
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 11 November 2022
Sec. Endovascular and Interventional Neurology
Volume 13 - 2022 | https://doi.org/10.3389/fneur.2022.1029613
This article is part of the Research Topic Safety and Efficacy of Stents and Flow Diverters Used for Embolization of Acutely-Ruptured Intracranial Aneurysms in the Acute Stage View all 11 articles
 Rundong Chen†
Rundong Chen† Yanpeng Wei†
Yanpeng Wei† Guanghao Zhang†
Guanghao Zhang† Renkun Zhang
Renkun Zhang Xiaoxi Zhang
Xiaoxi Zhang Dongwei Dai
Dongwei Dai Qiang Li
Qiang Li Rui Zhao
Rui Zhao Yi Xu
Yi Xu Qinghai Huang
Qinghai Huang Pengfei Yang
Pengfei Yang Qiao Zuo*
Qiao Zuo* Jianmin Liu*
Jianmin Liu*Background: Stenting is a common clinical practice to treat acutely ruptured intracranial aneurysm (RIA). Although multiple studies have demonstrated its long-term safety and effectiveness, there is currently a lack of bibliometric analysis on stent application in acutely RIA. This study sought to summarize the current status of research in this field and lay a foundation for further study.
Materials and methods: Related publications were searched in the Web of Science Core Collection (WoSCC) database. Data analysis and visualization were performed by R and CiteSpace software.
Results: A total of 275 publications published in English from 1997 to 2022 were included in this study. The growth of publications slowed down. The reference co-citation network identified 13 clusters with a significant network (Q = 0.7692) and convincing clustering (S = 0.9082). The research focus was acutely RIA and the application of stents during interventional procedures. The main trends of research were: (1) development of materials, and (2) safety of stent application in acutely RIA. The United States contributed the most articles, and Jianmin Liu was the most prolific author. Mayo Clinic was the leading institution in this field. Most articles were published in Interventional Neuroradiology.
Conclusions: This study analyzed the research trends, hotspots and frontiers of stent application in acutely RIA. It is our hope that the results obtained could provide useful information to researchers to get a clearer picture about their future research directions in this field.
The past decades have witnessed remarkable advances in the endovascular treatment of acutely ruptured intracranial aneurysms (RIA), and the safety and effectiveness of stent application in acutely RIA have been explored (1). RIA is the most common cause of subarachnoid hemorrhage (SAH), which is often a devastating event with high mortality and morbidity (2). About 4% and 1% SAH patients have an increased risk of rebleeding in the first 24 h and every day in the first month respectively (3). Endovascular and surgical treatments are available for aneurysm repair, which are the only effective treatments to prevent rebleeding at present (4). However, for some complex aneurysms, giant aneurysms and aneurysms with a low fundus-to-neck ratio, specialized skills are required to obtain satisfactory embolization, including stent-assisted coiling (SAC), balloon-assisted coiling (BAC), flow diverters (FD), and the use of new embolic materials including liquids (5–7). Stent placement has been commonly applied in acutely RIA, including classic laser-cut stents, braided stents, drug-eluting stents, and covered stents (8–10). These skills are expected to enable aneurysms previously considered unsuitable for the endovascular procedure to be treated in the future (5, 11). Early studies suggested a high incidence of adverse events with stent application in acutely RIA, including stent-related thrombosis and hemorrhagic complications due to the use of antiplatelet drugs (12–14). However, with the progress in endovascular skills, materials, devices and antiplatelet strategies, the perioperative safety of stent application in acutely RIA has been continuously improved (1, 15–17). Exploration and summary of the research trends of stent application in acutely RIA treatment is significant to those who want to carry out this research.
Bibliometrics uses statistical methods to analyze publications, especially those of scientific content. Bibliometric mapping allows data to be presented in ways that make relationships more understandable and provide researchers with relatively macro information (18). The method of bibliometric analysis has become increasingly mature and has been widely used in clinical disease research (19).
However, there is a lack of data on bibliometric analysis of stent application in acutely RIA. To fill this gap, we conducted a bibliometric study to discuss publications on stent application in acutely RIA from 1997 to 2022 both quantitatively and qualitatively. In addition, we summarized the main research trends and frontiers, provided the latest insights and findings, and looked forward to the future development of this field.
The primary objective of the study was to systematically map how stenting is evolved in the treatment of patients with acutely RIA, and identify the main trends and hot topics of research in this field by constructing networks of co-cited references and co-occurring keywords. The secondary objective was to render the research network in terms of countries, authors, institutions and journals.
We searched publications from the Web of Science Core Collection (WoSCC) through the Science Citation Index Expanded (SCI-E). The search terms combined Medical Subject Headings words and keywords:[TS = (stent*) OR TS=(“stent assisted”)] AND TS=(“ruptured intracranial aneurysm*”). The language was limited to “English.” The main document type was “articles” and “reviews” with no time limitation. All the search result records, including the title, author information, keyword, abstract and reference were exported in TXT format for analysis on July 15, 2022.
The raw files were analyzed by R software (4.1.3) and Citespace software (6.1.R2). The “bibliometrix” R package is an open-source tool for quantitative research in bibliometrics. It summarizes the preliminary information, country scientific production, and the cumulate occurrence of journal articles in this study. CiteSpace is a Java application for visualizing patterns and trends in scientific publications by focusing on identifying critical points in developing a particular field. It was used to explore networks of co-cited references and co-occurring keywords, as well as collaboration networks between countries, authors, institutions, and journals.
A total of 275 publications about stent application in acutely RIA from 1997 to 2022 were included in this study, of which 236 were original articles, and 39 were review articles (Figure 1). The growth of the overall number of articles and the mean article citations per year slowed down. The COVID-19 pandemic may lead to a decline. The cumulative number of citations for these publications was 5,041 (4,464 without self-citations), with a mean number of citations per item of 18.33. The mean H-index in this field was 38. The analysis showed significant progress in this field in the past 20 years, especially in 2013 and 2019.
Co-citation references were two or more articles appearing simultaneously in the references of other documents. The association of co-citations may reveal how groupings have evolved independently from the original publication (19). The top 10 most cited documents and the top 10 most cited references were shown in Tables 1, 2 respectively. There were 693 nodes and 2,830 links constructed by Citespace for a map of reference co-citations with corresponding clusters (Figures 2A,B). The first article was issued in 1997 (20). At that time, stenting was attempted for the treatment of acutely RIA through endovascular therapy. Thirteen clusters were identified in this network with significant modularity Q scores and silhouette scores (Q = 0.7692, S = 0.9082). We found a research focus and two different research trends in this map. The research focus was acutely SAH and the application of stents during interventional procedures. These clusters, with the indication of the label, silhouette score, size, the mean year of publications, and most representative reference were: cluster#5 (cerebrovascular disease, S = 0.912, size = 49, mean year = 2009) (21), cluster#3 (subarachnoid hemorrhage, S = 0.903, size = 71, mean year = 2011) (22), cluster #7 (interventional radiology, S=0.864, size = 32, mean year = 2016) (23), and cluster#15 (stent, S = 0.994, size = 5, mean year = 2018) (24). The first trend was concerned with the development of materials. It started with cluster #6 (liquid embolic agents, S = 0.993, size = 48, mean year = 2002) (25), which developed research on cluster #2 (neuroform stent, S = 0.908, size = 81, mean year = 2007) (26) and cluster #10 (matrix coil, S = 0.959, size = 16, mean year = 2008) (27). More recently, these clusters became cluster #0 (pipeline embolization device, S = 0.851, size = 92, mean year = 2014) (28), with strong links to cluster#1 (woven endobridge, S = 0.875, size = 89, mean year = 2020) (29). The second major research trend was concerned with the safety of stent application in acutely RIA. This trend began with cluster #9 (vascular accident, S = 0.952, size = 17, mean year = 2014) (30) and cluster #14 (para-ophthalmic, S = 0.996, size = 10, mean year = 2016) (31), which has currently evolved into cluster#4 (safety, S = 0.941, size = 59, mean year = 2019) (32).
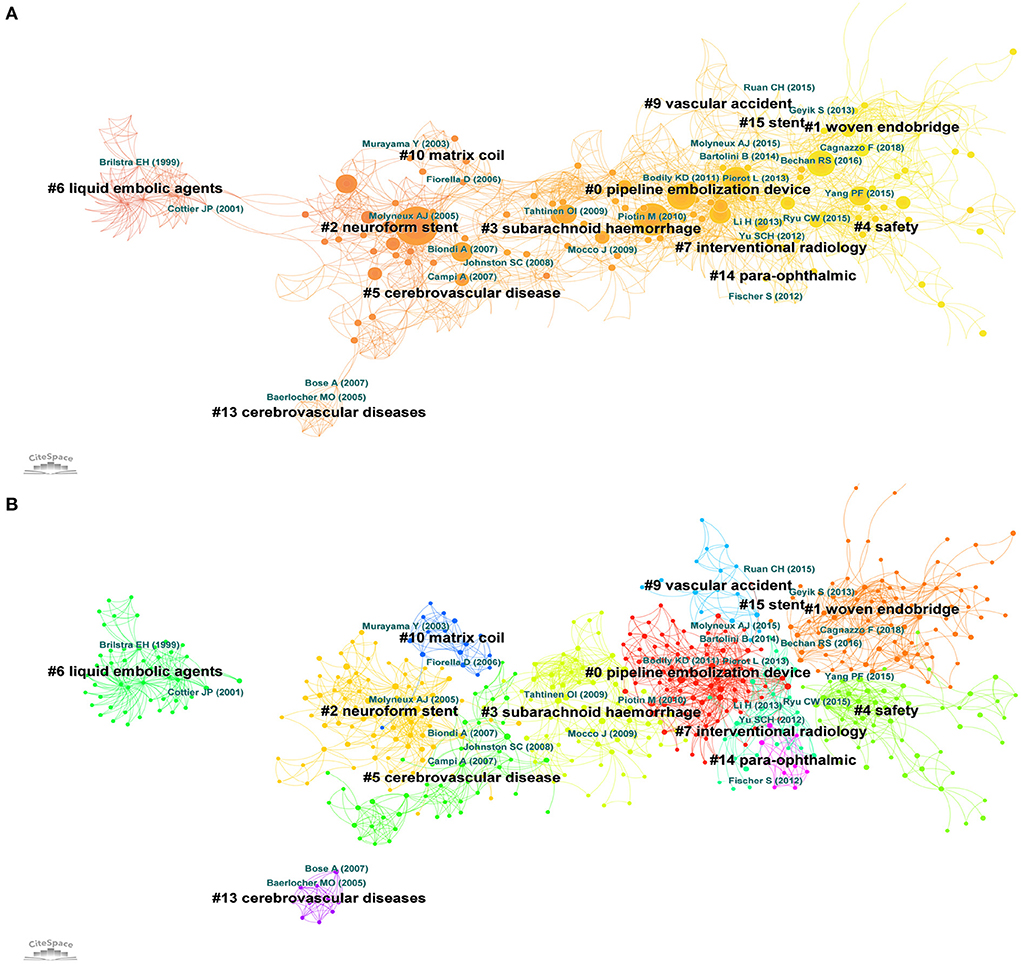
Figure 2. (A) Co-citation reference network with cluster visualization. The node's size (article) is proportional to the number of times the publication has been co-cited. (B) Visualization map of the corresponding clusters. Publication topics of the same type are clustered in the same color block.
We extracted the timeline of the co-occurring keywords network (1997–2022) by Citespace (Figure 3A). Eleven clusters of keywords were identified with modularity Q score = 0.3962 and silhouette score = 0.7111. The most critical cluster was “clopidogrel,” followed by “intracranial aneurysm,” “coil embolization,” “isat” (international subarachnoid aneurysm trial), “covered stent,” “dsa,” “antiplatelet therapy,” “aneurysm coiling,” “stent assisted coiling,” “retreatment,” and “antiplatelet drug resistance.” We further extracted the same network from 2015 to 2022 (Figure 3B), and identified nine clusters of keywords with modularity Q score = 0.3924 and silhouette score = 0.7414. The most essential cluster was “ruptured intracranial aneurysm,” followed by “coil embolization,” “flow diversion,” “stent assisted coiling,” “vascular disorders,” “therapy,” “endovascular occlusion,” “cerebrovascular disease,” and “neuroradiography.” Moreover, keyword bursts represented keywords that were frequently cited over a period of time (Figure 3C). The earliest burst keyword was “Gugliemi detachable coil,” which began in 2002 and lasted 8 years. Subsequently emerging keywords were “neuroform stent,” “trial isat,” “endovascular coiling,” and “reconstruction,” all of which focused on the feasibility of the stent application in acutely RIA. These keywords further evolved into “stent,” “single center experience,” “outcome,” and “stent assisted coiling” in 2013, which were mainly concerned with the safety of stent application in acutely RIA. More recently, these keywords became “flow diversion,” “complication,” “therapy,” “risk,” and “efficacy.”
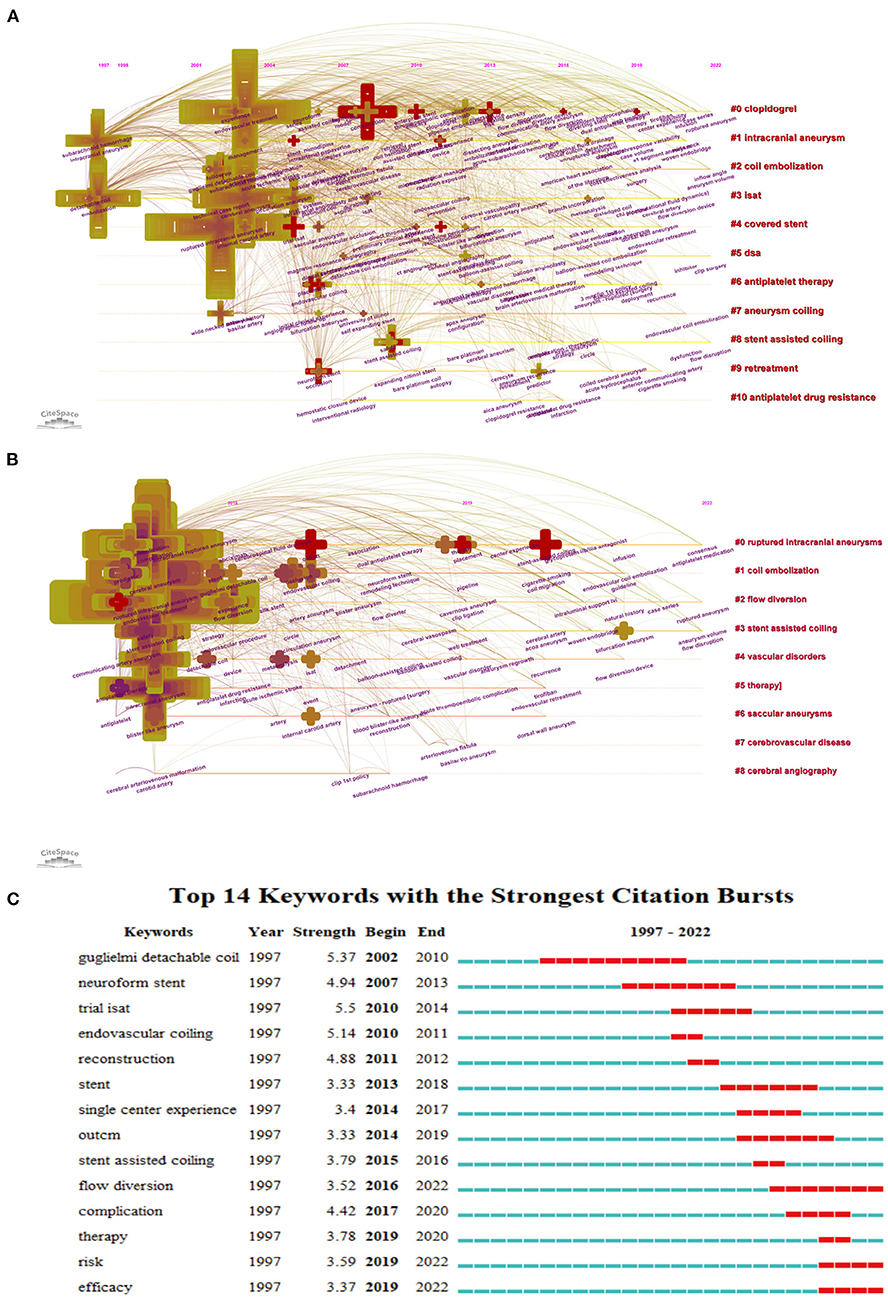
Figure 3. Timeline visualization of co-occurring author keyword networks [(A) 1980–2021 and (B) 2015–2022]. The size of a cross is proportional to the burstness of keywords co-occurrence. The co-occurring keyword network is weighted on total link strength across different keyword nodes and scored on the mean publication years. The clusters are labeled in red at the right of the timeline maps. (C) Top14 keywords with the strongest citation bursts.
Based on the analysis of cooperation networks across countries or regions, 37 countries or regions were identified, of which the United States (US) contributed the most with 102 publications, followed by the People's Republic of China (n = 57), South Korea (n = 29), Germany (n = 22), and France (n = 21) (Supplementary Table 1). A country scientific production map was shown in Figure 4A and the cooperation networks across countries were mapped in Figure 4B. The US, as the landmark node, had extensive collaborations with other countries or regions worldwide.
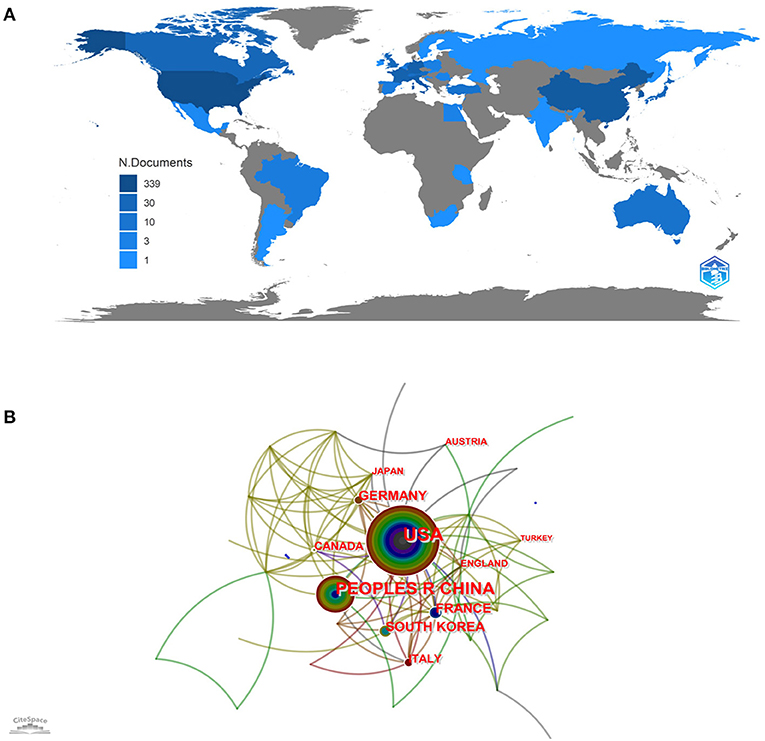
Figure 4. (A) Country-specific production. Dark blue = high productivity. Gray = no documents. (B) Country cooperation network map. The size of each node represents the number of publications published by the country, and the thickness of each link represents the strength of the cooperative relationship between two countries.
The cooperation network between authors is shown in Figure 5A, and the top 10 influential authors are shown in Supplementary Table 2. There were 477 nodes and 1,075 links, and the results showed that Jianmin Liu contributed the largest number (n = 16) of publications with the highest centrality (0.17), followed by Jeongjun Lee (n = 9), NohraChalouhi (n = 9), Robert M Starke (n = 8), and David J Fiorella (n = 7). Jianmin Liu and Jeongjun Lee constituted the two pivot nodes that connected the network diagram, which was why these two authors had a higher degree of centrality. The collaboration between other authors was relatively decentralized. The cooperation network between institutions is shown in Figure 5B. The top 5 institutions by citation counts were Mayo Clinic (n = 9), Thomas Jefferson University (n = 9), Shanghai Jiao Tong University (n = 8), Capital Medical University (n = 8), and Jefferson Hospital for Neuroscience (n = 7) (Supplementary Table 3).
The top five journals with the most references were the American Journal of Neuroradiology (n = 26), Journal of NeuroInterventional Surgery (n = 25), Neurosurgery (n = 24), interventional Neuroradiology (n = 21), and World Neurosurgery (n = 16) (Figure 6A, Supplementary Table 4). The co-cited journal network over the past 20 years is shown in (Figure 6B). The American Journal of Neuroradiology, Neurosurgery, Journal of Neurosurgery, Stroke and Lancet were the top five journals that enjoyed the largest number of citations (Supplementary Table 5). This shows that the American Journal of Neuroradiology made the most outstanding contribution and had the greatest influence in this field.

Figure 6. (A) Source growth of publications. (B) The co-cited journal network with cluster visualization.
This study revealed the overall research results of stent application in acutely RIA in the past 25 years. The annual number of papers and literature trends may reflect the development speed and progress of research in this field. Before 2006, the number of publications in this field was roughly the same yearly. From 2006 to 2019, the number of publications increased obviously, reflecting the growing interest in this field, especially the evolution of materials and the safety in acutely RIA.
The co-cited references with the corresponding cluster network (1997–2022) described the coherent links between 13 different clusters and revealed the evolution of research trends about stent application in acutely RIA. The first trend was the evolution of materials, from liquid embolic agents to neuroform stents, then pipeline embolization devices and woven endobridge (WEB). The development of these new and exciting devices and materials has helped neurointerventionalists successfully treat aneurysmal SAH (16, 33, 34). But as the surface of the current stents is highly thrombotic, a dual antiplatelet regimen is required, which is still a controversial issue in the acute stage of SAH (35, 36). Therefore, the second major trend is the safety of stent application research in acutely RIA. In this aspect, the most concerned issues of researchers are the risk of increased hemorrhagic complications and acute stent thrombosis or even thromboembolic occlusion (37, 38), especially the ophthalmic artery (39). In addition, the focus on the past seven years showed that the latest research trends also aimed at developing materials and exploring technical security (Supplementary Figure 1). Analysis of the co-occurring keyword networks and burst keywords such as clopidogrel, ISAT, covered stent and antiplatelet resistance also verified these findings. The burst keywords in recent years, including flow diversion, complications, therapy, risk, and efficacy, also confirmed the current hot topic and research focus (Supplementary Figure 2). The safety and efficacy of stent application in acutely RIA have been a hot topic of discussion in recent years (32, 40, 41). Antiplatelet strategies have been found to be closely related to increased hemorrhagic complications. Furthermore, early use of anticoagulants after stent application in acutely RIA was identified as a risk factor for postoperative hemorrhagic complications. And dual antiplatelet agents were preferred by DELPHI consensus as a standard approach with aspirin and a glycoprotein IIb/IIIa receptor (35). Alternations based on anti-thrombogenic device coating might make stents used safely in the treatment of RIA (42). In terms of material selection, stents and coils made from LVIS and hydrogel are safer in the treatment of ruptured aneurysms because they can provide a higher immediate embolization rate (43, 44). For blood blister-like aneurysms, FD was a more sensible choice at present, owing to its high metal coverage and the change in blood flow to promote intrasaccular thrombosis for better isolating blood from entering the aneurysm (45). Although a wealth of experience and treatment guidelines have been gleaned from 25 years of research into stent application in acutely ruptured intracranial aneurysms, many questions still need to be further addressed. Future research may focus on the development of novel stent materials which would reduce the reliance on antiplatelet drugs during the perioperative period and consequently reduce the potential risk of hemorrhagic complications.
As shown in Supplementary Table 1, the country with the most significant number of publications was the US. Centrality represents the algorithm that calculates unweighted shortest paths between all pairs of nodes in a graph. The US had the highest centrality of 0.87, indicating that the US occupied a leading position in this field. The further cluster analysis revealed that the US and the People's Republic of China mainly focused on preoperative evaluation of stent application in acutely RIA (46) (Supplementary Figure 3). The most productive author was Jianmin Liu, and the author team headed by him was mainly concerned with stent placement (1). Studies by other authors were more concerned with endobridge devices and balloon remodeling (47) (Supplementary Figure 4). Among the top ten research institutions, five were in the US, four were in the People's Republic of China, and the rest in South Korea. However, the centrality of institutions is low, indicating a lack of academic collaboration between institutions. Nevertheless, cluster analysis suggested that some institutional collaborations still contributed to the multicenter experience and perioperative preparation of stent application in acutely RIA (48) (Supplementary Figure 5). Publication source analysis can help researchers identify core journals in their fields, and top-ranked co-cited journals can serve as authoritative references. The American Journal of Neuroradiology had the greatest number of articles published and the greatest number of articles cited simultaneously. In addition, those top co-cited and prolific journals mainly published systematic reviews, endovascular treatment devices, and recent advances in this field (29, 49) (Supplementary Figure 6).
This study inevitably had some limitations. The data were simply retrieved from the WoSCC database, which may lead to incomplete literature collection. In addition, the literature retrieved was limited to articles published in English, leading to some linguistic bias in the study results. With further research and exploration in this field, the findings of this study may be different from the realistic results in the future.
To the best of our knowledge, this is the first systematic and multidimensional analysis of the research trends, hotspots and frontiers of stent application in acutely RIA in an objective way, which we hope can be used as a comprehensive guide for clinicians and scholars engaged in this field, and help researchers get a clearer picture of their future research directions.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
RC, YW, and GZ made substantial contributions to the conception and design, acquisition of data, analysis, and drafting of the manuscript. QZ, JL, RZhang, XZ, DD, QL, RZhao, YX, QH, and PY assisted in the evaluation of analysis and their interpretation. All authors read and approved the final manuscript.
This research was supported by the 234 Discipline Peak Climbing Program of Changhai Hospital (2020YXK060).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1029613/full#supplementary-material
Supplementary Figure 1. (A) Co-citation reference network with cluster visualization from 2015 to 2022. (B) Visualization map of the corresponding clusters from 2015 to 2022. (C) Timeline visualization of co-citation references network. (D) Top 12 references with the strongest citation bursts.
Supplementary Figure 2. Co-occurring author keyword networks with cluster visualization [(A) 1980–2021 and (C) 2015–2022]. Visualization map of the corresponding clusters [(B) 1980–2021 and (D) 2015–2022].
Supplementary Figure 3. (A) Country cooperation network with cluster visualization. (B) Timeline visualization of the country cooperation network.
Supplementary Figure 4. (A) Author cooperation network with cluster visualization. (B) Timeline visualization of the author cooperation network.
Supplementary Figure 5. (A) Institution cooperation network with cluster visualization. (B) Timeline visualization of the institution cooperation network.
Supplementary Figure 6. (A) Co-cited journal network map. (B) Timeline visualization of the co-cited journals network map.
1. Zhang X, Zuo Q, Tang H, Xue G, Yang P, Zhao R, et al. Stent assisted coiling versus non-stent assisted coiling for the management of ruptured intracranial aneurysms: a meta-analysis and systematic review. J Neurointerv Surg. (2019) 11:489–96. doi: 10.1136/neurintsurg-2018-014388
2. Schatlo B, Fung C, Stienen MN, Fathi AR, Fandino J, Smoll NR, et al. Incidence and outcome of aneurysmal subarachnoid hemorrhage: the swiss study on subarachnoid hemorrhage (Swiss SOS). Stroke. (2021) 52:344–7. doi: 10.1161/STROKEAHA.120.029538
3. Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. (2009) 40:994–1025. doi: 10.1161/STROKEAHA.108.191395
4. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. (2012) 43:1711–37. doi: 10.1161/STR.0b013e3182587839
5. Pierot L, Wakhloo AK. Endovascular treatment of intracranial aneurysms: current status. Stroke. (2013) 44:2046–54. doi: 10.1161/STROKEAHA.113.000733
6. Lin N, Brouillard AM, Keigher KM, Lopes DK, Binning MJ, Liebman KM, et al. Utilization of Pipeline embolization device for treatment of ruptured intracranial aneurysms: US multicenter experience. J Neurointerv Surg. (2015) 7:808–15. doi: 10.1136/neurintsurg-2014-011320
7. Spiotta AM, Bellon RJ, Bohnstedt BN, Park MS, Sattur MG, Woodward BK, et al. Registry: Safety and Performance of the Penumbra SMART COIL System for Patients With Intracranial Aneurysms 4 mm and Smaller. Neurosurgery. (2022) 91:555–61. doi: 10.1227/neu.0000000000002073
8. Voigt P, Schob S, Jantschke R, Nestler U, Krause M, Weise D, et al. Stent-assisted coiling of ruptured and incidental aneurysms of the intracranial circulation using moderately flow-redirecting, braided leo stents-initial experience in 39 patients. Front Neurol. (2017) 8:602. doi: 10.3389/fneur.2017.00602
9. Zhao Y, Liu Z, Sun R, Pan L, Yang M, Song J, et al. The clinical efficacy analysis of treatment with a willis covered stent in traumatic pseudoaneurysm of the internal carotid artery. Front Neurol. (2021) 12:739222. doi: 10.3389/fneur.2021.739222
10. Zhang Y, Wang J, Xiao J, Fang T, Hu N, Li M, et al. An electrospun fiber-covered stent with programmable dual drug release for endothelialization acceleration and lumen stenosis prevention. Acta Biomater. (2019) 94:295–305. doi: 10.1016/j.actbio.2019.06.008
11. Chua MMJ, Silveira L, Moore J, Pereira VM, Thomas AJ, Dmytriw AA. Flow diversion for treatment of intracranial aneurysms: Mechanism and implications. Ann Neurol. (2019) 85:793–800. doi: 10.1002/ana.25484
12. Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke. (2013) 44:1348–53. doi: 10.1161/STROKEAHA.111.000641
13. Muto M, Giurazza F, Ambrosanio G, Vassallo P, Briganti F, Tecame M, et al. Stent-assisted coiling in ruptured cerebral aneurysms: multi-center experience in acute phase. Radiol Med. (2017) 122:43–52. doi: 10.1007/s11547-016-0686-6
14. Lodi YM, Latorre JG, El-Zammar Z, Swarnkar A, Deshaies E, Fessler RD. Stent assisted coiling of the ruptured wide necked intracranial aneurysm. J Neurointerv Surg. (2012) 4:281–6. doi: 10.1136/neurintsurg-2011-010035
15. Zuo Q, Yang P, Lv N, Huang Q, Zhou Y, Zhang X, et al. Safety of coiling with stent placement for the treatment of ruptured wide-necked intracranial aneurysms: a contemporary cohort study in a high-volume center after improvement of skills and strategy. J Neurosurg. (2018) 131:435–41. doi: 10.3171/2018.3.JNS172199
16. Xue G, Zuo Q, Tang H, Zhang X, Duan G, Feng Z, et al. Comparison of low-profiled visualized intraluminal support stent-assisted coiling and coiling only for acutely ruptured intracranial aneurysms: safety and efficacy based on a propensity score-matched cohort study. Neurosurgery. (2020) 87:584–91. doi: 10.1093/neuros/nyaa110
17. Yan Y, He X, Fang Y, Xu Y, Hong B, Liu J, et al. The safety and efficacy of low-dosage tirofiban for stent-assisted coiling of ruptured intracranial aneurysms. Neurosurg Rev. (2021) 44:2211–8. doi: 10.1007/s10143-020-01398-w
18. Nakagawa S, Samarasinghe G, Haddaway NR, Westgate MJ, O'Dea RE, Noble DWA, et al. Research Weaving: Visualizing the Future of Research Synthesis. Trends Ecol Evol. (2019) 34:224–38. doi: 10.1016/j.tree.2018.11.007
19. Sabe M, Pillinger T, Kaiser S, Chen C, Taipale H, Tanskanen A, et al. Half a century of research on antipsychotics and schizophrenia: a scientometric study of hotspots, nodes, bursts, and trends. Neurosci Biobehav Rev. (2022) 136:104608. doi: 10.1016/j.neubiorev.2022.104608
20. Higashida RT, Smith W, Gress D, Urwin R, Dowd CF, Balousek PA, et al. Intravascular stent and endovascular coil placement for a ruptured fusiform aneurysm of the basilar artery. Case report and review of the literature. J Neurosurg. (1997) 87:944–9. doi: 10.3171/jns.1997.87.6.0944
21. Campi A, Ramzi N, Molyneux AJ, Summers PE, Kerr RS, Sneade M, et al. Retreatment of ruptured cerebral aneurysms in patients randomized by coiling or clipping in the International Subarachnoid Aneurysm Trial (ISAT). Stroke. (2007) 38:1538–44. doi: 10.1161/STROKEAHA.106.466987
22. Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. (2009) 64:632-42; discussion 642-3; quiz N6. doi: 10.1227/01.NEU.0000339109.98070.65
23. Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. (2013) 44:29–37. doi: 10.1161/STROKEAHA.112.663559
24. Geyik S, Yavuz K, Yurttutan N, Saatci I, Cekirge HS. Stent-assisted coiling in endovascular treatment of 500 consecutive cerebral aneurysms with long-term follow-up. AJNR Am J Neuroradiol. (2013) 34:2157–62. doi: 10.3174/ajnr.A3574
25. Brilstra EH, Rinkel GJ, van der Graaf Y, van Rooij WJ, Algra A. Treatment of intracranial aneurysms by embolization with coils: a systematic review. Stroke. (1999) 30:470–6. doi: 10.1161/01.STR.30.2.470
26. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. (2005) 366:809–17. doi: 10.1016/S0140-6736(05)67214-5
27. Fiorella D, Albuquerque FC, McDougall CG. Durability of aneurysm embolization with matrix detachable coils. Neurosurgery. (2006) 58:51–9; discussion 51-9. doi: 10.1227/01.NEU.0000194190.45595.9E
28. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. (2010) 41:110–5. doi: 10.1161/STROKEAHA.109.558114
29. Cagnazzo F, di Carlo DT, Cappucci M, Lefevre PH, Costalat V, Perrini P. Acutely ruptured intracranial aneurysms treated with flow-diverter stents: a systematic review and meta-analysis. AJNR Am J Neuroradiol. (2018) 39:1669–75. doi: 10.3174/ajnr.A5730
30. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT). Lancet. (2015) 385:691–7. doi: 10.1016/S0140-6736(14)60975-2
31. Puffer RC, Kallmes DF, Cloft HJ, Lanzino G. Patency of the ophthalmic artery after flow diversion treatment of paraclinoid aneurysms. J Neurosurg. (2012) 116:892–6. doi: 10.3171/2011.11.JNS111612
32. Ryu CW, Park S, Shin HS, Koh JS. Complications in stent-assisted endovascular therapy of ruptured intracranial aneurysms and relevance to antiplatelet administration: a systematic review. AJNR Am J Neuroradiol. (2015) 36:1682–8. doi: 10.3174/ajnr.A4365
33. Manning NW, Cheung A, Phillips TJ, Wenderoth JD. Pipeline shield with single antiplatelet therapy in aneurysmal subarachnoid haemorrhage: multicentre experience. J Neurointerv Surg. (2019) 11:694–8. doi: 10.1136/neurintsurg-2018-014363
34. Youssef PP, Dornbos Iii D, Peterson J, Sweid A, Zakeri A, Nimjee SM, et al. Woven EndoBridge (WEB) device in the treatment of ruptured aneurysms. J Neurointerv Surg. (2021) 13:443–6. doi: 10.1136/neurintsurg-2020-016405
35. Ospel JM, Brouwer P, Dorn F, Arthur A, Jensen ME, Nogueira R, et al. Antiplatelet management for stent-assisted coiling and flow diversion of ruptured intracranial aneurysms: a DELPHI consensus statement. AJNR Am J Neuroradiol. (2020) 41:1856–62. doi: 10.3174/ajnr.A6814
36. Lobsien D, Clajus C, Behme D, Ernst M, Riedel CH, Abu-Fares O, et al. Aneurysm treatment in acute SAH with hydrophilic-coated flow diverters under single-antiplatelet therapy: a 3-center experience. AJNR Am J Neuroradiol. (2021) 42:508–15. doi: 10.3174/ajnr.A6942
37. Takase H, Tatezuki J, Salem MM, Tayama K, Nakamura Y, Burkhardt JK, et al. Antiplatelet therapy for standalone coiling of ruptured intracranial aneurysms: a systematic review and meta-analysis. J Neurointerv Surg. (2022). doi: 10.1136/neurintsurg-2021-018346
38. Roh H, Kim J, Bae H, Chong K, Kim JH, Suh SI, et al. Comparison of stent-assisted and no-stent coil embolization for safety and effectiveness in the treatment of ruptured intracranial aneurysms. J Neurosurg. (2020) 133:814–20. doi: 10.3171/2019.5.JNS19988
39. Yoon CH, Lee HW, Kim YS, Lee SW, Yeom JA, Roh J, et al. Preliminary study of tirofiban infusion in coil embolization of ruptured intracranial aneurysms. Neurosurgery. (2018) 82:76–84. doi: 10.1093/neuros/nyx177
40. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF. Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol. (2011) 32:1232–6. doi: 10.3174/ajnr.A2478
41. Yang PF, Huang QH, Zhao WY, Hong B, Xu Y, Liu JM. Safety and efficacy of stent placement for treatment of intracranial aneurysms: a systematic review. Chin Med J (Engl). (2012) 125:1817–23.
42. Aguilar Perez M, AlMatter M, Hellstern V, Wendl C, Ganslandt O, Bäzner H, et al. Use of the pCONus HPC as an adjunct to coil occlusion of acutely ruptured aneurysms: early clinical experience using single antiplatelet therapy. J Neurointerv Surg. (2020) 12:862–8. doi: 10.1136/neurintsurg-2019-015746
43. Jiang C, Yu Y, Hong B, Fu QL, Liu JM, Huang QH. Stent-assisted coil embolization for the treatment of ruptured aneurysms at the anterior circulation: comparison between HydroSoft coils and bare platinum coils. Cardiovasc Intervent Radiol. (2014) 37:935–41. doi: 10.1007/s00270-013-0769-x
44. Jiang W, Zuo Q, Xue G, Zhang X, Tang H, Duan G, et al. Low profile visualized intraluminal support stent-assisted Hydrocoil embolization for acutely ruptured wide-necked intracranial aneurysms: a propensity score-matched cohort study. Clin Neurol Neurosurg. (2022) 218:107302. doi: 10.1016/j.clineuro.2022.107302
45. Zhu D, Yan Y, Zhao P, Duan G, Zhao R, Liu J, et al. Safety and efficacy of flow diverter treatment for blood blister-like aneurysm: a systematic review and meta-analysis. World Neurosurg. (2018) 118:e79–86. doi: 10.1016/j.wneu.2018.06.123
46. Ayling OG, Ibrahim GM, Drake B, Torner JC, Macdonald RL. Operative complications and differences in outcome after clipping and coiling of ruptured intracranial aneurysms. J Neurosurg. (2015) 123:621–8. doi: 10.3171/2014.11.JNS141607
47. Chitale R, Chalouhi N, Theofanis T, Starke RM, Amenta P, Jabbour P, et al. Treatment of ruptured intracranial aneurysms: comparison of stenting and balloon remodeling. Neurosurgery. (2013) 72:953–9. doi: 10.1227/NEU.0b013e31828ecf69
48. Cortez GM, Akture E, Monteiro A, Arthur AS, Peterson J, Dornbos D, et al. Woven EndoBridge device for ruptured aneurysms: perioperative results of a US multicenter experience. J Neurointerv Surg. (2021) 13:1012–6. doi: 10.1136/neurintsurg-2020-017105
Keywords: stent application, stent-assisted coiling, ruptured intracranial aneurysms, bibliometric, cluster analysis, Citespace
Citation: Chen R, Wei Y, Zhang G, Zhang R, Zhang X, Dai D, Li Q, Zhao R, Xu Y, Huang Q, Yang P, Zuo Q and Liu J (2022) Worldwide productivity and research trends of publications concerning stent application in acutely ruptured intracranial aneurysms: A bibliometric study. Front. Neurol. 13:1029613. doi: 10.3389/fneur.2022.1029613
Received: 27 August 2022; Accepted: 31 October 2022;
Published: 11 November 2022.
Edited by:
Cong-Hui Li, The First Hospital of Hebei Medical University, ChinaReviewed by:
Yong Cao, Beijing Tiantan Hospital, Capital Medical University, ChinaCopyright © 2022 Chen, Wei, Zhang, Zhang, Zhang, Dai, Li, Zhao, Xu, Huang, Yang, Zuo and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiao Zuo, ZHJfenVvQDEyNi5jb20=; Jianmin Liu, Y2hzdHJva2VAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.