne R, Learmonth Y, Mateen FJ. Social determinants of health in multiple sclerosis. Nat Rev Neurol. (2022) 18:723–34. doi: 10.1038/s41582-022-00735-5
13. Contentti EC, Lopez PA, Pettinicchi JP, Tkachuk V, Balbuena ME, Caride A. Employment status in people with relapsing multiple sclerosis from Argentina : impact of disability and neuropsychological factors. Work. (2021) 68:1171–7. doi: 10.3233/WOR-213446
14. Bakirtzis C, Artemiadis A, Nteli E, Boziki MK, Karakasi M, Honan C, et al. A Greek validation study of the multiple sclerosis work difficulties questionnaire-23. Healthcare. (2021) 9:897. doi: 10.3390/healthcare9070897
15. Alberto R, Giovannetti AM, Schiavolin S, Brambilla L, Brenna G, Confalonieri PA, et al. Older age, higher perceived disability and depressive symptoms predict the amount and severity of work-related difficulties in persons with multiple sclerosis. Disabil Rehabil. (2019) 41:2255–63. doi: 10.1080/09638288.2018.1461937
16. Raggi A, Covelli V, Schiavolin S, Scaratti C, Leonardi M, Willems M. Work-related problems in multiple sclerosis: a literature review on its associates and determinants. Disabil Rehabil. (2016) 38:936–44. doi: 10.3109/09638288.2015.1070295
17. Ellenberger D, Parciak T, Brola W, Hillert J, Middleton R, Stahmann A, et al. Comparison of employment among people with multiple sclerosis across Europe. Mult Scler J Exp Transl Clin. (2022) 8:20552173221090653. doi: 10.1177/20552173221090653
18. Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. (2018) 17:162–73. doi: 10.1016/S1474-4422(17)30470-2
19. Guidi S, Bagnara S, Fichera GP. The HSE indicator tool, psychological distress and work ability. Occup Med. (2012) 62:203–9. doi: 10.1093/occmed/kqs021
20. Capra R, Morra VB, Mirabella M, Gasperini C, Scandellari C, Totaro R, et al. Natalizumab is associated with early improvement of working ability in relapsing-remitting multiple sclerosis patients: WANT observational study results. Neurol Sci. (2021) 42:2837–45. doi: 10.1007/s10072-020-04838-z
21. Battaglia M, Kobelt G, Ponzio M, Berg J, Capsa D, Dalén J. New insights into the burden and costs of multiple sclerosis in Europe: results for Italy. Mult Scler J. (2017) 23:104–16. doi: 10.1177/1352458517708176
22. Solaro C, Trabucco E, Signori A, Martinelli V, Radaelli M, Centonze D, et al. Depressive symptoms correlate with disability and disease course in multiple sclerosis patients: an Italian multi-center study using the beck depression inventory. PLoS ONE. (2016) 11:1–9. doi: 10.1371/journal.pone.0160261
23. Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM, et al. Validity of the italian version of the pittsburgh sleep quality index (PSQI). Neurol Sci. (2013) 34:511–9. doi: 10.1007/s10072-012-1085-y
24. Ottonello M, Pellicciari L, Giordano A, Foti C. Rasch analysis of the fatigue severity scale in Italian subjects with multiple sclerosis. J Rehabil Med. (2016) 48:597–603. doi: 10.2340/16501977-2116
25. Goretti B, Niccolai C, Hakiki B, Sturchio A, Falautano M, Minacapelli E, et al. The brief international cognitive assessment for multiple sclerosis (BICAMS): normative values with gender, age and education corrections in the Italian population. BMC Neurol. (2014) 14:171. doi: 10.1186/s12883-014-0171-6
26. Saccà F, Costabile T, Carotenuto A, Lanzillo R, Moccia M, Pane C, et al. The EDSS integration with the brief international cognitive assessment for multiple sclerosis and orientation tests. Mult Scler. (2017) 23:1289–96. doi: 10.1177/1352458516677592
27. Fantoni-Quinton S, Kwiatkowski A, Vermersch P, Roux B, Hautecoeur P, Leroyer A. Impact of multiple sclerosis on employment and use of job-retention strategies: the situation in France in 2015. J Rehabil Med. (2016) 48:535–40. doi: 10.2340/16501977-2093
28. Llorian ER, Zhang W, Khakban A, Patten S, Traboulsee A, Oh J, et al. Productivity loss among people with early multiple sclerosis: A Canadian study. Mult Scler. (2022) 28:1414–23.
29. Vanotti S, Eizaguirre M, Ciufia N, Yastremiz C, Roman M, Martinez Canyazo C, et al. Employment status monitoring in an Argentinian population of patients with multiple sclerosis : particularities of a developing country. Work. (2021) 68:1121–31. doi: 10.3233/WOR-213442
30. Persechino B, Fontana L, Buresti G, Fortuna G, Valenti A, Iavicoli S. Improving the job-retention strategies in multiple sclerosis workers : the role of occupational physicians. Ind Health. (2019) 57:52–69. doi: 10.2486/indhealth.2017-0214
31. Ford HL, Wicks CR, Stroud A, Tennant A. Psychological determinants of job retention in multiple sclerosis. Mult Scler. (2019) 25:419–26. doi: 10.1177/1352458518754362
32. Srpova B, Sobisek L, Novotna K, Uher T, Friedova L, Vaneckova M, et al. The clinical and paraclinical correlates of employment status in multiple sclerosis. Neurol Sci. (2022) 43:1911–20. doi: 10.1007/s10072-021-05553-z
33. Vlahiotis A, Sedjo R, Cox ER, Burroughs TE, Rauchway A, Lich R. Gender differences in self-reported symptom awareness and perceived ability to manage therapy with disease-modifying medication among commercially insured multiple sclerosis patients. J Manag Care Pharm. (2010) 16:206–16. doi: 10.18553/jmcp.2010.16.3.206
34. van der Hiele K, van Gorp DAM, van Egmond EEA, Jongen PJ, Reneman MF, van der Klink JJL, et al. Self-reported occupational functioning in persons with relapsing-remitting multiple sclerosis: does personality matter? J Neurol Sci. (2021) 427:117561. doi: 10.1016/j.jns.2021.117561
35. Schreiber M, Ullrich J, Penner M. The brief international cognitive assessment in multiple sclerosis (BICAMS): results from the German validation study. J Neurol. (2018) 265:2587–93. doi: 10.1007/s00415-018-9034-1
36. Moccia M, Lanzillo R, Palladino R, Chang KC-M, Costabile T, Russo C, et al. Cognitive impairment at diagnosis predicts 10-year multiple sclerosis progression. Mult Scler. (2016) 22:659–67. doi: 10.1177/1352458515599075
37. Palladino R, Lee JT, Hone T, Filippidis FT, Millett C. The great recession and increased cost sharing in European health systems. Health Aff. (2016) 35:1204–13. doi: 10.1377/hlthaff.2015.1170
38. Iavicoli I, Gambelunghe A, Magrini A, Mosconi G, Soleo L, Vigna L, et al. Diabetes and work: the need of a close collaboration between diabetologist and occupational physician. Nutr Metab Cardiovasc Dis. (2019) 29:220–7. doi: 10.1016/j.numecd.2018.10.012
Keywords: multiple sclerosis, working, job, disability, fatigue, mood, cognitive
Citation: Moccia M, Fontana L, Palladino R, Falco F, Finiello F, Fedele M, Lanzillo R, Reppuccia L, Triassi M, Brescia Morra V and Iavicoli I (2022) Determinants of early working impairments in multiple sclerosis. Front. Neurol. 13:1062847. doi: 10.3389/fneur.2022.1062847
Received: 06 October 2022; Accepted: 24 November 2022;
Published: 09 December 2022.
Edited by:
Alessandra Lugaresi, University of Bologna, ItalyReviewed by:
Bahia Hakiki, IRCCS Don Carlo Gnocchi Firenze, ItalyGiampaolo Brichetto, Associazione Italiana Sclerosi Multipla, Italy
Copyright © 2022 Moccia, Fontana, Palladino, Falco, Finiello, Fedele, Lanzillo, Reppuccia, Triassi, Brescia Morra and Iavicoli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcello Moccia, bWFyY2VsbG8ubW9jY2lhQHVuaW5hLml0
 Marcello Moccia
Marcello Moccia Luca Fontana
Luca Fontana Raffaele Palladino
Raffaele Palladino Fabrizia Falco6
Fabrizia Falco6 Roberta Lanzillo
Roberta Lanzillo Liberata Reppuccia
Liberata Reppuccia Maria Triassi
Maria Triassi Vincenzo Brescia Morra
Vincenzo Brescia Morra Ivo Iavicoli
Ivo Iavicoli