- 1Department of Physical Medicine and Rehabilitation, Harvard Medical School, Boston, MA, United States
- 2Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Charlestown, MA, United States
- 3Spaulding Research Institute, Charlestown, MA, United States
- 4MassGeneral Hospital for Children Sports Concussion Program, Boston, MA, United States
- 5Home Base, A Red Sox Foundation and Massachusetts General Hospital Program, Charlestown, MA, United States
- 6Vanderbilt Sports Concussion Center, Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, TN, United States
Background: There is growing public concern regarding the potential long-term effects of playing football on brain health, specifically that playing football before and during high school might cause damage to the brain that manifests years or decades later as depression or suicidality. This study examined if playing high school football was associated with increased lifetime risk for depression, suicidality over the past year, or depressed mood in the past week in men aged between their middle 30 s to early 40 s.
Methods: Publicly available data from the National Longitudinal Study of Adolescent to Adult Health were analyzed. This longitudinal, prospective cohort study sampled nationally representative U.S. youth starting in 1994–1995 (Wave I) and most recently in 2016–2018 (Wave V). A total of 3,147 boys participated in Wave I (median age = 15), of whom 1,805 were re-assessed during Wave V (median age = 38).
Results: Of the 1,762 men included in the study, 307 (17.4%) men reported being diagnosed with depression and 275 (15.6%) reported being diagnosed with an anxiety disorder or panic disorder at some point in their life. When comparing men who played high school football to those who did not, there were no differences in the proportions of the sample who had a lifetime diagnosis of depression, lifetime diagnosis of anxiety/panic disorders, suicidal ideation in the past year, psychological counseling in the past year, or current depressed mood. However, men who received psychological counseling and/or experienced suicidal ideation during adolescence were significantly more likely to report a lifetime history of depression, suicidal ideation in the past year, and current depressed mood.
Conclusion: Individuals who reported playing football during adolescence did not have an increased risk of depression or suicidal ideation when they were in their middle 30 s to early 40 s, but mental health problems during adolescence were associated with an increased risk for psychological health difficulties more than 20 years later.
Introduction
American football has been popular for generations, and more than one million youth participate at the high school level annually (1). In recent years, there has been significant public concern regarding possible long-term effects on brain health associated with playing football. In one study, 54% of adults reported that they would not allow their child to play youth football (2). A central concern is that playing youth football, before and during high school, might cause damage to the brain that manifests clinically years or decades later as depression, suicidality, cognitive impairment, or neurological disease. It has been documented that playing youth football results in a large exposure to blows to the head, with the average player sustaining hundreds of head impacts per season (3, 4). Football players also are more likely to experience concussions than youth participating in other sports (5, 6). Researchers have reported that playing a single season of high school football is associated with changes in the brain measurable with structural and functional experimental neuroimaging (7, 8), as well as changes in cognition (9) and other clinical metrics, though results have been mixed Walter et al. (10). Concerns about long-term brain health have likely been fueled by extensive media coverage of research relating to chronic traumatic encephalopathy (CTE) in former National Football League (NFL) players (11, 12). Some researchers have asserted that depression and suicidality are clinical features of CTE (13–19), although multiple reviews of the literature have not identified suicide to be a clinical feature (20–25).
A personal history of multiple concussions has been associated with increased risk for later-in-life depression, or symptoms of depression, in former National Collegiate Athletic Association (NCAA) players (26) and retired NFL players (27–31). Survey studies reveal that some retired NFL players experience symptoms of depression (27), and these symptoms have been associated with chronic pain (32), pain catastrophizing (33), current opioid use (34), decline in physical functioning (27), and insufficient sleep (28). However, retired NFL players are at lower risk for suicide, not greater risk, than men from the general population (25, 35, 36).
Several studies have examined whether participating in high school football is associated with later in life psychological health problems. Three research teams used The National Longitudinal Study of Adolescent to Adult Health database to examine whether boys who played high school football are more likely to have mental health problems during early adulthood (i.e., late 20 s) (37–39). Those researchers reported that individuals who played high school football did not report greater lifetime rates of anxiety (38) or depression (37–39), suicidal ideation within the past year (37–39), or current symptoms of depression (i.e., within the past seven days) (38). An obvious limitation of those studies is that there were only a few years between high school graduation and follow-up—and having a longer interval would be important to better assess whether football confers risk for mental health problems in early or middle adulthood. A survey of more than 400 middle-aged men from the United States, ages 35–55, revealed that those who played high school football were not more likely to have a lifetime history of treatment for mental health problems, nor did they have higher rates of depression, anxiety, and anger in the preceding year, compared to men who did not play high school football (40), although these participants were recruited from an online platform and may not be representative of the general population. Two research teams examining data from older adult men participating in the Wisconsin Longitudinal Study reported no association between playing high school football and later in life psychological health or self-rated physical health at the average age of 65 (41, 42).
Between 2016 and 2018, another wave of interviews were completed as part of the National Longitudinal Study of Adolescent to Adult Health, when the participants were in their middle 30 s to early 40 s—and the data has been made publicly available. The purpose of this study was to determine whether playing high school football is associated with increased lifetime risk for depression, suicidality over the past year, or depressed mood in the past week in men who are in their middle 30 s to early 40 s. This is an important time period in life to study given that the possibility of experiencing depression or suicidality at some point during one's life increases over time, and the prior studies that found a relationship between football and depression examined former collegiate and professional players who were in their mid-to-late 30 s (26) and older (27, 28). Moreover, according to the recent consensus criteria for traumatic encephalopathy syndrome (43), former high school football players are considered to be at risk decades after exposure and depression and suicidality are reported to be “supportive” features that are often present in traumatic encephalopathy syndrome (although not part of the diagnostic criteria for the syndrome). We identified possible risk factors for suicidality during adolescence and examined them as predictors for suicidality more than two decades later. We hypothesized that having mental health difficulties during adolescence, especially suicidality, would be an important predictor of experiencing suicidality later in life, a hypothesis consistent with findings from when these participants were interviewed 10 years prior, during Wave IV (39). In contrast, as the primary focus of the study, we hypothesized that playing football during adolescence would not be significantly related to depression and suicidality in these men, consistent with findings from when they were interviewed ~10 years prior (37–39).
Materials and Methods
Participants
Public-use data collected via the National Longitudinal Study of Adolescent to Adult Health (i.e., “Add Health”) was used for this study (44). This longitudinal study started during the 1994–1995 school year when the participants were adolescents (i.e., grades 7–12; Wave I). The sample was collected using systematic sampling methods from 80 high schools and 50 middle schools to ensure that the demographics of participants were representative of U.S. schools regarding size, type, ethnicity, region, and urbanicity. During the first Wave, 20,745 youth completed the full Add Health study, and in the public use version of the database that was used in this specific study, Wave I data was available for 6,504 participants. Some of these individuals completed follow-up interviews in 2016–2018 when the participants were ~34–44 years old (Wave V, n = 4,196) (45). Separate databases from Waves I and V were merged using participant identification numbers so that data could be examined longitudinally. From this merged database, participants were included in this study if they identified as male in the Wave I database (variable “BIO_SEX; ”n = 3,147 total boys at Wave I) and completed the main outcome measures related to depression and suicidality at the Wave V assessment (variables H5ID6G and H5MN8; n = 1,805; 1,342 lost to follow-up).
Survey Questions
Football exposure was assessed during the Wave I assessment with the question “Are you participating/Do you plan to participate in the following clubs, organizations and teams (check all that apply): Football” (question S44A21). All questions relating to participation in specific sports were asked in this manner—and thus it is not possible to determine with certainty, whether all the boys who reported yes actually played football. Related to mental health at Waves I and V, we extracted data related to a lifetime history of depression (Wave V question H5ID6G: “Has a doctor, nurse or other health care provider ever told you that you have or had depression?”), lifetime history of anxiety (Wave V question H5ID6I: “Has a doctor, nurse, or other health care provider ever told you that you have or had anxiety or panic disorder?”), suicidal ideation (Wave I question H1SU1 and Wave V question H5MN8: “During the past 12 months, have you ever seriously thought about committing suicide?”), psychological treatment (Wave I question H1HS3 and Wave V question H5ID13: “In the past 12 months, have you received psychological or emotional counseling?”), and current depressed mood (question H5SS0B “During the past 7 days, I felt depressed;” response options: never or rarely, sometimes, a lot of the time, most of the time or all the time).
Statistical Analyses
SPSS version 28.0 was used for all analyses. The threshold for statistical significance was set at p < 0.05. Descriptive statistics were used to summarize characteristics from the sample. Chi-square tests of association were used to examine whether football participation during adolescence was associated with the proportion of the sample who endorsed a lifetime history of depression, suicidal ideation over the past year, and depressed mood over the past 7 days.
Results
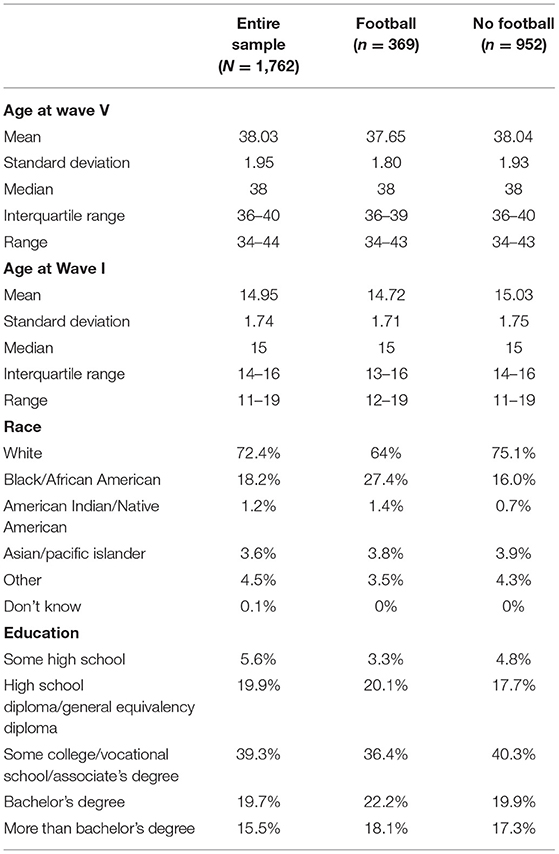
The publicly available database includes 3,147 boys who participated in Wave I of the study during their adolescence. Of these, 1,805 men participated in the Wave V follow-up ~21–24 years after the initial study (57.3%). A small number of participants were excluded because they did not provide answers to the main outcome questions (i.e., lifetime history of depression and/or suicidal thoughts in the past year, n = 43). The final sample included 1,762 men. Demographics for the final sample are included in Table 1. The sample was, on average, 38 years old at the Wave V assessment. Data collection for Wave V occurred in 2016 (26.3%), 2017 (50.3%), and 2018 (23.3%).
Football in High School and Mental Health During Adulthood
During the Wave V assessment, 307 (17.4%) men reported being diagnosed with depression at some point in their life, 275 (15.6%) being diagnosed with an anxiety disorder or panic disorder at some point in their life, 211 (12.0%) having received psychological or emotional counseling in the past 12 months, 125 (7.1%) reported seriously thinking about suicide in the past year, and 101 (5.8%) reported feeling depressed in the previous week (i.e., “a lot of the time” or “most of the time or all of the time” over the past 7 days). Examining responses the participants gave during the Wave I assessment when they were adolescents, 369 (20.9%) reported playing (or intending to play) football in high school and 952 (54.0%) reported not intending to play football in high school. Of note, 441 participants (25% of the sample) did not answer this question and were excluded from analyses pertaining to football participation. Participants who played football, compared to participants who did not, had similar rates of (i) being diagnosed with depression at some point in their life [13.6 vs. 17.5%; = 3.09, p = 0.08, OR = 0.74 95% CI = 0.52–1.04; see Figure 1], (ii) being diagnosed with an anxiety disorder or panic disorder at some point in their life [13.4 vs. 16.1%, = 1.53, p = 0.22, OR = 0.80, 95% CI = 0.59–1.14], (iii) having received psychological or emotional counseling in the past 12 months [10.4 vs. 11.6%, = 0.37, p = 0.54, OR = 0.89, 95% CI = 0.60–1.31], (iv) suicidal ideation in the past year [6.0 vs. 7.0%; = 0.49, p = 0.48, OR = 0.84, 95% CI = 0.51–1.38], and (v) feeling depressed in the past 7 days [4.1 vs. 6.2%; = 2.12, p = 0.15, OR = 0.65, 95% CI = 0.37–1.17].
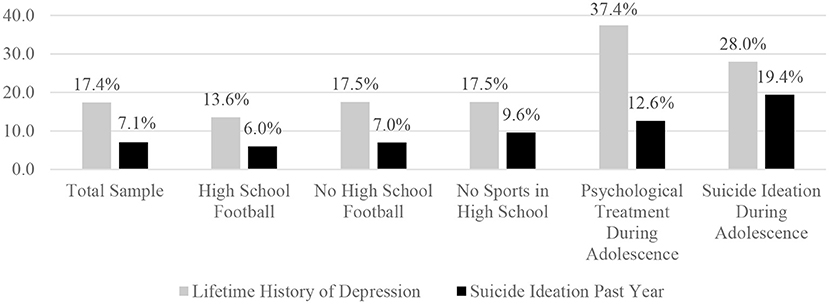
Figure 1. Percentages of men who reported experiencing suicide ideation in the past year during the Wave V interview. The percentages are based on the number of men who reported experiencing suicidal ideation during the past year. The total sample included 1,762 men who were interviewed at, on average, age 38 during the Wave V interview. The sample sizes for the subgroups are as follows: high school football n = 369; no high school football n = 952; no sports in high school n = 460; psychological treatment during adolescence n = 174; and suicide ideation during adolescence n = 186.
Mental Health in Adolescence and Depression and Suicide Ideation in Adulthood
During Wave I, there were 174 boys (9.9%) who reported undergoing psychological counseling in the past year while in high school. During the Wave V interview, ~24 years later, those individuals who underwent psychological counseling during adolescence were much more likely to report (i) a lifetime history of depression [37.4 vs. 15.3%, = 53.17, p < 0.001, OR = 3.31, 95% CI = 2.37–4.64], (ii) a lifetime history of anxiety disorder or panic disorder [27.0 vs. 14.4%, = 18.88, p < 0.001, OR = 2.20, 95% CI = 1.53–3.16], (iii) having received psychological or emotional counseling in the past 12 months [21.3 vs. 11.0%, = 14.48, p < 0.001, OR = 2.18, 95% CI = 1.47–3.24], (iv) suicidal ideation in the past year [12.6 vs. 6.4%, = 9.24, p = 0.002, OR = 2.11, 95% CI = 1.29–3.44], and (v) current depression [11.6 vs. 5.1%, = 11.77, p < 0.001, OR = 2.41, 95% CI = 1.43–4.04], compared to those who did not.
When interviewed during adolescence, 186 boys (10.6%) endorsed thoughts of suicide in the past year. At the follow-up assessment, ~24 years later, those men who reported suicide ideation during adolescence, compared to those who did not, were more likely to report (i) a lifetime history of depression [28.0 vs. 16.0%, = 16.54, p < 0.001, OR = 2.03, 95% CI = 1.44–2.88], (ii) having received psychological or emotional counseling in the past 12 months [21.5 vs. 10.8%, = 17.95, p < 0.001, OR = 2.26, 95% CI = 1.54–3.31], (iii) suicide ideation in the past year [19.4 vs. 5.6%, = 48.18, p < 0.001, OR = 4.06, 95% CI = 2.66–6.20], and (iv) feeling depressed within the past 7 days [13.0 vs. 4.8%, = 20.79, p < 0.001, OR = 2.97, 95% CI = 1.82–4.84]. Those who reported suicidal ideation during adolescence had a higher lifetime history of anxiety disorder or panic disorder, but this result was not statistically significant [20.4 vs. 15.0%, = 3.78, p = 0.052, OR = 1.46, 95% CI = 0.995–2.14].
Discussion
The present study found no association between playing high school football and lifetime history of anxiety or depression more than 20 years later. Moreover, men in their middle 30 s and early 40 s, who played high school football, did not report greater rates of receiving mental health treatment in the past year, experiencing suicidal ideation in the past year, or experiencing current symptoms of depression. In contrast, men who underwent mental health treatment during their youth or experienced suicidal ideation were significantly more likely to undergo mental health treatment and/or experience suicidal ideation more than 20 years later.
The National Longitudinal Study of Adolescent to Adult Health has been used by researchers to examine whether playing high school football is associated with mental health problems in early to middle adulthood. The longitudinal study began in 1994, and the most recent wave of data collection was completed 24 years later, in 2018. Including the present study, four studies have relied on Wave III (2001–2001; median age of 22, IQR = 20–23), Wave IV (2007–2009; median age of 29, IQR = 28–31), and Wave V (2016–2018, median age of 38, IQR = 36–40) data from this study. Researchers have reported that men who played high school football, when surveyed later, at the average age of 29, did not report a greater lifetime history of anxiety (38) or depression (37–39), a greater rate of receiving mental health treatment in the past year (39), or current symptoms of depression (i.e., within the past seven days) (39). Those were the same findings in the present study, for all of those variables, a decade later, when they were an average age of 38. These longitudinal data also reveal that young men who played high school football were not more likely to report suicidal ideation within the past year at an average age of 22 (39), 29 (37–39), or 38 (present study). In sum, none of these studies found an effect between high school football participation and higher rates of mental health problems or suicidality at the follow-up time point.
Three additional studies have reported that men who played high school football did not report greater mental health problems during middle age (40) or older adulthood (41, 42). A recent post-mortem study, from a brain donation program, reported that there was no statistically significant difference in the proportions of suicide as a manner of death among those men with a personal history of playing football compared to men who did not play football or who did not play sports (46). Moreover, those who played football were significantly less likely to have a lifetime history of a suicide attempt (46). In aggregate, the above-mentioned studies suggest that men who played high school football are not at greater risk for suicidality in early adulthood, during middle age, or as older adults.
Implications for Traumatic Encephalopathy Syndrome
Traumatic Encephalopathy Syndrome (TES) (43, 47) is conceptualized as the clinical syndrome that might be associated with chronic traumatic encephalopathy (CTE) neuropathologic change (48). The National Institute of Neurological Disorders and Stroke (NINDS) Consensus Diagnostic Criteria for TES were published in 2021 (43). According to these criteria, everyone who played organized football for five or more years, with at least 2 years at the high school level, is at risk for TES. Depression, anxiety, and suicidality are not considered core diagnostic features of TES, but they are considered to be supportive features that are believed to frequently occur. The cumulative literature published to date (described above), including the present study, does not support a belief that a large percentage of former high school football players will develop TES with associated serious mental health problems including depression and suicidality.
Limitations
There are several important limitations related to this study. First, all data were self-reported and could be affected by reporting biases. Second, as noted in the Methods section, the football exposure variable assessed if the students were currently participating in football or planned to participate in football; this was the format of the question used for all sports because the survey would have been conducted at different points in time during the school year. There may be some students who planned to play football but ultimately did not, as well as students who did not plan to play football but nonetheless joined the team. Third, several pieces of information about the participants' football/contact sport exposure were not collected (e.g., age of first exposure, length of career, position, and number of concussions), limiting the ability to examine these data in a more continuous manner based on one's cumulative football or repetitive neurotrauma exposure. Lastly, this study examined men who played, or planned to play, high school football and may not be applicable to those who played other contact or collision sports—and the results of this study are not applicable to women.
Sports and Exercise: Protective Factors
It is possible that playing high school football confers “risk” for future mental health problems through exposure to concussions, repetitive mild neurotrauma, and/or orthopedic injuries leading to later in life chronic pain—while at the same time being “protective,” through various resistance and resilience factors. There are many general health benefits to participating in sports, such as lower rates of obesity (49), better cardiovascular fitness (50), and greater lean muscle mass (51). There are diverse psychosocial benefits (52) such as greater social connectedness (51, 53, 54), and greater self-confidence (54) and self-esteem (55, 56). Not exercising or participating in sports is associated with lower life satisfaction in high school students (57). There are mental health benefits, such as less anxiety and other psychological health problems (52), and lower rates of depression (58, 59) and suicide (60–62). Involvement in sports and exercise might also be associated with positive differences in brain neurobiology (63) and better cognitive functioning (63–65), at least in some studies.
If youth who participate in sports are more likely to exercise during adulthood (66, 67), then this would confer a number of protective health benefits across the lifespan. Greater physical activity and exercise (especially with dietary modifications) are associated with reduced risk for obesity, hypertension, diabetes, and metabolic syndrome in adults (68–70), better sleep (71–73), and better mental health (74, 75). Moreover, there is a strong rationale for using exercise and physical activity for health promotion, disease prevention, and treatment in older adults (76).
Conclusions
With an annual participation rate of more than 1 million per year (1), it is reasonable to assume that many millions of men, over the past few decades, in the United States participated in high school football. It is important to study these men to determine if they experience later-in-life mental health problems that might be associated with repetitive neurotrauma, chronic pain, or other health issues. There are several studies to date suggesting that men who played high school football are not at greater risk for depression or suicidality in early adulthood (37–39), during middle age (40), or as older adults (41, 42). The results of this study are consistent with prior studies that do not find an association between high school football exposure and later mental health problems, including depression, anxiety, and suicidality.
Without question, however, some men who played high school football will later experience depression, suicidality, or both—just like other men in the general population. Suicidality is a clinical feature of depression, and when people are depressed some risk factors for completing suicide include a family history of a psychiatric disorder, previous attempted suicide, more severe depression, hopelessness, comorbid anxiety, and misuse of alcohol or drugs (77). High risk patterns of thinking associated with suicidality include hopelessness (78, 79), perceived burdensomeness (80), and mental pain (81). Related to family history of depression there are several genetic and epigenetic factors that likely influence the clinical manifestation of depression and suicidality (82, 83). In older adults, suicidality is associated with a broad range of medical problems including malignant diseases, neurological disorders, arthritis, chronic obstructive pulmonary disease, and liver disease (84). Moreover, in older adults, moderate to severe pain is associated with increased risk for suicidal ideation and attempts, and pain is a much stronger predictor for suicide in men than in women (85). It is important to appreciate that there are evidence-based treatments for depression and suicidality that can greatly reduce suffering and improve quality of life in these men.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: Add Health, https://addhealth.cpc.unc.edu/data/#public-use.
Ethics Statement
Add Health participants provided written informed consent for participation in accordance with the University of North Carolina School of Public Health Institutional Review Board guidelines. The data used in this manuscript were de-identified and is publicly available. No additional approvals were necessary in accordance with the local legislation and institutional requirements.
Disclosure
GI serves as a scientific advisor for NanoDX®, Sway Operations, LLC, and Highmark, Inc. He has a clinical and consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including former athletes), and on the topic of suicide. He has received research funding from several test publishing companies, including ImPACT Applications, Inc., CNS Vital Signs, and Psychological Assessment Resources (PAR, Inc.). He has received research funding as a principal investigator from the National Football League, and subcontract grant funding as a collaborator from the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members. He also has research funding from the Wounded Warrior Project®. DT has served as a consultant for REACT Neuro, Inc. He has a consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including former athletes).
Author Contributions
GI conceptualized the study, conducted the literature review, helped conceptualized the statistical analyses, wrote portions of the manuscript, and agrees to be accountable for the content of the work. DT helped conceptualize the study, the statistical analyses, conducted the statistical analyses, wrote portions of the manuscript, and agrees to be accountable for the content of the work. Both authors contributed to the article and approved the submitted version.
Funding
GI acknowledges unrestricted philanthropic support from ImPACT Applications, Inc., the Mooney-Reed Charitable Foundation, the Boston Bolts, the National Rugby League, and the Spaulding Research Institute. These entities were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
GI has a clinical and consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including former athletes), and on the topic of suicide.
The authors declare that the research was conducted in the absence of any commercial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Add Health is directed by Robert A. Hummer and funded by the National Institute on Aging cooperative agreements U01 AG071448 (Hummer) and U01 AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Waves I-V data are from the Add Health Program Project, grant P01 HD31921 (Harris) from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill.
References
1. National Federation of State High School Associations. High School Athletics Participation Survey. (2019). Available online at: https://www.nfhs.org/sports-resource-content/high-school-participation-survey-archive/ (accessed October 18, 2021).
2. Taranto E, Fishman M, Garvey K, Perlman M, Benjamin HJ, Ross LF. Public attitudes and knowledge about youth sports participation and concussion risk in an Urban Area. J Natl Med Assoc. (2018) 110:635–43. doi: 10.1016/j.jnma.2018.10.001
3. Broglio SP, Eckner JT, Martini D, Sosnoff JJ, Kutcher JS, Randolph C. Cumulative head impact burden in high school football. J Neurotrauma. (2011) 28:2069–78. doi: 10.1089/neu.2011.1825
4. Broglio SP, Martini D, Kasper L, Eckner JT, Kutcher JS. Estimation of head impact exposure in high school football: implications for regulating contact practices. Am J Sports Med. (2013) 41:2877–84. doi: 10.1177/0363546513502458
5. Hammer E, Brooks MA, Hetzel S, Arakkal A, Comstock RD. Epidemiology of injuries sustained in boys' high school contact and collision sports, 2008-2009 through 2012-2013. Orthop J Sports Med. (2020) 8:2325967120903699. doi: 10.1177/2325967120903699
6. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. (2012) 40:747–55. doi: 10.1177/0363546511435626
7. Kelley ME, Urban JE, Jones DA, Davenport EM, Miller LE, Snively BM, et al. Analysis of longitudinal head impact exposure and white matter integrity in returning youth football players. J Neurosurg Pediatr. (2021) 2021:1–10. doi: 10.3171/2021.1.PEDS20586
8. Abbas K, Shenk TE, Poole VN, Robinson ME, Leverenz LJ, Nauman EA, et al. Effects of repetitive sub-concussive brain injury on the functional connectivity of default mode network in high school football athletes. Dev Neuropsychol. (2015) 40:51–6. doi: 10.1080/87565641.2014.990455
9. Vogelpohl RE, Lindsey RA, Stickley CD, Hetzler RK, Williams W, Kimura IF. A prospective evaluation on the effects of one high school football season on neurocognitive test scores in high school football athletes. Int J Athl Ther Train. (2017) 22:49–55. doi: 10.1123/ijatt.2016-0083
10. Walter AE, Wilkes JR, Arnett PA, Miller SJ, Sebastianelli W, Seidenberg P, et al. The accumulation of subconcussive impacts on cognitive, imaging, and biomarker outcomes in child and college-aged athletes: a systematic review. Brain Imaging Behav. (2021). doi: 10.1007/s11682-021-00489-6
11. Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a national football league player. Neurosurgery. (2005) 57:128–34; discussion 128–34. doi: 10.1227/01.NEU.0000163407.92769.ED
12. Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. J Am Med Assoc. (2017) 318:360–70. doi: 10.1001/jama.2017.8334
13. McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. (2013) 136:43–64. doi: 10.1093/brain/aws307
14. Stern RA, Daneshvar DH, Baugh CM, Seichepine DR, Montenigro PH, Riley DO, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. (2013) 81:1122–9. doi: 10.1212/WNL.0b013e3182a55f7f
15. Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. (2011) 30:179–88, xi. doi: 10.1016/j.csm.2010.09.007
16. Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PMR. (2011) 3:S460–7. doi: 10.1016/j.pmrj.2011.08.008
17. Baugh CM, Stamm JM, Riley DO, Gavett BE, Shenton ME, Lin A, et al. Chronic traumatic encephalopathy: neurodegeneration following repetitive concussive and subconcussive brain trauma. Brain Imag Behav. (2012) 6:244–54. doi: 10.1007/s11682-012-9164-5
18. Omalu BI, Bailes J, Hammers JL, Fitzsimmons RP. Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes: the role of the forensic pathologist. Am J Forensic Med Pathol. (2010) 31:130–2. doi: 10.1097/PAF.0b013e3181ca7f35
19. Omalu B. Chronic traumatic encephalopathy. Prog Neurol Surg. (2014) 28:38–49. doi: 10.1159/000358761
20. Victoroff J. Traumatic encephalopathy: review and provisional research diagnostic criteria. Neuro Rehabil. (2013) 32:211–24. doi: 10.3233/NRE-130839
21. Iverson GL. Chronic traumatic encephalopathy and risk of suicide in former athletes. Br J Sports Med. (2014) 48:162–5. doi: 10.1136/bjsports-2013-092935
22. Wortzel HS, Shura RD, Brenner LA. Chronic traumatic encephalopathy and suicide: a systematic review. Biomed Res Int. (2013) 2013:424280. doi: 10.1155/2013/424280
23. Maroon JC, Winkelman R, Bost J, Amos A, Mathyssek C, Miele V. Chronic traumatic encephalopathy in contact sports: a systematic review of all reported pathological cases. PLoS ONE. (2015) 10:e0117338. doi: 10.1371/journal.pone.0117338
24. Iverson GL. Suicide and chronic traumatic encephalopathy. J Neuropsychiatry Clin Neurosci. (2016) 28:9–16. doi: 10.1176/appi.neuropsych.15070172
25. Iverson GL. Retired national football league players are not at greater risk for suicide. Arch Clin Neuropsychol. (2020) 35:332–41. doi: 10.1093/arclin/acz023
26. Kerr ZY, Thomas LC, Simon JE, McCrea M, Guskiewicz KM. Association between history of multiple concussions and health outcomes among former college football players: 15-year follow-up from the NCAA concussion study (1999-2001). Am J Sports Med. (2018) 46:1733–41. doi: 10.1177/0363546518765121
27. Brett BL, Kerr ZY, Walton SR, Chandran A, Defreese JD, Mannix R, et al. Longitudinal trajectory of depression symptom severity and the influence of concussion history and physical function over a 19-year period among former national football league (NFL) players: an NFL-LONG study. J Neurol Neurosurg Psychiatry. (2021). doi: 10.1136/jnnp-2021-326602
28. Walton SR, Kerr ZY, Brett BL, Chandran A, DeFreese JD, Smith-Ryan AE, et al. Health-promoting behaviours and concussion history are associated with cognitive function, mood-related symptoms and emotional-behavioural dyscontrol in former NFL players: an NFL-LONG study. Br J Sports Med. (2021) 55:683–90. doi: 10.1136/bjsports-2020-103400
29. Vos BC, Nieuwenhuijsen K, Sluiter JK. Consequences of traumatic brain injury in professional american football players: a systematic review of the literature. Clin J Sport Med. (2018) 28:91–9. doi: 10.1097/JSM.0000000000000432
30. Kerr ZY, Marshall SW, Harding Jr HP, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. (2012) 40:2206–12. doi: 10.1177/0363546512456193
31. Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Harding HP Jr., et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. (2007) 39:903–9. doi: 10.1249/mss.0b013e3180383da5
32. Schwenk TL, Gorenflo DW, Dopp RR, Hipple E. Depression and pain in retired professional football players. Med Sci Sports Exerc. (2007) 39:599–605. doi: 10.1249/mss.0b013e31802fa679
33. Mannes ZL, Ferguson EG, Perlstein WM, Waxenberg LB, Cottler LB, Ennis N. Negative health consequences of pain catastrophizing among retired national football league athletes. Health Psychol. (2020) 39:452–62. doi: 10.1037/hea0000847
34. Mannes ZL, Dunne EM, Ferguson EG, Cottler LB, Ennis N. History of opioid use as a risk factor for current use and mental health consequences among retired national football league athletes: a 9-year follow-up investigation. Drug Alcohol Depend. (2020) 215:108251. doi: 10.1016/j.drugalcdep.2020.108251
35. Baron SL, Hein MJ, Lehman E, Gersic CM. Body mass index, playing position, race, and the cardiovascular mortality of retired professional football players. Am J Cardiol. (2012) 109:889–96. doi: 10.1016/j.amjcard.2011.10.050
36. Lehman EJ, Hein MJ, Gersic CM. Suicide mortality among retired national football league players who played 5 or more seasons. Am J Sports Med. (2016) 44:2486–91. doi: 10.1177/0363546516645093
37. Bohr AD, Boardman JD, McQueen MB. Association of adolescent sport participation with cognition and depressive symptoms in early adulthood. Orthop J Sports Med. (2019) 7:2325967119868658. doi: 10.1177/2325967119868658
38. Deshpande SK, Hasegawa RB, Weiss J, Small DS. The association between adolescent football participation and early adulthood depression. PLoS ONE. (2020) 15:e0229978. doi: 10.1371/journal.pone.0229978
39. Iverson GL, Merz ZC, Terry DP. Playing high school football is not associated with an increased risk for suicidality in early adulthood. Clin J Sport Med. (2021) 31:469–74. doi: 10.1097/JSM.0000000000000890
40. Iverson GL, Merz ZC, Terry DP. High school football and midlife brain health problems. Clin J Sport Med. (2021). doi: 10.1097/JSM.0000000000000898
41. Deshpande SK, Hasegawa RB, Rabinowitz AR, Whyte J, Roan CL, Tabatabaei A, et al. Association of playing high school football with cognition and mental health later in life. JAMA Neurol. (2017) 74:909–18. doi: 10.1001/jamaneurol.2017.1317
42. Gaulton TG, Deshpande SK, Small DS, Neuman MD. Observational study of the associations of participation in high school football with self-rated health, obesity, and pain in adulthood. Am J Epidemiol. (2020) 189:592–601. doi: 10.1093/aje/kwz260
43. Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, Adler CH, et al. National institute of neurological disorders and stroke consensus diagnostic criteria for traumatic encephalopathy syndrome. Neurology. (2021) 96:848–63. doi: 10.1212/WNL.0000000000011850
44. Harris KM. The National Longitudinal Study of Adolescent to Adult Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007-2009 [Machine-Readable Data File and Documentation]. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill (2009).
45. Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P. The National Longitudinal Study of Adolescent to Adult Health: Research Design [WWW document]. (2009). Available online at: http://www.cpc.unc.edu/projects/addhealth/design (accessed November 3, 2021).
46. Iverson GL, Deep-Soboslay A, Hyde TM, Kleinman JE, Erskine B, Fisher-Hubbard A, et al. Suicide in older adult men is not related to a personal history of participation in football. Front Neurol. (2021) 12:1–10. doi: 10.3389/fneur.2021.745824
47. Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. (2014) 6:68. doi: 10.1186/s13195-014-0068-z
48. Bieniek KF, Cairns NJ, Crary JF, Dickson DW, Folkerth RD, Keene CD, et al. The second NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. J Neuropathol Exp Neurol. (2021) 80:210–219. doi: 10.1093/jnen/nlab001
49. Lee JE, Pope Z, Gao Z. The role of youth sports in promoting children's physical activity and preventing pediatric obesity: a systematic review. Behav Med. (2018) 44:62–76. doi: 10.1080/08964289.2016.1193462
50. Carlisle CC, Weaver RG, Stodden DF, Cattuzzo MT. Contribution of organized sport participation to health-related fitness in adolescents. Glob Pediatr Health. (2019) 6:2333794X19884191. doi: 10.1177/2333794X19884191
51. Agata K, Monyeki MA. Association between sport participation, body composition, physical fitness, and social correlates among adolescents: the PAHL study. Int J Environ Res Public Health. (2018) 2793:1–16. doi: 10.3390/ijerph15122793
52. Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. (2013) 10:98. doi: 10.1186/1479-5868-10-98
53. Linver MR, Roth JL, Brooks-Gunn J. Patterns of adolescents' participation in organized activities: are sports best when combined with other activities? Dev Psychol. (2009) 45:354–67. doi: 10.1037/a0014133
54. Zarrett N, Fay K, Li Y, Carrano J, Phelps E, Lerner RM. More than child's play: variable- and pattern-centered approaches for examining effects of sports participation on youth development. Dev Psychol. (2009) 45:368–82. doi: 10.1037/a0014577
55. Guddal MH, Stensland SO, Smastuen MC, Johnsen MB, Zwart JA, Storheim K. Physical activity and sport participation among adolescents: associations with mental health in different age groups. Results from the Young-HUNT study: a cross-sectional survey. BMJ Open. (2019) 9:e028555. doi: 10.1136/bmjopen-2018-028555
56. Erkut S, Tracy AJ. Predicting adolescent self-esteem from participation in school sports among latino subgroups. Hisp J Behav Sci. (2002) 24:409–429. doi: 10.1177/0739986302238212
57. Valois RF, Zullig KJ, Huebner ES, Drane JW. Physical activity behaviors and perceived life satisfaction among public high school adolescents. J Sch Health. (2004) 74:59–65. doi: 10.1111/j.1746-1561.2004.tb04201.x
58. Sanders CE, Field TM, Diego M, Kaplan M. Moderate involvement in sports is related to lower depression levels among adolescents. Adolescence. (2000) 35:793–7. Available online at: https://pubmed.ncbi.nlm.nih.gov/11214216/
59. Ferron C, Narring F, Cauderay M, Michaud PA. Sport activity in adolescence: associations with health perceptions and experimental behaviours. Health Educ Res. (1999) 14:225–33. doi: 10.1093/her/14.2.225
60. Taliaferro LA, Rienzo BA, Miller MD, Pigg RM Jr., Dodd VJ. High school youth and suicide risk: exploring protection afforded through physical activity and sport participation. J Sch Health. (2008) 78:545–53. doi: 10.1111/j.1746-1561.2008.00342.x
61. Harrison PA, Narayan G. Differences in behavior, psychological factors, and environmental factors associated with participation in school sports and other activities in adolescence. J Sch Health. (2003) 73:113–20. doi: 10.1111/j.1746-1561.2003.tb03585.x
62. Taliaferro LA, Eisenberg ME, Johnson KE, Nelson TF, Neumark-Sztainer D. Sport participation during adolescence and suicide ideation and attempts. Int J Adolesc Med Health. (2011) 23:3–10. doi: 10.1515/ijamh.2011.002
63. Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. (2016) e20161642:1–13. doi: 10.1542/peds.2016-1642
64. Herting MM, Chu X. Exercise, cognition, and the adolescent brain. Birth Defects Res. (2017) 109:1672–79. doi: 10.1002/bdr2.1178
65. Donnelly JE, Hillman CH, Castelli D, Etnier JL, Lee S, Tomporowski P, et al. Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Med Sci Sports Exerc. (2016) 48:1197–222. doi: 10.1249/MSS.0000000000000901
66. Jose KA, Blizzard L, Dwyer T, McKercher C, Venn AJ. Childhood and adolescent predictors of leisure time physical activity during the transition from adolescence to adulthood: a population based cohort study. Int J Behav Nutr Phys Act. (2011) 8:54. doi: 10.1186/1479-5868-8-54
67. Telama R, Yang X, Hirvensalo M, Raitakari O. Participation in organized youth sport as a predictor of adult physical activity: a 21-year longitudinal study. Pediatr Exerc Sci. (2006) 18:76–88. doi: 10.1123/pes.18.1.76
68. Lakka TA, Laaksonen DE. Physical activity in prevention and treatment of the metabolic syndrome. Appl Physiol Nutr Metab. (2007) 32:76–88. doi: 10.1139/h06-113
69. Carroll S, Dudfield M. What is the relationship between exercise and metabolic abnormalities? A review of the metabolic syndrome. Sports Med. (2004) 34:371–418. doi: 10.2165/00007256-200434060-00004
70. Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O'Keefe JH, et al. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J. (2013) 77:281–92. doi: 10.1253/circj.CJ-13-0007
71. Brupbacher G, Gerger H, Zander-Schellenberg T, Straus D, Porschke H, Gerber M, et al. The effects of exercise on sleep in unipolar depression: a systematic review and network meta-analysis. Sleep Med Rev. (2021) 59:101452. doi: 10.1016/j.smrv.2021.101452
72. Xie Y, Liu S, Chen XJ, Yu HH, Yang Y, Wang W. Effects of exercise on sleep quality and insomnia in adults: a systematic review and meta-analysis of randomized controlled trials. Front Psychiatry. (2021) 12:664499. doi: 10.3389/fpsyt.2021.664499
73. Li S, Li Z, Wu Q, Liu C, Zhou Y, Chen L, et al. Effect of exercise intervention on primary insomnia: a meta-analysis. J Sports Med Phys Fitness. (2021) 61:857–66. doi: 10.23736/S0022-4707.21.11443-4
74. Kandola A, Stubbs B. Exercise and anxiety. Adv Exp Med Biol. (2020) 1228:345–52. doi: 10.1007/978-981-15-1792-1_23
75. Bueno-Antequera J, Munguia-Izquierdo D. Exercise and depressive disorder. Adv Exp Med Biol. (2020) 1228:271–87. doi: 10.1007/978-981-15-1792-1_18
76. Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. (2021) 25:824–53. doi: 10.1007/s12603-021-1665-8
77. Hawton K, Casanas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. (2013) 147:17–28. doi: 10.1016/j.jad.2013.01.004
78. Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. (1985) 142:559–63. doi: 10.1176/ajp.142.5.559
79. Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry. (1990) 147:190–5. doi: 10.1176/ajp.147.2.190
80. Van Orden KA, Merrill KA, Joiner TE. Interpersonal-psychological precursors to suicidal behavior: a theory of attempted and completed suicide. Curr Psychiatry Rev. (2005) 1:187–96. doi: 10.2174/1573400054065541
81. Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, Bech P. Mental pain and suicide: a systematic review of the literature. Front Psychiatry. (2016) 7:108. doi: 10.3389/fpsyt.2016.00108
82. Levinson DF. The genetics of depression: a review. Biol Psychiatry. (2006) 60:84–92. doi: 10.1016/j.biopsych.2005.08.024
83. Lockwood LE, Su S, Youssef NA. The role of epigenetics in depression and suicide: a platform for gene-environment interactions. Psychiatry Res. (2015) 228:235–42. doi: 10.1016/j.psychres.2015.05.071
84. Fassberg MM, Cheung G, Canetto SS, Erlangsen A, Lapierre S, Lindner R, et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment Health. (2016) 20:166–94. doi: 10.1080/13607863.2015.1083945
Keywords: suicide, concussion, head injury, traumatic brain injury, football, depression, mental health, anxiety
Citation: Iverson GL and Terry DP (2022) High School Football and Risk for Depression and Suicidality in Adulthood: Findings From a National Longitudinal Study. Front. Neurol. 12:812604. doi: 10.3389/fneur.2021.812604
Received: 10 November 2021; Accepted: 29 December 2021;
Published: 09 February 2022.
Edited by:
Vassilis E. Koliatsos, Johns Hopkins University, United StatesReviewed by:
Douglas N. Martini, University of Massachusetts Amherst, United StatesDiego Iacono, Biomedical Research Institute of New Jersey, United States
Copyright © 2022 Iverson and Terry. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Grant L. Iverson, Z2l2ZXJzb25AbWdoLmhhcnZhcmQuZWR1
 Grant L. Iverson
Grant L. Iverson Douglas P. Terry
Douglas P. Terry