
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol., 18 December 2018
Sec. Stroke
Volume 9 - 2018 | https://doi.org/10.3389/fneur.2018.01095
 Joong Hyun Park1
Joong Hyun Park1 Sang Won Han1
Sang Won Han1 Kyung-Yul Lee2
Kyung-Yul Lee2 Hye-Yeon Choi3
Hye-Yeon Choi3 Kyeongyeol Cheon2
Kyeongyeol Cheon2 Han-Jin Cho4
Han-Jin Cho4 Yo Han Jung5
Yo Han Jung5 Hyung Jong Park6
Hyung Jong Park6 Hyo Suk Nam6
Hyo Suk Nam6 Ji Hoe Heo6
Ji Hoe Heo6 Hye Sun Lee7
Hye Sun Lee7 Gustavo Saposnik8
Gustavo Saposnik8 Young Dae Kim6*
Young Dae Kim6*Introduction: Discontinuation of oral anticoagulants such as non-vitamin K antagonist oral anticoagulants (NOACs) may induce a hypercoagulable state, leading to severe stroke and poor outcomes. This study aimed to compare stroke outcomes between NOACs withdrawal and other prior medication statuses in patients with non-valvular atrial fibrillation (NVAF).
Methods: Consecutive patients who had pre-existing NVAF and were admitted for an acute ischemic stroke or transient ischemic attack- at five hospitals between January 2013 and December 2016 were included. Prior medication status was categorized into seven groups such as no antithrombotics, antiplatelet-only, warfarin with subtherapeutic intensity, warfarin with therapeutic intensity, NOAC, warfarin withdrawal, and NOAC withdrawal. We compared initial National Institute of Health Stroke Scale (NIHSS) scores between groups
Results: Among 719 patients with NVAF, The median NIHSS score at admission was 5 (IQR 1-13). The NOAC withdrawal group had the highest median NIHSS scores at stroke onset [16, interquartile range, IQR (1–17)], followed by the warfarin withdrawal group [11, IQR (1–14, 18)], the no antithrombotic group [5, IQR (1–13, 18, 19)], and the warfarin with subtherapeutic intensity group [5, IQR (1–10, 18, 19)]. A Multivariable analysis demonstrated that NOAC withdrawal was independently associated with higher NIHSS scores at stroke onset (B 4.645, 95% confidence interval 0.384–8.906, P = 0.033). The median interval from drug withdrawal to ischemic stroke or TIA was 7 days (IQR 4-15) in the NOAC group.
Conclusions: Stroke that occurred after stopping oral anticoagulants, especially NOAC, and was more severe at presentation and associated with poorer outcomes.
Non-valvular atrial fibrillation (NVAF) is the most common etiology of cardioembolic ischemic stroke (20). Although NVAF-related stroke is associated with an increased risk of stroke or fatal stroke, oral anticoagulation may effectively prevent ischemic events including an ischemic stroke or a transient ischemic attack (TIA) (19). Following the publication of studies which showed the benefits of non-vitamin K oral anticoagulants (NOACs) compared to warfarin, NOACs became widely used in clinical practice worldwide (1, 18).
The discontinuation of antithrombotics can be associated with an increased risk of cardiovascular events and poor outcomes (2, 3). Abrupt warfarin withdrawal may induce a rebound or a paradoxical prothrombotic state, subsequently leading to an increased incident risk of stroke for up to 3 months (4). Considering the potent anticoagulant effect of NOACs on the suppression of thrombogenesis, NOAC withdrawal may also be associated with severe stroke at presentation and poor outcomes in NVAF-related stroke. However, to date, there is limited information on the existence of this phenomenon.
The aim of this study was to compare the initial stroke severity associated with NOAC withdrawal to those associated with other prior medication statuses including warfarin withdrawal in patients with NVAF.
We retrospectively reviewed the medical records of consecutive patients with an acute ischemic stroke or TIA and NVAF, who were admitted within 7 days at the Department of Neurology at four regional stroke centers (Severance Stroke Center, Gangnam Severance Stroke Center, Kyung Hee University Hospital Stroke Center, and Inje Paik Hospital) and one general hospital (Changwon Fatima Hospital) between January 2013 and December 2016. During hospitalization, all patients underwent brain imaging and were managed through a standardized care pathway based on current guidelines. For each patient, demographic data, previous medical history, vascular risk factors, clinical manifestations, standard blood tests, and underlying vascular disease were systematically investigated.
This study was approved by the institutional review board at each participating hospital, and the requirement for informed consent was waived because the database was accessed only for analysis purposes and personal information was not used.
We collected data on demographics and traditional vascular risk factors such as hypertension, diabetes, dyslipidemia, and current smoking status (5). History of previous ischemic heart disease, congestive heart failure, peripheral arterial occlusive disease, or ischemic stroke was also investigated. TIA was defined as a transient episode of neurologic dysfunction caused by focal brain or retinal ischemia without acute infarction on a brain MRI including diffusion-weighted imaging. Data on international normalized ratio (INR) levels, lipid profile at admission, and creatinine clearance rate using the Cockcroft-Gault equation were collected. The blood levels of the NOACs were not measured in this study. We also calculated the CHA2DS2-VASc score in all patients based on their comorbid conditions (6). In patients with acute ischemic lesions on the brain imaging, we determined whether the stroke mechanism was caused by cardioembolism or if it had more than two causes according to the Trial of Org 10172 in Acute Stroke Treatment classification (7).
Based on medical records or interviews with the patients or their next of kin or caregiver, we determined the medication that was taken prior to the index stroke. Using data on the medications used prior to the stroke and the laboratory results at stroke presentation, we categorized the patients into seven groups as follows: (1) no antithrombotics, (2) antiplatelet-only, (3) warfarin with subtherapeutic intensity (INR < 2), (4) warfarin with therapeutic intensity (INR≥2), (5) NOAC, (6) warfarin withdrawal, and (7) NOAC withdrawal. Warfarin withdrawal and NOAC withdrawal were defined as those patients who had previously taken an oral anticoagulant but had discontinued the drug within 2 months before the index stroke (8). If a patient had stopped taking warfarin or NOACs, we determined the reason for the discontinuation. We also collected data on the prior use of statins before the index stroke.
We collected data on the initial stroke severity at stroke presentation. The neurological status of each patient during hospitalization was determined regularly at our study centers using the National Institute of Health Stroke Scale (NIHSS) scores which were obtained by a senior neurology resident or stroke specialist.
Statistical analysis was performed using the Windows SPSS package (version 23.0, IBM Corp., Armonk, NY, USA) and the R package (version 3.1.0, http://www.R-project.org). Categorical variables between groups were compared using the chi-square test or Fisher's exact test, while the independent t-test or Kruskall-Wallis test was used for the comparison of continuous variables. When we investigated whether NIHSS scores differed between the groups, Tobit analysis was used to determine the factors influencing initial stroke severity. Tobit regression was used to address the ceiling and floor effects noted in clinical outcomes (9). Using Tobit regression analysis adjusted for the potential confounders (P < 0.05 on univariable analysis), the independent association between prior antithrombotics and stroke severity was evaluated. Results were expressed as B (95% confidence intervals [CIs]) with the no antithrombotics group as the reference group. Finally, statistical significance was set at P < 0.05.
Of the 1,361 patients with atrial fibrillation who were admitted at the study hospitals during the study period, we excluded the patients with valvular heart disease (n = 66) and those with atrial fibrillation detected for the first time at hospitalization (n = 576). Finally, 719 patients with pre-existing NVAF (707 ischemic stroke and 12 TIA) were included in this study.
Mean age was 73.9 ±10.2 years, and 397 (55.2%) patients were male. Median CHA2DS2-VASc score was 4 (interquartile range [IQR] 3-5). There were 16 patients in the NOAC withdrawal group, 47 in the warfarin withdrawal group, 57 in the NOAC group, 31 in the warfarin with therapeutic intensity group, 130 in the warfarin with subtherapeutic intensity group, 298 in the antiplatelet-only group, and 140 in the no antithrombotic group. Differences in baseline characteristics are summarized in Table 1. The NOAC withdrawal group was more likely to have hypertension and higher CHA2DS2-VASc scores, while the NOAC group was more likely to have a history of ischemic heart disease or ischemic stroke and prior statin use (all P < 0.05).
The median interval from drug withdrawal to ischemic stroke or TIA was 7 days (IQR 4-15) in the NOAC group and 9 days (IQR 5-20) in the warfarin group (Figure 1). Among the 16 patients who had a stroke after NOAC withdrawal, it occurred in 6 patients after dabigatran discontinuation, 3 after apixaban discontinuation, and 7 after rivaroxaban discontinuation. Among the reasons for NOAC or warfarin cessation, recent bleeding event or self-discontinuation of drug without any specific medical reason was common (Table 2).
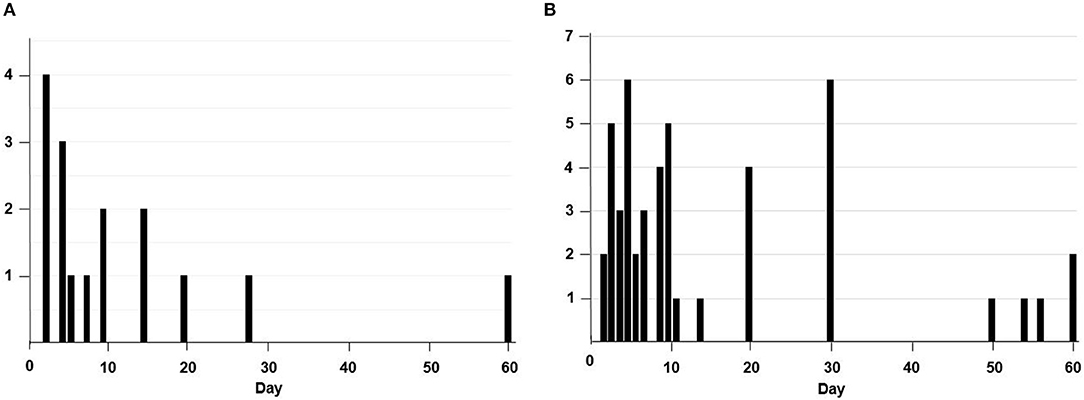
Figure 1. The number of patients who stopped taking non-vitamin K antagonist oral anticoagulans (A) or warfarin (B) according to the duration (days) of the discontinuation.
The median NIHSS score at admission was 5 (IQR 1-13). The NOAC withdrawal group had the highest median NIHSS score [16, IQR (1–17)], followed by the warfarin withdrawal group [11, IQR (1–14, 18)], the no antithrombotic group [5, IQR (1–13, 18, 19)], and the warfarin with subtherapeutic intensity group [5, IQR (1–10, 18, 19)] (Figure 2A and Table 3). When we categorized the stroke severity into three levels such as low (NIHSS ≤ 6), moderate (NIHSS 7-15), and severe (NIHSS ≥16), moderate to severe stroke was more common in NOAC withdrawal or warfarin withdrawal group (Figure 2B). There was no difference in initial NIHSS scores according to the reason for either NOAC withdrawal or warfarin withdrawal.
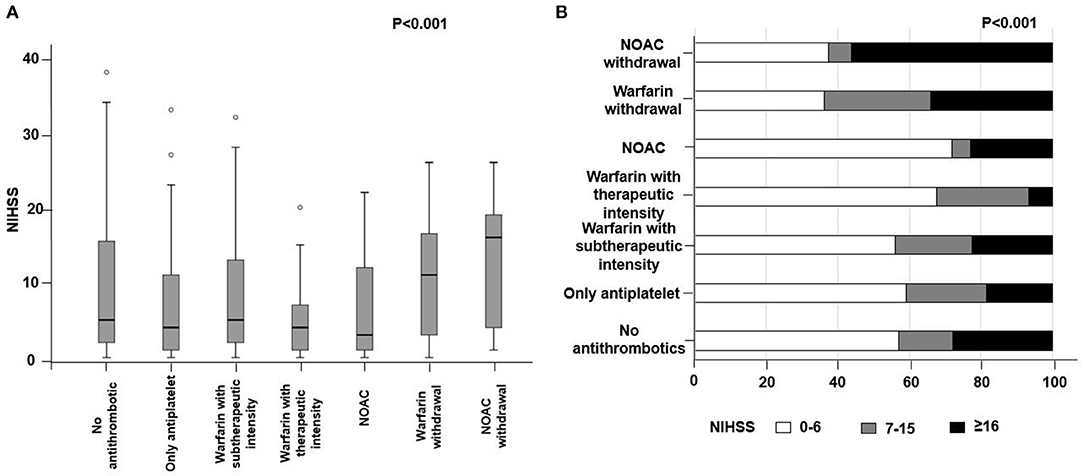
Figure 2. Difference in (A) initial National Institute of Health Stroke Scale (NIHSS) and (B) stroke severity according to the medication status. NOAC, non-vitamin K antagonist oral anticoagulant.
The multivariable Tobit regression analysis adjusting for the CHA2DS2-VASc score and current smoking status showed that NOAC withdrawal was independently associated with higher NIHSS scores (B 4.645, 95% CI 0.384–8.906, P = 0.033), while prior warfarin with therapeutic intensity (B −4.968, 95% CI −8.273 to −1.663, P = 0.003) and antiplatelets only (B −1.918, 95% CI −3.606 to −0.23, P = 0.033) were associated with lower NIHSS scores. The results remained consistent when we excluded patients with TIA (n = 12) (Table 3) or defined the withdrawal as stopping the drug within 1 month before the index stroke (Supplementary Table 1).
We conducted a large cohort study, compriised of stroke patients with NVAF, to determine the association of NOAC withdrawal and stroke outcomes. Our study revealed that withdrawal of oral anticoagulants, especially NOACs, was associated with higher NIHSS scores at stroke presentation in patients with NVAF. Stroke severity was relatively milder among patients on warfarin with therapeutic intensity or antiplatelets only.
Although there are several studies regarding the risk of thromboembolic events after stopping NOACs (2, 10, 11), the present study is the first to examine stroke characteristics in patients who experienced an ischemic stroke or TIA after abrupt NOAC withdrawal. Previous reports showed that abrupt discontinuation of anticoagulants could cause a rebound phenomenon involving a significant increase in procoagulant markers such as thrombin-antithrombin III complex, fibrinopeptide A and subsequently enhance thrombosis (4, 12, 13). In terms of NOAC withdrawal, some clinical trials, along with several anecdotal reports on patients with deep vein thrombosis or knee replacement surgery, suggested a potential prothrombotic rebound phenomenon after NOAC withdrawal. Most thromboembolic events occurred soon (median 1–2 weeks) following the cessation of dabigatran or rivaroxaban (2, 10, 11, 14, 15). In our study, the median interval between NOAC withdrawal and ischemic events was also 7 days, which may imply the occurrence of a rebound phenomenon associated with NOAC withdrawal.
In our study, stroke severity at presentation was most severe in the NOAC withdrawal group, followed by the warfarin withdrawal group, while prior use of warfarin with therapeutic intensity or antiplatelets alone were associated with lower NIHSS scores. There are some potential explanations to understand this phenomenon. Stroke severity in NVAF is strongly correlated with thrombus characteristics determined by the prothrombotic state in the left atrium and the anticoagulant activity (16, 17). The anticoagulant effect of NOAC decreases rapidly after 12–24 h (21). The transient hypercoagulable state caused by abrupt anticoagulant withdrawal may enhance thrombogenesis, leading to larger sized thrombi. Moreover, thrombin overproduced after cessation of anticoagulation by itself may promote excitotoxic neuronal injury (22, 23). Considering the higher NIHSS scores in the NOAC withdrawal group than in the warfarin withdrawal group, NOAC withdrawal may more strongly suppress thrombin/thrombin activity generation. Together with coagulation activity, thrombus formation in AF can be influenced by other factors including platelet activity (24). The prior use of antiplatelets may prevent thrombus formation in the left atrium and be associated with a milder stroke, although it was not found to be superior to the optimal anticoagulant therapy (25, 26). These assumptions regarding changes in coagulation and platelet activity support our results that demonstrate differences in stroke severity at stroke presentation according to prior medication status.
Although the NOACs have many benefits for clinical use including a fixed dose without the need for frequent monitoring, dietary precautions, and bridging therapy, NOAC use is not always well-maintained in actual clinical practice (18, 27, 28). Among patients requiring NOAC withdrawal because of a planned invasive procedure, the duration of the medication interruption seemed to be prolonged in clinical practice (2). In our study cohort, many patients who stopped medication because of a scheduled invasive procedure, did not re-start medication for a prolonged period, as the time between anticoagulant withdrawal and the ischemic event was found to be long (ranged between 5–20 days in patients using NOACs and 3–56 days in patients using warfarin). Furthermore, patients often stopped anticoagulants without any medical reason. Current guidelines indicated that it is not necessary to discontinue anticoagulant treatment during a low bleeding risk procedure such as dental procedures or diagnostic endoscopy (29). In addition, 18% (3/18) in the NOAC withdrawal group and 17% (8/47) in the warfarin withdrawal group discontinued in these situations. In our study population, 31% in the NOAC withdrawal group and 60% in the warfarin withdrawal group had not specific a medical reason. To improve adherence to medication, the implementation of educational programs and tools to help identify the patients who are more likely to be non-compliant is necessary (18).
Our study had several limitations. First, although we collected data on prior medication status for each patient, there is a possibility that some stroke patients were missed after stopping medication owing to patients' neurologic deficits, especially language dysfunction. However, it was routine practice in our study hospitals for physician or nurses to inquire about the prior medication status at the time of admission with their next of kin or caregiver as well as with the patients themselves. Second, the number of patients included the NOAC withdrawal group was not large in this retrospective study, which could lead to selection bias. The number of TIA patients was also small. In this study, TIA was diagnosed based on a tissue-based definition, not a time-based definition. Previous studies demonstrated that the acute ischemic lesion was detected in over 50% of TIA patients (30). Nearly all patients underwent the brain magnetic resonance image including DWI in this study. Further, although it was not difficult for TIA patients to be admitted to the hospital in Korea, there was still a possibility that TIA patients might be managed on the outpatient clinic, rather than being hospitalized (31). This might have led to the small number of TIA patients in our study population. Third, we did not thoroughly investigate the reason why oral anticoagulation was not resumed. Fourth, this study enrolled only Korean patients, which limited the generalizability of the study findings to other geographic regions or ethnic groups.
Our findings demonstrated that stroke occurred after discontinuing oral anticoagulant medication, especially NOACs, which was independently associated with severe stroke at presentation. Although NOACs offer many advantages for long-term use in patients with NVAF, concerns of adhering to or persisting with NOACs are warranted and physicians should avoid discontinuation of NOACs for prolonged periods (more than 7 days). The reason for NOAC and warfarin withdrawal was unknown in 3 to 6 out of 10 patients with NVAF. Our results revealed the potential harm of NOAC withdrawal which may be useful for physicians to better educate patients and improve the quality of anticoagulation therapy such that effective prevention of thromboembolic events can be achieved in patients with NVAF.
JP acquired, analyzed, and interpreted the data, and wrote the original manuscript draft. SH, K-YL, H-YC, KC, H-JC, YJ, and HP acquired and interpreted the data. HN, JH, and GS interpreted the data and provided a critical revision of the manuscript for intellectual content. HL analyzed and interpreted the data. YK conceptualized and designed the study, analyzed and interpreted the data, and provided critical revision of the manuscript for intellectual content.
This work was supported by a grant from the Korea Heath Technology R&D Project through the Korea Health Industry Development (KHIDI), funded by the Ministry of Health & Welfare, Republic from Korea (HI08C2149) and a faculty research grant from the Yonsei University College of Medicine (6-2017-0128).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2018.01095/full#supplementary-material
1. Ntaios G, Papavasileiou V, Makaritsis K, Vemmos K, Michel P, Lip GYH. Real-World setting comparison of nonvitamin-K antagonist oral anticoagulants versus vitamin-K antagonists for stroke prevention in atrial fibrillation: a systematic review and meta-analysis. Stroke (2017) 48:2494–503. doi: 10.1161/STROKEAHA.117.017549
2. Vene N, Mavri A, Gubenšek M, Tratar G, ViŽintin Cuderman T, Pohar Perme M, et al. Risk of thromboembolic events in patients with non-valvular atrial fibrillation after dabigatran or rivaroxaban discontinuation – data from the ljubljana registry. PLoS ONE (2016) 11:e0156943. doi: 10.1371/journal.pone.0156943
3. Kim JM, Jung KH, Kim TJ, Lee KJ, Han JY, Roh JK. Impact of stroke after antithrombotics withdrawal on early neurological deterioration. Int J Stroke (2015) 10:E42. doi: 10.1111/ijs.12504
4. Genewein U, Haeberli A, Straub PW, Beer JH. Rebound after cessation of oral anticoagulant therapy: the biochemical evidence. Br J Haematol. (1996) 92:479–85.
5. Kim YD, Jung YH, Saposnik G. Traditional risk factors for stroke in East Asia. J Stroke (2016) 18:273–85. doi: 10.5853/jos.2016.00885
6. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest (2010) 137:263–72. doi: 10.1378/chest.09-1584
7. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke (1993) 24:35–41.
8. Broderick JP, Bonomo JB, Kissela BM, Khoury JC, Moomaw CJ, Alwell K, et al. Withdrawal of antithrombotic agents and its impact on ischemic stroke occurrence. Stroke (2011) 42:2509–14. doi: 10.1161/STROKEAHA.110.611905
9. Tobin J. Estimation of relationships for limited dependent variables. Econometrica (1958) 26:24–36. doi: 10.2307/1907382
10. Patel MR, Hellkamp AS, Lokhnygina Y, Piccini JP, Zhang Z, Mohanty S, et al. Outcomes of discontinuing rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: analysis from the ROCKET AF trial (Rivaroxaban Once-Daily, Oral, Direct Factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation). J Am Coll Cardiol. (2013) 61:651–8. doi: 10.1016/j.jacc.2012.09.057
11. Van Thiel D, Kalodiki E, Wahi R, Litinas E, Haque W, Rao G. Interpretation of benefit-risk of enoxaparin as comparator in the RECORD program: rivaroxaban oral tablets (10 milligrams) for use in prophylaxis in deep vein thrombosis and pulmonary embolism in patients undergoing hip or knee replacement surgery. Clin Appl Thromb Hemost. (2009) 15:389–94. doi: 10.1177/1076029609340163
12. Grip L, Blomback M, Schulman S. Hypercoagulable state and thromboembolism following warfarin withdrawal in post-myocardial-infarction patients. Eur Heart J. (1991) 12:1225–33.
13. Perzborn E, Heitmeier S, Buetehorn U, Laux V. Direct thrombin inhibitors, but not the direct factor Xa inhibitor rivaroxaban, increase tissue factor-induced hypercoagulability in vitro and in vivo. J Thromb Haemost. (2014) 12:1054–65. doi: 10.1111/jth.12591
14. Agarwal A, Patel A, Mufti O, Jbara Y, Jabbar AA. Rivaroxaban rebound acute coronary event: a post marketing experience. Cardiol Res. (2013) 4:207–10. doi: 10.4021/cr294w
15. Nagasayi S, Varman S, Ting YY, Ang W. Rivaroxaban withdrawal and rebound hypercoagulability leading to upper extremity deep vein thrombosis: a case report. Age Age. (2017) 46:870–1. doi: 10.1093/ageing/afx073
16. Yoo J, Song D, Baek JH, Kim YD, Nam HS, Hong GR, et al. Poor outcome of stroke patients with atrial fibrillation in the presence of coexisting spontaneous echo contrast. Stroke (2016) 47:1920–2. doi: 10.1161/STROKEAHA.116.013351
17. Kim YD, Park B, Cha MJ, Nam CM, Nam HS, Ha JW, et al. Stroke severity in concomitant cardiac sources of embolism in patients with atrial fibrillation. J Neurol Sci. (2010) 298:23–7. doi: 10.1016/j.jns.2010.08.011
18. Raparelli V, Proietti M, Cangemi R, Lip GY, Lane DA, Basili S. Adherence to oral anticoagulant therapy in patients with atrial fibrillation. Focus on non-vitamin K antagonist oral anticoagulants. Thromb Haemost. (2017) 117:209–18. doi: 10.1160/TH16-10-0757
19. López-López JA, Sterne JAC, Thom HHZ, Higgins JPT, Hingorani AD, Okoli GN, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ (2017) 359:j5058. doi: 10.1136/bmj.j5058
21. Laliberte F, Nelson WW, Lefebvre P, Schein JR, Rondeau-Leclaire J, Duh MS. Impact of daily dosing frequency on adherence to chronic medications among nonvalvular atrial fibrillation patients. Adv Ther. (2012) 29:675–90. doi: 10.1007/s12325-012-0040-x
22. Chen B, Friedman B, Whitney MA, Winkle JAV, Lei I-F, Olson ES, et al. Thrombin activity associated with neuronal damage during acute focal ischemia. J Neurosci. (2012) 32:7622–31. doi: 10.1523/jneurosci.0369-12.2012
23. Sheehan JJ Tsirka SE Fibrin-modifying serine proteases thrombin tPA and plasmin in ischemic stroke: a review. Glia (2005) 50:340–50. doi: 10.1002/glia.20150
24. Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet (2009) 373:155–66. doi: 10.1016/S0140-6736(09)60040-4
25. Investigators A, Connolly SJ, Pogue J, Hart RG, Hohnloser SH, Pfeffer M, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. (2009) 360:2066–78. doi: 10.1056/NEJMoa0901301
26. Xian Y, O'Brien EC, Liang L, Xu H, Schwamm LH, Fonarow GC, et al. Association of preceding antithrombotic treatment with acute ischemic stroke severity and in-hospital outcomes among patients with atrial fibrillation. JAMA (2017) 317:1057–67. doi: 10.1001/jama.2017.1371
27. Yao X, Abraham NS, Alexander GC, Crown W, Montori VM, Sangaralingham LR, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. (2016) 5:e003074. doi: 10.1161/JAHA.115.003074
28. Borne RT, O'Donnell C, Turakhia MP, Varosy PD, Jackevicius CA, Marzec LN, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. (2017) 17:236. doi: 10.1186/s12872-017-0671-6
29. Nematullah A, Alabousi A, Blanas N, Douketis JD, Sutherland SE. Dental surgery for patients on anticoagulant therapy with warfarin: a systematic review and meta-analysis. J Can Dent Assoc. (2009) 75:41.
30. Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke (2009) 40:2276–93. doi: 10.1161/STROKEAHA.108.192218
Keywords: stroke, non-valvular atrial fibrillation, outcome, cardiac embolism, anticoagulation
Citation: Park JH, Han SW, Lee K-Y, Choi H-Y, Cheon K, Cho H-J, Jung YH, Park HJ, Nam HS, Heo JH, Lee HS, Saposnik G and Kim YD (2018) Impact of Non-vitamin K Antagonist Oral Anticoagulant Withdrawal on Stroke Outcomes. Front. Neurol. 9:1095. doi: 10.3389/fneur.2018.01095
Received: 15 October 2018; Accepted: 29 November 2018;
Published: 18 December 2018.
Edited by:
Antonio Arauz, Instituto Nacional de Neurología y Neurocirugía (INNN), MexicoReviewed by:
Christoph Gumbinger, Universität Heidelberg, GermanyCopyright © 2018 Park, Han, Lee, Choi, Cheon, Cho, Jung, Park, Nam, Heo, Lee, Saposnik and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Young Dae Kim, bmV1cm8wNUB5dWhzLmFj
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.