- Department of Cerebrovascular Disease, Henan Provincial People's Hospital, Zhengzhou University People's Hospital, Zhengzhou, Henan, China
Objective: Endovascular recanalization in patients with non-acute symptomatic middle cerebral artery occlusion remains clinically challenging. Here, we aimed to evaluate the feasibility and safety of endovascular recanalization for non-acute symptomatic middle cerebral artery occlusion and propose a new patient classification.
Methods: Between January 2019 and December 2021, 88 patients with non-acute symptomatic middle cerebral artery occlusion underwent prospective endovascular recanalization at our hospital. All patients were divided into three groups according to occlusion length, occlusion duration, occlusion nature, calcification of the occlusion site, and occlusion angulation. The indicators of each group were analyzed, including general baseline data, imaging data, surgical conditions, and follow-up results.
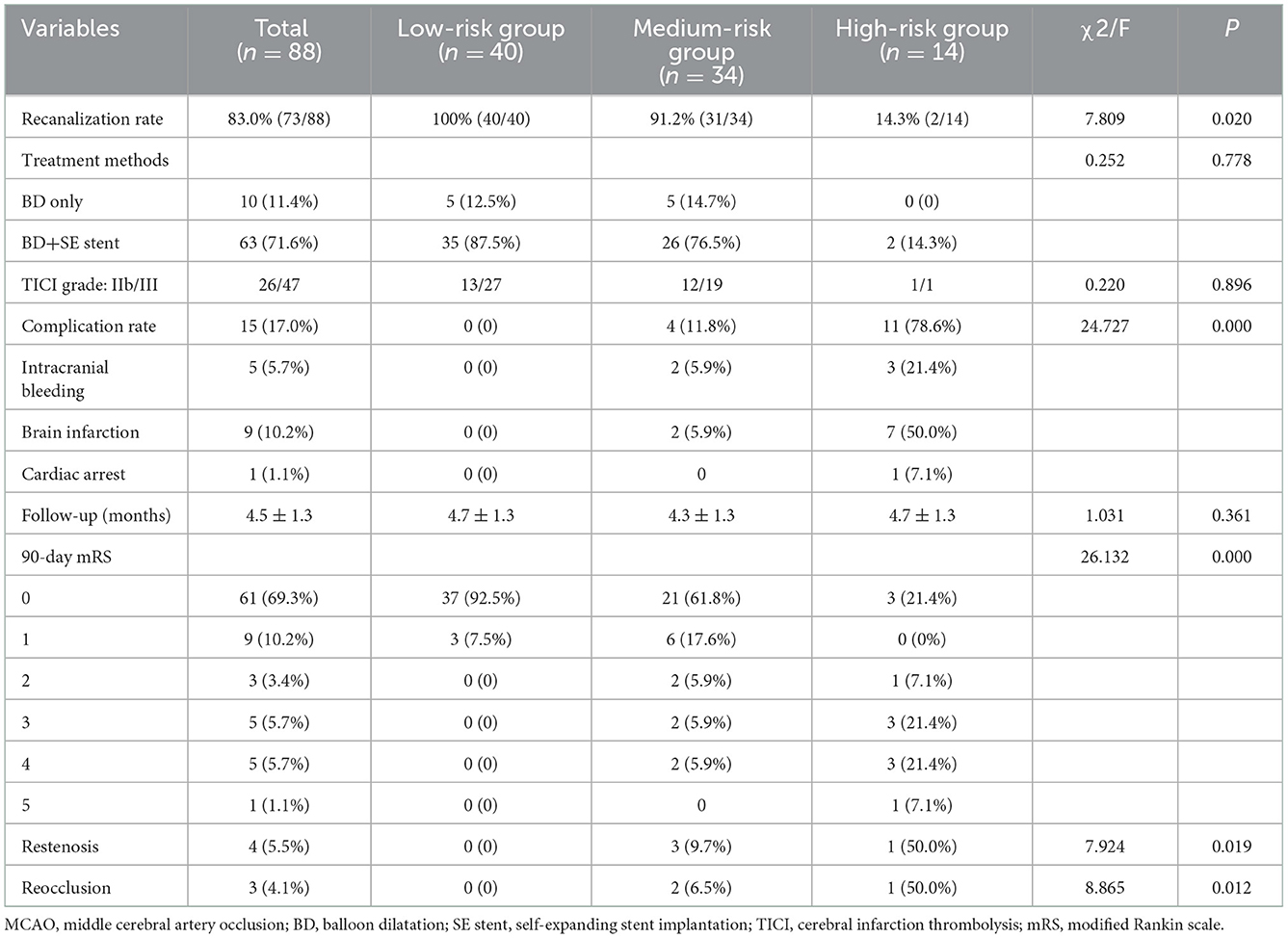
Results: Of the 88 patients, 73 were successfully recanalized and 15 were abandoned because the instruments either could not reach the distal true lumen of the occlusion or broke through the blood vessels. The overall technical success rate was 83.0% (73/88), and perioperative complications occurred in 15 patients. Preoperatively, all patients were divided into three risk groups: low, medium, and high. From the low- to high-risk groups, the recanalization rate gradually decreased (100.0, 91.7, and 16.7%, respectively, P = 0.020), the perioperative complication rate gradually increased (0, 13.9, and 83.3%, respectively, P < 0.001), the proportion of the modified Rankin scale scores >2 at 90 days increased (0, 11.7, and 50.0%, P < 0.001), and the restenosis/reocclusion rates in the 73 cases of successful recanalization increased (0, 16.1, and 100%, P = 0.012) during follow-up.
Conclusion: Endovascular recanalization may be feasible and safe in well-selected patients with non-acute symptomatic middle cerebral artery occlusion, especially in the low- and medium-risk groups.
1. Introduction
Middle cerebral artery occlusion (MCAO) is devastating and associated with high morbidity and mortality rates. The optimal treatment for non-acute MCAO remains unclear. Despite optimal medical therapy, such patients are still at high risk of recurrent ischemic stroke (1). Although some patients do not have symptoms of cerebral ischemia, long-term cerebral hypoperfusion can lead to brain atrophy, which can manifest as cognitive impairment, especially for non-acute MCAO in the dominant hemisphere (2). Currently, there is no effective treatment for non-acute symptomatic MCAO, and previous superficial temporal artery–middle cerebral artery bypass surgery has been confirmed with little to no benefit (3, 4). In recent years, endovascular techniques (ETs) have been shown to be an effective treatment for patients with acute ischemic stroke within 6 h, rescuing ischemic brain tissue and leading to good patient prognosis (5, 6). Some recent studies using ETs to treat chronic internal carotid artery occlusion (ICAO) achieved satisfactory results (7, 8). However, the heterogeneity of perioperative outcomes and the high rate of complications prompted us to explore which patients are the best candidates and perform individualized risk stratification. In this study, we propose a classification of patients for preoperative assessment based on preoperative imaging, including the length of occlusion, occlusion duration, nature of occlusion, calcification at the occlusion site, and angulation of the occlusion segment. The patients were scored and classified to evaluate the technical risk of endovascular recanalization surgery, explore the feasibility and safety of ETs for non-acute symptomatic MCAO, and provide a reference for patient selection and risk stratification.
2. Materials and methods
2.1. Patient selection
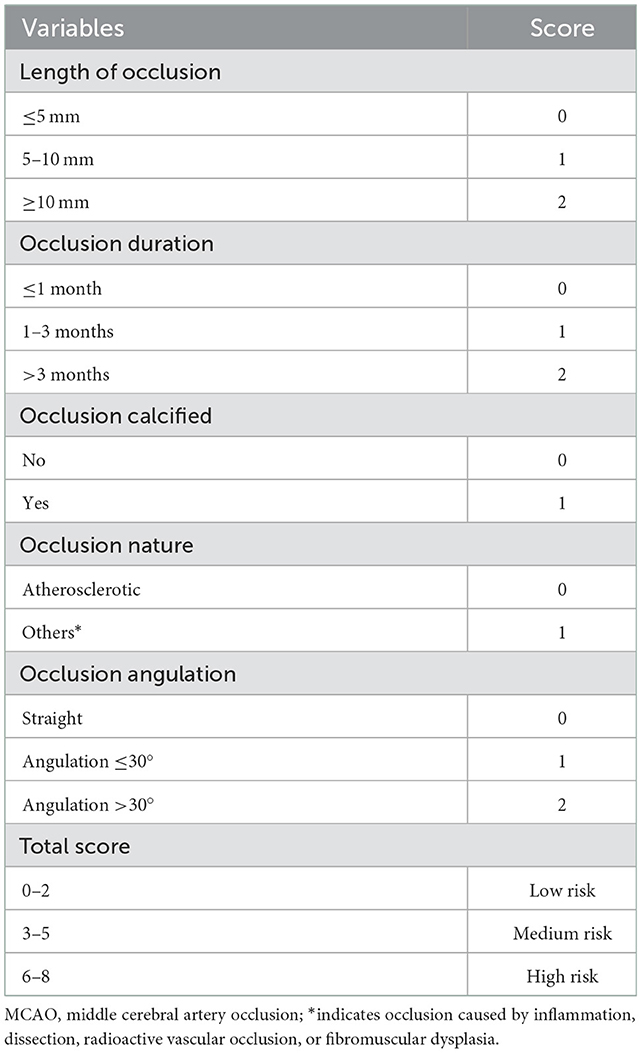
A total of 88 patients with non-acute symptomatic MCAO (M1 segment) were admitted to our hospital from January 2019 to December 2021, according to the patient's imaging examination, occlusion length, duration, and nature, calcification of the occlusion site, and angulation of the occluded segments (Table 1). All patients were divided into three groups: low-risk (0–2 points), medium-risk (3–4 points), and high-risk (5–7 points). Occlusion length was defined as the distance between the proximal end of the occlusion and the visible distal segment on preoperative imaging (computed tomography angiography [CTA] or digitally subtracted angiography [DSA]). Occlusion duration was defined as 100% occlusion of the vascular lumen cross-section on CTA or magnetic resonance angiography (MRA), with the occlusions confirmed by DSA and the duration from the date of initial diagnosis to the day of surgery determined by a three-person expert group consultation. The occlusion nature was determined according to the patient's past history of atherosclerosis risk factors and preoperative examination to confirm the diagnosis. Occlusion calcification was defined as “any form of calcified lesions within the outline of the blood vessel” on CT and determined by a three-person expert group consultation. Occlusion angulation was defined as the included angle of the axial extension line of the occlusion distal and proximal vessels; if the occluded end was flush or the segment was too short to determine the axial direction, the occlusion angle of the blood vessel was compared with the normal side. Informed consent was obtained from all the patients, and the study was approved by the institutional review board. The inclusion criteria were as follows: (1) MCAO diagnosed by CTA or MRA and confirmed using DSA; (2) occlusion duration >12 days, defined as the time from the date of initial diagnosis to the day of surgery; and (3) recurrent transient ischemic attack or stroke associated with MCAO despite optimal medical treatment. The exclusion criteria were as follows: (1) intracranial aneurysm and any bleeding disorder; (2) life expectancy <1 year due to other medical conditions; (3) large infarct core (ASPECT score <6 points); and (4) occlusion of the middle cerebral artery that continued to the internal carotid artery bifurcation without a stump.
2.2. Operative method
All procedures were performed by neurointerventional doctors with the patients under general anesthesia. After placement of the sheath introducer, heparin was administered intravenously to maintain an activated clotting time of 200–300 s. The 6F guiding catheter was advanced into the internal carotid artery, and the micro-guide wire cooperated with the microcatheter to reach the distal true lumen through the occluded segment. The angioplasty balloon catheter ascended along the exchange micro-guide wire, passed through the occluded lesion for expansion (the balloon size was selected according to the diameter of the proximal normal middle cerebral artery), and inflated to 6 atm for 30–60 s. If dissection or slow blood flow occurred after angioplasty, stent implantation was performed, mainly using the LVIS stent (MicroVention, USA), Neuroform EZ stent (Stryker Neurovascular, USA), or Enterprise stent (Codman, USA), with the choice of stents depending on the judgment of the operator. Successful recanalization was defined as modified thrombolysis in cerebral infarction score (mTICI) of ≥2b and residual stenosis of <50%.
2.3. Surgical management
Combination therapy with oral aspirin (100 mg) and clopidogrel (75 mg) was initiated at least 3 days before endovascular surgery. Thromboelastography was used to assess platelet reactivity. Aspirin resistance was defined as arachidonic acid-induced platelet aggregation inhibition <50%, and clopidogrel resistance was defined as <30% inhibition of ADP-induced platelet aggregation. None of the patients were aspirin-resistant, while 12 patients were resistant to clopidogrel and were treated instead with ticagrelor 90 mg twice daily. Dual antiplatelet therapy was maintained for 3–6 months, followed by lifelong maintenance of aspirin or clopidogrel monotherapy.
2.4. Clinical follow-up
Angiography and clinical follow-up were performed 3–6 months after surgery to assess the patency status of recanalized vessels, such as recurrence of stenosis, which should be measured by two neurointerventional specialists, according to the WASID criteria (9). Clinical follow-up mainly identified whether the patient had neurological deficits. If present, evaluation was conducted to determine whether it was related to the patient's surgery, stenting, or recanalization, and CT or magnetic resonance imaging (MRI) examination was performed. The initial and final angiography results were intervened by two neurointerventional experts to reach a consensus. In-stent restenosis was defined as angiographically proven in-stent or within 5 mm of the stent margin, with stenosis >50% and lumen diameter loss of 20% immediately after surgery. The mRS scores were divided into good (mRS, 0–2), moderate (mRS, 3), and poor (mRS, 4–5).
2.5. Statistical methods
Normally distributed quantitative variables are presented as mean ± standard deviation for all continuous variables, non-normally distributed variables are presented as a median and interquartile range, and categorical variables are presented as numbers and proportions. Comparisons between groups were performed using the Kruskal–Wallis test for continuous variables or the approximate chi-square test for categorical variables. The chi-square test was used for comparisons between the three groups, and differences were considered statistically significant when P < 0.05. All statistical analyses were performed using SPSS 22.0.
3. Results
3.1. Baseline characteristics and overall results
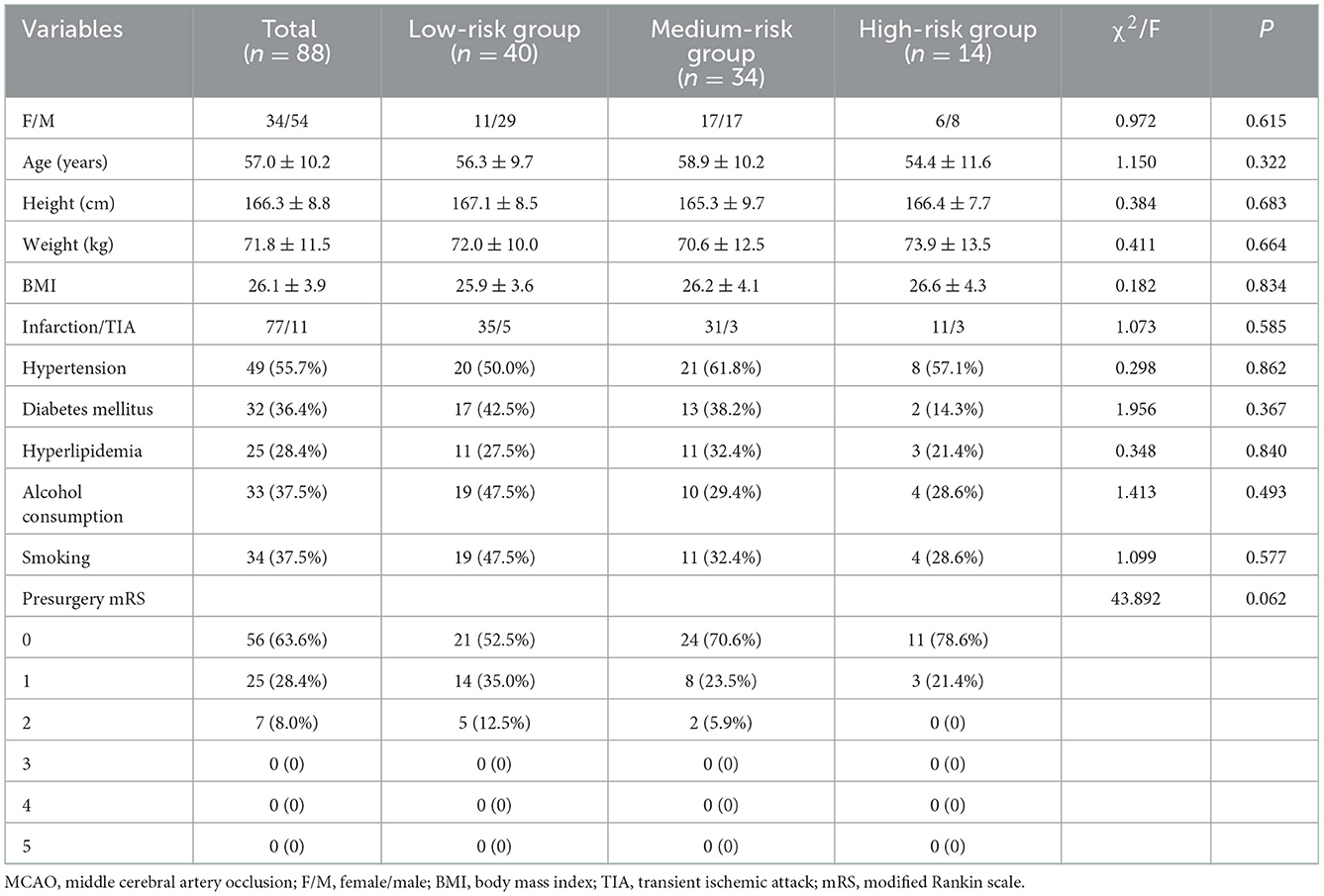
From January 2019 to December 2021, 88 consecutive patients underwent endovascular recanalization therapy for non-acute symptomatic MCAO. Table 2 summarizes the patients' baseline data. Of the 88 patients, 54 were men and 34 were women, with ages ranging from 31 to 80 years (mean, 57.0 ± 10.2 years). All patients had a history of ischemic stroke or TIA. The median duration from imaging diagnosis of occlusion to the day of recanalization surgery was 37 days (interquartile range 25–55). The overall technical success rate was 83.0% (73/88). The perioperative complication rate was 17.0% (15/88), with postoperative complications in 15 cases, of which three cases were asymptomatic, mild ischemic stroke occurred in six cases (National Institutes of Health Stroke Scale [NIHSS] score ≤4), three cases suffered an intracerebral hemorrhage, subarachnoid hemorrhage occurred in two cases, and one patient died from cardiac arrest. Stroke or death within 30 days occurred in 2.3% (2/88) of patients. Out of 88 patients, 84 (four patients lost to follow-up) had a mean clinical follow-up time of 4.52 ± 1.29 months. Stroke or mortality after 30 days occurred in 6.0% (5/84) of patients, with one death due to intracerebral hemorrhage, severe ischemic strokes in two patients (NIHSS score was 15, and modified Rankin scale [mRS] score was 5), and mild ischemic strokes in two patients (NIHSS score ≤4). The mean angiographic follow-up time of 75 patients was 4.79 ± 1.48 months, with four in-stent restenosis and three reocclusions.
3.2. Subgroup analysis
Table 3 summarizes the clinical data of the 88 patients. From the low- to high-risk groups, the recanalization rate gradually decreased (100.0, 91.7, and 16.7%, respectively, P = 0.020), the perioperative complication rate gradually increased (0, 13.9, and 83.3%, respectively, P < 0.001), the proportion of mRS scores >2 at 90 days increased (0, 11.7, and 50.0%, respectively, P < 0.001), and the restenosis/reocclusion rates in the 73 cases of successful recanalization increased (0, 16.1, and 100%, respectively, P = 0.012) during follow-up. Figure 1 shows the clinical data of a low-risk patient.
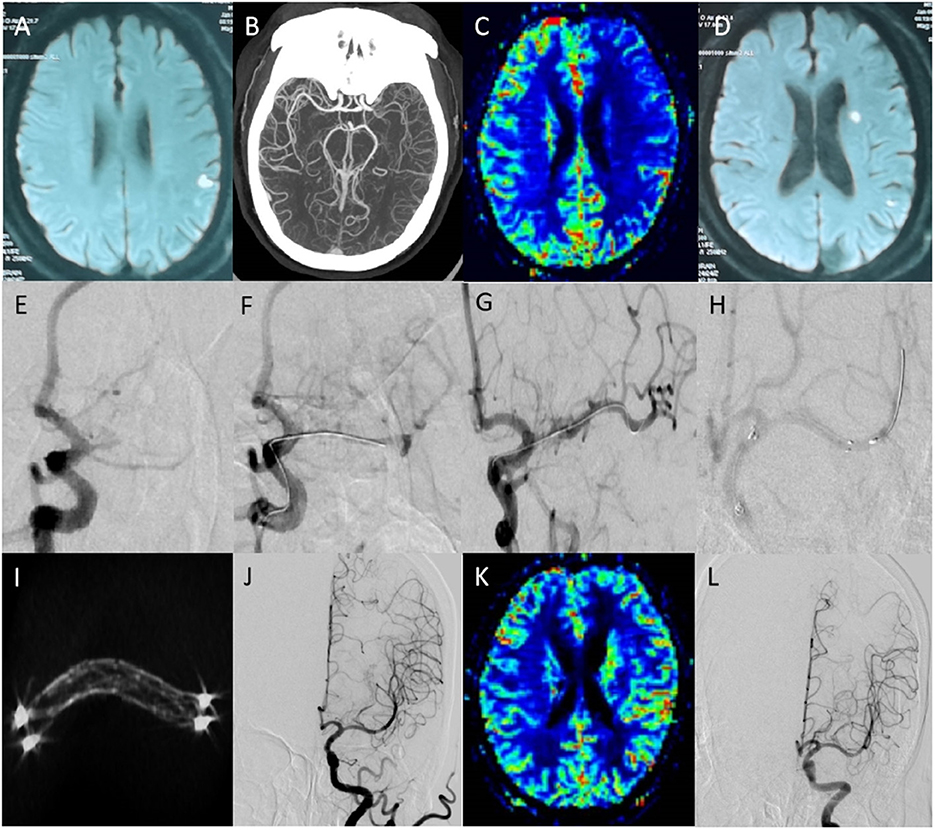
Figure 1. Clinical data of a low-risk patient. Male patient, 65 years old; chief complaint: right limb weakness with slurred speech for 21 days, relapsed for 3 days; past medical history: hypertension for 6 years; physical examination: the right limb muscle strength was grade 3, and the muscle tone was normal; the mRS score was 2. (A) Preoperative magnetic resonance imaging (MRI) shows acute cerebral infarction in the left cerebral parietal lobe. (B) Computed tomography angiography shows the M1 segment occlusion of the left middle cerebral artery. (C) Preoperative perfusion-weighted imaging (PWI) shows left cerebral hypoperfusion. (D) MRI after symptom recurrence shows left basal ganglia and parietal lobe acute cerebral infarction. (E) Preoperative digitally subtracted angiography (DSA) shows the left middle cerebral artery occlusion (occlusion length <5 mm, occlusion duration <3 months, atherosclerotic, no calcification, straight). (F) The micro-guide wire passed through the occluded segment during the operation. (G) The Gateway 2.0 × 10 mm balloon was used for accurate positioning and 4ATM expansion. (H) Neuroform 3.5 × 20 mm was ascended along the stent catheter, accurately positioned, and released. (I) The reconstructed stent is visible, and the stent is well expanded. (J) Postoperative anteroposterior angiography. (K) PWI shows that the bilateral perfusion was symmetrical, and the left cerebral perfusion was significantly improved. (L) Angiography was repeated 5 months later, which showed stent patency, and the mRS score was 0.
4. Discussion
Non-acute MCAO is a chronic vascular occlusion, which can be caused by atherosclerosis. It is the end result of the natural development of atherosclerosis. The continuous enlargement of the local atherosclerotic plaque or the formation of a new thrombus based on atherosclerotic plaque leads to vascular occlusion (10, 11). Non-acute MCAO is a highly heterogeneous disease, and its clinical manifestations and prognosis vary greatly among individuals owing to the degree of cerebrovascular collateral compensation (12, 13). The collateral circulation is well compensated, and patients may not have any clinical symptoms. Patients with poor collateral circulation compensation may experience repeated events such as cerebral infarction/TIA; therefore, active intervention measures for the non-acute phase occlusion of the middle cerebral artery with poor collateral circulation compensation have gradually been recognized (14). In recent years, many medical centers have attempted endovascular recanalization therapy for patients with non-acute symptomatic large vessel occlusion based on the experience of intravascular recanalization in acute intracranial large vessel occlusion (15–18). Patients with large intracranial artery occlusions are selected to undergo endovascular recanalization, which can help prevent repeated cerebrovascular ischemia events and promote functional recovery in patients with disabilities (17, 18). It is critical to select patients who could benefit from revascularization therapy. Previous studies on endovascular recanalization for non-acute symptomatic intracranial large artery occlusion have shown that patients with clinical symptoms caused by hypoperfusion can benefit most from endovascular recanalization therapy (19). In this study, only patients with non-acute MCAO with poorly compensated collateral circulation and a poor response to medical drug treatment were selected for endovascular recanalization. Such patients have hemodynamic disorders in their pathogenesis and theoretically obtain the most potential benefit from endovascular recanalization therapy. In this study, the low-risk group patients with a recanalization rate of 100% and a low risk of perioperative complications (0%) were identified as the best candidates for endovascular recanalization treatment. To the best of our knowledge, this study represents the largest serial case study on endovascular recanalization treatment in patients with non-acute symptomatic MCAO.
Whether the micro-guide wire can pass through the occlusion segment smoothly is the key to the success of the recanalization operation, but it is related to the occlusion length, duration, nature, calcification of the occlusion site, and occlusion angulation. The longer the occlusion length, the more difficult it is to pass. This study demonstrated that the technical challenges of occlusion and patency are related to the occlusion length, with the low-risk group characterized by shorter lesions having the highest recanalization rates, and in the high-risk group, an occlusion length of >10 mm was one of the factors leading to failure of recanalization. Also, the more severe the angulation of the occlusion segment, the greater the possibility of vessel perforation during the exploration of the micro-guide wire, which is related to the difficulty in identifying true vessels when crossing the occlusion. Furthermore, the longer the occlusion duration, the more severe the calcification or fibrosis of the occluded segment and the more difficult the recanalization process will be. Coronary recanalization experience in chronic occlusion also shows that when the occlusion nature is atherosclerotic and the occlusion duration is <3 months, the successful recanalization rate is high; however, when the occlusion length is >5 mm, calcification and angulation of the occluded segment are severe, and the recanalization rate is low (20–22). In this study, all patients were divided into three groups according to occlusion length, duration, and nature, calcification of the occlusion site, and angulation of the occluded segments. From the low- to high-risk groups, the recanalization rate gradually decreased, whereas the complication rate, 90-day mRS score, and follow-up rate of restenosis/reocclusion in patients with successful recanalization increased gradually. In addition, in the low- and medium-risk groups, recanalization rates (100 and 91.7%, respectively) and perioperative complication rates (0 and 13.9%, respectively) were acceptable; hence, patients categorized in these groups should be considered the best candidates for endovascular recanalization therapy.
In 1998, Mori et al. proposed a cerebral arteriography classification that classifies lesions according to the length and geometry of intracranial atherosclerotic stenosis (23). However, unlike stent placement surgery for stenosis, the anatomical direction and course of intracranial occlusions cannot be determined through imaging. Therefore, endovascular recanalization surgery in chronic total occlusion was more dependent on the surgeon's experience. For surgeons, the length of occlusion judged by angiography is mainly based on the distance between the proximal occlusion and distal collateral vessel reconstruction, which may be longer than the true length of the underlying atherosclerotic lesion. Preoperative high-resolution MRI, the original image of CTA, or MRA can also help to determine the shape and length of the occluded segment. When the surgeon tries to pass the micro-guide wire through the occlusion segment at an invisible angle, attention should be paid to the deviation of the axial direction of the blood vessel; otherwise, the blood vessel would perforate and rupture. In this study, we used the ipsilateral advanced arterial image as a road map to simultaneously display the distal and proximal ends of the occluded vessel so that the operator can more intuitively observe the direction of the occluded vessel and predictably manipulate the guide wire; this approach reduced complications and increased the success rate of recanalization.
There were some limitations to our study. First, the study was a single-center study and relatively small sample size. Second, this study was non-randomized controlled trials and lack of quantitative perfusion studies comparing regional blood volumes. Third, patient's heterogeneity and Chinese patients enrolled only may produce some bias to affect the generalization of the study. Finally, the lack of long-term follow-up data may limit the assessment of the overall restenosis rates.
In conclusion, endovascular recanalization may be feasible and safe in carefully selected patients with non-acute symptomatic MCAO, and it represents a potential alternative treatment approach, especially in low- and medium-risk groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Zhengzhou University People's hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JX established the study idea and designed the manuscript structure. KZ and HL were responsible for the data collection. ZW analyzed the data and wrote the manuscript. TL modified and revised the manuscript. All authors have read and approved the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1036661/full#supplementary-material
References
1. Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke. (2008) 39:2396–9. doi: 10.1161/STROKEAHA.107.505776
2. Marshall RS, Festa JR, Cheung YK, Chen R, Pavol MA, Derdeyn CP, et al. Cerebral hemodynamics and cognitive impairment: baseline data from the RECON trial. Neurology. (2012) 78:250–5. doi: 10.1212/WNL.0b013e31824365d3
3. Galkin P, Gushcha A, Chechetkin A, Krotenkova I. Superficial temporal artery to middle cerebral artery bypass with interposed saphenous vein graft in patients with atherosclerotic internal carotid artery occlusive disease and impaired cerebral hemodynamics. J Neurosurg Sci. (2017) 61:22–32. doi: 10.23736/S0390-5616.16.03234-3
4. Kanamaru K, Araki T, Kawakita F, Hamada K, Kanamaru H, Matsuura K, et al. STA-MCA bypass for the treatment of ischemic stroke. Acta Neurochir Suppl. (2011) 112:55–7. doi: 10.1007/978-3-7091-0661-7_10
5. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. (2018) 378:11–21. doi: 10.1056/NEJMoa1706442
6. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. (2018) 378:708–18. doi: 10.1056/NEJMoa1713973
7. Fan YL, Wan JQ, Zhou ZW, Chen L, Wang Y, Yao Q, et al. Neurocognitive improvement after carotid artery stenting in patients with chronic internal carotid artery occlusion: a prospective, controlled, single-center study. Vasc Endovascular Surg. (2014) 48:305–10. doi: 10.1177/1538574414525863
8. Zanaty M, Howard S, Roa JA, Alvarez CM, Kung DK, McCarthy DJ, et al. Cognitive and cerebral hemodynamic effects of endovascular recanalization of chronically occluded cervical internal carotid artery: single-center study and review of the literature. J Neurosurg. (2019) 132:1158–66. doi: 10.3171/2019.1.JNS183337
9. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. (2000) 21:643–6.
10. Winder K, Seifert F, Ohnemus T, Sauer EM, Kloska S, Dörfler A, et al. Neuroanatomic correlates of poststroke hyperglycemia. Ann Neurol. (2015) 77:262–8. doi: 10.1002/ana.24322
11. Stone GW, Colombo A, Teirstein PS, Moses JW, Leon MB, Reifart NJ, et al. Percutaneous recanalization of chronically occluded coronary arteries: procedural techniques, devices, and results. Catheter Cardiovasc Interv. (2005) 66:217–36. doi: 10.1002/ccd.20489
12. Gao F, Guo X, Han J, Sun X, Zhou Z, Miao Z. Endovascular recanalization for symptomatic non-acute middle cerebral artery occlusion: proposal of a new angiographic classification. J Neurointerv Surg. (2021) 13:900–5. doi: 10.1136/neurintsurg-2020-016692
13. Ma N, Mo DP, Gao F, Miao ZR. Endovascular recanalization for chronic symptomatic middle cerebral artery total occlusion. J Neurointerv Surg. (2013) 5:e15. doi: 10.1136/neurintsurg-2012-010304
14. Gao F, Sun X, Zhang H, Ma N, Mo D, Miao Z. Endovascular recanalization for nonacute intracranial vertebral artery occlusion according to a new classification. Stroke. (2020) 51:3340–3. doi: 10.1161/STROKEAHA.120.030440
15. Hasan D, Zanaty M, Starke RM, Atallah E, Chalouhi N, Jabbour P, et al. Feasibility, safety, and changes in systolic blood pressure associated with endovascular revascularization of symptomatic and chronically occluded cervical internal carotid artery using a newly suggested radiographic classification of chronically occluded cervical internal carotid artery: pilot study. J Neurosurg. (2018) 10:3171. doi: 10.3171/2018.1.JNS172858
16. Shojima M, Nemoto S, Morita A, Miyata T, Namba K, Tanaka Y, et al. Protected endovascular revascularization of subacute and chronic total occlusion of the internal carotid artery. AJNR Am J Neuroradiol. (2010) 32:481–6. doi: 10.3174/ajnr.A1843
17. Takagi T, Yoshimura S, Yamada K, Enomoto Y, Iwama T. Angioplasty and stenting of totally occluded common carotid artery at the chronic stage. Neurol Med Chir (Tokyo). (2010) 50:998–1000. doi: 10.2176/nmc.50.998
18. Bhatt A, Majid A, Kassab M, Gupta R. Chronic total symptomatic carotid artery occlusion treated successfully with stenting and angioplasty. J Neuroimaging. (2009) 19:68–71. doi: 10.1111/j.1552-6569.2008.00212.x
19. Chen YH, Leong WS, Lin MS, Huang CC, Hung CS, Li HY, et al. Predictors for successful endovascular intervention in chronic carotid artery total occlusion. JACC Cardiovasc Interv. (2016) 9:1825–32. doi: 10.1016/j.jcin.2016.06.015
20. Puma JA, Sketch MH Jr, Tcheng JE, Harrington RA, Phillips HR, Stack RS, et al. Percutaneous revascularization of chronic coronary occlusions: an overview. J Am Coll Cardiol. (1995) 26:1–11. doi: 10.1016/0735-1097(95)00156-T
21. Roy S, Sharma J. Role of CT coronary angiography in recanalization of chronic total occlusion. Curr Cardiol Rev. (2015) 11:317–22. doi: 10.2174/1573403X11666150909105616
22. Touma G, Ramsay D, Weaver J. Chronic total occlusions-current techniques and future directions. Int J Cardiol Heart Vasc. (2015) 7:28–39. doi: 10.1016/j.ijcha.2015.02.002
Keywords: endovascular, recanalization, anterior circulation, symptomatic, middle cerebral artery, non-acute phase
Citation: Xia J, Li H, Zhang K, Wang Z and Li T (2023) Clinical study on endovascular recanalization of non-acute symptomatic middle cerebral artery occlusion. Front. Neurol. 13:1036661. doi: 10.3389/fneur.2022.1036661
Received: 04 September 2022; Accepted: 09 December 2022;
Published: 09 January 2023.
Edited by:
Ichiro Nakagawa, Nara Medical University, JapanReviewed by:
Huaizhang Shi, First Affiliated Hospital of Harbin Medical University, ChinaFangwang Fu, Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical University, China
Copyright © 2023 Xia, Li, Zhang, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tianxiao Li,  ZHIuMWl0aWFueGlhb0B2aXAuMTYzLmNvbQ==
ZHIuMWl0aWFueGlhb0B2aXAuMTYzLmNvbQ==
 Jinchao Xia
Jinchao Xia Hao Li
Hao Li Ziliang Wang
Ziliang Wang