
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Neurol. , 08 April 2021
Sec. Stroke
Volume 12 - 2021 | https://doi.org/10.3389/fneur.2021.582149
This article is part of the Research Topic Challenges in Posterior Circulation Ischemic Stroke View all 17 articles
Aim: Unilateral vertebral artery hypoplasia is considered a risk factor for posterior circulation infarction. Despite the increasing attention on unilateral vertebral artery hypoplasia, few studies have discussed bilateral vertebral artery hypoplasia, its influence on stroke, or its collateral supply from the circle of Willis. We aimed to identify its characteristics, stroke pattern, and unique ultrasonographic and brain imaging findings.
Materials and Methods: Of the 1,301 consecutive in-patients diagnosed with acute ischemic stroke from January 2013 to December 2015, medical and laboratory data and stroke or transient ischemic attack history were recorded. We enrolled patients who underwent both brain magnetic resonance imaging and sonography examinations. Vertebral artery and posterior cerebral artery analyses were conducted in accordance with clinical criteria.
Results: Adequate imaging data were available for 467 patients. Of these, eight patients met the criteria for bilateral vertebral artery hypoplasia. The mean age was 62.9 ± 12.1 years. There were six male (75.0%) and two female patients (25.0%). A high prevalence of hypertension (7/8, 87.5%) was noted.
Sonograms displayed a very low net flow volume in the vertebral arteries, with the average net flow volume being 28.9 ± 9.7 mL/min. A high frequency (6/8; 75.0%) of the fetal variant posterior cerebral artery from the carotids was found. The infarction patterns in these patients were all bilateral, scattered, and in multiple vascular territories.
Conclusion: Patients with bilateral vertebral hypoplasia displayed a unique collateral supply, special stroke pattern, and younger stroke onset. Early recognition and stroke prevention should be considered critical in clinical practice.
Posterior circulation is comprised of two vertebral arteries that join to form a single basilar artery at the level of the pons. The basilar artery divides into two posterior cerebral arteries at the level of the midbrain (1–3). Conventionally, the major hemodynamics of this area is supplied by the net flow of the vertebral arteries and partially by the collateral flow from the spinal arteries or the fetal-type posterior cerebral artery (1, 4).
Case series studies suggest that vertebral artery hypoplasia (VAH) may contribute to posterior ischemic events, especially in patients with other cerebrovascular risk factors (5, 6). The concept of regional hypoperfusion is associated with unilateral VAH and posterior circulation stroke (7). The risk of posterior ischemia is related to an increasing degree of VAH (5, 6, 8), regardless of the net flow (7). Although an increasing number of studies highlight the importance of unilateral VAH on ischemic stroke (5, 6, 8, 9), literature discussing the influence of bilateral VAH on ischemic stroke is limited (10, 11).
With regard to bilateral VAH, low flow volume in a single vertebral artery as well as inadequate net flow volume in the basilar artery ensues. Because of the chronic nature of congenital hypoplasia, the clinical symptoms and stroke patterns of this vascular disorder would differ from unilateral VAH. Chronic inadequate posterior circulation leads to the development of intracranial and extracranial collateral flow (10, 12). Recently, a case series paper correlated the fetal-type posterior circle of Willis with vertebrobasilar hypoplasia (12, 13).
In order to identify obscure clinical features, we reviewed the characteristics of patients with bilateral VAH by analyzing their clinical presentations, stroke patterns, risk factors, and the hemodynamics of collateral flow using ultrasonography and brain magnetic resonance imaging (MRI).
This is a retrospective, observational cross-sectional study. We reviewed 1,301 consecutive in-patients diagnosed with acute ischemic stroke at the Chung Shan Medical University Hospital from January 2013 to December 2015.
Upon admission, the series examination included an MRI, sonography exam, and a stroke risk factor survey. Patients who did not receive a brain MRI or sonography exam were excluded.
Patient medical and laboratory data were recorded; this included the age, sex, presence of systemic diseases, renal function, lipid profile, drug use, electrocardiogram, and history of previous stroke or transient ischemic attacks and related clinical manifestations.
This study was approved by the Institutional Review Board of Chung Shan Medical University Hospital, Taichung, Republic of China.
The infarction lesions were identified and classified by vascular territory according to MRI and three-dimensional time of flight (3D TOF) magnetic resonance angiography (MRA) examinations. A 3-T MRI system (Siemens, Germany) with the following settings was used T2-weightedimages, TR/TE 6000/100 ms, diffusion-weighted images TR/TE 5100/60 ms, and 3D TOF TR/TE20/4 ms. The locations of ischemic stroke were categorized as proximal (medulla and posterior inferior cerebellum), middle (pons and anterior inferior cerebellum), and distal (rostral brainstem, superior cerebellum, and occipital and temporal lobes) intracranial posterior circulation territories (14, 15).
A fetal type posterior cerebral artery (PCA) was classified as complete or partial according to MRA (12, 13). A complete fetal-type PCA is considered if the P1 segment is not visualized, and a partial fetal-type PCA is considered if the P1 segment is smaller than the posterior communicating artery on brain MRI.
The basilar artery hypoplasia (BAH) was defined as a basilar artery (BA) diameter <2 mm. The BA diameter was calculated on TOF source images at the mid-pons level. Vascular dissection was diagnosed if intramural hematoma, intimal flap, the pearl-and-string, or the double lumen signs were visualized on MRI.
Brain images were reviewed by neuroradiologists and neurologists, with the former interpreting the fetal-type PCA.
Color-coded carotid duplex and transcranial color-coded duplex examinations were reviewed for all enrolled patients. Intracranial and extracranial vessels conducted by experienced technicians using an IE-33 system (Philips Medical System, USA), equipped with a 2.0-MHz transducer. Routine measurements included thorough examinations of the bilateral neck carotid and transforaminal windows. The angle between the ultrasound beam and the direction of blood flow was adjusted manually. Blood flow examinations were targeted at the V2 and V4 segments of the vertebral artery as well as the region proximal to the distal basilar artery. The diameter and flow volume of each extracranial vertebral artery, as well as the mean velocity, and pulsatility index of the intracranial vertebrobasilar arteries were recorded and analyzed. VAH was defined according to sonographic criteria (4, 16, 17), including a ≤2.2 mm diameter over the V2 segment or a decreased vertebral flow volume of ≤30 mm/s. Bilateral VAH was defined as both vertebral arteries meeting the sonographic criteria of VAH and there was no evidence of dissection findings on MRI.
All statistical analyses were performed using SPSS software (version 22.0; SPSS Inc., Chicago, IL, USA). Continuous data is expressed as mean±SD.
Of the 1,301 patients diagnosed with acute ischemic stroke, 467 (149 pateints with posterior circulation infarction) underwent both MRI and sonographic examinations and were enrolled in the present study. In patients with posterior circulation, 80 of them met the criteria of unilateral VAH. Eight of the enrolled patients met the diagnostic criteria for bilateral VAH. The mean BA diameter was 2.68 ± 0.20 mm (range from 2.29 to 3.08 mm). In our study, the frequency of bilateral VAH was 1.7% (8/467), which is similar to that found in previous studies (11, 18). The characteristics of patients with bilateral VAH are listed in Table 1. There were six male (75.0%) and two female patients (25.0%). The average age was 62.9 years (range, 46–87). None of these patients had atrial fibrillation or heart disease. A high prevalence of hypertension (7/8, 87.5%) was noted. The prevalence of other stroke risk factors, including diabetes mellitus, dyslipidemia, smoking, and alcohol consumption ranged from 12.5 to 25.0%. We compared net flow volume, onset age, and stroke location analysis in bilateral VAH, unilateral VAH, and non-VAH groups, listed in Table 2. The mean net flow volume was 28.9 ± 9.7 mL/min, which is below the criteria of vertebrobasilar insufficiency (<100 mL/min) (7), and the defined value of unilateral VAH (30 mL/min) (16). In the bilateral VAH group, we found their onset age was younger and with more multiple vascular territory lesions.
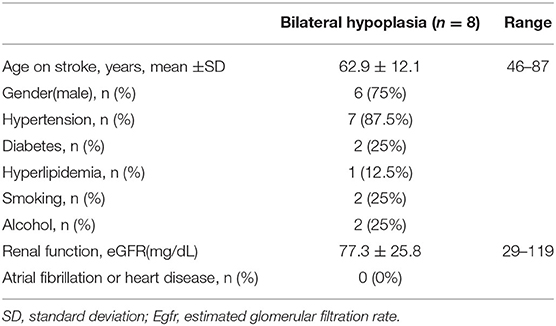
Table 1. Demographic and clinical characteristics of eight patients with bilateral vertebral artery hypoplasia.
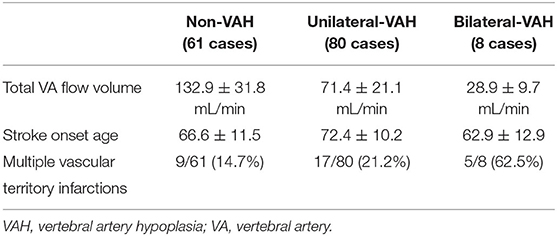
Table 2. Total VA flow volume, onset age and stroke location analysis in bilateral, unilateral, or non-vertebral artery hypoplasia groups.
The distribution of stroke and individual PCA types is listed in Table 3. Most of the infarctions were bilateral and multiple (5/8, 62.5%). A fetal-type PCA was recognized in six patients (6/8, 75.0 %), two with a complete bilateral, two with a partial bilateral, and two with a complete unilateral fetal-type PCA.
The prevalence of VAH ranges from 4 to 7% in the normal population (6, 7, 17). In posterior circulation stroke, the prevalence is increased to more than 40% according to different clinical studies (5, 18). Bilateral VAH is recognized in 1.6 to 3.4 % of patients with ischemic stroke (9, 18).
In our previous study, compared to anterior circulation infarction, there was a significantly higher frequency of VAH in posterior circulation infarction (22.38 vs. 44.75%, p < 0.0001) (7). Literature has demonstrated that VAH plays an important role in posterior circulation stroke (5–7, 9).
In this study, we found that patients with bilateral VAH developed stroke at a younger age (six patients <66 years) than the mean age of ischemic stroke, which ranges from 66 to 70 years (19), and other groups with posterior circulation infarctions (Table 2). The prevalence of hypertension in this group was significantly higher than the general stroke population (20). Cerebral autoregulation for chronic vertebrobasilar insufficiency may explain the blood pressure response (21).
Table 3 displays the initial manifestation of the patient population, which included dizziness, severe dysarthria, hemiplegia, and ataxia. In unilateral VAH-related stroke, the location of the infarct is usually limited to the territory of the ipsilateral artery, particularly in lateral medullar infarction and posterior inferior cerebellar artery infarction (2, 22, 23). In bilateral VAH, the infarction territory was mostly bilateral, involving multiple vascular territories, despite receiving collateral blood supply from the fetal-type PCA (Table 3 and Figure 1). The clinical presentation of these patients illustrates the high variability and burden of posterior circulation infarction. Most cases of multiple infarctions resulted in severe handicap or coma; therefore, it is important to detect at-risk patients.
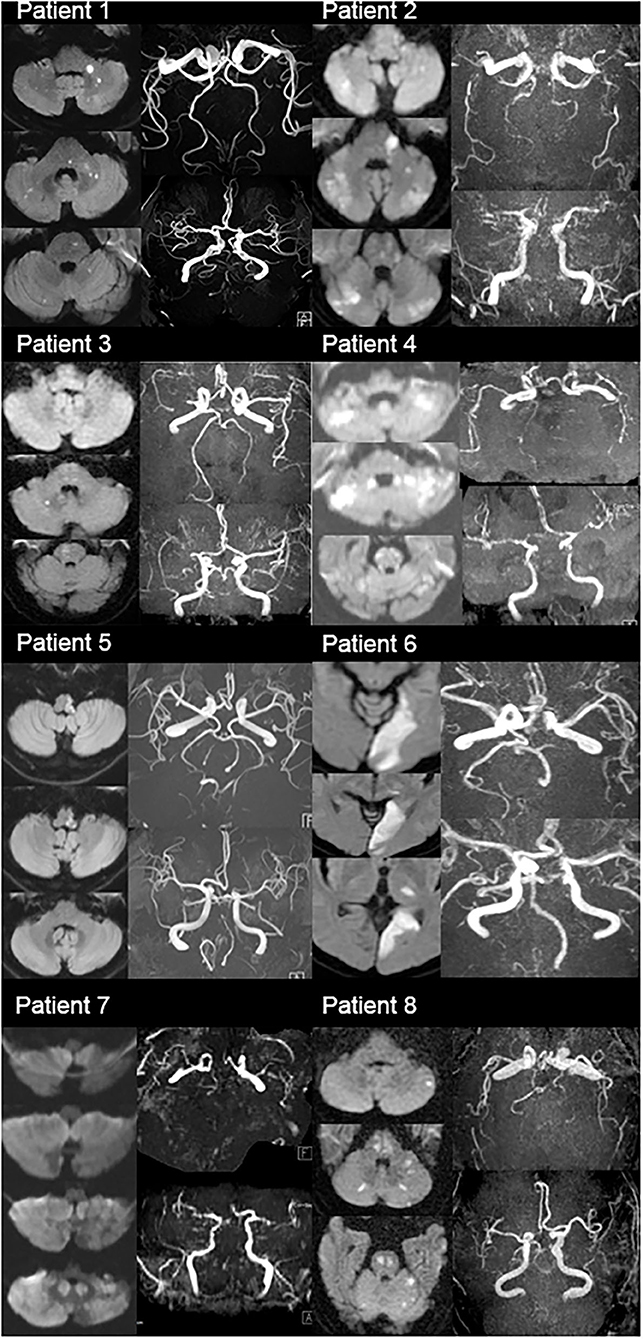
Figure 1. MRI diffusion-weighted images (DMI) and MRA images of total eight patients (MRI DWI showed multiple infarctions in these patients; MRA showed fetal type PCA, vertebral hypoplasia, small caliber of basilar artery, or invisible vertebrobasilar arteries).
Scattered brain infarction is usually related to cardioembolic stroke or artery-to- artery embolism (24); however, no patients in our population had atrial fibrillation, other heart disease, or significant atherosclerosis across the major arteries, suggesting the effect of hypoperfusion in bilateral VAH-related stroke. Several studies reported unilateral VAH to be associated with relative hypoperfusion in the dependent vascular territory (5, 7). According to the extracranial ultrasonography of our patient group, the mean (±SD) of the total vertebral flow volume was low(28.9 ± 9.7 mL/min, Table 2), compared with the non-VAH or unilateral VAH group (Table 2), which suggest severe hypoperfusion of the vertebrobasilar system, and as a consequence, development of an earlier and more severe posterior circulation infarction (Table 2).
In this study, bilateral VAH evolving into a smaller basilar artery (mean BA diameter 2.68 ± 0.20 mm, range from 2.29 to 3.08 mm) was recognized. Artery to artery embolism from vertebrobasilar hypoplasia would also contribute to scattered infarctions. Literature has demonstrated (25) BAH was associated with pontine infarction and VAH was associated with the medulla and inferior cerebellum. Emboli were known to preferentially reach the distal posterior circulation arteries (14). However, it is difficult to recognize the true origin of embolism since the artery to artery embolism and large artery hemodynamic should be one of concern.
For the treatment of bilateral VAH, early preventive drugs for ischemic insults, including antiplatelet or anticoagulant drugs, could be considered in symptomatic patients. Reconstruction of the blood supply, such as bypass surgery, would be another option (26).
Conventionally, a fetal-type PCA was thought to be a normal variant and common in the general population; however, in some reports this vascular type was associated with a higher risk for ischemic stroke, both in the anterior and posterior circulation (3, 4, 27, 28). Until now, its significance has been under debate.
In the literature, the incidence of a unilateral and bilateral fetal-type PCA ranged from 4 to 26% and 2 to 4%, respectively (13, 27, 28). Studies state commonly reported symptoms in patients with a fetal-type PCA to be dizziness, headache, and focal neurological deficits (3, 28). In our population, 75% of patients with bilateral VAH also displayed a fetal-type PCA, illustrating a sizable co-existence (75%) of bilateral VAH and a unilateral or bilateral fetal-type PCA. This finding corresponds to findings from previous studies that suggest the simultaneous occurrence of a hypoplastic vertebrobasilar system and fetal-type circle of Willis, and the increased development of ischemic events in the posterior circulation (3, 12).
From an embryological perspective, due to the delayed development of the P1 segment, the PCAs are supplied by the internal carotid arteries via the posterior communicating arteries temporally.
Typically, an adult PCA is complete at 6–7 weeks of embryological development (29). Inadequate flow of the basilar PCA system may interrupt the normal development of the PCA. Nevertheless, it is not clear how a fetal-type circle of Willis responds to unilateral VAH (30) or significantly inadequate basilar flow (in this study), or how it evolves to the adult configuration, which leads to a higher risk for both anterior and post-ischemic strokes (12, 27). However, the significance and pathophysiology of a fetal-type PCA in stroke remains unclear. Further comprehensive research is necessary.
In this study, most patients with bilateral VAH displayed a fetal variant of the PCA, supplied from the anterior circulation via the posterior communicating artery segment. However, with such hemodynamic compensation, supplementation via the fetal-type PCA still failed to support the vertebrobasilar system, resulting in a multifocal scattered infarction in the posterior circulation.
There were several limitations in this study. First, the case number of bilateral VAH is small, and we enrolled our samples from in-patients and not in healthy subjects. Overestimated frequencies and symptoms of bilateral VAH would be suspected. Because we applied the duplex ultrasonographic criteria of VAH, stenosis over the VA orifice or decreased VA flow volume due to atherosclerosis stenosis is a possible trap as applying the sonographic criteria of VAH diagnosis. Compared evaluation of the contrast-enhanced MRA images at the same time would result in a more reliable diagnosis.
We evaluated the clinical and vascular characteristics of patients with stroke and bilateral VAH. We found a younger age at stroke onset, obvious hypertension, bilateral and multiple vertebrobasilar infarcts, and a high prevalence of the fetal PCA in our enrolled patients.
Clinically, bilateral VAH may pose a significant risk to the posterior circulation; therefore, early detection and prevention are crucial in this patient group.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Review Board of Chung Shan Medial University Hospital, Taichung, Republic of China. The patients/participants provided their written informed consent to participate in this study.
H-YC designed the study. C-FH, K-WC, C-HS, and C-YS collected and organized data. C-FH and H-YC analyzed and interpreted the data. All authors read and approved the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank the neurologists, radiographers, and radiologists at Chung Shan Medical University Hospital.
1. Scheel P, Ruge C, Schoning M. Flow velocity and flow volume measurements in the extracranial carotid and vertebral arteries in healthy adults: reference data and the effects of age. Ultrasound Med Biol. (2000) 26:1261–6. doi: 10.1016/S0301-5629(00)00293-3
2. Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. (2014) 5:30. doi: 10.3389/fneur.2014.00030
3. Arjal RK, Zhu T, Zhou Y. The study of fetal-type posterior cerebral circulation on multislice CT angiography and its influence on cerebral ischemic strokes. Clin Imaging. (2014) 38:221–5. doi: 10.1016/j.clinimag.2014.01.007
4. Schoning M, Walter J, Scheel P. Estimation of cerebral blood flow through color duplex sonography of the carotid and vertebral arteries in healthy adults. Stroke. (1994) 25:17–22. doi: 10.1161/01.STR.25.1.17
5. Thierfelder KM, Baumann AB, Sommer WH, Armbruster M, Opherk C, Janssen H, et al. Vertebral artery hypoplasia: frequency and effect on cerebellar blood flow characteristics. Stroke. (2014) 45:1363–8. doi: 10.1161/STROKEAHA.113.004188
6. Zhang DP, Lu GF, Zhang JW, Zhang SL, Ma QK, Yin S. Vertebral artery hypoplasia and posterior circulation infarction in patients with isolated vertigo with stroke risk factors. J Stroke Cerebrovasc Dis. (2017) 26:295–300. doi: 10.1016/j.jstrokecerebrovasdis.2016.09.020
7. Chi HY, Hsu CF, Chen AC, Su CH, Hu HH, Fu WM. Extracranial and intracranial ultrasonographic findings in posterior circulation infarction. J Ultrasound Med. (2018) 37:1605–10. doi: 10.1002/jum.14501
8. Sauer T, Wolf ME, Ebert AD, Szabo K, Chatzikonstantinou A. Vertebral artery hypoplasia does not influence lesion size and clinical severity in acute ischemic stroke. J Stroke Cerebrovasc Dis. (2016) 25:1770–5. doi: 10.1016/j.jstrokecerebrovasdis.2016.03.050
9. Mitsumura H, Miyagawa S, Komatsu T, Hirai T, Kono Y, Iguchi Y. Relationship between vertebral artery hypoplasia and posterior circulation ischemia. J Stroke Cerebrovasc Dis. (2016) 25:266–9. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.027
10. Janzen A, Steinhuber CR, Bogdahn UR, Schuierer GR, Schlachetzki F. Ultrasound findings of bilateral hypoplasia of the vertebral arteries associated with a persistent carotid-hypoglossal artery. BMJ Case Rep. (2009) 2009:bcr07.2008.0486. doi: 10.1136/bcr.07.2008.0486
11. Mestan MA. Posterior fossa ischemia and bilateral vertebral artery hypoplasia. J Manipulative Physiol Ther. (1999) 22:245–9. doi: 10.1016/S0161-4754(99)70051-5
12. Lochner P, Golaszewski S, Caleri F, Ladurner G, Tezzon F, Zuccoli G, et al. Posterior circulation ischemia in patients with fetal-type circle of Willis and hypoplastic vertebrobasilar system. Neurol Sci. (2011) 32:1143–6. doi: 10.1007/s10072-011-0763-5
13. Shaban A, Albright KC, Boehme AK, Martin-Schild S. Circle of willis variants: fetal PCA. Stroke Res Treat. (2013) 2013:105937. doi: 10.1155/2013/105937
14. Caplan L, Chung CS, Wityk R, Glass T, Tapia J, Pazdera L, et al. New England medical center posterior circulation stroke registry: I. Methods, data base, distribution of brain lesions, stroke mechanisms, and outcomes. J Clin Neurol. (2005) 1:14–30. doi: 10.3988/jcn.2005.1.1.14
15. Caplan L, Wityk R, Pazdera L, Chang HM, Pessin M, Dewitt L. New England medical center posterior circulation stroke registry II. Vascular lesions. J Clin Neurol. (2005) 1:31–49. doi: 10.3988/jcn.2005.1.1.31
16. Jeng JS, Yip PK. Evaluation of vertebral artery hypoplasia and asymmetry by color-coded duplex ultrasonography. Ultrasound Med Biol. (2004) 30:605–9. doi: 10.1016/j.ultrasmedbio.2004.03.004
17. Chen YY, Chao AC, Hsu HY, Chung CP, Hu HH. Vertebral artery hypoplasia is associated with a decrease in net vertebral flow volume. Ultrasound Med Biol. (2010) 36:38–43. doi: 10.1016/j.ultrasmedbio.2009.08.012
18. Park JH, Kim JM, Roh JK. Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. J Neurol Neurosurg Psychiatry. (2007) 78:954–8. doi: 10.1136/jnnp.2006.105767
19. Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology. (2013) 81:264–72. doi: 10.1212/WNL.0b013e31829bfde3
20. Moreno-Rojas AJ, Gonzalez-Marcos JR, Gil-Peralta A, Serrano-Castro V. Vascular risk factors in patients with infratentorial vertebrobasilar ischemia. Revista de neurologia. (1998) 26:113–7. doi: 10.33588/rn.26149.981096
21. Gong X, Liu J, Dong P, Zhang P, Li N, Zhao X, et al. Assessment of dynamic cerebral autoregulation in patients with basilar artery stenosis. PLoS ONE. (2013) 8:e77802. doi: 10.1371/journal.pone.0077802
22. Tao WD, Liu M, Fisher M, Wang DR, Li J, Furie KL, et al. Posterior versus anterior circulation infarction: how different are the neurological deficits? Stroke. (2012) 43:2060–5. doi: 10.1161/STROKEAHA.112.652420
23. Searls DE, Pazdera L, Korbel E, Vysata O, Caplan LR. Symptoms and signs of posterior circulation ischemia in the new England medical center posterior circulation registry. Arch Neurol. (2012) 69:346–51. doi: 10.1001/archneurol.2011.2083
24. Koennecke HC, Bernarding J, Braun J, Faulstich A, Hofmeister C, Nohr R, et al. Scattered brain infarct pattern on diffusion-weighted magnetic resonance imaging in patients with acute ischemic stroke. Cerebrovasc Dis. (2001) 11:157–63. doi: 10.1159/000047632
25. Olindo S, Khaddam S, Bocquet J, Chausson N, Aveillan M, Cabre P, et al. Association between basilar artery hypoplasia and undetermined or lacunar posterior circulation ischemic stroke. Stroke. (2010) 41:2371–4. doi: 10.1161/STROKEAHA.110.593145
26. Raheja A, Taussky P, Kumpati GS, Couldwell WT. Subclavian-to-Extracranial vertebral artery bypass in a patient with vertebrobasilar insufficiency: 3-dimensional operative video. Oper Neurosurg (Hagerstown). (2018) 14:312. doi: 10.1093/ons/opx130
27. Lambert SL, Williams FJ, Oganisyan ZZ, Branch LA, Mader EC Jr. Fetal-type variants of the posterior cerebral artery and concurrent infarction in the major arterial territories of the cerebral hemisphere. J Investig Med High Impact Case Rep. (2016) 4(3):2324709616665409. doi: 10.1177/2324709616665409
28. Wu HM, Chuang YM. The clinical relevance of fetal variant of the circle of Willis and its influence on the cerebral collateral circulation. Acta Neurol Taiwan. (2011) 20:232–42. doi: 10.29819/ANT.201112.0002
29. Menshawi K, Mohr JP, Gutierrez J. A Functional perspective on the embryology and anatomy of the cerebral blood supply. J Stroke. (2015) 17:144–58. doi: 10.5853/jos.2015.17.2.144
Keywords: posterior circulation infarction, vertebral artery hypoplasia, posterior cerebral artery, vertebrobasilar insufficiency, ultrasonagraphy
Citation: Hsu C-F, Chen K-W, Su C-H, Shen C-Y and Chi H-Y (2021) Bilateral Vertebral Artery Hypoplasia and Fetal-Type Variants of the Posterior Cerebral Artery in Acute Ischemic Stroke. Front. Neurol. 12:582149. doi: 10.3389/fneur.2021.582149
Received: 10 July 2020; Accepted: 11 March 2021;
Published: 08 April 2021.
Edited by:
Simon Nagel, Heidelberg University Hospital, GermanyReviewed by:
Yuishin Izumi, Tokushima University, JapanCopyright © 2021 Hsu, Chen, Su, Shen and Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hsin-Yi Chi, YW5uLmppaEBtc2EuaGluZXQubmV0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.