- Henan Provincial People's Hospital, Zhengzhou, China
Background and purpose: Clinical outcome in patients who received thrombectomy treatment is time-dependent. The purpose of this study was to evaluate the efficacy of the one-stop stroke management (OSSM) platform in reducing in-hospital workflow times in patients receiving thrombectomy compared with the traditional model.
Methods: The data of patients who received thrombectomy treatment through the OSSM platform and traditional protocol transshipment pathway were retrospectively analyzed and compared. The treatment-related time interval and the clinical outcome of the two groups were also assessed and compared. The primary efficacy endpoint was the time from door to groin puncture (DPT).
Results: There were 196 patients in the OSSM group and 210 patients in the control group, in which they were treated by the traditional approach. The mean DPT was significantly shorter in the OSSM group than in the control group (76 vs. 122 min; P < 0.001). The percentages of good clinical outcomes at the 90-day time point of the two groups were comparable (P = 0.110). A total of 121 patients in the OSSM group and 124 patients in the control group arrived at the hospital within 360 min from symptom onset. The mean DPT and time from symptom onset to recanalization (ORT) were significantly shorter in the OSSM group than in the control group. Finally, a higher rate of good functional outcomes was achieved in the OSSM group than in the control group (53.71 vs. 40.32%; P = 0.036).
Conclusion: Compared to the traditional transfer model, the OSSM transfer model significantly reduced the in-hospital delay in patients with acute stroke receiving thrombectomy treatment. This novel model significantly improved the clinical outcomes of patients presenting within the first 6 h after symptom onset.
Introduction
Thrombectomy recanalization of large-vessel occlusion in acute ischemic stroke is strongly time-dependent, and thus shortening the time between onset and recanalization can improve the prognosis of patients (1, 2). Hence, several pre-hospital and in-hospital measures for improvement have been implemented to shorten the time from onset to recanalization (ORT) (3, 4). In this regard, the development of a green channel that integrates medical specialists in multidisciplinary cooperation for hospital treatment of acute stroke considerably shortened the time from the door admission to recanalization treatment (5).
In most stroke centers, patients undergo imaging examination at an imaging center and are then transferred to the emergency department to receive intravenous thrombolysis and then transferred to the catheter room for thrombectomy. However, the long transfer times often cause delays in the treatment of patients with stroke. The one-stop stroke management (OSSM) platform combines computed tomography (CT), magnetic resonance imaging (MRI), and digital subtraction angiography (DSA) equipment in one space, using the same track to transfer patients from one device to another without switching beds. Thus, preoperative imaging examination and thrombectomy procedure are completed in the same space. Such an integrated combination of examination and treatment can dramatically shorten in-hospital transportation time. Our center, in collaboration with Siemens Healthcare, developed an OSSM platform to reduce the in-hospital delays of patients with acute stroke. In this study, we compared the data of patients who received thrombectomy via the OSSM platform with those who underwent the procedure via the traditional workflow to establish the effect of the OSSM platform model on the reduction of the delay of in-hospital stroke treatment.
Methods
The data of patients who received thrombectomy through the OSSM platform and those of patients who underwent thrombectomy through the protocol transshipment pathway, defined as the control group, were retrospectively analyzed.
Inclusion criteria
All the included patients received thrombectomy treatment at our center between January 2017 and December 2021. The data were retrieved from a prospectively maintained database. The inclusion criteria were as follows: (1) aged ≥18 years; (2) treated within 24 h from onset; (3) the National Institutes of Health Stroke Scale (NIHSS) ≥6; (4) Alberta Stroke Program Early Computed Tomography Score (ASPECT) ≥6; (5) pre-stroke Modified Rankin Scale (mRS) score ≤1; (6) the treatment protocols were consistent with those in the OSSM group or the control group; (7) the follow-up data were completed; and (8) informed consent was received from the patient or a family member.
Treatment protocol
In our center, patients with acute stroke typically arrive at the emergency department are then evaluated by a stroke physician, and receive the necessary treatment. The patients in the OSSM group were transferred to the OSSM platform for imaging examination, followed by thrombectomy. Patients who met the criteria of intravenous thrombolytic therapy (IVT) received IVT in the platform before thrombectomy therapy (Figure 1). Patients in the traditional protocol transshipment pathway group were transported from the emergency department to the imaging center for pretreatment imaging examination. Which imaging modality to choose was a comprehensive consideration based on the patient's actual condition, including the time from onset, severity, and the presence or absence of contraindications. Imaging examinations included noncontrast CT, CTP, MRI, and PWI, as well as noninvasive vascular imaging including CTA and MRA. Patients were then transferred to the catheter unit for thrombectomy therapy. Mechanical thrombectomy was performed under local or general anesthesia; heparin was used selectively. Endovascular thrombectomy methods included stent retrieval, aspiration thrombectomy, balloon dilatation, stent implantation, or other treatments based on the specific subject's clinical conditions.
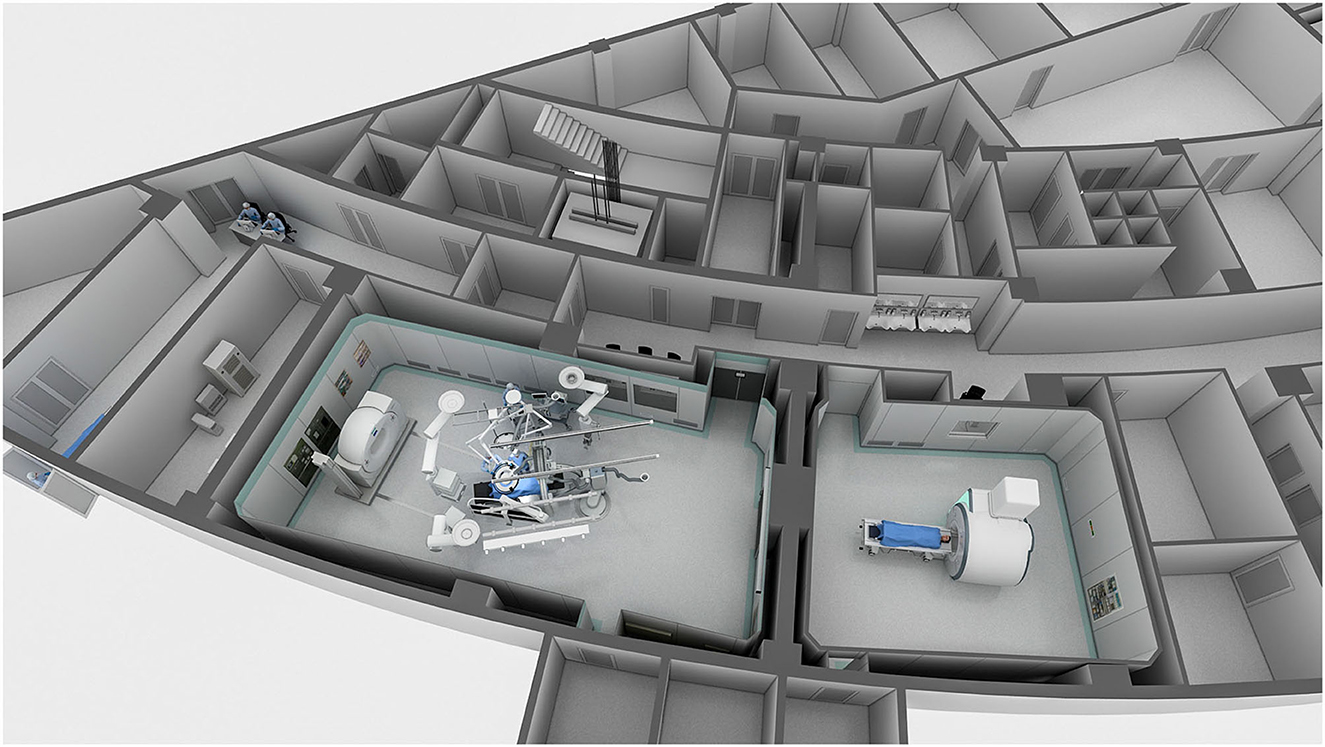
Figure 1. This overview of the one-stop stroke management (OSSM) platform shows the layout of the computed tomography (CT), magnetic resonance imaging (MRI), and digital subtraction angiography (DSA) equipment rooms.
Relevant efficacy observation and follow-up examinations
The primary efficacy endpoint was the time from door to groin puncture (DPT). The secondary efficacy endpoints were the time from imaging to groin puncture (IPT), the time from door to successful reperfusion (DRT) or final angiographic results, the time from symptom onset to successful reperfusion (ORT), and the time from groin puncture to successful reperfusion (PRT). The rate of successful reperfusion of target vessels (modified thrombolysis in cerebral infarction, mTICI ≥ 2b) was defined as successful reperfusion; the rate of good functional independence was defined as an mRS score from 0 to 2 for a postoperative follow-up period of 90 ± 14 days. Safety outcomes included the rate of symptomatic intracranial hemorrhage (sICH) and all-cause mortality during the follow-up period. The complications of sICH were defined as any form of intracranial hemorrhage with an increase in NIHSS score of ≥ 4 points during the perioperative period.
Statistical analysis
Statistical analysis was performed using the SPSS version 22.0 software. Continuous data that met normal distribution were represented with interquartile range or means with SD, comparison between groups used independent sample t-test, whereas categorical data were expressed as several cases and percentages. P < 0.05 was considered to be statistically significant.
Results
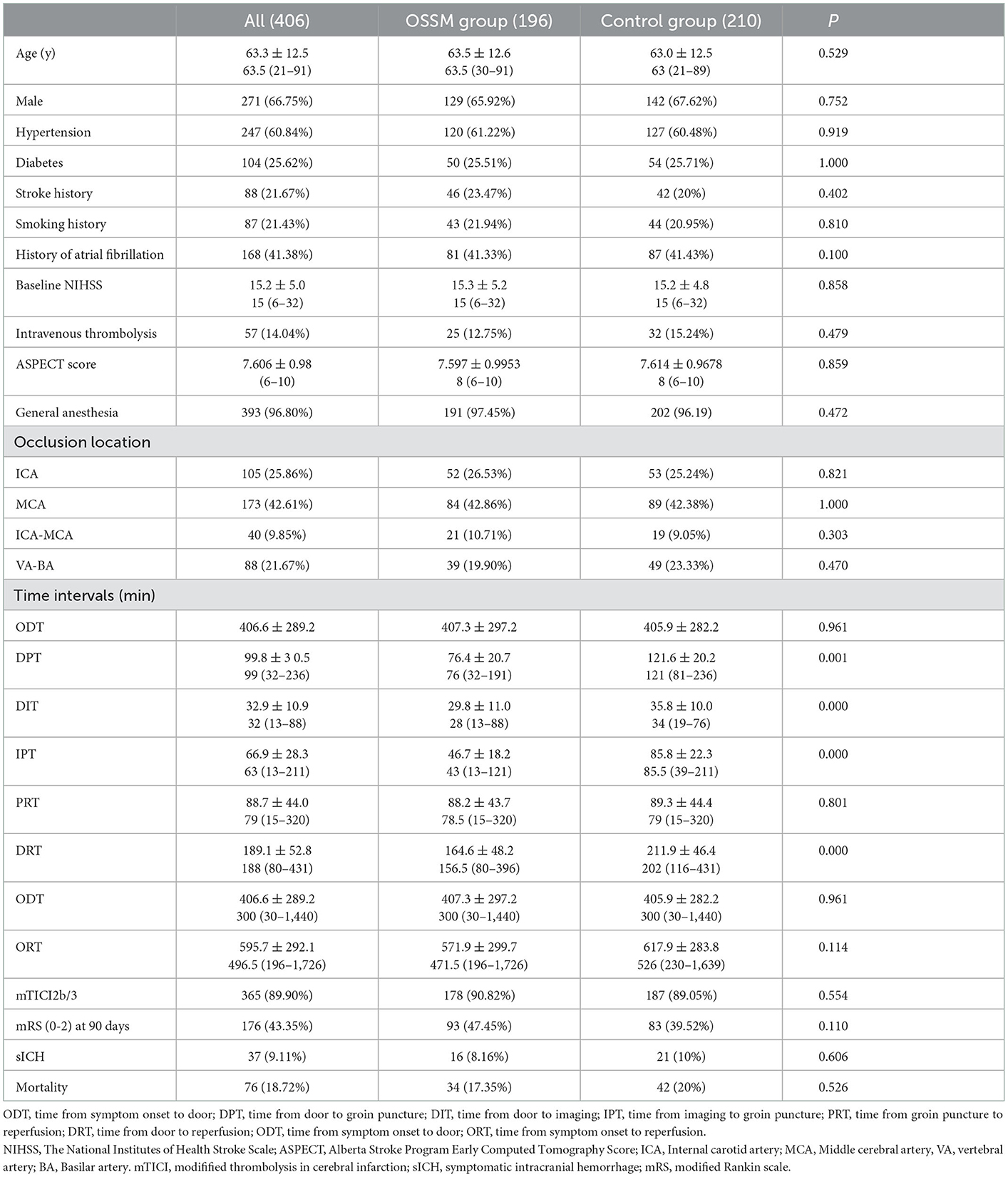
A total of 406 patients were included in the analysis, of whom 196 were in the OSSM group and 210 were in the control group. The mean age was 63 years, the mean NIHSS score was 15, and the mean ODT was 407 min. The baseline data of the two groups of patients are presented in Table 1. No statistically significant differences were observed between the baseline data of the two groups, such as the baseline NIHSS score, gender, ASPECT, occlusion location, and the time from symptom onset to hospital admission. Furthermore, no significant differences were detected in the risk factors, such as a history of hypertension, diabetes, stroke history, and atrial fibrillation.
The mean DPT was 76 min in the OSSM group and 122 min in the control group (P < 0.001). Notably, a 44 min reduction was observed in the OSSM group compared to the control group. The median DIT was significantly shorter in the OSSM group than in the control group (30 vs. 36 min; P < 0.001). The mean DPT was 47 in the OSSM group, whereas it was 86 min in the control group (P < 0.001). The mean DRT was 165 min in the OSSM group, whereas it was 212 min in the control group, and the difference between the two groups was statistically significant (P < 0.001). The mean PRT was comparable between the two groups (88 vs. 89 min; P = 0.701). The mean ORT was shorter in the OSSM group (572 min) than in the control group (618 min) but with no significant difference between the two groups (P = 0.114).
There was no significant between-group difference in the rate of successful reperfusion (90.82 vs. 89.05%, P = 0.554). The percentages of good clinical outcomes at the 90-day follow-up examination were 47% in the OSSM group and 40% in the control group. No statistical differences were present between the two groups (P = 0.110). The rate of all-cause 90-day mortality was 17% in the OSSM group and 20% in the control group (P = 0.526), the rate of symptomatic hemorrhage was 8% in the OSSM group and 10% in the control group, and the rate did not differ significantly across groups in pairwise comparisons (P = 0.606).
Subgroup analyses
A total of 245 patients arrived at the hospital within 360 min from symptom onset, of whom 121 were in the OSSM group and 124 were in the control group (Table 2). There were no statistically significant differences in the baseline data between the two groups. Their mean ODT and PRT were comparable. In the OSSM group, the mean DPT, IRT, DRT, and ORT were significantly shorter than those in the control group. There was no significant between-group difference in the rate of successful reperfusion (90.82 vs. 89.05%, P = 0.554. A higher rate of good functional outcomes was achieved in the OSSM group than in the control group (53.71 vs. 40.32% P = 0.036). The rate of all-cause 90-day mortality and sICH were comparable between the two groups.
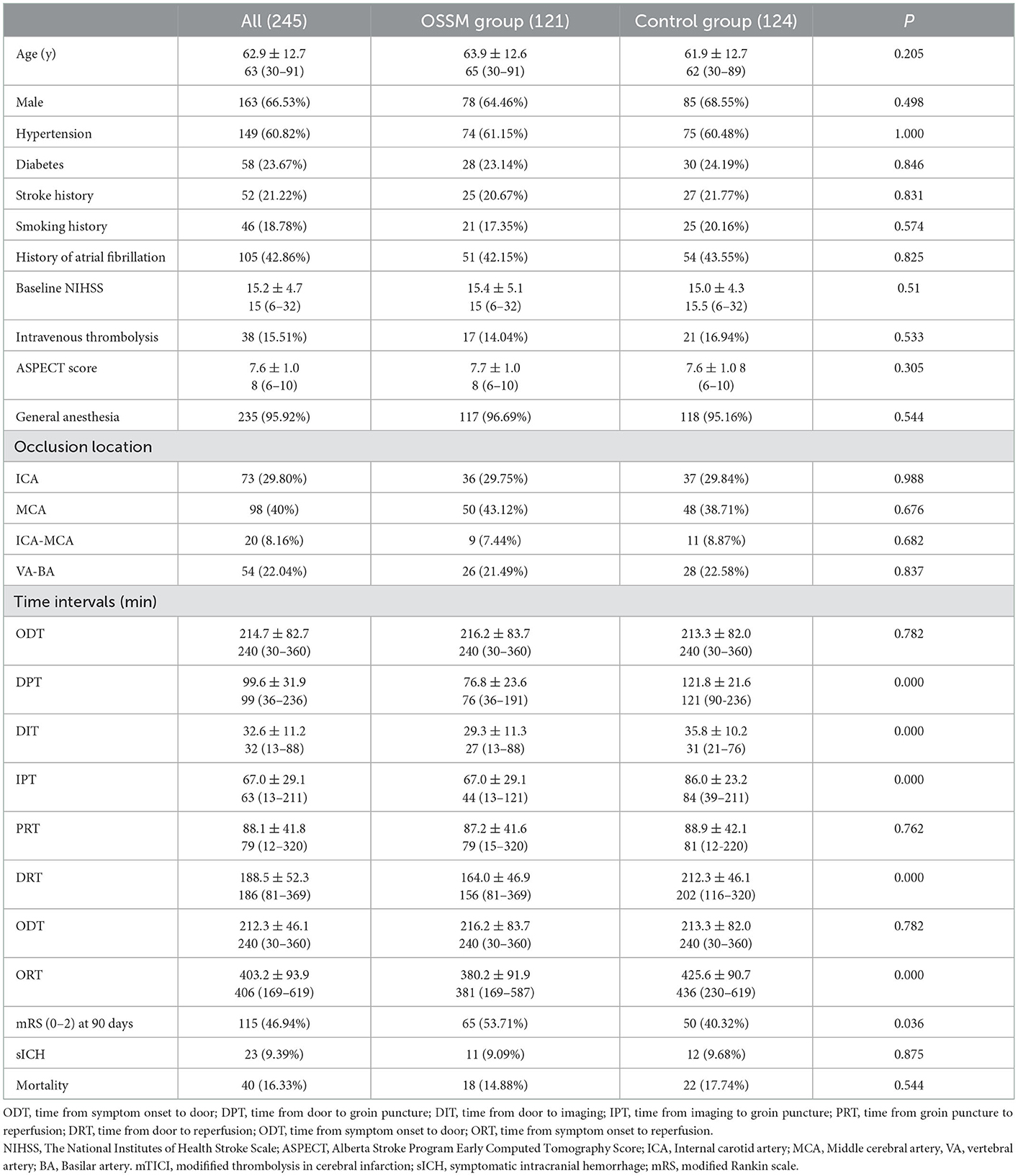
Table 2. Comparison of data between the two groups of patients underwent thrombectomy therapy within 6h from symptom onset.
Discussion
This retrospective cohort study showed that the OSSM platform incorporating CT, MRI, and DSA equipment can significantly reduce in-hospital delays in the thrombectomy treatment of patients with stroke compared to traditional workflow. The patients who arrived in the OSSM platform of the hospital within 6 h from symptom onset had a significantly shorter DPT and a better clinical outcome than those in the traditional protocol transshipment pathway.
Early ischemic brain reperfusion is critical for achieving good clinical outcomes in patients with stroke. A meta-analysis of five randomized clinical trials showed that of every 1,000 patients in whom substantial endovascular reperfusion was achieved; for every 15-min faster emergency department door-to-reperfusion time, an estimated 39 patients would have had a less-disabled outcome at 3 months (1). In the ESCAPE trial, the shorter imaging-to-reperfusion time significantly improved the chance of achieving a functionally independent outcome (6). A number of measures have been taken to reduce delays in the treatment of patients with stroke, particularly in improving the process of in-hospital imaging examination (7, 8).
Compared with multidetector CT, the latest generation of flat-panel CT (FPCT) is of high diagnostic value in the detection of ischemic changes. In addition, occluded vessels and cerebral collaterals can be detected with FP-CTA, and make it possible to be used as a peri-interventional diagnostic tool. Bypassing the CT suite, with direct transfer to angiosuite (DTAS), has been implemented in many centers and has contributed to a significant reduction in hospital workflow times (9). Marios-Nikos reported the case of a first mothership patient who was transported directly to the angiography suite and received nonenhanced FPCT (10). This patient was diagnosed with large-vessel occlusion, based on the FPCT-angiography results, and treated by endovascular thrombectomy, with a door-to-groin time (DNT) reduction to 23 min (10). A prospective, randomized trial showed that patients with acute stroke who were directly transferred to the angiosuite (DTAS) and received noncontrast-enhanced FPCT had a significantly reduced time from stroke imaging to groin puncture (by ~7 min) in comparison with the CT transit (CTT) pathway (11). Another study showed that DTAS protocols significantly increased the odds ratio of achieving a favorable outcome (12).
However, it should be pointed out that patients with DTAS directly transported to the angiography suite and received a noncontrast enhanced FPCT as preoperative imaging examination but not a CT-angiography or perfusion imaging, and as a result, patients evaluated by FPCT did not have large-vessel occlusion. Mendez reported the cases of patients, n = 7/97 (7.2%), whose initial angiogram did not show a treatable occlusion (12). The study of Psychogios included patients with NIHSS score > 10, but large-vessel occlusion was detected in the angiograms of only 18 of 30 patients (13). In addition, blindly transferring patients directly to the angiography room for plate CT examination also interferes with the normal operation of the C-arm for patients undergoing endovascular treatment. In our study, we creatively integrated CT, MR, and C-arm into the same space, and noninvasive vascular examinations such as CTA and MRA were performed to determine whether the patients were suitable for thrombectomy. For patients beyond 6 h from symptom onset, multimodal imaging was to be employed for treatment guidance, which was hard to be completed by FPCT.
In the present study, the OSSM model significantly shortened DPT compared to the traditional model. However, the time from admission to treatment was still long in comparison with those reported in previous publications, since more than 97% of the patients received general anesthesia during the operation, which requires a longer time than local anesthesia. For the majority of the patients, the preoperative imaging evaluation of patients in our center was based mainly on MR results, and thus a longer time was needed to complete an MR scan than a CT examination. This was also one of the main reasons that might have led to a longer delay.
It should be pointed out that with the extension of the thrombectomy time window to 24 h (14, 15), part of the thrombectomy patients arrived in the hospital beyond the 6-h time point. In this investigation, the median time from symptom onset to hospital admission was 6.7 h. The model described here did not significantly shorten the time from symptom onset to treatment; it did not significantly improve the clinical outcomes of the patients either. For patients who arrive at the hospital for treatment within a short time from onset, the OSSM transport mode is more likely to reduce the time from symptom onset to treatment, which can improve the prognosis of these patients compared with those in whom the traditional transport mode has been implemented.
Our study has some limitations. First of all, this was a retrospective analysis and comparison with a retrospective patient cohort. Certain selection biases in the baseline data might have been present, although the primary baseline data did not differ significantly between the two groups. Second, the study was carried out in a single center, and the equipment distribution, personnel allocation, and patient treatment process might have been different from those employed in other centers. Thus, the results of this study may not be applicable to other centers.
In conclusion, compared to the traditional transfer model, the OSSM platform significantly reduced the in-hospital delay in patients with acute stroke who received thrombectomy treatment. Furthermore, this model significantly improved the clinical outcomes in patients presenting within the first 6 h after symptom onset.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Henan Provincial People's Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
TZ: conception and design, drafting the article, and revising it critically for important intellectual content. TL: conception and design and final approval of the version to be published. LZ, ZL, QL, ZW, LW, YH, YL, ZZ, MG, ZM, Xp, SM, YF, GZ, WZ, XL, and MW: acquisition of data, analysis, and interpretation of data. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: A meta-analysis. JAMA. (2016) 316:1279–88. doi: 10.1001/jama.2016.13647
2. Fransen PS, Berkhemer OA, Lingsma HF, Beumer D, van den Berg LA, Yoo AJ, et al. Time to reperfusion and treatment effect for acute ischemic stroke: A randomized clinical trial. JAMA Neurol. (2016) 73:190–6. doi: 10.1001/jamaneurol.2015.3886
3. Meretoja A, Weir L, Ugalde M, Yassi N, Yan B, Hand P, et al. Helsinki model cut stroke thrombolysis delays to 25 minutes in melbourne in only 4 months. Neurology. (2013) 81:1071–6. doi: 10.1212/WNL.0b013e3182a4a4d2
4. Hassan AE, Rabah RR, Preston L, Tekle WG. Steps-t program improves endovascular treatment outcomes of acute ischemic stroke; a 6-year study. Front Neurol. (2019) 10:1251. doi: 10.3389/fneur.2019.01251
5. Ren Y, Ma QF, Yan CM, Zhang YJ. [green channel construction mode and development of stroke center in china]. Zhonghua yi xue za zhi. (2022) 102:15–20. doi: 10.3760/cma.j.cn112137-20210416-00914
6. Menon BK, Sajobi TT, Zhang Y, Rempel JL, Shuaib A, Thornton J, et al. Analysis of workflow and time to treatment on thrombectomy outcome in the endovascular treatment for small core and proximal occlusion ischemic stroke (escape) randomized, controlled trial. Circulation. (2016) 133:2279–86. doi: 10.1161/CIRCULATIONAHA.115.019983
7. Kansagra AP, Wallace AN, Curfman DR, McEachern JD, Moran CJ, Cross III DT, et al. Streamlined triage and transfer protocols improve door-to-puncture time for endovascular thrombectomy in acute ischemic stroke. Clin Neurol Neurosurg. (2018) 166:71–5. doi: 10.1016/j.clineuro.2018.01.026
8. Mehta BP, Leslie-Mazwi TM, Chandra RV, Bell DL, Sun CH, Hirsch JA, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: A pilot quality improvement project. J Am Heart Assoc. (2014) 3:e000963. doi: 10.1161/JAHA.114.000963
9. Requena M, Olive-Gadea M, Muchada M, Hernandez D, Rubiera M, Boned S, et al. Direct to angiography suite without stopping for computed tomography imaging for patients with acute stroke: A randomized clinical trial. JAMA Neurol. (2021) 78:1099–107. doi: 10.1001/jamaneurol.2021.2385
10. Psychogios MN, Bahr M, Liman J, Knauth M. One stop management in acute stroke: First mothership patient transported directly to the angiography suite. Clin Neuroradiol. (2017) 27:389–91. doi: 10.1007/s00062-017-0574-z
11. Pfaff JAR, Schonenberger S, Herweh C, Ulfert C, Nagel S, Ringleb PA, et al. Direct transfer to angio-suite versus computed tomography-transit in patients receiving mechanical thrombectomy: A randomized trial. Stroke. (2020) 51:2630–8. doi: 10.1161/STROKEAHA.120.029905
12. Mendez B, Requena M, Aires A, Martins N, Boned S, Rubiera M, et al. Direct transfer to angio-suite to reduce workflow times and increase favorable clinical outcome. Stroke. (2018) 49:2723–7. doi: 10.1161/STROKEAHA.118.021989
13. Psychogios MN, Behme D, Schregel K, Tsogkas I, Maier IL, Leyhe JR, et al. One-stop management of acute stroke patients: Minimizing door-to-reperfusion times. Stroke. (2017) 48:3152–5. doi: 10.1161/STROKEAHA.117.018077
14. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. doi: 10.1056/NEJMoa1713973
Keywords: stroke, time, puncture, thrombectomy, outcome
Citation: Zhou T, Li T, Zhu L, Li Z, Li Q, Wang Z, Wu L, He Y, Li Y, Zhou Z, Guan M, Ma Z, pei X, Meng S, Feng Y, Zhang G, Zhao W, Liu X and Wang M (2023) One-stop stroke management platform reduces workflow times in patients receiving mechanical thrombectomy. Front. Neurol. 13:1044347. doi: 10.3389/fneur.2022.1044347
Received: 14 September 2022; Accepted: 23 December 2022;
Published: 18 January 2023.
Edited by:
Bin Qiu, Yale University, United StatesReviewed by:
Zhiming Zhou, First Affiliated Hospital of Wannan Medical College, ChinaHuaizhang Shi, First Affiliated Hospital of Harbin Medical University, China
Copyright © 2023 Zhou, Li, Zhu, Li, Li, Wang, Wu, He, Li, Zhou, Guan, Ma, pei, Meng, Feng, Zhang, Zhao, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tianxiao Li,  bGl0aWFueGlhbzY2NjZAMTI2LmNvbQ==
bGl0aWFueGlhbzY2NjZAMTI2LmNvbQ==
 Tengfei Zhou
Tengfei Zhou Tianxiao Li
Tianxiao Li Liangfu Zhu
Liangfu Zhu