- 1King Abdullah International Medical Research Center (KAIMRC)/Department of Neurosurgery-King Abdulaziz Medical City (KAMC), Ministry of National Guard Health Affairs (MNG-HA), Jeddah, Saudi Arabia
- 2King Abdullah International Medical Research Center/Department of interventional radiology-King Abdulaziz medical city (KAMC), Ministry of National Guard Health Affairs (MNG-HA), Jeddah, Saudi Arabia
- 3King Abdullah International Medical Research Center/College of Medicine – King Saud bin Abdulaziz University for Health Sciences (KSAUHS), Ministry of National Guard Health Affairs (MNG-HA), Jeddah, Saudi Arabia
Background and importance: The tendency of posterior fossa arteriovenous malformations (pfAVM) to develop associated aneurysms (AA) is a well-known phenomenon with an increased total risk of rupture. Most pfAVM and AA develop in the territory of the posterior inferior cerebellar artery while the involvement of the anterior inferior cerebellar artery (AICA) is extremely rare. We describe an unusual case of an arteriovenous malformation (AVM) supplied by the AICA with a “proximal” AA. This unique combination of vascular lesions has been reported in only four cases so far, limiting the available experience that can safely guide the therapeutic intervention.
Clinical presentation: This study describes a 59-year-old female presented with a subarachnoid hemorrhage, Hunt and Hess grade 4. Angiography demonstrated an AVM fed mainly by the right AICA and draining superficially into the transverse sinus (Spetzler–Martin grade II). In addition, there was a ruptured proximal AICA aneurysm. An endovascular approach was chosen to coil the aneurysm and obliterate the AVM using ONYX in a multi-staged process. The patient recovered well without residual deficit at 6-month follow-up.
Conclusion: To the best of our knowledge, this is the first report describing a proximal AICA aneurysm and AVM treated by endovascular means. The outcome was very good, considering the technically demanding location. All previously reported cases with exactly similar lesions were managed surgically, with inconclusive outcomes. The data presented in this study are meant to help in decision-making process for similar cases till more data are available.
Background and Importance
Only 8–12% of intracranial aneurysm and 5–15% of arteriovenous malformations (AVMs) occur in the posterior circulation (1, 2). The association between an AVM and aneurysm of the same artery is a well-known phenomenon, reported in 2.8–9.3% of all AVMs (3). Notably, posterior fossa AVM’s have an increased tendency to develop associated aneurysms compared to AVMs of the anterior circulation (2), and mostly involve the posterior inferior cerebellar artery. The involvement of the anterior inferior cerebellar artery (AICA) is extremely rare (2). Reviewing the literature, only 16 cases of coincident AICA aneurysm and AVM have previously been reported (1, 3–9). Proximal aneurysms, exactly as the index case of this study, occurred in only four cases (7–9).
Herein, we describe an extremely rare case of a cerebellar AVM supplied by the AICA and a proximal aneurysm fed by the same artery, which was managed completely using an endovascular approach. In contrast, all previously reported cases with similar lesion complex were managed surgically. This study provides justifications why endovascular approach was chosen. We also provide a comprehensive review of similar cases reported in the literature.
Methods
This study has been approved by the independent ethics committee (Institutional Review Board) at the King Abdullah International Medical Research Center—Jeddah, Saudi Arabia. A written informed consent was obtained from the index case of this study to participate and publish the paper once the study is done. All related information utilized in this paper was obtained through chart review, patient history, and clinical examination.
Clinical Presentation
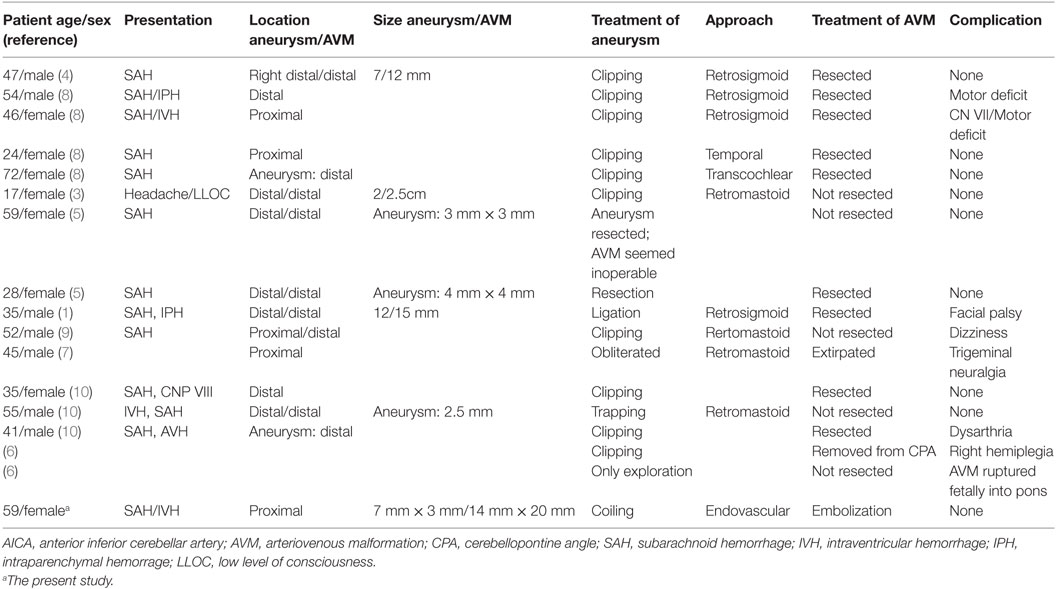
A 59-year-old Saudi woman presented with a deteriorated level of consciousness after 2 days of severe headaches and multiple episodes of vomiting. A non-enhanced brain CT scan showed a subarachnoid hemorrhage (SAH) (Hunt and Hess grade 4–5), intraventricular hemorrhage, and generalized brain edema (Figure 1). Angiographic series delineated a cerebellar AVM with a nidus of 14 mm × 20 mm in diameter, situated on the post meatal segment of AICA and draining superficially into the transverse sinus (Spetzler–Martin grade II). The nidus was primarily supplied by the AICA, which developed a pre-nidal saccular aneurysm measuring 7 mm × 3 mm (Figure 2). The aneurysm was the source of bleeding.
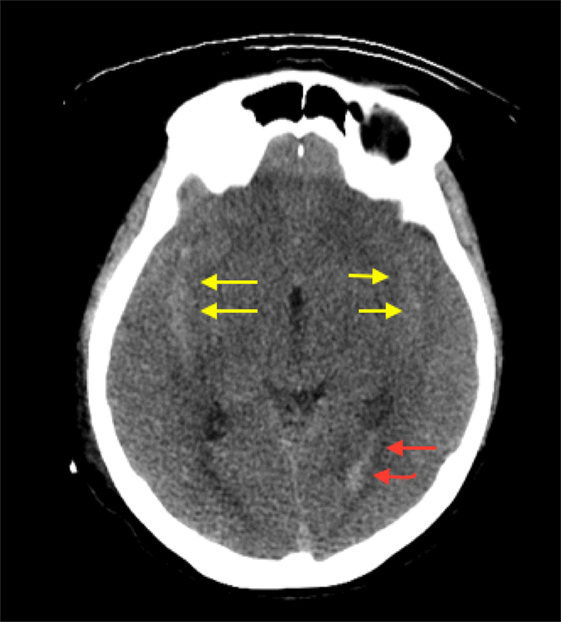
Figure 1. Axial section CT demonstrating diffuse brain edema evident by effacement of cortical sulci and the subarachnoid hemorrhage in both Sylvian fissures (yellow arrows) with seeding into the ventricular system (red arrows).
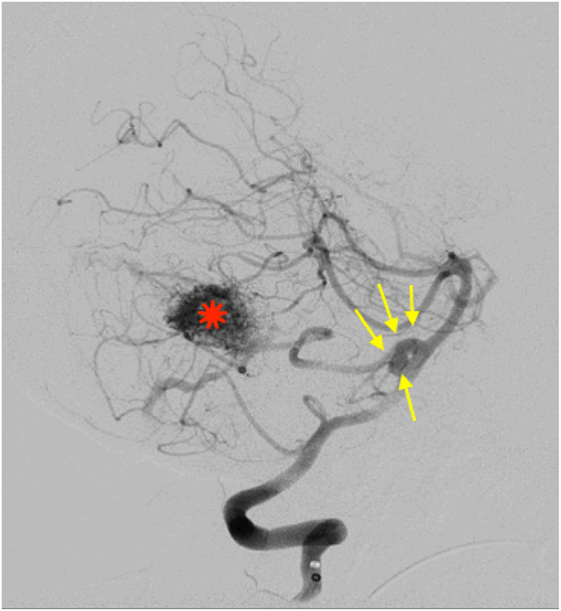
Figure 2. Lateral view of a right vertebral angiography revealing a ruptured proximal aneurysm (7 mm × 3 mm) at the origin of AICA (yellow arrows). Distally on the same trunk, a nidus of an arteriovenous malformation is demonestrated (diameter = 2.6 cm) (red star).
Considering the size and the proximal location of the aneurysm, along with the low grade of the AVM, as well as the generalized brain edema and SAH, an endovascular approach was decided. The aneurysm was accessed using a 5-French wire-guided catheter inserted, within a 6-French sheath, into the right femoral artery and progressed under fluoroscopy road-map guidance. Coiling of the aneurysm was achieved using three platinum-made, detachable coils (3 mm × 8mm, 2 mm × 8mm, 1.5 mm × 4mm). During the same procedure, the distally located AVM was embolized using a liquid-based suspension consisting of Ethylene–Vinyl–Alcohol copolymers (ONYX), applied through a micro-catheter (APOLLO 38), with a 5-cm detachable tip. Seventy percent of the AVM was obliterated initially and then completed after 6 months. The final series of X-Ray (Figure 3) confirmed the proper positioning of the coils within the aneurysmal sac and occlusion of the AVM. The patient recovered well upon rehabilitation with no evidence of rebleeding or focal neurological deficits at 6-month follow-up. She is fully mobile and independent with a Glasgow outcome score of 4–5.
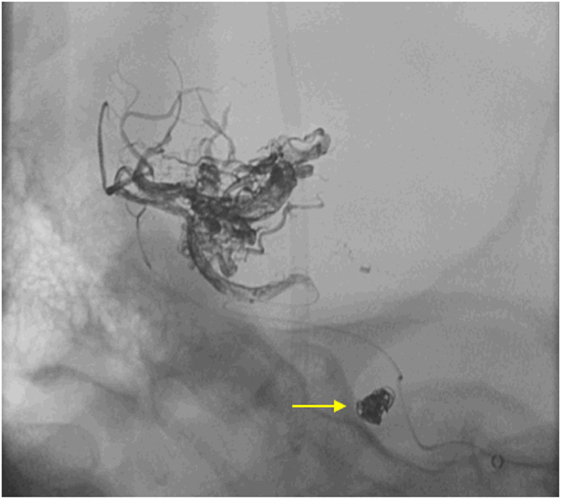
Figure 3. Final run X-Ray demonstrating the position and configuration of the platinum coils inside the sac of the aneurysm (yellow arrow) as well as the ONYX filling the vascular channels of the arteriovenous malformation after the procedure.
Discussion
AVM with AA: The Theory of Hemodynamic Interaction
The therapeutic intervention for AVMs with associated pre-nidal aneurysms is complex and multifaceted. A key concept to consider is that both lesions are equally exposed to the same high-pressure arterial flow simultaneously. Therefore, the hemodynamic stress is distributed on both lesions in a way determined by function of the vascular capacitance of each lesion (2). Thus, treatment of either lesion alone can cause the other one to rupture, owing to the hemodynamic alteration that occurs after the procedure (3). Some authors have, therefore, recommended treating the symptomatic lesion first, and subsequently securing the other lesion during the same procedure (3). In this study, we attempted to secure the ruptured aneurysm first by coiling, followed by the embolization of the AVM with no adverse outcomes observed.
Approach Consideration: The Decision to Coil or to Clip
The decision to coil or to clip an aneurysm has been debated for many years. Unfortunately, no simple and straightforward answer can be provided. However, clipping of AICA aneurysm presents a magnificent challenge because of its small caliber, torturous course and proximity to eloquent areas and multiple cranial nerves (3). Complications are reported to occur after this procedure in up to 60% of cases, even when performed by experienced surgeons (3). Classically, clipping of AICA aneurysms is usually done through a retrosigmoid approach as it provides an adequate surgical corridor exposing the entire area of the AICA (8). However, in a state of acute cerebellar edema, as seen with the index case, more laborious retractions of the cerebellum would be necessary to achieve an adequate exposure. This can potentially jeopardize the nearby vital structures such as the cranial nerves V–VIII, the brainstem, and the cerebellum itself (8).
On the other side, endovascular coiling has been in clinical use since 1995 (8). In a single-center study, five out of 34 patients diagnosed with isolated AICA aneurysms were treated with an endovascular approach, which was successful in 3/5 (8).
As the evidence is somehow still conflicting, and the absolute benefit of either coiling or clipping these lesions was not clearly provided in the literature, “do no harm” was the principle of our priority. Endovascular intervention was chosen as it provides an easy access for both lesions without disturbing the integrity of nearby structures complicated by edema and SAH-related vasospasm.
A Comparison with Similar Cases
None of the previous 16 cases of aneurysms and AVMs of AICA were treated with endovascular intervention (1, 3–9); see (Table 1). We suggest that endovascular approach, whenever affordable and technically feasible, should be considered in the treatment of an AVM and proximal aneurysm that are both fed by AICA. Supporting this, previously published data indicated that coil embolization was particularly useful for proximal AICA aneurysms associated with distal AVM and probably being the treatment of choice (1). A stronger evidence has come from a landmark multi-center study, the ISAT trial (10). However, it should be noted that this trial did not specifically consider the presence of associated AVMs and most of the enrolled cases were having aneurysms in the anterior circulation, not in the posterior fossa. This would create a potential bias.
The case reported here, being managed by endovascular approach, sustained an uneventful course in the immediate post interventional period as well as on 6-month follow up. No residual neurological deficit occurred and the patient was fully mobile and independent.
Conclusion
To the best of our knowledge, this study is the first report describing a proximal AICA aneurysm and AVM treated by endovascular means. The outcome was highly promising, considering the technically demanding location and the complexity of the target lesions. In comparison, all previously reported cases with exactly similar lesions were managed surgically, with inconclusive outcomes. A collaboration of a multi-disciplinary team, including a neurosurgeon, an interventional radiologist, intensivists, and physiotherapists, is highly suggested, with potential impact on the outcome. The results of the reported case are meant to help in the decision-making process for similar cases till more data are available on this rare occasions.
Ethics Statement
This study was carried out in accordance with the recommendations of “King Abdullah International Medical Research Center” with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the “independent ethics committee (Institutional Review Board—IRB) at the King Abdullah International Medical Research Center (KAIMRC)—Jeddah, Saudi Arabia.”
Author Contributions
All authors of this manuscript have actively participated in data acquisition of this paper and they all revise and approve the final form of this paper. They are also responsible for the accuracy and integrity of this work. HK and RS participated in the design of the study. FA and AA did work on the interpretation of the data.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Li X, Zhang D, Zhao J. Anterior inferior cerebellar artery aneurysms: six cases and a review of the literature. Neurosurg Rev (2011) 35(1):111–9. doi:10.1007/s10143-011-0338-1
2. Magro E, Chainey J, Chaalala C, Al Jehani H, Fournier JY, Bojanowski MW. Management of ruptured posterior fossa arteriovenous malformations. Clin Neurol Neurosurg (2015) 128:78–83. doi:10.1016/j.clineuro.2014.11.007
3. Lee SH, Koh JS, Bang JS, Kim GK. A case of ruptured peripheral aneurysm of the anterior inferior cerebellar artery associated with an arteriovenous malformation: a less invasive image-guided transcortical approach. J Korean Neurosurg Soc (2009) 46(6):577–80. doi:10.3340/jkns.2009.46.6.577
4. Menovsky T, André Grotenhuis J, Bartels RHMA. Aneurysm of the anterior inferior cerebellar artery (AICA) associated with high-flow lesion: report of two cases and review of literature. J Clin Neurosci (2002) 9:207–11. doi:10.1054/jocn.2001.0945
5. Gács G, Viñuela F, Fox AJ, Drake CG. Peripheral aneurysms of the cerebellar arteries. Review of 16 cases. J Neurosurg (1983) 58(1):63–8. doi:10.3171/jns.1983.58.1.0063
6. Arnaout OM, Gross BA, Eddleman CS, Bendok BR, Getch CC, Batjer HH. Posterior fossa arteriovenous malformations. Neurosurg Focus (1986) 26(5):E12. doi:10.3171/2009.2.FOCUS0914
7. Kenji K, Nobuo K, Jinichi S, Kazuo W, Masayoshi K. Trigeminal neuralgia associated with posterior fossa arteriovenous malformation and aneurysm fed by the same artery case report. Neurol Med Chir (Tokyo) (1990) 30:918–21. doi:10.2176/nmc.30.918
8. Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms: surgical approaches and outcomes – a review of 34 cases. Neurosurgery (2004) 55(5):1025–35. doi:10.1227/01.NEU.0000141083.00866.82
9. Akyüz M, Tuncer R. Multiple anterior inferior cerebellar artery aneurysms associated with an arteriovenous malformation: case report. Surg Neurol (2005) 64(Suppl 2):106–8. doi:10.1016/j.surneu.2005.07.037
10. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, sezuires, rebleeding, subgroups, and aneurysm occlusion. Lancet (2005) 366:809–17. doi:10.1016/S0140-6736(05)67214-5
Keywords: arteriovenous malformation, aneurysm, anerior inferior cerebellar artery, endovascular approach, posterior fossa
Citation: Khayat HA, Alshareef F, Alshamy A, Algain A, Alhejaili E, Alnabihi O, Alzahrani S and Stendel R (2017) Pure Endovascular Management of an Arteriovenous Malformation and an Aneurysm Both Supplied by Anterio-Inferior Cerebellar Artery: A Case Report and a Review of Literature. Front. Neurol. 8:382. doi: 10.3389/fneur.2017.00382
Received: 04 May 2017; Accepted: 18 July 2017;
Published: 02 August 2017
Edited by:
Ossama Yassin Mansour, Alexandria University, EgyptReviewed by:
Nabil Kitchener, General Organization for Teaching Hospitals and Institutes GOTHI, EgyptEdgard Pereira, Aventura Hospital and Medical Center, United States
Copyright: © 2017 Khayat, Alshareef, Alshamy, Algain, Alhejaili, Alnabihi, Alzahrani and Stendel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hassan A. Khayat, hasssan.a.k@gmail.com
 Hassan A. Khayat
Hassan A. Khayat Fawaz Alshareef2
Fawaz Alshareef2 Omar Alnabihi
Omar Alnabihi Ruediger Stendel
Ruediger Stendel