
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Neurol. , 12 November 2020
Sec. Stroke
Volume 11 - 2020 | https://doi.org/10.3389/fneur.2020.592458
This article is part of the Research Topic Current Challenges in Cardioembolic Stroke View all 9 articles
 Cristina Sarti1,2*
Cristina Sarti1,2* Miroslava Stolcova3
Miroslava Stolcova3 Giulia Domna Scrima1
Giulia Domna Scrima1 Fabio Mori4
Fabio Mori4 Ylenia Failli1
Ylenia Failli1 Donatella Accavone1
Donatella Accavone1 Silvia Biagini1
Silvia Biagini1 Costanza Maria Rapillo1
Costanza Maria Rapillo1 Patrizia Nencini2
Patrizia Nencini2 Alessio Mattesini3
Alessio Mattesini3 Carlo Di Mario3
Carlo Di Mario3 Francesco Meucci3 on behalf of the Heart-Brain Team of Careggi University Hospital, Florence, Italy
Francesco Meucci3 on behalf of the Heart-Brain Team of Careggi University Hospital, Florence, ItalyIntroduction: Patients with atrial fibrillation (AF) can experience ischemic stroke despite adequate anticoagulant therapy. The secondary prevention strategy of these so-called “resistant strokes” is empirical. Since about 90% of patients with ischemic stroke due to atrial fibrillation have thrombus in left atrial appendage (LAA) we sought to explore the possibility that resistant stroke could have a LAA morphology resistant to anticoagulants.
Case Report: A 77 years old man affected by AF experienced two cardioembolic ischemic stroke while on anticoagulants. The study of LAA showed a windsock-like morphology in the proximal part while distally the LAA presented a cauliflower morphology with a large amount of pectinate muscles and blood stagnation. The precise characteristics of LAA were properly understood integrating images obtained by cardiac CT, transesophageal echocardiography, and selective angiography. A high risky LAA for thrombus formation was diagnosed and its occlusion (LAAO) as an add-on therapy to anticoagulants was proposed and performed. Six month follow-up was uneventfully.
Conclusion: The systematic study of LAA in patients with resistant-stroke could help to identify LAA malignant morphology. The efficacy on stroke recurrence of the combined therapy (anticoagulants plus LAAO) is worthy to be tested in randomized trials.
Anticoagulant therapy is the first option for ischemic stroke prevention in patients with atrial fibrillation. However, ~1–2% of patients experience an ischemic stroke while taking anticoagulants (1). An unproperly conducted therapy, such as suboptimal dosage, poor adherence, drugs interactions, or a pathogenesis of stroke not related to atrial fibrillation are possible explanations. If the cardioembolic stroke occurs despite the anticoagulant therapy being well conducted, the event should be classified as a “resistant” stroke, a condition little studied for which the therapeutic approach remains empirical (2).
A 77-year-old man with high blood pressure, diabetes, coronary artery disease, and permanent atrial fibrillation was referred to our Heart-Brain Outpatient Clinic for a second opinion on the best secondary prevention therapy after two previous ischemic strokes.
The first event was characterized by right-sided hemiparesis affecting mainly the arm associated with right hemianopia and hypoesthesia. Neuroimaging revealed a left temporo-parieto-insular cortico-subcortical ischemic lesion (Figures 1A,B).
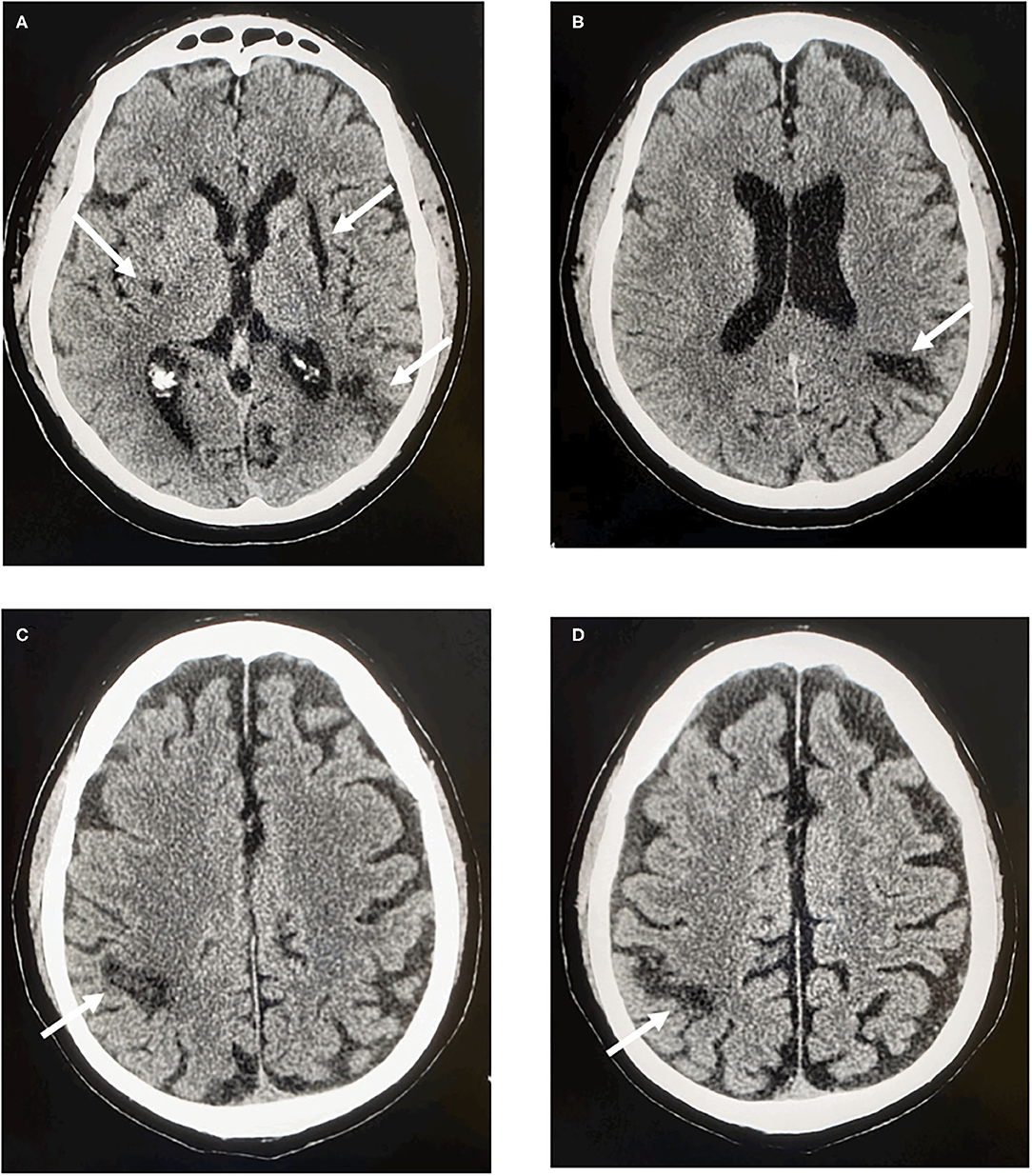
Figure 1. CT scan of the brain. (A) Left side: cortico-subcortical temporo-parieto-insular hypodensity. Right side: subcortical lenticular hypodensity. (B) Left side: cortico-subcortical parietal hypodensity. (C,D) Right side: cortico-subcortical parietal hypodensity.
At the time of the event the patient was taking apixaban 2.5 mg twice daily even though he had normal kidney function and a body weight of 85 kg. Therapy was then changed to dabigatran 150 mg twice daily. Two months later the patient had another ischemic stroke characterized by motor impairment in the left hand associated with a right cortico-subcortical parietal ischemic lesion (Figures 1C,D).
Based on the results of thorough stroke work-up, excluding among others atherosclerotic plaques in cervical and intracranial arteries, aortic-arch atherosclerosis, and occult cancer, atrial fibrillation was considered to be the most likely etiology of patient's recurrent stroke.
Patient reported excellent adherent to anticoagulation therapy. Trough and peak dabigatran plasma levels were within the expected therapeutic range (71 ng/ml, range 61–143; 134 ng/ml, range 117–275, respectively).
The use of concomitant medications that may have altered the dabigatran effect was excluded.
The event was therefore classified as “resistant stroke.”
The patient underwent a thorough cardiological study. Cardiac computed tomography (CT) scan was performed to assess the left atrial appendage (LAA). It revealed an oval-shaped LAA with windsock-like morphology in the proximal part (ostium and landing zone) while distally the LAA presented multi-lobated with a large amount of pectinate muscles and a small retro-verse distal lobe with a small amount of blood stagnation (Figure 2A), configuring a cauliflower morphology according to Di Biase criteria (3) (Figure 2B). The mean diameter of the landing zone was 21 mm. The morphology of this LAA was considered to be at high risk for thrombus formation due to its dimensions, distal fragmentation and presence of small lobatures, favoring blood stagnation.
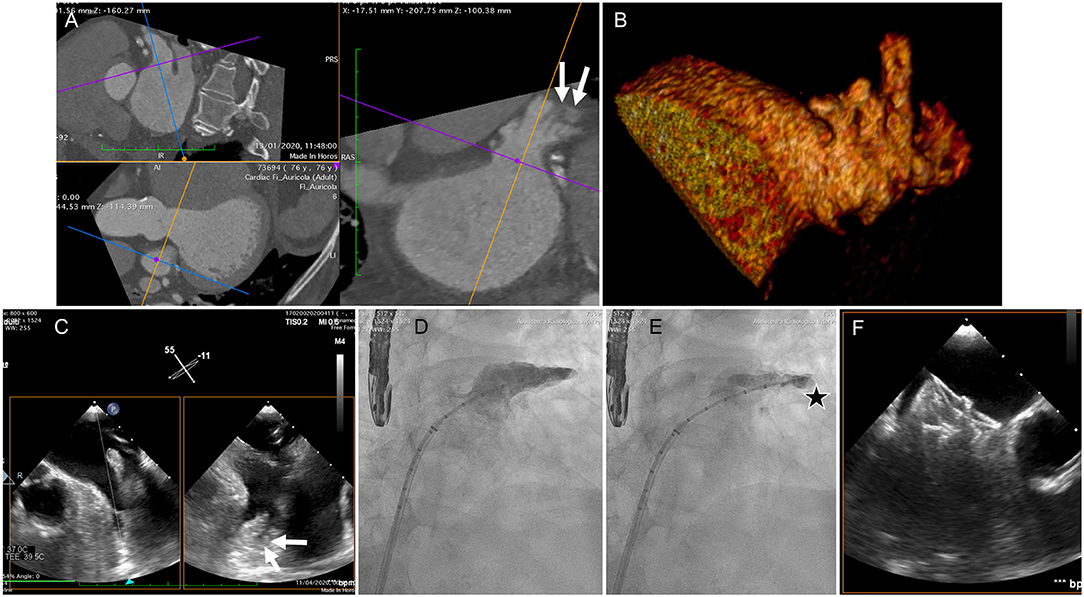
Figure 2. (A) CT scan of the LAA. Proximally the LAA presented a single lobe with oval-shaped ostium while distally it divided into multiple lobes, favoring blood stagnation (arrows), configuring a cactus morphology (B). (C) Transesophageal echocardiography, performed intraprocedurally revealed a “plus” image in the distal part of the appendage (arrows). (D) selective angiography revealed stagnation of dye in the distal lobe, with a slow wash out (E – star). (F) Final result after successful LAA occlusion with implantation of a 25 mm Amplatzer Amulet device (Abbott, Chicago, IL, USA).
Taking into account the patient's clinical history, the occlusion of LAA as an adjunct therapy to oral anticoagulants was considered and proposed to the patient who, after adequate information, gave his consent.
Transesophageal echocardiography was performed prior to the procedure revealing a “plus” image in the distal part of the appendage suspected of being a clot (Figure 2C). Selective angiography showed stagnation of contrast in the distal lobe, with a slow wash out (Figures 2D,E). The integrated evaluation of the three imaging modalities allowed to attribute the anomalies to a prominent pectinate muscle.
LAA-occlusion was successfully performed with a 25 mm Amplatzer Amulet occluder (Abbott, Chicago, IL, USA) (Figure 2F) and subsequent recovery was uneventful. Patient was discharged with dabigatran 150 mg twice daily and an indication to maintain it lifelong.
The patient was asymptomatic at 6-months follow-up.
About 90% of heart clots in patients with atrial fibrillation develop within the LAA. LAA has a highly variable form and preliminary data suggest an association between LAA morphology and stroke (3, 4). Other LAA features, such as trabeculation, orifice area, LAA flow velocity, seem to identify LAA at high risk of thrombosis (5). One study explored the safety and efficacy of LAAO as secondary prevention in patients with nonvalvular atrial fibrillation who have experienced a stroke/transient ischemic attack despite anticoagulant treatment (6). A recent prospective, observational study on 19 patients explored the efficacy to combine LAAO to anticoagulants (7).
No data are however available on LAA morphology in resistant stroke.
This case highlights that an integrated study with different techniques (CT, echo, angiography) can be of help to identify LAA with high-risk characteristics. The LAA classification in use, limited to the external form, seems too simple and unable to meet this clinical need (3).
In the absence of specific studies focusing on patients with recurrent stroke despite optimal anticoagulation (“resistant” stroke), guidelines are lacking.
Such patients could have a malignant LAA “resistant” to anticoagulants.
A systematic study of LAA morphology may suggest that anticoagulant failure in some of these patients could be caused by an unfavorable form of LAA with high thrombotic risk for which anticoagulants alone may not be sufficient. Consequently, LAA occlusion can be considered not as an alternative but as an adjunct to anticoagulation in selected cases.
The efficacy of this “add-on” combination therapy on stroke recurrence deserves to be tested in randomized trials.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CS and FMe: contributed to the clinical part of the study, design and conceptualized study, drafted and revised the manuscript. MS: drafted and revised the manuscript. GDS: contributed to the design of the study and revised the manuscript. FMo: contributed to the clinical part of the study and revised the manuscript. YF, PN, AM, and CDM: revised the manuscript. DA, SB, and CMR: contributed to the clinical part of the study. All authors contributed to the article and approved the submitted version.
CDM received institutional funding from Edwards, Medtronic, Astra-Zeneca, Daiichi Sankyo, and Shockwave medical.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. López-López JA, Sterne JA, Thom HH, Higgins JP, Hingorani AD, Okoli GN, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. (2017) 359:j5058. doi: 10.1136/bmj.j5058
2. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. (2016) 50:e1–88. doi: 10.1093/ejcts/ezw313
3. Di Biase L, Santangeli P, Anselmino M, Mohanty P, Salvetti I, Gili S, et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J Am Coll Cardiol. (2012) 60:531–8. doi: 10.1016/j.jacc.2012.04.032
4. Khurram IM, Dewire J, Mager M, Maqbool F, Zimmerman SL, Zipunnikov V, et al. Relationship between left atrial appendage morphology and stroke in patients with atrial fibrillation. Heart Rhythm. (2013) 10:1843–9. doi: 10.1016/j.hrthm.2013.09.065
5. Yaghi S, Song C, Gray WA. Left atrial appendage function and stroke risk. Stroke. (2015) 46:3554–9. doi: 10.1161/STROKEAHA.115.011273
6. Cruz-González I, González-Ferreiro R, Freixa X, Gafoor S, Shakir S, Omran H, et al. Left atrial appendage occlusion for stroke despite oral anticoagulation(resistant stroke). Results from the Amplatzer Cardiac Plug registry. Rev Esp Cardiol. (2020) 73:28–34. doi: 10.1016/j.rec.2019.02.013
Keywords: case-report, resistant stroke, left atrial appendage occlusion, atrial fibrillation, anticoagulants, recurrent stroke
Citation: Sarti C, Stolcova M, Scrima GD, Mori F, Failli Y, Accavone D, Biagini S, Rapillo CM, Nencini P, Mattesini A, Di Mario C and Meucci F (2020) Atrial Fibrillation and Resistant Stroke: Does Left Atrial Appendage Morphology Matter? A Case Report. Front. Neurol. 11:592458. doi: 10.3389/fneur.2020.592458
Received: 07 August 2020; Accepted: 14 October 2020;
Published: 12 November 2020.
Edited by:
George Ntaios, University of Thessaly, GreeceReviewed by:
Leonidas Palaiodimos, Albert Einstein College of Medicine, United StatesCopyright © 2020 Sarti, Stolcova, Scrima, Mori, Failli, Accavone, Biagini, Rapillo, Nencini, Mattesini, Di Mario and Meucci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cristina Sarti, Y3Jpc3RpbmEuc2FydGlAdW5pZmkuaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.