- 1Department of Neurology, Miller School of Medicine, University of Miami, Miami, FL, United States
- 2Department of Systems Medicine, School of Medicine, University of Rome Tor Vergata, Rome, Italy
- 3Department of Human Sciences and Quality of Life Promotion, San Raffaele Roma Open University, Rome, Italy
- 4Department of Neurology, Kansas University Medical Center, Kansas City, MO, United States
- 5Division of Stroke, Department of Neurology, Columbia University, New York, NY, United States
Background and purpose: Carotid plaque (CP), carotid intima media thickness (cIMT), and stiffness (STIFF) are pre-clinical markers of atherosclerosis and predictors of cerebrovascular disease (CVD). We sought to investigate whether STIFF is a significant determinant of cIMT and CP, which may provide an insight into the mechanism by which STIFF adds to the risk of CVD.
Methods: We analyzed 876 stroke-free subjects from the Northern Manhattan Study with available ultrasound measures. To obtain the associations with STIFF, we performed multivariable-adjusted regression, negative binomial regression (for CP number), and multinomial logistic regression (for plaque area).
Results: The mean age was 64 ± 9 years; 63% women and 65% Caribbean Hispanics. The mean cIMT was 0.93 ± 0.9 mm, the mean diastolic diameter 6.24 ± 0.94 mm, and STIFF 8.6 ± 6.2 ln mmHg. Prevalence of CP was 57%, and the mean total plaque area was 22.6 ± 23.0 mm2. STIFF was positively associated with cIMT but not with CP. There was an association between diastolic diameter and thick plaque. For each millimeter increase in diastolic diameter, there was about a 20% increased risk of having thick plaque (vs. no plaque). In longitudinal analyses, each millimeter increase in diastolic diameter was associated with a 37% increased risk of incident plaque.
Conclusion: Increased STIFF was associated with increased cIMT and carotid artery dilatation with greater plaque burden. Increased cIMT and plaque burden represent vascular remodeling likely resulting from the two different age-related mechanisms, one that includes diffuse wall thickening (cIMT) with STIFF and another that incorporates focal atherosclerosis (plaque) with luminal dilatation.
Introduction
Atherosclerosis is the underlying process of most cardiovascular disease (CVD) (1) leading to luminal stenosis with flow restriction or to plaque rupture (2). Carotid plaque (CP), carotid intima media thickness (cIMT), and arterial stiffness (STIFF) are well-established subclinical markers of atherosclerosis and significant predictors of CVD (2, 3). They are biologically and genetically distinct phenotypes of atherosclerosis (4, 5). CP thickness and area assessed by ultrasound are direct measures of atherosclerotic plaque burden (6) and better predictors of CVD than cIMT (4, 7, 8).
Stiffness is a functional measure of the arterial wall’s resistance to pressure deformation during the cardiac cycle (9). STIFF and arterial dilatation result from a degenerative process affecting mainly the extracellular matrix of elastic arteries where the principal risk factor is aging. Arterial dilatation and STIFF may be early markers of structural atherosclerotic changes and potentially targeted for early anti-atherosclerotic interventions (10). However, information on the relationship between arterial wall function and structure in the general population is sparse. We sought to investigate these associations in a stroke-free population from the Northern Manhattan Study (NOMAS).
Materials and Methods
Study Population
Northern Manhattan Study is a population-based study designed to determine the incidence of stroke and CVD described previously (11). A total of 3,298 subjects were enrolled. As a part of the Carotid Imaging Study (2), 876 individuals with available ultrasonographic measurements and signed written informed consents in accordance with the Declaration of Helsinki were included in analyses. NOMAS was approved by the Institutional Review Boards of Columbia University and the University of Miami.
Data were collected through interviews using standardized collection instruments, review of the medical records, and physical examination (11). Vascular risk factors (vRF) and physical activity were described previously (2, 12).
Carotid Ultrasound
High-resolution two-dimensional carotid ultrasound imaging (Figure S1 in Supplementary Material) was performed according to the standardized scanning and reading protocols (2). The left and right carotid bifurcations, the internal carotid arteries (ICA), and common carotid arteries (CCA) were imaged (13). Plaque was defined as focal wall thickening or protrusion in the lumen more than 50% greater than the surrounding wall thickness. CP boundaries were traced offline using automatic edge detection system (M’Ath Inc., Paris, France). The sum of plaque areas in all carotid arteries from the both side of the neck was expressed as total plaque area (TPA) in square millimeter. IMT (mm) in all carotid segments was measured in areas free of plaque. cIMT was calculated as a composite measure combining the near and the far walls of CCA IMT, bifurcation IMT, and ICA IMT of both neck sides and examined continuously as a mean of the mean measurements of the 12 sites. The offline measurement of STIFF was performed as described (14). STIFF (ln mmHg) was calculated as [(the natural log transformation of (systolic BP − diastolic BP))/strain], where strain was [(systolic diameter − diastolic diameter)/diastolic diameter].
A subgroup of 267 individuals with two carotid ultrasound images apart were included in an analysis of the relationship between DD, STIFF, and strain with incident plaques and the change in the maximum plaque thickness and cIMT. Incident plaque was defined as an increase in the number of plaques between carotid ultrasound measurements, and the change in maximal plaque thickness and cIMT was defined as the thickness at follow-up minus the thickness at baseline.
Statistical Analysis
In cross-sectional analyses, independent variables were DD, strain, and STIFF and each examined continuously. The dependent variables were the mean cIMT, plaque number, plaque thickness, and TPA. TPA was examined in three categories: no plaque and tertiles of TPA distribution (tertile 1–2 and the top tertile). Plaque thickness was also examined in three categories: no plaque, plaque < 1.9 mm, and plaque > 1.9 mm. The latter cutoff was used to define thick plaque as it has been significantly associated with clinical outcomes in this cohort (2). Multinomial logistic regression was used to examine the associations of DD, strain, and STIFF with plaque thickness and TPA, with no plaque as the reference. Due to overdispersion of plaque number, negative binomial regression was used to examine the associations with plaque number, examined continuously as dependent variable. cIMT was examined as a continuous outcome using linear regression. We used a sequence of multivariable-adjusted regression models. The first model controlled for demographic variables (age, sex, and race/ethnicity), the second model controlled for demographics and anti-hypertensive medication, and the third model additionally controlled for current smoking, diabetes, moderate alcohol use, moderate to heavy physical activity, BMI, and hypercholesterolemia. We did not adjust for hypertension in order to avoid overadjustment as STIFF is a metric that includes systolic and diastolic BP measurements. We examined potential effect modification by demographic variables, diabetes, smoking, and lipids, using interaction terms in the third model.
An exploratory prospective analysis was conducted for strain, STIFF, and DD in association with incident plaque using logistic regression and with the change in maximal plaque thickness and cIMT using linear regression models. The same three models described earlier were used, additionally controlling for the time span between carotid measurements.
Results
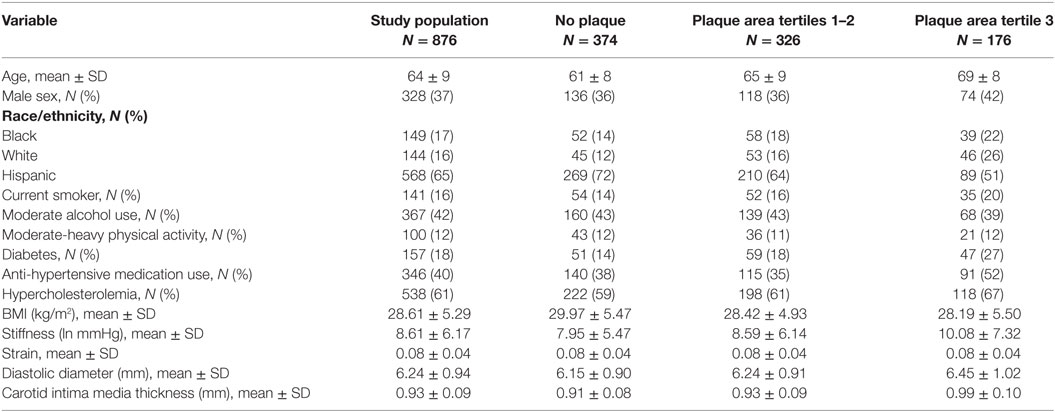
Among 876 subjects (mean age 64 ± 9 years), 63% were women, 65% Caribbean Hispanic, 17% black, and 16% white. The mean cIMT was 0.93 ± 0.9 mm, the mean STIFF 8.6 ± 6.2 ln mmHg (median = 6.9, range = 1.6–51.5), the mean strain 0.08 ± 0.04 (median = 0.07, range = 0.01–0.30), and the mean DD 6.24 ± 0.94 mm (median = 6.10, range = 3.90–10.50). Prevalence of CP was 57% (plaque number distribution: 1 plaque = 19%, 2 = 17%, 3 = 9%, 4 = 5%, 5 = 4%, 6 = 2%, 7 = 1%, 8 = < 1%, and 9 = < 1%), and 38% had plaque > 1.9 mm. Among those with plaque, the mean TPA was 22.6 (±23.0) mm2, median = 14.8 mm2. TPA distribution for the first two tertiles (N = 326) ranged from 2.2 to 21.6 mm2 and for the third tertile (N = 176) from 21.7 to 168.8 mm2. Table 1 shows the covariate characteristics of the study population overall and by TPA categories.
In univariate analysis, significant association was present between age and STIFF (p < 0.0001), DD (p < 0.0001), and strain (p = 0.0003). Table 2 shows the relationship between DD and STIFF with cIMT and the plaque phenotypes and in the sequence of multivariable-adjusted models. DD and STIFF were both positively associated with cIMT in all three models. For the plaque phenotypes, the only association observed was a positive association between DD and thick plaque (>1.9 mm). Each millimeter increase in DD was associated with a 20% increased risk of thick plaque (vs. no plaque). Strain and STIFF were not associated with plaque thickness. DD and STIFF were not associated with plaque number neither with plaque area. No significant effect modifications were observed.
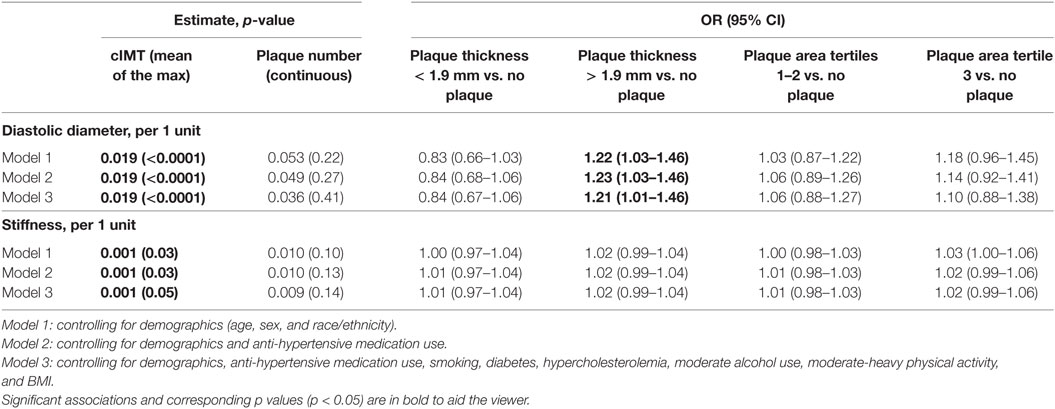
Table 2. Association of carotid stiffness and diastolic diameter with carotid intima media thickness (cIMT) and plaque phenotypes.
In a longitudinal analysis, 115 individuals had a new plaque at follow-up, including 30 new plaques among 101 without plaque at baseline. The mean time span between measurements was 3.2 years (range = 2.8–5.4), the mean change in maximal plaque thickness was 0.35 ± 1.07 mm, and the mean change in cIMT was 0.16 ± 0.15 mm. In model 1, STIFF was not associated with incident plaque (data not shown), but DD was positively associated with incident plaque in model 1 (OR = 1.36, 95% CI = 1.01–1.82) and model 3 (OR = 1.37, 95% CI = 1.00–1.89). There was a suggested positive association of DD with maximum plaque thickness (model 1, beta = 0.15, p = 0.05; model 3 beta = 0.15, p = 0.06). No association of DD nor STIFF was found with the change in cIMT.
Discussion
In our elderly community cohort, we report a significant association between increased STIFF and cIMT and between larger carotid diameter and CP burden. These associations were independent of demographics and major vRF, directly linking parameters of arterial function and structure through the arterial wall remodeling processes. Our findings may help to better understand the link between arterial wall mechanics and arterial remodeling in early atherosclerosis.
The associations of STIFF with cIMT and plaques have been reported previously (10, 15). In the Atherosclerosis Risk in Communities, the positive association between STIFF and cIMT was found only in the thickest cIMT that represented 10% of the carotids, likely representing plaque. This relationship was explained by the presence of endothelial damage enhanced by intraluminal stress in STIFF arteries and accumulation of atherosclerotic material in arterial wall. However, the mechanisms of arterial remodeling leading to increased cIMT in contrast to arterial plaque may be different and remains largely unexplained. Our study may suggest different remodeling mechanisms leading to either diffuse arterial wall thickness (cIMT) that is largely dependent on arterial STIFF or to focal atherosclerotic changes (plaque) dependent on luminal dilatation. According to the Glagov’s vascular remodeling mechanism, arteries remodel to maintain constant flow despite increases in atherosclerotic lesion mass (16). In an experimental model of the carotid arteries in rabbits, flow-induced arterial dilatation was accompanied by an adaptive remodeling of carotid intima (17), suggesting that arterial dilatation is an early marker of atherosclerotic lesion.
Traditional and less-traditional vRF impact arterial remodeling and contribute to the stiffening of the arterial tree (14, 18, 19). In our study, the association between STIFF and cIMT was not modified by vRF, suggesting a direct flow-pressure contribution to the wall injury that deserves further exploration.
We found a positive association between DD and thick plaque. A study conducted in hypertensive patients demonstrated that change in diameter of CCA directly impacted plaque thickness, supporting our findings (20). Based on the Glagov’s remodeling mechanism (21), the enlargement of the DD may preferentially induce one phenotype of atherosclerosis, i.e., plaque, over another, i.e., cIMT (22, 23). However, the mechanism leading to the preferential atherosclerotic phenotype remains unclear.
In our longitudinal analysis, we found independent associations between enlargement of DD and incident plaque and increased maximum plaque thickness. Conversely, no associations were found for STIFF with plaque and cIMT and for DD and cIMT. In support, the Plaque At RISK study (24) has demonstrated a stronger association for DD, plaque progression, and CVD than for cIMT. These results suggest that plaque development may be more affected by the arterial remodeling mechanism than cIMT. Driving forces that induce plaque progressing with aging may be associated with the lumen dilatation as an adaptive response to increased pressure in the arteries (25). Moreover, a significant interaction between plaque and STIFF is present only in advanced stage of the atherosclerotic lesion (26). Larger longitudinal studies with multiple follow-up ultrasound measurements are needed to establish temporal associations between these phenotypes of atherosclerosis.
A lack of the association between STIFF and plaque in our study is in contrast to the findings from the Rotterdam Study (15), where this correlation was present. The discrepancy may be related to different study populations, ultrasound methodologies, and the measurement of STIFF (carotid ultrasound vs. pulse wave velocity), which depends by several parameters and may not be accurate. Local measurement of STIFF by ultrasound evaluation of arterial distensibility and compliance is able to a better evaluation of the absolute or relative changes in the arterial volume and distending pressure.
Various studies have adopted different plaque and cIMT definitions (27). Our cIMT method is based on the Mannheim consensus to avoid discrepancies reported in major cIMT studies (28). Development of novel methods such as non-invasive vascular ultrasound elastography may provide more direct measurements of the arterial walls mechanical properties at the level of plaque with increased accuracy and validity. Strengths of the current study include a population-based design, inclusion of both cross-sectional and prospective analyses, and the use of multiple plaque phenotypes for comparisons. The major limitation is that our study cohort is old and results may not be generalizable to younger populations. The prospective analysis had limited power and as in any epidemiology study, confounding is a possibility, and causality cannot be inferred.
Ethics Statement
As a part of the Carotid Imaging Study (26), 876 individuals with available ultrasonographic measurements and signed written informed consents in accordance with the Declaration of Helsinki were included in analyses. NOMAS was approved by the Institutional Review Boards of Columbia University and the University of Miami.
Author Contributions
DD-M: conceived the presented idea, conceived and planned the analysis of the data, contributed to the interpretation of the results, and wrote the manuscript. HG: performed statistical analysis, contributed to the interpretation of the results, and made a critical revision of the manuscript. CD: performed statistical analysis, contributed to the interpretation of the results, and made a critical revision of the manuscript. MM: contributed to the interpretation of the results and made a critical revision of the manuscript. DC: collected the data for the analysis. ME: contributed to the interpretation of the results and made a critical revision of the manuscript. RS: handled funds, conceived the presented idea, conceived and planned the analysis of the data, contributed to the interpretation of the results, and made a critical revision of the manuscript. TR: handled funds, conceived the presented idea, conceived and planned the analysis of the data, contributed to the interpretation of the results, and wrote the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This work was supported by the National Institute of Neurologic Disorders and Stroke grants: R37 NS29993 (Dr. Sacco), R01 NS047655 (Dr. Rundek), and K24 NS062737 (Dr. Rundek) and the Evelyn F. McKnight Brain Institute (Drs. Sacco, Rundek, Della-Morte, and Dong).
Supplementary Material
The Supplementary Material for this article can be found online at https://www.frontiersin.org/articles/10.3389/fneur.2018.00246/full#supplementary-material.
Figure S1. Carotid Ultrasound procedures. High-resolution two-dimensional carotid ultrasound imaging was performed to measure carotid function and structure in 876 subjects from the Northern Manhattan Study (NOMAS). BP, blood pressure; CCA, common carotid arteries; cIMT, carotid intima media thickness; DBP, diastolic blood pressure; DD, diastolic diameter; ECA, external carotid arteries; ICA, internal carotid arteries; SBP, systolic blood pressure; DD, diastolic diameter; SD, systolic diameter; TPA, total plaque area (mm2).
References
1. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation (2012) 125(1):e2–220. doi:10.1161/CIR.0b013e31823ac046
2. Rundek T, Arif H, Boden-Albala B, Elkind MS, Paik MC, Sacco RL. Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan Study. Neurology (2008) 70(14):1200–7. doi:10.1212/01.wnl.0000303969.63165.34
3. Bots ML, Dijk JM, Oren A, Grobbee DE. Carotid intima-media thickness, arterial stiffness and risk of cardiovascular disease: current evidence. J Hypertens (2002) 20(12):2317–25. doi:10.1097/00004872-200212000-00002
4. Spence JD. Measurement of intima-media thickness vs. carotid plaque: uses in patient care, genetic research and evaluation of new therapies. Int J Stroke (2006) 1(4):216–21. doi:10.1111/j.1747-4949.2006.00068.x
5. Rundek T, Brook RD, Spence JD. Letter by Rundek et al regarding article, “Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis”. Circulation (2007) 116(9):e317; author reply e318. doi:10.1161/CIRCULATIONAHA.107.696385
6. Spence JD, Eliasziw M, DiCicco M, Hackam DG, Galil R, Lohmann T. Carotid plaque area: a tool for targeting and evaluating vascular preventive therapy. Stroke (2002) 33(12):2916–22. doi:10.1161/01.STR.0000042207.16156.B9
7. Mathiesen EB, Johnsen SH, Wilsgaard T, Bonaa KH, Lochen ML, Njolstad I. Carotid plaque area and intima-media thickness in prediction of first-ever ischemic stroke: a 10-year follow-up of 6584 men and women: the Tromso Study. Stroke (2011) 42(4):972–8. doi:10.1161/STROKEAHA.110.589754
8. Sillesen H, Muntendam P, Adourian A, Entrekin R, Garcia M, Falk E, et al. Carotid plaque burden as a measure of subclinical atherosclerosis: comparison with other tests for subclinical arterial disease in the High Risk Plaque BioImage study. JACC Cardiovasc Imaging (2012) 5(7):681–9. doi:10.1016/j.jcmg.2012.03.013
9. Hoeks AP, Brands PJ, Smeets FA, Reneman RS. Assessment of the distensibility of superficial arteries. Ultrasound Med Biol (1990) 16(2):121–8. doi:10.1016/0301-5629(90)90139-4
10. van Popele NM, Grobbee DE, Bots ML, Asmar R, Topouchian J, Reneman RS, et al. Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke (2001) 32(2):454–60. doi:10.1161/01.STR.32.2.454
11. White H, Boden-Albala B, Wang C, Elkind MS, Rundek T, Wright CB, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation (2005) 111(10):1327–31. doi:10.1161/01.CIR.0000157736.19739.D0
12. Sacco RL, Gan R, Boden-Albala B, Lin IF, Kargman DE, Hauser WA, et al. Leisure-time physical activity and ischemic stroke risk: the Northern Manhattan Stroke Study. Stroke (1998) 29(2):380–7. doi:10.1161/01.STR.29.2.380
13. Kuo F, Hannah G, Dong C, Cabral D, Della-Morte D, Blanton SH, et al. Traditional cardiovascular risk factors explain only small proportion of the variability in carotid plaque. Stroke (2012) 43(7):1755–60. doi:10.1161/STROKEAHA.112.651059
14. Della-Morte D, Gardener H, Denaro F, Boden-Albala B, Elkind MS, Paik MC, et al. Metabolic syndrome increases carotid artery stiffness: the Northern Manhattan Study. Int J Stroke (2010) 5(3):138–44. doi:10.1111/j.1747-4949.2010.00421.x
15. Riley WA, Evans GW, Sharrett AR, Burke GL, Barnes RW. Variation of common carotid artery elasticity with intimal-medial thickness: the ARIC Study. Atherosclerosis risk in communities. Ultrasound Med Biol (1997) 23(2):157–64. doi:10.1016/S0301-5629(96)00211-6
16. Glagov S. Hemodynamic factors in localisation of atherosclerosis. Acta Cardiol (1965) Suppl 11:311+.
17. Masuda H, Zhuang YJ, Singh TM, Kawamura K, Murakami M, Zarins CK, et al. Adaptive remodeling of internal elastic lamina and endothelial lining during flow-induced arterial enlargement. Arterioscler Thromb Vasc Biol (1999) 19(10):2298–307. doi:10.1161/01.ATV.19.10.2298
18. Chirinos JA. Arterial stiffness: basic concepts and measurement techniques. J Cardiovasc Transl Res (2012) 5(3):243–55. doi:10.1007/s12265-012-9359-6
19. Gomez-Marcos MA, Martinez-Salgado C, Gonzalez-Sarmiento R, Hernandez-Rivas JM, Sanchez-Fernandez PL, Recio-Rodriguez JI, et al. Association between different risk factors and vascular accelerated ageing (EVA study): study protocol for a cross-sectional, descriptive observational study. BMJ Open (2016) 6(6):e011031. doi:10.1136/bmjopen-2016-011031
20. Beaussier H, Masson I, Collin C, Bozec E, Laloux B, Calvet D, et al. Carotid plaque, arterial stiffness gradient, and remodeling in hypertension. Hypertension (2008) 52(4):729–36. doi:10.1161/HYPERTENSIONAHA.108.115972
21. Korshunov VA, Schwartz SM, Berk BC. Vascular remodeling: hemodynamic and biochemical mechanisms underlying Glagov’s phenomenon. Arterioscler Thromb Vasc Biol (2007) 27(8):1722–8. doi:10.1161/ATVBAHA.106.129254
22. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, et al. Mannheim intima-media thickness consensus. Cerebrovasc Dis (2004) 18(4):346–9. doi:10.1159/000081812
23. Seeger JM, Barratt E, Lawson GA, Klingman N. The relationship between carotid plaque composition, plaque morphology, and neurologic symptoms. J Surg Res (1995) 58(3):330–6. doi:10.1006/jsre.1995.1051
24. Steinbuch J, van Dijk AC, Schreuder F, Truijman M, Hendrikse J, Nederkoorn PJ, et al. Definition of common carotid wall thickness affects risk classification in relation to degree of internal carotid artery stenosis: the Plaque At RISK (PARISK) study. Cardiovasc Ultrasound (2017) 15(1):9. doi:10.1186/s12947-017-0097-4
25. Polak JF, Kronmal RA, Tell GS, O’Leary DH, Savage PJ, Gardin JM, et al. Compensatory increase in common carotid artery diameter. Relation to blood pressure and artery intima-media thickness in older adults. Cardiovascular Health Study. Stroke (1996) 27(11):2012–5. doi:10.1161/01.STR.27.11.2012
26. Santelices LC, Rutman SJ, Prantil-Baun R, Vorp DA, Ahearn JM. Relative contributions of age and atherosclerosis to vascular stiffness. Clin Transl Sci (2008) 1(1):62–6. doi:10.1111/j.1752-8062.2008.00014.x
27. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol (2010) 30(2):177–81. doi:10.1161/ATVBAHA.108.173609
28. Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the advisory board of the 3rd and 4th watching the risk symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis (2007) 23(1):75–80. doi:10.1159/000097034
Keywords: carotid artery, carotid intima media thickness, stiffness, atherosclerosis, carotid plaque, carotid ultrasound, arterial remodeling
Citation: Della-Morte D, Gardener H, Dong C, Markert M, Cabral D, Elkind MSV, Sacco RL and Rundek T (2018) Association Between Carotid Artery Function and Structure in the Northern Manhattan Study. Front. Neurol. 9:246. doi: 10.3389/fneur.2018.00246
Received: 08 February 2018; Accepted: 28 March 2018;
Published: 16 April 2018
Edited by:
Antonio Arauz, Instituto Nacional de Neurología y Neurocirugía (INNN), MexicoReviewed by:
Carlos Cantu-Brito, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, MexicoMaurizio Acampa, Azienda Ospedaliera Universitaria Senese, Italy
Copyright: © 2018 Della-Morte, Gardener, Dong, Markert, Cabral, Elkind, Sacco and Rundek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David Della-Morte, ZGRlbGxhbW9ydGUmI3gwMDA0MDttZWQubWlhbWkuZWR1
 David Della-Morte
David Della-Morte Hannah Gardener1
Hannah Gardener1 Matthew Markert
Matthew Markert Tatjana Rundek
Tatjana Rundek