
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Neurol. , 23 June 2020
Sec. Movement Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fneur.2020.00455
This article is part of the Research Topic Managing Parkinson's Disease with a Multidisciplinary Perspective View all 13 articles
Background: Caregiver strain is recognized globally with Parkinson's disease (PD). Comparatively little is understood about caregiver burden and strain in Asia.
Objective: To investigate caregiver strain for families living with PD in Singapore, in light of international data.
Methods: Ninety-four caregivers were recruited via people living with idiopathic PD in Singapore. Caregiver strain was assessed using the Zarit Burden Interview (ZBI); health status was assessing using the Cumulative Illness Rating Scale for Geriatrics (CIRS-G). PD disability measures were the Unified Parkinson's Disease Rating Scale (UPDRS) and modified Hoehn and Yahr (1967) Scale.
Results: Primary caregivers of people living with PD in Singapore were mostly cohabiting spouses, partners or offspring. Around half employed foreign domestic helpers. Mean caregiving duration was 5.9 years with an average of eight hours per day spent in caregiving roles. Most care providers were comparatively healthy. Caregivers reported significant levels of strain which increased with greater level of disability (r = 0.36, n = 94, p < 0.001). Associations were significant between caregiver strain and scores on the UPDRS mentation, behavior, and mood subscales [r = 0.46, n = 94, p < 0.001, 95% CI (0.28, 0.60)]. High scores on the UPDRS activities of daily living subscale were associated with caregiver strain [r = 0.50, n = 94, p < 0.001, CI (0.33, 0.64)].
Conclusion: Most caregivers in this Singapore sample reported high levels of strain, despite comparatively good physical function. Caregiver strain in PD spans geopolitical and cultural boundaries and correlates with disease severity. These results support the need for better early recognition, education, and support for caregivers of people living with PD.
Parkinson's disease (PD) is a debilitating and progressive condition that impacts the lives of individuals and their families (1). Although caregiver burden associated with PD is well-documented for Europe (2–7) and North America (8–11), there is a lack of published data for the south-east Asia region. Most elderly people with PD in countries such as Singapore live at home (12, 13). It is important to understand how PD affects their caregivers because the prevalence of PD in South-East Asia ranges from 79 to 193 per 100,000 population (14). More than six million people will be living with PD in Asia by 2030 due to rapid population aging and lifestyle factors (15). People with PD experience movement disorders, falls, and non-motor symptoms that can reduce mobility and quality of life (1, 16). As the disease progresses, it can place a heavy burden on primary caregivers (17, 18). The individual and societal costs of PD are substantial (8, 19–23), yet are not fully understood for Asia.
With PD progression, caregiving can sometimes be perceived as the main role of some family members (24, 25). Studies in Australia (19, 26), Europe (6), and the USA (8) have reported considerable caregiver burden associated with PD. Caregiver burden refers to the negative physical, mental, and socioeconomic sequelae associated with caring for a person living with a disability (27). Martinez-et al. (28) and Kelly et al. (29) reported associations between PD caregiver burden and caregiver health-related quality of life (HRQoL). Caregiver HRQoL as measured on the EuroQoL has also been shown to correlate with burden, as measured on the Zarit Carer Burden Inventory (ZBI) (r = −0.33 to −0.49, p < 0.01) (28). Studies in western societies have also reported that psychological aspects of caregiver strain are associated with the level of PD disability (3). For example, disability in PD measured by the Barthel Index was associated with increased caregiver burden (r = 0.46–0.53, p < 0.01) (17). Many of the studies in the literature have focused on US and European populations with comparatively low ethnic and cultural diversity (30). The results for PD caregivers and care recipients might not be generalizable to south-east Asia, where there are geographical, cultural, and geopolitical differences. For example, Tan et al. (31) found that overall PD incidence rates were comparable between Singapore and the West, yet there were significance differences in the inter-ethnic incidence rates of PD between Chinese, Malays, and Indians.
The current study aimed to increase understanding of the dimensions of caregiver strain and burden in Singapore and to consider the findings in the context of global reports. We also aimed to determine the factors associated with strain in caregivers of this sample of people living with this progressive neurological condition.
We conducted a cross-sectional survey with a convenience sample of 94 caregivers of individuals with PD. Patient data was also collected through associated caregivers. Recruitment was via a neurology specialist outpatient clinic at an acute tertiary hospital and a PD society in Singapore. For a 2-tailed bivariate analysis test with power of 0.80 and statistical significance at 0.05, a sample size of 85 care providers was required to detect a moderately strong relationship between variables (32). Criteria for the selection of caregiver participants included: (i) above 21 years of age; (ii) primary caregiver of a patient (care recipient) diagnosed with idiopathic PD by a neurologist; (iii) providing at least 3 h of daily care for 6 months or more; (iv) able to understand spoken English. The research protocol was approved by institutional review boards of The University of Melbourne (Ethics ID: 0719562) and Singapore General Hospital (Ethics ID: 2008/122/A). All subjects gave written informed consent in accordance with the Declaration of Helsinki.
A structured questionnaire was administered to the caregiver participants. It contained items on (i) care recipient and caregiver sociodemographic characteristics; (ii) health information about the care recipients, measured using the modified Hoehn and Yahr Scale (HY) (33), and the Unified Parkinson's Disease Rating Scale (UPDRS) (34); (iii) information on the burden and health status of the caregivers quantified by the ZBI (35) as well as the Cumulative Illness Rating Scale for Geriatrics (CIRS-G) (36).
The ZBI has 22 items relating to the impact of care-recipient disabilities on caregiver physical and emotional health, and social, and financial distress. The ZBI score sums individual items (range 0–88), with a higher score indicating greater caregiver personal strain or role strain (35). The maximum possible scores are 24 (six items) for personal strain and 48 (12 items) for role strain. The ZBI has previously been shown to be a valid and reliable instrument for caregivers with dementia in Singapore (37). We also used the CIRS-G to estimate medical and psychiatric multi-morbidity burden in care providers (38). This scale rates the severity of problems as mild (1), moderate (2), severe (3), or extremely severe (4) (36).
When applicable, Spearman's rank correlation coefficients (r) were calculated to assess the direction and magnitude of the associations between variables. The strength of the relationships was interpreted following Cohen's guidelines (39); relationships were deemed as small where correlations ranged from r = 0.10–0.29; medium when r = 0.30–0.49 to large r = 0.50–1.00. Multiple regression analyses were used to explore the relationships between caregiver coping and well-being with sociodemographic, caregiving, and disease severity variables. Data were entered and analyzed using Predictive Analytics Software (PASW) Statistics 18. All reported p-values were 2-tailed with alpha set at 0.05.
We also conducted a comprehensive literature search of global PD caregiver burden on PubMed (1 April 2020) using the terms “Caregiver burden/strain AND Parkinson's disease” where studies included both caregivers and PD participants. Initially, the titles were screened by two people for keywords. The abstracts were then screened to ensure that studies were conducted on PD and caregiver strain or burden. Full-text articles 2018-2020 were reviewed to extract data on caregiver burden inventory utilized, caregiver demographics/duration, and descriptive statistics (e.g., mean, median) reported for the caregiver burden inventory utilized in the studies.
Of the 94 Singaporean care recipients, 60 (64%) were male. The majority of the care recipients with PD were 51 years or older (n = 88, 93.6%). Six were aged 31–50 years. The age at which the care recipients were diagnosed with PD ranged from 33 to 89 years (M = 61.8, SD = 11.8). The mean duration of PD was 6.9 years (SD 5.6). Their mean UPDRS mentation, behavior and mood score was 3.4 (SD 2.9). The mean UPDRS ADL score was 15.4 (SD = 9.5). People living with PD had a range of levels of disease severity when functioning at their best (Table 1). It is notable that despite being rated five on the modified Hoehn and Yahr scale, 14% people with PD in the sample were being cared for at home.
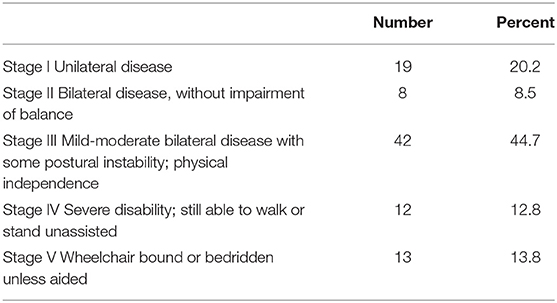
Table 1. Hoehn and Yahr (33) stage when functioning at best.
Most caregivers were females (n = 74, 78.7%). They were mainly spouses, partners, or daughters who lived with the people who had PD. The mean number of caregiving years was 5.9 years (range 0.25–25, SD 5.2). The care providers dedicated a mean of 8 h per day (SD = 7.0) in their PD caregiving roles. As shown in Table 2, foreign domestic helpers were often engaged to assist with personal care, rehabilitation, social engagement, and mobility (30). Notwithstanding, 58% of carers preferred help from family and friends, who were mainly siblings and sons, and daughters of care recipients. Approximately a quarter of the caregivers attended caregiver education or support groups to obtain more information about caring and rehabilitation for individuals with PD. Only a small percentage of caregivers attended more than 1 h of caregiver education and support.
Caregivers in this Singapore sample reported a mean ZBI score of 23 out of 88. The personal strain and role strain domains are shown in Table 3. In order to interpret the relative intensity of burden experienced by caregivers of people living with PD, the following cut-off values were used: 0–20 little strain; 21–40 mild to moderate strain; 41–60 moderate to severe strain; 61–88 severe strain (35). Some caregivers (n = 45, 47.9%) reported little burden; 37 caregivers (39.4%) had mild to moderate burden and 11 caregivers (12.8%) reported moderate to severe levels of burden.
Most care providers were older women who were comparatively healthy, although some reported a range of health problems and multi-morbidities of mild to moderate severity as measured by the CIRS-G. The mean score for CIRS-G was 2 (SD = 2) and the CIRS-G Severity Index mean was 0.12 (SD = 0.15). In this sample, there were more healthy caregivers than those with multi-morbidity.
There was a statistically significant, moderately strong positive correlation between modified HY scores, and caregiver burden when the people with PD functioned at their best (rs = 0.36, n = 94, p < 0.001). Statistically significant moderate positive correlations were also obtained between the HY scores and caregiver burden when the people with PD functioned at their worst (rs = 0.38, n = 94, p < 0.001, 95% CI [0.19, 0.54]). This was particularly notable for the UPDRS Mentation, Behavior, Mood score (rs = 0.46, n = 94, p < 0.001, 95% CI [0.28, 0.60]). The relationship between UPDRS Activities of Daily Living score and caregiver burden also showed a strong positive correlation (rs = 0.50, n = 94, p < 0.001, CI [0.33, 0.64]). The personal strain and role strain for care providers increased with PD severity.
Table 4 summarizes data from our evaluation of key recent international studies of PD caregiver strain. The results show world-wide data demonstrating that care-giver strain is challenging and common, with many shared features between south-east Asia and other regions of the globe, as seen in the world-wide literature (40–79).
Regardless of geographical, cultural, and geopolitical differences, caregiver strain in PD is a major problem world-wide and correlates with disease severity (40–79). Our study showed that most south-east Asian PD caregivers are family members. Although many received support from domestic workers, they often experienced high levels of burden and strain. Both role strain and physical strain were reported, warranting consideration of systems to be put in place for early recognition, education, and support for caregiver strain.
Our results are consistent with European (8) and American literature [eg., (28, 40, 41)] showing more female than male PD care providers, given that Parkinsonism more often affects men. Previous studies have also shown close relationships between disability and quality of life in people with PD and the level of burden in caregivers (42). Caregiver strain is particularly associated with immobility in PD care recipients and the severity of non-motor symptoms associated with PD (7, 43). A Malaysian study by Razali et al. also found that patient age, stage and severity of illness were significantly associated with feelings of burden in caregivers (44). However, caregiver burden in this Malaysian study was not related to social status, kinship or duration of care (44).
Approximately one quarter of the care providers in our study attended caregiver education or support groups to obtain more information on how best to support people living with PD. This was rarely more than an hour in duration. The small amount of PD education concurs with the findings of Mehta et al. who reported that caregivers who lived in Singapore often did not receive very much formal training to care for people living with PD (45).
The caregivers in our sample reported more personal strain than role strain. Overall, they exercised a reasonable level of control over their caregiving roles even though it sometimes affected their personal health and social life. This was consistent with regional studies showing associations between caregiving and perceived burden (23, 43, 46). For example, a Singapore qualitative analysis (47) reported that many caregivers experienced lifestyle restrictions and felt physically and emotionally drained. Others (24, 48–50) reported that increased involvement in caring can sometimes be perceived to disrupt a caregiver's personal life and roles. Mehta noted that some (but not all) Singaporean caregivers interpreted their role to be obligatory “having no choice (but to care for the patient)” (45).
The results of our investigation also showed that caregiver burden had a moderately strong positive relationship with PD disease stage (Table 4). It also escalated with severe disability. This finding is consistent with global reports (Table 4). Of interest, a Malaysian study reported that respite in the form of caregiver support group or day care attendance for patients can reduce caregiver burden (44). Thommessen et al. (51) and Schrag et al. (43) found that only the mental health of care recipients was associated with caregiver burden. In contrast, we found that both poor mental health and activities of daily living were associated with caregiver strain.
There was no correlation between caregiver multimorbidity and perceived caregiver burden in our sample. This was in contrast to Martinez-Martin et al. (2) who found that Spanish caregivers tended to be less physically and mentally healthy compared to the general population. The care recipients in our study had a higher disease severity than counterparts in Spain (12). Differences in race, culture, and healthcare systems might also have contributed to the disparate results.
Although this is the largest PD caregiver study undertaken in the Asia-Pacific region to have identified critical elements in caring, it is not known whether the Singapore results generalize to other locations in Asia such as Indonesia, Malaysia, Vietnam, Thailand, Cambodia, or China. The sample mainly included men with PD and caregivers who were women. Further clarification of gender issues in caregiving is warranted. The sample size for each ethnic group also did not allow for critical analysis of differences in caregiving as a result from race, ethnicity, and culture that could have affected caregiving experiences. In addition, variations in treatment options for different countries could affect caregiver burden and strain. Longitudinal changes in caregiver burden and coping strategies were not examined. Further trials are needed to better understand how caregiver strain varies according to the stage of progression of Parkinsonism as well as the effects of different interventions to improve health, well-being and quality of life in care providers and care-recipients.
As with international data, care providers of people living with PD in Singapore often had raised levels of personal strain and role strain that were associated with the level of PD disability. The caregivers in our sample provided care for an average of 8 h per day for 6 years or more. Although foreign employed workers often gave assistance, around 80% of care providers were family members. Many care providers were elderly spouses. In Singapore, as for throughout the world, there is a need for systems to reduce caregiver burden that are responsive to the progressive trajectory of this common and chronic neurological disease.
The datasets generated for this study are available on request to the corresponding author.
The studies involving human participants were reviewed and approved by the research protocol was approved by institutional review boards of The University of Melbourne (Ethics ID: 0719562) and Singapore General Hospital (Ethics ID: 2008/122/A). The patients/participants provided their written informed consent to participate in this study.
S-BT, AW, E-KT, and MM: contributed to research project conception and design. S-BT: original concept and research project organization and execution, data collection, statistical analysis, design and execution, and manuscript writing. AW: statistical analysis design, review, and critique. E-KT: statistical analysis review and critique, and manuscript: review and critique. MM: research project conception and design, and statistical analysis review and critique, and manuscript: review and critique. All authors contributed to manuscript revision, read and approved the submitted version.
This paper was also supported by Parkinson's Singapore and La Trobe University. Financial Disclosures of all authors (for the preceding 12 months) S-BT: nil relevant, AW: nil relevant, E-KT: supported by national medical research council grants; STaR and Parkinson disease clinical translational program, SPARKS 2, RC: nil relevant, MM: receives funding from the National Health and Medical Research Council Australia and Healthscope.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We acknowledge the financial support of the Singapore General Hospital Research Fund—Quality of life and coping for caregivers of people with Parkinson's disease (SRF#143/08); 2008, Singapore General Hospital. This data was collected when S-BT was a PhD student at The University of Melbourne, supervised by Prof Williams.
1. Morris ME, Martin CL, Schenkman ML. Striding out with Parkinson disease: evidence-based physical therapy for gait disorders. Phys Ther. (2010) 90:280–8. doi: 10.2522/ptj.20090091
2. Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ, Frades-Payo B, Aguera-Ortiz L, Weintraub D, et al. Neuropsychiatric symptoms and caregiver's burden in Parkinson's disease. Parkinsonism Relat Disord. (2015) 21:629–34. doi: 10.1016/j.parkreldis.2015.03.024
3. Martinez P, Rodriguez-Blazquez C, Paz S, Lizan L, Forjaz MJ, Frades B, et al. The burden of Parkinson disease amongst caregivers in Spain over 4 years. Value Health. (2014) 17:A390–1. doi: 10.1016/j.jval.2014.08.857
4. Hiseman JP, Fackrell R. Caregiver burden and the non-motor symptoms of Parkinson's disease. Int Rev Neurobiol. (2017) 133:479–97. doi: 10.1016/bs.irn.2017.05.035
5. Hagell P, Alvariza A, Westergren A, Arestedt K. Assessment of burden among family caregivers of people with Parkinson's disease using the zarit burden interview. J Pain Symptom Manage. (2017) 53:272–8. doi: 10.1016/j.jpainsymman.2016.09.007
6. Corallo F, De Cola MC, Lo Buono V, Di Lorenzo G, Bramanti P, Marino S. Observational study of quality of life of Parkinson's patients and their caregivers. Psychogeriatrics. (2017) 17:97–102. doi: 10.1111/psyg.12196
7. Grun D, Pieri V, Vaillant M, Diederich NJ. Contributory factors to caregiver burden in Parkinson disease. J Am Med Dir Assoc. (2016) 17:626–32. doi: 10.1016/j.jamda.2016.03.004
8. Martinez-Martin P, Macaulay D, Jalundhwala YJ, Mu F, Ohashi E, Marshall T, et al. The long-term direct and indirect economic burden among Parkinson's disease caregivers in the United States. Mov Disord. (2019) 34:236–45. doi: 10.1002/mds.27579
9. Shah SP, Glenn GL, Hummel EM, Hamilton JM, Martine RR, Duda JE, et al. Caregiver tele-support group for Parkinson's disease: a pilot study. Geriatr Nurs. (2015) 36:207–11. doi: 10.1016/j.gerinurse.2015.02.002
10. Roland KP, Chappell NL. Caregiver experiences across three neurodegenerative diseases: Alzheimer's, Parkinson's, and Parkinson's with dementia. J Aging Health. (2019) 31:256–79. doi: 10.1177/0898264317729980
11. Roland KP, Jenkins ME, Johnson AM. An exploration of the burden experienced by spousal caregivers of individuals with Parkinson's disease. Mov Disord. (2010) 25:189–93. doi: 10.1002/mds.22939
12. Tan SB, Williams AF, Morris ME, Tan EK. Health-related quality of life of caregivers of people with Parkinson's disease in Singapore. Proc. Singapore Healthcare. (2010) 19:297–302. doi: 10.1177/201010581001900404
13. Tan MMJ, Lim EC, Nadkarni NV, Lye WK, Tan EK, Prakash KM. The characteristics of patients associated with high caregiver burden in Parkinson's disease in Singapore. Front Neurol. (2019) 10:561. doi: 10.3389/fneur.2019.00561
14. Abbas MM, Xu Z, Tan LCS. Epidemiology of Parkinson's disease: east versus west. Mov Disord Clin Pract. (2018) 5:14–28. doi: 10.1002/mdc3.12568
16. Morris ME, Taylor NF, Watts JJ, Evans A, Horne M, Kempster P, et al. A home program of strength training, movement strategy training and education did not prevent falls in people with Parkinson's disease: a randomised trial. J Physiother. (2017) 63:94–100. doi: 10.1016/j.jphys.2017.02.015
17. Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ. Quality of life and burden in caregivers for patients with Parkinson's disease: concepts, assessment and related factors. Expert Rev Pharmacoecon Outcomes Res. (2012) 12:221–30. doi: 10.1586/erp.11.106
18. Bhimani R. Understanding the burden on caregivers of people with Parkinson's: a scoping review of the literature. Rehabil Res Pract. (2014) 2014:718527. doi: 10.1155/2014/718527
19. Bohingamu Mudiyanselage S, Watts JJ, Abimanyi-Ochom J, Lane L, Murphy AT, Morris ME, et al. Cost of living with Parkinson's disease over 12 months in Australia: a prospective cohort study. Parkinsons Dis. (2017) 2017:5932675. doi: 10.1155/2017/5932675
20. Fredericks D, Norton JC, Atchison C, Schoenhaus R, Pill MW. Parkinson's disease and Parkinson's disease psychosis: a perspective on the challenges, treatments, and economic burden. Am J Manag Care. (2017) 23(5 Suppl):S83–92.
21. Hermanowicz N, Edwards K. Parkinson's disease psychosis: symptoms, management, and economic burden. Am J Manag Care. (2015) 21(10 Suppl):s199–206.
22. Boland DF, Stacy M. The economic and quality of life burden associated with Parkinson's disease: a focus on symptoms. Am J Manag Care. (2012) 18(7 Suppl):S168–75.
23. Houghton D, Barbour P, Leopold N, Lee J, Siderowf A. Clinical and economic determinants of caregiver burden in Parkinson's disease. Twentieth Annual Symposia on Etiology, Pathogenesis, and Treatment of Parkinson's Disease and Other Movement Disorders: Wiley Online, (Milton). (2006). p. 1558.
24. McLaughlin D, Hasson F, Kernohan WG, Waldron M, McLaughlin M, Cochrane B, et al. Living and coping with Parkinson's disease: perceptions of informal carers. Palliat Med. (2011) 25:177–82. doi: 10.1177/0269216310385604
25. Moroz A, Edgley SR, Lew HL, Chae J, Lombard LA, Reddy CC, et al. Rehabilitation interventions in Parkinson disease. PMR. (2009) 1(3 Suppl):S42–8. doi: 10.1016/j.pmrj.2009.01.018
26. Zhong M, Peppard R, Velakoulis D, Evans AH. The relationship between specific cognitive defects and burden of care in Parkinson's disease. Int Psychogeriatr. (2016) 28:275–81. doi: 10.1017/S1041610215001593
27. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. (1986) 26:260–6. doi: 10.1093/geront/26.3.260
28. Martinez-Martin P, Forjaz MJ, Frades-Payo B, Rusinol AB, Fernandez-Garcia JM, Benito-Leon J, et al. Caregiver burden in Parkinson's disease. Mov Disord. (2007) 22:924–31. doi: 10.1002/mds.21355
29. Kelly DH, McGinley JL, Huxham FE, Menz HB, Watts JJ, Iansek R, et al. Health-related quality of life and strain in caregivers of Australians with Parkinson's disease: an observational study. BMC Neurol. (2012) 12:57. doi: 10.1186/1471-2377-12-57
30. Kim KS, Kim BJ, Kim KH, Choe MA, Yi M, Hah YS, et al. Subjective and objective caregiver burden in Parkinson's disease. Taehan Kanho Hakhoe Chi. (2007) 37:242–8. doi: 10.4040/jkan.2007.37.2.242
31. Tan LC, Venketasubramanian N, Jamora RD, Heng D. incidence of Parkinson's disease in Singapore. Parkinsonism Relat Disord. (2007) 13:40–3. doi: 10.1016/j.parkreldis.2006.07.003
33. Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality 1967. Neurology. (2001) 57(10 Suppl 3):S11–26. doi: 10.1212/wnl.17.5.427
34. Martinez-Martin P, Rodriguez-Blazquez C, Alvarez-Sanchez M, Arakaki T, Bergareche-Yarza A, Chade A, et al. Expanded and independent validation of the Movement Disorder Society-Unified Parkinson's Disease Rating Scale (MDS-UPDRS). J Neurol. (2013) 260:228–36. doi: 10.1007/s00415-012-6624-1
35. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. (1980) 20:649–55. doi: 10.1093/geront/20.6.649
36. Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. (1968) 16:622–6. doi: 10.1111/j.1532-5415.1968.tb02103.x
37. Seng BK, Luo N, Ng WY, Lim J, Chionh HL, Goh J, et al. Validity and reliability of the zarit burden interview in assessing caregiving burden. Ann Acad Med Singapore. (2010) 39:758–63.
38. Fortin M, Hudon C, Dubois MF, Almirall J, Lapointe L, Soubhi H. Comparative assessment of three different indices of multimorbidity for studies on health-related quality of life. Health Qual Life Outcomes. (2005) 3:74. doi: 10.1186/1477-7525-3-74
39. Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression / correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: L. Erlbaum Associates (2003).
40. Parrish M, Giunta N, Adams S. Parkinson's disease caregiving: implications for care management. Care Manag J. (2003) 4:53–60. doi: 10.1891/cmaj.4.1.53.57471
41. Sturm D, Folkerts AK, Kalbe E. Easing Burden and stress: intervention needs of family members of patients with Parkinson's disease. J Parkinsons Dis. (2019) 9:221–7. doi: 10.3233/JPD-181456
42. Rodriguez-Violante M, Camacho-Ordonez A, Cervantes-Arriaga A, Gonzalez-Latapi P, Velazquez-Osuna S. Factors associated with the quality of life of subjects with Parkinson's disease and burden on their caregivers. Neurologia. (2015) 30:257–63. doi: 10.1016/j.nrleng.2014.01.002
43. Schrag A, Hovris A, Morley D, Quinn N, Jahanshahi M. Caregiver-burden in Parkinson's disease is closely associated with psychiatric symptoms, falls, and disability. Parkinsonism Relat Disord. (2006) 12:35–41. doi: 10.1016/j.parkreldis.2005.06.011
44. Razali R, Ahmad F, Rahman FN, Midin M, Sidi H. Burden of care among caregivers of patients with Parkinson disease: a cross-sectional study. Clin Neurol Neurosurg. (2011) 113:639–43. doi: 10.1016/j.clineuro.2011.05.008
45. Mehta KK. Stress among family caregivers of older persons in Singapore. J Cross Cult Gerontol. (2005) 20:319–34. doi: 10.1007/s10823-006-9009-z
46. Caap-Ahlgren M, Dehlin O. Factors of importance to the caregiver burden experienced by family caregivers of Parkinson's disease patients. Aging Clin Exp Res. (2002) 14:371–7. doi: 10.1007/BF03324464
47. Tan SB, Williams AF, Morris ME. Experiences of caregivers of people with Parkinson's disease in Singapore: a qualitative analysis. J Clin Nurs. (2012) 21:2235–46. doi: 10.1111/j.1365-2702.2012.04146.x
48. Hounsgaard L, Pedersen B, Wagner L. The daily living for informal caregivers with a partner with Parkinson's disease: an interview study of women's experiences of care decisions and self-management. J Nurs Healthc Chronic Illn. (2011). 3:504–12. doi: 10.1111/j.1752-9824.2011.01126.x
49. McCabe MP, Roberts C, Firth L. Work and recreational changes among people with neurological illness and their caregivers. Disabil Rehabil. (2008) 30:600–10. doi: 10.1080/09638280701400276
50. Goldsworthy B, Knowles S. Caregiving for Parkinson's disease patients: an exploration of a stress-appraisal model for quality of life and burden. J Gerontol B Psychol Sci Soc Sci. (2008) 63:P372–6. doi: 10.1093/geronb/63.6.P372
51. Thommessen B, Aarsland D, Braekhus A, Oksengaard AR, Engedal K, Laake K. The psychosocial burden on spouses of the elderly with stroke, dementia and Parkinson's disease. Int J Geriatr Psychiatry. (2002) 17:78–84. doi: 10.1002/gps.524
52. Trapp SK, Ertl MM, Gonzalez-Arredondo S, Rodriguez-Agudelo Y, Arango-Lasprilla JC. Family cohesion, burden, and health-related quality of life among Parkinson's disease caregivers in Mexico. Int Psychogeriatr. (2018) 31:1039–1045. doi: 10.1017/S1041610218001515
53. Vatter S, McDonald KR, Stanmore E, Clare L, Leroi I. Multidimensional care burden in Parkinson related dementia. J Geriatr Psychiatry Neurol. (2018) 31:319–28. doi: 10.1177/0891988718802104
54. Yuksel B, Ak PD, Sen A, Sariahmetoglu H, Uslu SC, Atakli D. Caregiver burden and quality of life in early stages of idiopathic Parkinson's disease. Ideggyogy Sz. (2018) 71:343–50. doi: 10.18071/isz.71.0343
55. Fider CRA, Lee JW, Gleason PC, Jones P. Influence of religion on later burden and health of new black and white caregivers. J Appl Gerontol. (2019) 38:1282–303. doi: 10.1177/0733464817703017
56. Genc F, Yuksel B, Tokuc FEU. Caregiver burden and quality of life in early and late stages of idiopathic Parkinson's disease. Psychiatry Investig. (2019) 16:285–91. doi: 10.30773/pi.2019.02.20
57. Kumar D, Ashwini K, Hegde S, Prasanna L, Joseph B, Bose A, et al. Caregiver assisted home-based cognitive remediation for individuals diagnosed with schizophrenia: a pilot study. Asian J Psychiatr. (2019) 42:87–93. doi: 10.1016/j.ajp.2019.03.010
58. Kumar H, Ansari S, Kumar V, Barry HD, Tahir A. Severity of caregiver stress in relation to severity of disease in persons with Parkinson's. Cureus. (2019) 11:e4358. doi: 10.7759/cureus.4358
59. Lee GB, Woo H, Lee SY, Cheon SM, Kim JW. The burden of care and the understanding of disease in Parkinson's disease. PLoS ONE. (2019) 14:e0217581. doi: 10.1371/journal.pone.0217581
60. Smith ER, Perrin PB, Tyler CM, Lageman SK, Villasenor T. Parkinson's symptoms and caregiver burden and mental health: A cross-cultural mediational model. Behav Neurol. (2019) 2019:1396572. doi: 10.1155/2019/1396572
61. Tinetti ME, Naik AD, Dindo L, Costello DM, Esterson J, Geda M, et al. Association of patient priorities aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions. JAMA Intern Med. (2019) 179:1688–97. doi: 10.1001/jamainternmed.2019.4235
62. Yang Z, Tian Y, Fan Y, Liu L, Luo Y, Zhou L, et al. The mediating roles of caregiver social support and self-efficacy on caregiver burden in Parkinson's disease. J Affect Disord. (2019) 256:302–8. doi: 10.1016/j.jad.2019.05.064
63. Drexel SC, Klietz M, Kollewe K, Paracka L, Kutschenko A, Kopp B, et al. Caregiver burden and health-related quality of life in idiopathic dystonia patients under botulinum toxin treatment: a cross-sectional study. J Neural Transm. (2020) 127:61–70. doi: 10.1007/s00702-019-02109-6
64. Fox S, Azman A, Timmons S. Palliative care needs in Parkinson's disease: focus on anticipatory grief in family carers. Ann Palliat Med. (2020) 9(Suppl.1):S34–43. doi: 10.21037/apm.2020.02.04
65. Henry RS, Lageman SK, Perrin PB. The relationship between Parkinson's disease symptoms and caregiver quality of life. Rehabil Psychol. (2020) 65:137–44. doi: 10.1037/rep0000313
66. Klietz M, Schnur T, Drexel S, Lange F, Tulke A, Rippena L, et al. Association of motor and cognitive symptoms with health-related quality of life and caregiver burden in a German cohort of advanced Parkinson's disease patients. Parkinsons Dis. (2020) 2020:5184084. doi: 10.1155/2020/5184084
67. Lee G-B, Woo H, Lee S-Y, Cheon SM. The burden of care and the understanding of disease in Parkinson's disease. PLoS One. (2019) 14:e0217581. doi: 10.1371/journal.pone.0217581
68. Macchi ZA, Koljack CE, Miyasaki JM, Katz M, Galifianakis N, Prizer LP, et al. Patient and caregiver characteristics associated with caregiver burden in Parkinson's disease: a palliative care approach. Ann Palliat Med. (2020) 9(Suppl.1):S24–33. doi: 10.21037/apm.2019.10.01
69. Tyler CM, Henry RS, Perrin PB, Watson J, Villasenor T, Lageman SK, et al. Structural equation modeling of Parkinson's caregiver social support, resilience, and mental health: a strength-based perspective. Neurol Res Int. (2020) 2020:7906547. doi: 10.1155/2020/7906547
70. Tessitore A, Marano P, Modugno N, Pontieri FE, Tambasco N, Canesi M, et al. Caregiver burden and its related factors in advanced Parkinson's disease: data from the PREDICT study. J Neurol. (2018) 265:1124–37. doi: 10.1007/s00415-018-8816-9
71. Karlstedt M, Fereshtehnejad SM, Aarsland D, Lokk J. Mediating effect of mutuality on caregiver burden in Parkinson's disease partners. Aging Ment Health. (2019) 1–8. doi: 10.1080/13607863.2019.1619165
72. Torny F, Videaud H, Chatainier P, Tarrade C, Meissner WG, Couratier P. Factors associated with spousal burden in Parkinson's disease. Rev Neurol. (2018) 174:711–5. doi: 10.1016/j.neurol.2018.01.372
73. Mosley PE, Breakspear M, Coyne T, Silburn P, Smith D. Caregiver burden and caregiver appraisal of psychiatric symptoms are not modulated by subthalamic deep brain stimulation for Parkinson's disease. NPJ Parkinsons Dis. (2018) 4:12. doi: 10.1038/s41531-018-0048-2
74. Balash Y, Korczyn AD, Migirov AA, Gurevich T. Quality of life in Parkinson's disease: a gender-specific perspective. Acta Neurol Scand. (2019) 140:17–22. doi: 10.1111/ane.130954
75. Bartolomei L, Pastore A, Meligrana L, Sanson E, Bonetto N, Minicuci GM, et al. Relevance of sleep quality on caregiver burden in Parkinson's disease. Neurol Sci. (2018) 39:835–9. doi: 10.1007/s10072-018-3252-2
76. Rajiah K, Maharajan MK, Yeen SJ, Lew S. Quality of life and caregivers' burden of Parkinson's disease. Neuroepidemiology. (2017) 48:131–7. doi: 10.1159/000479031
77. Crespo-Burillo JA, Rivero-Celada D, Saenz-de Cabezon A, Casado-Pellejero J, Alberdi-Vinas J, Alarcia-Alejos R. Deep brain stimulation for patients with Parkinson's disease: effect on caregiver burden. Neurologia. (2018) 33:154–9. doi: 10.1016/j.nrl.2016.05.017
78. Dahodwala N, Shah K, He Y, et al. Sex disparities in access to caregiving in Parkinson disease. Neurology. (2018) 90:e48–e54. doi: 10.1212/WNL.0000000000004764
79. Carrilho PEM, Rodrigues MA, de Oliveira BCR, da Silva EB, Silva T, Schran LDS, et al. Profile of caregivers of Parkinson's disease patients and burden measured by Zarit Scale Analysis of potential burden-generating factors and their correlation with disease severity. Dement Neuropsychol. 2018;12:299–305. doi: 10.1590/1980-57642018dn12-030011
Keywords: caregiver, carer, Parkinson's disease, well-being, quality of life, rehabilitation
Citation: Tan S-B, Williams AF, Tan E-K, Clark RB and Morris ME (2020) Parkinson's Disease Caregiver Strain in Singapore. Front. Neurol. 11:455. doi: 10.3389/fneur.2020.00455
Received: 28 February 2020; Accepted: 28 April 2020;
Published: 23 June 2020.
Edited by:
Daniel Martinez-Ramirez, Tecnológico de Monterrey, MexicoReviewed by:
Simon J. G. Lewis, Brain and Mind Research Institute, NSW, AustraliaCopyright © 2020 Tan, Williams, Tan, Clark and Morris. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meg E. Morris, bS5tb3JyaXNAbGF0cm9iZS5lZHUuYXU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.