- 1Pharmacology/Institute of Basic Medical Sciences, Khyber Medical University, Peshawar, Pakistan
- 2Center for Neuroscience, Shantou University Medical College, Shantou, China
- 3Neurology Departments, Lady Reading Hospital Peshawar, Peshawar, Pakistan
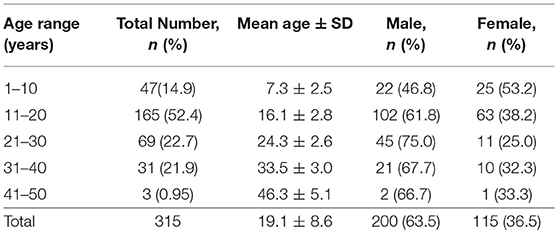
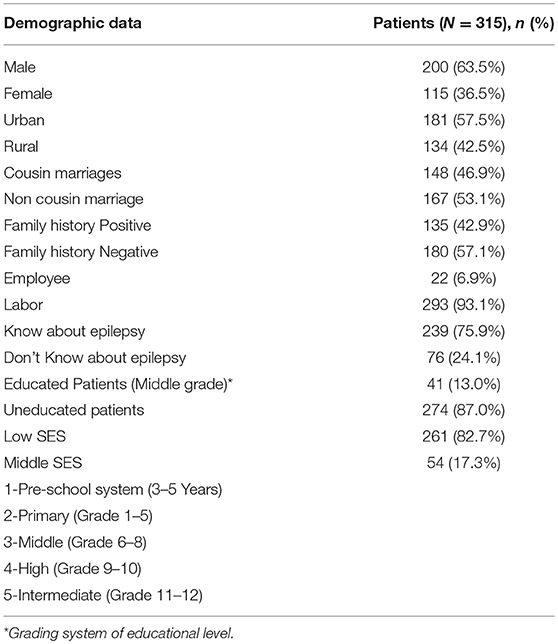
Previous studies have shown that Khyber Pakhtunkhwa, Pakistan has a high incidence of epilepsy and a high proportion of low socioeconomic background and high treatment gap. Considering the changes over the past 20 years little is known about the current epidemiological characteristics of epilepsy in Khyber Pakhtunkhwa, Pakistan. The current study was focused to find the impact of various contributing factors on the clinical response to anti-epileptic drugs in the KP population, Pakistan. A total of 315 participants aged 19.1 ± 8.6 years were examined. Mean age of the patients was 18 ± 8.1 year. Epilepsy was high in male patients (64.39%) and urban areas (60.1%). Mostly, 88.6% of patients were belonging to low socioeconomic status background. 42.4% patients have positive family history for epilepsy and 42.8% patients had consanguineous marriages. Middle SES class patients (OR, 2.22 [CI, 0.54–9.1]) were slightly associated with controlled response to CBZ and VPA therapy. Absence seizure (OR, 1.16 [CI, 0.59–2.3]), and Complex partial seizure (OR, 1.29 [CI, 0.58–6.3]) showed good response to CBZ therapy while, Myoclonic seizure (OR, 2.23 [CI, 0.05–8.8]) was responsive to VPA therapy. However, non-compliance (R2 0.82, P < 0.0001) and nature of seizures (R2 0.83, P < 0.0001) were associated with the high risk for poor response to both CBZ and VPA therapy. Epilepsy was high in male patients and in urban areas. Most patients were belonging to low socioeconomic status. Non-compliance, low socioeconomic and nature of seizures strongly predict poor clinical response of anti-epileptic drugs therapy.
Introduction
Epilepsy is a neurological disease, which is characterized by recurrent seizures that may occur suddenly without any provoking factors (1). Approximately 70 million people are suffering from epilepsies throughout the world. Epilepsy contributes 1% burden to global diseases while this contribution is 80% in the developing countries (2). Both developing and developed countries have different health-care priorities according to the need for primary prevention, to the recognition of seizures, and access to sustainable and appropriate therapy. Different approaches are used to properly treat epilepsy in the context of regional resources depend on the prevalence of a disease. Diversities in demographic factors such as gender (3), race (4), age (3), geographic area (5), religion, and culture (5) along with provoking factors are associated with poor responsive epilepsy.
Demographic and clinical factors have a crucial role in the management of epilepsy. False believes, low SES have a very important role in the poor management of epilepsy. Similarly, consanguineous marriages among the positive family history for epilepsy can increase the burden of epilepsy in a society. It is well-known that the incidence of epilepsy is linked to low socioeconomic status, positive family histories of epilepsy, limited access to health care system and environmental factors (6). Reports suggest that socioeconomically deprived people are more susceptible to epilepsy. The association is strongly supported by the facts that the incidence of epilepsy is high in developing countries as compared to developed countries (7). Several other studies also corroborate that socioeconomic status (SES), positive family history and poor compliance has an established association with resistant epilepsy (8–10). Health related quality of life (HRQL) is associated to proper response to AEDs and it has been reported that clinical response may vary across epileptic patients with different clinical, demographic, and socioeconomic variations (11, 12). With regard to clinical variables, seizures types and frequency have been found to be significant predictors of HRQL scores and clinical response (13–5). It has been found that psycho-social factors is also related to quality of life (QOL) in Korean epilepsy patients. Good QOL is directly related to better clinical response to AEDs and recognition of these factors will lead health professionals to develop different strategies to improve the QOL of these patients (15). Common clinical factors, seizure frequency, is closely associated with poor outcomes, QOL, and mortality (16). As these above variables are associated with epilepsy. Therefore, it has been suggested that demographic factors, gender difference, culture aspects, beliefs in different religion, geographic variations, and SES of an patients with epilepsy may also affect clinical response of a drug and will widen treatment gap. These are the factors in which interventions are very easy and treatment response can be improved which can reduce the treatment gap. Therefore, the purpose of the present study is used to examine the impact of these factors on the clinical outcomes of CBZ and VPA therapy in epileptic in Pakhtun population of Khyber Pakhtunkhwa, Pakistan. It will help us to improve the clinical response to carbamazepine and valproic acid therapy by exploring the impact of demographic and social profile of the patients during treatment.
Materials and Methods
Study Design and Protocol
Patients with epilepsy sample size (N = 323) was calculated at 95% CI with SD of 8 and marginal error of 1. Keeping in view 20% drop out total patients included in the study were 315. Patients from Khyber Pakhtunkhwa, Pakistan who visited the Neurology Department of Government Lady Reading Hospital for opting treatment were included in the study on consent, assent, and surrogate assent form. The study was started in August 2014 and completed in April, 2016. The study was executed according to the CONSORT flow chart presented in Figure 1.
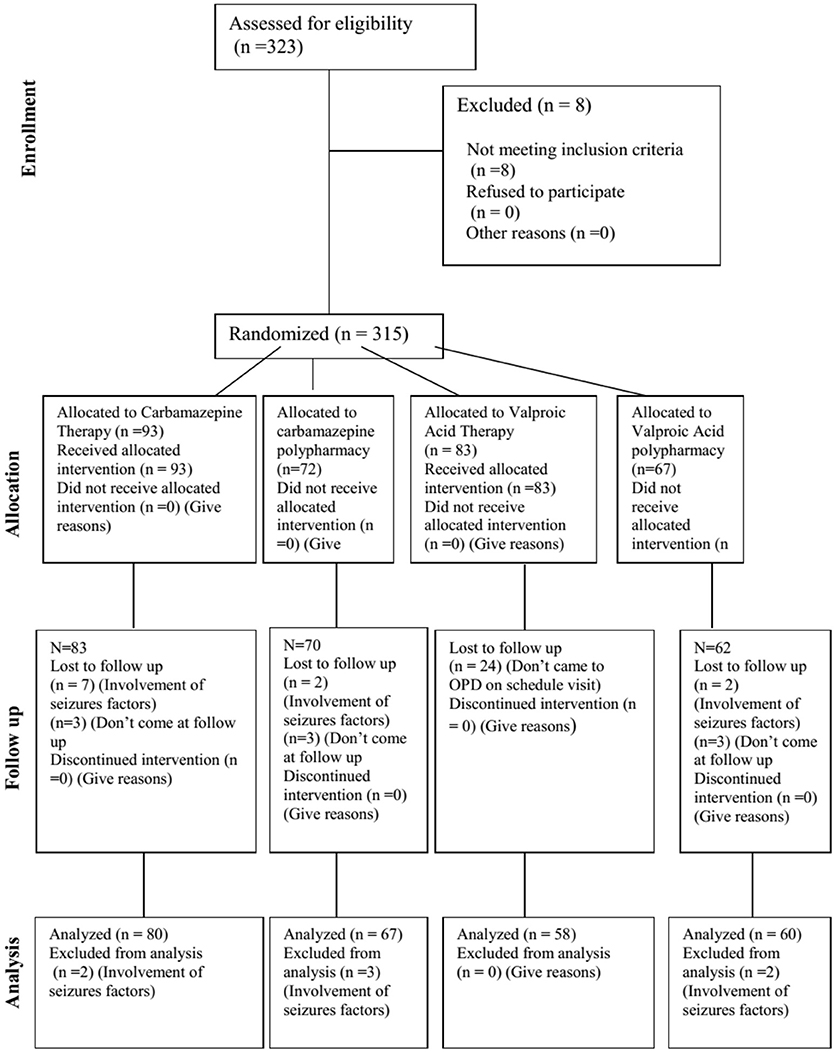
Figure 1. CONSORT diagram. CONSORT diagram showing the flow of participants through each stage of a randomized trial.
Ethics Board of the Khyber Medical University, Peshawar approved the study via no: DIR/KMU-EB/AC/000047 dated 04/07/2014. The study was conducted according to Helsinki declarations. The data was collected on a standard questionnaire designed according to the protocol of the WHO which includes all those necessary information to reduce the biases in the study.
Mean dose of carbamazepine was 452 mg/day and valproic acid 859 mg/day and was titrated for better management of epilepsy at scheduled visits.
Inclusion Criteria
Patients with epilepsy who were suitable candidate for carbamazepine and valproic acid as monotherapy or polypharmacy for first time or newly diagnosed for epilepsy were enrolled in the study. Patients with epilepsy who were willing to participate in the study after explaining the steps and the aim of the study in the context of local language were included in the study upon consent and surrogate consent form. Seizures provocative factors were controlled by proper counselling of the patients and ensure proper clinical response to CBZ and VPA as monotherapy or polypharmacy.
Exclusion Criteria
Patients with epilepsy were not included in the study who was not suitable candidate for carbamazepine and valproic acid as monotherapy or polypharmacy. Patients were also excluded from the study that was not willing to participate in the study or were suffering from some other co-morbidity. Non-compliant patients were also excluded from the study.
Assessments of Seizure Characteristics and Socioeconomic Status
Types of epilepsy were diagnosed according to guidelines of International League against Epilepsy (ILAE), witness presentation; family history; EEG report and expert opinion of concern OPD/Ward neurologists. All available information was considered in the classifications of seizures, including the medical record, interviews, EEG, and brain imaging. The SES of patients was are classified as reported by Association American Psychology report 2011 (17). The higher Socioeconomic class will have 50–100 and above, Middle class 15–49, and Low economic class will have below 15 Per capita monthly income limits (Rs.) (17).
Measurement of Seizure Control in Patients With Epilepsy
Seizures' control was recorded in the form of reduction of frequencies of seizures using standardized proforma in local language. The numbers of seizures per week were recorded at baseline and these patients were then evaluated for seizure control at 3rd and 6th month of the therapy. The patients with epilepsy compliance to the medication were checked by counting the pills remaining in the strip on scheduled visits. Drug response was determined as either freedom from seizures or reduction in number of seizure per week after initiation of carbamazepine and valproic acid therapy at 3rd and 6th month.
Statistical Analysis
The distribution of age, clinical, and demographic characteristic of epileptic patients were presented in the form of percentage. The Mean ± SD were determined for age. The expected outcome (EXP B) was determined using univariate logistic regression analysis. The prediction of clinical response with respect to all variables was determined using multivariate regression analysis by incorporating step by step variables and to determine the combined as well as individual impact of each variable on clinical outcomes of CBZ and VPA as monotherapy or polypharmacy. SPSS 20 and Stata version 12 was used for analysis.
Results
Demographic Features of Epileptic Patients
Mean age of epileptic patients were 19.1 ± 8.6 years (range 1–42) (Table 1). The prevalence of epilepsy was higher in patients having age of 10–20 years. Epilepsy was high in male (64.39%) than female (35.98%) patients in study population (Table 2). The percentage of cousin marriage and positive family history of epilepsy was (42.8%) and (42.4%) (Table 2). The level of education was very low in these patients. Furthermore, these patients were having low socioeconomic status (SES) (88.63%).
Phenomenology
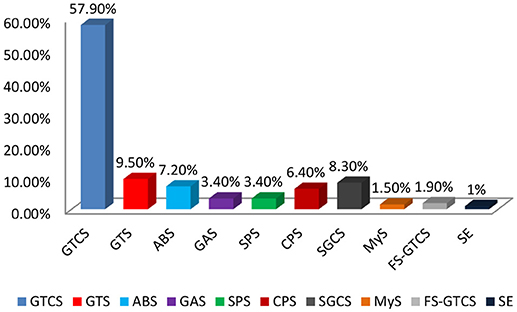
Types of seizures were classified according to the ILAE guidelines and clinical presentation of patients with epilepsy. Generalized tonic clonic seizures was commonly observed 153 (57.9%) during this study in epileptic patients of KP (Figure 2). Other types of seizures were Generalized tonic seizures 25 (9.5%), Absence seizures 19 (7.2%), Generalized atonic 8 (3.4%) secondary generalized complex seizures 22 (8.3%), simple partial seizures 9 (3.4%), and complex partial seizures 17 (6.4%) were found in the target population (Figure 2).
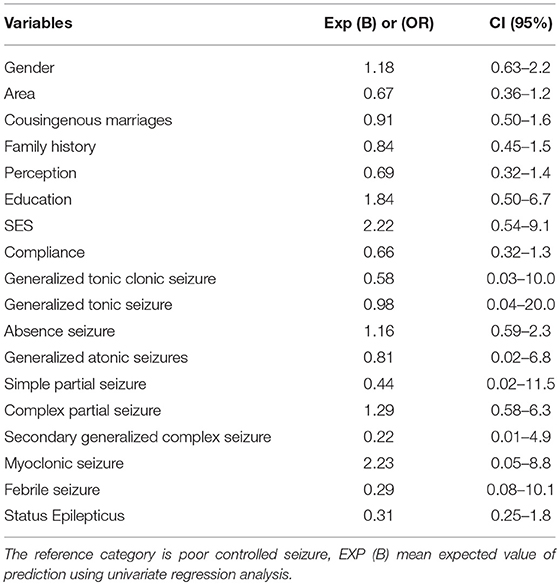
Impact of Demographic and Clinical Features vs. Response of Anti-Epileptic Drugs
The association of different demographic variables with clinical outcome were determined using univariate logistic regression analysis (Table 3). It has been found that high education level were slightly associated with controlled response (OR, 1.84 [CI, 0.50–6.7]) to CBZ and VPA as monotherapy or polypharmacy. Similarly, good SES was also associated with good response (OR, 2.22 [CI, 0.54–9.1]) to CBZ and VPA as monotherapy or polypharmacy. Absence seizure (OR, 1.16 [CI, 0.59–2.3]), Complex partial seizure (OR, 1.29 [CI, 0.58–6.3]), and Myoclonic seizure (OR, 2.23 [CI, 0.05–8.8]) showed a good response to CBZ and VPA as monotherapy or polypharmacy (Table 3).
Similarly, multivariate regression models were applied to demographic variables to predict clinical response of CBZ and VPA as monotherapy or polypharmacy in epileptic patients. Over all the factors added in Model 9 (R2 0.82, P < 0.0001) and model 10 (R2 0.83, P < 0.0001) were found to increase the risk of poor response to AEDs.
Discussion
In our study the prevalence rate of epilepsies was high in male patients where most of them were belonging to urban areas. Our observations were in line to Khan et al. (18) that epilepsy was high in male population and urban areas (18). Though we found an inverse figure as reported by Mohammad et al. where epilepsy is more prevalent in female than male patients in Iran (19). We found that epilepsy was common in patients having age group of 10–20 years. These findings were in line with the reports of previous studies conducted in Pakistan and India (20–26). The percentage of consanguineous marriages and positive family history of epilepsy was high in the study population. The SES of most patients observed in our study was very low. Heaney et al. observed that low SES has an association with epilepsy because of low quality of life increased the susceptibility of an individuals to different provoking factors of epilepsy (27). Other studies also show that low SES was associated with an increased risk for epilepsy in individuals with seizures of unknown etiology (28–35). Luengo et al. reported that genetic history of patients with epilepsy have a 2.5 times higher risk for epilepsy in their coming generation (36). GTCS was common among other types of seizures in the target population which is in line with Nowshad et al. observations (18). It has been found that clinical outcome in patients with absence seizures and myoclonic seizures were good compared to other types of seizure. Poor response was also high in non-compliance patients. Regression model showed that poor compliance and nature of seizures significantly associated with poor response to CBZ and VPA as monotherapy or polypharmacy even at optimal adjusted dose of CBZ and VPA as monotherapy or polypharmacy. Thomson et al. (38) stat that compliance has a direct association with seizure response (37, 38). Dragoumi et al. (39) demonstrate that types of seizure also affect clinical outcome in epileptic patients (39). If patients show non-compliance with therapy and do not take their AEDs according to prescription then it leads to poor clinical outcome. Similarly, low SES of patient is also a hurdle in proper compliance and lead to poor clinical response. Low SES also responsible for large treatment gap. Nature of seizure is also a main factor for resistant epilepsy.
Limitations and Strength of the Study
It is a hospital based study which doesn't show the clear picture of whole society. It has an advantage that this study will provide the platform to conduct a community based study to determine the prevalence and stigmatization of epilepsy.
Conclusion
Male patients were having a high prevalence (64.39%) of epilepsies where 60.1% were from urban areas. Epilepsy was high in patients with age ranging 11–20 years. Positive family history of epilepsy and consanguineous marriages was the key characteristics of the epileptic patients. Non-compliance and nature of seizures strongly predict poor clinical response of Anti-epileptic drugs therapy.
Availability of Data and Material
The analyzed dataset during the current study will be provided from the corresponding author on reasonable request.
Author Contributions
SU carried out experimental work as Ph.D. Scholar. Also prepared the 1st draft of manuscript. NA extensively revised the manuscript. He is also designed the study and wrote the research project. AK helped in diagnosis and patients follow up for their seizures control. SA helped in Clinical scoring of epilepsies. HN helped in experimental work. All authors approved the final version of manuscript.
Funding
The authors want to thank the Directorate of Science & Technology, Govt. of Khyber Pakhtunkhwa for providing funds for some of the consumable items (chemicals and plastic wares) involved in the study. Grant No: dirrtt:/S&T/KPK/BT/RP/FS/2013-14 (1592).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors also want to thank AK and then Chief Executive of Govt. Lady Reading Hospital Peshawar for providing opportunity for research work.
Abbreviations
AEDs, Anti-epileptic drugs; CBZ, Carbamazepine; HRQL, Health related quality of life; ILAE, International League against Epilepsy; QOL, quality of life; SES, Socioeconomic Status; VPA, Valproic Acid.
References
1. Brodie M, Engel J, Lee P, de Boer H. European white paper on epilepsy-Call to action. EPILEPSIA (2003) 44:4–4.
3. Ernst MM, Johnson MC, Stark LJ. Developmental and psychosocial issues in cystic fibrosis. Child Adolesc Psychiatr Clin N Am. (2010) 19:263–83. doi: 10.1016/j.chc.2010.01.004
4. Barr HL, Britton J, Smyth AR, Fogarty AW. Association between socioeconomic status, sex, and age at death from cystic fibrosis in England and Wales (1959 to 2008): cross sectional study. BMJ (2011) 343:d4662. doi: 10.1136/bmj.d4662
5. Djibuti M, Shakarishvili R. Influence of clinical, demographic, and socioeconomic variables on quality of life in patients with epilepsy: findings from Georgian study. J Neurol Neurosurg Psychiatry (2003) 74:570–3. doi: 10.1136/jnnp.74.5.570
6. World Health Organization. Epilepsy: aetiology, epidemiology, and prognosis. In: Epilepsy: Aetiology, Epidemiology, and Prognosis. World Health Organization (2001) p. 4.
7. Neligan A, Hauser W, Sander J. The epidemiology of the epilepsies. Handb Clin Neurol. (2012) 107:113. doi: 10.1016/B978-0-444-52898-8.00006-9
8. Birbeck G, Chomba E, Atadzhanov M, Mbewe E, Haworth A. The social and economic impact of epilepsy in Zambia: a cross-sectional study. Lancet Neurol. (2007) 6:39–44. doi: 10.1016/S1474-4422(06)70629-9
9. Kelvin EA, Hesdorffer DC, Bagiella E, Andrews H, Pedley TA, Shih TT, et al. Prevalence of self-reported epilepsy in a multiracial and multiethnic community in New York City. Epilepsy Res. (2007) 77:141–50. doi: 10.1016/j.eplepsyres.2007.09.012
10. Noronha AL, Borges MA, Marques LH, Zanetta DM, Fernandes PT, De Boer H, et al. Prevalence and pattern of epilepsy treatment in different socioeconomic classes in Brazil. Epilepsia (2007) 48:880–5. doi: 10.1111/j.1528-1167.2006.00974.x
11. Baker GA, Jacoby A, Buck D, Brooks J, Potts P, Chadwick DW. The quality of life of older people with epilepsy: findings from a UK community study. Seizure (2001) 10:92–9. doi: 10.1016/S1059-1311(00)90465-5
12. Suurmeijer TP, Reuvekamp MF, Aldenkamp BP. Social functioning, psychological functioning, and quality of life in epilepsy. Epilepsia (2001) 42:1160–8. doi: 10.1046/j.1528-1157.2001.37000.x
13. Baker GA, Gagnon D, McNulty P. The relationship between seizure frequency, seizure type and quality of life: findings from three European countries. Epilepsy Res. (1998) 30:231–40. doi: 10.1016/S0920-1211(98)00010-2
14. Berto P. Quality of life in patients with epilepsy and impact of treatments. Pharmacoeconomics (2002) 20:1039–59. doi: 10.2165/00019053-200220150-00002
15. Choi-Kwon S, Chung C, Kim H, Lee S, Yoon S, Kho H, et al. Factors affecting the quality of life in patients with epilepsy in Seoul, South Korea. Acta Neurol Scand. (2003) 108:428–34. doi: 10.1046/j.1600-0404.2003.00151.x
16. Baker GA, Nashef L, Hout BA. Current issues in the management of epilepsy: the impact of frequent seizures on cost of illness, quality of life, and mortality. Epilepsia (1997) 38:S1–8. doi: 10.1111/j.1528-1157.1997.tb04511.x
18. Khan N, Jehan B, Khan A, Khan H. Audit of 100 cases of epilepsy in a tertiary care hospital. Gomal J Med Sci. (2011), 42–5.
19. Mohammadi MR, Ghanizadeh A, Davidian H, Mohammadi M, Norouzian M. Prevalence of epilepsy and comorbidity of psychiatric disorders in Iran. Seizure (2006) 15:476–82. doi: 10.1016/j.seizure.2006.05.011
20. Aziz H, Güvener A, Akhtar S, Hasan K. Comparative epidemiology of epilepsy in Pakistan and Turkey: population-based studies using identical protocols. Epilepsia (1997) 38:716–22. doi: 10.1111/j.1528-1157.1997.tb01242.x
21. Lee W, Low P, Murugasu B, Rajan U. Epidemiology of epilepsy in Singapore children. Neurol J Southeast Asia (1997) 2:31–5.
22. Mani K, Rangan G, Srinivas H, Kalyanasundaram S, Narendran S, Reddy A. The Yelandur study: a community-based approach to epilepsy in rural South India—epidemiological aspects. Seizure (1998) 7:281–8. doi: 10.1016/S1059-1311(98)80019-8
23. Sridharan R, Murthy B. Prevalence and pattern of epilepsy in India. Epilepsia (1999) 40:631–6. doi: 10.1111/j.1528-1157.1999.tb05566.x
24. Ng K, Ng P, Tsang K. Clinical characteristics of adult epilepsy patients in the 1997 Hong Kong epilepsy registry. Chin Med J. (2001) 114:84–7.
25. Rajbhandari KC. Epilepsy in Nepal. Can J Neurol Sci. (2004) 31:257–60. doi: 10.1017/S0317167100053919
26. Tran D-S, Odermatt P, Le T-O, Huc P, Druet-Cabanac M, Barennes H, et al. Prevalence of epilepsy in a rural district of central Lao PDR. Neuroepidemiology (2006) 26:199–206. doi: 10.1159/000092407
27. Heaney DC, MacDonald BK, Everitt A, Stevenson S, Leonardi GS, Wilkinson P, et al. Socioeconomic variation in incidence of epilepsy: prospective community based study in south east England. BMJ (2002) 325:1013–6. doi: 10.1136/bmj.325.7371.1013
28. Faggiano F, Partanen T, Kogevinas M, Boffetta P. Socioeconomic differences in cancer incidence and mortality. IARC Sci Publ. (1996) (138):65–176.
29. Guthmundsson K, Hartharson P, Sigvaldason H, Sigfusson N. [Relationship between education and risk factors for coronary artery disease]. Nordisk Med. (1997) 112:169–75.
30. Jones IR, Urwin G, Feldman RA, Banatvala N. Social deprivation and bacterial meningitis in north east Thames region: three year study using small area statistics. BMJ (1997) 314:794. doi: 10.1136/bmj.314.7083.794
31. Hemmingsson T, Lundberg I, Diderichsen F. The roles of social class of origin, achieved social class and intergenerational social mobility in explaining social-class inequalities in alcoholism among young men. Soc Sci Med. (1999) 49:1051–9. doi: 10.1016/S0277-9536(99)00191-4
32. Cubbin C, LeClere FB, Smith GS. Socioeconomic status and the occurrence of fatal and nonfatal injury in the United States. Am J Public Health (2000) 90:70.
33. Vrijheid M, Dolk H, Stone D, Abramsky L, Alberman E, Scott J. Socioeconomic inequalities in risk of congenital anomaly. Arch Dis Childhood (2000) 82:349–52. doi: 10.1136/adc.82.5.349
34. Chang C-L, Marmot MG, Farley TM, Poulter NR. The influence of economic development on the association between education and the risk of acute myocardial infarction and stroke. J Clin Epidemiol (2002) 55:741–7. doi: 10.1016/S0895-4356(02)00413-4
35. Karp A, Kåreholt I, Qiu C, Bellander T, Winblad B, Fratiglioni L. Relation of education and occupation-based socioeconomic status to incident Alzheimer's disease. Am J Epidemiol. (2004) 159:175–83. doi: 10.1093/aje/kwh018
36. Luengo A, Parra J, Colas J, Ramos F, Carreras T, Fernandez-Pozos M, et al. Prevalence of epilepsy in northeast Madrid. J Neurol. (2001) 248:762–7. doi: 10.1007/s004150170091
37. Hovinga CA, Asato MR, Manjunath R, Wheless JW, Phelps SJ, Sheth RD, et al. Association of non-adherence to antiepileptic drugs and seizures, quality of life, and productivity: survey of patients with epilepsy and physicians. Epilepsy Behav. (2008) 13:316–22. doi: 10.1016/j.yebeh.2008.03.009
38. Thomson KE, Modi AC, Glauser TA, Rausch JR, Steve White H. The impact of nonadherence to antiseizure drugs on seizure outcomes in an animal model of epilepsy. Epilepsia (2017) 58:1054–62. doi: 10.1111/epi.13742
Keywords: epilepsy, demographics, clinical outcome, social profile, socioeconomic status, types of seizures, carbamazepine, valproic acid
Citation: Ullah S, Ali N, Khan A, Ali S and Nazish HR (2018) The Epidemiological Characteristics of Epilepsy in the Province of Khyber Pakhtunkhwa, Pakistan. Front. Neurol. 9:845. doi: 10.3389/fneur.2018.00845
Received: 14 July 2018; Accepted: 20 September 2018;
Published: 06 November 2018.
Edited by:
Ding Ding, Fudan University, ChinaReviewed by:
Tomas Mesa, Pontificia Universidad Católica de Chile, ChileEdward Bertram, University of Virginia, United States
Copyright © 2018 Ullah, Ali, Khan, Ali and Nazish. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shakir Ullah, c2hha2lyLmlibXNAa211LmVkdS5waw==
 Shakir Ullah
Shakir Ullah Niaz Ali1
Niaz Ali1