
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 09 July 2021
Sec. Neuroepidemiology
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.669174
 Dandan Guo1†
Dandan Guo1† Xin Zhang1†
Xin Zhang1† Changqing Zhan1,2†
Changqing Zhan1,2† Qiuxing Lin1,3,4
Qiuxing Lin1,3,4 Jie Liu1,3,4
Jie Liu1,3,4 Qiaoxia Yang5
Qiaoxia Yang5 Jun Tu1,3,4
Jun Tu1,3,4 Xianjia Ning1,3,4*
Xianjia Ning1,3,4* Jinghua Wang1,3,4*
Jinghua Wang1,3,4* Yijun Song6*
Yijun Song6*Background: Obesity is a potentially modifiable risk factor for cognitive impairment. However, sex-specific relationships between obesity and cognitive impairment in late life remain unclear.
Objective: We aimed to assess sex differences in the association between various obesity parameters and cognitive impairment in a low-income elderly population in rural China.
Methods: A population-based cross-sectional study was conducted to collect basic information from elderly residents aged 60 years and older from April 2014 to August 2014 in rural areas of Tianjin, China. Obesity parameters, including body mass index (BMI) and waist circumference (WC), and Mini Mental State Examination scores were measured, and the relationships between these variables were assessed.
Results: A total of 1,081 residents with a mean age of 67.70 years were enrolled in this study. After adjusting for age, educational attainment, smoking status, drinking status, physical exercise participation, and the presence of diabetes and hyperlipidemia, blood pressure group; a high BMI was found to be associated with an increased prevalence of cognitive impairment in elderly women. Each 1-unit increase in BMI was associated with a 5.9% increase in the prevalence of cognitive impairment. WC was related to the prevalence of cognitive impairment in elderly men, and each 1-cm increase in WC was associated with a 4.0% decrease in the prevalence of cognitive impairment. However, there were no significant associations between WC and cognitive function in women or between BMI and cognitive impairment in men.
Conclusion: A greater WC was positively associated with better cognitive function in low-income elderly men in rural China, whereas a higher BMI was associated with an increased risk of cognitive impairment in elderly women, independent of sociodemographic, lifestyle, and health-related comorbid factors. Our results suggest weight management of elderly women in rural China may have cognitive benefits. However, randomized controlled trials would be needed to confirm causality.
Cognitive disorders, including dementia and mild cognitive impairment, have become a global public health priority for aging populations (1, 2). According to the World Alzheimer Report 2019, there were over 50 million people living with dementia globally, and this number is estimated to increase to more than 152 million by 2050 (3). The current annual costs related to dementia worldwide were approximately 1 trillion USD in 2019, a figure set to double by 2030 (3). Moreover, the prevalence of dementia has been increasing rapidly over the past two decades in China, from 2.30 to 6.44%, especially among populations in rural areas with low educational attainment (4, 5). Meanwhile, the prevalence of obesity is also increasing worldwide and has become a global epidemic among older people (6). In China, the overall prevalence of general obesity among adults has increased 3-fold, from 3.3% in 2004 to 14.0% in 2014, posing a huge economic and social burden (7).
Obesity has often been recognized in the literature as a potentially modifiable risk factor for cognitive impairment (8, 9). The effects of obesity on cognitive function appear to vary by age and obesity status. Most of the recent studies have demonstrated that general obesity at midlife was related to an increased risk of cognitive decline in later life, especially for episodic memory and executive function (10–12). However, the association between obesity and cognitive impairment in the elderly is unclear. Several studies have demonstrated that general obesity as classified using body mass index (BMI) was associated with a decreased risk of cognitive impairment in the elderly, while abdominal obesity was harmful to cognitive function (13–15). In contrast, other studies have reported that both general and abdominal obesity were associated with an increased risk of cognitive dysfunction in old age (16, 17). Furthermore, few studies have reported the sex-related relationships between obesity and cognitive impairment, and these results were inconsistent (18–20).
The prevalence of cognitive impairment in rural China is notably higher than that in urban areas (5). However, the relationship between obesity in late life and cognitive impairment remains unclear among low-income populations in rural China. Additionally, sex differences in the associations between obesity and cognitive impairment are not well-known in China. Thus, the aim of this study was to assess the sex differences in the association between obesity and cognitive impairment among a low-income elderly population in rural China.
This was a population-based, cross-sectional study conducted from April 2014 to August 2014 in rural areas of Tianjin, China. The participants were from the Tianjin Brain Study, which has been described previously (21, 22). All residents aged 60 years and older without vision and auditory dysfunction were invited to participate in this study. However, individuals with a history of myocardial infarction, stroke, congenital hypophrenia, and mental illness were excluded from participation.
The study was approved by the ethics committee of Tianjin Medical University General Hospital and conformed to the Declaration of Helsinki regarding the use of human subjects. Written informed consent was obtained from each patient during recruitment.
This study was conducted through face-to-face interviews by a trained research staff. A pre-designed questionnaire was used to collect the following information: demographic information (including name, sex, date of birth, and educational level), individual medical history (including the presence of hypertension, diabetes mellitus, and hyperlipidemia), and lifestyle factors (including smoking, drinking, and physical exercise). A physical examination was performed to obtain information on height, weight, and waist circumference (WC) with subjects wearing thin clothes. BMI was calculated as the individual's weight (kg) divided by the square of the individual's height (m2). Blood pressure (BP) measurements were performed using an electronic sphygmomanometer. Subjects were asked to remain resting in a sitting position for 15 min before testing; BP was measured three times, and the mean was obtained. The levels of fasting blood glucose (FBG), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were tested in the central laboratory of Tianjin Ji County People's Hospital. Both the Mini Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) scales were used for screening cognitive impairment owing to their high sensitivity and specificity (23). However, considering that the content of the MoCA questionnaire was not suitable for elderly with low education in rural China, the MMSE questionnaire was used to assess cognitive impairment.
The diagnostic criteria for cognitive impairment were based on MMSE scores and educational levels. Cognitive impairment was defined as an MMSE score <17 points in the group with no formal schooling, <22 points in the group with a primary school education, and <26 points in the group with a junior school education and above (24).
Hypertension was defined as a systolic blood pressure (SBP) ≥ 140 mm Hg, diastolic blood pressure (DBP) ≥ 90 mmHg, the use of antihypertensive drugs, or a history of hypertension. Stage I hypertension was defined as SBP ≥ 140 mm Hg and < 160 mm Hg or DBP ≥ 90 mm Hg and < 100 mm Hg, stage II hypertension was defined as SBP ≥ 160 mm Hg and < 180 mm Hg or DBP ≥ 100 mm Hg and < 110 mm Hg, and stage III hypertension was defined as SBP ≥ 180 mm Hg or DBP ≥ 110 mm Hg. Diabetes was defined as FBG ≥ 7.0 mmol/L, the use of diabetes medication, or a self-reported history of diabetes. Hyperlipidemia was defined as total cholesterol ≥5.18 mmol/L, low-density lipoprotein cholesterol ≥3.37 mmol/L, triglycerides ≥ 1.70 mmol/L, or high-density lipoprotein cholesterol < 1.04 mmol/L, or with diagnosis of hyperlipidemia. General obesity was defined as a BMI ≥ 28.0 kg/m2, and overweight was defined as a BMI ≥ 24.0 kg/m2 and < 28.0 kg/m2. Central obesity was defined as a WC >90 cm for men and >80 cm for women. Besides, BMI and WC were categorized into sex-specific quartiles. For men, first quartile of BMI was defined as <22.23 kg/m2; second quartile was 22.23–24.45 kg/m2; third quartile was 24.46–26.69 kg/m2 and fourth quartile was ≥ 26.70 kg/m2. First quartile of WC in men was defined as < 82 cm; second quartile was 82–87 cm; third quartile was 88–95 cm and fourth quartile was ≥ 96 cm. For women, first quartile of BMI was defined as <22.85 kg/m2; second quartile was 22.85–25.10 kg/m2; third quartile was 25.11–27.58 kg/m2 and fourth quartile was ≥ 27.59 kg/m2. First quartile of WC in women was defined as < 84 cm; second quartile was 84–88 cm; third quartile was 89–94 cm and fourth quartile was ≥95 cm. Smoking was defined as smoking ≥ 1 cigarette daily for more than 1 year. Drinking was defined as drinking >50 mL of alcohol at least once per week for more than 6 months.
Continuous variables are summarized as means and standard deviations; Student's t-test was used to compare the differences between the two groups. Categorical variables are summarized as numbers with frequencies; the chi-square test was performed to compare the differences between the two groups. The participants were categorized into four age groups (60–64, 65–69, 70–74, and ≥75 years), three educational groups according to the length of formal education (0–5, 6–8, and ≥9 years), and four BP groups (normal, stage I hypertension, stage II hypertension, and stage III hypertension). Multiple logistic regression analyses were used to evaluate the relationship between BMI or WC (continuous variables) and cognitive impairment by sex. Independent variables in the multivariate analyses were those factors found to be significant in the univariate analyses. Box-Tidwell method (25) was used to test linear relationship between continuous independent variables (BMI/WC) and dependent variable logit conversion values (all P > 0.05). Thus, BMI and WC were considered as continuous variables in multiple logistic regression analyses. Moreover, BMI and WC were also evaluated as categorical variables in multiple logistic regression analyses, divided by sex-specific quartiles. BMI and WC were included in different equations separately because of their high collinearity.
The multivariate analysis results are presented as adjusted odds ratios (ORs) and 95% confidence intervals (CIs) after adjusting for covariates. Additionally, three logistic regression models were developed to examine the associations of BMI and WC with cognitive impairment by sex. Model 1 involved adjusting for age and educational level (categorical variables). Model 2 was based on Model 1 and additionally adjusted for lifestyle factors (smoking, drinking, and physical exercise). Model 3 was based on Model 2 and additionally adjusted for BP group, diabetes, and hyperlipidemia.
All statistical analyses were performed with SPSS version 25.0 statistical software (SPSS Inc., Chicago, IL), and a two-sided P-value < 0.05 was considered statistically significant.
A total of 1,081 residents aged 60 years and older were enrolled in this study. There were 500 men (46.3%) and 581 women (53.7%), with a mean age of 67.70 years overall (67.96 years for men and 67.47 years for women). In this rural population, the prevalence of cognitive impairment was 33.2% overall (26.6% in men and 38.9% in women). Moreover, there was a higher prevalence of central and general obesity in women than in men (88.1 vs. 44.0% and 22.5 vs. 16.2%, respectively; both P < 0.01) among residents with cognitive impairment. In this population, women were more likely to have lower educational attainment and MMSE scores and higher BMI, DBP, FBG, TC, TG, HDL, and LDL levels than men (P < 0.05) (Table 1).
For elderly men, cognitive impairment was associated with older age, lower educational attainment, and higher SBP. Moreover, WC and were associated with cognitive impairment in men. The prevalence of cognitive impairment in men with central obesity was lower than that without central obesity (Table 2).
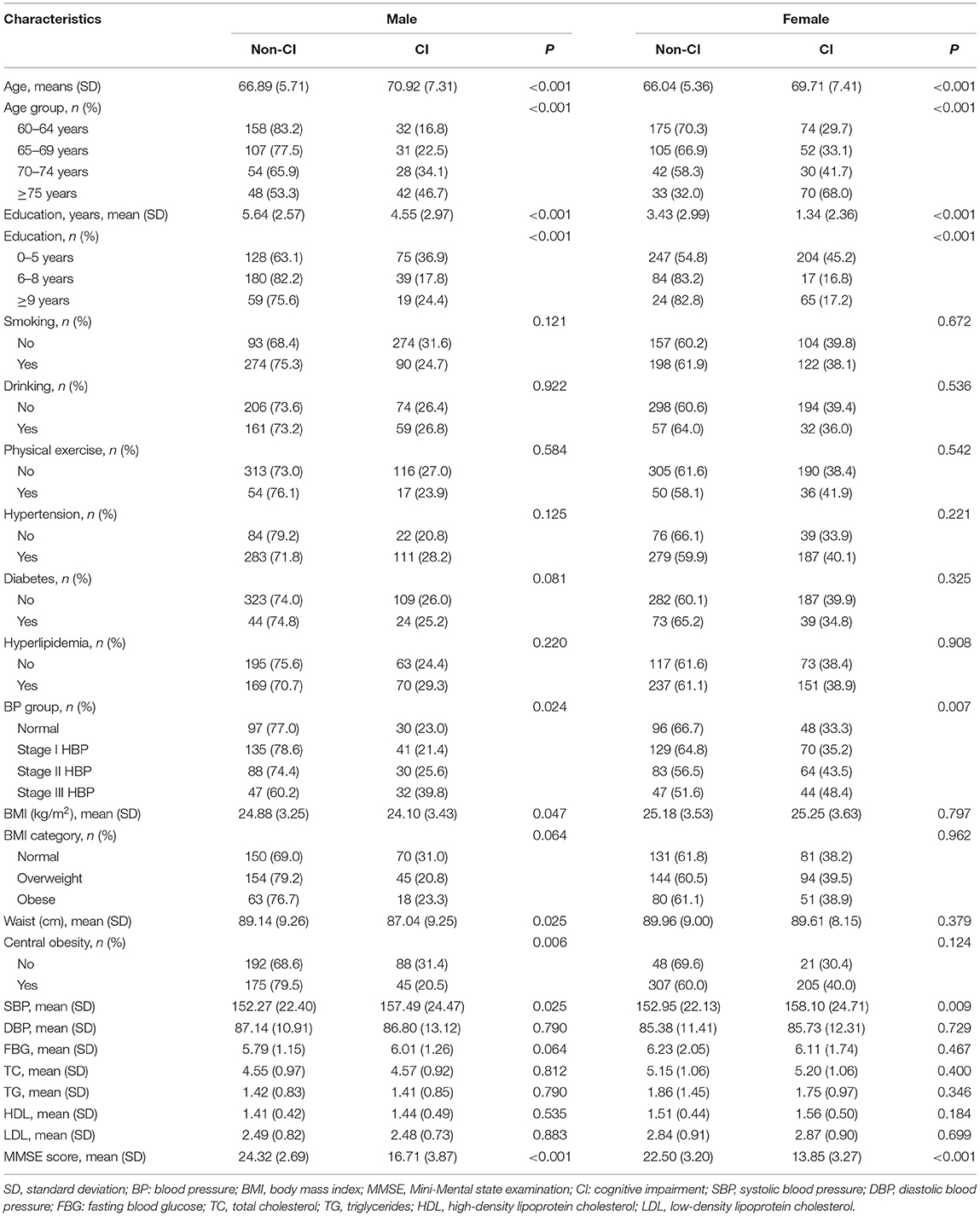
Table 2. Association of cognitive impairment with demographic characteristics and risk factors by gender in univariate analysis.
For elderly women, cognitive impairment was associated with older age, lower educational attainment, and higher SBP. However, neither BMI nor WC was associated with cognitive impairment in women (Table 2).
For elderly men, there was no significant association between BMI and cognitive impairment after adjusting for age, educational level, and BP group. WC was associated with cognitive impairment in elderly men, and each 1-cm increase in WC was associated with a 3% decrease in the prevalence of cognitive impairment after adjusting for age, educational level, and BP group (95% CI 0.95–0.99; P = 0.013). In a subgroup analysis, the association remained consistent among men aged 60–64 years and each 1-cm increase in WC was associated with a 5% decrease in the prevalence of cognitive impairment (95% CI 0.91–0.99; P = 0.042) (Table 3).
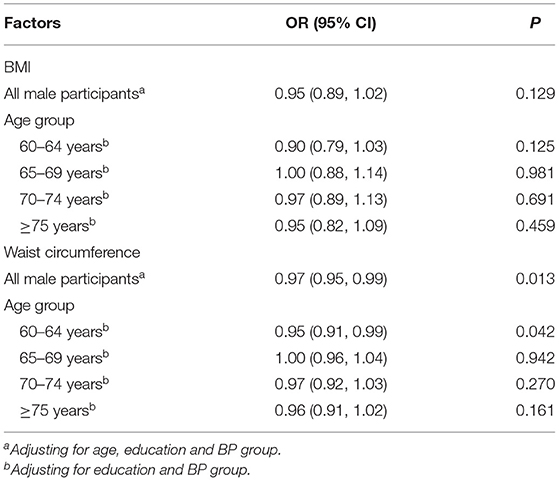
Table 3. Association of BMI and waist circumference with cognitive impairment by age groups among elderly men in the multivariate analysis.
BMI was associated with the prevalence of cognitive impairment in elderly women in Models 1, 2, and 3, while BMI was not associated with cognitive impairment in any multivariate model in elderly men. Each 1-unit increase in BMI was associated with a 5.9% increase in the prevalence of cognitive impairment in elderly women after adjusting for age, educational level, smoking, drinking, physical exercise, BP group, diabetes, and hyperlipidemia in Model 3 (95% CI 1.003–1.119; P = 0.038; Table 4).
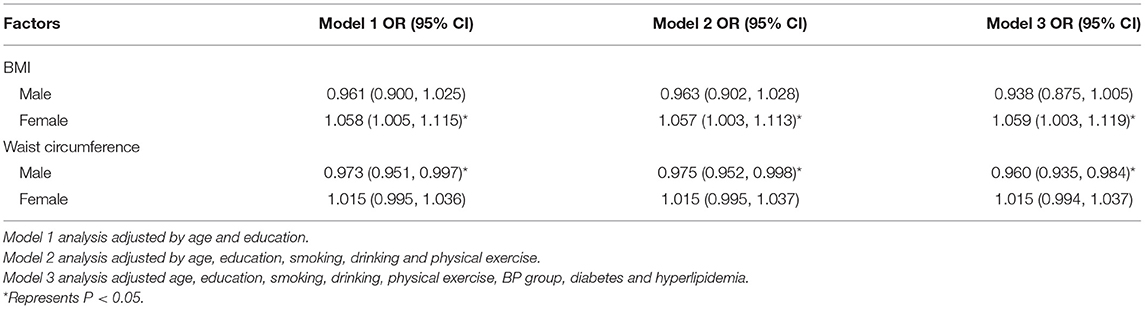
Table 4. Association of BMI and waist circumference with cognitive impairment by sex, according to demographic characteristics and risk factor groups in the multivariate analysis.
For elderly men, WC was related to the prevalence of cognitive impairment in Models 1, 2, and 3. Each 1-cm increase in WC was associated with a 4.0% decrease in the prevalence of cognitive impairment after adjusting for age, educational level, smoking, drinking, physical exercise, BP group, diabetes, and hyperlipidemia in Model 3 (95% CI 0.935–0.984; P = 0.002). However, there was no significant association between WC and cognitive impairment in elderly women (Table 4).
This study further explored the relationships between cognitive impairment with sex-specific quartiles of BMI and WC. Compared with the first quartile of BMI, the OR of the third quartile group among elderly women was 1.79 (95% CI 1.05–3.05) after adjusting for age, education, and BP group. For elderly men, the risk of cognitive impairment in the highest WC quartile decreased by 55% when compared with that in the lowest quartile (Table 5).
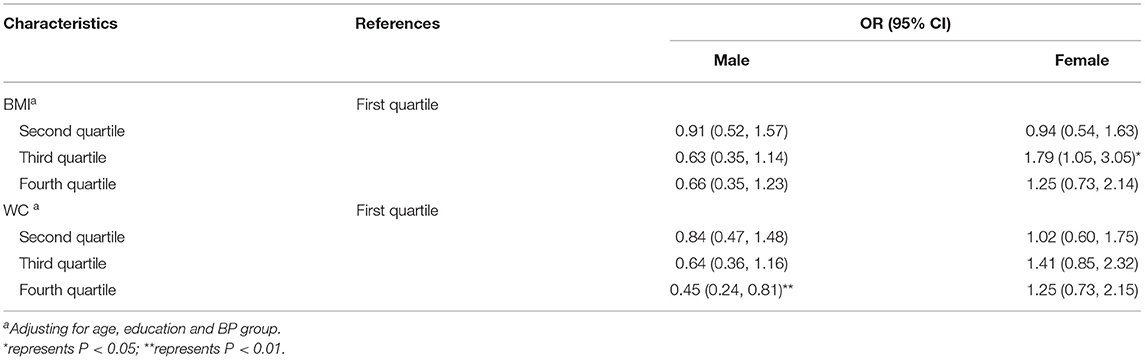
Table 5. Association of BMI and waist circumference quartiles with cognitive impairment by sex in the multivariate analysis.
When the interaction term was introduced, the analyses revealed a significant interaction between sex and BMI as well as sex and WC (Table 6).

Table 6. The interaction analysis between sex and BMI/ WC in multivariate logistic regression analysis.
The relationship between obesity and cognitive impairment in old age has been a controversial issue for many years. In the present population-based study, we evaluated the sex differences in the associations of BMI and WC with cognitive impairment in a low-income elderly population in rural China. We found that BMI was related to the prevalence of cognitive impairment in elderly women, not in elderly men; each 1-unit increase in BMI corresponded to a 5.9% increase in cognitive impairment in elderly women. Besides, each 1-cm increase in WC corresponded to a 4.0% decrease in prevalence of cognitive impairment in the fully adjusted model in elderly men. In the age subgroup analysis, the association remained consistent among men aged 60–64 years. However, there were no significant associations between WC and cognitive impairment in elderly women.
Obesity is often recognized as a public health issue worldwide because of its contribution to increased mortality and morbidity from cardiovascular diseases (26). However, the association between BMI and cognitive decline in the elderly is complex and controversial. Most studies have reported that being overweight in later life was associated with a lower risk of cognitive impairment and dementia in the elderly, which supported the “jolly fat” hypothesis of cognitive function (18, 20, 27–29). A clinical retrospective cohort study over two decades was conducted in the UK, and almost two million participants aged 40 years and older were included. In that study, being overweight or even obese in middle age and old age was associated with a decreased risk of dementia. Obese individuals (i.e., BMI >40 kg/m2) had a 29% lower (95% CI 22–36%) dementia risk than individuals with a healthy weight, while underweight people (i.e., BMI <20 kg/m2) had a 34% higher (95% CI 29–38%) risk of dementia (30). However, a recent systematic review failed to find a beneficial effect of being overweight on cognitive function in later life (31). Additionally, a few studies have reported that obesity is negatively associated with cognitive function in old age (16, 17). A population-based cross-sectional study in central Spain suggested that overweight and obese elderly adults had poorer neuropsychological performance than elderly adults with normal weight in verbal fluency, delayed-free recall, and immediate logical memory (16). Another population-based study revealed that increased BMI and visceral fat mass were associated with severe cognitive impairment in older men (17). In our study, a high BMI was associated with an increased prevalence of cognitive impairment in elderly women. In contrast, a high BMI appeared to be a protective factor for elderly men, although not to a significant degree, which was partly consistent with results of previous studies (18, 20). A prospective study of community-dwelling Koreans demonstrated that increased obesity, as defined using BMI, over time was associated with better cognitive function in elderly men. However, for elderly women, increased obesity, as defined using WC and waist-to-hip ratio (WHR), over time was associated with cognitive decline (18). The beneficial effects of obesity seemed to be applicable to elderly men and not to elderly women.
WC is a more accurate indicator of abdominal visceral obesity than BMI, percent body fat, and WHR (32). Moreover, abdominal obesity as classified using WC is a component of metabolic syndrome and is generally regarded as harmful to health. Most previous studies have demonstrated that a large WC is a risk factor for both cognitive impairment and dementia in the elderly (13, 16, 33–35). A longitudinal community-based study with an 8-year follow-up period revealed that abdominal obesity in late life carried an increased risk of cognitive impairment. Compared with the low WC tertile, the middle and high WC tertiles were associated with 80 and 90% higher incidence rates of cognitive impairment, respectively (13). In China, a hospital-based study found that abdominal obesity as defined by WHR was an independent risk factor for cognitive impairment (OR 1.532; 95% CI 1.037–2.263) (36). In contrast, we found that a large WC was associated with a decreased prevalence in cognitive impairment in elderly men, independent of sociodemographic, lifestyle, and health-related factors. Each 1-cm increase in WC corresponded to 4.0% decrease in prevalence of cognitive impairment in elderly men. Furthermore, results of two Asian population-based studies are consistent with our findings. One population-based study suggested that abdominal obesity (i.e., WC ≥90 cm for men and ≥80 cm for women) might be a protective factor for cognitive function in the elderly (OR 0.72; 95% CI 0.56–0.92) in the rural area of Shenyang, China (37). In addition, a prospective community-dwelling Korean study illustrated that WC had a U-shaped correlation with cognitive function in the elderly, and increased central obesity over time as assessed using WC and WHR was associated with better cognitive function in elderly men (18).
In addition to obesity indicators, other cardiovascular risk factors, including hypertension, diabetes mellitus, hyperlipidemia, and smoking, have been linked with cognitive decline in adults (38–40). In our previous studies, a high blood pressure proved to be a risk factor for cognitive impairment (9, 19). However, there was no association between diabetes and cognitive impairment in this population (9, 19). Previous studies have reported that hyperlipidemia is associated with cognitive impairment (41, 42). Several studies suggested both WC and BMI were ideal indicators for hyperlipidemia (43, 44). A cross-sectional study found BMI and WC were comparable to body fat mass in identifying metabolic risk factors including hyperlipidemia (45). In present study, after adjusting for hyperlipidemia and other confounding factors, BMI and WC were associated with cognitive decline in elderly women and men, respectively.
In this study, there were different associations between obesity and cognitive function according to sex. Obesity appears to be protective for cognitive function only in elderly men, not elderly women. Several mechanisms may account for these results. First, female sex is a risk factor for cognitive decline (9). Women are more likely to develop central obesity in this population. Second, testosterone is an important neuroprotective hormone, as it decreases the accumulation of amyloid β-protein and inhibits the hyperphosphorylation of tau (46). Men are likely to maintain more testosterone in body fat, which may prevent cognitive decline (47). Third, in rural China, men tend to obtain higher educational levels, have more social contact, and be less depressed. Therefore, they are more likely to seek cognitive rehabilitation to improve cognitive disorders.
There are several limitations in this study. First, the study population was from a low-income, low-education rural population in northern China; thus, its representation and generalizability are limited. Second, cognitive impairment was evaluated with MMSE scores; therefore, different types of cognitive impairment could not be further diagnosed in the study. Third, other confounding factors, including apolipoprotein E genotype, frailty, and diet, are important factors for cognitive decline but were not assessed in this study because of limited funding. In the future, we plan to conduct a study including physical capability markers. Fourth, this was a cross-sectional study; thus, causal relationships could not be established. A prospective cohort study will be conducted using this study as reference.
A higher WC was positively associated with better cognitive function in low-income elderly men in rural China, whereas a higher BMI was associated with increased cognitive impairment in low-income elderly women in China, independent of sociodemographic, lifestyle, and health-related comorbid factors. The beneficial effects of obesity on cognitive impairment seemed to be applicable to elderly men, not women. Our results suggest weight management of elderly women in rural China may have cognitive benefits. However, randomized controlled trials would be needed to confirm causality.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Tianjin Medical University General Hospital. The patients/participants provided their written informed consent to participate in this study.
JW, XN, and YS contributed to the study design, performed data collection, data interpretation, and critical review. JW performed data analysis. DG, XZ, and CZ contributed to drafting of the article. DG, XZ, CZ, QL, JL, QY, and JT performed data collection, case diagnoses, and confirmation of case diagnoses. All authors read, revised, and approved the final version of the paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1859–922. doi: 10.1016/S0140-6736(18)32335-3
2. Wortmann M. Dementia: a global health priority - highlights from an ADI and World Health Organization report. Alzheimers Res Ther. (2012) 4:40. doi: 10.1186/alzrt143
3. World Alzheimer Report 2019. Attitudes to Dementia. Available online at: https://www.alzint.org/resource/world-alzheimer-report-2019/ (accessed on May 1, 2020).
4. Ding D, Zhao Q, Wu W, Xiao Z, Liang X, Luo J, et al. Prevalence and incidence of dementia in an older Chinese population over two decades: the role of education. Alzheimers Dement. (2020) 16:1650–62. doi: 10.1002/alz.12159
5. Jia J, Wang F, Wei C, Zhou A, Jia X, Li F, et al. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. (2014) 10:1–9. doi: 10.1016/j.jalz.2013.01.012
6. Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. (2008) 32:1431–7. doi: 10.1038/ijo.2008.102
7. Zhang X, Zhang M, Zhao Z, Huang Z, Deng Q, Li Y, et al. Geographic variation in prevalence of adult obesity in China: results from the 2013-2014 national chronic disease and risk factor surveillance. Ann Intern Med. (2020) 172:291–3. doi: 10.7326/M19-0477
8. Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. (2011) 10:819–28. doi: 10.1016/S1474-4422(11)70072-2
9. Ren L, Bai L, Wu Y, Ni J, Shi M, Lu H, et al. Prevalence of and risk factors for cognitive impairment among elderly without cardio- and cerebrovascular diseases: a population-based study in rural China. Front Aging Neurosci. (2018) 10:62. doi: 10.3389/fnagi.2018.00062
10. West NA, Lirette ST, Cannon VA, Turner ST, Mosley TH Jr, Windham BG. Adiposity, change in adiposity, and cognitive decline in mid- and late life. J Am Geriatr Soc. (2017) 65:1282–8. doi: 10.1111/jgs.14786
11. Hartanto A, Yong JC, Toh WX. Bidirectional associations between obesity and cognitive function in midlife adults: a longitudinal study. Nutrients. (2019) 11:2343. doi: 10.3390/nu11102343
12. Dye L, Boyle NB, Champ C, Lawton C. The relationship between obesity and cognitive health and decline. Proc Nutr Soc. (2017) 76:443–54. doi: 10.1017/S0029665117002014
13. West NA, Haan MN. Body adiposity in late life and risk of dementia or cognitive impairment in a longitudinal community-based study. J Gerontol A Biol Sci Med Sci. (2009) 64:103–9. doi: 10.1093/gerona/gln006
14. Vidyanti AN, Hardhantyo M, Wiratama BS, Prodjohardjono A, Hu CJ. Obesity is less frequently associated with cognitive impairment in elderly individuals: a cross-sectional study in Yogyakarta, Indonesia. Nutrients. (2020) 12:367. doi: 10.3390/nu12020367
15. Zhang J, Tang G, Xie H, Wang B, He M, Fu J, et al. Higher adiposity is associated with slower cognitive decline in hypertensive patients: secondary analysis of the china stroke primary prevention trial. J Am Heart Assoc. (2017) 6:e005561. doi: 10.1161/JAHA.117.005561
16. Benito-León J, Mitchell AJ, Hernández-Gallego J, Bermejo-Pareja F. Obesity and impaired cognitive functioning in the elderly: a population-based cross-sectional study (NEDICES). Eur J Neurol. (2013) 20:899–906. doi: 10.1111/ene.12083
17. Papachristou E, Ramsay SE, Lennon LT, Papacosta O, Iliffe S, Whincup PH, et al. The relationships between body composition characteristics and cognitive functioning in a population-based sample of older British men. BMC Geriatr. (2015) 15:172. doi: 10.1186/s12877-015-0169-y
18. Han C, Jo SA, Seo JA, Kim BG, Kim NH, Jo I, et al. Adiposity parameters and cognitive function in the elderly: application of “Jolly Fat” hypothesis to cognition. Arch Gerontol Geriatr. (2009) 49:e133–133e138. doi: 10.1016/j.archger.2008.11.005
19. Liu W, Wu Y, Bai L, Ni J, Tu J, Liu J, et al. Sex differences in the prevalence of and risk factors for nonvascular cognitive function in rural, low-income elderly in Tianjin, China. Neuroepidemiology. (2018) 51:138–48. doi: 10.1159/000490496
20. Zhang L, Li JL, Zhang LL, Guo LL, Li H, Yan W, et al. Relationship between adiposity parameters and cognition: the “fat and jolly” hypothesis in middle-aged and elderly people in China. Medicine. (2019) 98:e14747. doi: 10.1097/MD.0000000000014747
21. Wang J, Ning X, Yang L, Tu J, Gu H, Zhan C, et al. Sex differences in trends of incidence and mortality of first-ever stroke in rural Tianjin, China, from 1992 to 2012. Stroke. (2014) 45:1626–31. doi: 10.1161/STROKEAHA.113.003899
22. Hu Y, Zhao L, Zhang H, Yu X, Wang Z, Ye Z, et al. Sex Differences in the recurrence rate and risk factors for primary giant cell tumors around the knee in China. Sci Rep. (2016) 6:28173. doi: 10.1038/srep28173
23. Canadian Task Force on Preventive Health Care, Pottie K, Rahal R, Jaramillo A, Birtwhistle R, Thombs BD. Recommendations on screening for cognitive impairment in older adults. CMAJ. (2016) 188:37–46. doi: 10.1503/cmaj.141165
24. Nunes B, Silva RD, Cruz VT, Roriz JM, Pais J, Silva MC. Prevalence and pattern of cognitive impairment in rural and urban populations from Northern Portugal. BMC Neurol. (2010) 10:42. doi: 10.1186/1471-2377-10-42
25. Box GEP, Tidwell PW. Transformation of the independent variables. Technometrics. (1962) 4:531–50.
26. Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res. (2016) 118:1752–70. doi: 10.1161/CIRCRESAHA.115.306883
27. Kim S, Kim Y, Park SM. Body mass index and decline of cognitive function. PLoS ONE. (2016) 11:e0148908. doi: 10.1371/journal.pone.0148908
28. Tikhonoff V, Casiglia E, Guidotti F, Giordano N, Martini B, Mazza A, et al. Body fat and the cognitive pattern: a population-based study. Obesity. (2015) 23:1502–10. doi: 10.1002/oby.21114
29. Ghaderpanahi M, Fakhrzadeh H, Sharifi F, Mirarefin M, Badamchizade Z, Larijani B, et al. Association between late-life body mass index, waist circumference, and dementia: Kahrizak Elderly Study. J Am Geriatr Soc. (2012) 60:173–4. doi: 10.1111/j.1532-5415.2011.03751.x
30. Qizilbash N, Gregson J, Johnson ME, Pearce N, Douglas I, Wing K, et al. BMI and risk of dementia in two million people over two decades: a retrospective cohort study. Lancet Diabetes Endocrinol. (2015) 3:431–6. doi: 10.1016/S2213-8587(15)00033-9
31. Danat IM, Clifford A, Partridge M, Zhou W, Bakre AT, Chen A, et al. Impacts of overweight and obesity in older age on the risk of dementia: a systematic literature review and a meta-analysis. J Alzheimers Dis. (2019) 70:S87–99. doi: 10.3233/JAD-180763
32. Rankinen T, Kim SY, Pérusse L, Després JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat Metab Disord. (1999) 23:801–9. doi: 10.1038/sj.ijo.0800929
33. Masi S, Georgiopoulos G, Khan T, Johnson W, Wong A, Charakida M, et al. Patterns of adiposity, vascular phenotypes and cognitive function in the 1946 British Birth Cohort. BMC Med. (2018) 16:75. doi: 10.1186/s12916-018-1059-x
34. Fergenbaum JH, Bruce S, Lou W, Hanley AJ, Greenwood C, Young TK. Obesity and lowered cognitive performance in a Canadian First Nations population. Obesity. (2009) 17:1957–63. doi: 10.1038/oby.2009.161
35. Yao Q, Jiang GX, Zhou ZM, Chen JM, Cheng Q. Metabolic syndrome and mild cognitive impairment: a case-control study among elderly in a Shanghai Suburb. J Alzheimers Dis. (2016) 51:1175–82. doi: 10.3233/JAD-150920
36. Hou Q, Guan Y, Yu W, Liu X, Wu L, Xiao M, et al. Associations between obesity and cognitive impairment in the Chinese elderly: an observational study. Clin Interv Aging. (2019) 14:367–73. doi: 10.2147/CIA.S192050
37. Wang X, Luan D, Xin S, Liu Y, Gao Q. Association Between Individual Components of Metabolic Syndrome and Cognitive Function in Northeast Rural China. Am J Alzheimers Dis Other Demen. (2019) 34:507–12. doi: 10.1177/1533317519865428
38. Lourenco J, Serrano A, Santos-Silva A, Gomes M, Afonso C, Freitas P, et al. Cardiovascular Risk Factors Are Correlated with Low Cognitive Function among Older Adults Across Europe Based on The SHARE Database. Aging Dis. (2018) 9:90–101. doi: 10.14336/AD.2017.0128
39. Yaffe K, Bahorik AL, Hoang TD, Forrester S, Jacobs DR Jr, Lewis CE, et al. Cardiovascular risk factors and accelerated cognitive decline in midlife: The CARDIA Study. Neurology. (2020) 95:e839–839e846. doi: 10.1212/WNL.0000000000010078
40. Yaffe K, Vittinghoff E, Hoang T, Matthews K, Golden SH, Zeki Al Hazzouri A. Cardiovascular risk factors across the life course and cognitive decline: a pooled cohort study. Neurology. (2021) 96:e2212–9. doi: 10.1212/WNL.0000000000011747
41. Zhao B, Shang S, Li P, Chen C, Dang L, Jiang Y, et al. The gender- and age- dependent relationships between serum lipids and cognitive impairment: a cross-sectional study in a rural area of Xi'an, China. Lipids Health Dis. (2019) 18:4. doi: 10.1186/s12944-018-0956-5
42. Zou Y, Zhu Q, Deng Y, Duan J, Pan L, Tu Q, et al. Vascular risk factors and mild cognitive impairment in the elderly population in Southwest China. Am J Alzheimers Dis Other Demen. (2014) 29:242–7. doi: 10.1177/1533317513517042
43. Zhang P, Sun X, Jin H, Zhang FL, Guo ZN, Yang Y. Association between obesity type and common vascular and metabolic diseases: a cross-sectional study. Front Endocrinol. (2019) 10:900. doi: 10.3389/fendo.2019.00900
44. Lee BJ, Yim MH. Comparison of anthropometric and body composition indices in the identification of metabolic risk factors. Sci Rep. (2021) 11:9931. doi: 10.1038/s41598-021-89422-x
45. Bosy-Westphal A, Geisler C, Onur S, Korth O, Selberg O, Schrezenmeir J, et al. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes. (2006) 30:475–83. doi: 10.1038/sj.ijo.0803144
46. Papasozomenos SC. The heat shock-induced hyperphosphorylation of tau is estrogen-independent and prevented by androgens: implications for Alzheimer disease. Proc Natl Acad Sci USA. (1997) 94:6612–7. doi: 10.1073/pnas.94.13.6612
Keywords: cognitive impairment, obesity, body mass index, waist circumstance, sex difference
Citation: Guo D, Zhang X, Zhan C, Lin Q, Liu J, Yang Q, Tu J, Ning X, Wang J and Song Y (2021) Sex Differences in the Association Between Obesity and Cognitive Impairment in a Low-Income Elderly Population in Rural China: A Population-Based Cross-Sectional Study. Front. Neurol. 12:669174. doi: 10.3389/fneur.2021.669174
Received: 18 February 2021; Accepted: 10 June 2021;
Published: 09 July 2021.
Edited by:
Seana Gall, University of Tasmania, AustraliaReviewed by:
Senthil Selvaraj, Sidra Medicine, QatarCopyright © 2021 Guo, Zhang, Zhan, Lin, Liu, Yang, Tu, Ning, Wang and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianjia Ning, eG5pbmdAdG11LmVkdS5jbg==; Jinghua Wang, andhbmczQHRtdS5lZHUuY24=; Yijun Song, c29uZ3lqQHRtdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.