
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 31 May 2021
Sec. Endovascular and Interventional Neurology
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.606673
This article is part of the Research Topic Advances in the Endovascular Treatment for Cerebrovascular Diseases and its Complications View all 31 articles
 Sheng-Ta Tsai1,2†
Sheng-Ta Tsai1,2† Wei-Chun Wang1,2†
Wei-Chun Wang1,2† Yu-Ting Lin3,4
Yu-Ting Lin3,4 Wei-Shih Huang1,2
Wei-Shih Huang1,2 Hung-Yu Huang1
Hung-Yu Huang1 Chun-Ju Wang1
Chun-Ju Wang1 En-Zu Lin5
En-Zu Lin5 Wei-Ling Kung6
Wei-Ling Kung6 Yuh-Cherng Guo1,2
Yuh-Cherng Guo1,2 Kang-Hsu Lin1,2
Kang-Hsu Lin1,2 Ming-Kuei Lu1,2,7
Ming-Kuei Lu1,2,7 Pao-Sheng Yen8
Pao-Sheng Yen8 Wei-Laing Chen9
Wei-Laing Chen9 Ying-Lin Tseng9
Ying-Lin Tseng9 Chin-Chi Kuo2,3,10
Chin-Chi Kuo2,3,10 Der-Yang Cho5,11
Der-Yang Cho5,11 Chun-Chung Chen5,11
Chun-Chung Chen5,11 Chon-Haw Tsai1,2,7*
Chon-Haw Tsai1,2,7*Background: In most countries, large cerebral artery occlusion is identified as the leading cause of disability. In 2015, five large-scale clinical trials confirmed the benefit of intra-arterial thrombectomy. However, thrombectomy is a highly technical and facility-dependent procedure. Primary stroke centers need to transfer patients to comprehensive stroke centers to perform thrombectomy. The time-lapse during interhospital transfer would decrease the chance of the patient's proper recovery. Communication barriers also contribute to this delay.
Aims: We used a smartphone application to overcome communication barriers between hospitals. We aimed to shorten the door-to-puncture time of interhospital transfer patients.
Methods: We began using a smartphone application, “LINE,” to facilitate interhospital communication on May 01, 2018. We carried out retrospective data analyses for all the transfer patients (n = 351), with the primary outcome being the door-to-puncture time in our comprehensive stroke center (China Medical University Hospital). We compared the three periods: May 01 to Dec 31, 2017 (before the use of the smartphone application); May 01 to Dec 31, 2018 (the 1st year of using the smartphone application); and May 01 to Dec 31, 2019 (the 2nd year of using the smartphone application). We also compared the transfer data with non-transfer thrombectomies in the same period.
Results: We compared 2017, 2018, and 2019 data. The total number of transfer patients increased over the years: 63, 113, 175, respectively. The mean door-to-puncture time decreased significantly, going from 109, through 102, to 92 min. Meanwhile, the mean door-to-puncture time in non-transfer patients were 140.3, 122.1, and 129.3 min. The main reason of time saving was the change of the way of communication, from point-to-point interhospital communication to hub-to-spoke interhospital communication.
Conclusions: We used this smartphone application to enhance interhospital communication, changed from the point-to-point to hub-to-spoke method. It made us overcome the communication barrier and build up interhospital connection, thus shortening the door-to-puncture time. Our experience demonstrated the importance of close communication and teamwork in hyperacute stroke care, especially in interhospital transfer for thrombectomy.
Stroke has been identified as one of the leading causes of morbidity and mortality around the world (1). Large vessel occlusion (LVO) is the most devastating form of stroke (2, 3). About the definition of LVO, we used the broad definition that included internal carotid artery (ICA), the first segment of the middle cerebral artery (M1), the second segment of the middle cerebral artery (M2), the basilar artery (BA), anterior cerebral artery (ACA), posterior cerebral artery (PCA), and vertebral artery (VA) occlusions (4). Every 1-min delay of recanalization will lead to the death of 1.9 million neurons (5). Thus, it is crucial to save the brain immediately (6–8). The most modifiable factor in salvaging the brain is door-to-puncture (DTP) time (9).
In 2015, five large-scale clinical trials confirmed the benefits of intra-arterial thrombectomy (10–14). However, thrombectomy is deemed as a highly technical and facility-dependent procedure (15). Thrombectomy capabilities are not exclusive to comprehensive stroke centers. The time-lapse during interhospital transfer would then decrease the chance of adequate recovery of patients (16–18).
There are many factors affecting the timeliness of interhospital transfer of patients for thrombectomy (19). Previous research reported that interhospital communication barriers are a major cause of time delay (20). Several teams have developed smartphone applications in order to facilitate communication (20, 21).
In Taiwan, the most popular smartphone application for social communication is “LINE.” In 2019, “LINE” had over 21 million users in Taiwan (89% of the total population, 23.6 million) (22), with each user spending more than 1 h on it per day (23).
As a result, after several interhospital transfer meetings with primary stroke centers, we created an encrypted group in “LINE” in order to overcome communication barriers and speed up the workflow of thrombectomy.
We aimed to decrease the DTP time in the comprehensive stroke center (China Medical University Hospital) by using this smartphone application called “LINE” to facilitate communication between doctors. We also supposed that the percentage of patients with good outcomes would increase (modified Rankin Scale = 0, 1, or 2 at 3 months) (24).
The China Medical University Hospital (CMUH) is a Medical Center in central Taiwan, with a total of 2,054 beds. The stroke center had 21 attending physicians, 16 residents, and 3 nurse practitioners. We had 55 ordinary beds and 10 intensive care unit beds. Our stroke center got the Joint Commission International accreditation in 2010. Each year, we had around 1,300 acute ischemic stroke patients, 90 tissue plasminogen activator thrombolyses, and 120 intra-arterial thrombectomies. We are a tertiary referral center in central Taiwan, receiving transfer patients from 38 primary stroke centers, with the distance of transfer ranging from 1.8 to 126 km (Supplementary Table 1 and Figure 1).
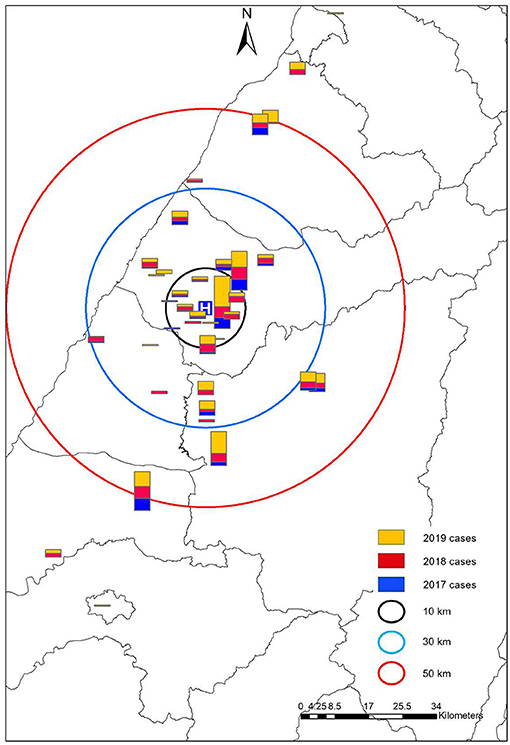
Figure 1. The geographic distribution of primary stroke centers and the interhospital transfer cases. We found an increasing number of transfers in almost all the hospitals, irrespective of the distance.
“LINE” has been determined to be the most commonly used social smartphone application in Taiwan. The application used LINE Event Delivery Gateway (LEGY) to encrypt messages and protect the privacy of its users. The LINE company got the International Organization for Standardization (ISO) ISO 27001 accreditation for information security in 2007. They also got the accreditation of Service Organization Controls (SOC) SOC2, SOC3, and SysTrust (25).
The neurologists at the CMUH created an encrypted group for interhospital transfer and invited the neurologists, emergency department doctors, or nurse practitioners in the primary stroke centers. Patients' identification details such as name and chart number have to be deleted during communication. A screenshot of one real communication was taken from the “LINE” smartphone application as an example (Figure 2).

Figure 2. A real communication on the “LINE” smartphone application. “A 67-year-old hypertensive male who took aspirin every day. He developed sudden-onset weakness of the left limbs and slurred speech, with NIHSS = 12. The EKG revealed atrial fibrillation. Ask for transfer”.
CMUH set up the comprehensive stroke center in February 2007. We provided thrombolysis and thrombectomy services 365 days a year, 24 h a day. We followed the treatment guidelines of the Taiwan Stroke Society (26, 27). Our workflow for interhospital transfer of patients has been summarized in Figure 3.
We began using the smartphone application known as “LINE” to facilitate interhospital communication on May 01, 2018. We then performed retrospective data analysis for all transfer patients (n = 351) during the study period, with the primary outcome being the DTP time at CMUH. The three periods are then compared: May 01 to Dec 31, 2017 (before the use of the smartphone application); May 01 to Dec 31, 2018 (the 1st year of using the smartphone application); and May 01 to Dec 31, 2019 (the 2nd year of using the smartphone application). We chose the same period of comparison to eliminate other confounding factors such as weather [especially atmospheric pressure (28)] and the experience of first-line residents (our resident started visiting acute ischemic stroke patients at the emergency department after 16 months training in the neurology department, often started in January; they might attain minimal time-lapses in the first 3 to 4 months).
We also collected the similar data for the “non-transfer” (or “front door arrival”) thrombectomies in the same three periods, that means the patients were directly presented to our emergency department without an interhospital transfer. By comparison, we could eliminate other factors such as overall improvement in the thrombectomy workflow, or the gain of more experience over time in the thrombectomy team members.
This study was able to secure an ethical approval from CMUH, CMUH109-REC3-099.
The primary outcome in this study is the DTP of interhospital transfer and non-transfer thrombectomy cases. We have also calculated the total number of transfers, total thrombectomies, successful recanalization rate (modified TICI score (29) = 2b, 2c, and 3), symptomatic intracerebral hemorrhage rate, and the percentage of good outcomes (modified Rankin scale (30) = 0, 1, or 2 at 3 months).
The characteristics of this study population have been expressed as the mean (standard deviation [SD]) for continuous variables and frequency (percentage) for categorical variables. We used the one-way ANOVA and χ2 tests to calculate p-values for continuous and categorical variables, respectively. Moreover, p-values for trends (31) were calculated using Pearson's correlation for continuous variables and Cochran-Armitage trend test for dichotomous variables. All statistical analyses were performed using SAS (SAS Institute, Cary, NC, USA), version 9.4. The threshold for statistical significance was set at P = 0.05 based on a two-sided test.
We summarized the main results in Tables 1, 2. After the introduction of the “LINE” smartphone application, the total number of transfer cases increased from 63 to 113 and then to 175. We stratified by the distance of transfer and found consistently increasing numbers (Figure 1). The total number of thrombectomies has also increased. Between the three periods, the basic characteristics of transfer patients, including age, gender, initial NIH Stroke Scale (NIHSS), and time of arrival at work hour (8:00 A.M. to 5:00 P.M., Monday to Friday) were similar. The primary outcome was the DTP time, which decreased from 109.3 to 102.4 min and then 92 min (p = 0.045), showing a significant decreasing trend (P = 0.013). We also observed that the rate of successful reperfusion exhibited a significant increasing trend through the years (P = 0.033) (Table 1). However, there was no significant difference between the symptomatic intracerebral hemorrhage and the percentage of good outcomes over the years.
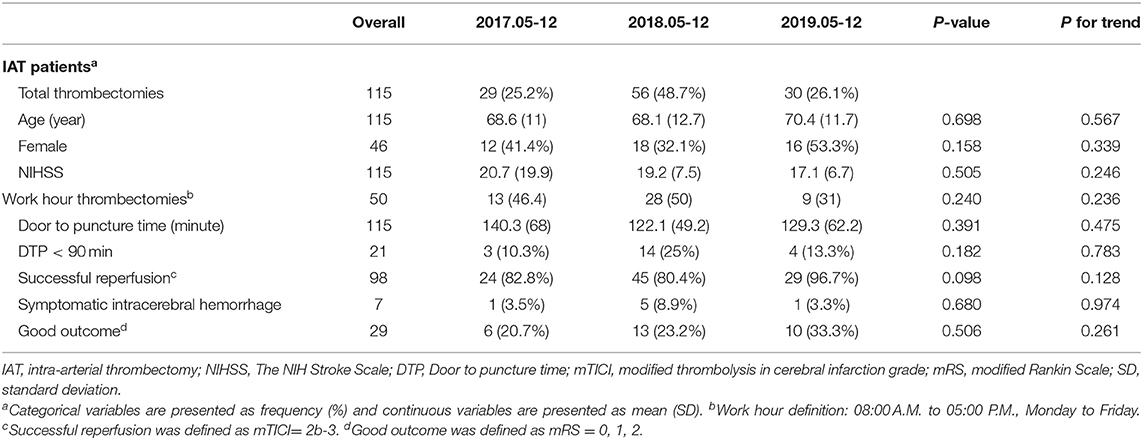
Table 2. Characteristics of non-transfer cases with intra-arterial thrombectomy of the three periods.
We put the data of non-transfer patients in Table 2, and the DTP times were 140.3, 122.1, and 129.3 min, respectively, with P-value of 0.391. It did not have the similar decreasing trend as the transfer patients. We could also find a trend of increased successful reperfusion rate in 2019, but the data did not reach statistical significance (P = 0.098).
The distance during our interhospital transfer ranges from 1.8 to 126 km. We did the subgroup analysis between short and long transfer distance, divided by the mean transfer distance, 35 km (Table 3). The result didn't show significant difference between these two groups, including DTP time, successful reperfusion, symptomatic intracerebral hemorrhage, and good functional outcome.
In large artery ischemic stroke, every 10-min delay of recanalization can decrease one's chance of functional independence per 100 patients treated (32). It is very important to treat the stroke patient immediately.
We used the smartphone application called “LINE” to shorten the DTP time. The main benefit is to overcome the communication barriers between hospitals and our stroke team members (20). The biggest change was the way of communication, from phone-base-point-to-point to LINE-base-hub-to-spoke (Figure 4). Before the introduction of smartphone application, the neurologists in primary stroke centers needed to present their situation to the emergency department doctor or nurse practitioner. Then the doctor or nurse practitioner repeated the words and made a phone call to our emergency department. Our emergency staff then made a phone call to our neurologist, repeated the same message (onset time, NIHSS, age, etc.) and asked for availability of thrombectomy. Then our nurse practitioner called back to reply to the emergency department of the primary stroke center. And during these processes, no one could see the patient's image; they only got messages by oral dictation. If our neurologists or intervention radiologist needed more information (such as comorbidities, lab data), then the process would repeat again and waste more time. After we introduced this smartphone application, we invited the neurologists in primary stroke centers, the doctor or nurse practitioner in emergency departments, our neurologists, and intervention radiologists to the encrypted group. All the related people could see the first-hand message delivered by the primary stroke center neurologists. Our team could respond or ask questions immediately. A rapid review of brain images is also available via the application. Then we delivered the final decision to all the members. Meanwhile, every related staff member could start to prepare for the interhospital transfer for thrombectomy. Moreover, we have invited the neurologists in other comprehensive stroke centers into the group so that we can pass a transfer request message to them; that is, we ask directly if any other comprehensive stroke center is available for thrombectomy in case our hospital is full to receive a second transfer patients or there are simultaneous stoke activations in two different primary stroke centers (Figure 5). Because the patient's information is posted on the same group, it is not necessary to be repeated by the primary stroke center and thus prevents time wasting.
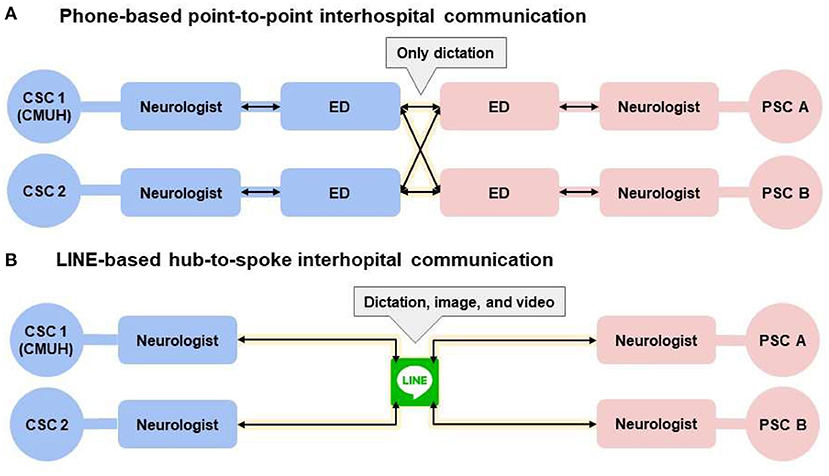
Figure 4. The way of communication changed by smartphone application, LINE. (A) Indicates the original way of communication. Doctor or nurse practitioner in each hospital needed to communicate by phone call. (B) Indicates the novel way of communication. All the related staff could see the message at the same time, including the dictation, image, or video. We put the circle of CSC2, because sometimes our hospital could not receive the transfer patients. For example, we are doing another thrombectomy or stoke activations in two different primary stroke centers. We invited the neurologists in CSC2 to let them know the need of transfer immediately if we could not receive the PSC patients. CSC, comprehensive stroke center; ED, emergency department; PSC, primary stroke center.
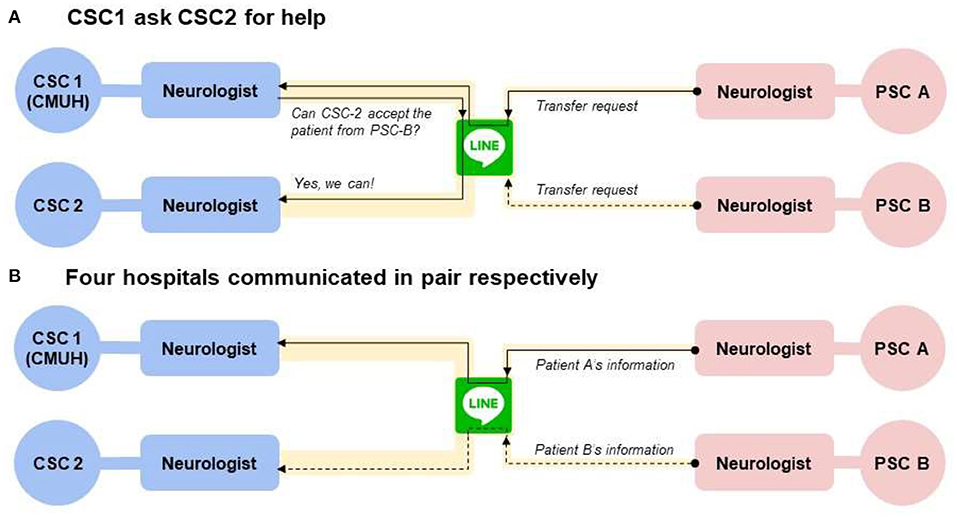
Figure 5. The way of communication if there are simultaneous stoke activations in two different primary stroke centers. (A) Indicates the way CSC1 (our hospital) asked CSC2 for help. If CSC2 was available for thrombectomy, they would send the message on “Line” and both the CSC1 and PSC B could see it. Then the process moved to the (B), that PSC A communicated with CSC1, and PSC B communicated with CSC2, respectively. CSC, comprehensive stroke center; ED, emergency department; PSC, primary stroke center.
A team member at Massachusetts General Hospital Telestroke Network found a frequent contact as this hub-to-spoke method is associated with improved stroke care (33). The hub-to-spoke organization design was used in the healthcare industry to serve patients better (34). And in the hospitals' perspectives, hub-to-spoke telestroke networks are cost-effective in acute stroke management (35, 36).
In addition, it has decreased the time needed to obtain informed consent from the family of the patient, because we sent the important message of thrombectomy to the primary stroke center through a smartphone application. The procedure could then be explained while the patient is waiting for the transfer. In the previous thrombolysis research in south Taiwan, obtaining informed consent was identified as one of the most important factors causing delay (37). In addition, failure to obtain informed consent was the reason why 21.1% of the eligible patients did not receive tissue plasminogen thrombolysis (38).
In 2007, our hospital set up the stroke center and further organized the emergency department, neurology department, and radiology department to improve the quality of thrombolysis and thrombectomy. We performed the first thrombectomy in 2008. After the five large-scale clinical trials in 2015, we started to have annual training of the NIHSS and hold monthly interdepartmental committee meetings to discuss the thrombectomy cases and try to reduce the DTP time (39). However, the reduction of DTP time remains to be limited. The DTP time at the same three periods in the non-transfer patients was 140.3 min in 2017, 122.1 min in 2018, and 129.3 min in 2019 (Table 2). The data convinced us that the significant improvement meant that the DTP time in transfer patients is different from that of the non-transfer [or “front door arrival” (40)] patients. This improvement might then be accounted for by the smartphone application use in interhospital communication, rather than the overall improvement in the thrombectomy workflow, or the gain of more experience over time in the thrombectomy team members.
We also found the rate of successful reperfusion (mTICI = 2b-3) was 97.1% (in transfer patients) and 96.7% (non-transfer patients) in 2019, which might have contributed to the introduction of novel thrombectomy techniques and devices. That is “a direct aspiration first pass technique (ADAPT)” (41) by contact aspiration (42) catheters, such as ACE 068, and Sofia Plus.
Although we had a shorter DTP time and a higher percentage of successful reperfusion, the percentage of good outcomes did not significantly increase. The reason for this could be the relatively small sample we used.
The major limitation of our study was the use of a commercially available smartphone application “LINE.” Although the company passed the accreditation for information security (ISO 27001, SOC2, SOC3, and SysTrust) (25), it is not an application designed solely for medical information transfer. We then used the encrypted function of the application but still did not have full control of the data. We will develop novel smartphone applications for interhospital transfer in the future to overcome this hindrance.
Another limitation is the lack of exact transfer time, because we didn't collect the data recorded in the emergent medical service system. But a previous study (43) demonstrated that the transfer time was directly correlated with the hospital-to-hospital distance. We did the subgroup analysis according to short and long transfer distance (divided by the mean transfer distance, as 35 km), and we found the distance of interhospital transfer did not confound our results (Table 3).
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by China Medical University Hospital, CMUH109-REC3-099. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
S-TT, W-CW, and W-SH: study conception and design. Y-TL and C-CK: analysis and interpretation of data. S-TT and W-CW: drafting the article. H-YH, C-JW, E-ZL, W-LK, P-SY, W-LC, and Y-LT: substantial acquisition of data for the study. Y-CG, K-HL, and M-KL: revising the article. D-YC, C-CC, and C-HT: general supervision of the research project. All authors contributed to the article and approved the submitted version.
The study was supported in part by grants from the Ministry of Science and Technology (MOST 107-2314-B-039−017-MY3, MOST 108-2314-B-039−038-MY3, MOST 109-2321-B-468−001), and China Medical University Hospital (DMR-106-180, DMR-107-189, DMR-110-218).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank the Department of Medical Research and Big Data Center at China Medical University Hospital for conducting the data management and analysis for this study. We thank doctor Cheng-Yang Hsieh for external consultation. And we thank Enago (www.enago.tw) for the English language review.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.606673/full#supplementary-material
1. Hsieh FI, Lien LM, Chen ST, Bai CH, Sun MC, Tseng HP, et al. Get with the guidelines-stroke performance indicators: surveillance of stroke care in the taiwan stroke registry: get with the guidelines-stroke in Taiwan. Circulation. (2010) 122:1116–23. doi: 10.1161/circulationaha.110.936526
2. Seder DB, Mayer SA. Critical care management of subarachnoid hemorrhage and ischemic stroke. Clin Chest Med. (2009) 30:103–22. doi: 10.1016/j.ccm.2008.11.004
3. Zahuranec DB, Majersik JJ. Percentage of acute stroke patients eligible for endovascular treatment. Neurology. (2012) 79:S22–5. doi: 10.1212/WNL.0b013e31826957cf
4. Waqas M, Mokin M, Primiani CT, Gong AD, Rai HH, Chin F, et al. Large vessel occlusion in acute ischemic stroke patients: a dual-center estimate based on a broad definition of occlusion site. J Stroke Cerebrovasc Dis. (2020) 29:104504. doi: 10.1016/j.jstrokecerebrovasdis.2019.104504
5. Saver Jeffrey L. Time is brain—quantified. Stroke. (2006) 37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab
6. Meretoja A, Keshtkaran M, Tatlisumak T, Donnan GA, Churilov L. Endovascular therapy for ischemic stroke: save a minute-save a week. Neurology. (2017) 88:2123–7. doi: 10.1212/wnl.0000000000003981
7. Mulder MJHL, Jansen IGH, Goldhoorn R-JB, Venema E, Chalos V, Compagne KCJ, et al. Time to endovascular treatment and outcome in acute ischemic stroke. Circulation. (2018) 138:232–40. doi: 10.1161/CIRCULATIONAHA.117.032600
8. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. (2016) 316:1279–88. doi: 10.1001/jama.2016.13647
9. Jahan R, Saver JL, Schwamm LH, Fonarow GC, Liang L, Matsouaka RA, et al. association between time to treatment with endovascular reperfusion therapy and outcomes in patients with acute ischemic stroke treated in clinical practice. JAMA. (2019) 322:252–63. doi: 10.1001/jama.2019.8286
10. Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic stroke. N Engl J Med. (2014) 372:11–20. doi: 10.1056/NEJMoa1411587
11. Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. (2015) 372:1009–18. doi: 10.1056/NEJMoa1414792
12. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. (2015) 372:1019–30. doi: 10.1056/NEJMoa1414905
13. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. (2015) 372:2296–306. doi: 10.1056/NEJMoa1503780
14. Saver JL, Goyal M, Bonafe A, Diener H-C, Levy EI, Pereira VM, et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA alone in stroke. (2015) 372:2285–95. doi: 10.1056/NEJMoa1415061
15. Papanagiotou P, Ntaios G. Endovascular thrombectomy in acute ischemic stroke. Circ Cardiovasc Interv. (2018) 11:e005362. doi: 10.1161/circinterventions.117.005362
16. Froehler MT, Saver JL, Zaidat OO, Jahan R, Aziz-Sultan MA, Klucznik RP, et al. Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the STRATIS registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke). Circulation. (2017) 136:2311–21. doi: 10.1161/circulationaha.117.028920
17. Regenhardt RW, Mecca AP, Flavin SA, Boulouis G, Lauer A, Zachrison KS, et al. Delays in the air or ground transfer of patients for endovascular thrombectomy. Stroke. (2018) 49:1419–25. doi: 10.1161/strokeaha.118.020618
18. Venema E, Groot AE, Lingsma HF, Hinsenveld W, Treurniet KM, Chalos V, et al. Effect of interhospital transfer on endovascular treatment for acute ischemic stroke. Stroke. (2019) 50:923–30. doi: 10.1161/STROKEAHA.118.024091
19. Ng FC, Low E, Andrew E, Smith K, Campbell BCV, Hand PJ, et al. Deconstruction of interhospital transfer workflow in large vessel occlusion: real-world data in the thrombectomy era. Stroke. (2017) 48:1976–9. doi: 10.1161/strokeaha.117.017235
20. Alotaibi NM, Sarzetto F, Guha D, Lu M, Bodo A, Gupta S, et al. Impact of smartphone applications on timing of endovascular therapy for ischemic stroke: a preliminary study. World Neurosurg. (2017) 107:678–83. doi: 10.1016/j.wneu.2017.08.042
21. Martins SCO, Weiss G, Almeida AG, Brondani R, Carbonera LA, Souza ACd, et al. Validation of a smartphone application in the evaluation and treatment of acute stroke in a comprehensive stroke center. Stroke. (2020) 51:240–6. doi: 10.1161/STROKEAHA.119.026727
22. Corporate Announcement. Available online at: https://linecorp.com/zh-hant/pr/news/zh-hant/2019/2651 (accessed March 29, 2019).
23. Corporate Announcement. Available online at: https://linecorp.com/zh-hant/pr/news/zh-hant/2020/3308 (accessed July 13, 2020).
24. Fuentes B, Alonso de Leciñana M, Ximénez-Carrillo A, Martínez-Sánchez P, Cruz-Culebras A, Zapata-Wainberg G, et al. Futile interhospital transfer for endovascular treatment in acute ischemic stroke: the madrid stroke network experience. Stroke. (2015) 46:2156–61. doi: 10.1161/strokeaha.115.009282
25. Liu D. Line Safe and Security. (2017). Available pnline at: https://engineering.linecorp.com/zh-hant/blog/line-safty-security/ (accessed April 21, 2017).
26. Chen CH, Sung SF, Hsieh CY, Chen PL, Tsai LK, Huang HY, et al. 2019 Taiwan stroke society guideline for intravenous thrombolysis in acute ischemic stroke patients. Formosan J Stroke. (2019) 1:2019. doi: 10.6318/FJS.201906_1(1)0.0001
27. Tang SC, Chen CJ, Lee CW, Wang KC, Lai YJ, Chi NF, et al. 2019 Taiwan stroke society guideline for endovascular thrombectomy in acute ischemic stroke patients. Formosan J Stroke. (2019) 2:2019. doi: 10.6318/FJS.201909_1(2)0.0001
28. Lee HC, Hu CJ, Chen CS, Lin HC. Seasonal variation in ischemic stroke incidence and association with climate: a six-year population-based study. Chronobiol Int. (2008) 25:938–49. doi: 10.1080/07420520802551469
29. Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. (2016) 387:1723–31. doi: 10.1016/S0140-6736(16)00163-X
30. Swieten JCV, Koudstaal PJ, Visser MC, Schouten HJ, Gijn JV. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. (1988) 19:604–7. doi: 10.1161/01.STR.19.5.604
31. Ingram DD, Malec DJ, Makuc DM, Kruszon-Moran D, Gindi RM, Albert M, et al. National center for health statistics guidelines for analysis of trends. Vital Health Stat. (2018) 2:1–71.
32. Lansberg MG, Schrooten M, Bluhmki E, Thijs VN, Saver JL. Treatment time-specific number needed to treat estimates for tissue plasminogen activator therapy in acute stroke based on shifts over the entire range of the modified Rankin Scale. Stroke. (2009) 40:2079–84. doi: 10.1161/strokeaha.108.540708
33. Moreno A, Schwamm LH, Siddiqui KA, Viswanathan A, Whitney C, Rost N, et al. Frequent hub–spoke contact is associated with improved spoke hospital performance: results from the massachusetts general hospital telestroke network. Telemed e-Health. (2017) 24:678–83. doi: 10.1089/tmj.2017.0252
34. Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res. (2017) 17:457. doi: 10.1186/s12913-017-2341-x
35. Moynihan B, Davis D, Pereira A, Cloud G, Markus HS. Delivering regional thrombolysis via a hub-and-spoke model. J R Soc Med. (2010) 103:363–9. doi: 10.1258/jrsm.2010.090434
36. Switzer JA, Demaerschalk BM, Xie J, Fan L, Villa KF, Wu EQ. Cost-effectiveness of hub-and-spoke telestroke networks for the management of acute ischemic stroke from the hospitals' perspectives. Circ Cardiovasc Qual Outcomes. (2013) 6:18–26. doi: 10.1161/circoutcomes.112.967125
37. Hsieh CY, Chen WF, Chen CH, Wang CY, Chen CJ, Lai EC, et al. Efforts to reduce the door-to-needle time of thrombolysis in acute ischemic stroke: video-assisted therapeutic risk communication. J Formos Med Assoc. (2014) 113:929–33. doi: 10.1016/j.jfma.2013.11.012
38. Huang P, Khor GT, Chen CH, Lin RT, Liu CK. Eligibility and rate of treatment for recombinant tissue plasminogen activator in acute ischemic stroke using different criteria. Acad Emerg Med. (2011) 18:273–8. doi: 10.1111/j.1553-2712.2011.01006.x
39. Ford AL, Connor LT, Tan DK, Williams JA, Lee J-M, Nassief AM. Resident-based acute stroke protocol is expeditious and safe. Stroke. (2009) 40:1512–4. doi: 10.1161/STROKEAHA.108.527770
40. George BP, Pieters TA, Zammit CG, Kelly AG, Sheth KN, Bhalla T. Trends in interhospital transfers and mechanical thrombectomy for United States acute ischemic stroke inpatients. J Stroke Cerebrovasc Dis. (2019) 28:980–7. doi: 10.1016/j.jstrokecerebrovasdis.2018.12.018
41. Vargas J, Spiotta A, Fargen K, Turner R, Chaudry I, Turk A. Long term experience using the ADAPT technique for the treatment of acute ischemic stroke. J NeuroIntervent Surg. (2017) 9:437. doi: 10.1136/neurintsurg-2015-012211
42. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. (2017) 318:443–52. doi: 10.1001/jama.2017.9644%J
Keywords: stroke, thrombectomy, interhospital transfer, door-to-puncture time, communication, smartphone, application, hub-to-spoke
Citation: Tsai S-T, Wang W-C, Lin Y-T, Huang W-S, Huang H-Y, Wang C-J, Lin E-Z, Kung W-L, Guo Y-C, Lin K-H, Lu M-K, Yen P-S, Chen W-L, Tseng Y-L, Kuo C-C, Cho D-Y, Chen C-C and Tsai C-H (2021) Use of a Smartphone Application to Speed Up Interhospital Transfer of Acute Ischemic Stroke Patients for Thrombectomy. Front. Neurol. 12:606673. doi: 10.3389/fneur.2021.606673
Received: 15 September 2020; Accepted: 07 April 2021;
Published: 31 May 2021.
Edited by:
Gustavo J. Rodriguez, Texas Tech University Health Sciences Center El Paso, United StatesReviewed by:
Luis Rafael Moscote-Salazar, University of Cartagena, ColombiaCopyright © 2021 Tsai, Wang, Lin, Huang, Huang, Wang, Lin, Kung, Guo, Lin, Lu, Yen, Chen, Tseng, Kuo, Cho, Chen and Tsai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chon-Haw Tsai, d2luZHltb3ZlbWVudEBnbWFpbC5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.