- 1Department of Pediatrics and Children's Learning Institute, McGovern Medical School, University of Texas Health Science Center at Houston, Houston, TX, United States
- 2Department of Pediatrics, Division of Critical Care, School of Medicine, University of Utah, Salt Lake City, UT, United States
- 3Department of Pediatric Surgery, McGovern Medical School, University of Texas Health Science Center at Houston, Houston, TX, United States
Objective: To model pre-injury child and family factors associated with the trajectory of internalizing and externalizing behavior problems across the first 3 years in children with pediatric traumatic brain injury (TBI) relative to children with orthopedic injuries (OI). Parent-reported emotional symptoms and conduct problems were expected to have unique and shared predictors. We hypothesized that TBI, female sex, greater pre-injury executive dysfunction, adjustment problems, lower income, and family dysfunction would be associated with less favorable outcomes.
Methods: In a prospective longitudinal cohort study, we examined the level of behavior problems at 12 months after injury and rate of change from pre-injury to 12 months and from 12 to 36 months in children ages 4–15 years with mild to severe TBI relative to children with OI. A structural equation model framework incorporated injury characteristics, child demographic variables, as well as pre-injury child reserve and family attributes. Internalizing and externalizing behavior problems were indexed using the parent-rated Emotional Symptoms and Conduct Problems scales from the Strengths and Difficulties questionnaire.
Results: The analysis cohort of 534 children [64% boys, M (SD) 8.8 (4.3) years of age] included 395 with mild to severe TBI and 139 with OI. Behavior ratings were higher after TBI than OI but did not differ by TBI severity. TBI, higher pre-injury executive dysfunction, and lower income predicted the level and trajectory of both Emotional Symptoms and Conduct Problems at 12 months. Female sex and poorer family functioning were vulnerability factors associated with greater increase and change in Emotional Symptoms by 12 months after injury; unique predictors of Conduct Problems included younger age and prior emotional/behavioral problems. Across the long-term follow-up from 12 to 36 months, Emotional Symptoms increased significantly and Conduct Problems stabilized. TBI was not a significant predictor of change during the chronic stage of recovery.
Conclusions: After TBI, Emotional Symptoms and Conduct Problem scores were elevated, had different trajectories of change, increased or stayed elevated from 12 to 36 months after TBI, and did not return to pre-injury levels across the 3 year follow-up. These findings highlight the importance of addressing behavioral problems after TBI across an extended time frame.
Introduction
Exposure to physical trauma during childhood is associated with increases in emotional symptoms and behavior problems in a substantial number of children (1, 2). Among children with physical trauma due to traumatic brain injury (TBI), up to 50% of children are at risk for developing behavior problems and disorders (3). TBI has been linked to both an increase in behavior problems (4–6), and an onset or exacerbation of a variety of psychiatric disorders, including attention deficit/hyperactivity disorder, major depression, post-traumatic stress disorder, and anxiety (7–10). The behavioral and psychiatric problems following TBI are a major source of disability for survivors and a primary cause of family burden. As over 800,000 children seek care for TBI annually, including over 23,000 hospitalizations and 2,500 deaths, disability after TBI is an important public health problem (11).
Post-traumatic emotional symptoms and behavior problems are often assessed dimensionally using rating scales. These scales typically distinguish between internalizing problems such as anxiety and depression that are directed inward, and externalizing problems such as oppositionality or conduct problems directed toward the external environment. In a number of studies, TBI severity is associated with post-traumatic behavioral changes. Ratings completed by parents and/or children indicated greater internalizing and/or externalizing symptoms after moderate to severe TBI than in children with orthopedic injuries (OI) (5, 12) or healthy children (13). Some studies identified greater problems following severe TBI than complicated/mild, moderate, and/or mild TBI for conduct, affective, anxiety, and ADHD problems (5, 6, 12), externalizing problems (14–18), and total behavior problems (19, 20). Conversely, others did not report differences between TBI severity groups in terms of internalizing and/or externalizing problems (21–23). When assessed during adolescence or adulthood, children with a range of TBI severity show elevated risk for internalizing and/or externalizing problems (24–27).
Despite the high incidence and persistence of emotional and behavioral problems following TBI, little is known about the non-injury factors that place children at elevated risk for chronic psychological health concerns. Due to the dearth of methodologically rigorous longitudinal studies, it is unclear whether children's emotional and behavioral profiles stabilize or whether the presence of certain factors contributes to positive outcomes or to a negative cascade and worsening of psychological health over time. Non-injury factors that may place the child at higher risk for poor post-injury functioning include the quality of children's psychological health prior to the injury. Poorer pre-injury adjustment is a risk factor for poorer post-injury adjustment across the spectrum of TBI severity (5, 28). Pre-injury family and environmental factors also significantly influence child behavioral outcomes, such that lower income, lower social and community connectivity, greater family dysfunction, and parental psychiatric symptoms act as vulnerability factors contributing to worse post-injury problems (5, 19, 29–32).
Other child characteristics prior to TBI, such as adequacy of executive functions (EF) supporting cognitive and behavioral self-regulation, may play a key role in shaping outcomes. EF regulate focusing and sustaining attention, resisting distraction, managing frustration, controlling emotional responses, monitoring behavior, considering consequences of behavior, reflecting on past experiences, and planning for the future (33, 34). Although it is well-known that TBI disrupts EF (35–39), there is very limited understanding of how the quality of EF prior to injury shapes behavioral outcomes.
Understanding of multiple factors influencing the long-term trajectory of behavior problems after TBI requires incorporating an assessment of pre-injury behavior and injury comparison groups. Controlling for pre-injury adjustment is essential to discriminate lifetime problems from injury-related changes. It is important to dissociate pre-injury tendencies, such as impulsivity, that may pre-dispose children to injury, from post-injury changes. In addition, using an injured comparison group allows identification of the effects of TBI above and beyond changes that may occur due to the known stresses simply from being injured and receiving medical intervention. The few longitudinal cohort studies controlling for pre-injury behavior and incorporating an orthopedic injury comparison group have identified increases in parent-reported internalizing and externalizing problems across the first year across the spectrum of TBI severity (5, 12, 40).
In this prospective, longitudinal cohort study, we examined parent-reported behavioral outcomes in the largest sample to date of children ages 4–15 with mild to severe TBI relative to an OI comparison group. We used structural equation and growth modeling to examine pre-injury child and family factors shaping long-term internalizing and externalizing problems across the first 3 years after injury. We hypothesized that behavior problems would increase after TBI relative to OI. The level and change over time from pre-injury to 36 months after injury would be related to injury type (TBI or OI), pre-injury child functioning, and family factors. Vulnerability factors including child sex, greater pre-injury EF and adjustment problems, lower income, and family dysfunction were expected to increase the level of emotional symptoms and behavior problems and flatten the trajectory of recovery. Internalizing and externalizing problems were expected to have both shared and unique predictors.
Materials and Methods
Participants
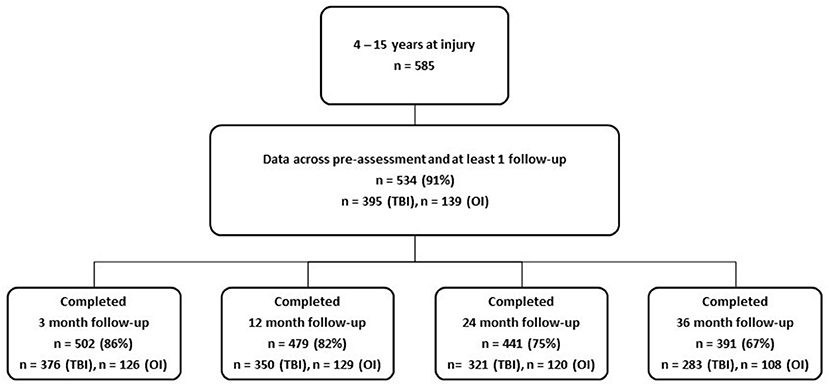
Children ages 0–15 years (n = 834) with TBI or OI were recruited for a longitudinal, prospective cohort study from two level 1 pediatric trauma centers, University of Texas Health Science Center at Houston (UTHealth)/Children's Memorial Hermann Hospital and Primary Children's Hospital (PCH) in Salt Lake City, UT. Parents and children provided written permission and assent per IRB guidelines at UTHealth and University of Utah. Children were recruited in the ED or hospital from January, 2013 through September, 2015 sequentially to fill strata of injury type, severity and age group. Exclusionary criteria included the presence of severe developmental delay or psychiatric diagnoses requiring a closed classroom setting. Children 4–15 years old at injury (n = 585) were eligible for all measures. Of those, 534 (91%) contributed data across pre-assessment and at least 1 follow-up (see procedures for more details on follow-up data collections). Figure 1 shows the number of TBI and OI participants contributing data at the 3, 12, 24, and 36 month follow-ups. Approximately 67% were retained across all 3 years.
Traumatic Brain Injury Group
TBI severity was measured using the lowest Glasgow Coma Scale (GCS) score in the ED assessing motor, eye, and verbal responses (41). TBI was categorized by severity: mTBI was defined as a GCS ≥ 13 in the ED with a GCS of 15 at discharge or after 24 h if hospitalized, and one or more focal signs including a period of transient confusion, loss of consciousness for 30 min or less, and/or transient neurological abnormalities (11). Mild TBI was sub-classified as complicated mild based on CT evidence of an intracranial hemorrhage (42). Moderate and severe TBI were categorized as a GCS of 9–12 and 3–8, respectively. Intubated and sedated children were scored 3T to indicate that the verbal response could not be assessed due to intubation.
Orthopedic Injury Group
The OI comparison group included children with an upper or lower extremity long bone fracture without TBI to isolate the effect of TBI from more general injury effects and to account for pre-injury child characteristics, such as impulsivity, that may pre-dispose children to injury. Injury severity was measured with the trauma registrar assigned Abbreviated Injury Scale (AIS) (43).
Study Design
Parents completed baseline surveys of family demographics, family functioning, social support, and child outcome measures a median of 8 days (IQR: 3, 15) after injury in English or Spanish to represent pre-injury values. Follow-up assessments were collected at 3, 12, 24 and 36 months on-line or by telephone. Clinical and injury variables were abstracted from medical records by study coordinators using standardized forms.
Measures
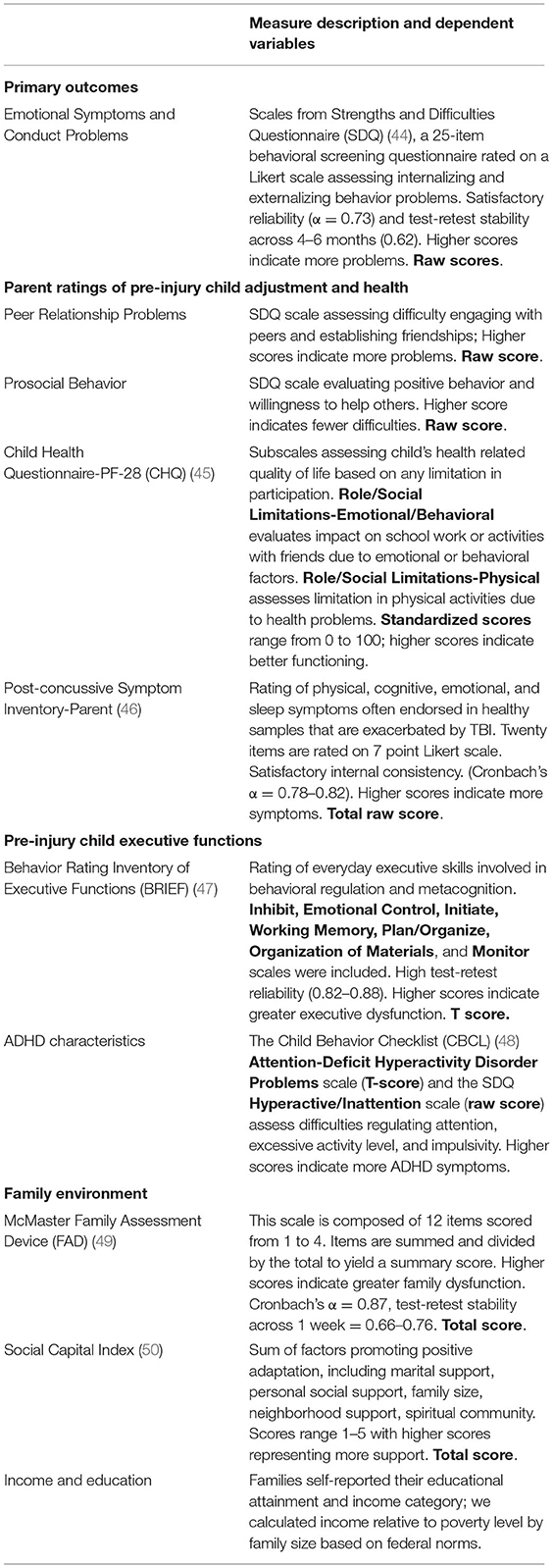
All measures are presented in Table 1. Longitudinal trajectories of internalizing and externalizing behavior problems were evaluated using the Strengths and Difficulties Questionnaire (SDQ) Emotional Symptoms and Conduct Problems scales, respectively (44). Parent-reported measures of pre-injury child psychological health and EFs, as well as the family environment, were selected to highlight child behavior and family characteristics potentially related to subacute and chronic behavior problems. All measures are gold standard common data elements recommended for pediatric TBI by the National Institute of Neurologic Disorder and Stroke (51). Child and family variables include psychosocial support factors that are strongly related to positive child outcomes in children facing medical and environmental challenges (52).
Data Reduction
In order to create a latent EF factor, confirmatory factor analysis was used to combine EF data including BRIEF variables, SDQ Hyperactivity and CBCL ADHD Problems at the pre-injury time point as is commonly done (53, 54). We examined fit via the Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA). CFIs >0.90, and RMSEAs <0.08 were used to evaluate whether a model demonstrated “acceptable fit” (55). Initially the model did not fit well (CFI = 0.80, RMSEA = 17). However, modification indices indicated some measurement variance associated with the BRIEF. We allowed residual correlations among subscales for the BRIEF which improved fit to acceptable levels (RMSEA = 0.07, CFI = 0.99). Given field results suggesting that a two factor (hot/affective regulation and cool/decontextualized) may fit better, we also fit a 2 factor model with residual correlations for the BRIEF. We defined hot regulation via the BRIEF emotional control and inhibit scales as well as the ADHD subscale of the CBCL. All other scales defined the cool/de-contextual factor. The two factor did not fit as well (RMSEA = 0.13, CFI = 0.92); thus, we retained the one factor.
Statistical Analyses
First, we wanted to identify any significant differences between the OI and the different TBI groups. To do this, we performed within time point ANOVAs with planned group comparisons at all time points. The TBI and OI groups were similar at the pre-injury time point, but there were consistent, significant differences between the TBI group and OI group at most subsequent time points. When examining differences among the TBI severity groups, we first combined complicated mild and moderate TBI into one group due to the small number of children with moderate TBI (42). However, the ANOVAs with planned comparisons indicated that for both Emotional Symptoms and Conduct Problems, there were no significant differences between the TBI groups across all time points. Therefore, TBI was collapsed into a single group for the remaining analyses.
Next, we evaluated how best to model change in SDQ Emotional Symptoms and Conduct Problems between pre-injury and 36-months post. Five growth models were fit separately to the Emotional Symptoms and Conduct Problem data: linear, quadratic, and cubic growth as well as two spline models: a linear-linear spline model and a quadratic-linear spline model with the knot point set at 12-month post. This approach allowed us to (i) accurately model expected slope changes related to disruption and recovery in child functioning around an injury, and (ii) build a larger model focused on child and family level predictors that affect the injury related change process. Fit statistics including the Akaike Information Criterion (AIC), the adjusted Bayesian Information Criterion (aBIC), RMSEA, and CFI, were used to evaluate model fit (55). For the cubic and quad-linear spline models, the variance for the cubic term, and the quadratic term, respectively, were set to zero to ensure enough degrees of freedom to estimate the model. Note even with variance (random effect) fixed, the mean for each of these terms (fixed effect) is still estimated and mean change across predictors can also be estimated. Spline models were used because they are capable of modeling different phases of change by including more than one slope factor. For both spline models, the knot point was set to 12-months, thus the spline models included separate parameters for the slope to capture the change from pre-injury to 12 months post-injury and then from 12 months post to 36-month post-injury. This is a theoretically significant point as substantial recovery occurs by 12 months after TBI (35) and our goal was to evaluate factors influencing the recovery trajectory after 12 months. Models were performed in Mplus 8.2 using maximum likelihood estimation (56) with an ML estimator for all analyses to account for missing data.
Injury Predictor
After building the growth curve models, we then included injury type as a predictor of the level of both outcomes at 12-months post-injury and of the change parameters. Our first hypothesis is that internalizing and externalizing problems would increase more after TBI relative to OI. Including injury first allowed us to evaluate and describe the main effect of injury on both the increase/decrease in change and the rate of change, as well as differences in levels of the behavior.
Child and Family Predictors
After the inclusion of injury type, we added demographic, pre-injury child characteristics (latent executive factor, parent ratings of adjustment and health) and family environment predictors to the model. These were added simultaneously as we did not have strong hypotheses regarding order of effects. Simultaneous inclusion allowed us to look at each predictor while controlling for the influence of all other predictors.
Results
Participants
The cohort consists of 395 children with TBI: 146 mild, 132 complicated mild, 28 moderate, and 89 with severe TBI. There are 139 children with OI. As noted above, there were no demographic or pre-injury differences between the TBI severity groups. Additionally, there were no differences among the TBI severity groups on the primary SDQ outcomes at any time point. Consequently, they were combined into an overall TBI group. Comparison of baseline demographic variables, child characteristics, and family environment indicated no significant differences across TBI and OI groups (Table 2).
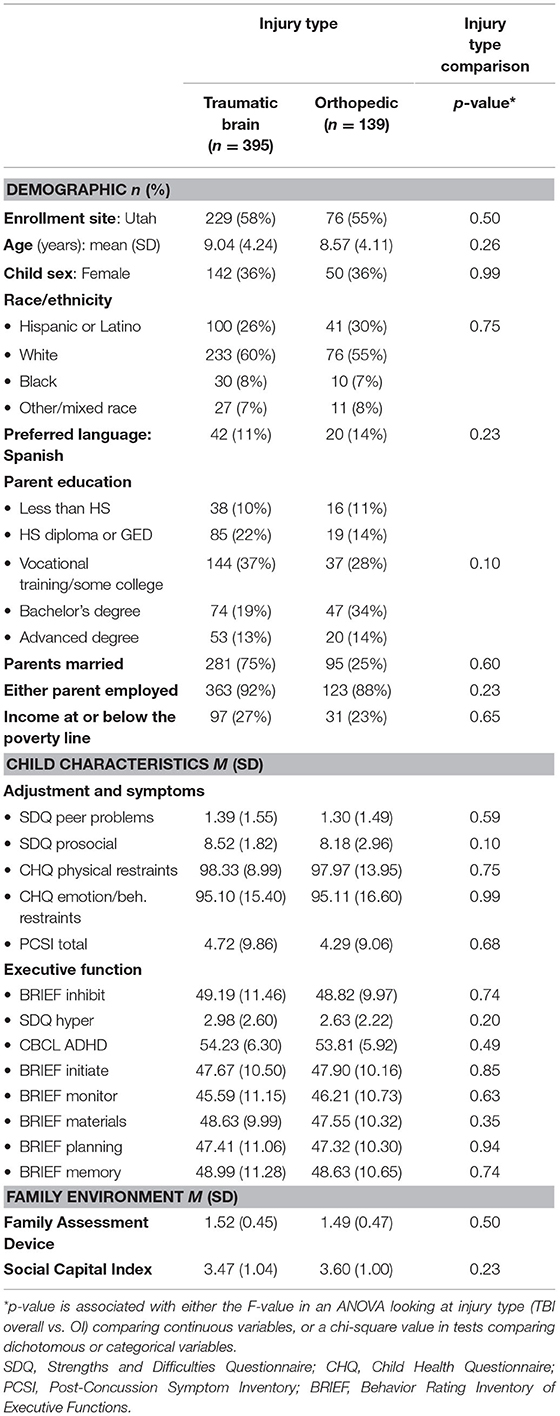
Table 2. Comparison of baseline demographic variables, child characteristics, and family environment by injury type.
Raw and Fitted Change in Outcome Scores
Descriptive statistics and ANOVA group comparisons of SDQ Emotional Symptoms and Conduct Problem outcomes for TBI and OI groups at each time point are in Table 3. Correlations between these variables are presented in Supplementary Table 1. Ratings across all time points met assumptions of normality (57, 58), ensuring parametric analyses such as ANOVA and subsequent SEM modeling were appropriate. Pre-injury ratings did not differ significantly by group. The TBI group had higher scores than the OI group on both measures at the 3, 24, and 36 month follow-ups. Groups did not differ at the 12 month interval. Figures 2A,B shows the longitudinal trajectory of the raw and fitted scores by group.
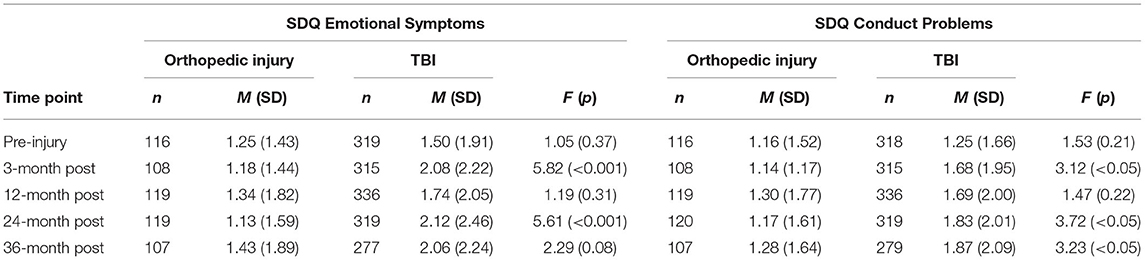
Table 3. Descriptive statistics and comparisons of Strengths and Difficulties subtest scores by injury type and time point.
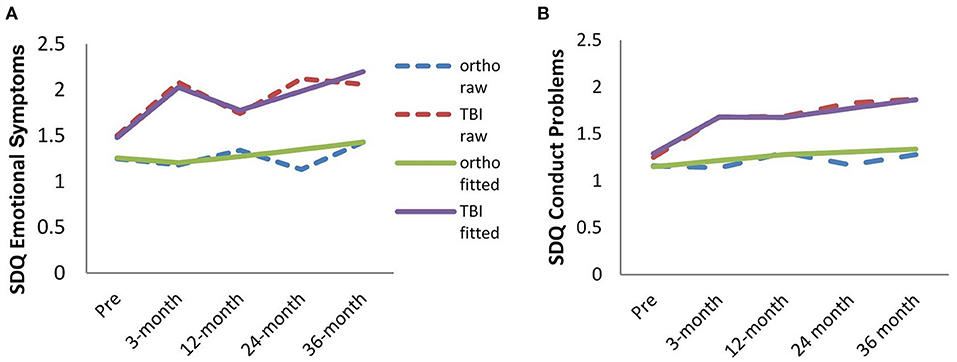
Figure 2. Raw and fitted change in Emotional Symptoms (A) and Conduct Problems (B) scores from pre-injury through 36-months post-injury for TBI and OI groups.
Growth Curve Models
Fitted data from the 5 growth models evaluated were examined to inform the best model representing the raw data at each time point. Latent growth fit statistics for each model are in Supplementary Table 2. The quadratic-linear spline model best fit both outcome variables, indicating quadratic change between pre-injury and 12-month post, and linear change between 12- and 36-month post, with the level estimates at the knot point (12-months post). The addition of the quadratic term (from pre-injury to 12-months pots) for Emotional Symptoms describes a period of rapid increase followed by rapid decrease. For Conduct Problems, the quadratic captures the rate change with a rapid increase that levels off. The linear term fit well for both outcomes from 12- to 36-months.
Emotional Symptoms
Injury Type
The level and change parameters for injury type and all pre-injury predictors of Emotional Symptoms are presented in Table 4 and Figure 3. Injury type was a significant predictor of the level at 12 months post-injury (p < 0.05) such that children with TBI reported 0.11 of a standard deviation increase in Emotional Symptoms (approximately a half a point increase on the SDQ compared to orthopedic peers). In contrast, children with an OI demonstrated few changes in Emotional Symptoms at the 12 month time point. Injury type was important for both the pre-injury to 12-months linear and quadratic change parameters (linear β = 0.34, p < 0.05, quadratic β = 0.49, p < 0.01) indicating that Emotional Symptoms in children with TBI demonstrated a rapid increase after injury and then declined prior to the 12-month time point, whereas OI group demonstrated little to no changes in Emotional Symptoms.
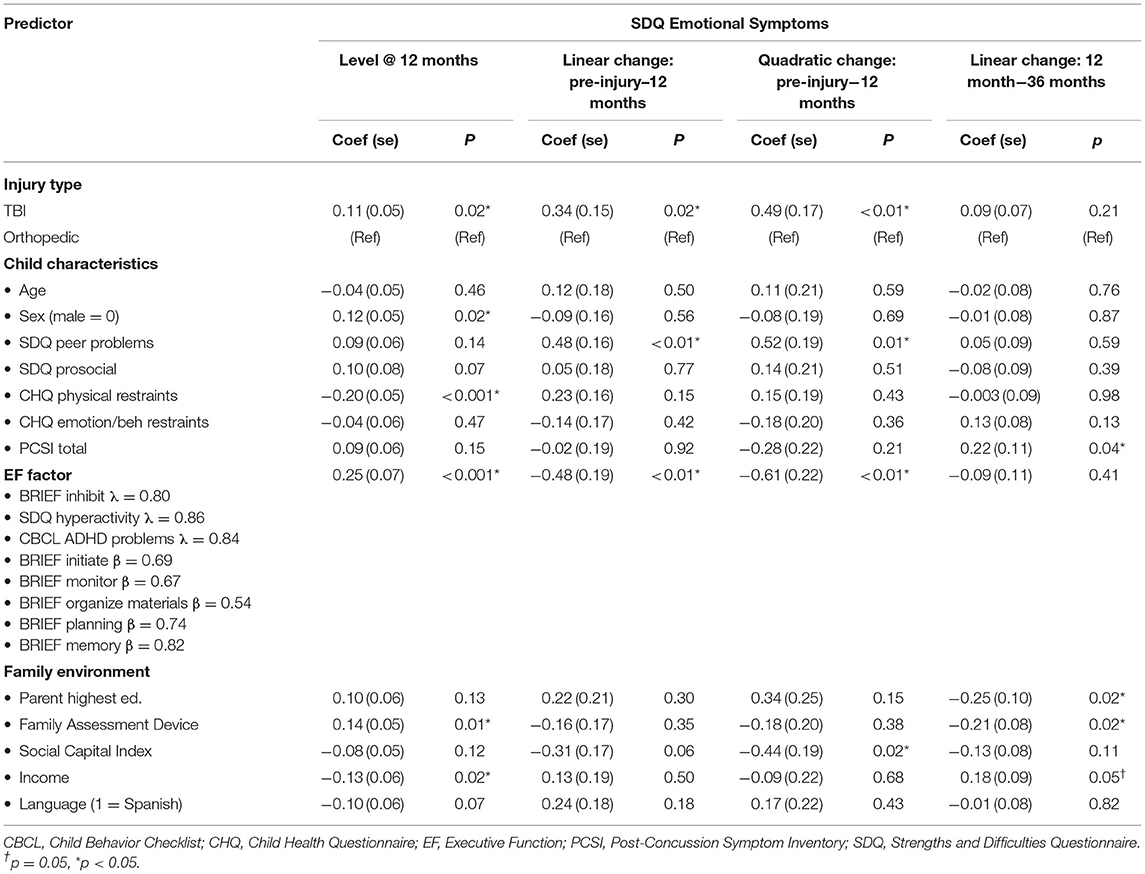
Table 4. Summary of injury type and pre-injury child and family predictors of change in Emotional Symptoms.
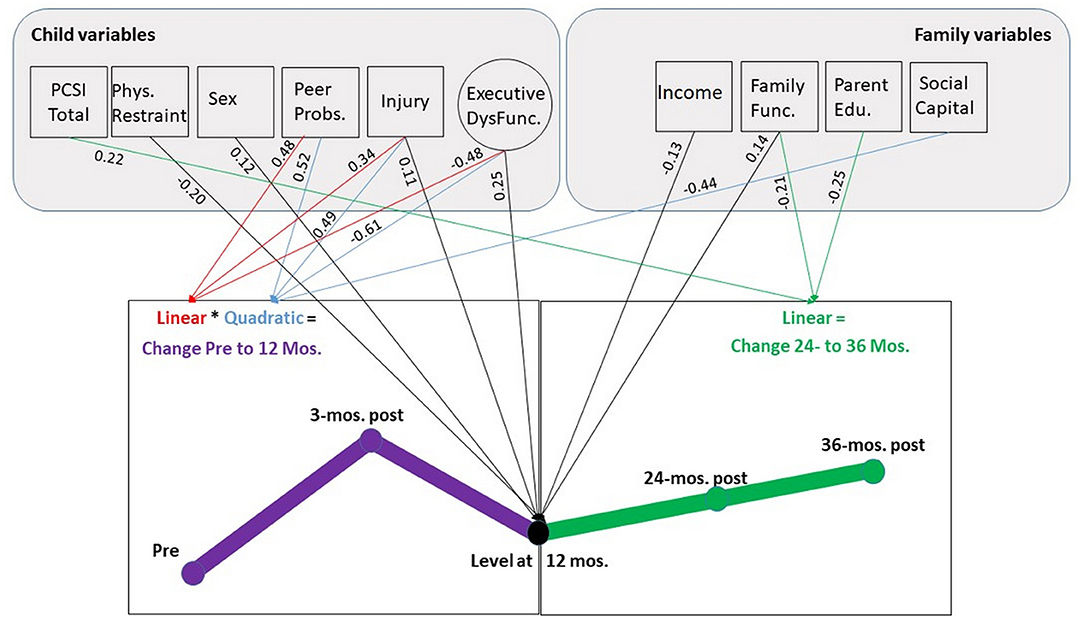
Figure 3. SEM model of change in Emotional Symptoms as predicted by injury type and pre-injury EFs, child and family factors. Predictor variables with no significant relationships, correlations between pre-injury variables, variances, and residual variances are suppressed. Direct relationships are denoted by arrows. Circles represent latent constructs. Boxes represent measured constructs. Coefficients are shown for measures at 12 months, linear and quadratic change. PCSI, peer problems, executive dysfunction, and family function scores indicate more problems and are expected to positively associated with emotion symptoms. Higher physical restraint and social capital scores indicate better functioning/ more social connections and are expected to negatively associate with Emotional Symptoms. Sex is coded 0 for males and 1 for females. Injury is coded 0 for the orthopedic group and 1 for the TBI group. Income is coded such that higher values indicate less poverty. Parent education is coded such that higher values indicate greater educational attainment.
The third change parameter examined linear change from 12- to 36-months post-injury. The overall change with no predictors in the model was significant β = 0.26, p < 0.05. This means that for every 1 year, there is a 0.26 standard deviation increase in Emotional Symptoms. However, injury type was not a significant predictor of this change (β = 0.09, p = 0.21). Both injury groups had linear increases, even though the change in scores for the OI group was minor. Across the extended follow-up, the TBI group did not return to pre-injury levels of Emotional Symptoms and remained elevated above OI peers.
Pre-Injury Child and Family Predictors of Change
Briefly, greater Emotional Symptoms 12-month after injury were predicted by TBI, female sex, as well as greater pre-injury executive dysfunction and physical limitations measured on the CHQ. Family burden also played a key role with higher levels of family dysfunction and lower income associated with higher levels of emotional difficulties. The linear and quadratic slope from pre-injury status to 12 months post-injury were predicted by TBI, less pre-injury executive dysfunction, and higher peer problems in conjunction with lower family social capital. The direction of the EF parameter was unexpected; higher levels of pre-injury executive dysfunction dampened the increase and rate of change in Emotional Symptoms. Higher social capital was negatively associated with the quadratic parameter, suggesting that more social support dampened the rapid rise and fall of Emotional Symptoms in the first 12-months post.
The linear slope from 12 to 36 months was not predicted by injury type or most child characteristics. The one exception was that higher total PCSI symptoms prior to injury was associated with an increase in Emotional Symptoms. For pre-injury family factors, higher levels of parent education and family dysfunction dampened the increase in Emotional Symptoms from 12 to 36 months.
Conduct Problems
Injury Type
Whether a child sustained a TBI or OI was also a significant predictor of the level of Conduct Problems at 12 months post-injury (β = 0.11, p < 0.05). Children with TBI reported 0.11 of a standard deviation increase in Conduct Problems (a little under a half a point increase compared to OI) at the 12 month time point. Type of injury was not related to the linear change parameter from pre-injury to 12-months, but it was related to the quadratic parameter (linear β = 0.23, p = 0.16, quadratic β = 0.36, p < 0.05). As can be seen in Figure 2B, this suggests a significant difference in the rate of change as Conduct Problems increase particularly between pre-injury and 3-months after TBI.
Across the long-term follow-up from 12 to 36 months, the base model with no predictors found an increase in the slope that approached significance, β = 0.21, p = 0.09. Injury type was not a significant predictor of change (β = 0.11, p = 0.48), with problems remaining elevated after TBI compared to the OI group across the follow-up. While a linear model fit best, it did not suggest upward linear change. Rather, a flatline linear constant model may best characterize the slope across both groups.
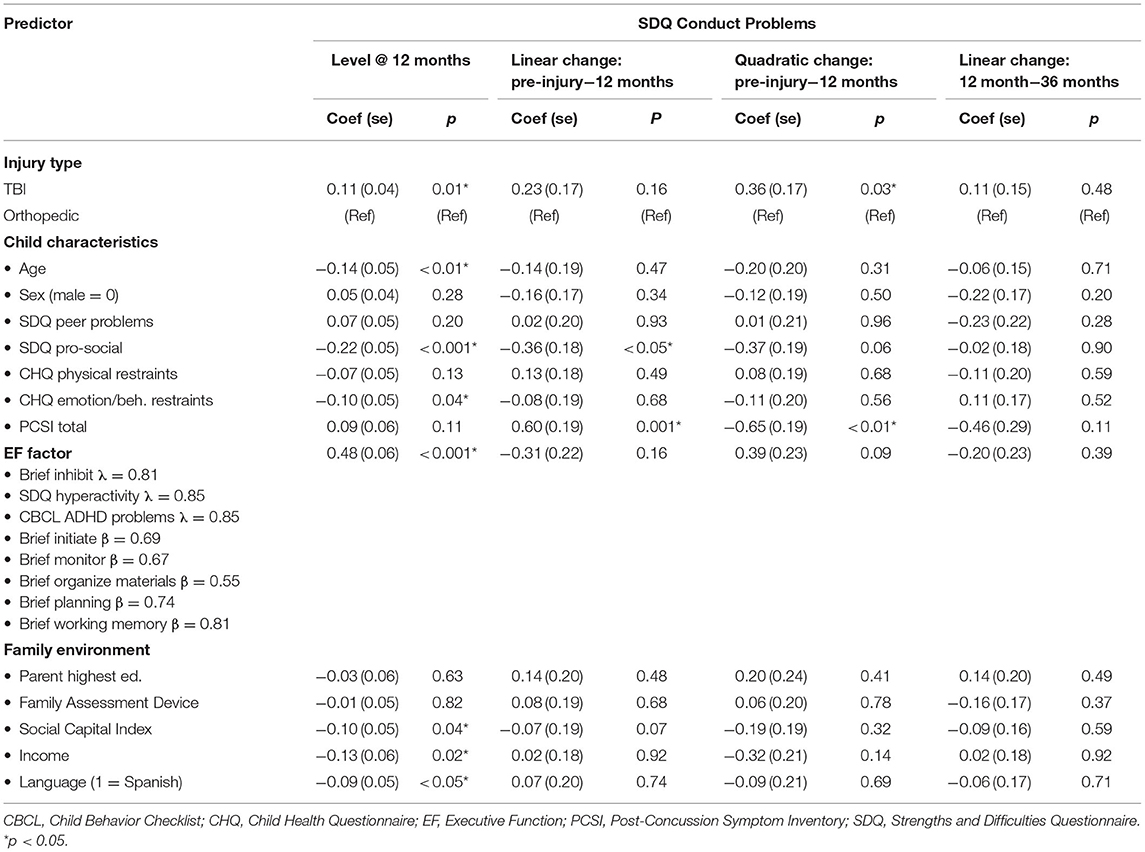
Pre-Injury Child Characteristics and Family Predictors of Change
The level and change parameters on all pre-injury predictors are presented in Table 5 and Figure 4. At 12-months post-injury, seven child and family variables predicted the level of Conduct Problems. Higher scores were predicted by TBI (β = 0.11, p < 0.01) and executive dysfunction (β = 0.48, p < 0.001). For every one factor unit increase in executive dysfunction, there was a 0.48 (or nearly half a standard deviation) increase in Conduct Problems. Other child predictors were younger age (β = −0.14, p < 0.01), more CHQ emotional/behavioral restraints, and lower SDQ prosocial behaviors. Higher scores on the CHQ emotional/behavioral restraints scale (with higher indicating better functioning) were associated with a 0.10 standard deviation reduction in 12-months post-injury Conduct Problems. Likewise lower levels of pro-social behavior were associated with a 0.22 standard deviation increase in Conduct Problems at 12-months post-injury. Among family characteristics, higher Conduct Problems were predicted by lower social capital (β = −0.10, p < 0.05), being an English language speaker (β = −0.09, p < 0.05), and lower income (β = −0.13, p < 0.05).
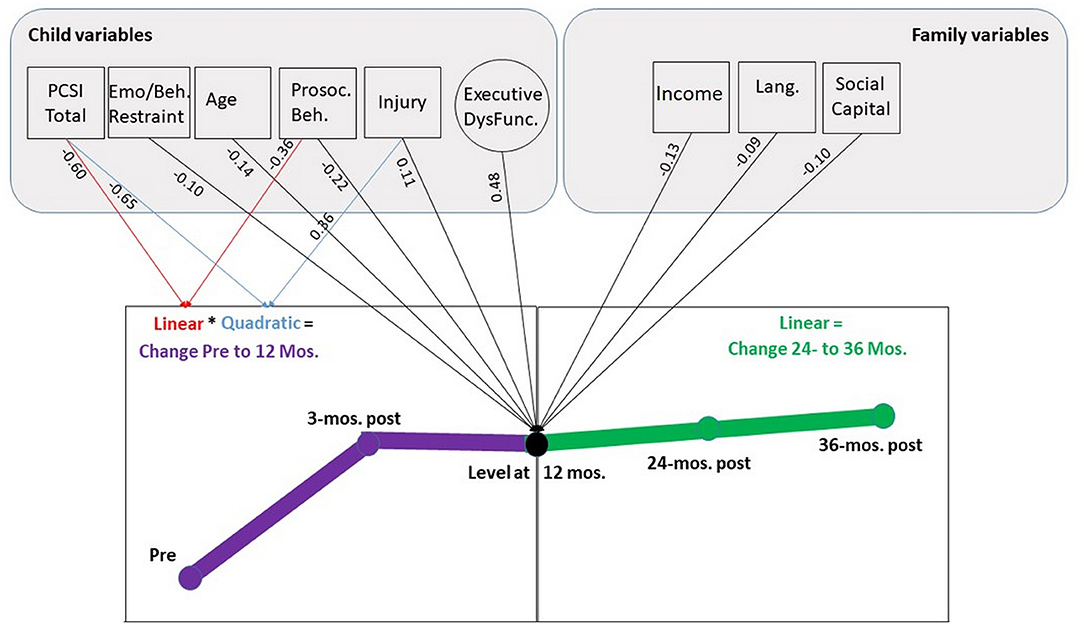
Figure 4. SEM model of change in Conduct Problems as predicted by child and family factors prior to injury. Predictor variables with no significant relationships, correlations between pre-injury variables, variances, and residual variances are suppressed. Higher PCSI and executive dysfunction scores indicate more problems and are expected to positively associated with conduct problems. Higher emotion and behavior restraints, pro-social behavior, and social capital scores indicate better functioning/more social connections and are expected to negatively associate with Conduct Problems. Injury is coded 0 for the orthopedic group and 1 for the TBI group. Income is coded such that higher values indicate less poverty. Language is coded 0 = prefer English, and 1 = prefer Spanish. Parent education is coded such that higher values indicate greater educational attainment.
The only predictors of the rate of change in Conduct Problems from pre-injury to 12 months were children's pre-injury prosocial behaviors (linear β = −0.36, p < 0.05, quadratic: β = −0.37, p = 0.06) such that higher levels of pro-social behavior predicted less of an increase (and a dampened rate of increase). Similarly, higher pre-injury concussion-type symptoms were actually associated with a decrease in the change and rate of change of Conduct Problems. Pre-injury family characteristics predicted neither linear nor quadratic change across the first year after injury.
The linear slope from 12 to 36 months was not predicted by injury type, child characteristics, or family characteristics.
Discussion
In this longitudinal prospective cohort study, we followed the recovery of Emotional Symptoms and Conduct Problems as proxies of internalizing and externalizing behavior problems across the first 3 years after pediatric TBI vs. OI. We found that among children with TBI, both Emotional Symptoms and Conduct Problems were significantly elevated at 12 months and did not recover to pre-injury levels over the subsequent 2 years relative to the OI group. This is in contrast to children with OI, who showed minimal increases in either Emotional Symptoms or Conduct Problems across time. Our findings suggest that the elevations in problems may be attributed to the TBI and not to the experience of sustaining an injury per se. Growth models revealed that TBI was associated with a steeper non-linear increase in Emotional Symptoms and Conduct Problems from pre-injury to 12 months and increased level at 12 months relative to the OI group. Growth from 12 to 36 months was relatively flat in both groups, which suggests that children do not have increasing problems, but also do not recover.
Consistent with our hypotheses, we identified both shared and unique vulnerability factors affecting the level and change in Emotional Symptoms and Conduct Problems over time. Shared vulnerability factors included experiencing a TBI and having more pre-injury executive dysfunction. The increase in Emotional Symptoms and Conduct Problems at 12 months is consistent with prior longitudinal studies reporting increased internalizing and/or externalizing problems during the year after TBI after accounting for pre-injury status (12, 19, 35, 59). There is limited information regarding whether internalizing and externalizing problems increase systematically as TBI severity increases. In our sample, there were no differences in behavior problems between patients with mild, moderate, or severe TBI at any timepoints Although few studies have examined behavior problems across the spectrum of TBI severity, there is evidence that children with mild TBI (19, 59) and complicated-mild to severe TBI (5, 12) are at increased risk.
The centrality of EF as a predictor of both internalizing and externalizing outcomes is a novel finding. Although EF are key markers predicting future attainments across a variety of ages and developmental conditions (60, 61), the influence of pre-injury EF on outcomes has rarely been considered. Children who experience difficulties in inhibition, working memory, and attention-deficit hyperactivity problems appear to be at elevated risk for a broad range of behavior problems after TBI. After TBI in early childhood, Narad et al. found that greater pre-injury executive dysfunction was associated with greater likelihood of clinically significant EF symptoms persisting up to 7 years after injury (39). While It is unclear to what extent pre-existing EFs problems shape post-injury cognition and behavior in school-aged children and adolescents, there is a growing body of evidence showing significant and persistent adverse effects of TBI on EFs across the first 2 years after injury, with greater disruption following severe TBI than less severe injuries (35, 38). Long term follow up studies examining EF outcomes from 3 to 10 years after injury have also shown persistent problems, with EFs not returning to pre-injury levels (35, 62–64). Executive dysfunction after TBI has serious consequences for post-traumatic adjustment (65) and contributes to poorer educational outcomes (66, 67) and reduced social competence (68). TBI may exacerbate pre-existing EF problems in children and may magnify vulnerability to an array of poorer outcomes. Future studies should disentangle the effects of pre-existing vs. acquired EF on both cognitive and behavioral outcomes.
In addition to TBI and EFs, specific pre-injury child and family factors uniquely predicted the rate of change and level of Emotional Symptoms during the first year after TBI. After controlling for pre-injury ratings, girls had increased Emotional Symptoms 12 months post-injury. There were no differences in the rate of change over time for girls and boys. This finding is consistent with prior literature suggesting vulnerability of girls after both TBI (10, 69–72) and the broader category of pediatric acquired brain injury (73). Similarly, increased internalizing and ADHD symptoms were noted in girls compared to boys when assessed during the first year after injury after accounting for pre-injury ratings (5). Longer term follow-up studies found increases in internalizing symptoms over several years after TBI in both sexes; additionally, younger boys showed greater oppositional defiant problems and older girls showed greater ADHD symptoms (6). Developmentally, internalizing behavior problems tend to increase more in girls than boys during adolescence (74, 75), while externalizing problems are elevated in boys relative to girls (76). However, we did not identify vulnerability of boys to increases in either outcome domain. Scott et al. assessed adulthood outcomes after pediatric TBI. They found that women reported more internalizing problems and men reported more externalizing problems (26). To better understand the influence of sex, age, and time since injury, future studies should examine the risk of both internalizing and externalizing problems in boys and girls across different developmental stages.
In our sample, increased Emotional Symptoms were also predicted by specific pre-injury child factors including problems in peer relations and physical limitations such as low energy that reduced participation in everyday activities. Interestingly, while poor EF was associated with elevated Emotional Symptoms at 12 months, it was also associated with a slower rate of increase in symptoms from injury to 12 months. It is possible that children with greater pre-injury executive dysregulation are less likely to develop the types of somatic, anxiety, and depression symptoms tapped by this subtest. Such children may be more likely to develop externalizing than internalizing behaviors over time. This is indicated by the positive quadratic change parameter for the EF factor that approached significance in the Conduct Problem analysis. Family risk factors, including increased family dysfunction, as well as lower parental education, income, and social integration into the community were also important predictors of increased Emotional Symptoms. The influence of family factors on a variety of outcomes after TBI is supported by prior literature (29, 77, 78). Changes across long-term follow-ups were largely related to both pre-existing post-concussion-like symptoms and family factors rather than injury factors. Additional work should characterize whether prior emotional, somatic, or fatigue concussion-like symptoms drive this relation. Given the contribution of family factors and the growing recognition of the contribution of family and parenting factors to child behavioral outcomes after TBI (6, 79), psychological interventions including a family component are appropriate targets for intervention.
Conduct Problems also had unique vulnerability factors. A higher level of Conduct Problems at year 1 was found in younger children and children with more prior emotional/behavioral difficulties and lower prosocial behaviors. As expected, family indicators were also related to the level of Conduct Problems 1 year post-injury; higher social capital, higher income and Spanish as preferred language were associated with fewer Conduct Problems. In contrast to Emotional Symptoms, change from pre-injury to 1 year after injury was related to unique child characteristics. Poorer prosocial behavior was associated with increased Conduct Problems while more PCS-like symptoms were associated with less increase or a dampening of Conduct Problems. Also differing from Emotional Symptoms, no variables predicted change in Conduct Problems over the extended follow-up. This suggests that Conduct Problems became stable deficits by 1 year after TBI and showed no trend toward recovery. Our findings are similar to Ryan et al., who found a high rate of externalizing behavior problems persisting into young adulthood that were not related to either TBI severity or to family characteristics (80). Previous studies have linked EFs to changes in externalizing problems over time. Additionally, parent characteristics and parenting practices are associated with child externalizing problems after TBI (31, 81). Consequently, comprehensive intervention strategies that target parenting practices, in addition to addressing EFs and externalizing symptoms, may be fruitful targets to improve outcomes after TBI. Evidence-based programs that can be delivered online and customized to family structure offer advantages for improving family outcomes (82).
Conclusions and Limitations
Our findings should be viewed in relation to study limitations. We included only parent-reported outcomes, which may result in a limited view of behavior concerns, especially internalizing problems. Our findings are based on behavior ratings and do not incorporate any direct measures of child abilities or characteristics. Although we used well-validated measures that are common data elements for TBI outcomes, all measures were collected online or by telephone, which may differ from in-person evaluations. Our intent was to examine pre-injury predictors of outcome. However, including post-injury child and family changes may provide additional insight into factors influencing the trajectory of long-term outcomes.
Strengths of the study include the longitudinal, prospective design including a large and well-characterized sample with a broad spectrum of TBI severity and age range. Statistical approaches incorporated multivariable predictors in a structural equation modeling framework and identified factors contributing to the level and change in internalizing and externalizing behavior problems across the first 3 years after TBI. We emphasized a range of pre-injury child and family characteristics as potential influences on long-term adjustment. Including pre-injury EF as a predictor of outcomes is novel and has potential to improve understanding of child vulnerability and protective factors.
In conclusion, our findings indicated significant increases in both internalizing and externalizing behavior problems after TBI. This increase was stable across the prospective extended 3 year follow-up, indicating that problems accelerated across the first year after TBI and then either stayed stable or increased from 12 to 36 months after TBI, resulting in chronic behavior changes. We identified both shared and unique influences shaping behavior. During the first year after injury, shared vulnerability factors for internalizing and externalizing behavior problems included TBI, less favorable pre-injury child EFs, and poverty. All other child and family factors were uniquely related to the level of Emotional Symptoms and Conduct Problems. Our finding that long term internalizing problems were more strongly related to family factors and that externalizing problems were more strongly related to child factors suggests that personalized approaches to child and family intervention may be warranted.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Committee for the Protection of Human Subjects at University of Texas Health Science Center and at University of Utah Medical School. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
LE-C, JM, and HK conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. CC made substantial contributions to acquisition of data, critically reviewed, and revised the manuscript for important intellectual content. JM, AC, and RH made substantial contributions to the analysis, interpretation of data, and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Centers for Disease Control under Cooperative Agreement U01/CE002188. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease COntrol and PRevention. This study was also supported by the National Institute of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development K24HD072984. Neither the CDC nor the NICHD played a role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Additional funding was provided by the Nicole and Evan Katz Neurodevelopmental Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.687740/full#supplementary-material
References
1. Price J, Kassam-Adams N, Alderfer MA, Christofferson J, Kazak AE. Systematic review: a reevaluation and update of the integrative (trajectory) model of pediatric medical traumatic stress. J Pediatr Psychol. (2016) 41:86–97. doi: 10.1093/jpepsy/jsv074
2. McLaughlin KA, Lambert HK. Child trauma exposure and psychopathology: mechanisms of risk and resilience. Curr Opin Psychol. (2017) 14:29–34. doi: 10.1016/j.copsyc.2016.10.004
3. Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev Med Child Neurol. (2013) 55:37–45. doi: 10.1111/j.1469-8749.2012.04414.x
4. Geraldina P, Mariarosaria L, Annarita A, Susanna G, Michela S, Alessandro D, et al. Neuropsychiatric sequelae in TBI: a comparison across different age groups. Brain Inj. (2003) 17:835–46. doi: 10.1080/0269905031000088612
5. Keenan HT, Clark AE, Holubkov R, Cox CS, Ewing-Cobbs L. Psychosocial and executive function recovery trajectories one year after pediatric traumatic brain injury: the influence of age and injury severity. J Neurotrauma. (2017) 35:286–96. doi: 10.1089/neu2017.5265
6. Wade SL, Kaizar EE, Narad ME, Zang H, Kurowski BG, Miley AE, et al. Behavior problems following childhood TBI: the role of sex, age, and time since injury. J Head Trauma Rehabil. (2020) 35:E393–404. doi: 10.1097/HTR.0000000000000567
7. Bloom DR, Levin HS, Ewing-Cobbs L, Saunders AE, Song J, Fletcher JM, et al. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry. (2001) 40:572–9. doi: 10.1097/00004583-200105000-00017
8. Max JE. Neuropsychiatry of pediatric traumatic brain injury. Psychiatr Clin North Am. (2014) 37:125–40. doi: 10.1016/j.psc.2013.11.003
9. Max JE, Friedman K, Wilde EA, Bigler ED, Hanten G, Schachar RJ, et al. Psychiatric disorders in children and adolescents 24 months after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. (2015) 27:112–20. doi: 10.1176/appi.neuropsych.13080190
10. Gerring JP, Slomine BS, Vasa R, Grados MA, Chen A, Rising W, et al. Clinical predictors of posttraumatic stress disorder after closed head injury in children. J Am Acad Child Adolesc Psychiatry. (2002) 41:157–65. doi: 10.1097/00004583-200202000-00009
11. National Center for Injury Prevention and Control on Mild Traumatic Brain Injury in the US: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention (2003).
12. Kirkwood M, Janusz J, Yeates KO, Taylor HG, Wade SL, Stancin T, et al. Prevalence and correlates of depressive symptoms following traumatic brain injuries in children. Child Neuropsychol. (2000) 6:195–208. doi: 10.1076/chin.6.3.195.3157
13. Pastore V, Galbiati S, Recla M, Colombo K, Beretta E, Strazzer S. Psychological and behavioural difficulties following severe TBI in adolescence: a comparison with a sample of peers with brain lesions of other origin and with a control group. Brain Inj. (2018) 32:1011–20. doi: 10.1080/02699052.2018.1469041
14. Knights RM, Iran LP, Ventureyra EC, Bentirogrio C, Stoddart C, Winogron HW, et al. The effects of head injury in children on neuropsychological and behavioral functioning. Brain Inj. (1991) 5:339–51. doi: 10.3109/02699059109008107
15. Walz NC, Yeates KO, Wade SL, Mark E. Social information processing skills in adolescents with traumatic brain injury: relationship with social competence and behavior problems. J Pediatr Rehabil Med. (2009) 2:285–95. doi: 10.3233/PRM-2009-0094
16. Wetherington CE, Hooper SR, Keenan HT, Nocera M, Runyan D. Parent ratings of behavioral functioning after traumatic brain injury in very young children. J Pediatr Psychol. (2010) 35:662–7. doi: 10.1093/jpepsy/jsp081
17. Chapman LA, Taylor HG, Wade SL, Walz NC, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabil Psychol. (2010) 55:48–57. doi: 10.1037/a0018418
18. Catroppa C, Hearps S, Crossley L, Yeates K, Beauchamp M, Fusella J, et al. Social and behavioral outcomes following childhood traumatic brain injury: what predicts outcome at 12 months post-insult? J Neurotrauma. (2017) 34:1439–47. doi: 10.1089/neu.2016.4594
19. Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. (2002) 16:15–27. doi: 10.1037/0894-4105.16.1.15
20. Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J Pediatr Psychol. (2003) 28:251–63. doi: 10.1093/jpepsy/jsg013
21. Andrews TK, Rose FD, Johnson DA. Social and behavioural effects of traumatic brain injury in children. Brain Inj. (1998) 12:133–8. doi: 10.1080/026990598122755
22. Hayman-Abello SE, Rourke BP, Fuerst DR. Psychosocial status after pediatric traumatic brain injury: a subtype analysis using the child behavior checklist. J Int Neuropsychol Soc. (2003) 9:887–98. doi: 10.1017/S1355617703960097
23. Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation and social and behavioral functioning following childhood traumatic brain injury. J Int Neuropsychol Soc. (2006) 12:609–21. doi: 10.1017/S1355617706060796
24. McKinlay A, Grace R, Horwood J, Fergusson D, MacFarlane M. Adolescent psychiatric symptoms following preschool childhood mild traumatic brain injury: evidence from a birth cohort. J Head Trauma Rehabil. (2009) 24:221–7. doi: 10.1097/HTR.0b013e3181a40590
25. Albicini M, McKinlay A. Internalizing disorders in adults with a history of childhood traumatic brain injury. J Clin Exp Neuropsychol. (2015) 37:776–84. doi: 10.1080/13803395.2015.1053843
26. Scott C, McKinlay A, McLellan T, Britt E, Grace R, MacFarlane M. A comparison of adult outcomes for males compared to females following pediatric traumatic brain injury. Neuropsychology. (2015) 29:501–8. doi: 10.1037/neu0000074
27. McCormick BF, Connolly EJ, Nelson DV. Mild traumatic brain injury as a predictor of classes of youth internalizing and externalizing psychopathology. Child Psychiatry Hum Dev. (2021) 52:166–78. doi: 10.1007/s10578-020-00992-9
28. Emery CA, Barlow KM, Brooks BL, Max JE, Villavicencio-Requis A, Gnanakumar V, et al. A systematic review of psychiatric, psychological, and behavioural outcomes following mild traumatic brain injury in children and adolescents. Can J Psychiatry Revue Can Psychiatr. (2016) 61:259–69. doi: 10.1177/0706743716643741
29. Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO, Minich N. A prospective study of long-term caregiver and family adaptation following brain injury in children. J Head Trauma Rehabil. (2002) 17:96–111. doi: 10.1097/00001199-200204000-00003
30. Peterson RL, Kirkwood MW, Taylor HG, Stancin T, Brown TM, Wade SL. Adolescents' internalizing problems following traumatic brain injury are related to parents' psychiatric symptoms. J Head Trauma Rehabil. (2013) 28:E1–12. doi: 10.1097/HTR.0b013e318263f5ba
31. Raj SP, Wade SL, Cassedy A, Taylor HG, Stancin T, Brown TM, et al. Parent psychological functioning and communication predict externalizing behavior problems after pediatric traumatic brain injury. J Pediatr Psychol. (2014) 39:84–95. doi: 10.1093/jpepsy/jst075
32. Petranovich CL, Smith-Paine J, Wade SL, Yeates KO, Taylor HG, Stancin T, et al. From early childhood to adolescence: lessons about traumatic brain injury from the ohio head injury outcomes study. J Head Trauma Rehabil. (2020) 35:226–39. doi: 10.1097/HTR.0000000000000555
33. Diamond A. Executive functions. Annu Rev Psychol. (2013) 64:135–68. doi: 10.1146/annurev-psych-113011-143750
34. Zelazo PD. Executive function and psychopathology: a neurodevelopmental perspective. Ann Rev Clin Psychol. (2020) 16:431–54. doi: 10.1146/annurev-clinpsy-072319-024242
35. Keenan HT, Clark AE, Holubkov R, Cox CS Jr., Ewing-Cobbs L. Trajectories of children's executive function after traumatic brain injury. JAMA Netw Open. (2021) 4:e212624. doi: 10.1001/jamanetworkopen.2021.2624
36. Johnson CP, Juranek J, Kramer LA, Prasad MR, Swank PR, Ewing-Cobbs L. Predicting behavioral deficits in pediatric traumatic brain injury through uncinate fasciculus integrity. J Int Neuropsychol Soc. (2011) 17:663–73. doi: 10.1017/S1355617711000464
37. Gorman S, Barnes MA, Swank PR, Ewing-Cobbs L. Recovery of working memory following pediatric traumatic brain injury: a longitudinal analysis. Dev Neuropsychol. (2017) 42:127–45. doi: 10.1080/87565641.2017.1315581
38. Sesma HW, Slomine BS, Ding R, McCarthy ML. Executive functioning in the first year after pediatric traumatic brain injury. Pediatrics. (2008) 121:e1686–95. doi: 10.1542/peds.2007-2461
39. Narad ME, Treble-Barna A, Peugh J, Yeates KO, Taylor HG, Stancin T, et al. Recovery trajectories of executive functioning after pediatric TBI: a latent class growth modeling analysis. J Head Trauma Rehabil. (2017) 32:98–106. doi: 10.1097/HTR.0000000000000247
40. Taylor HG, Orchinik LJ, Minich N, Dietrich A, Nuss K, Wright M, et al. Symptoms of persistent behavior problems in children with mild traumatic brain injury. J Head Trauma Rehabil. (2015) 30:302–10. doi: 10.1097/HTR.0000000000000106
41. Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. (1974) 2:81–4. doi: 10.1016/S0140-6736(74)91639-0
42. Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, et al. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatr. (2008) 1:461–70. doi: 10.3171/PED/2008/1/6/461
43. Abbreviated Injury Scale. Des Plaines, IL: Association for the Advancement of Automotive Medicine (1990).
44. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
45. Landgraf JM. Child health questionnaire (CHQ). In: Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer Netherlands (2014). p. 698–702.
46. Sady MD, Vaughan CG, Gioia GA. Psychometric characteristics of the postconcussion symptom inventory in children and adolescents. Arch Clin Neuropsychol. (2014) 29:348–63. doi: 10.1093/arclin/acu014
47. Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function (BRIEF). Odessa: Psychological Assessment Resources, Inc. (2000).
48. Achenbach T. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont College of Medicine (1991).
49. Miller IW, Bishop DS, Epstein NB, Keitner GI. The McMaster family assessment device: reliability and validity. J Marital Fam Ther. (1985) 11:345–56. doi: 10.1111/j.1752-0606.1985.tb00028.x
50. Runyan DK, Hunter WM, Socolar RR, Amaya-Jackson L, English D, Landsverk J, et al. Children who prosper in unfavorable environments: the relationship to social capital. Pediatrics. (1998) 101:12–8. doi: 10.1542/peds.101.1.12
51. McCauley SR, Wilde E, Hicks R, Anderson VA, Bedell G, Beers SR, et al. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. J Neurotrauma. (2012) 29:678–705. doi: 10.1089/neu.2011.1838
52. Cicchetti D. Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry. (2010) 9:145–54. doi: 10.1002/j.2051-5545.2010.tb00297.x
53. Sulik MJ, Huerta S, Zerr AA, Eisenberg N, Spinrad TL, Valiente C, et al. The factor structure of effortful control and measurement invariance across ethnicity and sex in a high-tisk sample. J Psychopathol Behav Assess. (2009) 32:8–22. doi: 10.1007/s10862-009-9164-y
54. Willoughby MT, Wirth RJ, Blair CB. Executive function in early childhood: longitudinal measurement invariance and developmental change. Psychol Assess. (2012) 24:418–31. doi: 10.1037/a0025779
55. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. (1999) 6:1–55. doi: 10.1080/10705519909540118
56. Muthen B, Muthen L. Mplus User's Guide: Fourth Edition. Los Angeles: Muthen & Muthen, Inc. (2006).
57. Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. New York, NY: Routledge (2010).
58. Hair JB, William C, Babin BJ, Anderson RE. Multivariate Data Analysis. 7th ed. Upper Saddle River, NJ: Pearson Educational International (2010).
59. Asarnow RF, Satz P, Light R. Behavioral problems and adaptive functioning in children with mild and severe closed head injury. J Pediatr Psychol. (1991) 16:543–55. doi: 10.1093/jpepsy/16.5.543
60. Montroy JJ, Bowles RP, Skibbe LE, McClelland MM, Morrison FJ. The development of self-regulation across early childhood. Dev Psychol. 52:1744–62. doi: 10.1037/dev0000159
61. Toll SW, Van der Ven SH, Kroesbergen EH, Van Luit JE. Executive functions as predictors of math learning disabilities. J Learn Disabil. (2011) 44:521–32. doi: 10.1177/0022219410387302
62. Muscara F, Catroppa C, Eren S, Anderson V. The impact of injury severity on long-term social outcome following paediatric traumatic brain injury. Neuropsychol Rehabil. (2009) 19:541–61. doi: 10.1080/09602010802365223
63. Beauchamp M, Catroppa C, Godfrey C, Morse S, Rosenfeld JV, Anderson V. Selective changes in executive functioning ten years after severe childhood traumatic brain injury. Dev Neuropsychol. (2011) 36:578–95. doi: 10.1080/87565641.2011.555572
64. Le Fur C, Câmara-Costa H, Francillette L, Opatowski M, Toure H, Brugel D, et al. Executive functions and attention 7 years after severe childhood traumatic brain injury: results of the Traumatisme Grave de l'Enfant (TGE) cohort. Ann Phys Rehabil Med. (2020) 63:270–9. doi: 10.1016/j.rehab.2019.09.003
65. Narad ME, Riemersma J, Wade SL, Smith-Paine J, Morrison P, Taylor HG, et al. Impact of secondary ADHD on long-term outcomes after early childhood traumatic brain injury. J Head Trauma Rehabil. (2020) 35:E271–9. doi: 10.1097/HTR.0000000000000550
66. Arnett AB, Peterson RL, Kirkwood ML, Taylor HG, Stancin T, Brown TM, et al. Behavioral and cognitive predictors of educational outcomes in pediatric traumatic brain injury. J Int Neuropsychol Soc. (2013) 19:881–9. doi: 10.1017/S1355617713000635
67. Ewing-Cobbs L, Barnes MA, Fletcher JM, Levin HS, Swank PR, Song J. Modeling of longitudinal academic achievement scores after pediatric traumatic brain injury. Dev Neuropsychol. (2004) 25:107–33. doi: 10.1080/87565641.2004.9651924
68. Ganesalingam K, Yeates KO, Taylor HG, Walz NC, Stancin T, Wade S. Executive functions and social competence in young children 6 months following traumatic brain injury. Neuropsychology. (2011) 25:466–76. doi: 10.1037/a0022768
69. Ewing-Cobbs L, Cox CS Jr., Clark AE, Holubkov R, Keenan HT. Persistent postconcussion symptoms after injury. Pediatrics. (2018) 142:e20180939. doi: 10.1542/peds.2018-0939
70. Desai N, Wiebe DJ, Corwin DJ, Lockyer JE, Grady MF, Master CL. Factors affecting recovery trajectories in pediatric female concussion. Clin J Sport Med. (2019) 29:361–7. doi: 10.1097/JSM.0000000000000646
71. Grados MA, Slomine BS, Gerring JP, Vasa R, Bryan N, Denckla MB. Depth of lesion model in children and adolescents with moderate to severe traumatic brain injury: use of SPGR MRI to predict severity and outcome. J Neurol Neurosurg Psychiatry. (2001) 70:350–8. doi: 10.1136/jnnp.70.3.350
72. Fisher ER, Montroy JJ, Duque G, Cox CS, Ewing-Cobbs L. Post-concussion and post-traumatic stress symptoms after pediatric traumatic brain injury: shared vulnerability factors? J Neurotrauma. (2021). doi: 10.1089/neu.2020.7541. [Epub ahead of print].
73. Hendry K, Ownsworth T, Waters AM, Jackson M, Lloyd O. [Formula: see text] Investigation of children and adolescents' mood and self-concept after acquired brain injury. Child Neuropsychol. (2020) 26:1005–25. doi: 10.1080/09297049.2020.1750577
74. Durbeej N, Sörman K, Norén Selinus E, Lundström S, Lichtenstein P, Hellner C, et al. Trends in childhood and adolescent internalizing symptoms: results from Swedish population based twin cohorts. BMC Psychol. (2019) 7:50. doi: 10.1186/s40359-019-0326-8
75. Gutman LM, Codiroli McMaster N. Gendered pathways of internalizing problems from early childhood to adolescence and associated adolescent outcomes. J Abnorm Child Psychol. (2020) 48:703–18. doi: 10.1007/s10802-020-00623-w
76. Bongers IL, Koot HM, van der Ende J, Verhulst FC. Developmental trajectories of externalizing behaviors in childhood and adolescence. Child Dev. (2004) 75:1523–37. doi: 10.1111/j.1467-8624.2004.00755.x
77. Anderson VA, Catroppa C, Haritou F, Morse S, Rosenfeld JV. Identifying factors contributing to child and family outcome 30 months after traumatic brain injury in children. J Neurol Neurosurg Psychiatry. (2005) 76:401–8. doi: 10.1136/jnnp.2003.019174
78. Yeates KO, Taylor HG, Rusin J, Bangert B, Dietrich A, Nuss K, et al. Premorbid child and family functioning as predictors of post-concussive symptoms in children with mild traumatic brain injuries. Int J Dev Neurosci. (2012) 30:231–7. doi: 10.1016/j.ijdevneu.2011.05.008
79. Jones KM, Ameratunga S, Starkey NJ, Theadom A, Barker-Collo S, Ikeda T, et al. Psychosocial functioning at 4-years after pediatric mild traumatic brain injury. Brain Inj. (2021) 35:416–25. doi: 10.1080/02699052.2021.1878553
80. Ryan NP, Hughes N, Godfrey C, Rosema S, Catroppa C, Anderson VA. Prevalence and predictors of externalizing behavior in young adult survivors of pediatric traumatic brain injury. J Head Trauma Rehabil. (2015) 30:75–85. doi: 10.1097/HTR.0000000000000123
81. Chavez-Arana C, Catroppa C, Yáñez-Téllez G, Prieto-Corona B, de León MA, García A, et al. Parenting and the dysregulation profile predict executive functioning in children with acquired brain injury. Child Neuropsychol. (2019) 25:1125–43. doi: 10.1080/09297049.2019.1589442
Keywords: traumatic brain injury, behavioral symptoms, psychological adjustment, emotional symptoms, conduct problems, executive functions, long-term outcome, pediatric
Citation: Ewing-Cobbs L, Montroy JJ, Clark AE, Holubkov R, Cox CS Jr and Keenan HT (2021) As Time Goes by: Understanding Child and Family Factors Shaping Behavioral Outcomes After Traumatic Brain Injury. Front. Neurol. 12:687740. doi: 10.3389/fneur.2021.687740
Received: 30 March 2021; Accepted: 25 May 2021;
Published: 05 July 2021.
Edited by:
Bridgette D. Semple, Monash University, AustraliaReviewed by:
Kelly Marie Jones, Auckland University of Technology, New ZealandAmery Treble-Barna, University of Pittsburgh, United States
Copyright © 2021 Ewing-Cobbs, Montroy, Clark, Holubkov, Cox and Keenan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linda Ewing-Cobbs, bGluZGEuZXdpbmctY29iYnNAdXRoLnRtYy5lZHU=
†These authors have contributed equally to this work and share first authorship
 Linda Ewing-Cobbs
Linda Ewing-Cobbs Janelle J. Montroy
Janelle J. Montroy Amy E. Clark2
Amy E. Clark2 Charles S. Cox Jr.
Charles S. Cox Jr. Heather T. Keenan
Heather T. Keenan