- 1Department of Respiratory and Critical Care Medicine, West China Medical School/West China Hospital, Sichuan University, Chengdu, China
- 2Department of Neurosurgery, West China Medical School/West China Hospital, Sichuan University, Chengdu, China
- 3Department of Neurosurgery, Affiliated Hospital of Chengdu University, Chengdu, China
- 4Department of Orthopedics, Dandong Central Hospital, China Medical University, Shenyang, China
Background and Purpose: Chronic obstructive pulmonary disease (COPD) has been associated with several complications and mortality in acutely ill patients. For patients with aneurysmal subarachnoid hemorrhage (aSAH), the association between COPD and clinical outcomes remains unclear.
Methods: In this retrospective cohort study, we analyzed consecutive aSAH patients admitted to the West China Hospital between 2014 and 2019. Propensity score matching analysis and cox regression models was used to assess the association between COPD and mortality. The primary outcome was long-term mortality.
Results: Using a clinical database from a large university medical center, 2,925 patients with aSAH were identified, of whom 219 (7.5%) also had COPD. Patients were followed-up for a median of 3.8 years, and during follow-up 633 patients (21.6%) died. Long-term mortality was higher in patients with COPD compared to patients without COPD in the Cox regression models [adjusted hazard ratio (HR) 1.52, 95% confidence interval (CI) 1.14–2.02]. Propensity score matching analysis also showed similar associations between COPD and mortality in hospital, at 1 year, at 2 years, and at long-term. Similarly, patients with COPD had significantly higher incidence of infections, such as pneumonia [odds ratio (OR) 3.24, 95% CI 2.30–4.56], urinary tract infection (OR 1.81, 95% CI 1.20–2.73), bloodstream infection (OR 3.83, 95% CI 1.84–7.99), and hospital infection (OR 3.24, 95% CI 2.28–4.61).
Conclusions: Among aSAH patients, COPD is associated with increased mortality. COPD represents a significant risk factor for infections. Given that these are preventable complications, our findings are of clinical relevance.
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death in the world (1–3) and is currently characterized by systemic involvement and multiple comorbidities (4). Growing evidence indicated that COPD independently predicts mortality and morbidity in patients undergoing surgery and patients with critically ill (5–8). However, the impact of COPD on outcomes in patients with aneurysmal subarachnoid hemorrhage (aSAH) remains unclear (9). Only one observational study has addressed the association between COPD and mortality in patients with aSAH (10). That study demonstrated that COPD did not increase in-hospital mortality after adjusting confounders. The published literature is sparse with respect to the long-term mortality of patients with COPD after aSAH.
Moreover, there is no data identifying the impact of COPD on infectious complications in patients with aSAH. The question of the potential impact of COPD on infectious complications in patients with aSAH is important because if COPD was indeed associated with infections, patients with COPD after aSAH would benefit from prophylactic antibiotics. A Cochrane review concluded that use of prophylactic antibiotics results in a benefit in reducing exacerbations in COPD patients (11). However, evidence from two large randomized clinical trials did not found the benefits of use of prophylactic antibiotics in lower risk of pneumonia or death for patients with stroke (12, 13). A possible explanation for the failure is that the included patients in the trials have low risk of infection, with 7 and 16% patients developing pneumonia, respectively. For patients with aSAH, about 20% of them develop pneumonia (14). COPD is also one of the most frequent comorbid conditions and a risk factor for developing pneumonia in critically ill patient (15).
With the increasing global incidence of COPD (16) and its high prevalence in patient with aSAH (10), we assessed the impact of COPD on outcomes in patient with aSAH, using propensity score matching (PSM) to form groups for comparison with near-identical distributions of background and potential confounder variables.
Materials and Methods
Study Design
We performed a retrospective cohort study. We consecutively evaluated the electronic health record of patients with aSAH admitted to the West China Hospital, Sichuan University, from January 2014 to June 2019, which is the largest hospital in Sichuan province, with a population of 91 million. This study was approved by the ethics committee of West China hospital (No. 20191133). The ethics committee has exempted written informed consent of patients included in the study because this study posed minimal-risk research and used only observational data.
Study Population
Patients were eligible if they had an intracranial aneurysm identified by imaging in the presence of SAH. Intracranial aneurysms were identified by cerebral angiography, MRA, CTA, or operation. SAH was confirmed with neuroimaging (including CT, MRI, or angiography), cerebrospinal fluid analysis, or intraoperatively by a neurosurgeon.
Participants were excluded in case of aneurysms related to trauma, arteriovenous malformations, fusiform aneurysms, or non-definitive aneurysms, aneurysms that were treated before the presentation, or trauma SAH. Moreover, we also excluded patients whose household registration was not in Sichuan province or whose personal identification number was not found in the electronic medical record system, because we used personal identification number to identify mortality by searching the databases of the Household Registration Administration System in Sichuan province.
Demographics Characteristics
The primary exposure was COPD. Diagnosis of COPD was based on medical reports. Demographic and clinical data included age, sex, hypertension, diabetes mellitus, coronary heart disease, smoking (current, ever, never), alcohol use, size of aneurysm, location of aneurysm, external ventricular drain, and treatment of aneurysm. Hunt & Hess grade and Fisher grade were also obtained on admission.
Outcomes
The primary outcome was long-term mortality, which was defined as the mortality at the longest follow-up. The time of death was determined by searching the data bases of the Household Registration Administration System. In China, every resident has a unique identification number. If one dies, a death certificate should be reported to the household registration offices in the bureau of public security within 30 days as required by law. As the death certificate database is accurate and complete, the rate of loss to follow-up of our cohort was negligible.
Secondary outcomes included mortality in hospital, 1 year, and 2 years, neurological complications, infectious complications, acute kidney injury, length of hospital stay, and poor functional outcome at the time of discharge. Infectious outcomes were pneumonia, intracranial infection, urinary tract infection, and bloodstream infection. Neurological complications were hydrocephalus, delayed neurological ischemic deficits, rebleeding, and seizures.
Pneumonia is defined as a state of lung tissue inflammation of infectious etiology with the radiographic demonstration of parenchymal disease. Bloodstream infection was defined as positive blood culture necessitating treatment with antibiotics. Urinary tract infection was a positive urine culture or positive leukocyte esterase and positive nitrite on a urinalysis that necessitates treatment with antibiotics. Intracranial infection was defined as a positive cerebrospinal fluid culture requiring treatment with antibiotics. Poor functional outcome was defined as modified Rankin Scale (mRS) 4-6. Re-bleeding was defined as acute worsening in neurologic status along with an increase in hemorrhage volume which was confirmed in a repeat CT or MRI scan. Delayed ischemic neurological deficits was defined as angiographic vasospasm associated with a decline in neurological status lasting >2 h and with other causes being ruled out. Infections were diagnosed by treating physicians.
Statistical Analysis
We used SPSS, version 24 (SPSS Inc) and R software version R3.3.2 (Matching and Frailty pack packages, R Foundation for Statistical Computing) for statistical analyses.
From our experience and from previous reports, age, sex, hypertension, diabetes mellitus, chronic renal failure, coronary heart disease, smoking, alcohol use, Hunt and Hess grade and Fisher grade were considered important confounders. Propensity score matching (17) was used to minimize bias from confounding variables when comparing patients with COPD and patients without COPD in the cohort study. The propensity score for each patient was calculated through the logistic regression modeling. Exact matching was performed in patients with and without COPD in a 1:5 ratio, with a caliper size of 0.2. We then compared the characteristics of patients with and without COPD using absolute standardized differences, and a difference more than 0.1 is considered meaningful.
We also adjusted potential confounding factors using logistic regression. Each variable was screened by univariable logistic regression model for each outcome. Variables with a p-value < 0.10 were entered into the multivariable logistic regression model which was created using backward elimination.
The Kaplan–Meier curve was generated for mortality. The relationships between COPD and long-term mortality were further assessed with pre-specified Cox regression models with adjustment for confounder using backward elimination.
For proportional outcomes comparing patients with COPD and patients without COPD after PSM, the paired t-test was used for continuous variables, and univariable logistic regression was used for binary variables. Two-sided P < 0.05 was considered statistically significant.
We used the E-value to assesses how large the effect from unmeasured confounding would be to negate the study results (18). E-values were computed with an online E-value calculator (https://mmathur.shinyapps.io/evalue/) (19).
Results
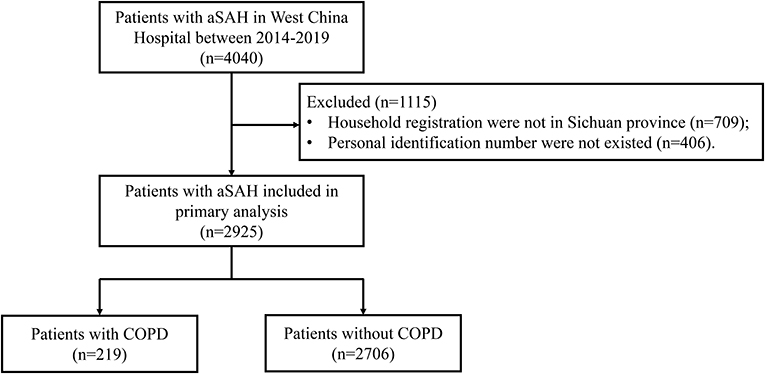
We screened 4,040 consecutive individuals with aSAH in West China hospital during the study period. After excluding 709 patients whose household registration were not in Sichuan province and 406 patients whose personal identification number were not existed in electronic medical record system, a total of 2,925 patients were included in this study (Figure 1). In patients with aSAH, 219 (7.5%) patients had COPD. Patient demographics stratified by COPD are shown in Table 1. Before matching, there were more old patients in the COPD group than in the non-COPD group. Compared with patients without COPD, patients with COPD more frequently had diabetes, and more patients with COPD are smokers. Patients with COPD have higher Hunt & Hess grade. There was a total of 166:830 matched pairs (1:5). After matching, the variables were balanced between patients with COPD and patients without COPD.
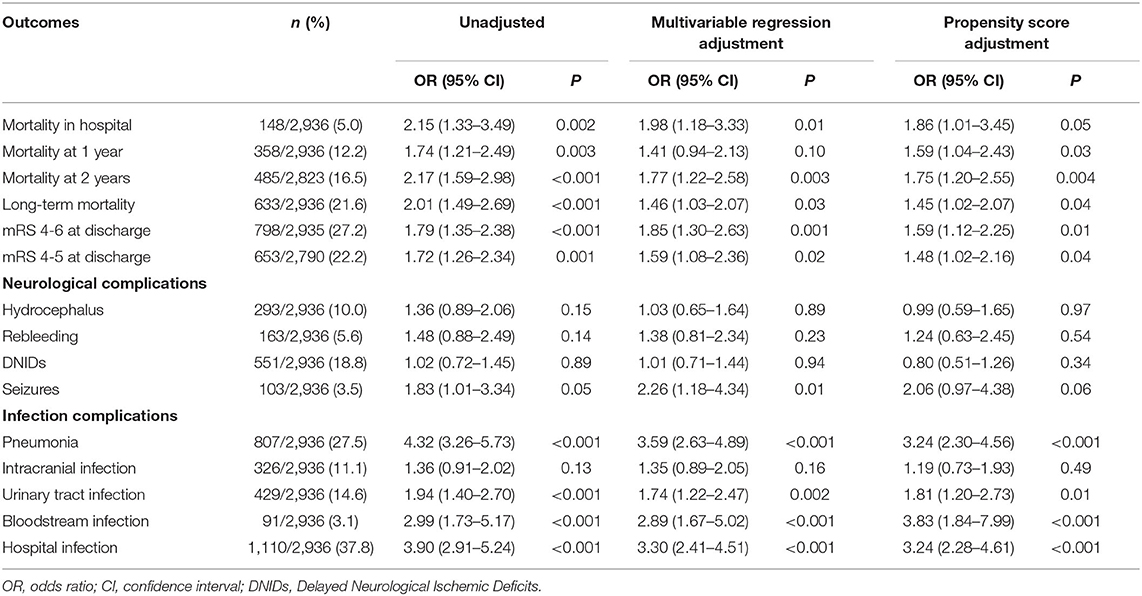
The univariable logistic regression and multivariable logistic regression for the association between COPD and long-term mortality was shown in Supplementary Table 1. In univariate analysis, COPD was associated with increased odds of long-term mortality (OR 2.01, 95% CI 1.49–2.69). After adjusted for variables of age, hypertension, diabetes, size of aneurysm, external ventricular drain, and treatment of aneurysm in multivariable logistic regression, the association between COPD and long-term mortality was not changed (OR 2.01, 95% CI 1.49–2.69). Even after propensity score matching, our findings remained robust: COPD was associated with higher mortality (OR 1.63, 95% CI 1.02–2.62; Table 2). Propensity score matching analysis also showed similar associations between COPD and other mortality, such as in-hospital, 1 and 2 years.
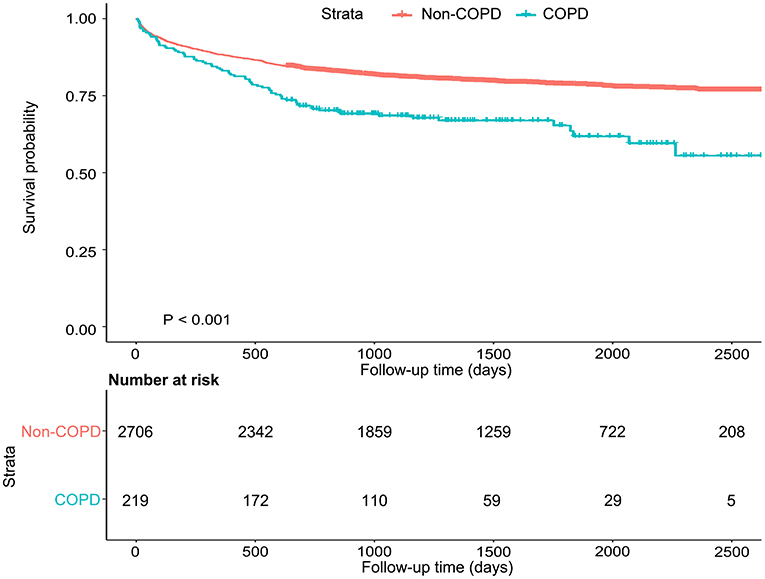
Patients were followed-up for a median of 3.8 years, and during follow-up 633 patients (21.6%) died. The impact of COPD on mortality throughout follow-up period was shown in the Kaplan–Meier plot (Figure 2). Long-term mortality was higher in patients with COPD compared to patients without COPD in the Cox regression models [adjusted hazard ratio (HR) 1.52, 95% CI 1.14–2.02].
Before and after matching, COPD was associated with an increased risk of infectious complications, including pneumonia (OR 3.24, 95% CI 2.30–4.56), urinary tract infection (OR 1.81, 95% CI 1.20–2.73), bloodstream infection (OR 3.83, 95% CI 1.84–7.99), and hospital infection (OR 3.24, 95% CI 2.28–4.61). Before matching, COPD was associated with several neurological complications [hydrocephalus (OR 1.90, 95% CI 1.43–2.52), re-bleeding (OR 1.72, 95% CI 1.24–2.39), and seizures (OR 1.78, 95% CI 1.12–2.84)]. After matching, however, COPD was associated with an increased incidence of seizures, but not hydrocephalus and rebleeding. After matching, the length of hospital stay was significantly longer in patients with COPD (P < 0.001).
The E-value for long-term mortality (HR) was 2.01 with a lower limit of 1.42, suggesting that unmeasured confounding was unlikely to explain the findings.
We further assessed interactions by other variables on COPD. Except for subgroup analyses of age, external ventricular drain, operation, and pneumonia, there is no significant effect modification of the change in COPD and long-term mortality on these variables (Figure 3).
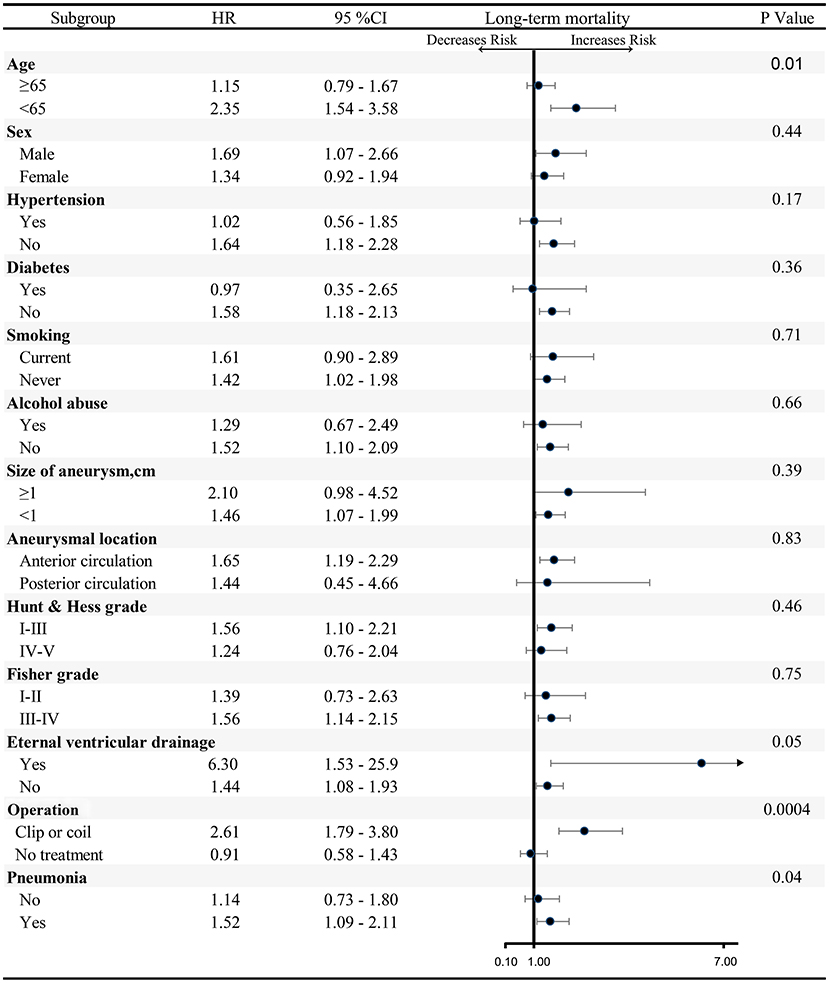
Figure 3. Subgroup analysis of association between COPD and long-term mortality. EVD, External ventricular drain; COPD, chronic obstructive pulmonary disease; HR, hazard ratio.
Discussion
In this cohort study of patients with aSAH, we found that compared to patients without COPD, patients with COPD have increased odds of short-term and long-term death and poor functional outcome at discharge. Moreover, COPD is associated with an increased incidence of seizures and infectious complications, especially pneumonia, which may contribute to the increased mortality observed in aSAH patients with COPD.
Mechanisms
Several mechanisms may explain the association between COPD and poor outcomes. First, COPD causes spillover of multiple pro-inflammatory markers into the circulation, leading to chronic low-grade systemic inflammation, ultimately resulting in unstable plaque formation and prothrombotic events (20). Second, COPD, especially during exacerbation, are hypoxemic and hypercapnic at baseline which may increase their susceptibility to brain injury. The intraneural hypoxemia can occur in ~40–50% of patients with mild COPD (21). Third, COPD have associated comorbid conditions after stroke, such as seizure (22). Fourth, COPD are commonly treated with corticosteroids, and hospitalized patients on corticosteroids have a heightened risk of nosocomial infection.
Mortality
For ischemic stroke patients, the association between COPD and the increased in-hospital mortality have been demonstrated both before (OR: 1.30, 95% CI: 1.26–1.35) and after adjusting confounders (OR: 1.08, 95% CI: 1.03–1.13) (10). Recently, the study by de Miguel-Díez et al. further confirmed this conclusion (23). However, for patients with aSAH, only one study related to this topic assessed the association between mortality and COPD in stroke patients (10). COPD was associated with increased odds of in-hospital mortality (OR 1.29, 95% CI 1.16–1.42) in univariate analysis; however, the association was not significant after adjusting confounders (adjusted OR 0.98, 95% CI 0.85–1.13) (10). The previous study was limited by short-term follow-up and the epidemiologic study design that was unadjusted for important confounders (e.g., hemorrhage severity), which led to the uncertainty of their conclusions.
Functional Outcome
This study found an association of COPD with poor functional outcomes in patients with aSAH. While such an association has not been previously assessed in patients with aSAH, a study found that COPD increased the incidence of discharge to nursing homes and rehabilitation facilities after surgery (24), and another study found that the discharge destination is a surrogate for mRS functional outcome in stroke survivors (25). More research is needed to confirm the association of COPD with poor functional outcomes in patients with aSAH.
Infection Complications
In this study, COPD was associated with an increased frequency of a variety of infection complications. In a cohort study by Lee et al., COPD is an independent risk factor for pneumonia and septic shock after total shoulder arthroplasty (26). Yakubek et al. published a study found that in patients undergoing total hip arthroplasty, patients with COPD are more likely to experience pneumonia and deep surgical site infection (24).
Two large randomized clinical trials conducted in patients hospitalized for stroke found that prophylactic antibiotics did not reduce the incidence of pneumonia (12, 13). A possible explanation for the lack of benefit is that the included patients have a general risk for pneumonia but not high risk, with 7–16% patients developing pneumonia in the control group. In the present study, half of the patients with COPD have pneumonia. The use of prophylactic antibiotics in patients with COPD may reduce the risk of progression to clinically overt pneumonia better than in general patients.
Strengths and Limitations
One of the major strengths of our study is the high-quality, standardized, single-institution database, the large sample size, and the use of PSM to adjust for confounders. We determined all-cause mortality based on the household registration in systems, which is accurate and complete, without lost to follow-up.
However, the limitations of this study must also be considered. First, based on the retrospective study, the interpretation of the specific causal relationship for COPD on mortality was is limited. Secondly, pulmonary function testing was not recorded in our database. We cannot assess the association between severity of COPD and outcomes, limiting the strength of our conclusions. Moreover, the results of this study are contingent on the accuracy and reliability of COPD status data, which were based on patient self-report and family members of incapacitated patients. It is possible that some patients in the control group also had COPD, leading to reporting and recall biases; however, these biases may serve to increase the confidence in our conclusion.
Conclusions
In aSAH patients, COPD was associated with a significant increase in short-term and long-term mortality. COPD increased the risk of infectious complications, especially pneumonia. Since these complications can potentially be prevented by antibiotics drugs, our findings are of clinical relevance and can open up new lines of inquiry. Certainly, future RCTs are needed to explore whether the use of prophylactic antibiotic therapy could improve the outcomes among these patients.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of West China Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
FF and WL: study concept and design. YZ, LY, and WY: acquisition, analysis, or interpretation of data. YZ and WY: statistical analysis. YZ and LY: drafting of the manuscript. All authors: critical revision of the manuscript for important intellectual content.
Funding
This research was funded by National Natural Science Foundation of China (grant number 81871890 and 91859203), National Key R&D Program of China (2018YFA0108604), the project of Health Commission of Sichuan province (19PJ003), the project of Sichuan Science and Technology Bureau (2020YFS0490), the 1.3.5 project for disciplines of Excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (21HXFH046), and Clinical Incubation Program of West China Hospital, SCU (2018HXFU008). The funders of the study had no role in study design, data analysis, data interpretation, or writing of the report.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.723115/full#supplementary-material
References
1. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2095–128. doi: 10.1016/S0140-6736(12)61728-0
2. Macdonald RL, Schweizer TA. Spontaneous subarachnoid haemorrhage. Lancet. (2017) 389:655–66. doi: 10.1016/S0140-6736(16)30668-7
3. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. (2012) 43:1711–37. doi: 10.1161/STR.0b013e3182587839
4. Corlateanu A, Covantev S, Mathioudakis AG, Botnaru V, Siafakas N. Prevalence and burden of comorbidities in chronic obstructive pulmonary disease. Respir Investig. (2016) 54:387–96. doi: 10.1016/j.resinv.2016.07.001
5. Efird JT, Griffin W, O'Neal WT, Davies SW, Shiue KY, Grzybowski M, et al. Long-term survival after cardiac surgery in patients with chronic obstructive pulmonary disease. Am J Crit Care. (2016) 25:266–76. doi: 10.4037/ajcc2016119
6. Leavitt BJ, Ross CS, Spence B, Surgenor SD, Olmstead EM, Clough RA, et al. Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation. (2006) 114 (1 Suppl.):I430–4. doi: 10.1161/CIRCULATIONAHA.105.000943
7. Distelmaier K, Niessner A, Haider D, Lang IM, Heinz G, Maurer G, et al. Long-term mortality in patients with chronic obstructive pulmonary disease following extracorporeal membrane oxygenation for cardiac assist after cardiovascular surgery. Intens Care Med. (2013) 39:1444–51. doi: 10.1007/s00134-013-2931-y
8. Shin B, Lee H, Kang D, Jeong BH, Kang HK, Chon HR, et al. Airflow limitation severity and post-operative pulmonary complications following extra-pulmonary surgery in COPD patients. Respirology. (2017) 22:935–41. doi: 10.1111/resp.12988
9. Corlateanu A, Covantev S, Mathioudakis AG, Botnaru V, Cazzola M, Siafakas N. Chronic obstructive pulmonary disease and stroke. COPD. (2018) 15:405–13. doi: 10.1080/15412555.2018.1464551
10. Lekoubou A, Ovbiagele B. Prevalance and influence of chronic obstructive pulmonary disease on stroke outcomes in hospitalized stroke patients. eNeurologicalSci. (2017) 6:21–4.11. doi: 10.1016/j.ensci.2016.11.007
11. Herath SC, Normansell R, Maisey S, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. (2018) 10:Cd009764. doi: 10.1002/14651858.CD009764.pub3
12. Kalra L, Irshad S, Hodsoll J, Simpson M, Gulliford M, Smithard D, et al. Prophylactic antibiotics after acute stroke for reducing pneumonia in patients with dysphagia (STROKE-INF): a prospective, cluster-randomised, open-label, masked endpoint, controlled clinical trial. Lancet. (2015) 386:1835–44. doi: 10.1016/S0140-6736(15)00126-9
13. Westendorp WF, Vermeij JD, Zock E, Hooijenga IJ, Kruyt ND, Bosboom HJ, et al. The preventive antibiotics in stroke study (PASS): a pragmatic randomised open-label masked endpoint clinical trial. Lancet. (2015) 385:1519–26. doi: 10.1016/S0140-6736(14)62456-9
14. Stevens RD, Nyquist PA. The systemic implications of aneurysmal subarachnoid hemorrhage. J Neurol Sci. (2007) 261:143–56. doi: 10.1016/j.jns.2007.04.047
15. Restrepo MI, Sibila O, Anzueto A. Pneumonia in patients with chronic obstructive pulmonary disease. Tuberc Respir Dis. (2018) 81:187–97. doi: 10.4046/trd.2018.0030
16. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease study. Lancet. (1997) 349:1498–504. doi: 10.1016/S0140-6736(96)07492-2
17. Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. (2008) 27:2037–49. doi: 10.1002/sim.3150
18. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. (2017) 167:268–74. doi: 10.7326/M16-2607
19. Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Web site and r package for computing E-values. Epidemiology. (2018) 29:e45–7. doi: 10.1097/EDE.0000000000000864
20. Maclay JD, MacNee W. Cardiovascular disease in COPD: mechanisms. Chest. (2013) 143:798–807. doi: 10.1378/chest.12-0938
21. Stewart AG, Waterhouse JC, Howard P. Cardiovascular autonomic nerve function in patients with hypoxaemic chronic obstructive pulmonary disease. Eur Respir J. (1991) 4:1207–14.
22. De Reuck J, Proot P, Van Maele G. Chronic obstructive pulmonary disease as a risk factor for stroke-related seizures. Eur J Neurol. (2007) 14:989–92. doi: 10.1111/j.1468-1331.2007.01829.x
23. de Miguel-Díez J, López-de-Andrés A, Jiménez-García R, Hernández-Barrera V, Jiménez-Trujillo I, Ji Z, et al. Sex differences in the incidence and outcomes of COPD Patients hospitalized with ischemic stroke in spain: a population-based observational study. Int J Chron Obstruct Pulmon Dis. (2021) 16:1851–62. doi: 10.2147/COPD.S311826
24. Yakubek GA, Curtis GL, Khlopas A, Faour M, Klika AK, Mont MA, et al. Chronic obstructive pulmonary disease is associated with short-term complications following total knee arthroplasty. J Arthroplasty. (2018) 33:2623–6. doi: 10.1016/j.arth.2018.03.011
25. Qureshi AI, Chaudhry SA, Sapkota BL, Rodriguez GJ, Suri MF. Discharge destination as a surrogate for modified Rankin scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil. (2012) 93:1408–13.e1. doi: 10.1016/j.apmr.2012.02.032
26. Lee R, Lee D, Mamidi IS, Probasco WV, Heyer JH, Pandarinath R. Patients with chronic obstructive pulmonary disease are at higher risk for pneumonia, septic shock, and blood transfusions after total shoulder arthroplasty. Clin Orthop Relat Res. (2019) 477:416–23. doi: 10.1097/CORR.0000000000000531
Keywords: intracranial aneurysm, chronic obstructive pulmonary disease, subarachnoid hemorrhage, risk factor, prognosis
Citation: Yang L, Zhang Y, Yao W, Fang F and Li W (2021) Impact of Chronic Obstructive Pulmonary Disease on Infectious Complications and Mortality in Patients With Aneurysmal Subarachnoid Hemorrhage. Front. Neurol. 12:723115. doi: 10.3389/fneur.2021.723115
Received: 10 June 2021; Accepted: 12 October 2021;
Published: 12 November 2021.
Edited by:
Roland Faigle, Johns Hopkins University, United StatesReviewed by:
Jörn Grensemann, University Medical Center Hamburg-Eppendorf, GermanyMichelle Lin, Mayo Clinic Florida, United States
Copyright © 2021 Yang, Zhang, Yao, Fang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Fang, ZmFuZ2ZhbmcwMUBzY3UuZWR1LmNu; Weimin Li, d2VpbWluMDAzQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share corresponding authorship
 Lan Yang
Lan Yang Yu Zhang
Yu Zhang Wei Yao
Wei Yao Fang Fang2*‡
Fang Fang2*‡ Weimin Li
Weimin Li