
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Neurol., 19 May 2020
Sec. Neurotrauma
Volume 11 - 2020 | https://doi.org/10.3389/fneur.2020.00350
Objective: Mild traumatic brain injury (mTBI) is associated with depressed mood acutely post-injury, but there is little evidence regarding long-term depression. The aim of this study was to determine the odds ratio (OR) of depression chronically following mTBI.
Methods: We searched Medline (PubMed), ProQuest, and Web of Science from date of database creation to January 23, 2019, for eligible studies examining depression at least 6 months post-injury in adult subjects with mTBI of any etiology, including civilians and military. Three authors independently reviewed titles and abstracts for study eligibility. Data were extracted and collated by two investigators. Risk of bias was assessed with the SIGN methodology. Study data were pooled using random-effects meta-analysis. The primary exposure was mTBI, and the primary outcome was depression. Secondary exploratory variables were time of assessment, age at injury, age at assessment, sex, and etiology.
Results: We included 47 cross-sectional studies (n = 25,103 mTBI and 29,982 control), 26 cohort studies (n = 70,119 mTBI, 262,034 control), four prospective observational studies (n = 1,058 mTBI and 733 control), two prospective longitudinal studies (n = 119 mTBI, 81 control), two case-control studies (n = 56 mTBI, 56 control), and one randomized controlled trial (n = 252 mTBI, 3,214 control). mTBI was associated with a 3.29-fold increased risk of depression (OR 3.29, 95% CI 2.68–4.03, I2 = 96%). The OR for depression did not change when subjects were assessed at 6–12 months (OR 2.43, 1.45–4.07), years 1–2 (OR 4.12, 2.10–8.07); 2–10 (OR 3.28, 2.42–4.46), or 10+ (OR 3.42, 1.51–7.77). Similar risk of depression was sustained across different age at injury (<25: OR 2.26, 1.82–2.81; 25–35: OR 4.67, 3.06–7.14; >35: OR 2.69, 1.42–5.10) and different age at assessment (<40 years: OR 3.14, 2.48–3.99; >40 years: OR 4.57, 2.54–8.24). Female sex had a non-significant increase in OR (OR 19.97, 2.39–166.93) compared to male (OR 3.0, 2.33–3.86). mTBI etiology had no impact on depression.
Conclusions: Those experiencing mTBI are more than three times more likely to experience depression compared to those without a history of mTBI, and this risk remains decades beyond the mTBI event. Future longitudinal studies are needed to identify and mitigate this risk.
Mild traumatic brain injury (mTBI) occurs at an incidence exceeding 42 million per year worldwide (1). mTBI is defined as “an acute brain injury resulting from mechanical injury to the head from external physical forces” (2). The causes of mTBI are numerous, including sporting collisions, blast neurotrauma, and motor vehicle accidents, among others (3). mTBI is associated with acute neuropsychiatric dysfunction, with depression a commonly described sequel. Many acute symptoms dissipate with resolution of the physiological injury; however, depression may persist (or develop) in the post-acute or chronic time frame (4). While much is known about the long-term physical and cognitive consequences of mTBI, the mechanisms underlying emotional dysregulation after mTBI are less understood (5).
Depression has many direct consequences, and elucidation of the burden attributable to depression is essential to understanding the impact of this disorder in the post-mTBI setting. Depression may mediate the relationships between mTBI and poor physical health (6), diminish functional capacity (7), impair executive control (4), and hinder social function (8). Depression also decreases quality of life after mTBI (7) and has a substantial personal and economic burden (9). In studies encompassing TBI of all severities, post-injury depression may occur in over 40% of subjects, with a relative risk of 7.5 (10, 11). The true prevalence of depression in the chronic period following mTBI is uncertain, with most studies focusing on mTBI in the acute phase (days–weeks) as part of a constellation of post-concussive symptoms or on moderate-to-severe injuries. Suggested risk factors for post-TBI depression are heterogeneous across available data; indeed, no clear consensus has emerged regarding such factors such as female sex (11–13) and age at injury (14, 15). Moreover, the likelihood of depression following mTBI sustained via different injury modalities has not been investigated.
Major depressive disorder (MDD) has a lifetime prevalence of 20.6% and known overlap with mTBI. Given that mTBI is an extremely common injury with an approximate lifetime prevalence of 22% [range: 12–46% (16)], the degree of association between mTBI and depression is therefore important to quantify. Evaluation of any causal link between mTBI and depression is problematic due to the heterogeneity of primary injuries and outcomes, late emergence of symptomology, and lack of formal large-scale trials in the area. In lieu of definitive large-scale longitudinal clinical assessments, a meta-analysis of literature spanning decades post-mTBI is the only realistic means to elucidate the association between mTBI and depression and identify the true odds of occurrence.
The aim of this study was to conduct a meta-analysis on all published data assessing depression after adult mTBI from a mean of 6 months post-injury onward to determine the lifetime odds ratio (OR) of depression chronically following an mTBI event.
This study was conducted according to the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) Checklist for Meta-analyses of Observational Studies criteria (eTable 1).
We performed a random-effects meta-analysis. Operational definitions of mTBI and depression [obtained through Medical Subject Headings (MeSH) thesauruses and non-MeSH terms] were used to determine the search strategy. Our initial search in PubMed contained the keywords “mild traumatic brain injury,” “depression,” and “mood disorder” (see eMethods for full search strategy). Literature was searched from the date of database inception to January 23, 2019.
Studies were chosen according to the “PICOS” principles, with studies eligible if meeting the following criteria:
1) Population: Human adults assessed more than 6 months post-injury
2) Indicator: At least one instance of mTBI
3) Comparison: A control comparison group matched in age and sex
4) Outcome: Depression assessed using a measure validated in accordance with the standard operationalized diagnostic criteria [Feighner criteria, Research Diagnostic Criteria, Diagnostic, and Statistical Manual of Mental Disorders (DSM)-III, DSM-III-R, DSM-IV, DSM-5, and International Classification of Diseases (ICD)-10].
5) Study design: Original reports of case-control, cohort, cross-sectional, and prospective observational studies. Where possible, randomized controlled trials were included, provided that baseline (pretreatment) assessments were reported. Due to the nature of mTBI research, the vast majority of studies were non-randomized, thus we included randomized and non-randomized study designs.
Three investigators (SH, CB, TW) independently selected the studies and screened articles for exclusion on the basis of title and abstract, followed by review of full manuscripts and Supplementary Material. Studies examining moderate or severe TBI, combining injury severities, or including depression when present before injury were excluded. Studies reporting continuous data categorizing subjects as positive or negative for depression symptoms were examined for agreement in questionnaire cutoff values.
Studies straddling exclusion criteria were discussed for agreement among at least two authors. Three investigators (SH, CB, and TW) assessed the risk of bias. Any discrepancies at this stage were resolved by discussion among all authors until consensus was reached.
Our primary outcome of interest was presence or absence of depression at any time beyond 6 months post-mTBI. Planned secondary analyses examined the ORs of (1) depression with increasing chronicity post-mTBI from 6 months onward; (2) influence of age at injury (under 25, 25–35, over 35); (3) influence of age at assessment (under 40, over 40); (4) relationship of biological sex and odds of depression; (5) whether mTBIs of different etiologies confer a different risk of depression; (6) whether repeated injuries increase the odds of post-mTBI depression.
To assess the risk of bias in included studies, we combined the SIGN Methodology Checklist 3 for cohort studies and Checklist 4 for case-control studies. Heterogeneity was quantified using the I2 test statistic, where an I2 of below 50% indicates no/low heterogeneity, 50–75% moderate heterogeneity, and above 75% indicates high heterogeneity. Due to expected variation in effect sizes arising from methodological differences and sampling bias inherent to the type of studies examined, heterogeneity was handled by use of a random-effects model. Funnel plots were produced to assess publication bias, with calculation of Failsafe-N (17). Subgroup analyses (defined under “outcomes”) were also planned to determine whether differences in effect sizes were due to variations in methodology (18).
The following information was extracted for each study: measure of depression used in assessment and score for depression (dichotomous data: number classed as depressed for mTBI or control and total number of participants in each group; continuous data: mean and standard deviation for mTBI and control groups). For subgroup analysis, we also extracted mean time since mTBI, mean current age (with age at injury calculated from these two variables if not reported), and etiology of injury classified as sports mTBI, motor vehicle accident (MVA), military injuries or “other/unclassified.” In the case of multiple studies reporting data from the same cohort, we included only the study for which the most complete data set was available. We estimated summary ORs for dichotomous data, and mean differences (MDs) for continuous outcomes (see eMethods for further information). To combine these data sets, MDs were converted to ORs using the formula of Chinn (19). We used The Cochrane Collaboration RevMan software (20) to collate data and produce forest plots, funnel plots, and figures for risk of bias. One-way ANOVAs and Student's T-tests were calculated to determine statistical differences between subgroups using GraphPad Prism version 7.00 for Mac OS X (GraphPad Software, La Jolla, CA). Unless specified, p-values are representative of significance at the meta-analysis level.
Figure 1 describes the screening process for 1,972 studies assessed for inclusion or exclusion in the meta-analysis. The 82 studies ultimately included in the meta-analysis comprised a total of 392,834 subjects. Thirty-seven studies reported assessment of post-mTBI depression using dichotomous data (361,814 subjects) while 45 reported findings as continuous data (30,991 subjects). Table 1 summarizes the characteristics of included studies. We included two case-control studies, one randomized trial, 48 cross-sectional studies, 26 cohort studies, and six prospective longitudinal studies. Of the total 392,834 subjects, 96,688 had mTBI and 296,117 were controls. Control subjects fell into the following categories: healthy control or population samples (28 studies), veterans or active military without mTBI (36 studies), sportsplayer peers or peers of cases (13 studies), and non-mTBI injuries or illnesses (five studies; see eResults 1 for further analysis). In the dichotomous data, the frequency of depression across the mTBI cohorts was 8% compared to 3% across the control cohorts.
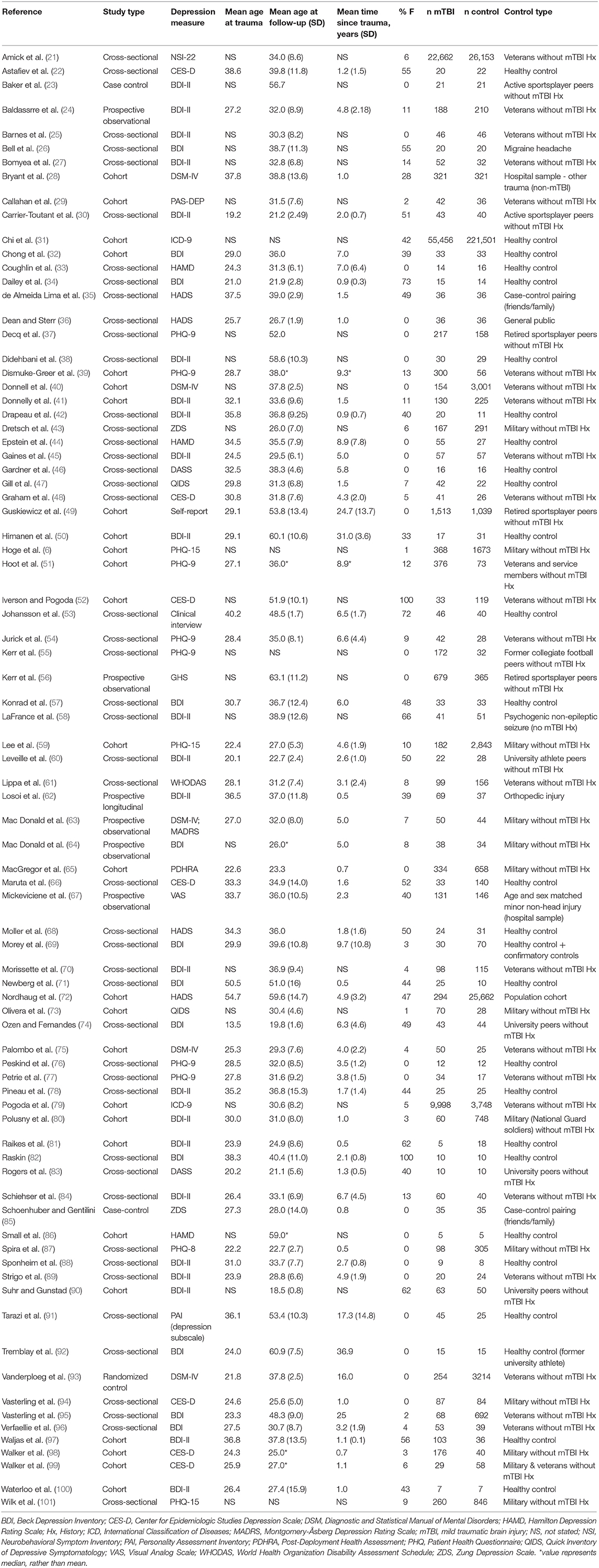
Table 1. Characteristics of studies examining depression chronically after mTBI meeting the criteria for inclusion.
A random-effects meta-analysis was conducted to examine the odds of depression at least 6 months after adult mTBI. We examined Forest plots of continuous and dichotomous data to assess trend similarity (eFigures 1, 2) before pooling these data. The overall OR of depression chronically after mTBI was 3.29 (95% CI 2.68–4.03, I2 = 96%, p < 0.00001) at the meta-analysis level (Figure 2).
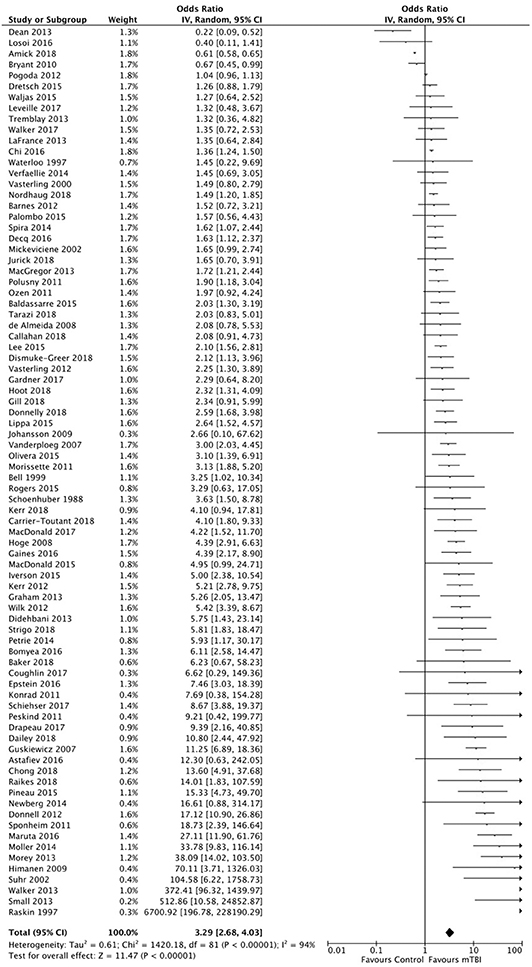
Figure 2. Forest plot representing pooled data from 82 studies reporting depression assessments at least 6 months after mild traumatic brain injuiry (mTBI). In each study, data for mTBI patient groups were compared with control groups for odds of depression. OR, odds ratio. Risk of bias was assessed using the SIGN methodological checklist.
Four studies (21, 31, 72, 79) accounted for a large number of the total subjects (365,480/392,834; 93%); however, this contribution largely resulted from control subjects in one study [n = 221,501 (31)]. Taking into account the relative frequency of mTBI vs. control subjects, these studies each contributed <2% of the overall weight, for a total contribution of 7.1%. No significant relationship was detected between mTBI and depression when these studies were assessed in isolation (OR 1.06, 95% CI 0.70–1.62; I2 = 100%, p = 0.78). However, removal of these studies from the pooled dataset only resulted in marginal change from the overall OR of post-mTBI depression (OR 3.61, 95% CI 2.89–4.52; I2 = 85%, p < 0.00001).
A number of studies (25, 28, 49, 56, 58, 61, 69, 82, 93–97) described assessment of lifetime depression but did not clearly stipulate whether participants were excluded if screening positively for pre-injury depression. To determine whether these studies unduly influenced findings, we removed these studies and repeated our analysis. We found that the OR remained stable without those studies (OR 3.34, 95% CI 2.96–4.15, I2 = 94%, p < 0.00001) and was similar when these studies were assessed in isolation (OR 3.13, 95% CI 1.72–5.71, I2 = 94%, p = 0.00002).
As a sub-analysis, we investigated the stability of the odds of post-mTBI depression over time. Studies were divided into four categories based on the distribution of time points: 6 months−1 year post-mTBI (nine studies, n = 1,906), 1–2 years (17 studies, n = 3,526), 2–10 years (27 studies, n = 32,093), and more than 10 years post-mTBI (six studies, n = 6,339). Twenty-two studies did not report a time interval post-injury and thus were excluded from this sub-analysis. No significant differences were observed between subgroups (p = 0.99, one-way ANOVA), although the calculated OR values were uniformly higher following the first subgroup (6 months−1 year). The meta-analysis level ORs and CIs are presented in Figure 3A and were as follows: 6 months−1 year post-mTBI: OR 2.43, 95% CI 1.45–4.07, I2 = 69%, p = 0.0007; 1–2 years: OR 4.12, 95% CI 2.10–8.07, I2 = 92%, p < 0.0001; 2–10 years: OR 3.28, 95% CI 2.42–4.46, I2 = 76%, p < 0.00001; 10+ years: OR 3.23, 95% CI 2.39–4.36, I2 = 86%, p < 0.00001. Three of the included studies performed longitudinal assessment with time points beyond those included in our meta-analysis. Their findings at time points relevant to our study also revealed stable depression symptoms over the following 1 (41), 5 (72), or 9 (56) years post-mTBI, with no apparent reduction in rate of depression. We next investigated whether depression persisted at a similar OR relative to age at mTBI. Studies were divided into those with mean ages of <25 years (18 studies, n = 9,622) 25–35 years (29 studies, n = 14,652), and more than 35 years of age (12 studies, n = 27,243). No significant difference was found between subgroups (p = 0.73, one-way ANOVA), although the pooled OR for 25–35 years was numerically higher (Figure 3B). The ORs were as follows: aged under 25: OR 2.26, 95% CI 1.82–2.81, I2 = 41%, p < 0.00001; aged 25–35: OR 4.67, 95% CI 3.06–7.14, I2 = 87%, p < 0.00001; aged over 35: OR 2.69, 95% CI 1.42–5.10, I2 = 84%, p = 0.002.
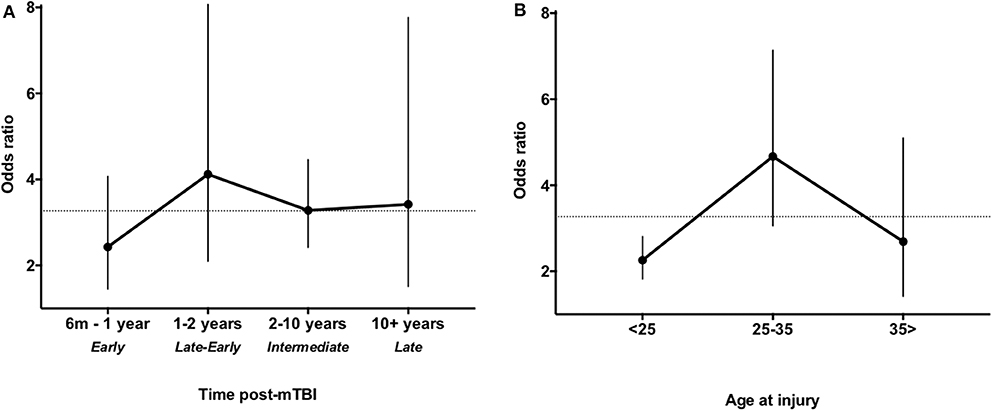
Figure 3. Odds ratio (OR) of depression over time post mild traumatic brain injury (mTBI) (A) and age at injury (B). (A) Data were stratified into early phase (6 months−1 year post-mTBI), late-early phase (1–2 years post-mTBI), intermediate phase (2–10 years post-mTBI), and late phase (more than 10 years post-mTBI). (B) Data were stratified by mean age at injury under 25 years, 25–35 years, or over 35 years. Dashed lines indicate the overall OR.
To examine the possible influence of cohort composition, we further evaluated the impact of age at assessment, biological sex, injury etiology, repeated mTBI, method of depression assessment, and study design. We tested the effect of age at assessment by dividing studies into groups where the mean age was under 40 (63 studies, n = 81,860) and over 40 years (15 studies, n = 30,650). No significant difference between groups was seen (p = 0.25, Student's T-test). ORs were as follows: aged under 40: OR 3.14, 95% CI 2.48–3.99, I2 = 94%, p < 0.00001; aged over 40: OR 4.57, 95% CI 2.54–8.24, I2 = 87%, p < 0.00001. Two studies included only females, for which the pooled OR was 147.68, 95% CI 169, 110.38, I2 = 93%, p = 0.16. We also compared data for the four studies which included more than 70% females (n = 287) to 55 studies including more than 70% males (n = 88,239). No statistical difference was found between males and females (p = 0.08, Student's T-test). The ORs were as follows: Male: OR 3.00, 95% CI 2.33–3.86, I2 = 95%, p < 0.00001; Female: OR 19.97, 95% CI 2.39–166.93, I2 = 81%, p = 0.006.
The relationship between post-mTBI depression and injury etiology was tested by stratifying studies as sport mTBI (17 studies, n = 4,827), military-related mTBI (including blast-related brain injury; 34 studies, n = 75,348), MVAs (nine studies, n = 30,043), and mTBIs uncategorized or of unspecified etiology (36 studies, n = 311,687). There was no statistical difference in the OR of depression relative to any mTBI etiology (p = 0.61, one-way ANOVA). The ORs for each category were as follows: sports-related injury: OR 3.51, 95% CI 2.01–6.11, I2 = 78%, p < 0.00001; military injury: OR 3.19, 95% CI 2.36–4.32, I2 = 96%, p < 0.00001; MVA: OR 2.3, 95% CI 1.36–3.88, I2 = 81%, p = 0.002; other injury: OR 3.26, 95% CI 2.45–4.35, I2 = 88%, p < 0.00001.
Repetitive injuries were reported in 35/82 (41%) of studies, with 30 (86%) of these studies reporting a majority of subjects with repetitive mTBIs. The odds of depression after repetitive or single mTBI were identical, with an OR for repetitive injuries of 3.66 (95% CI 2.56–5.22, I2 = 90%, p < 0.00001) and an OR for single injuries of 3.48 (95% CI 2.56–5.73, I2 = 96%, p < 0.00001).
The impact of the most frequently utilized six depression assessment methods on OR of depression after mTBI is presented in eResults 2, with no statistical difference in the OR of depression relative to assessment method. The influence of study design (cohort or cross-sectional) is presented in eResults 3, with no statistical difference observed in the odds of depression between these study designs.
Risk of bias is presented in Figure 4 (and eTable 2, in full), with bias risk expressed as a percentage for each assessed item. Risk of bias was greatest for multiple assessment of mTBI exposure (reported in <25% of studies), provision of CIs, and blinding of assessment, which was infrequently reported. The vast majority of studies reported a clear objective, had an appropriate and well-defined control group, and used validated measures of depression and mTBI, with an overall evaluation of low risk of bias and high applicability of results. A funnel plot of the pooled data (eFigure 3) demonstrated substantial asymmetry, representing publication bias. The majority of studies were clustered in the top section of the plot, indicative of more precise effect estimates, with a low number of low-powered studies reporting ORs <1. Orwin's Failsafe-N formula (17) showed that 115 additional studies with an OR of 1.0 would be required to decrease the effect size below a Cohen's d of 0.5.
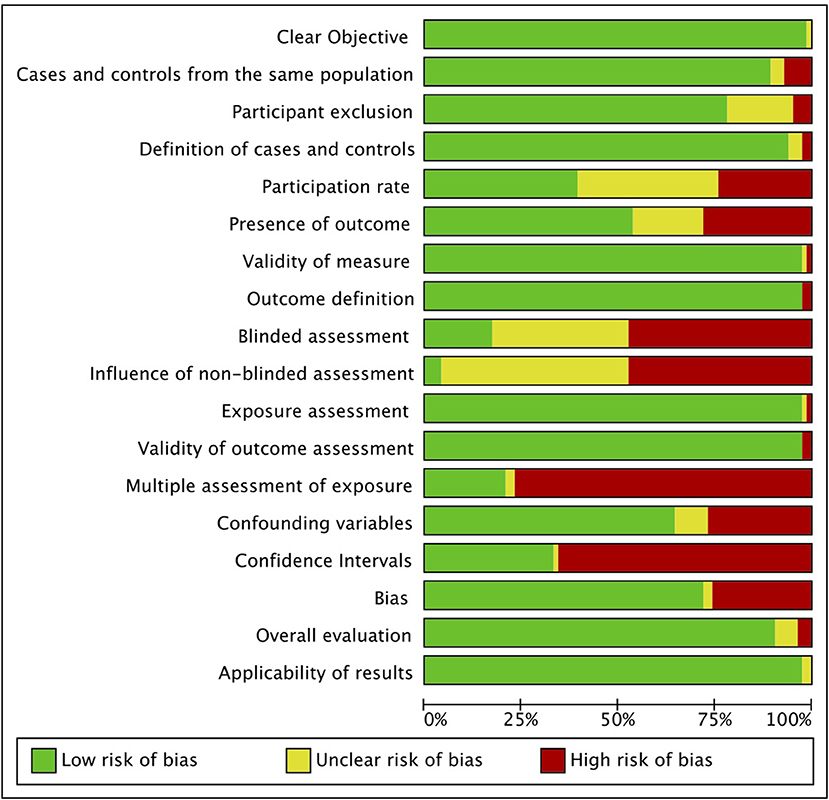
Figure 4. Risk of bias graph. Authors' judgments for each risk of bias item are presented as percentages across all included studies.
In this meta-analysis of 82 studies and 392,834 participants (96,709 mTBI subjects and 296,125 controls), we found that the OR for depression associated with mTBI (more than 6 months post-injury) was 3.29 when compared with those without a history of mTBI. Given the substantial prevalence of concussion in society, mTBI should now be considered as a significant driver of the overall population risk of depression.
A key secondary finding was that odds of depression occurring after mTBI are maintained or may even increase with chronicity and do not dissipate in the acute or subacute period. This finding indicates that “mild” TBI has repercussions extending over years, if not decades across a lifetime. Depression in the chronic recovery phase has been most frequently reported for moderate or severe injuries (102), likely because the higher degree of clinical management and follow-up these patients require renders them more accessible to researchers. In contrast to TBIs classed as moderate or severe, those experiencing mTBI are typically discharged rapidly with no or only short-term follow-up. The current Centers for Disease Control and Prevention guidelines (103) specify that patients with isolated mTBI and normal neurological evaluation can be discharged if head CT is negative, with no follow-up required unless post-concussive symptoms persist.
The consensus has been that the emotional sequelae of mTBI generally resolve by 12 weeks post-injury (104). Our data provide the first large-scale evidence to contradict this notion, highlighting a need for management strategies for mTBI to be reexamined. Further comprehensive longitudinal studies are required to elucidate this chronology. To date, a single longitudinal study has documented chronological rates of depression after TBI, following subjects (n = 423) monthly or every 2 months over a year (105). The authors found that depression was transient acutely but reemerged in the chronic phase, with a prevalence of 31% at 1 month and 21% at 6 months. This supports previous work suggesting that post-mTBI depression is biphasic, with transient symptomology acutely (13, 105) and a reemergence chronically (106). Together with this finding, our data highlight the importance of longitudinal assessment to thoroughly characterize emotional disturbance beyond the acute and subacute recovery phases (107).
We found no significant relationship between depression and the age at which mTBI occurred, although the pooled OR for those aged 25–35 years was numerically higher than those aged under 25. Several studies have now demonstrated a relationship between age at injury and risk of depression (12, 14, 105), whereby experiences of depression increase with advancing age. Although poorly understood, this may be influenced by a decrease in synaptic pruning, reduced neural plasticity, and/or diminished neurogenesis (108) as accompaniments to both depression and older age. Further research is required to determine whether a specific age vulnerability to post-mTBI depression truly exists, with potential need for age-specific management guidelines.
The role of biological sex in mTBI outcome is one of growing interest as females increasingly participate in collision sports and combat roles in military operations. Of 82 studies we included, only two exclusively examined females, while 24 focused only on male subjects. Given the disparity in outcome recoveries (11), more research is clearly needed to identify sex-specific consequences of mTBI. Including studies with more than 70% of either sex, we did not observe a statistical difference in depression, although the pooled OR for females was higher than males. There was substantial disparity between the number of subjects in these studies, potentially increasing the CIs. Ambiguity exists around the susceptibility of female sex to post-TBI depression, with several studies reporting increased post-mTBI depression in females (12, 109), while others have found no such relationship (13).
Blast neurotrauma and militarily acquired injuries are often excluded in meta-analyses on the assumption that these are polytrauma cases with a complicated pathology. We chose to include military injuries in our analysis to provide a full assessment of the scope of depression post-mTBI without imposing any prior assumptions on the data. While the injury modality may differ, many of these forms are also likely to include a polytrauma component (e.g., MVA, assaults) or have injury multipliers, as is the case for collision sports in which the concussed subject lands heavily on the ground. We found that the OR for depression in the chronic recovery phase was comparable no matter the etiology, suggesting that the mode of injury is not a significant factor in post-mTBI depression. This finding echoes two recent studies comparing blast vs. non-blast TBI, which reported similarities in the rate of post-traumatic outcomes (61, 110).
We also found that, at present, there is no compelling evidence for a cumulative effect of mTBI on post-mTBI depression, though further research is certainly required. Repetitive mTBI was documented almost entirely in the sports or military mTBI categories, for which subjects may experience many mTBIs across a career. The influence of repetitive injuries on emotional outcomes is one of contention, with several publications [including a recent systematic review of 47 studies (111)] finding that repetitive mTBI is associated with deteriorating mental health (56, 87), while others have found little psychological consequences of repeated injuries (112).
Our findings should be considered in the context of several important limitations. First, bias in subject selection may have been present in these longer-term studies either by direct selection of patients for which post-concussive symptoms predominates or selection bias due to lingering problems. We found that studies overwhelmingly focused on young adults and the middle aged rather than older participants, and thus our findings may not extend to post-mTBI depression in elderly participants who are more likely to sustain mTBI from other causes, e.g., falls. We also chose not to include pediatric populations, which would require a separate analysis to examine post-mTBI depression in the context of neurodevelopment. Participants in included studies may also have experienced concomitant disorders such as anxiety or posttraumatic stress disorder (PTSD), which might influence results toward an increase or decrease in risk (11). A key inclusion criterion for our research was the presence of a validated instrument to assess the likely presence or absence of depression, chosen to ensure a maximal synthesis of the available data. Aside from structured interviews, a general limitation of these instruments is their lack of confirmatory diagnoses. However, symptom-based scales are frequently used as screening tools for depression and are unlikely to give false negatives. We also did not specify a particular severity of depression in order to avoid bias introduced by any possible threshold effect. We excluded studies for which lifetime or pre-injury depression status was documented; however, the presence of pre-injury depression could not be ruled out for the majority of studies, and therefore we cannot be certain that depression only emerged after injury. To answer this, future studies would need to employ a longitudinal design in a non-injured population (e.g., sportspeople or military) with thorough lifetime assessment of depression and monitor emergence of depression over months and years post-injury.
Our inclusion of studies with a mean time post-injury of 6 months meant that few studies had a lower time limit of <6 months. The majority of studies we included were non-randomized cohort, case-control, cross-sectional, and prospective observational studies, and the inherent heterogeneity and risk of bias for such studies (as compared to randomized controlled trials) should be weighed in context of our findings. While the risk of bias overall was low, we found significant heterogeneity and publication bias, with the majority of high-powered studies showing either a positive or negative effect coupled with small standard errors. A small number of studies were low powered with positive findings; there were no low-powered negative studies that met our inclusion criteria. This is likely a consequence of “file-drawer” bias, for which smaller studies with negative findings are less likely to be published. Using Orwin's Failsafe-N formula, we found that an additional 115 low-powered negative studies would be required to skew the data toward the null hypothesis, providing confidence that our findings are robust. The high degree of between-study heterogeneity could not be explained by subgroup analyses and could potentially limit generalizability of the study results.
Our data show a positive relationship between mTBI and depression in the chronic phase of injury recovery. The size of this effect is substantial, representing a >3-fold increase in risk of depression after 6 months post-mTBI. This finding should prompt a reevaluation of our standard of care for 42 million mTBI cases occurring per year worldwide.
SH, CB, and SG conceived the study. SH and CB performed literature search. SH, CB, and TW reviewed literature for suitability to study criteria and collected data. SH, CB, TW, and SG analyzed the data, interpreted the data, and critically reviewed the manuscript. SH made figures. SH, TW, and SG wrote the manuscript.
This study was funded by NHMRC Grant 1130609. The funder had no role in writing, content, or decision to submit this manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors are grateful for the assistance of Jim Matthews and Maryam Montazerolghaem, statistical consultants at the Sydney Informatics Hub at the University of Sydney. SG acknowledges the support of the Heart Research Institute, Sydney Medical School, the Frecker Foundation, and the Parker-Hughes Bequest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2020.00350/full#supplementary-material
1. Cassidy JD, Carroll LJ, Peloso PM, Borg J, von Holst H, Holm L, et al. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. (2004) (43Suppl.):28–60. doi: 10.1080/16501960410023732
2. Kristman VL, Borg J, Godbolt AK, Salmi LR, Cancelliere C, Carroll LJ, et al. Methodological issues and research recommendations for prognosis after mild traumatic brain injury: results of the international collaboration on mild traumatic brain injury prognosis. Archiv Phys Med Rehabil. (2014) 95:S265–77. doi: 10.1016/j.apmr.2013.04.026
3. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury. J Head Trauma Rehabil. (2006) 21:375–8. doi: 10.1097/00001199-200609000-00001
4. Clarke LA, Genat RC, Anderson JFI. Long-term cognitive complaint and post-concussive symptoms following mild traumatic brain injury: the role of cognitive and affective factors. Brain Injury. (2012) 26:298–307. doi: 10.3109/02699052.2012.654588
5. van der Horn HJ, Liemburg EJ, Scheenen ME, de Koning ME, Marsman JB, Spikman JM, et al. Brain network dysregulation, emotion, and complaints after mild traumatic brain injury. Hum Brain Mapping. (2016) 37:1645–54. doi: 10.1002/hbm.23126
6. Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. (2008) 358:453–63. doi: 10.1056/NEJMoa072972
7. Haagsma JA, Scholten AC, Andriessen T, Vos PE, Van Beeck EF, Polinder S. Impact of depression and post-traumatic stress disorder on functional outcome and health-related quality of life of patients with mild traumatic brain injury. J Neurotrauma. (2015) 32:853–62. doi: 10.1089/neu.2013.3283
8. Theadom A, McDonald S, Starkey N, Barker-Collo S, Jones KM, Ameratunga S, et al. Social cognition 4 years after mild-TBI: an age-matched prospective longitudinal cohort study. Neuropsychology. (2019) 33:560–7. doi: 10.1037/neu0000516
9. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. (2015) 76:155–62. doi: 10.4088/JCP.14m09298
10. van Reekum R, Cohen T, Wong J. Can traumatic brain injury cause psychiatric disorders? J Neuropsychiatry Clin Neurosci. (2000) 12:316–27. doi: 10.1176/appi.neuropsych.12.3.316
11. Scholten AC, Haagsma JA, Cnossen MC, Olff M, van Beeck EF, Polinder S. Prevalence of and risk factors for anxiety and depressive disorders after traumatic brain injury: a systematic review. J Neurotrauma. (2016) 33:1969–94. doi: 10.1089/neu.2015.4252
12. Glenn MB, O'Neil-Pirozzi T, Goldstein R, Burke D, Jacob L. Depression amongst outpatients with traumatic brain injury. Brain Injury. (2001) 15:811–8. doi: 10.1080/02699050010025777
13. Roy D, Koliatsos V, Vaishnavi S, Han D, Rao V. Risk factors for new-onset depression after first-time traumatic brain injury. Psychosomatics. (2018) 59:47–57. doi: 10.1016/j.psym.2017.07.008
14. Rao V, Bertrand M, Rosenberg P, Makley M, Schretlen DJ, Brandt J, et al. Predictors of new-onset depression after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. (2010) 22:100–4. doi: 10.1176/jnp.2010.22.1.100
15. Albrecht JS, Barbour L, Abariga SA, Rao V, Perfetto EM. Risk of depression after traumatic brain injury in a large national sample. J Neurotrauma. (2019) 36:300–7. doi: 10.1089/neu.2017.5608
16. Frost RB, Farrer TJ, Primosch M, Hedges DW. Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology. (2013) 40:154–9. doi: 10.1159/000343275
17. Orwin RG. A fail-safe N for effect size in meta-analysis. J Edu Statistics. (1983) 8:157–9. doi: 10.2307/1164923
18. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. West Sussex: John Wiley & Sons (2009). doi: 10.1002/9780470743386
19. Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics Med. (2000) 19: 3127–31. doi: 10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M
20. The Cochrane Collaboration. Review Manager (RevMan). In: Collaboration TC, editor. Version 5.3. Copenhagen: The Nordic Cochrane Centre (2014).
21. Amick MM, Meterko M, Fortier CB, Fonda JR, Milberg WP, McGlinchey RE. The deployment trauma phenotype and employment status in veterans of the wars in Iraq and Afghanistan. J Head Trauma Rehabil. (2018) 33:E30–40. doi: 10.1097/HTR.0000000000000308
22. Astafiev SV, Zinn KL, Shulman GL, Corbetta M. Exploring the physiological correlates of chronic mild traumatic brain injury symptoms. NeuroImage. (2016) 11:10–9. doi: 10.1016/j.nicl.2016.01.004
23. Baker JG, Leddy JJ, Hinds AL, Haider MN, Shucard J, Sharma T, et al. An exploratory study of mild cognitive impairment of retired professional contact sport athletes. J Head Trauma Rehabil. (2018) 33:E16–23. doi: 10.1097/HTR.0000000000000420
24. Baldassarre M, Smith B, Harp J, Herrold A, High WM, Babcock-Parziale J, et al. Exploring the relationship between mild traumatic brain injury exposure and the presence and severity of postconcussive symptoms among veterans deployed to Iraq and Afghanistan. PM R. (2015) 7:845–58. doi: 10.1016/j.pmrj.2015.03.003
25. Barnes SM, Walter KH, Chard KM. Does a history of mild traumatic brain injury increase suicide risk in veterans with PTSD? Rehabil Psychol. (2012) 57:18–26. doi: 10.1037/a0027007
26. Bell BD, Primeau M, Sweet JJ, Lofland KR. Neuropsychological functioning in migraine headache, non-headache chronic pain, and mild traumatic brain injury patients. Archiv Clin Neuropsychol. (1999) 14:389–99. doi: 10.1093/arclin/14.4.389
27. Bomyea J, Lang AJ, Delano-Wood L, Jak A, Hanson KL, Sorg S, et al. Neuropsychiatric predictors of post-injury headache after mild-moderate traumatic brain injury in veterans. Headache. (2016) 56:699–710. doi: 10.1111/head.12799
28. Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. Am J Psychiatry. (2010) 167:312–20. doi: 10.1176/appi.ajp.2009.09050617
29. Callahan ML, Binder LM, O'Neil ME, Zaccari B, Roost MS, Golshan S, et al. Sensory sensitivity in operation enduring freedom/operation Iraqi freedom veterans with and without blast exposure and mild traumatic brain injury. Appl Neuropsychol. (2018) 25:126–36. doi: 10.1080/23279095.2016.1261867
30. Carrier-Toutant F, Guay S, Beaulieu C, Leveille E, Turcotte-Giroux A, Papineau SD, et al. Effects of repeated concussions and sex on early processing of emotional facial expressions as revealed by electrophysiology. J Int Neuropsychol Soc. (2018) 24:673–83. doi: 10.1017/S1355617718000231
31. Chi YC, Wu HL, Chu CP, Huang MC, Lee PC, Chen YY. Traumatic brain injury and affective disorder: a nationwide cohort study in Taiwan, 2000–2010. J Affective Disord. (2016) 191:56–61. doi: 10.1016/j.jad.2015.11.035
32. Chong CD, Berisha V, Chiang CC, Ross K, Schwedt TJ. Less cortical thickness in patients with persistent post-traumatic headache compared with healthy controls: an MRI study. Headache. (2018) 58:53–61. doi: 10.1111/head.13223
33. Coughlin JM, Yuchuanwang Y, Minn I, Bienko N, Ambinder EB, Xu X, et al. Imaging of glial cell activation and white matter integrity in brains of active and recently retired national football league players. JAMA Neurol. (2017) 74:67–74. doi: 10.1001/jamaneurol.2016.3764
34. Dailey NS, Smith R, Vanuk JR, Raikes AC, Killgore WDS. Resting-state functional connectivity as a biomarker of aggression in mild traumatic brain injury. Neuroreport. (2018) 29:1413–7. doi: 10.1097/WNR.0000000000001127
35. de Almeida Lima DP, Filho CS, de Campos Vieira Abib S, Poli de Figueiredo LF. Quality of life and neuropsychological changes in mild head trauma. Late analysis and correlation with S100B protein and cranial CT scan performed at hospital admission. Injury. (2008) 39:604–11. doi: 10.1016/j.injury.2007.11.008
36. Dean PJA, Sterr A. Long-term effects of mild traumatic brain injury on cognitive performance. Front Human Neurosci. (2013) 7:30. doi: 10.3389/fnhum.2013.00030
37. Decq P, Gault N, Blandeau M, Kerdraon T, Berkal M, ElHelou A, et al. Long-term consequences of recurrent sports concussion. Acta Neurochirurgica. (2016) 158:289–300. doi: 10.1007/s00701-015-2681-4
38. Didehbani N, Cullum CM, Mansinghani S, Conover H, Hart J. Depressive symptoms and concussions in aging retired NFL players. Archiv Clin Neuropsychol. (2013) 28:418–24. doi: 10.1093/arclin/act028
39. Dismuke-Greer CE, Nolen TL, Nowak K, Hirsch S, Pogoda TK, Agyemang AA, et al. Understanding the impact of mild traumatic brain injury on veteran service-connected disability: results from Chronic Effects of Neurotrauma Consortium. Brain Injury. (2018) 32:1178–87. doi: 10.1080/02699052.2018.1482428
40. Donnell AJ, Kim MS, Silva MA, Vanderploeg RD. Incidence of postconcussion symptoms in psychiatric diagnostic groups, mild traumatic brain injury, and comorbid conditions. Clin Neuropsychol. (2012) 26:1092–101. doi: 10.1080/13854046.2012.713984
41. Donnelly K, Donnelly JP, Warner GC, Kittleson CJ, King PR. Longitudinal study of objective and subjective cognitive performance and psychological distress in OEF/OIF Veterans with and without traumatic brain injury. Clin Neuropsychologist. (2018) 32:436–55. doi: 10.1080/13854046.2017.1390163
42. Drapeau J, Gosselin N, Peretz I, McKerral M. Emotional recognition from dynamic facial, vocal and musical expressions following traumatic brain injury. Brain Injury. (2017) 31:221–9. doi: 10.1080/02699052.2016.1208846
43. Dretsch MN, Silverberg ND, Iverson GL. Multiple past concussions are associated with ongoing post-concussive symptoms but not cognitive impairment in active-duty army soldiers. J Neurotrauma. (2015) 32:1301–6. doi: 10.1089/neu.2014.3810
44. Epstein DJ, Legarreta M, Bueler E, King J, McGlade E, Yurgelun-Todd D. Orbitofrontal cortical thinning and aggression in mild traumatic brain injury patients. Brain Behav. (2016) 6:581. doi: 10.1002/brb3.581
45. Gaines KD, Soper HV, Berenji GR. Executive functioning of combat mild traumatic brain injury. Appl Neuropsychol. (2016) 23:115–24. doi: 10.1080/23279095.2015.1012762
46. Gardner AJ, Iverson GL, Wojtowicz M, Levi CR, Kay-Lambkin F, Schofield PW, et al. MR spectroscopy findings in retired professional rugby league players. Int J Sports Med. (2017) 38:241–52. doi: 10.1055/s-0042-120843
47. Gill J, Mustapic M, Diaz-Arrastia R, Lange R, Gulyani S, Diehl T, et al. Higher exosomal tau, amyloid-beta 42 and IL-10 are associated with mild TBIs and chronic symptoms in military personnel. Brain Injury. (2018) 32:1359–66. doi: 10.1080/02699052.2018.1471738
48. Graham DP, Helmer DA, Harding MJ, Kosten TR, Petersen NJ, Nielsen DA. Serotonin transporter genotype and mild traumatic brain injury independently influence resilience and perception of limitations in veterans. J Psychiatric Res. (2013) 47:835–42. doi: 10.1016/j.jpsychires.2013.02.006
49. Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Harding HP Jr, Matthews A, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exercise. (2007) 39:903–9. doi: 10.1249/mss.0b013e3180383da5
50. Himanen L, Portin R, Tenovuo O, Taiminen T, Koponen S, Hiekkanen H, et al. Attention and depressive symptoms in chronic phase after traumatic brain injury. Brain Injury. (2009) 23:220–7. doi: 10.1080/02699050902748323
51. Hoot MR, Levin HS, Smith AN, Goldberg G, Wilde EA, Walker WC, et al. Pain and chronic mild traumatic brain injury in the US military population: a Chronic Effects of Neurotrauma Consortium study. Brain Injury. (2018) 32:1169–77. doi: 10.1080/02699052.2018.1482427
52. Iverson KM, Pogoda TK. Traumatic brain injury among women veterans an invisible wound of intimate partner violence. Med Care. (2015) 53:S112–9. doi: 10.1097/MLR.0000000000000263
53. Johansson B, Berglund P, Ronnback L. Mental fatigue and impaired information processing after mild and moderate traumatic brain injury. Brain Injury. (2009) 23:1027–40. doi: 10.3109/02699050903421099
54. Jurick SM, Hoffman SN, Sorg S, Keller AV, Evangelista ND, DeFord NE, et al. Pilot investigation of a novel white matter imaging technique in Veterans with and without history of mild traumatic brain injury. Brain Injury. (2018) 32:1256–65. doi: 10.1080/02699052.2018.1493225
55. Kerr ZY, Thomas LC, Simon JE, McCrea M, Guskiewicz KM. Association between history of multiple concussions and health outcomes among former college football players 15-year follow-up from the NCAA concussion study (1999–2001). Am J Sports Med. (2018) 46:1733–41. doi: 10.1177/0363546518765121
56. Kerr ZY, Marshall SW, Harding HP Jr, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. (2012) 40:2206–12. doi: 10.1177/0363546512456193
57. Konrad C, Geburek AJ, Rist F, Blumenroth H, Fischer B, Husstedt I, et al. Long-term cognitive and emotional consequences of mild traumatic brain injury. Psychol Med. (2011) 41:1197–211. doi: 10.1017/S0033291710001728
58. LaFrance WC, DeLuca M, Machan JT, Fava JL. Traumatic brain injury and psychogenic non-epileptic seizures yield worse outcomes. Epilepsia. (2013) 54:718–25. doi: 10.1111/epi.12053
59. Lee JEC, Garber B, Zamorski MA. Prospective analysis of premilitary mental health, somatic symptoms, and postdeployment postconcussive symptoms. Psychosomatic Med. (2015) 77:1006–17. doi: 10.1097/PSY.0000000000000250
60. Leveille E, Guay S, Blais C, Scherzer P, De Beaumont L. Sex-related differences in emotion recognition in multi-concussed athletes. J Int Neuropsychol Soc. (2017) 23:65–77. doi: 10.1017/S1355617716001004
61. Lippa SM, Fonda JR, Fortier CB, Amick MA, Kenna A, Milberg WP, et al. Deployment-related psychiatric and behavioral conditions and their association with functional disability in OEF/OIF/OND veterans. J Traumatic Stress. (2015) 28:25–33. doi: 10.1002/jts.21979
62. Losoi H, Silverberg ND, Waljas M, Turunen S, Rosti-Otajarvi E, Helminen M, et al. Recovery from mild traumatic brain injury in previously healthy adults. J Neurotrauma. (2016) 33:766–76. doi: 10.1089/neu.2015.4070
63. Mac Donald CL, Barber J, Jordan M, Johnson AM, Dikmen S, Fann JR, et al. Early clinical predictors of 5-years outcome after concussive blast traumatic brain injury. JAMA Neurol. (2017) 74:821–9. doi: 10.1001/jamaneurol.2017.0143
64. Mac Donald CL, Adam OR, Johnson AM, Nelson EC, Werner NJ, Rivet DJ, et al. Acute post-traumatic stress symptoms and age predict outcome in military blast concussion. Brain. (2015) 138:1314–26. doi: 10.1093/brain/awv038
65. MacGregor AJ, Dougherty AL, Tang JJ, Galarneau MR. Postconcussive symptom reporting among US combat veterans with mild traumatic brain injury from operation Iraqi freedom. J Head Trauma Rehabil. (2013) 28:59–67. doi: 10.1097/HTR.0b013e3182596382
66. Maruta J, Spielman LA, Yarusi BB, Wang Y, Silver JM, Ghajar J. Chronic post-concussion neurocognitive deficits. Ii. relationship with persistent symptoms. Front Human Neurosci. (2016) 10:45. doi: 10.3389/fnhum.2016.00045
67. Mickeviciene D, Schrader H, Nestvold K, Surkiene D, Kunickas R, Stovner LJ, et al. A controlled historical cohort study on the post-concussion syndrome. Eur J Neurol. (2002) 9:581–7. doi: 10.1046/j.1468-1331.2002.00497.x
68. Moller MC, de Boussard CN, Oldenburg C, Bartfai A. An investigation of attention, executive, and psychomotor aspects of cognitive fatigability. J Clin Exp Neuropsychol. (2014) 36:716–29. doi: 10.1080/13803395.2014.933779
69. Morey RA, Haswell CC, Selgrade ES, Massoglia D, Liu CL, Weiner J, et al. Effects of chronic mild traumatic brain injury on white matter integrity in Iraq and Afghanistan war veterans. Human Brain Mapping. (2013) 34:2986–99. doi: 10.1002/hbm.22117
70. Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, et al. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabil Psychol. (2011) 56:340–50. doi: 10.1037/a0025462
71. Newberg AB, Serruya M, Gepty A, Intenzo C, Lewis T, Amen D, et al. Clinical comparison of Tc-99m exametazime and I-123 ioflupane SPECT in patients with chronic mild traumatic brain injury. PLoS ONE. (2014) 9:9. doi: 10.1371/journal.pone.0087009
72. Nordhaug LH, Hagen K, Vik A, Stovner LJ, Follestad T, Pedersen T, et al. Headache following head injury: a population-based longitudinal cohort study (HUNT). J Headache Pain. (2018) 19:2. doi: 10.1186/s10194-018-0838-2
73. Olivera A, Lejbman N, Jeromin A, French LM, Kim HS, Cashion A, et al. Peripheral total tau in military personnel who sustain traumatic brain injuries during deployment. JAMA Neurol. (2015) 72:1109–16. doi: 10.1001/jamaneurol.2015.1383
74. Ozen LJ, Fernandes MA. Effects of “diagnosis threat” on cognitive and affective functioning long after mild head injury. J Int Neuropsychol Soc. (2011) 17:219–29. doi: 10.1017/S135561771000144X
75. Palombo DJ, Kapson HS, Lafleche G, Vasterling JJ, Marx BP, Franz M, et al. Alterations in autobiographical memory for a blast event in operation enduring freedom and operation iraqi freedom veterans with mild traumatic brain injury. Neuropsychology. (2015) 29:543–9. doi: 10.1037/neu0000198
76. Peskind ER, Petrie EC, Cross DJ, Pagulayan K, McCraw K, Hoff D, et al. Cerebrocerebellar hypometabolism associated with repetitive blast exposure mild traumatic brain injury in 12 Iraq war Veterans with persistent post-concussive symptoms. Neuroimage. (2011) 54:S76–82. doi: 10.1016/j.neuroimage.2010.04.008
77. Petrie EC, Cross DJ, Yarnykh VL, Richards T, Martin NM, Pagulayan K, et al. Neuroimaging, behavioral, and psychological sequelae of repetitive combined blast/impact mild traumatic brain injury in Iraq and Afghanistan war veterans. J Neurotrauma. (2014) 31:425–36. doi: 10.1089/neu.2013.2952
78. Pineau H, Marchand A, Guay S. Specificity of cognitive and behavioral complaints in post- traumatic stress disorder and mild traumatic brain injury. Behav Sci. (2015) 5:43–58. doi: 10.3390/bs5010043
79. Pogoda TK, Hendricks AM, Iverson KM, Stolzmann KL, Krengel MH, Baker E, et al. Multisensory impairment reported by veterans with and without mild traumatic brain injury history. J Rehabil Res Dev. (2012) 49:971–83. doi: 10.1682/JRRD.2011.06.0099
80. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Archiv General Psychiatry. (2011) 68:79–89. doi: 10.1001/archgenpsychiatry.2010.172
81. Raikes AC, Bajaj S, Dailey NS, Smith RS, Alkozei A, Satterfield BC, et al. Diffusion Tensor Imaging (DTI) correlates of self-reported sleep quality and depression following mild traumatic brain injury. Front Neurol. (2018) 9:468. doi: 10.3389/fneur.2018.00468
82. Raskin SA. The relationship between sexual abuse and mild traumatic brain injury. Brain Injury. (1997) 11:587–603. doi: 10.1080/026990597123287
83. Rogers JM, Fox AM, Donnelly J. Impaired practice effects following mild traumatic brain injury: an event-related potential investigation. Brain Injury. (2015) 29:343–51. doi: 10.3109/02699052.2014.976273
84. Schiehser DM, Delano-Wood L, Jak AJ, Hanson KL, Sorg SF, Orff H, et al. Predictors of cognitive and physical fatigue in post-acute mild-moderate traumatic brain injury. Neuropsychol Rehabil. (2017) 27:1031–46. doi: 10.1080/09602011.2016.1215999
85. Schoenhuber R, Gentilini M. Anxiety and depression after mild head injury: a case control study. J Neurol Neurosurgery Psychiatry. (1988) 51:722–4. doi: 10.1136/jnnp.51.5.722
86. Small GW, Kepe V, Siddarth P, Ercoli LM, Merrill DA, Donoghue N, et al. PET scanning of brain tau in retired national football league players: preliminary findings. Am J Geriatric Psychiatry. (2013) 21:138–44. doi: 10.1016/j.jagp.2012.11.019
87. Spira JL, Lathan CE, Bleiberg J, Tsao JW. The impact of multiple concussions on emotional distress, post-concussive symptoms, and neurocognitive functioning in active duty United States Marines Independent of Combat Exposure or Emotional Distress. J Neurotrauma. (2014) 31:1823–34. doi: 10.1089/neu.2014.3363
88. Sponheim SR, McGuire KA, Kang SS, Davenport ND, Aviyente S, Bernat EM, et al. Evidence of disrupted functional connectivity in the brain after combat-related blast injury. Neuroimage. (2011) 54:S21–9. doi: 10.1016/j.neuroimage.2010.09.007
89. Strigo IA, Spadoni AD, Inslicht SS, Simmons AN. Repeated exposure to experimental pain differentiates combat traumatic brain injury with and without post-traumatic stress disorder. J Neurotrauma. (2018) 35:297–307. doi: 10.1089/neu.2017.5061
90. Suhr JA, Gunstad J. Postconcussive symptom report: the relative influence of head injury and depression. J Clin Exp Neuropsychol. (2002) 24:981–93. doi: 10.1076/jcen.24.8.981.8372
91. Tarazi A, Tator CH, Wennberg R, Ebraheem A, Green REA, Collela B, et al. Motor function in former professional football players with history of multiple concussions. J Neurotrauma. (2018) 35:1003–7. doi: 10.1089/neu.2017.5290
92. Tremblay S, De Beaumont L, Henry LC, Boulanger Y, Evans AC, Bourgouin P, et al. Sports concussions and aging: a neuroimaging investigation. Cerebral Cortex. (2013) 23:1159–66. doi: 10.1093/cercor/bhs102
93. Vanderploeg RD, Curtiss G, Luis CA, Salazar AM. Long-term morbidities following self-reported mild traumatic brain injury. J Clin Exp Neuropsychol. (2007) 29:585–98. doi: 10.1080/13803390600826587
94. Vasterling JJ, Brailey K, Proctor SP, Kane R, Heeren T, Franz M. Neuropsychological outcomes of mild traumatic brain injury, post-traumatic stress disorder and depression in Iraq-deployed US Army soldiers. Br J Psychiatry. (2012) 201:186–92. doi: 10.1192/bjp.bp.111.096461
95. Vasterling JJ, Constans JI, Hanna-Pladdy B. Head injury as a predictor of psychological outcome in combat veterans. J Traumatic Stress. (2000) 13:441–51. doi: 10.1023/A:1007781107513
96. Verfaellie M, Lafleche G, Spiro A, Bousquet K. Neuropsychological outcomes in OEF/OIF veterans with self-report of blast exposure: associations with mental health, but not mTBI. Neuropsychology. (2014) 28:337–46. doi: 10.1037/neu0000027
97. Waljas M, Iverson GL, Lange RT, Hakulinen U, Dastidar P, Huhtala H, et al. A prospective biopsychosocial study of the persistent post-concussion symptoms following mild traumatic brain injury. J Neurotrauma. (2015) 32:534–47. doi: 10.1089/neu.2014.3339
98. Walker WC, Franke LM, Sima AP, Cifu DX. Symptom trajectories after military blast exposure and the influence of mild traumatic brain injury. J Head Trauma Rehabil. (2017) 32:E16–26. doi: 10.1097/HTR.0000000000000251
99. Walker WC, McDonald SD, Ketchum JM, Nichols M, Cifu DX. Identification of transient altered consciousness induced by military-related blast exposure and its relation to postconcussion symptoms. J Head Trauma Rehabil. (2013) 28:68–76. doi: 10.1097/HTR.0b013e318255dfd0
100. Waterloo K, Ingebrigtsen T, Romner B. Neuropsychological function in patients with increased serum levels of protein S-100 after minor head injury. Acta Neurochirurgica. (1997) 139:26–31. doi: 10.1007/BF01850864
101. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosomatic Med. (2012) 74:249–57. doi: 10.1097/PSY.0b013e318244c604
102. Dikmen SS, Machamer JE, Powell JM, Temkin NR. Outcome 3 to 5 years after moderate to severe traumatic brain injury. Archiv Phys Med Rehabil. (2003) 84:1449–57. doi: 10.1016/S0003-9993(03)00287-9
103. Jagoda AS, Bazarian JJ, Bruns JJ Jr, Cantrill SV, Gean AD, Howard PK, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emergency Med. (2008) 52:714–48. doi: 10.1016/j.annemergmed.2008.08.021
104. Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. (2015) 14:506–17. doi: 10.1016/S1474-4422(15)00002-2
105. Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. (2010) 303:1938–45. doi: 10.1001/jama.2010.599
106. Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and national guard soldiers 3 and 12 months following combat in Iraq. Archiv General Psychiatry. (2010) 67:614–23. doi: 10.1001/archgenpsychiatry.2010.54
107. Seel RT, Kreutzer JS, Rosenthal M, Hammond FM, Corrigan JD, Black K. Depression after traumatic brain injury: a national institute on disability and rehabilitation research model systems multicenter investigation. Archiv Phys Med Rehabil. (2003) 84:177–84. doi: 10.1053/apmr.2003.50106
108. Pittenger C, Duman RS. Stress, depression, and neuroplasticity: a convergence of mechanisms. Neuropsychopharmacology. (2007) 33:88. doi: 10.1038/sj.npp.1301574
109. Ashman TA, Spielman LA, Hibbard MR, Silver JM, Chandna T, Gordon WA. Psychiatric challenges in the first 6 years after traumatic brain injury: cross-sequential analyses of Axis I disorders. Archiv Phys Med Rehabil. (2004) 85(4 Suppl.2):S36–42. doi: 10.1016/j.apmr.2003.08.117
110. Wilk JE, Thomas JL, McGurk DM, Riviere LA, Castro CA, Hoge CW. Mild traumatic brain injury (concussion) during combat: lack of association of blast mechanism with persistent postconcussive symptoms. J Head Trauma Rehabil. (2010) 25:9–14. doi: 10.1097/HTR.0b013e3181bd090f
111. Manley G, Gardner AJ, Schneider KJ, Guskiewicz KM, Bailes J, Cantu RC, et al. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. (2017) 51:969. doi: 10.1136/bjsports-2017-097791
Keywords: depression, concussion, mild traumatic brain injury, chronic mild traumatic brain injury, meta-analysis
Citation: Hellewell SC, Beaton CS, Welton T and Grieve SM (2020) Characterizing the Risk of Depression Following Mild Traumatic Brain Injury: A Meta-Analysis of the Literature Comparing Chronic mTBI to Non-mTBI Populations. Front. Neurol. 11:350. doi: 10.3389/fneur.2020.00350
Received: 18 October 2019; Accepted: 08 April 2020;
Published: 19 May 2020.
Edited by:
Vassilis E. Koliatsos, Johns Hopkins University, United StatesReviewed by:
Alana Conti, Wayne State University, United StatesCopyright © 2020 Hellewell, Beaton, Welton and Grieve. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stuart M. Grieve, c3R1YXJ0LmdyaWV2ZUBzeWRuZXkuZWR1LmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.