- 1Cognitive Aging and Impairment Neurosciences Lab, University of South Australia, Adelaide, SA, Australia
- 2Innovation IMPlementation and Clinical Translation (IIMPACT) in Health, University of South Australia, Adelaide, SA, Australia
- 3Allied Health and Human Performance, University of South Australia, Adelaide, SA, Australia
- 4Justice and Society, University of South Australia, Adelaide, SA, Australia
Objective: The objective of this scoping review was to capture the reported definitions for the subtypes of neglect post stroke and map the range of assessment tools employed for each neglect subtype.
Methods: EMBASE, Emcare, Medline, and psychINFO were searched from database inception. Searching included all allied terms and mesh headings for stroke, spatial neglect, measurement, screening tools, psychometric properties. Two reviewers independently screened studies for inclusion. Primary studies with documented protocols of a spatial neglect tool for adults post stroke, with some aspect of validity or reliability were included. Two reviewers independently reviewed the documented protocols of each tool to determine the underlying subtypes and disagreements were resolved through discussion.
Results: There were 371 articles included with 292 tools used for the screening or diagnosis of neglect. The majority of studies (67%) included a tool that did not specify the neglect subtype being assessed, therefore an analysis of the underlying subtypes for each tool is presented.
Conclusions: There is no consistency with the terms used to refer to the syndrome of spatial neglect with over 200 different terms used within the included studies to refer to the syndrome as a whole or one of its subtypes. It is essential to unify the terminology and definition for each neglect subtype. There are hundreds of neglect tools available, however many are not able to differentiate presenting subtypes. It is important for clinicians and researchers to critically evaluate the neglect tools being used for the screening and diagnosis of neglect.
Introduction
One in four adults in their lifetime will have a stroke (1). Stroke commonly results in spatial neglect, which can be defined as the neglect of any type of stimuli (such as visual, tactile, auditory or mental representations) from the side opposite the brain lesion or a lack of spontaneous movement of the contralesional side of the body (or any part of the body toward the contralesional side), despite the ability to do so (2, 3). Prevalence estimates of neglect range from 25 to 80% of stroke survivors (4–7), depending on the methods of assessment, stage of recovery and type of neglect (8, 9). Neglect is associated with poorer functional outcomes such as reduced independence in daily tasks, higher risk of falls, longer length of hospital stays, and reduced likelihood of home discharge (10, 11). It is essential to accurately identify the presence of neglect, to reduce the burden for individuals, their careers and the health system (12).
However, the identification of neglect can be challenging. Neglect manifestations are heterogeneous and no single test can accurately identify all types of neglect (13, 14). Additionally, neglect presents on a scale from very severe to mild (15), with mild neglect only becoming noticeable in certain situations (16) such as navigating a busy environment. Many current assessment tools can lack the sensitivity to detect mild or moderate neglect (14, 17–20) resulting in people with undiagnosed neglect.
Multiple taxonomies for how neglect is defined and categorized into subtypes have been proposed [for example, see (2, 21, 22)]. The taxonomy recently mentioned (21) to capture and classify the heterogenous behaviors of neglect into three dimensions will be used in this review. The three dimensions of neglect include: (1) reference frame (as either egocentric or allocentric); (2) processing stage which includes perceptual subtypes (visual, tactile or auditory), representational, and motor; and (3) spatial sector (as either personal, peripersonal, and extrapersonal) (21). Neglect can be multimodal and occur in any or all combinations of the three dimensions (12), which makes assessment so challenging.
It is important to identify the subtype(s) of neglect for several reasons. Firstly, clinicians will be able to predict which daily tasks are impacted by the neglect behavior if the subtype is known. For example, visual neglect present in the far extrapersonal space will impact the ability to cross a road safely, however tasks such as reading, shaving or putting on make-up will not be impacted. The clinician will therefore be able to educate the person to increase their awareness of the risks associated with specific tasks and target interventions to compensate for the symptoms of neglect and improve the person's independence. If neglect in a particular subtype is not detected, the person may remain unaware of the risks associated with returning to their daily routines, potentially putting themselves and others at risk when attempting particular activities such as cooking, driving or crossing a road (19, 23).
Secondly, recovery from neglect may depend on the subtype. More people recover completely after 6 months from personal and extrapersonal neglect in comparison to peripersonal neglect (24). Also, some interventions may be more effective for particular neglect subtypes in comparison to others. For example, visual scanning training in isolation has been shown to improve visual related tasks such as reading with minimal effect on non-visual neglect behavior (25). Prism adaptation has shown to improve motor neglect, with no effect on perceptual neglect (26), while monocular patching may have the opposite effect on the two subtypes (27). Also cold water caloric stimulation might be more effective for sensory neglect in comparison to motor neglect (28). Consequently, the results of intervention studies that do not assess neglect subtypes may be invalid, indicating a combination of improvement in one subtype and no change of another type (29).
Neglect subtypes are referred to inconsistently across the literature. There are five systematic reviews on the assessment of neglect according to our knowledge (8, 30–33), however, none of them have considered assessments for all neglect subtypes across the three dimensions proposed.
A gold standard tool to identify all types of neglect does not exist (8, 13). Therefore, there is a need to identify all the tools available for each neglect subtype; identify the most robust tools; and develop a consensus on the most appropriate battery of tools for the diagnosis of neglect. This scoping review is the first stage of this process. Scoping reviews are used to map the available evidence across multiple disciplines, clarify the conceptual boundaries of a topic, key concepts and working definitions (34–36). In accordance with these guidelines, the objectives of this scoping review are to capture the reported working definitions for the subtypes of neglect and map the range of tools employed for assessing each neglect subtype.
The questions and sub questions we will answer with this scoping review are:
1. What are the neglect subtypes and their definitions reported in the literature?
2. What are the reported tools for assessing each identified subtype of neglect?
• What subtypes do the tools measure? (as explicitly stated in the included studies and also analyzed by the researchers)
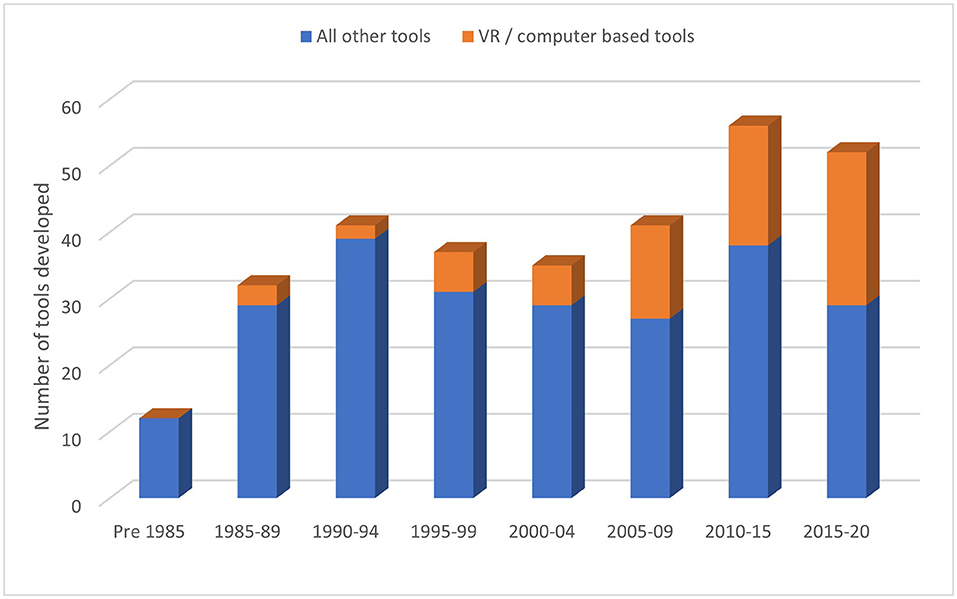
• How has tool development changed overtime?
Methods
This scoping review followed the guidelines for reporting outlined in the PRISMA extension for scoping reviews (PRISMA-Scr) (36). The study protocol is registered on the Open Science Framework (https://osf.io/bzv9q/). Any deviations from the protocol are described at the end of the paper.
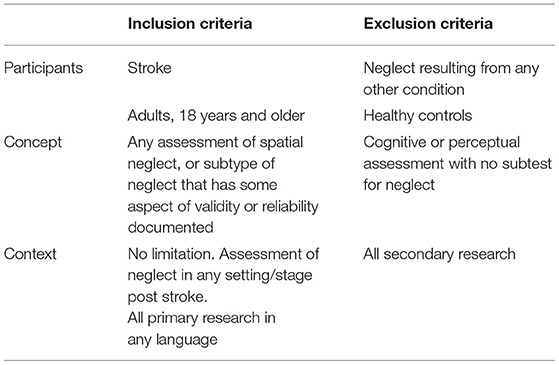
The study selection criteria are outlined in Table 1. Inclusion criteria under each heading of Participants, Concept and Context were used to determine eligibility for inclusion in accordance with the guidelines for conducting scoping reviews (34, 35).
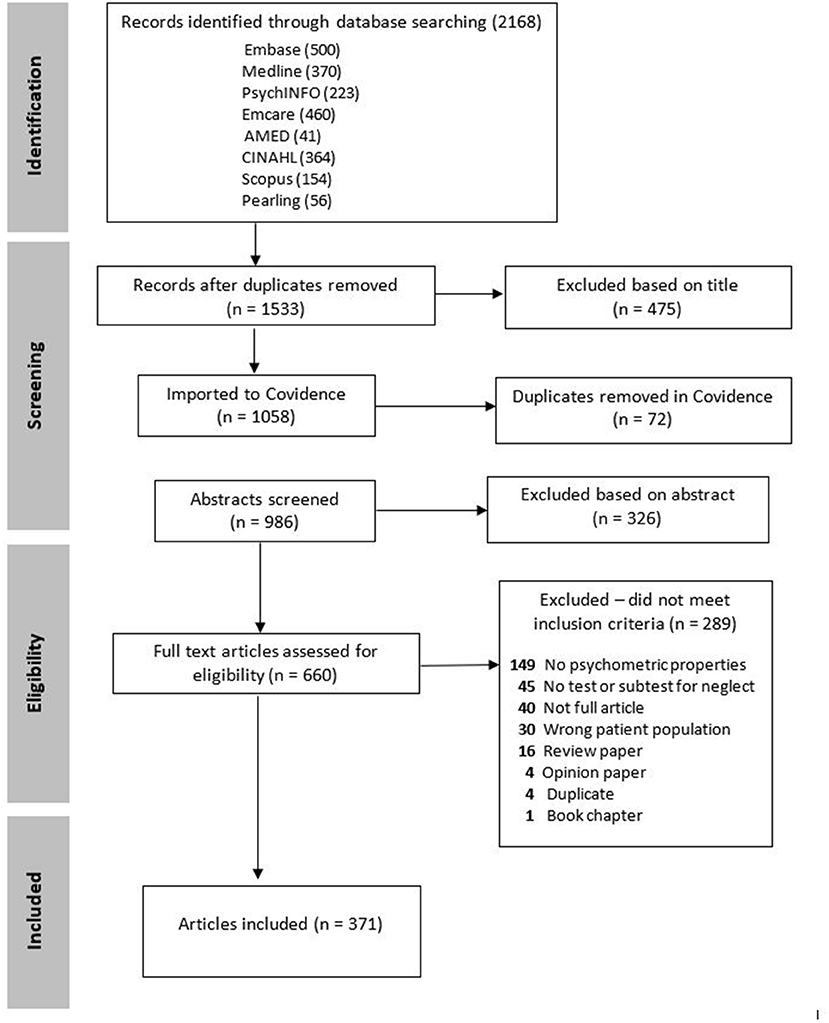
The following databases were searched on 17th July 2020 from database inception: EMBASE (EMBASE, RRID:SCR_001650), Emcare, Medline (MEDLINE, RRID:SCR_002185) and psychINFO. Additionally, AMED and CINAHL databases were searched in January 2018, however they were not accessible to the authors in 2020 when completing the updated search. The search strategy was developed in conjunction with a research librarian. Search terms included combinations of the following terms: Stroke, CVA, cerebrovascular accident; and unilateral spatial neglect, spatial neglect, visual neglect, visual inattention; and all allied terms of neglect, assessment, evaluation, measurement, screening tools, psychometric properties. Full details of the database search strategy are available in the Supplementary Table S1. The top 10 authors working in neglect based on number of publications were also searched according to their citation indexes using Scopus to confirm that all relevant publications were obtained. The reference lists of all secondary research identified by the search strategy and the final included studies were hand searched for any additional relevant studies. Refer to Figure 1 for the PRISMA flow diagram of included studies.
The references identified from each database were imported into Endnote X8.2 (EndNote, RRID:SCR_014001). The duplicates were removed in Endnote and the titles were screened by one author for the obviously irrelevant studies before the remaining studies were exported into Covidence (Covidence, RRID:SCR_016484) (37). Two authors independently screened the titles and abstracts for eligibility for inclusion. The full texts of potentially eligible studies were retrieved and assessed for eligibility independently by two authors. Any discrepancies over the eligibility of studies were resolved through discussion with a third author.
The following information was extracted from each study: neglect subtype(s) and definition(s); name of tool(s); abbreviated name; description of tool and protocols followed; purpose (what does each tool purport to measure)?; population; primary author; country of residence; and discipline according to the primary author's affiliation. If the discipline was not evident from the listed affiliation, then a google search was completed (primary author's name and affiliation) and the discipline was recorded as per their current work webpage if available. Extracting the data and documenting the results was an iterative process. The extraction form was trialed on ten studies with two independent researchers as recommended by The Joanna Briggs Institute (35). The extracted data from the ten studies was discussed with the research team and the form was refined to ensure that all the relevant information was extracted. (For example, the neglect subtypes were not explicitly stated for most tools. Therefore, all the documented protocols for each tool were collated in more detail so that the analysis of the underlying subtypes could be completed by the research team).
All the terms used within the studies to label neglect and each neglect subtype were collated and presented in figures to display the frequency of terms used for each discipline. The documented definitions for each neglect subtype were collated, grouped and summarized. All neglect tools with documented protocols used in the included studies were collated. The description of each neglect tool and the documented protocols were analyzed by two authors to determine the underlying subtypes of each tool. Disagreements were discussed with the authorship team until an agreement was determined.
Results
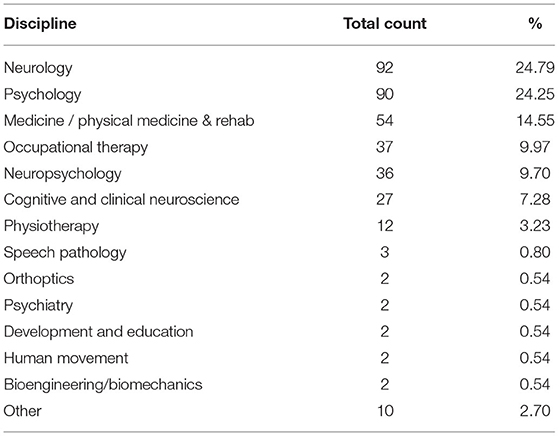
The systematic search produced 2,168 articles to be screened. After reviewing the titles and abstracts, the full texts of 660 articles were further reviewed for eligibility, resulting in 371 articles in the final sample for this review (see Figure 1 for details and full list of exclusion reasons). The included studies were published by a cross section of disciplines as listed in Table 2.
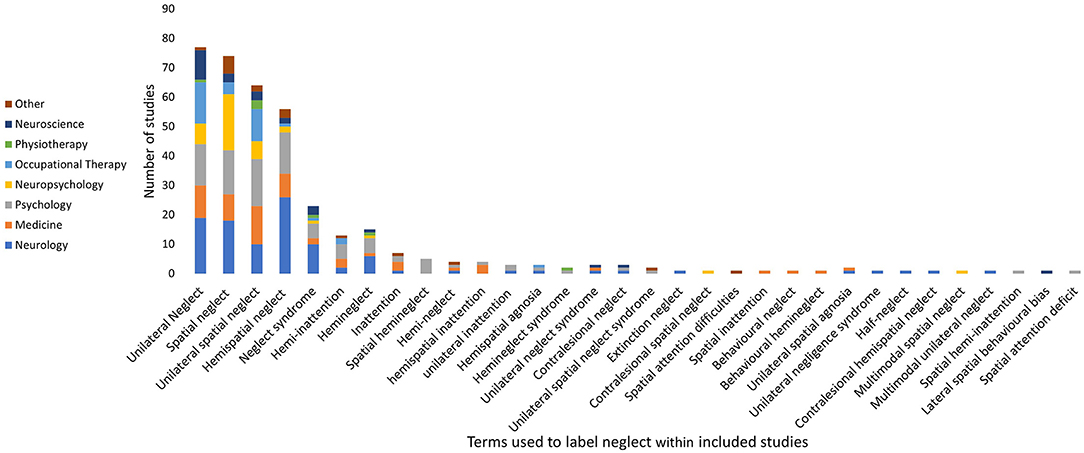
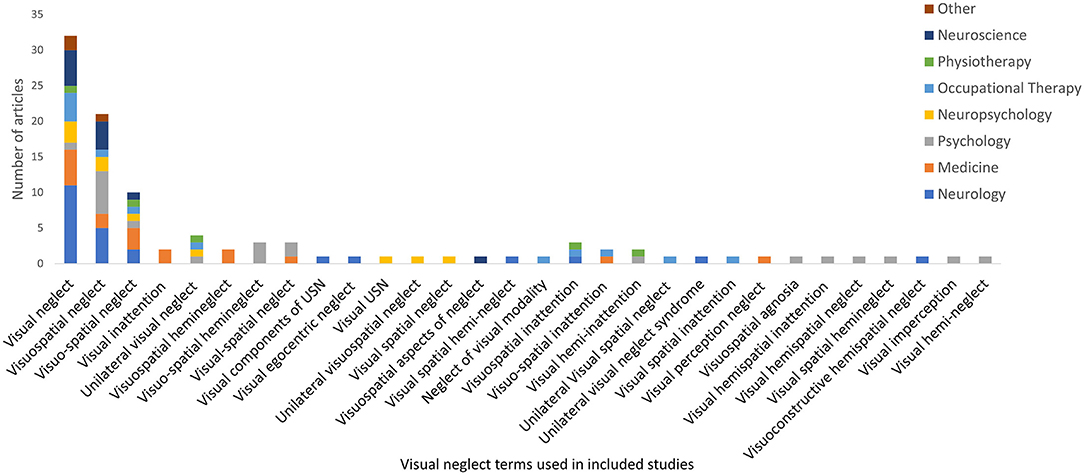
To determine the reported definitions in the included studies, first the terms used to label neglect and the subtypes were collated, and summarized. There was no agreement on the terms used to refer to this disorder with 33 different terms used in the included studies (see Figure 2). The term neglect (excluded from Figure 2) was the most frequently used (174 studies, 47.3%). However, only 23 studies (6.2%) used the term neglect in isolation, with the majority of studies using it within the article as a shortened version of another, more descriptive term. There was variability across the disciplines with neurology having a clear preference for the term hemispatial neglect, however this was not consistent with other disciplines, such as neuropsychology preferring the term spatial neglect, while psychology was evenly split across the top four terms. The definitions for each neglect subtype were grouped according to the three dimensions of neglect (21).
Dimension of Processing Stage
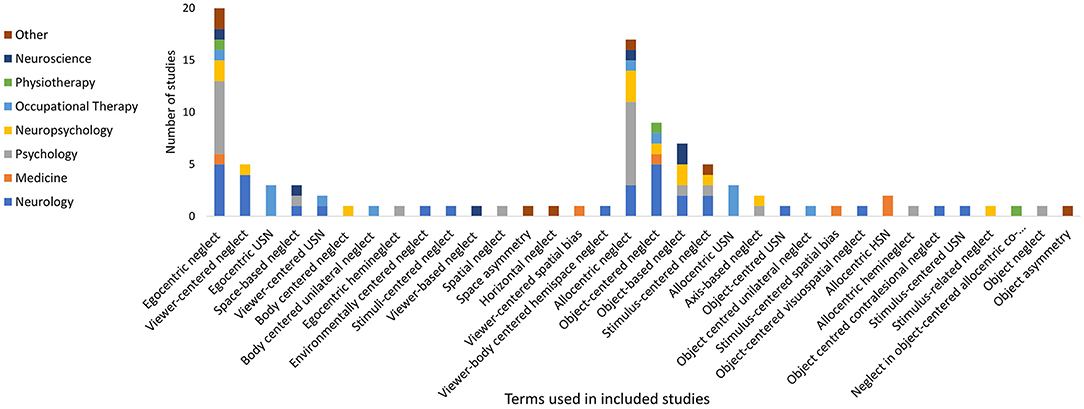
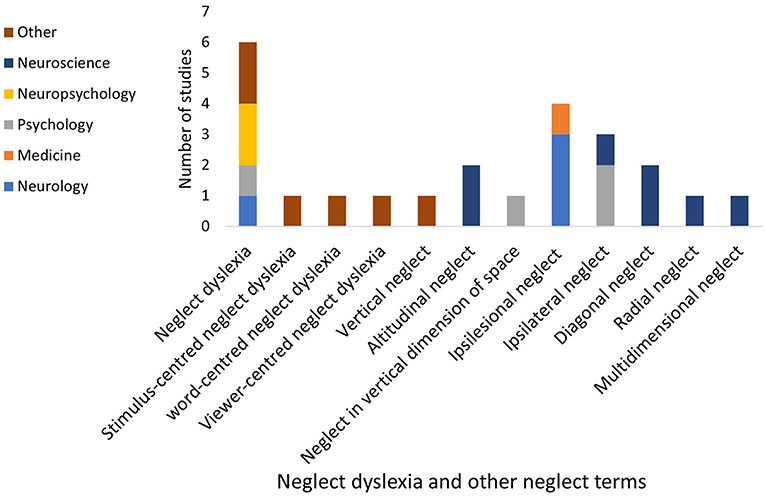
There were 105 different labels used for neglect subtypes under the dimension of processing stage, as displayed in Figures 3–5. These terms were grouped and labeled into the subtypes of perceptual (which includes the subtypes of visual, tactile and auditory), representational and, motor.
Perceptual neglect was reported in 38 studies with 17 different labels (Refer to Figure 4). The definitions varied considerably with some very broad definitions such as an impaired ability/failure to attend to or perceive stimuli in the contralesional hemispace (38, 39), while others specified the type of stimuli as including visual, auditory or tactile stimuli (40) or including both sensory/visuospatial and representational (mental imagery) aspects (41, 42).
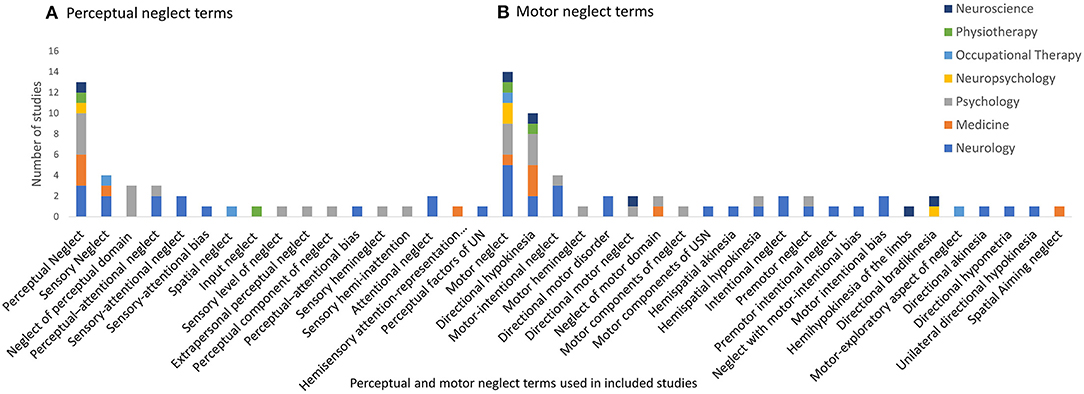
Figure 4. Perceptual and motor neglect terms used within included studies. (A) Perceptual and (B) Motor.
Visual neglect was the most frequently reported subtype (101 studies, 27.4%), with 30 different terms used to describe it. The term visual neglect (see Figure 3) was preferred by all disciplines, apart from psychology who preferred the term visuospatial neglect. Although visual neglect was the most frequently reported subtype, the definitions still varied with the majority of studies either not defining it, or reporting a broad definition of neglect without defining the visual neglect subtype [for example (43, 44)], while few studies explicitly defined it as neglecting “visual stimuli” [for example (45–47)].
Tactile neglect was referred to in 20 studies with 10 different labels. The label of tactile neglect was the most frequently used (30%) (Refer to Figure 5). The majority of studies did not specify the type of tactile stimuli included in this subtype, describing it simply as neglect in the tactile modality (42, 48–51). Only two studies specified the type of tactile stimuli as somatosensory stimuli, including touch, pain and sensation (47, 52). Two studies additionally described tactile neglect as only occurring within an egocentric reference frame (53, 54), with a gradient of tactile neglect behaviors that increases further toward the contralesional side and gradually decreases over egocentric space toward the ipsilesional side.
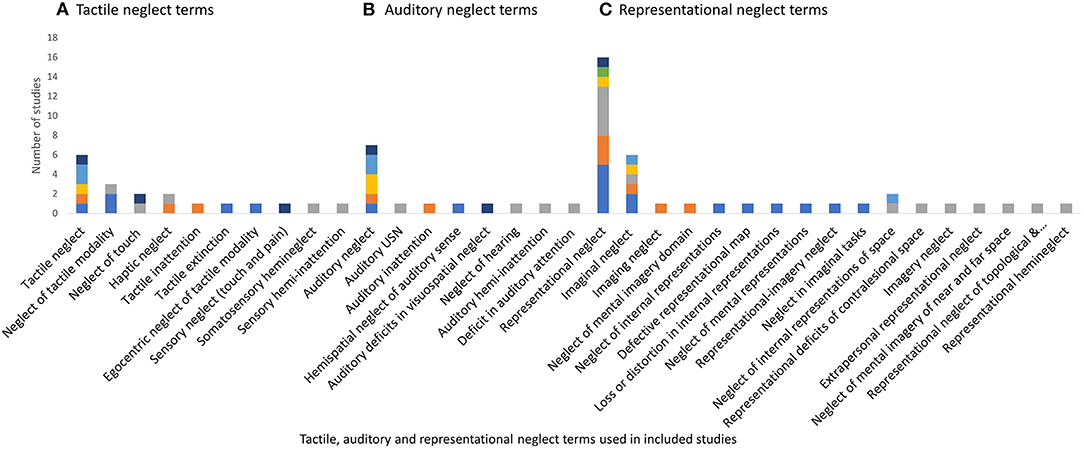
Figure 5. Tactile, auditory, and representational neglect terms used within included studies. (A) Tactile, (B) auditory, and (C) representational.
Auditory neglect had eight different labels (Refer to Figure 5). Auditory neglect was the most frequently used label (47%) with the majority of the studies describing it simply as “neglect of the auditory sense” (45, 49, 55, 56). The behaviors of auditory neglect were described by Pavani, Làdavas & Driver (p. 181) (57) as a failure “to detect or identify contralesional sounds under bilateral presentation”, and may include poor position discrimination of contralesional sounds and an ipsilesional bias when pointing to contralesional sounds. Zimmer, Lewald & Karnath (58) proposed from the results of their study that auditory neglect in the strictest sense, described as neglect of contralesional auditory stimuli, even with no concurrent stimuli on the ipsilesional side, does not appear to exist.
Representational neglect had 17 different labels across 38 studies. The label of representational neglect was the most frequent (n = 16, 42.1%), followed by imaginal neglect (n = 6, 15.8%), see Figure 5. Representational neglect was described as the neglect of internal representations/mental images (40, 59–63) loss or distortion of mental images (64, 65); or an inability to build or explore the contralesional side of internal representations (64, 66). An impairment of spatial memory has also been implied due to the inability to retrieve portions of remembered scenes (39, 67, 68). On the other hand, representational neglect has been further categorized into (1) neglect of near static objects/locations and (2) neglect of far (topological) images (69, 70). It has also been suggested that representational deficits impact the ability to attend to or explore external contralesional space (71, 72), thus impacting on the execution of all daily tasks.
Motor neglect was identified with 23 different labels across 54 studies. Motor neglect was the most frequently used label (25.9%), followed by directional hypokinesia, (18.5%), see Figure 4. The descriptions of this subtype (n = 19) fell into two distinct categories as labeled by Bisiach et al. (73); (1) impaired spontaneous movement of the contralesional limb and (2) a directional specific deficit with impaired movement toward the contralesional side. The majority of studies considered motor neglect to incorporate behaviors from both categories (28, 38–40, 68, 74, 75). Other studies solely described a direction specific deficit (41, 42, 76–81). Although Bisiach and colleagues (73) described the direction specific deficit was irrespective of the limb being used, other studies considered this for the ipsilesional limb only (40, 75, 82).
Dimension of Spatial Sector
Personal neglect had 12 different labels across 71 studies. The label of personal neglect was preferred by all disciplines (76%) (see Figure 6). Personal neglect was described as occurring on the body (n = 4); pertaining to the body surface (n = 5); occurring in personal space (n = 7); a lack of awareness (n = 5) or a lack of exploration (n = 3) of the contralesional side of the body. Alternatively, this subtype was also described by the impact on daily tasks (n = 4), such as neglecting to dress the left side of the body. The descriptions of this subtype were not consistent across all the studies, with six studies attributing this subtype of neglect to another underlying disorder such as representational neglect (having a disrupted representation of the contralesional side of the body) (83, 84), tactile (ignoring somatosensory stimuli) or motor neglect (underutilizing the contralesional side of the body) (84, 85), a disorder of the body schema (86, 87), or a disruption of the sense of ownership of the neglected side of the body (80, 86, 87).
Peripersonal neglect was referred to in 62 studies with 19 different labels. Peripersonal neglect (n = 15, 24.2%) and extrapersonal neglect (n = 13, 21%) were most frequently reported, with no clear preference for either term (see Figure 7). The majority of studies described this subtype as neglect within arm's length or reaching distance (n = 17). Other studies simply stated this subtype as neglect within; the peripersonal space (n = 3), near space (n = 2), near-extrapersonal space (n = 2) or space surrounding the body (n = 6). This subtype was categorized more broadly by combining the neglect of near and far extrapersonal space into the one subtype of extra-personal neglect, or neglect of the environment (88). Conversely two studies further distinguished near extrapersonal space into further sub-subtypes of near radial (bottom half of an A4 page), far radial (top half of an A4 page), or diagonal neglect (neglect of the near left part of the page) (89, 90).
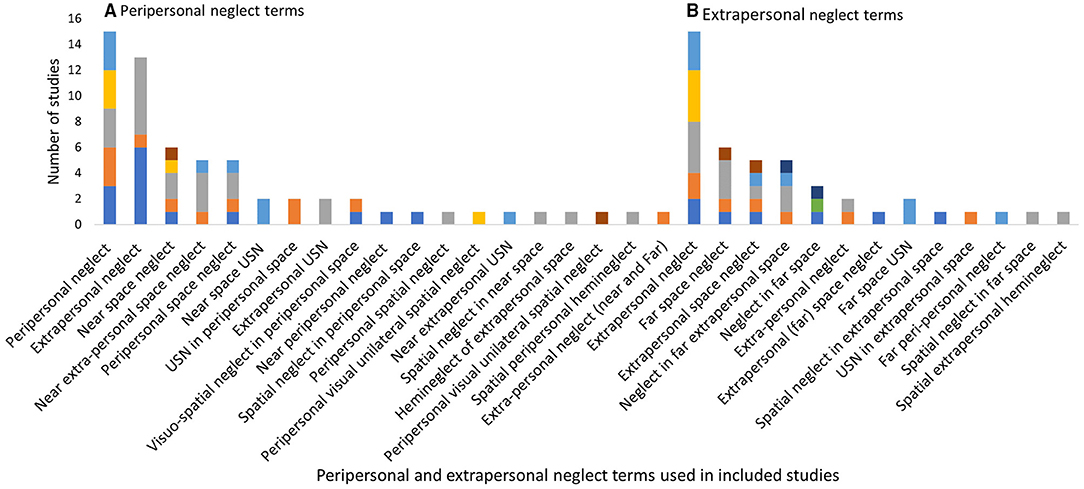
Figure 7. Peripersonal and extrapersonal neglect terms used within the included studies. (A) Peripersonal and (B) extrapersonal.
Extrapersonal neglect (neglect of the far space) had 13 different labels across 45 studies. The label of extrapersonal neglect was most frequently reported (n = 15) as displayed in Figure 7. The majority of studies (n = 19) described this subtype as “beyond reaching distance” (n = 19). Other descriptions include the neglect of the far space (70, 91, 92), or neglect of the navigational or walking space (93, 94).
Dimension of Reference Frame
Egocentric neglect had 16 different labels within 44 studies. The label of egocentric neglect was the most frequently used (n = 20) (Refer to Figure 8). The majority of the studies described this subtype as egocentric (viewer-centered) neglect (n = 11), with some additionally describing that contralesional stimuli from a body centered/egocentric viewpoint are neglected (40, 55, 95, 96). Some descriptions reported the contralesional side of the spatial environment is neglected (97, 98), while others reported the contralesional side of the body is neglected (99, 100) or the “boundaries of the neglected space are not constant” (101).
Allocentric Neglect was referred to in 56 studies with 18 different labels (see Figure 8). The label of allocentric neglect was most frequently reported (n = 17). Descriptions of this subtype varied, as grouped into the following three main categories: (1) Neglect of the contralesional side of objects/stimuli irrespective of their location (53, 79, 98, 99, 102) commonly labeled as stimulus-centered. The side of the neglected object is determined by egocentric coordinates (103). (2) One side of objects are neglected regardless of their orientation (53, 79, 102, 104), commonly labeled as object-centered. For objects that have intrinsic left and right sides, the same side is neglected even if the object is mirror reversed, with the neglected side now being positioned on the ipsilesional side of the person (not influenced by egocentric coordinates). (3) Allocentric neglect is associated with egocentric neglect. It has been suggested that allocentric deficits are only observed in combination with egocentric neglect (97), or that the severity of allocentric deficits are influenced by egocentric factors (allocentric deficits are more severe toward the contralesional side) (95, 100, 105). Allocentric neglect has been challenged as a legitimate subtype of neglect, suggesting it is a particular form of egocentric neglect with the attentional window restricted to the individual object/stimuli (53, 103).
Other neglect subtypes mentioned in the included studies, such as neglect dyslexia and ipsilesional neglect are displayed in Figure 9. Some of the studies considered extinction to be an aspect of spatial neglect [for example, (106, 107)] while others considered extinction to be a separate but related phenomenon [for example (52, 108)].
Assessment Tools
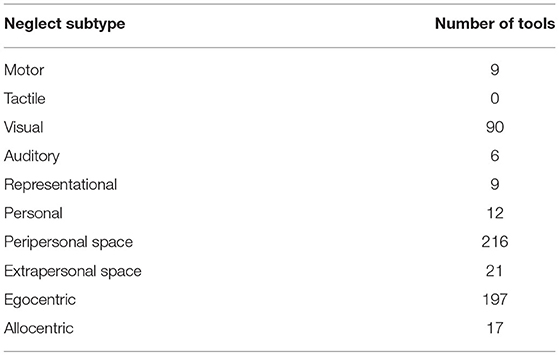
This scoping review identified 292 tools for the screening or diagnosis of neglect. Most studies (n = 248, 67%) included a tool or battery of tools that did not specify the neglect subtype being assessed. The subtype investigated the most within the included studies, as explicitly stated by the authors was visual neglect (n = 90 studies, 24%), followed by personal neglect (n = 42, 11%) and peripersonal neglect (n = 38, 10%). Supplementary Table S2 in the supplementary material presents the names and references of all the spatial neglect tools and the analysis of the underlying subtypes that each tool identified. Most of the tools (57%) were unable to differentiate the underlying subtypes of visual or motor neglect contributing to deficient performance in a task. For example, the majority of the pen and paper tools could not determine if the left side of the paper was neglected due to the person not visually attending to that side of the paper or whether they were neglecting to move their arm toward that side. However, standardized tools that differentiate the neglect subtypes do exist. The number of tools that can identify each subtype is presented in Table 3.
The International Classification of Functioning, Disability and Health (ICF) categories that each tool evaluates are also listed in Supplementary Table S2. Most tools (88%) evaluated at the impairment level (in body function or structure), 18% activity limitations (difficulties in executing activities) and only 1.7% evaluated participation restrictions (difficulties with participating in life roles) (109). With no gold-standard tool for neglect, neglect tools are continually being developed, along with an increasing number of virtual reality and computer-based tools (see Figure 10).
Discussion
The aim of this scoping review was to (1) collate the neglect subtypes and their definitions as reported in the literature and (2) to map the reported tools for assessing neglect and the identified subtypes.
It is evident from the results of this scoping review that there is a lot of variability with the terms used to label this syndrome as a whole and the individual subtypes. There is no consistency with the terms used for each subtype with some terms being used for multiple subtypes. For example, “extrapersonal” is sometimes used to refer to the reaching space (110), while many studies use this term to refer to the far space or outside of reaching (111–113). On the other hand, “extrapersonal” has also been used refer to neglect of the environment; encompassing both within and outside of reaching distance (80). Additionally, some subtypes are being described and grouped into different categories by different studies. For example, perceptual neglect is categorized as incorporating visual and representational neglect by some (41, 42), or visual, tactile and auditory by others (40). Some subtypes have multiple conflicting definitions such as personal neglect and allocentric neglect, which have both been challenged as legitimate neglect subtypes. This inconsistency with the terms and definitions used to refer to the neglect subtypes is creating confusion across the field and is a major barrier for clinicians to understand, compare and apply the literature to clinical practice.
Additionally, there is no agreement on the tools used for identifying neglect. This scoping review has revealed almost 300 neglect tools with documented protocols, and the development of new tools is not slowing down. The majority of tools are brief paper and pencil screening tools that are frequently used in combination with one or two other tools for screening, or as a suite of tools for the comprehensive diagnosis of neglect. Apart from a few validated batteries such as the Behavioral Inattention Test (114), many of the neglect batteries used in the included studies were made from different combinations of tools that have not been validated when used together as a diagnostic suite. This has resulted in high variability in the reported incidence of neglect and a plethora of research that cannot be effectively collated together.
It is important to identify the presenting neglect subtypes to assist with predicting and ameliorating the impact on daily life. Visual neglect in the peripersonal space is most commonly assessed, however the sheer number of tools available for these subtypes would be overwhelming for clinicians to navigate. Alternatively, very few standardized tools for tactile and representational neglect subtypes exist. Only one representational neglect tool (O'clock test) was identified in this review that is not dependent on knowledge of local landmarks and thus could be standardized for use in any country. However, this test has been found to be too difficult to complete for the majority of people with neglect (115). This may be due to the tool relying on other functions such as sustained attention and intact executive functions, which are often impaired after stroke. This can be said for many neglect tools, such as the mirror or pulley devices developed to dissociate motor and visual neglect [for example, see (71, 73, 116)], with impaired performance not necessarily reflecting true neglect behavior if executive functions are impaired. Gaps also exist for identifying motor or auditory neglect in clinical practice. Several tools exist for identifying both subtypes, however many of them are not feasible for use in clinical practice due to the individualized set up and equipment requirements.
Pen and paper tools are commonly used in clinical practice, however they only identify impairments in one spatial dimension—within peripersonal (reaching) space. The use of pen and paper tools may result in a person with undetected neglect in either personal or extrapersonal (outside of reaching) space. Another limitation with pen and paper tools is the inability to differentiate between motor and visual neglect as mentioned previously. Pen and paper tools may be useful to screen for neglect, however other methods of assessment need to be considered for the comprehensive diagnosis of all neglect behaviors.
Tools developed to tease apart the motor and perceptual aspects of neglect have not been able to categorize the two subtypes consistently (117, 118). It has been suggested that minor differences in task requirements such as reaching for a direct target vs. a spatial /delayed judgment may account for these discrepancies (119). Moreover, it is uncertain if neglect subtypes are transient or consistent over time. In the subacute phase post stroke, significant variability in the categorization of visual, motor and personal neglect was observed over three test sessions in 18 (86%) participants (120). The pattern of variability was not consistent with practice effects or spontaneous recovery. It is unclear whether these results can be explained by methodological limitations such as low test-retest reliability of the neglect tools, or actual fluctuations in the neglect behavior.
New tools for identifying neglect are continually being developed, possibly due to the existing tools not being able to detect milder forms of neglect, or an inability to detect the different neglect subtypes. The increasing number of virtual reality and computer-based tools being developed have the potential to increase the task demands, such as dual-task paradigms or speeded reaction time tests, in order to identify mild or subclinical neglect (121–123). However, many of these tools are not feasible to use in clinical settings due to the complex setup or cost requirements.
The following questions were raised by the research team during the process of mapping the subtypes identified with specific tools: (1) All tasks tap into eye movements—thus are all of them tapping into motor (oculomotor) aspects of neglect? It was decided that for the purpose of this review to indicate motor neglect only for the tasks that require a motor response, as opposed to a verbal response or the tracking of eye movements. And (2) If spatial neglect is due to an impairment of spatial representation (124, 125), then do all tasks that require a motor response also tap into representational neglect? For the purpose of this review only tasks that rely on visual memory, such as drawing objects from memory or completing tasks with the eyes closed, along with completing functional tasks in personal space were indicated as being influenced by representational neglect. However, these questions would benefit from further consideration in future studies.
Limitations
We acknowledge that by limiting the included studies to ones that have documented some psychometrics of a tool, this may have excluded some tools from the full analysis. However, we did this to ensure at least some level of investigation of robustness in the tools included. Additionally, determination of discipline of the first author based on their affiliations and work webpage may not be an accurate reflection. However, contacting all the authors to confirm was outside the scope of this review.
Conclusion
There was no consistency with the terms used to refer to neglect and presenting subtypes. It is essential to unify the terminology and definition for each subtype of neglect. There are hundreds of neglect tools available, however many are not able to differentiate presenting subtypes. There have been multiple tools developed to dissociate different types of neglect such as egocentric and allocentric neglect; however, the responsiveness, validity and reliability of these tools has not been compared. It is important for clinicians and researchers to critically evaluate the neglect tools being used for the screening and diagnosis of neglect. The results of this scoping review will inform the scope of tools to be included in a full systematic review summarizing the reliability, validity, responsiveness and utility of neglect tools used in clinical practice. We recommend further work to develop consensus around neglect subtypes, definitions, and assessment.
Deviations From Protocol
This scoping review has not answered the following sub-questions as originally proposed in the protocol of (1) “what definitions have been used by different disciplines?”; and (2) “how have the definitions evolved over time?” There were relatively few studies that described each subtype so trends between the different disciplines or over time were unable to be made. The definitions for each subtype were analyzed collectively. Additionally, it was deemed outside the scope of this review to comment on “what tools are being used by different disciplines?” as originally proposed. It was decided that the included studies may not be representative of all the tools used across the disciplines as the criteria for inclusion were only studies that examined some aspect of validity or reliability of a tool.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
LW completed the database searches and wrote the first draft of the manuscript. LW and TL contributed to the data extraction and analysis. All authors contributed to conception and design of the study, screening of abstracts and full texts, manuscript revision, and read and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Acknowledgment of financial support for LW through an Australian Government Research Training Program Scholarship. TL was funded by a National Health and Medical Research Council Dementia Research Leadership Fellowship (GNT1136269).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.742365/full#supplementary-material
References
1. World Stroke Organization. Learn about stroke. World Stroke Organization 2021. Available online at: https://www.world-stroke.org/world-stroke-day-campaign/why-stroke-matters/learn-about-stroke (accessed June 2, 2021).
2. Heilman KM, Watson RT, Valenstein E. Neglect and related disorders. In: Heilman KM, Valenstein E, editors. Clinical neuropsychology. 4th ed. US: Oxford University Press. (2003) p. 296–346. doi: 10.1016/B0-12-226870-9/00804-2
3. Vallar G, Calzolari E. Unilateral spatial neglect after posterior parietal damage. Handb Clin Neurol. (2018) 151:287–312. doi: 10.1016/B978-0-444-63622-5.00014-0
4. Chen P, Chen CC, Hreha K, Goedert KM, Barrett AM. Kessler Foundation neglect assessment process uniquely measures spatial neglect during activities of daily living. Arch Phys Med Rehabil. (2015) 96:869–76. doi: 10.1016/j.apmr.2014.10.023
5. Demeyere N, Gillebert CR. Ego- and allocentric visuospatial neglect: Dissociations, prevalence, and laterality in acute stroke. Neuropsychology. (2019) 33:490–8. doi: 10.1037/neu0000527
6. Li K, Malhotra PA. Spatial neglect. Pract Neurol. (2015) 15:333–9. doi: 10.1136/practneurol-2015-001115
7. Riestra AR, Barrett AM. Rehabilitation of spatial neglect. Handb Clin Neurol. (2013) 110:347–55. doi: 10.1016/B978-0-444-52901-5.00029-0
8. Bowen A, McKenna K, Tallis RC. Reasons for variability in the reported rate of occurrence of unilateral spatial neglect after stroke. Stroke. (1999) 30:1196–202. doi: 10.1161/01.STR.30.6.1196
9. Ricci R, Salatino A, Garbarini F, Ronga I, Genero R, Berti A, et al. Effects of attentional and cognitive variables on unilateral spatial neglect. Neuropsychologia. (2016) 92:158–66. doi: 10.1016/j.neuropsychologia.2016.05.004
10. Chen P, Hreha K, Kong Y, Barrett AM. Impact of spatial neglect on stroke rehabilitation: evidence from the setting of an inpatient rehabilitation facility. Arch Phys Med Rehabil. (2015) 96:1458–66. doi: 10.1016/j.apmr.2015.03.019
11. Di Monaco M, Schintu S, Dotta M, Barba S, Taperoo R. Severity of unilateral spatial neglect is an independent predictor of functional outcome after acute inpatient rehabilitation in individuals with right hemispheric stroke. Arch Phys Med Rehabil. (2011) 92:1250–6. doi: 10.1016/j.apmr.2011.03.018
12. Barrett AM, Buxbaum LJ, Coslett HB, Edwards E, Heilman KM, Hillis AE, et al. Cognitive rehabilitation interventions for neglect and related disorders: Moving from bench to bedside in stroke patients. J Cogn Neurosci. (2006) 18:1223–36. doi: 10.1162/jocn.2006.18.7.1223
13. Azouvi P. The ecological assessment of unilateral neglect. Ann Phys Rehabil Med. (2017) 60:186–90. doi: 10.1016/j.rehab.2015.12.005
14. Azouvi P, Samuel C, Louis-Dreyfus A, Bernati T, Bartolomeo P, Beis JM, et al. Sensitivity of clinical and behavioural tests of spatial neglect after right hemisphere stroke. J Neurology Neurosurgery and Psychiatry. (2002) 73:160–6. doi: 10.1136/jnnp.73.2.160
15. Suchan J, Rorden C, Karnath HO. Neglect severity after left and right brain damage. Neuropsychologia. (2012) 50:1136–41. doi: 10.1016/j.neuropsychologia.2011.12.018
16. Bonato M. Unveiling residual, spontaneous recovery from subtle hemispatial neglect three years after stroke. Front Hum Neurosci. (2015) 9:1–9. doi: 10.3389/fnhum.2015.00413
17. Azouvi P, Bartolomeo P, Beis J-M, Perennou D, Pradat-Diehl P, Rousseaux M, et al. battery of tests for the quantitative assessment of unilateral neglect. Restor Neurol Neurosci. (2006) 24:273–85.
18. Bonato M, Priftis K, Umilta C, Zorzi M. Computer-based attention-demanding testing unveils severe neglect in apparently intact patients. Behavioural Neurology. (2013) 26:179–81. doi: 10.1155/2013/139812
19. Hasegawa C, Hirono N, Yamadori A. Discrepancy in unilateral spatial neglect between daily living and neuropsychological test situations: a single case study. Neurocase. (2011) 6:518–26. doi: 10.1080/13554794.2010.547506
20. Pflugshaupt T, Bopp SA, Heinemann D, Mosimann UP, von Wartburg R, Nyffeler T, et al. Residual oculomotor and exploratory deficits in patients with recovered hemineglect. Neuropsychologia. (2004) 42:1203–11. doi: 10.1016/j.neuropsychologia.2004.02.002
21. Pitteri M, Chen P, Passarini L, Albanese S, Meneghello F, Barrett A. Conventional and functional assessment of spatial neglect: clinical practice suggestions. Neuropsychology. (2018) 32:835–42. doi: 10.1037/neu0000469
22. Vallar G. Spatial hemineglect in humans. Trends Cogn Sci. (1998) 2:87–97. doi: 10.1016/S1364-6613(98)01145-0
23. Deouell LY, Sacher Y, Soroker N. Assessment of spatial attention after brain damage with a dynamic reaction time test. J Int Neuropsychological Society. (2005) 11:697–707. doi: 10.1017/S1355617705050824
24. Appelros P, Nydevik I, Karlsson GM, Thorwalls A, Seiger Å. Recovery from unilateral neglect after right-hemisphere stroke. Disability & Rehabilitation. (2004) 26:471–7. doi: 10.1080/09638280410001663058
25. Kerkhoff G, Schenk T. Rehabilitation of neglect: an update. Neuropsychologia. (2012) 50:1072–9. doi: 10.1016/j.neuropsychologia.2012.01.024
26. Fortis P, Chen P, Goedert KM, Barrett AM. Effects of prism adaptation on motor-intentional spatial bias in neglect. Neuroreport. (2011) 22:700–5. doi: 10.1097/WNR.0b013e32834a3e20
27. Barrett AM, Burkholder S. Monocular patching in subjects with right-hemisphere stroke affects perceptual-attentional bias. J Rehabil Res Dev. (2006) 43:337–46. doi: 10.1682/JRRD.2005.01.0015
28. Adair JC, Na DL, Schwartz RL, Heilman KM. Caloric stimulation in neglect: Evaluation of response as a function of neglect type. J Int Neuropsychological Society. (2003) 9:983–8. doi: 10.1017/S1355617703970020
29. Barrett AM, Goedert KM, Carter AR, Chaudhari A. Spatial neglect treatment: The brain's spatial-motor Aiming systems. Neuropsychological Rehabilitation. (2021) 1–27. doi: 10.1080/09602011.2020.1862678
30. Menon A, Korner-Bitensky N. Evaluating unilateral spatial neglect post stroke: working your way through the maze of assessment choices. Top Stroke Rehabil. (2004) 11:41–66. doi: 10.1310/KQWL-3HQL-4KNM-5F4U
31. Ogourtsova T, Souza Silva W, Archambault PS, Lamontagne A. Virtual reality treatment and assessments for post-stroke unilateral spatial neglect: A systematic literature review. Neuropsychol Rehabil. (2017) 27:409–54. doi: 10.1080/09602011.2015.1113187
32. Ogourtsova T, Archambault P, Lamontagne A. Impact of post-stroke unilateral spatial neglect on goal-directed arm movements: Systematic literature review. Top Stroke Rehabil. (2015) 22:397–428. doi: 10.1179/1074935714Z.0000000046
33. Vahlberg B, Hellström K. Treatment and assessment of neglect after stroke – from a physiotherapy perspective: a systematic review. Adv Physiother. (2008) 10:178–87. doi: 10.1080/14038190701661239
34. Arskey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
35. The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers' Manaual. vol. 2015 edition/supplement. South Australia: University of Adelaide. (2015).
36. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation the PRISMA-ScR statement. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
38. Buxbaum LJ, Palermo MA, Mastrogiovanni D, Read MS, Rosenberg-Pitonyak E, Rizzo AA, et al. Assessment of spatial attention and neglect with a virtual wheelchair navigation task. J Clin Exp Neuropsychol. (2008) 30:650–60. doi: 10.1080/13803390701625821
39. Lee BH, Suh MK, Kim EJ, Seo SW, Choi KM, Kim GM, et al. Neglect dyslexia: Frequency, association with other hemispatial neglects, and lesion localization. Neuropsychologia. (2009) 47:704–10. doi: 10.1016/j.neuropsychologia.2008.11.027
40. Montedoro V, Alsamour M, Dehem S, Lejeune T, Dehez B, Edwards MG. Robot diagnosis test for egocentric and allocentric hemineglect. Archives of Clinical Neuropsychology. (2019) 34:481–94. doi: 10.1093/arclin/acy062
41. Bailey MJ, Riddoch MJ, Crome P. Evaluation of a test battery for hemineglect in elderly stroke patients for use by therapists in clinical practice. NeuroRehabilitation. (2000) 14:139–50. doi: 10.3233/NRE-2000-14303
42. Mancini F, Bricolo E, Mattioli FC, Vallar G. Visuo-haptic interactions in unilateral spatial neglect: The cross modal Judd illusion. Front Psychol. (2011) 2:341. doi: 10.3389/fpsyg.2011.00341
43. Jehkonen M, Ahonen J, Dastidar P, Koivisto A, Laippala P, Vilkki J, et al. Visual neglect as a predictor of functional outcome one year after stroke. Acta Neurol Scand. (2000) 101:195–201. doi: 10.1034/j.1600-0404.2000.101003195.x
44. Lunven M, Thiebaut De Schotten M, Bourlon C, Duret C, Migliaccio R, Rode G, et al. White matter lesional predictors of chronic visual neglect: a longitudinal study. Brain: A Journal of Neurology. (2015) 138:746–60. doi: 10.1093/brain/awu389
45. Pavani F, Làdavas E, Driver J. Selective deficit of auditory localisation in patients with visuospatial neglect. Neuropsychologia. (2002) 40:291–301. doi: 10.1016/S0028-3932(01)00091-4
46. Rowe FJ, Hepworth LR, Hanna KL, Howard C. Visual impairment screening assessment (VISA) tool: pilot validation. BMJ Open. (2018) 8:e020562. doi: 10.1136/bmjopen-2017-020562
47. Semrau J, Wang J, Herter T, Scott S, Dukelow S. Relationship between visuospatial neglect and kinesthetic deficits after stroke. Neurorehabil Neural Repair. (2015) 29:318–28. doi: 10.1177/1545968314545173
48. Na DL, Adair JC, Choi SH, Seo DW, Kang Y, Heilman KM. Ipsilesional versus contralesional neglect depends on attentional demands. Cortex. (2000) 36:455–67. doi: 10.1016/S0010-9452(08)70532-X
49. Park KC, Lee BH, Kim EJ, Shin MH, Choi KM, Yoon SS, et al. Deafferentation-disconnection neglect induced by posterior cerebral artery infarction. Neurology. (2006) 66:56–61. doi: 10.1212/01.wnl.0000191306.67582.7a
50. Vallar G, Rusconi ML, Geminiani G, Berti A, Cappa SF. Visual and nonvisual neglect after unilateral brain lesions: Modulation by visual input. Int J Neurosci. (1991) 61:229–39. doi: 10.3109/00207459108990740
51. Vallar G, Antonucci G, Guariglia C, Pizzamiglio L. Deficits of position sense, unilateral neglect and optokinetic stimulation. Neuropsychologia. (1993) 31:1191–200. doi: 10.1016/0028-3932(93)90067-A
52. Sambo CF, Vallar G, Fortis P, Ronchi R, Posteraro L, Forster B, et al. Visual and spatial modulation of tactile extinction: Behavioural and electrophysiological evidence. Front Hum Neurosci. (2012) 6:217. doi: 10.3389/fnhum.2012.00217
53. Marsh EB, Hillis AE. Dissociation between egocentric and allocentric visuospatial and tactile neglect in acute stroke. Cortex. (2008) 44:1215–20. doi: 10.1016/j.cortex.2006.02.002
54. Vallar G, Daini R, Antonucci G. Processing of illusion of length in spatial hemineglect: A study of line bisection. Neuropsychologia. (2000) 38:1087–97. doi: 10.1016/S0028-3932(99)00139-6
55. Basagni B, De Tanti A, Damora A, Abbruzzese L, Varalta V, Antonucci G, et al. The assessment of hemineglect syndrome with cancellation tasks: a comparison between the Bells test and the Apples test. Neurol Sci. (2017) 38:2171–6. doi: 10.1007/s10072-017-3139-7
56. Spreij LA, Ten Brink AF, Visser-Meily JMA, Nijboer TCW. Simulated driving: The added value of dynamic testing in the assessment of visuo-spatial neglect after stroke. J Neuropsychol. (2020) 14:28–45. doi: 10.1111/jnp.12172
57. Pavani F, Làdavas E, Driver J. Gaze direction modulates auditory spatial deficits in stroke patients with neglect. Cortex. (2005) 41:181–8. doi: 10.1016/S0010-9452(08)70892-X
58. Zimmer U, Lewald J, Karnath HO. Disturbed sound lateralization in patients with spatial neglect. J Cogn Neurosci. (2003) 15:694–703. doi: 10.1162/jocn.2003.15.5.694
59. Bartolomeo P. D'erme P, Gainotti G. The relationship between visuospatial and representational neglect. Neurology. (1994) 44:1710–4. doi: 10.1212/WNL.44.9.1710
60. Bourlon C, Pradat-Diehl P, Duret C, Azouvi P, Bartolomeo P. Seeing and imagining the “same” objects in unilateral neglect. Neuropsychologia. (2008) 46:2602–6. doi: 10.1016/j.neuropsychologia.2008.04.002
61. Lopes MAL, Ferreira HP, Carvalho JC, Cardoso L, Andre C. Screening tests are not enough to detect hemineglect. Arq Neuropsiquiatr. (2007) 65:1192–5. doi: 10.1590/S0004-282X2007000700019
62. Meador KJ, Loring DW, Bowers D, Heilman KM. Remote memory and neglect syndrome. Neurology. (1987) 37:522–6. doi: 10.1212/WNL.37.3.522
63. Rode G, Revol P, Rossetti Y, Boisson D, Bartolomeo P. Looking while imagining: The influence of visual input on representational neglect. Neurology. (2007) 68:432–7. doi: 10.1212/01.wnl.0000252936.54063.b0
64. Rode G, Cotton F, Revol P, Jacquin-Courtois S, Rossetti Y, Bartolomeo P. Representation and disconnection in imaginal neglect. Neuropsychologia. (2010) 48:2903–11. doi: 10.1016/j.neuropsychologia.2010.05.032
65. Vuilleumier P, Sergent C, Schwartz S, Valenza N, Girardi M, Husain M, et al. Impaired perceptual memory of locations across gaze-shifts in patients with unilateral spatial neglect. J Cogn Neurosci. (2007) 19:1388–406. doi: 10.1162/jocn.2007.19.8.1388
66. Bartolomeo P, Bachoud-Lévi AC, Azouvi P, Chokron S. Time to imagine space: A chronometric exploration of representational neglect. Neuropsychologia. (2005) 43:1249–57. doi: 10.1016/j.neuropsychologia.2004.12.013
67. Malhotra P, Jäger HR, Parton A, Greenwood R, Playford ED, Brown MM, et al. Spatial working memory capacity in unilateral neglect. Brain. (2005) 128:424–35. doi: 10.1093/brain/awh372
68. Mark VW, Kooistra CA, Heilman KM. Hemispatial neglect affected by non-neglected stimuli. Neurology. (1988) 38:1207–11. doi: 10.1212/WNL.38.8.1207
69. Guariglia C, Palermo L, Piccardi L, Iaria G, Incoccia C. Neglecting the left side of a city square but not the left side of its clock: prevalence and characteristics of representational neglect. PLoS ONE. (2013) 8:e67390. doi: 10.1371/journal.pone.0067390
70. Piccardi L, Bianchini F, Zompanti L, Guariglia C. Pure representational neglect and navigational deficits in a case with preserved visuo-spatial working memory. Neurocase. (2008) 14:329–42. doi: 10.1080/13554790802366012
71. Na DL, Adair JC, Williamson DJG, Schwartz RL, Haws B, Heilman KM. Dissociation of sensory-attentional from motor-intentional neglect. J Neurology Neurosurgery and Psychiatry. (1998) 64:331–8. doi: 10.1136/jnnp.64.3.331
72. Webster JS, Rapport LJ, Godlewski MC, Abadee PS. Effect of attentional bias to right space on wheelchair mobility. J Clin Exp Neuropsychol. (1994) 16:129–37. doi: 10.1080/01688639408402623
73. Bisiach E, Geminiani G, Berti A, Rusconi ML. Perceptual and premotor factors of unilateral neglect. Neurology. (1990) 40:1278. doi: 10.1212/WNL.40.8.1278
74. Barrett AM, Boukrina O, Saleh S. Ventral attention and motor network connectivity is relevant to functional impairment in spatial neglect after right brain stroke. Brain Cogn. (2019) 129:16–24. doi: 10.1016/j.bandc.2018.11.013
75. Làdavas E, Umiltà C, Ziani P, Brogi A, Minarini M. The role of right side objects in left side neglect: A dissociation between perceptual and directional motor neglect. Neuropsychologia. (1993) 31:761–73. doi: 10.1016/0028-3932(93)90127-L
76. Bartolomeo P, D'Erme P, Perri R, Gainotti G. Perception and action in hemispatial neglect. Neuropsychologia. (1998) 36:227–37. doi: 10.1016/S0028-3932(97)00104-8
77. Bartolomeo P, Chokron S, Gainotti G. Laterally directed arm movements and right unilateral neglect after left hemisphere damage. Neuropsychologia. (2001) 39:1013–21. doi: 10.1016/S0028-3932(01)00042-2
78. Bisiach E, Ricci R, Lualdi M, Colombo MR. Perceptual and response bias in unilateral neglect: two modified versions of the Milner Landmark Task. Brain and Cognition. (1998) 37:369–86 18p. doi: 10.1006/brcg.1998.1003
79. Khurshid S, Trupe LA, Newhart M, Davis C, Molitoris JJ, Medina J, et al. Reperfusion of specific cortical areas is associated with improvement in distinct forms of hemispatial neglect. Cortex: A Journal Devoted to the Study of the Nervous System & Behavior. (2012) 48:530–9. doi: 10.1016/j.cortex.2011.01.003
80. Vallar G, Zilli T, Gandola M, Bottini G. Productive and defective impairments in the neglect syndrome: graphic perseveration, drawing productions and optic prism exposure. Cortex: A Journal Devoted to the Study of the Nervous System & Behavior. (2006) 42:911–20. doi: 10.1016/S0010-9452(08)70435-0
81. Ye L-L, Cao L, Xie H-X, Shan G-X, Zhang Y-M, Song W-Q. Visual-spatial neglect after right-hemisphere stroke: behavioral and electrophysiological evidence. Chin Med J (Engl). (2019) 132:1063–70. doi: 10.1097/CM9.0000000000000218
82. Husain M, Mattingley JB, Rorden C, Kennard C, Driver J. Distinguishing sensory and motor biases in parietal and frontal neglect. Brain. (2000) 123:1643–59. doi: 10.1093/brain/123.8.1643
83. Beschin N, Robertson IH. Personal versus extrapersonal neglect: A group study of their dissociation using a reliable clinical test. Cortex: A Journal Devoted to the Study of the Nervous System and Behavior. (1997) 33:379–84. doi: 10.1016/S0010-9452(08)70013-3
84. Sposito AV, Bolognini N, Vallar G, Posteraro L, Maravita A. The spatial encoding of body parts in patients with neglect and neurologically unimpaired participants. Neuropsychologia. (2010) 48:334–40. doi: 10.1016/j.neuropsychologia.2009.09.026
85. Baas U, de Haan B, Grässli T, Karnath HO, Mueri R, Perrig WJ, et al. Personal neglect-A disorder of body representation? Neuropsychologia. (2011) 49:898–905. doi: 10.1016/j.neuropsychologia.2011.01.043
86. Chen-Sea MJ. Validating the Draw-A-Man Test as a personal neglect test. Am J Occupational Therapy. (2000) 54:391–7. doi: 10.5014/ajot.54.4.391
87. Chen-Sea M. Unilateral neglect and functional significance among patients with stroke. Occupational Therapy Journal of Research. (2001) 21:223–40. doi: 10.1177/153944920102100402
88. Wee JYM, Hopman WM. Comparing consequences of right and left unilateral neglect in a stroke rehabilitation population. American Journal of Physical Medicine & Rehabilitation. (2008) 87:910–20. doi: 10.1097/PHM.0b013e31818a58bd
89. Mark VW, Heilman KM. Diagonal neglect on cancellation. Neuropsychologia. (1997) 35:1425–36. doi: 10.1016/S0028-3932(97)00067-5
90. Mark VW, Heilman KM. Diagonal spatial neglect. Journal of Neurology Neurosurgery and Psychiatry. (1998) 65:348–52. doi: 10.1136/jnnp.65.3.348
91. Berti A, Smania N, Rabuffetti M, Ferrarin M, Spinazzola L, D'Amico A, et al. Coding of far and near space during walking in neglect patients. Neuropsychology. (2002) 16:390–9. doi: 10.1037/0894-4105.16.3.390
92. Lindell AB, Jalas MJ, Tenovuo O, Brunila T, Voeten MJ, Hamalainen H. Clinical assessment of hemispatial neglect: Evaluation of different measures and dimensions. Clin Neuropsychol. (2007) 21:479–97. doi: 10.1080/13854040600630061
93. De Nigris A, Piccardi L, Bianchini F, Palermo L, Incoccia C, Guariglia C. Role of visuo-spatial working memory in path integration disorders in neglect. Cortex: A Journal Devoted to the Study of the Nervous System & Behavior. (2013) 49:920–30 11p. doi: 10.1016/j.cortex.2012.03.009
94. Pizzamiglio L, Cappa S, Vallar G, Zoccolotti P, Bottini G, Ciurlil P, et al. Visual neglect for far and near extra-personal space in humans. Cortex. (1989) 25:471–7. doi: 10.1016/S0010-9452(89)80060-7
95. Rorden C, Hjaltason H, Fillmore P, Fridriksson J, Kjartansson O, Magnusdottir S, et al. Allocentric neglect strongly associated with egocentric neglect. Neuropsychologia. (2012) 50:1151–7. doi: 10.1016/j.neuropsychologia.2012.03.031
96. Shirani P, Thorn J, Davis C, Heidler-Gary J, Newhart M, Gottesman RF, et al. Severity of hypoperfusion in distinct brain regions predicts severity of hemispatial neglect in different reference frames. Stroke. (2009) 40:3563–6. doi: 10.1161/STROKEAHA.109.561969
97. Niemeier M, Karnath HO. Simulating and testing visual exploration in spatial neglect based on a new model for cortical coordinate transformation. Experimental Brain Research. (2002) 145:512–9. doi: 10.1007/s00221-002-1132-7
98. Verdon V, Schwartz S, Lovblad K-O, Hauert C-A, Vuilleumier P. Neuroanatomy of hemispatial neglect and its functional components: a study using voxel-based lesion-symptom mapping. Brain. (2010) 133:880–94. doi: 10.1093/brain/awp305
99. Prangrat T, Mann WC, Tomita M. Impact of unilateral neglect on assistive device use. Technology & Disability. (2000) 12:53–69. doi: 10.3233/TAD-2000-12107
100. Rorden C, Li D, Karnath HO. Biased temporal order judgments in chronic neglect influenced by trunk position. Cortex. (2018) 99:272–80. doi: 10.1016/j.cortex.2017.12.008
101. Tanaka T, Sugihara S, Nara H, Ino S, Ifukube T. A preliminary study of clinical assessment of left unilateral spatial neglect using a head mounted display system (HMD) in rehabilitation engineering technology. J Neuroeng Rehabil. (2005) 2:31. doi: 10.1186/1743-0003-2-31
102. Ota H, Fujii T, Suzuki K, Fukatsu R, Yamadori A. Dissociation of body-centered and stimulus-centered representations in unilateral neglect. Neurology. (2001) 57:2064–9. doi: 10.1212/WNL.57.11.2064
103. Driver J, Baylis GC, Goodrich SJ, Rafal RD. Axis-based neglect of visual shapes. Neuropsychologia. (1994) 32:1353–6. doi: 10.1016/0028-3932(94)00068-9
104. di Pellegrino G, Frassinetti F, Basso G. Coordinate frames for naming misoriented chimerics: a case study of visuo-spatial neglect. Cortex. (1995) 31:767–77. doi: 10.1016/S0010-9452(13)80027-5
105. Karnath HO, Mandler A, Clavagnier S. Object-based neglect varies with egocentric position. J Cogn Neurosci. (2011) 23:2983–93. doi: 10.1162/jocn_a_00005
106. Bienkiewicz MMN, Brandi ML, Hughes C, Voitl A, Hermsdorfer J. The complexity of the relationship between neuropsychological deficits and impairment in everyday tasks after stroke. Brain and Behavior. (2015) 5:e00371. doi: 10.1002/brb3.371
107. Liu CC, Veldhuijzen DS, Ohara S, Winberry J, Greenspan JD, Lenz FA. Spatial attention to thermal pain stimuli in subjects with visual spatial hemi-neglect: Extinction, mislocalization and misidentification of stimulus modality. Pain. (2011) 152:498–506. doi: 10.1016/j.pain.2010.10.017
108. Dombrowe I, Donk M, Wright H, Olivers CNL, Humphreys GW. The contribution of stimulus-driven and goal-driven mechanisms to feature-based selection in patients with spatial attention deficits. Cogn Neuropsychol. (2012) 29:249–74. doi: 10.1080/02643294.2012.712509
109. World Health Organization. Towards an common language for Functioning, Disability and Health: ICF - The International Classification of Functioning, Disability and Health 2002.
110. Bolognini N, Casanova D, Maravita A, Vallar G. Bisecting real and fake body parts: Effects of prism adaptation after right brain damage. Front Hum Neurosci. (2012). doi: 10.3389/fnhum.2012.00154
111. Ten Brink AF, Visser-Meily JM, Nijboer TC. Dynamic assessment of visual neglect: The mobility assessment course as a diagnostic tool. J Clin Exp Neuropsychol. (2018) 40:161–72. doi: 10.1080/13803395.2017.1324562
112. Cunningham LJ, O'Rourke K, Finlay C, Gallagher M. A preliminary investigation into the psychometric properties of the Dublin Extrapersonal Neglect Assessment (DENA): A novel screening tool for extrapersonal neglect. Neuropsychol Rehabil. (2017) 27:349–68. doi: 10.1080/09602011.2015.1084334
113. Kim DY, Ku J, Chang WH, Park TH, Lim JY, Han K, et al. Assessment of post-stroke extrapersonal neglect using a three-dimensional immersive virtual street crossing program. Acta Neurol Scand. (2010) 121:171–7. doi: 10.1111/j.1600-0404.2009.01194.x
114. Wilson B, Cockburn J, Halligan P. Development of a behavioral test of visuospatial neglect. Arch Phys Med Rehabil. (1987) 68:98–102.
115. Grossi D, Angelini R, Pecchinenda A, Pizzamiglio L. Left imaginal neglect in heminattention: experimental study with the O'clock Test. Behav Neurol. (1993) 6:155–8. doi: 10.1155/1993/586357
116. Goedert KM, Chen P, Botticello A, Masmela JR, Adler U, Barrett AM. Psychometric evaluation of neglect assessment reveals motor-exploratory predictor of functional disability in acute-stage spatial neglect. Archives of Physical Medicine & Rehabilitation. (2012) 93:137–42. doi: 10.1016/j.apmr.2011.06.036
117. Harvey M, Krämer-McCaffery T, Dow L, Murphy PJS, Gilchrist ID. Categorisation of “perceptual” and “premotor” neglect patients across different tasks: is there strong evidence for a dichotomy? Neuropsychologia. (2002) 40:1387–95. doi: 10.1016/S0028-3932(01)00202-0
118. Harvey M, Olk B. Comparison of the Milner and Bisiach Landmark Tasks: can neglect patients be classified consistently? Cortex. (2004) 40:659–65. doi: 10.1016/S0010-9452(08)70162-X
119. Harvey M, Rossit S. Visuospatial neglect in action. Neuropsychologia. (2012) 50:1018–28. doi: 10.1016/j.neuropsychologia.2011.09.030
120. Hamilton RH, Coslett HB, Buxbaum LJ, Whyte J, Ferraro MK. Inconsistency of performance on neglect subtype tests following acute right hemisphere stroke. Journal of the International Neuropsychological Society : JINS. (2008) 14:23–32. doi: 10.1017/S1355617708080077
121. Andres M, Geers L, Marnette S, Coyette F, Bonato M, Priftis K, et al. Increased cognitive load reveals unilateral neglect and altitudinal extinction in chronic stroke. J Int Neuropsychological Society. (2019) 25:644–53. doi: 10.1017/S1355617719000249
122. Blini E, Romeo Z, Spironelli C, Pitteri M, Meneghello F, Bonato M, et al. Multi-tasking uncovers right spatial neglect and extinction in chronic left-hemisphere stroke patients. Neuropsychologia. (2016) 92:147–57. doi: 10.1016/j.neuropsychologia.2016.02.028
123. Villarreal S, Linnavuo M, Sepponen R, Vuori O, Jokinen H, Hietanen M. Dual-task in large perceptual space reveals subclinical hemispatial neglect. J Int Neuropsychological Society. (2020) 26:993–1005. doi: 10.1017/S1355617720000508
124. Bisiach E, Luzzatti C. Unilateral neglect of representational space. Cortex. (1978) 14:129–33. doi: 10.1016/S0010-9452(78)80016-1
Keywords: perceptual disorders, stroke, patient outcome assessment, neuropsychological test, spatial neglect, neglect
Citation: Williams LJ, Kernot J, Hillier SL and Loetscher T (2021) Spatial Neglect Subtypes, Definitions and Assessment Tools: A Scoping Review. Front. Neurol. 12:742365. doi: 10.3389/fneur.2021.742365
Received: 16 July 2021; Accepted: 14 October 2021;
Published: 24 November 2021.
Edited by:
Pierluigi Zoccolotti, Sapienza University of Rome, ItalyCopyright © 2021 Williams, Kernot, Hillier and Loetscher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lindy J. Williams, bGluZHkud2lsbGlhbXNAdW5pc2EuZWR1LmF1
 Lindy J. Williams
Lindy J. Williams Jocelyn Kernot
Jocelyn Kernot Susan L. Hillier
Susan L. Hillier Tobias Loetscher
Tobias Loetscher