- Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
Background: Acupuncture is a proven technique of traditional Chinese medicine (TCM) for ischemic stroke. The purpose of this overview was to summarize and evaluate the evidence from current systematic reviews (SRs) of acupuncture for early recovery after acute ischemic stroke (AIS).
Methods: We performed a comprehensive search for SRs of acupuncture for AIS in seven electronic databases up to May 23, 2022. Two reviewers independently selected SRs, extracted data, evaluated the methodological quality using the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2), and rated evidence certainty using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE).
Results: Seven SRs were included. The overall methodological quality of SRs was critically low. As for GRADE, 3 outcomes had moderate-quality evidence, 14 had low-quality evidence, and 12 had very low-quality evidence. Moderate-quality evidence demonstrated that initiating acupuncture therapies within 30 days of AIS onset significantly improves neurological function and the total effective rate of patients. Low-quality evidence showed that for patients within 2 weeks of AIS onset Xingnao Kaiqiao acupuncture (XNKQ Ac) could reduce disability rate and might reduce mortality. Regarding the safety of acupuncture therapies, low-quality evidence showed that there was no difference in the incidence of adverse reactions between the 2 groups, and very-low quality evidence showed that acupuncture did not promote hemorrhagic conversion.
Conclusions: In the acute and early recovery phases after AIS onset, acupuncture is a promising therapeutic strategy to improve the curative effect of current treatments, especially in the recovery of neurological function. Patients in the acute phase might receive XNKQ Ac, and patients in the early recovery phase might receive EA1, CA, or SA. However, considering the current certainty of evidence, a solid recommendation warrants further exploration.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42022335426.
Introduction
At present, acute ischemic stroke (AIS) remains a prominent cause of death and disability worldwide (1), despite breakthroughs in emergency therapy over the past years. Intravenous thrombolysis (IVT) and endovascular therapies (EVTs) have been the preferred treatments for patients with AIS (2). However, the majority of AIS patients did not receive IVT or EVTs due to late arrival to emergency departments. As for patients fortunately treated with recanalization therapies, they may suffer from ischemia/reperfusion (I/R) injury caused by highly harmful oxidative stress (OS) (3). In other words, even with currently evidence-based, effective therapies, there is a lack of an optimum therapeutic strategy to timely protect the brain from damage in the acute or early recovery stages.
As one of the various modalities of traditional Chinese medicine (TCM), acupuncture has gained international recognition, particularly in recent years (4). In the treatment of ischemic stroke, previous studies have indicated that acupuncture might prevent secondary brain injury by reducing oxidation (5). This potential mechanism of acupuncture removing superoxide has also been demonstrated in other nervous system diseases, such as vascular dementia and spinal cord injury (6–8). In animal models of ischemic stroke, acupuncture therapies may not only suppress the excessive production of reactive oxygen species (ROS), but also activate the inherent antioxidant enzymes (9). Fundamentally, acupuncture therapies may ameliorate mitochondrial dysfunction, which is manifested in raising the activities of mitochondrial respiratory enzymes (10). Regarding clinical benefits, there were numerous systematic reviews (SRs) evaluating the efficacy of acupuncture therapies for ischemic stroke from acute to convalescent and sequela stages (11–14). Since oxidative damage is the most severe within 24 h after onset (15), it is of great significance to investigate the efficacy and safety of acupuncture for ischemic stroke during the acute stage. A network meta-analysis also showed that the optimal time-point of acupuncture for stroke was within 48 h post-stroke, and the vital validity period lasted until 15 days after the attack (16). However, the paucity of systematic evaluation of evidence certainty is the reason why acupuncture therapies cannot be brought to the bedside of patients with AIS. The overview of SRs has been generally recognized to facilitate clinical decision-making. A study published in the British Medical Journal strongly calls for more effective evidence dissemination of acupuncture to solve the dilemma that evidence on acupuncture is underused in clinical practice (4). Therefore, we conducted this overview to summarize the existing evidence and critically evaluate the overall evidence quality of acupuncture therapies for early recovery after AIS.
Methods
This overview was carried out according to the Cochrane Handbook for SRs of Interventions (17) and registered under the number CRD42022335426.
Inclusion and exclusion criteria
We included SRs of randomized controlled trials (RCTs), in which participants were diagnosed with AIS and in the acute and early recovery phases (within 1 month after AIS onset). Acupuncture therapies were used alone or combined with conventional therapy (CT, including recanalization treatments, controlling vascular risk factors, improving blood circulation, and protecting brain cells). Comparator interventions were CT alone, or CT combined with placebo or sham acupuncture. Outcomes included but were not limited to functional independence (modified Rankin Scale score 0–2), mortality, disability rate, neurologic deficit score (NDS), activities of daily living (ADL), and adverse reactions.
We excluded studies if they were repeated publications; if their full text were unavailable; if they had incomplete or inaccurate data; if they used other TCM treatments in either intervention or control group.
Search strategy
We searched seven electronic databases listed below from their inception to 23 May 2022: MEDLINE Ovid (1946 to 23 May 2022), EMBASE Ovid (1996 to 2022 Week 20), the Cochrane Library, Chinese Biomedical Literature Service System (SinoMed), China National Knowledge Infrastructure (CNKI), Chinese Scientific Journals Database (VIP), and WanFang database. The search strategies for all databases are shown in Supplementary Table 1.
Study selection and data extraction
Two independent authors (LDW and ZMX) screened the records yielded in searches by reading titles and abstracts. Full texts of preliminary included SRs were further checked, and finally, eligible SRs were identified. And then they used a standard form extracting the following data: (1) first author, country, and publication year; (2) the number of trials and participants, eligibility criteria, interventions, comparisons, outcomes, and conclusions. Disagreements were resolved by consensus.
Quality assessment
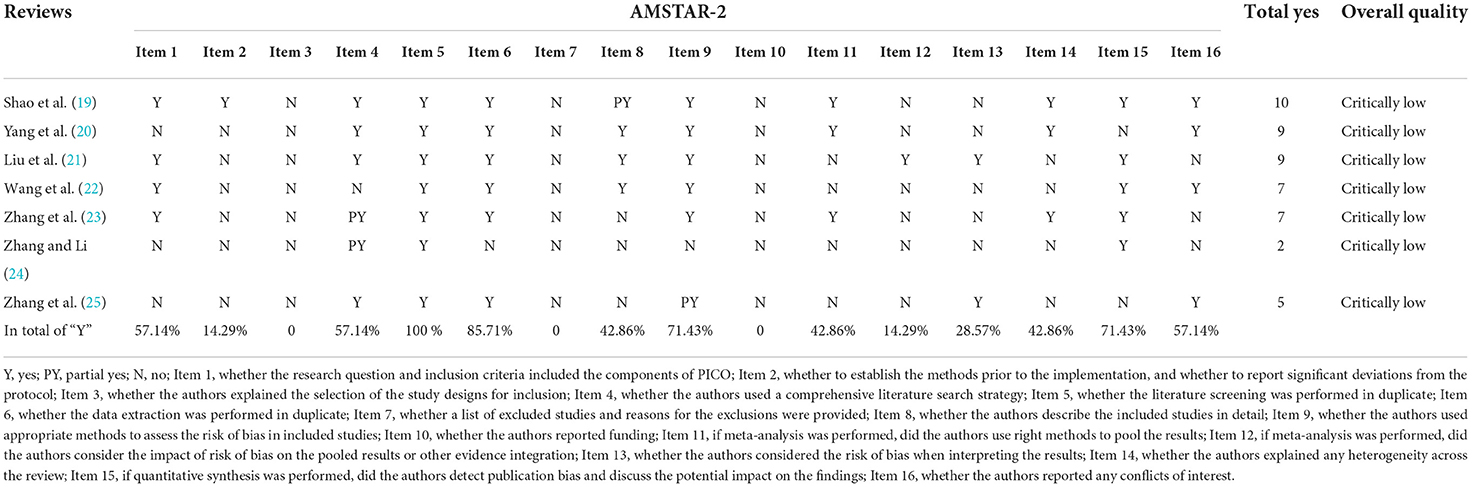
Methodological quality of included reviews
Two independent reviewers (XSC and GJF) used the Assessment of Multiple Systematic Reviews 2 (AMSTAR 2) to evaluate the methodological quality of SRs (18). Each of the 16 items was evaluated as “yes,” “partial yes,” or “no.” Items 2, 4, 7, 9, 11, and 13 were regarded as critical. The overall quality was rated as “high (no or 1 non-critical weakness),” “moderate (more than 1 non-critical weakness),” “low (1 critical flaw with or without non-critical weaknesses),” or “critically low (more than 1 critical flaw with or without non-critical weaknesses).” Disagreements were resolved by an expert in methodology (JL). We summarized these results and identified common methodological deficiencies.
Evidence certainty of included reviews
We used the Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) system to rate the certainty of evidence as “high,” “moderate,” “low” or “very low.” Certainty was downgraded for five factors (risk of bias, heterogeneity, detected publication bias, imprecision, and indirectness). If possible, we used the GRADEpro “Summary of findings” tables obtained from each included review. Two independent reviewers (WRQ and HXL) performed the evaluation. In cases of any disagreements, we consulted with an expert in methodology (JL).
Results
Literature search
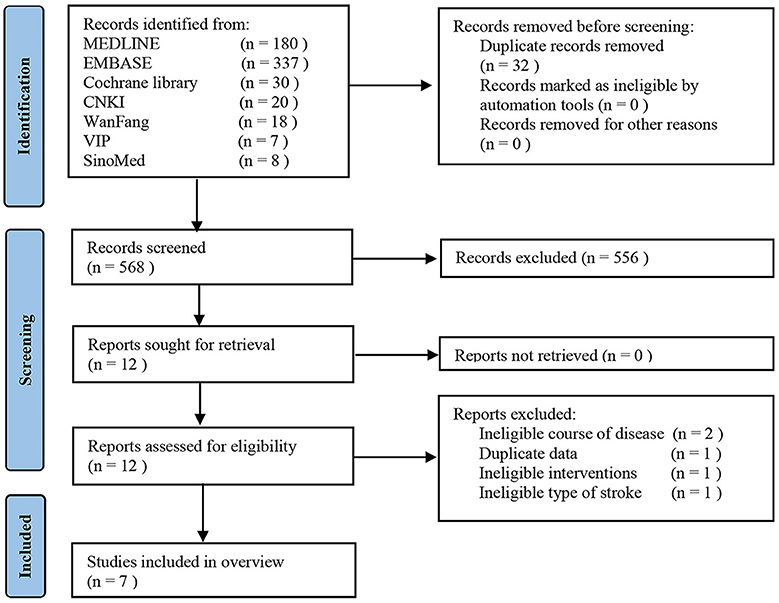
A total of 600 records were retrieved. After removing 32 duplicates, we screened the titles and the abstracts of 556 studies, and then assessed the full texts of 12 studies. A list of 5 studies, that appeared to meet the eligibility criteria but were excluded, is shown in Supplementary Table 2 along with reasons for exclusion. Ultimately, 7 SRs met the eligibility criteria (19–25). Figure 1 shows details of selecting studies.
Characteristics of included reviews
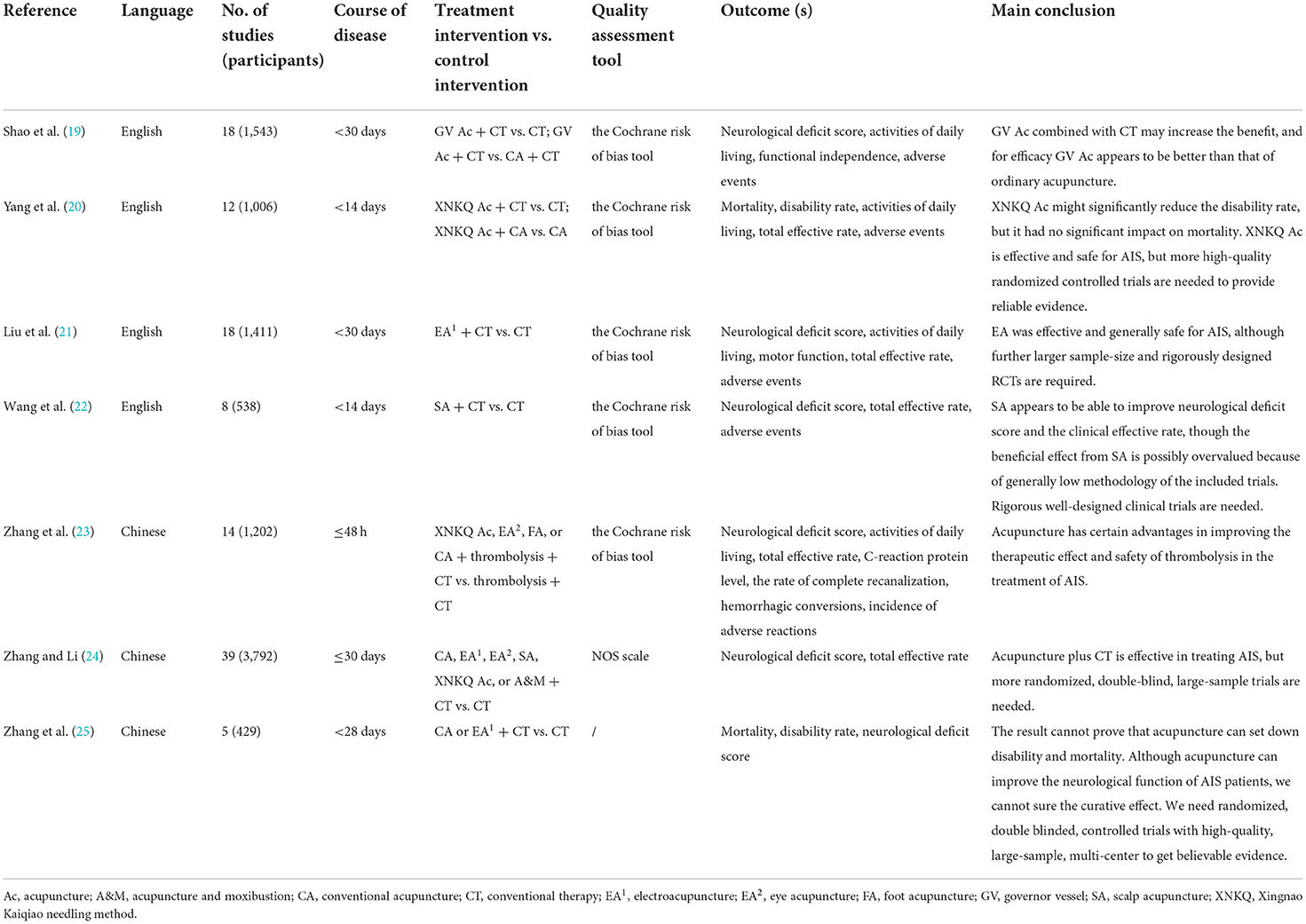
Table 1 presents a summary of included SRs. Original trials were published between 1996 and 2020. The date of the last retrieval in the SRs varied between October 2007 and December 2020. Four SRs were in the English language (19–22), and the other 3 were Chinese (23–25). The number of participants varied across SRs, ranging from 429 to 3,792. In total, 114 RCTs involving 9921 participants were included in 7 SRs. The time to initiate acupuncture therapies in patients was within 48 h of AIS onset in 1 SR (23), 14 days in 2 SRs (20, 22), and 1 month in 4 SRs (19, 21, 24, 25). Acupuncture therapies included conventional acupuncture (CA), electroacupuncture (EA1), eye acupuncture (EA2), foot acupuncture (FA), scalp acupuncture (SA), governor vessel acupuncture (GV Ac), and Xingnao Kaiqiao needling method acupuncture (XNKQ Ac). SRs reported outcomes: mortality, disability rate, modified Rankin Scale (mRS), NDS, ADL, motor impairment, total effective rate, complete recanalization, hemorrhagic conversion, C-reaction protein (CRP), adverse reactions, and adverse events. The measurements of NDS included the National Institute of Health Stroke Scale (NIHSS), the Chinese Stroke Scale/Modified Edinburgh-Scandinavia Stroke Scale (CSS/MESSS), and the Scandinavia Stroke Scale (SSS). ADL was assessed using the Barthel Index (BI). Motor impairment was measured with the Fugl–Meyer Assessment (FMA). Most SRs concluded that acupuncture is effective in treating AIS. Nevertheless, the paucity of high-quality RCTs downgraded the certainty of evidence.
Efficacy of acupuncture for AIS
Results of all efficacy outcomes are presented in tabular form (Supplementary Table 3).
NDS
Acupuncture + conventional therapy vs. conventional therapy
Four SRs adopted NIHSS measuring NDS and revealed that acupuncture therapies were associated with a significant reduction in NIHSS (19, 21, 23, 24). The heterogeneity of 2 SRs was insignificant (4 RCTs, MD = −1.18, 95% CI−1.52 to−0.83, P < 0.00001, I2 = 0%; 17 RCTs, MD = −1.86, 95% CI−2.06 to−1.66, P < 0.00001, I2 = 22%) (19, 24). The other SRs had significant heterogeneity (6 RCTs, SMD = −0.81, 95% CI−1.14 to−0.49, P < 0.00001, I2 = 51%; 12 RCTs, MD = −3.51, 95% CI−4.54 to−2.48, P < 0.00001, I2 = 90%).
Three SRs used CSS/MESSS to assess NDS and revealed that acupuncture therapies were associated with a significant reduction in CSS/MESSS (19, 21, 22). The heterogeneity of 1 SR was insignificant (3 RCTs, MD = −3.77, 95% CI−4.98 to−2.57, P < 0.00001, I2 = 0%) (19), and that of the other SRs was significant (5 RCTs, SMD = −1.27, 95% CI−2.18 to−0.37, P = 0.006, I2 = 94%; 7 RCTs, MD = −3.89, 95% CI −5.36 to −2.43, P < 0.00001, I2 = 57%).
One SR used SSS to assess NDS and reported that SSS in the acupuncture group was higher than that in the control group with statistical significance (25), but the heterogeneity was significant (3 RCTs, MD = 3.49, 95% CI 2.00 to 4.99, P < 0.00001, I2 =81.9%).
Governor vessel acupuncture vs. conventional acupuncture
One SR reported that NIHSS in the GV Ac group was lower than that in the CA group with statistical significance, but the heterogeneity was significant (2 RCTs, MD = −1.32, 95% CI−2.18 to−0.47, P = 0.002, I2 = 75%) (19).
One SR reported that CSS/MESSS in the GV Ac group was lower than that in the CA group with statistical significance (19), but the heterogeneity was significant (3 RCTs, MD = −4.63, 95% CI−5.91 to−3.35, P < 0.00001, I2 = 50%).
BI
Acupuncture + conventional therapy vs. conventional therapy
Three SRs showed that the acupuncture group was superior to the control group in improving BI with statistical significance. In these 3 SRs, 1 SR performed a subgroup analysis according to the course of treatment (2 RCTs, MD≤15d = 22.55, 95% CI 18.66 to 26.45, P < 0.00001, I2 = 0%; 3 RCTs, MD>15d = 8.80, 95% CI 5.87 to 11.72, P < 0.0001, I2 = 0%) (19). A subgroup analysis according to thrombolytic drugs was performed in another SR (23), which failed to explain the significant heterogeneity.
Governor vessel acupuncture vs. conventional acupuncture
One SR reported that BI in the GV Ac group was higher than that in the CA group with statistical significance (19), but the heterogeneity was significant (5 RCTs, MD = 8.27, 95% CI 4.29 to 12.26, P < 0.0001, I2 = 78%).
Xingnao kaiqiao needling method acupuncture + conventional acupuncture vs. conventional acupuncture
One SR reported that XNKQ Ac plus CA improved BI better than CA alone (1 RCT, MD = 17.17, 95% CI 9.15 to 25.19, P < 0.0001) (20).
mRS
Acupuncture + conventional therapy vs. conventional therapy
One SR reported that mRS at 1 month in the acupuncture group was lower than that in the control group (3 RCTs, MD = −0.63, 95% CI−0.95 to−0.32, P < 0.0001, I2 = 0%) (19). Although the difference had statistical significance, the effect size was far <1 point. As for the evaluation of mRS, 1 point is required per grade. In terms of clinical benefits, therefore, the clinical significance of the difference was insignificant.
FMA
Acupuncture + conventional therapy vs. conventional therapy
One SR reported that FMA in the acupuncture group was higher than that in the control group with statistical significance (8 RCTs, SMD = 0.98, 95% CI 0.75 to 1.22, P < 0.00001, I2 = 36%) (21).
Mortality and disability rate
Xingnao kaiqiao acupuncture + conventional acupuncture vs. conventional acupuncture
After 3 or 6 months of follow-up, 1 SR reported that XNKQ Ac plus CA might have additional effects in reducing disability rate with statistical significance and mortality without statistical significance (3 RCTs, RRdisability = 0.51, 95% CI 0.27 to 0.98, P = 0.04, I2 = 0%; 3 RCTs, RRmortality = 0.58, 95% CI 0.17 to 1.93, P = 0.37, I2 = 0%) (20). The confidence interval of disability rate was so wide that it was close to the invalid line, and the confidence interval of mortality even included the invalid line. Given the imprecision, the reliability of the results is questionable.
Acupuncture + conventional therapy vs. conventional therapy
One SR defined disabled as BI ≤ 60 (25), and reported that there was no statistical difference in the rate of death or disability at 6 months of follow-up between the acupuncture group and the control group. However, there was a trend toward reduced rate of death or disability with additional acupuncture therapies (3 RCTs, OR = 0.59, 95% CI 0.31 to 1.13, P = 0.11, I2 = 0%).
Total effective rate
Acupuncture + conventional therapy vs. conventional therapy
Four SRs reported that acupuncture might improve total effective rate with insignificant heterogeneity (6 RCTs, RR = 1.42, 95% CI 1.18 to 1.72, P = 0.0002, I2 = 16%; 4 RCT, RR = 1.23, 95% CI 1.11 to 1.37, P < 0.01, I2 = 0%; 13RCTs, RR = 1.19, 95% CI 1.13 to 1.25, P < 0.00001, I2 = 41%; 26 RCTs, OR = 3.95, 95% CI 3.02 to 5.16, P < 0.00001, I2 = 0%) (21–24). Another SR performed a subgroup analysis of different courses of disease (2 RCTs, RR≤24h = 1.40, 95% CI 1.06 to 1.86, P = 0.02, I2 = 2%; 2 RCT, RR6h − 72h = 1.63, 95% CI 1.03 to 2.59, P = 0.04, I2 = 45%) (20).
Xingnao kaiqiao acupuncture + conventional acupuncture vs. conventional acupuncture
One SR reported that the total effective rate in the XNKQ Ac plus CA group was higher than that in the CA group without statistical significance (1 RCT, RR = 1.80, 95% CI 1.00 to 3.23, P = 0.05) (20).
Rate of complete recanalization
Acupuncture + conventional therapy vs. conventional therapy
One SR found that the use of acupuncture after thrombolysis might improve the rate of complete recanalization without statistical significance (2 RCTs, RR = 1.20, 95% CI 1.00–1.44, P = 0.05, I2 = 0%) (23).
CRP
Acupuncture + conventional therapy vs. conventional therapy
One SR revealed that CRP in the acupuncture group was lower than that in the control group with statistical significance and insignificant heterogeneity (2 RCTs, MD = −3.99, 95% CI−4.35 to−3.63, P < 0.00001, I2 = 0%) (23).
Safety of acupuncture for AIS
Two SRs reported no adverse events (20, 22), and 3 SRs reported adverse events in detail (19, 21, 23). The adverse events in the acupuncture group mainly included subcutaneous hematoma, ecchymosis, and needle stagnation. One SR reported that the hemorrhagic conversion rate in the acupuncture group was lower than that in the control group without statistical significance (3 RCTs, RR = 0.72, 95% CI 0.14–3.62, P = 0.69, I2 = 51%) (23).
Quality assessment
Methodological quality of included reviews
We summarized the methodological quality of included SRs in Table 2 and Figure 2. Seven critical items were poorly reported. Just 1 SR provided a well-developed protocol (item 2) (19). Three SRs only searched electronic databases, but not clinical registries or gray literature (item 4) (22–24). None of the SRs presented a list of each excluded trial with specific reasons (item 7). Two SRs used an inappropriate technique to assess the risk of bias (RoB) (item 9) (24, 25). More than half of SRs lacked an exploration of substantial heterogeneity (item 11) (21, 22, 24, 25). And most SRs did not consider the impact of RoB when discussing their results (item 13) (19, 20, 22–24). One SR carried out a quantitative analysis, the Egger test, to detect the publication bias (19), 4 SRs performed a qualitative analysis (21–24), and 2 SRs did not mention it (item 15) (20, 25). As for 9 non-critical items, the poorly reported ones mainly were the reason for selecting RCTs (item 3), the sources of funding (item 10), and the assessment of the potential impact of RoB on meta-analysis (item 12).
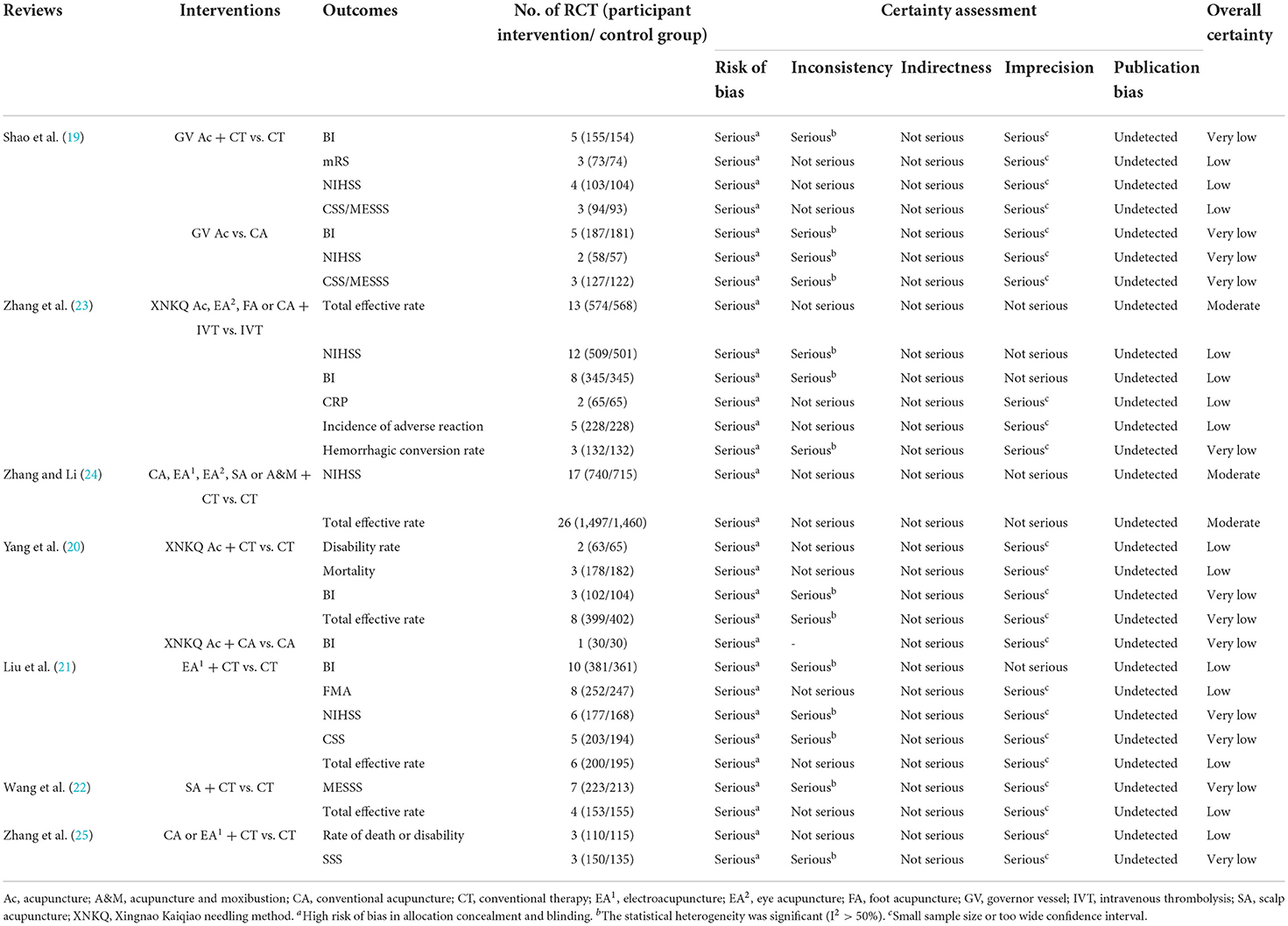
Evidence certainty of included reviews
One SR evaluated the certainty of evidence (21). Considering objectivity and impartiality, we used the GRADE approach to reevaluate important outcomes of all SRs. We summarized the overall certainty of evidence in Table 3. Ratings ranged from very low to moderate. Evidence of three outcomes was moderate-quality, 14 was low-quality, and 12 was very low-quality. The main reasons for downgrading the certainty across SRs were a high risk of bias (inadequate reporting of randomization, lack of blinding) (100 %), imprecision (79.31 %), and inconsistency (48.28 %).
Subgroup analysis
Providing practical guidance in clinical decision-making, we further performed subgroup analysis. As for the NIHSS in patients within 1 month after AIS, we collected original data from 2 SRs (21, 24), pooled these results, and performed subgroup analysis according to acupuncture methods. The results demonstrated that EA1, CA, and SA all significantly promoted early recovery of neurological function after AIS onset (Figure 3). The confidence intervals of the 3 subgroups were narrow and statistical heterogeneity was acceptable, indicating that the evidence was reliable. As for the NIHSS in patients within 48 hours after AIS onset, we collected original data from the SR (23) and performed subgroup analysis according to acupuncture methods. The results of all subgroups were statistically significant (Figure 4). But the larger sample size (750 participants) demonstrated that XNKQ Ac was the preferred acupuncture method for patients within 48 hours after AIS onset compared with other acupuncture methods, such as EA2, FA, and CA.
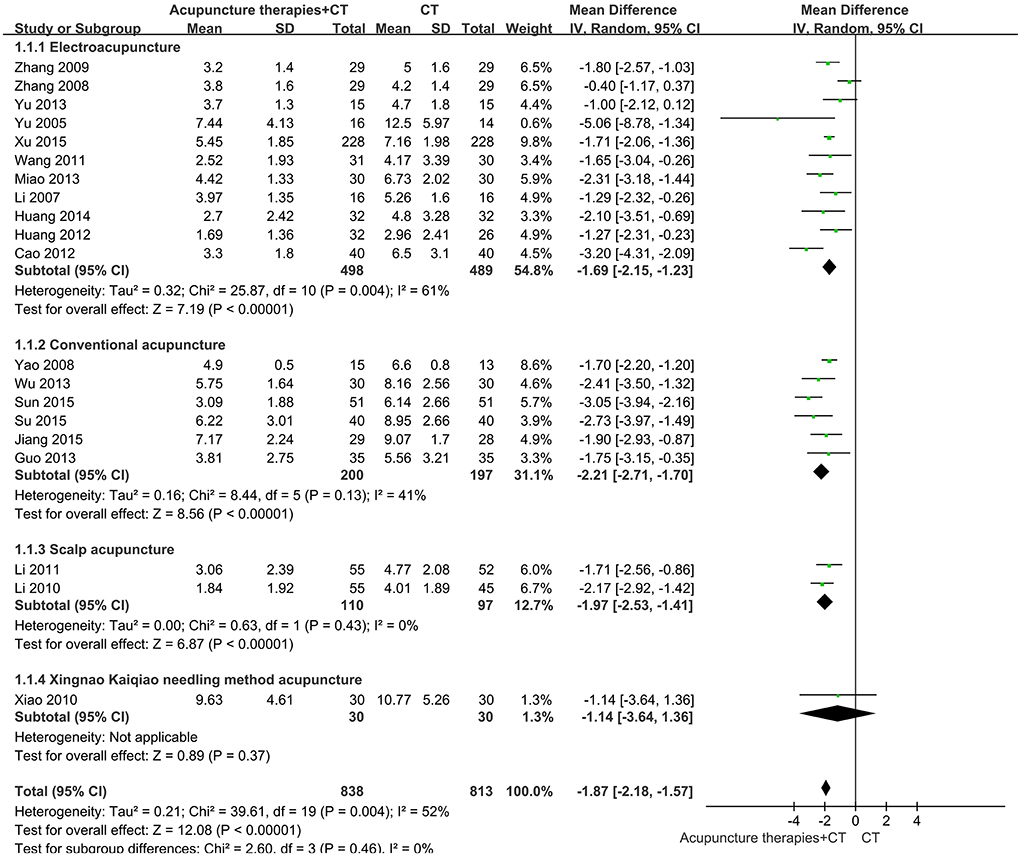
Figure 3. Subgroup analysis of the NIHSS in patients receiving acupuncture therapies within 1 month after AIS onset.
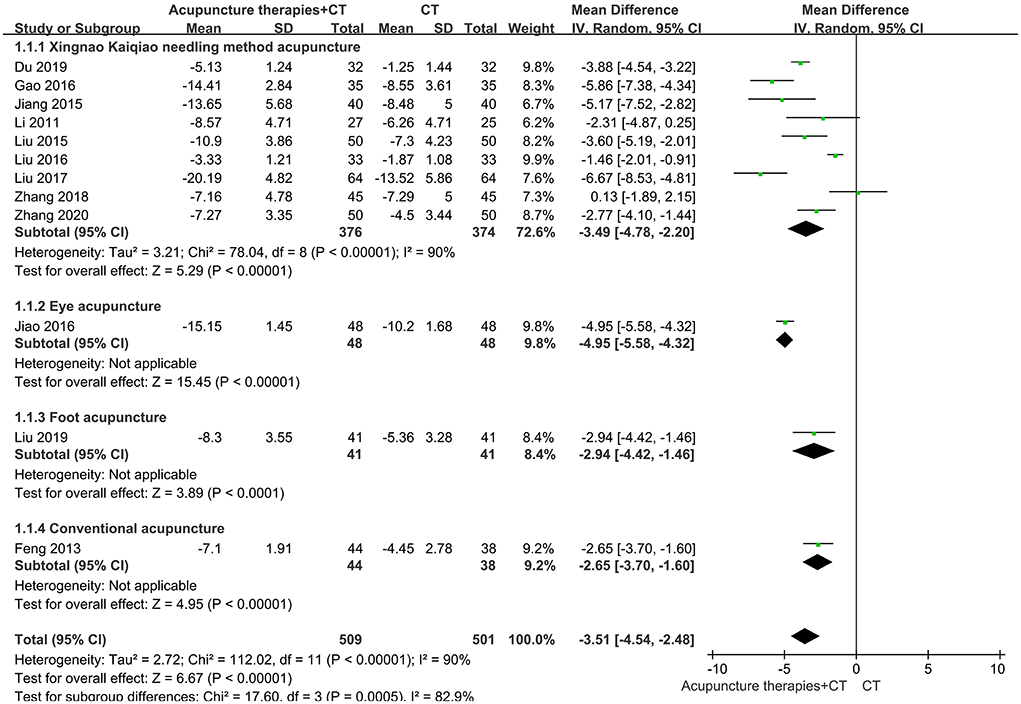
Figure 4. Subgroup analysis of the NIHSS in patients receiving acupuncture therapies within 48 h after AIS onset.
Discussion
The SR of RCTs is ranked as the most rigorous tool for clinical decision-making. Nevertheless, the uneven quality of original RCTs and the non-standard implementation of SR affected the certainty of evidence. A growing number of SRs of acupuncture for various diseases with positive results have been published. Therefore, an overview of SRs is of great significance (26). To our knowledge, this study is the first overview of SRs regarding acupuncture for AIS. In our overview, included SRs provided invaluable evidence on acupuncture therapies for AIS treatment, but many limitations do exist.
Summary of findings
We identified 7 SRs with 114 RCTs (9,921 participants). Overall methodological quality assessed by AMSTAR 2 was low, and most critical items were reported poorly, particularly in establishing an explicit statement before the conduct of the study, listing the excluded trials with precise explanation, performing sensitivity or subgroup analyses for substantial heterogeneity, and fully assessing the impact of RoB on results. Due to the high risk of bias, significant heterogeneity, and small samples, the level of evidence was correspondingly downgraded. The certainty of evidence was moderate to very low.
Moderate-quality evidence indicated that acupuncture therapies improve neurological function and the total effective rate of patients within 30 days of AIS onset. Several experiments studying rats with middle cerebral artery occlusion demonstrated that acupuncture therapies might ameliorate neurological function by regulating the opening of large-conductance Ca2+-activated potassium channels (27), and repressing ER stress-mediated autophagy and apoptosis (28).
Low-quality evidence suggested that initiating XNKQ Ac within 2 weeks of AIS onset might reduce the disability rate and mortality. Although there was no statistical difference in mortality, the trend of significantly reducing mortality deserves more research. XNKQ Ac was developed by Professor Shi Xuemin, academician of the Chinese Academy of Engineering, in 1972. Two decades ago, the effects of inhibiting free radicals and increasing superoxide dismutase (SOD) were verified in the rabbit model of acute I/R (29). There was an RCT conducted in Germany suggesting the modulation of functional connectivity in areas of motor function by XNKQ Ac (30). A recent clinical trial, comparing XNKQ Ac plus alteplase and alteplase alone, suggested that XNKQ Ac might promote the recovery of neurological function by improving lipid peroxidation (31). Lately, an RCT conducted by Shanghai Jiao Tong University found that the effects of XNKQ Ac may be associated with modulating brain rhythm oscillations of AIS patients (32).
Low-quality evidence demonstrated that the initiation of GV Ac within 3 days of AIS onset improves mRS at 1 month. The measurement of functional independence using mRS is generally considered the primary outcome (33). However, the effect size of mRS reduced by GV Ac was only 0.63, far < 1 point. The change just had statistical significance, instead of clinical significance. Additionally, we verified that this is the mRS observed at 1 month. Confirmation of long-term efficacy also depends on whether mRS changes significantly at 3 months.
Low-quality evidence and very low-quality evidence indicated that adjuvant acupuncture after thrombolysis might not increase the hemorrhagic conversion rate and incidence of other adverse reactions in patients within 48 h of AIS onset.
In addition to the aforementioned findings, we summarized the limitations of included SRs as follows: (1) All participants were diagnosed with AIS, but the definition of acute phase varied widely across SRs, including within 2 weeks of stroke onset, 4 weeks, 1 month, and 48 h. (2) Some SRs included 2 or more types of acupuncture, but there was no subgroup analysis based on different acupuncture therapies when performing meta-analyses. This clinical heterogeneity, to a certain extent, limited the generalizability of results.
Strengths and limitations
As the first overview of acupuncture for AIS, this study provided a series of clinical evidence, graded according to the GRADE, contributing to decision-making; revealed prevalent problems in current SRs and RCTs; and made constructive suggestions for future researchers. However, there was an inevitable limitation. The quality evaluation is subjective, although we guarantee strict adherence to internationally recognized standards.
Implications
To shorten the course of the disease, lengthen the duration of follow-up, increase sample sizes, and achieve blinding are the most critical implications for trialists. Firstly, the initiation time might be uniformly selected as the first 2 weeks after the onset of stroke. Generally, we define the acute phase as within 2 weeks (34). Moreover, the effect of acupuncture might be more significant during this period (16). Based on this premise, to further determine the optimum initiation time of acupuncture therapies, it is recommended to observe the difference in the efficacy of patients receiving acupuncture therapies within 6, 24, or 48 h of stroke onset. Secondly, given the potential advantages of acupuncture in improving disability rate and mortality after 3 or 6 months of follow-up (20), trialists should investigate endpoints, such as death, persistent disability, and recurrence of stroke, in more samples. Thirdly, trialists are suggested to blind outcome assessors, whereas sham acupuncture should be used with caution due to the underestimation of the acupuncture effect (35). As for placebo devices in acupuncture clinical trials, there was no definite evidence to support the blinding effects of these devices (36).
Reviewers of SRs should develop a protocol in advance to avoid performance bias; provide a complete list of excluded trials with exclusion reasons to avoid publication bias; fully address the heterogeneity and assess the impact of RoB on results to enhance credibility.
Conclusion
During the acute and early recovery phases after AIS onset, acupuncture therapies improve the curative effect of current treatments, especially in restoring neurological function. Based on the current evidence, it is suggested to select acupuncture methods according to the stages after AIS onset. Patients within 48 h or 2 weeks might receive XNKQ Ac, and patients within 1 month might receive EA1, CA, or SA. Considering the certainty of evidence, trialists should verify the benefits of acupuncture therapies in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
LW, XL, and YZ designed the study. JL provided help with methodology. XL and YZ made clinical suggestions and critically revised the manuscript. LW completed the introduction section. LW and ZX conducted study selection and data extraction. XC and GF performed AMSTAR 2 assessment. WQ and HL performed a GRADE assessment. SL and YL summarized the tables. LW and XC completed the manuscript writing. ZX helped with project supervision and language revisions. All authors contributed to the article and approved the submitted version.
Funding
The study was funded by the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine (No. ZYYCXTD-C-202007); the project from the China Center for Evidence-Based Traditional Chinese Medicine (No. 2020YJSZX-3); the projects from China Academy of Chinese Medical Sciences (Nos. CI2021B006 and CI2021A01301); 2019 the State Administration of traditional Chinese medicine TCM evidence-based capacity building project (ZZ13-024-3) and the National TCM Leading Personnel Support Program [NATCM Personnel and Education Department (2018) No. 12].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.1005819/full#supplementary-material
References
2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
3. Orellana-Urzúa S, Rojas I, Líbano L, Rodrigo R. Pathophysiology of ischemic stroke: role of oxidative stress. Curr Pharm Des. (2020) 26:4246–60. doi: 10.2174/1381612826666200708133912
4. Lu L, Zhang Y, Tang X, Ge S, Wen H, Zeng J, et al. Evidence on acupuncture therapies is underused in clinical practice and health policy. BMJ. (2022) 376:e67475. doi: 10.1136/bmj-2021-067475
5. Chen C, Hsieh C. Effect of acupuncture on oxidative stress induced by cerebral ischemia-reperfusion injury. Antioxidants. (2020) 9:248. doi: 10.3390/antiox9030248
6. Liu C, Zhou S, Guimarães S, Cho WC, Shi G. Acupuncture and oxidative stress. Evid Based Complementary Altern Med. (2015) 2015:1. doi: 10.1155/2015/424762
7. Zhu W, Wang X, Du S, Yan C, Yang N, Lin L, et al. Anti-oxidative and anti-apoptotic effects of acupuncture: role of thioredoxin-1 in the hippocampus of vascular dementia rats. Neuroscience. (2018) 379:281–91. doi: 10.1016/j.neuroscience.2018.03.029
8. Cheng M, Wu X, Wang F, Tan B, Hu J. Electro-acupuncture inhibits p66shc-mediated oxidative stress to facilitate functional recovery after spinal cord injury. J Mol Neurosci. (2020) 70:2031–40. doi: 10.1007/s12031-020-01609-5
9. Su X, Wang L, Ma S, Cao Y, Yang N, Lin L, et al. Mechanisms of acupuncture in the regulation of oxidative stress in treating ischemic stroke. Oxid Med Cell Longev. (2020) 2020:1–15. doi: 10.1155/2020/7875396
10. Zhang X, Wu B, Nie K, Jia Y, Yu J. Effects of acupuncture on declined cerebral blood flow, impaired mitochondrial respiratory function and oxidative stress in multi-infarct dementia rats. Neurochem Int. (2014) 65:23–9. doi: 10.1016/j.neuint.2013.12.004
11. Xu M, Li D, Zhang S. Acupuncture for acute stroke. Cochrane Database Syst Rev. (2018) 3:CD003317. doi: 10.1002/14651858.CD003317.pub3
12. Yang A, Wu HM, Tang JL, Xu L, Yang M, Liu GJ. Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev. (2016) 8:CD004131. doi: 10.1002/14651858.CD004131.pub3
13. Xin Z, Xue-Ting L, De-Ying K. GRADE in systematic reviews of acupuncture for stroke rehabilitation: recommendations based on high-quality evidence. Sci Rep. (2015) 5:1–11. doi: 10.1038/srep16582
14. Thomas LH, Coupe J, Cross LD, Tan AL, Watkins CL. Interventions for treating urinary incontinence after stroke in adults. Cochrane Database Syst Rev. (2019) 2:CD004462. doi: 10.1002/14651858.CD004462.pub4
15. Žitnanová I, Šiarnik P, Kollár B, Chomová M, Pazderová P, Andrezálová L et al. Oxidative stress markers and their dynamic changes in patients after acute ischemic stroke. Oxid Med Cell Longev. (2016) 2016:9761697. doi: 10.1155/2016/9761697
16. Zhuo Y, Xu M, Deng S, Zhang Y, Lu X, Wu B, et al. Efficacy and safety of dissimilar acupuncture intervention time-points in treating stroke: a systematic review and network meta-analysis. Ann Palliat Med. (2021) 10:10196–212. doi: 10.21037/apm-21-1127
17. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester (UK): John Wiley & Sons (2019). doi: 10.1002/9781119536604
18. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
19. Shao T, Zhou X, Ding M, Ye Z, Qian M, Jin Z. Governor vessel acupuncture for acute ischemic stroke: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10:7236–46. doi: 10.21037/apm-21-691
20. Yang ZX, Xie JH, Liu DD. Xingnao Kaiqiao needling method for acute ischemic stroke: a meta-analysis of safety and efficacy. Neural Regene Res. (2017) 12:1308–14. doi: 10.4103/1673-5374.213551
21. Liu A, Li J, Li H, Fu D, Zheng G, Lu L, et al. Electroacupuncture for acute ischemic stroke: a meta-analysis of randomized controlled trials. Am J Chin Med. (2015) 43:1541–66. doi: 10.1142/S0192415X15500883
22. Wang Y, Fu D, Chen C, Lu L, Lu L, Xie C, et al. Scalp acupuncture for acute ischemic stroke: a meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2012) 2012:480950. doi: 10.1155/2012/480950
23. Zhang Z, Zhang X, Ni G. Thrombolysis combined with acupuncture therapy for acute cerebral infarction: a meta-analysis of randomized controlled trials. Acupunct Res. (2021) 46:431–8. doi: 10.13702/j.1000-0607.200559
24. Zhang S, Li Z. The effectiveness of acupuncture and moxibustion in treating acute cerebral infarction: a meta-analysis. Chin J Phys Med Rehabil. (2018) 40:217–22.
25. Zhang T, Zhang L, Zhang H, Li Q. Systematic review of acupuncture therapy for acute ischemic stroke. Chin J Tradit Chin Med Pharm. (2009) 24:101–4.
26. Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. (2018) 7:1–9. doi: 10.1186/s13643-018-0695-8
27. Han L, Wang Y, Wang G, Chen Y, Lin H, Zhang Y, et al. Acupuncture ameliorates neurological function in rats with cerebral ischemia-reperfusion by regulating the opening of large-conductance Ca2+-activated potassium channels. Brain Behav. (2021) 11:e2286. doi: 10.1002/brb3.2286
28. Sun X, Liu H, Sun Z, Zhang B, Wang X, et al. Acupuncture protects against cerebral ischemia-reperfusion injury via suppressing endoplasmic reticulum stress-mediated autophagy and apoptosis. Mol Med. (2020) 26:105. doi: 10.1186/s10020-020-00236-5
29. Hu G, Tian F, Li P, Zhao L. Effect of Xingnao Kaiqiao acupuncture on pathological ultrastructure of brain free radicals in rabbits with cerebral ischemia and reperfusion. Chinese Critic Care Med. (1996) 8:5–7.
30. Nierhaus T, Chang Y, Liu B, Shi X, Yi M, Witt CM, et al. Somatosensory stimulation with XNKQ acupuncture modulates functional connectivity of motor areas. Front Neurosci. (2019) 13:147. doi: 10.3389/fnins.2019.00147
31. Zhang Q, Tian Z. Effects of xingnaokaiqiao acupuncture combined with alteplase on neurological deficit, lipid peroxidation and cerebrovascular reserve function in patients with acute cerebral infarction. Shanghai J Acupunct Moxibust. (2020) 39:25–30. doi: 10.13460/j.issn.1005-0957.2020.01.0025
32. Guo X, Zhang X, Sun M, Yu L, Qian C, Zhang J, et al. Modulation of brain rhythm oscillations by xingnao kaiqiao acupuncture correlates with stroke recovery: a randomized control trial. J Integr Complement Med. (2022) 28:436–4. doi: 10.1089/jicm.2021.0264
33. Broderick JP, Adeoye O, Elm J. Evolution of the modified rankin scale and its use in future stroke trials. Stroke. (2017) 48:2007–12. doi: 10.1161/STROKEAHA.117.017866
34. Chinese Society of Neurology, Chinese Stroke Society. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018. Chin J Neurol. (2018) 51:666–82. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004
35. Fei YT, Cao HJ, Xia RY, Chai QY, Liang CH, Feng YT, et al. Methodological challenges in design and conduct of randomised controlled trials in acupuncture. BMJ. (2022) 376:e64345. doi: 10.1136/bmj-2021-064345
Keywords: acupuncture, acute ischemic stroke, neurological function, GRADE, AMSTAR-2
Citation: Wang L, Chi X, Lyu J, Xu Z, Fu G, Liu Y, Liu S, Qiu W, Liu H, Liang X and Zhang Y (2022) An overview of the evidence to guide decision-making in acupuncture therapies for early recovery after acute ischemic stroke. Front. Neurol. 13:1005819. doi: 10.3389/fneur.2022.1005819
Received: 28 July 2022; Accepted: 20 September 2022;
Published: 13 October 2022.
Edited by:
Jingling Chang, Dongzhimen Hospital, Beijing University of Chinese Medicine, ChinaReviewed by:
Haijun Zhao, Shandong University of Traditional Chinese Medicine, ChinaJian Pei, Shanghai University of Traditional Chinese Medicine, China
Copyright © 2022 Wang, Chi, Lyu, Xu, Fu, Liu, Liu, Qiu, Liu, Liang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao Liang, bGlhbmd4aWFvMDIyQDEyNi5jb20=; Yunling Zhang, eXVubGluZ3poYW5nMjAwNEAxMjYuY29t
†These authors have contributed equally to this work
 Liuding Wang
Liuding Wang Xiansu Chi
Xiansu Chi Jian Lyu
Jian Lyu Zhenmin Xu
Zhenmin Xu Guojing Fu
Guojing Fu Yue Liu
Yue Liu Shaojiao Liu
Shaojiao Liu Wenran Qiu
Wenran Qiu Hongxi Liu
Hongxi Liu Xiao Liang
Xiao Liang Yunling Zhang
Yunling Zhang