- 1Department of Psychology, University of Memphis, Memphis, TN, United States
- 2Neuroalgology Division, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
- 3Neurology, Public Health and Disability Unit, Fondazione IRCCS Istituto Neurologico Carlo Besta, Neurology, Milan, Italy
Headache disorders are common in children and adolescents. Most of the studies on non-pharmacological treatments have however been carried out on adults. In this review we provide information on recent studies examining non-pharmacological approaches for managing headache in children and adolescents. Our search of SCOPUS for primary studies conducted between January 2010 and July 2018 uncovered 11 controlled studies, mostly addressing behavioral approaches, in which a total of 613 patients with a diagnosis of primary headache, and average age 10.2–15.7 years (30–89% females) were recruited. Non-pharmacological treatments were shown to produce sizeable effects on the classical primary endpoint, i.e., headache frequency, with reductions from baseline ranging between 34 and 78%. Among commonly reported secondary endpoints, particularly disability, quality of life, depression and anxiety, marked improvements were noted as well. Taken as a whole, our findings suggest that non-pharmacological treatments constitute a valid option for the prevention of primary headaches in young age. Future research with higher-quality studies is needed. Particular attention needs to be given to studies that randomize patients to condition, blind researchers in charge of evaluating treatment outcomes, routinely include headache frequency as the primary endpoint, include adequate-length follow-up, address changes in biomarkers of disease and other possible mediators of outcome, and that employ predictive models to enhance the level of evidence for these approaches.
Introduction
Headache disorders are common in children and adolescents, affecting up to 88% of the pediatric and adolescent population, with chronic headache types impacting up to 6% (1, 2). Headache can result in significant disability, including missed school days and limitations in extracurricular activities, such as social events with peers, family gatherings, and sports. Pharmacological treatment for acute episodes typically include non-steroidal anti-inflammatory drugs (NSAIDs), analgesics, and triptans. As with adults, appropriate administration is needed in order to be effective, with specific attention being given to providing information about the risk for medication overuse headache (3). Among preventive drugs, antiepileptics such as topiramate, are considered as first-line treatment (4), and several drugs used in the prevention of migraine in adults are commonly prescribed for children (5, 6). Side effects of particular relevance for children and adolescents include weight loss or weight gain, paresthesias, cognitive slowing, and sleepiness. Caution is warranted in adolescent females in particular due to the elevated risk of developing polycystic ovarian syndrome as well as possible teratogenic effects of many of these compounds. Drug treatment, however, is not always needed, and prophylactic treatment is not considered the first line treatment in the vast majority of cases (6, 7). In recent years, attention has been increasingly paid to non-pharmacological treatments of headache disorders, chiefly those that are cognitive, behavioral, or psychophysiological in nature, but with some attention to non-invasive neurostimulation (8–11). Overall, significant benefits, typically ranging from 35 to 50%, have been reported for the above-mentioned treatments with respect to reductions in headache frequency. However, most of the published studies on non-pharmacological treatments have been carried out on adults, and more recent literature reviews have not focused extensively on young headache patients. The aim of the present review is to help fill this gap by providing updated information on more recent investigations of non-pharmacological approaches to the treatment of headache in children and adolescents.
Methods
Search Strategy
We performed a comprehensive search on SCOPUS covering the period January 2010–July 2018 to identify primary research papers reporting either randomized clinical trials (RCTs) or observational studies that addressed non-pharmacological approaches for headaches disorders in children and adolescents. The following combinations of key-words were searched within the titles, abstracts, or key-words provided:
• headache OR “tension type headache” OR migraine OR “chronic tension type headache” OR “chronic migraine” OR “medication overuse headache.”
• young OR adolesc* OR juvenile.
• “cognitive behavio* therapy” OR “acceptance and commitment therapy” OR ACT OR mindfulness OR biofeedback OR “relaxation training” OR “lifestyle modification*” OR “complementary alternative medicine” OR neuromodulation OR neurostimulation OR “single pulse transcranial magnetic stimulation” OR “repetitive transcranial magnetic stimulation” OR “transcutaneous supraorbital nerve stimulation” OR “non-invasive vagal nerve stimulation” OR “caloric vestibular stimulation” OR “sphenopalatine ganglion stimulation” OR “occipital nerve stimulation.”
• Our search was limited to original studies, published in English language peer-reviewed journals, and filtered by the following subject areas: Medicine, Neurosciences, Health Profession, Pharmacology, Toxicology and Pharmaceutics, Biochemistry, Genetics and Molecular Biology and Psychology. Finally, we filtered for other key-words clearly not germane to our topic (the detailed search strategy is included in Supplementary Materials).
Inclusion and Exclusion Criteria for Articles Selected
We specifically searched for clinical trials and observational studies, either cross-sectional or longitudinal, and excluded reviews, commentaries, letters to the editors, editorials, qualitative studies, case reports and small case series (< 10 subjects).
To be included papers needed to provide sufficient information to extract the following: impact of non-pharmacological treatment on headache frequency or other outcomes, such as disability or quality of life, as assessed by patient-reported outcomes measures (PROMs) and/or parent report. Studies further had to focus on the primary headache disorders of migraine or tension-type headache. Studies drawing from populations that included other types of headache disorders (mixed disorders), or wherein the presence of headache was addressed chiefly as a symptom in the context of other general medical conditions were excluded. Finally, studies that included both adolescents and young adults were excluded if the findings were reported in aggregate and it was not possible to disentangle the outcomes for the adolescents or if the average age of the sample suggested that the study was predominantly carried out in a population of adults.
Paper Selection and Data Extraction
Selected abstracts were screened by a single researcher (EG) and, in order to ensure quality and consistency of data extraction, 20% of the abstracts along with the full texts were randomly selected for a second evaluation conducted by another reviewer (AR or ES) who was blind to the initial decision. We determined at the outset if agreement rates were below 70%, each of the double-checked abstract or manuscript would be re-reviewed by the two researchers to arrive at a final decision by consensus (however, as will be seen below, this did not surface as a problem).
Extracted information included the kind of non-pharmacological approach employed, broadly defined in terms of Cognitive Behavioral Therapy (CBT), a mindfulness-based approache, Biofeedback (BFT) treatment, Transcranial Magnetic Stimulation (TMS) and Multimodal treatment. We also recorded the main characteristics of selected studies, which included sample size, percentage of females, mean age, headache frequency at baseline and at follow-up, percent reduction and, when available, clinical significance of outcomes. We converted reported values for headache frequency to conform to a standard, comparable monthly period when authors described it differently (e.g., on a 3-month basis).
Results
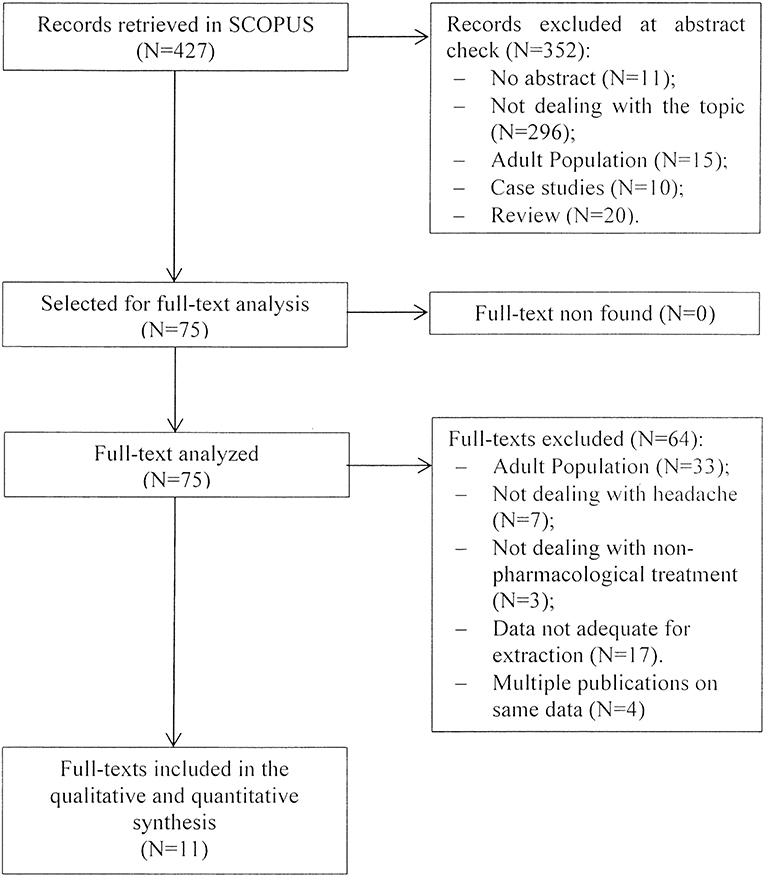
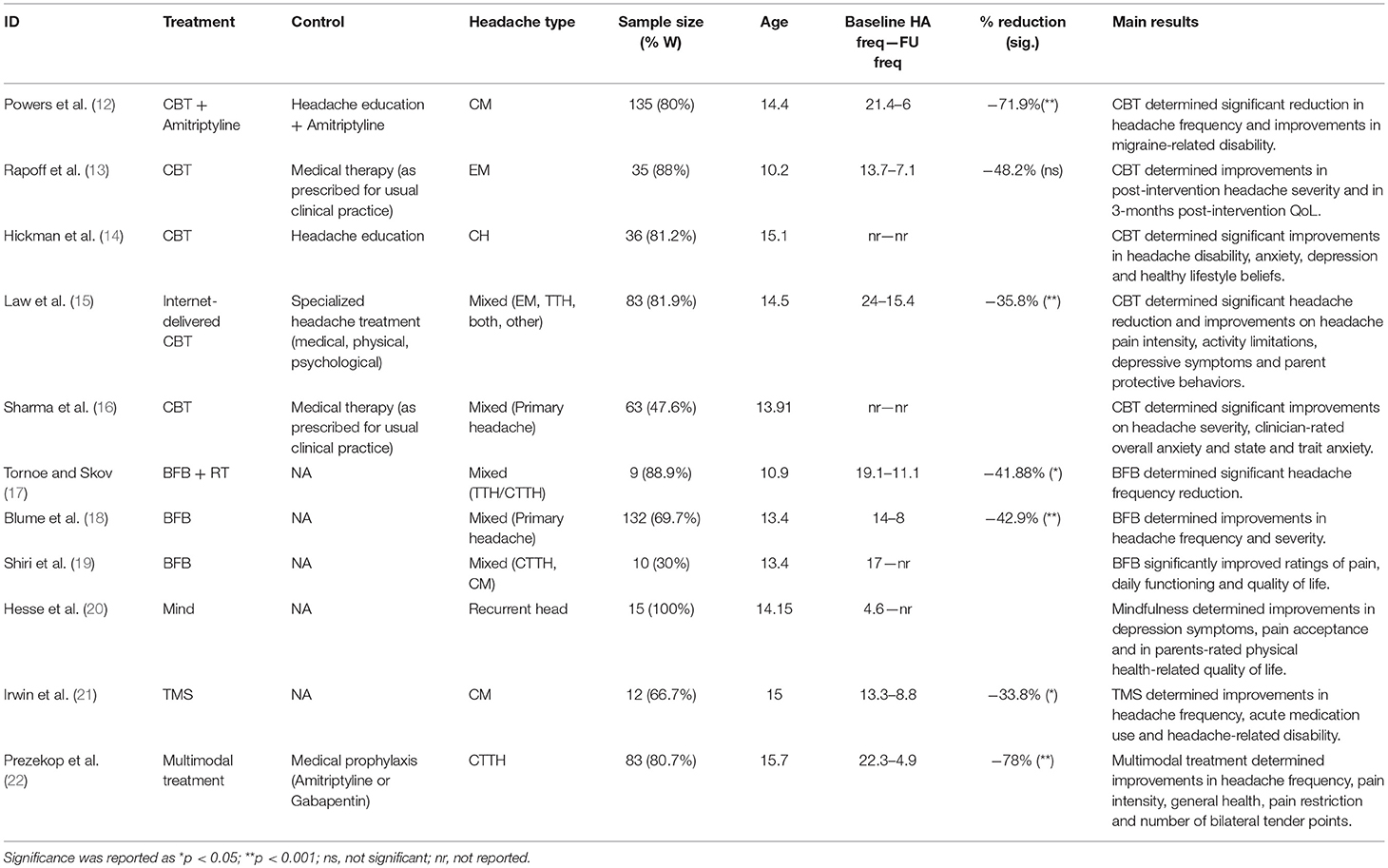
The initial search returned 427 records. Following abstract screening and full text assessment, 11 publications were selected for inclusion in this review (12–22). The rate of agreement between reviewers was 99.5% at the abstract check, and 100% at full-text check. Figure 1 shows the PRISMA flow diagram of our search process. Table 1 presents a summary of the main outcome of the publications included in this review.
Across the studies, 613 participants with a diagnosis of primary headache and average age ranging between 10.2 and 15.7 years were recruited. Patients were mostly females, ranging on average between 30 and 88.9%, with one study including females only (20). Six RCTs involved samples of patients with different primary headaches; two studies involved patients with chronic migraine, one with episodic migraine, one with chronic tension type headache, one describing patients only as “chronic headache,” and one addressing “recurrent headache.”
Five papers consisted of single group studies, while the remaining six were RCTs in which a given non-pharmacologic treatment was compared with either treatment as usual (TAU) (13, 16), headache education (14, 15), education plus amitriptyline (12), amitriptyline or gabapentin (22). The majority of the studies evaluated the effects of CBT (12–16). Three studies included BFB treatment (17–19). The remaining three studies evaluated mindfulness (20), single-pulse TMS (21) and a multimodal treatment (22).
Studies on CBT
Five RCTs assessed CBT, comparing it to education (13, 14), TAU (15, 16) or amitriptyline plus education (12). Two of these studies focused on adolescents experiencing different forms of primary headache (15, 16), whereas the other three trials evaluated CBT in patients with episodic migraine (13), chronic migraine (12) or “chronic headache” (14) alone. In all studies, CBT sessions were delivered weekly, for periods varying between 4 and 12 weeks.
CBT yielded significant reductions in headache frequency that ranged between 35.8 and 71.9% in two studies (12, 15). Although Rapoff and colleagues did not report a statistically significant reduction in headache frequency, the magnitude of improvement was sizeable 47.9%. Two trials did not report on change in headache frequency (14, 16).
Three of the above-mentioned studies (12–14) reported significant reductions in disability that ranged between 11.8 and 88.1%, as measured by the PedMIDAS. Other studies noted improvements in other secondary outcomes measured by PROMs investigating pain intensity (13, 15), quality of life (13), and parent protective behaviors, which include all parents' responses that, on one hand serve to reinforce pain complaints through increased parental attention and presence and, on the other hand, inappropriately lessen pain complaints by permitting children and adolescent to escape or avoid unwanted responsibilities or roles (15). Furthermore, the two studies that did not report on headache frequency focused their attention on other aspects that are often associated with headache, chiefly symptoms of anxiety and depression. The first of these two studies (14) evaluated the effects of a CBT intervention that focused on improving mental health overall (i.e., decrease perceived stress, anxiety and depression, while strengthening beliefs in ability to manage pain and to engage in a healthier lifestyle) and providing education about identifying and managing headache triggers. This 7-week treatment was compared to an education program of the same duration that focused on potential headache triggers (i.e., lifestyle, environmental, medication, hormonal, and dietary triggers) and headache hygiene measures (i.e., regular sleep and eating habits, moderate exercise, good hydration, and avoidance of caffeine, ethyl alcohol and other drugs). CBT produced significant reductions for symptoms of anxiety (11.3%) and depression (13.9%), as well as improvements with regards to headache disability and healthy lifestyle beliefs, when compared to headache education alone. In the second study, Sharma et al. (16) enrolled adolescents diagnosed as migraine or tension type headache, with comorbid anxiety disorders, who were randomized to either a transdiagnostic group CBT or a TAU control group. The intervention consisted of 12 weekly sessions that focused on identification of shared mechanisms across disorders, psychoeducation about headache and anxiety, cognitive restructuring, and stress management techniques. Adolescents within the CBT group showed significant improvements on headache severity and anxiety as assessed by clinical evaluations and PROMs.
Studies on BFB Treatment
Three single group outcome studies investigated various forms of BFB. The first study (17) included a sample of children with frequent or chronic tension-type headache who underwent 9 sessions of electromyographic biofeedback combined with computer animated relaxation therapy. Between baseline and 3-month follow-up, headache frequency decreased significantly, dropping from 19.1 to 11.1 headache days per month (49.1%). Furthermore, pericranial tenderness was significantly reduced among those who experienced frequent tension-type headache.
The second study, carried out by Blume et al. (18), involved children with different types of primary headaches, who underwent an average of 7 hand warming BFB sessions. Between baseline and the last training session, participants showed a significant reduction of 42.9% in headache frequency (decreasing from 14 to 8 headache/days per month). Median headache intensity also decreased significantly from a value of 6 at baseline to 5 at the final visit on a 10-point scale (16.7%).
Finally, Shiri et al. (19) evaluated the effects of a virtual reality system combined with BFB on a sample of children diagnosed with varied primary headaches. At the beginning of the treatment, participants had their picture taken in various emotional states to which they attached images representing their pain. During the 10 BFB sessions, children were instructed to watch their image and try to relax. Biofeedback yielded significantly improved ratings of pain by 51.9%, daily functioning by 67.4%, and quality of life by 20%. Moreover, the authors reported that most patients seemed to harness their new relaxation skills to relieve headache outside of the laboratory setting.
Mindfulness-Based Intervention
Hesse et al. (20) evaluated a mindfulness-based intervention in a sample composed entirely of female adolescents experiencing “recurrent headaches.” All participants underwent eight 2 h weekly mindfulness sessions and were instructed to practice learned techniques at least once per day. The intervention was tailored to address headache and the resultant related distress by teaching the adolescents to become more mindful of breath and sounds, which was supplemented with didactic lessons and group discussions. Due to the small number of adolescents providing headache daily diaries, no formal analyses of improvements for headache frequency and severity were performed. However, improvements were noted with respect to depression symptoms (21.6% lower) and pain acceptance (22.2% lower). Further, while parent-rated questionnaires showed improved physical health-related quality of life (13.4%), reports by the adolescents did not reveal any meaningful decreases in disability over time. Although by no means definitive, this study suggests that mindfulness can be a feasible and acceptable intervention for adolescents with recurrent headaches.
Transcranial Magnetic Stimulation (TMS)
One study investigated the efficacy of single-pulse TMS in adolescents diagnosed with chronic migraine (21). During the 12-week treatment period participants were instructed to apply the device twice daily, administering additional pulses as needed for acute treatment. A significant reduction in headache frequency (33.8%), as assessed by headache diaries, was found when comparing the 28 days prior to treatment (mean of 13.3 days) to the last 28 days of treatment (mean of 8.8 days). Post-treatment data were not provided, so maintenance of effects is unknown. Improvements in headache-related disability as assessed by PedMIDAS were also found, with scores decreasing from 63 ± 46 to 27 ± 27 (57%).
Multimodal Treatment
One study assessed the effects of a multimodal treatment in adolescents with chronic tension type headache (22). The intervention was compared to a group of patients who received a preventative medication, either amitriptyline or gabapentin. The multimodal treatment group was instructed to practice complementary techniques (mindfulness and qi gong) and received osteopathic manual treatments. At 6-month follow-up, patients showed a 78% decrease in headache frequency that dropped from 22.3 to 4.9 headache days per month. Improvements were also found in secondary outcomes, such as pain intensity (67.2%), general health (67.9%), pain restriction (63%) and number of bilateral tender points (80%).
Discussion
The results of the present literature review showed that various non-pharmacological treatments in populations of young headache patients produced sizeable effects on the primary endpoint, headache frequency, with reductions from baseline ranging between 34 and 78%. These findings are of particular interest as they are comparable to those usually found in trials on pharmacological treatments (23, 24). Moreover, many of the approaches herein reviewed produced meaningful effects on other commonly used patient-reported outcomes as well, particularly with respect to disability, quality of life, and symptoms of depression and anxiety.
The importance of considering non-pharmacological treatments in the array of possible prophylactic treatments in young headache patients lies in several factors. In particular, untoward side effects have not been reported for these procedures when applied with children and adolescents. In the rare instance when such effects have been reported for adults, they are noted to be short-lived and easily overcome (25). This stands in marked contrast to the array of side effects observed in drug prophylaxis, with the most common being sedation or somnolence, dizziness, mood/behavioral changes, constipation, increased appetite, and weight gain (6, 23). Second, in recent years these treatments—particularly behavioral ones—have gained in popularity among adult patients, while conventional pharmacological treatments are being viewed as sometimes ineffective or too expensive (26, 27). It is therefore likely that a similar trend will emerge not only among the parents of child and adolescent patients, but also among the patients themselves. Third, but no less important, non-pharmacological treatments are thought to enable young patients to enhance their abilities to handle pain and cope more effectively with pain episodes absent medications. In the long run, these learned skills may serve to reduce the risk of overusing medication as the adolescents become adults. These mentioned factors—together with the results of the present review—support the idea that non-pharmacological treatments should no longer be considered only as alternative or complementary to pharmacological treatments for headaches. Rather, they merit inclusion in the array of possible first line treatments for headache disorders, in particular among populations of children and adolescents.
Although effects are in general pronounced, mechanisms by which non-pharmacological treatments exert their effects has received only scant attention. Results from the present review suggest that, with regard to CBT and Mindfulness-based treatments in particular, headache improvement may be related in part to concurrent improvements in symptoms of anxiety and depression (14, 15, 20). In fact, available literature suggests that children and adolescents with headache disorders, and migraine in particular, may have higher symptoms of anxiety and depression when compared to healthy counterparts (28–32). We emphasize “suggestive” because of the possibility of false positive responses based on screening tools wherein certain scale items overlap some symptoms of depression, anxiety, and migraine (e.g., mood and energy level changes may incur in both premonitory and post-drome phases of migraine and are core symptoms of anxiety and depression). Taken as a whole, the conclusions of the aforementioned literature reviews indicate that the majority of young patients with headache disorders do not show diagnosable psychiatric comorbidities. However, when present, they deserve attention and appropriate treatments to improve patients' prognoses (29, 30, 33).
Headaches are regarded as bio-behavioral disorders, which means that both dysfunction in several brain areas and behavioral responses to stimuli, such as stress or pain, concur to the maintenance of the disease, which in fact may arise from the complex interaction between biological and psychosocial variables (34). The brain of patients with headache, particularly in migraineurs, is hyper-reactive to prolonged repeated stimuli, and altered inter-ictal information processing is associated with limbic system dysfunction (35). Studies specifically examining cognitive processes related to pain modulation in healthy individuals shed light on core brain regions involved in cognitive interventions, such as the prefrontal cortex, the midcingulate cortex, the thalamus, and the amygdala; i.e., the same brain areas which are involved in the cognitive and affective components of pain (36). However, these have to be taken as hypotheses, since the aforementioned studies are derived from populations of healthy adults. With regard to sTMS, it is proposed that the fluctuating magnetic field delivered by the device may induce electrical currents that disrupt cortical spreading depression (37); i.e., a wave of excitation followed by a wave of inhibition of both neurons and glia, which spreads across the cortical mantle that is purported to be a physiological substrate of migraine with aura (38). It is not associated with side effects, and it is therefore considered a safe treatment for migraine. Among adults, several studies have been carried out on both single-pulse and repetitive TMS (39–42), while the data for pediatric populations is—to the best of our knowledge—confined to the single study included in the present review. Finally, BFB is a bio-behavioral approach through which patients learn to voluntarily modify their bodily reactions via feedback-mediated awareness of physiologic parameters, such as peripheral skin temperature or electromyography (43). It is deemed to act, in part, by reducing cortical excitability and affecting resonance and oscillations of essential feedback loops in the brain (44) induced by modifications of bodily reactions through feedback-mediated awareness of physiologic parameters.
The evidence generated by the present review needs to be tempered somewhat due to certain shortcomings in the available studies, all of which need to be addressed in future research in the field of non-pharmacological treatments for pediatric headache in young patients. Many of the results herein reported have in fact been derived from single group open-label outcome studies, which preclude us from addressing comparative efficacy of these treatments. The inability to implement double-blinding for behavioral treatments remains a contentious issue for some. Although this concern cannot be addressed fully, rigor can be enhanced by randomizing participants to study and control or comparison groups and blinding those in charge of selecting, assigning, and evaluating treatment outcomes. With studies on non-invasive neurostimulation, sham procedures can be employed to enable double-blinding. Also, headache frequency was not always employed as the primary endpoint, which is specified as critical in all existing trial guidelines. Two studies reported only descriptive baseline information on headache frequency, while two studies did not report frequency at all, thus relying on measures that are traditionally employed as secondary endpoints, such as disability or quality of life. Duration of follow-up is another critical element, as most of the studies reviewed herein that reported data collection beyond the end of treatment did so only for a few months (e.g., around 3–4). This leaves us unable to draw any meaningful conclusions about stability of effects over the long term. Finally, future studies need to examine factors that mediate and/or are associated with positive outcomes. This can be accomplished in a number of ways, such as addressing changes in biomarkers associated with non-pharmacological approaches, based on neuroimaging and biological assays, and developing predictive models. In fact patient selection is of paramount importance in pediatric populations, and thus future studies should encompass a wide spectrum of clinical, psychosocial and biological indicators, in order to identify which are the most relevant patient features that are associated with positive clinical changes.
Our search was confined to SCOPUS because its search engine is noted to be wide ranging and journals within it are indexed from both medical and social science fields. Further, great care was taken to employ quality control measures aimed to reduce the possibility that relevant papers were excluded. Nonetheless, we cannot be certain that all relevant articles were included in our review process. Given our resultant small sample size, overlooking just a few salient articles may have altered our conclusions. Nutraceuticals, another prominent area of non-pharmacological treatments, were not included in the present review because an extensive literature review of this domain was published at the time we launched our search (45). This more recent review confirmed the results of previous current reviews (46, 47); i.e., that few studies exist, most are of low quality, and, consequently, the evidence generated thus far remains sparse.
Conclusions
Our review on the use of non-pharmacological approaches in young patients with primary headaches showed that these treatments produced sizeable effects on headache frequency, with reductions from baseline ranging between 34 and 78%, which in fact is comparable to that obtained when treating patients with pharmacological compounds. When reported, these treatments led to positive outcomes in various secondary endpoints as well.
Our findings reinforce the conclusions expressed by authors of other recent literature reviews (6, 7). We share the opinion that preventive drug treatment for headache is not always needed in young headache patients, and that the risk of side effects must always be taken into account. Conversely, clinicians should consider non-pharmacological treatments of headache disorders as a first line strategy in children and adolescents with primary headaches.
Future studies, incorporating random assignment, relying on headache frequency as the primary endpoint, employing more extended follow-up periods, and assessing possible mechanisms of treatment, such as changes in relevant biomarkers, would help to shore up the existing data base for the overall value of non-pharmacological treatments for children and adolescents experiencing recurrent headache. Determining factors predictive of outcome merits intensive study as well.
Author Contributions
FA, LG, and DD led the initiative and revised the drafted document. ES selected abstracts and revised the drafted document. AR and EG selected abstract, extracted data and drafted the manuscript. All authors approved the final version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2018.01009/full#supplementary-material
References
1. Seshia SS. Chronic daily headache in children and adolescents. Curr Pain Headache Rep. (2012) 16:60–72. doi: 10.1007/s11916-011-0228-9
2. Krogh AB, Larsson B, Linde M. Prevalence and disability of headache among Norwegian adolescents: a cross-sectional school-based study. Cephalalgia (2015) 35:1181–91. doi: 10.1177/0333102415573512
3. Langdon R, DiSabella MT. Pediatric headache: an overview. Curr Probl Pediatr Adolesc Health Care (2017) 47:44–65. doi: 10.1016/j.cppeds.2017.01.002
4. Winner P, Pearlman E, Linder S. Topiramate for migraine prevention in children: a randomized, double-blind, placebo-controlled trial. Headache (2005) 45:1304–12. doi: 10.1111/j.1526-4610.2005.00262.x
5. Hershey AD, Powers SW, Bentti AL, Degrauw TJ. Effectiveness of amitriptyline in the prophylactic management of childhood headaches. Headache (2000) 40:539–49. doi: 10.1046/j.1526-4610.2000.00085.x
6. Whitehouse WP, Agrawal S. Management of children and young people with headache. Arch Dis Child Educ Pract Edu. (2017) 102:58–65. doi: 10.1136/archdischild-2016-311803
7. Lanteri-Minet M, Valade D, Geraud G, Lucas C, Donnet A. Revised French guidelines for the diagnosis and management of migraine in adults and children. J Headache Pain (2014) 15:2. doi: 10.1186/1129-2377-15-2
8. Raggi A, Grignani E, Leonardi M, Andrasik F, Sansone E, Grazzi L, D'Amico D. Behavioral approaches for primary headaches: recent advances. Headache (2018) 58:913–25. doi: 10.1111/head.13337
9. Rains JC, Penzien DB, McCrory DC, Gray RN. Behavioral headache treatment: History, review of the empirical literature, and methodological critique. Headache (2005) 45:S92–109. doi: 10.1111/j.1526-4610.2005.4502003.x
10. Maasumi K, Tepper SJ, Rapoport AM. New treatments for headache. Neurol Sci. (2017) 38 (Suppl. 1):145–56. doi: 10.1007/s10072-017-2910-0
11. Schoenen J, Roberta B, Magis D, Coppola G. Noninvasive neurostimulation methods for migraine therapy: the available evidence. Cephalalgia (2016) 36:1170–80. doi: 10.1177/0333102416636022
12. Powers SW, Kashikar-Zuck SM, Allen JR, LeCates SL, Slater SK, Zafar M., et al. Cognitive behavioral therapy plus amitriptyline for chronic migraine in children and adolescents: a randomized clinical trial. J Am Med Assoc. (2013) 310:2622–30. doi: 10.1001/jama.2013.282533
13. Rapoff MA, Connelly M, Bickel JL, Powers SW, Hershey AD, Allen JR., et al. Headstrong intervention for pediatric migraine headache: a randomized clinical trial. J Headache Pain (2014) 15:12. doi: 10.1186/1129-2377-15-12
14. Hickman C, Jacobson D, Melnyk BM. Randomized controlled trial of the acceptability, feasibility, and preliminary effects of a cognitive behavioral skills building intervention in adolescents with chronic daily headaches: a pilot study. J Pediatr Health Care (2015) 29:5–16. doi: 10.1016/j.pedhc.2014.05.001
15. Law EF, Beals-Erickson SE, Noel M, Claar R, Palermo TM. Pilot randomized controlled trial of internet-delivered cognitive-behavioral treatment for pediatric headache. Headache (2015) 55:1410–25. doi: 10.1111/head.12635
16. Sharma P, Mehta M, Sagar R. Efficacy of transdiagnostic cognitive-behavioral group therapy for anxiety disorders and headache in adolescents. J Anxiety Disord. (2017) 46:78–84. doi: 10.1016/j.janxdis.2016.11.001
17. Tornoe B, Skov L. Computer animated relaxation therapy in children between 7 and 13 years with tension-type headache: a pilot study. Appl Psychophysiol Biofeedback (2012) 37:35–44. doi: 10.1007/s10484-011-9173-y
18. Blume HK, Brockman LN, Breuner CC. Biofeedback therapy for pediatric headache: factors associated with response. Headache (2012) 52:1377–86. doi: 10.1111/j.1526-4610.2012.02215.x.
19. Shiri S, Feintuch U, Weiss N, Pustilnik A, Geffen T, Kay B., et al. A virtual reality system combined with biofeedback for treating pediatric chronic headache–a pilot study. Pain Med. (2013) 14:621–7. doi: 10.1111/pme.12083
20. Hesse T, Holmes LG, Kennedy-Overfelt V, Kerr LM, Giles LL. Mindfulness-based intervention for adolescents with recurrent headaches: a pilot feasibility study. Evid Based Compl Alt Med. (2015) 2015:508958. doi: 10.1155/2015/508958
21. Irwin SL, Qubty W, Allen IE, Patniyot I, Goadsby PJ, Gelfand AA. Transcranial magnetic stimulation for migraine prevention in adolescents: a pilot open label study. Headache (2018) 58:724–31. doi: 10.1111/head.13284
22. Przekop P, Przekop A, Haviland MG. Multimodal compared to pharmacologic treatments for chronic tension-type headache in adolescents. J Bodyw Mov Ther. (2016) 20:715–21. doi: 10.1016/j.jbmt.2015.02.003
23. Kacperski J, Hershey AD. Preventive drugs in childhood and adolescent migraine. Curr Pain Headache Rep. (2014) 18:422. doi: 10.1007/s11916-014-0422-7
24. Papetti L, Spalice A, Nicita F, Paolino MC, Castaldo R, Iannetti P., et al. Migraine treatment in developmental age: guidelines update. J Headache Pain (2010) 11:267–76. doi: 10.1007/s10194-010-0205-4
25. Schwartz MS, Schwartz NM, Monastra VJ. Problems associated with relaxation procedures and biofeedback and guidelines for management. In: Schwartz MS, Andrasik F, editors. Biofeedback. New York, NY: The Guilford Press (2003). p. 249–59.
26. Wells RE, Bertisch SM, Buettner C, Phillips RS, McCarthy EP. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache (2011) 51:1087–97. doi: 10.1111/j.1526-4610.2011.01917.x
27. Wells RE, Phillips RS, Schachter SC, McCarthy EP. Complementary and alternative medicine use among US adults with common neurological conditions. J Neurol. (2010) 257:1822–31. doi: 10.1007/s00415-010-5616-2
28. Andrasik F, Kabela E, Quinn S, Attanasio V, Blanchard EB, Rosenblum EL. Psychological functioning of children who have recurrent migraine. Pain (1988) 34:43–52.
29. Qubty W, Gelfand AA. Psychological and behavioral issues in the management of migraine in children and adolescents. Curr Pain Headache Rep. (2016) 20:69. doi: 10.1007/s11916-016-0597-1
30. O'Brien HL, Slater SK. Comorbid psychological conditions in pediatric headache. Semin Pediatr Neurol. (2016) 23:68–70. doi: 10.1016/j.spen.2016.01.002
31. Gelfand AA. Psychiatric comorbidity and paediatric migraine: examining the evidence. Curr Opin Neurol. (2015) 28:261–4. doi: 10.1097/WCO.0000000000000192
32. Bellini B, Arruda M, Cescut A, Saulle C, Persico A, Carotenuto M., et al. Headache and comorbidity in children and adolescents. J Headache Pain (2013) 14:79. doi: 10.1186/1129-2377-14-79
33. Waldie KE, Poulton R. Physical and psychological correlates of primary headache in young adulthood: a 26 year longitudinal study. J Neurol Neurosurg Psychiatry (2002) 72:86–92. doi: 10.1136/jnnp.72.1.86
34. Andrasik F, Flor H, Turk DC. An expanded view of psychological aspects in head pain: the biopsychosocial model. Neurol Sci. (2005) 26 (Suppl. 2):S87–91. doi: 10.1007/s10072-005-0416-7
35. Coppola G, Di Lorenzo C, Serrao M, Parisi V, Schoenen J, Pierelli F. Pathophysiological targets for non-pharmacological treatment of migraine. Cephalalgia (2016) 36:1103–11. doi: 10.1177/0333102415620908
36. Flor H. Psychological pain interventions and neurophysiology: implications for a mechanism-based approach. Am Psychol. (2014) 69:188–96. doi: 10.1037/a0035254
37. Barker AT, Shields K. Transcranial magnetic stimulation: basic principles and clinical applications in migraine. Headache (2017) 57:517–24. doi: 10.1111/head.13002
38. Tfelt-Hansen PC. History of migraine with aura and cortical spreading depression from 1941 and onwards. Cephalalgia (2010) 30:780–92. doi: 10.1111/j.1468-2982.2009.02015.x
39. Bhola R, Kinsella E, Giffin N, Lipscombe S, Ahmed F, Weatherall M., et al. Single-pulse transcranial magnetic stimulation (sTMS) for the acute treatment of migraine: evaluation of outcome data for the UK post market pilot program. J Headache Pain (2015) 16:535. doi: 10.1186/s10194-015-0535-3
40. Lipton RB, Dodick DW, Silberstein SD, Saper JR, Aurora SK, Pearlman SH., et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. (2010) 9:373–80. doi: 10.1016/S1474-4422(10)70054-5
41. Misra UK, Kalita J, Bhoi SK. High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled study. J Neurol. (2013) 260:2793–801. doi: 10.1007/s00415-013-7072-2
42. Teepker M, Hötzel J, Timmesfeld N, Reis J, Mylius V, Haag A., et al. Low-frequency rTMS of the vertex in the prophylactic treatment of migraine. Cephalalgia (2010) 30:137–44. doi: 10.1111/j.1468-2982.2009.01911.x
43. Schwartz NM, Schwartz MS. Definitions of biofeedback and applied psychophysiology. In: Schwartz MS, Andrasik F, editors. Biofeedback. New York, NY: The Guilford Press (2003). p. 27–39
44. Lehrer P, Eddie D. Dynamic processes in regulation and some implications for biofeedback and biobehavioral interventions. Appl Psychophysiol Biofeedback (2013) 38:143–55. doi: 10.1007/s10484-013-9217-6
45. Orr SL. The evidence for the role of nutraceuticals in the management of pediatric migraine: a review. Curr Pain Headache Rep. (2018) 22:37. doi: 10.1007/s11916-018-0692-6
46. Sangermani R, Boncimino A. The use of nutraceutics in children's and adolescent's headache. Neurol Sci (2017) 38 (Suppl 1):121–124. doi: 10.1007/s10072-017-2896-7
Keywords: cognitive-behavioral therapy, biofeedback, mindfulness, transcranial magnetic stimulation, migraine, tension-type headache, disability, depression
Citation: Andrasik F, Grazzi L, Sansone E, D'Amico D, Raggi A and Grignani E (2018) Non-pharmacological Approaches for Headaches in Young Age: An Updated Review. Front. Neurol. 9:1009. doi: 10.3389/fneur.2018.01009
Received: 03 October 2018; Accepted: 08 November 2018;
Published: 27 November 2018.
Edited by:
Massimiliano Valeriani, Bambino Gesù Ospedale Pediatrico (IRCCS), ItalyReviewed by:
Marco Carotenuto, Università degli Studi della Campania “Luigi Vanvitelli”, ItalyLaura Papetti, Bambino Gesù Ospedale Pediatrico (IRCCS), Italy
Copyright © 2018 Andrasik, Grazzi, Sansone, D'Amico, Raggi and Grignani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frank Andrasik, Zm5kcmFzaWtAbWVtcGhpcy5lZHU=
 Frank Andrasik
Frank Andrasik