
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Behav. Neurosci., 06 December 2022
Sec. Motivation and Reward
Volume 16 - 2022 | https://doi.org/10.3389/fnbeh.2022.1061877
Introduction: Kaixinsan (KXS) has been in use as an effective classic formulation of traditional Chinese medicine for depression. However, its active components and action mechanism against depression remain elusive. The purpose of this study was to summarize and evaluate the efficacy and potential pharmacological mechanisms of KXS in antidepressant treatment.
Materials and methods: Reports on the use of KXS in the treatment of depression were systematically collected from PubMed, Web of Science, Embase, China National Knowledge Infrastructure, Chongqing VIP, and Wanfang Data from the establishment to July 2022, including those on mood disorders in neurological diseases such as Alzheimer’s disease. Meta-analysis was conducted with the Review Manager 5.3 software. Online datasets, traditional Chinese medicine system pharmacological analysis platform, GeneCards, online Mendelian inheritance in man, and DisGeNET were used to investigate the depression-related genes. The gene ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichments were performed to construct the ‘component-target-pathways’ network using Metascape online analyses.
Result: Ten studies were included in the analysis. Meta-analysis showed that both low-dose KXS (SMD = 19.66, Z = 7.96, and I2 = 42%) and high-dose KXS (SMD = 23.84, Z = 8.46, and I2 = 13%) could increase the sucrose preference in depression models. In addition, 5-hydroxytryptamine (5-HT) (SMD = 10.91, Z = 2.95, and I2 = 50%) returned to normal level after the treatment at low dose KXS. In network pharmacology, 50 active components and 376 gene targets were screened out. AKT1, GAPDH, ALB, TNF, and TP53 were the core target proteins. GO analysis showed that KXS mainly treats depression in biological processes such as response to drugs, cellular calcium ion homeostasis, and regulation of chemical synaptic signal transmission. KEGG results show that the mechanism of action of KXS in treating depression is through neural activity ligand-receptor interaction, the calcium signaling and CAMP signaling pathways.
Discussion: The study reveals the active components and potential molecular mechanism of KXS in the treatment of depression and provides evidence for future basic research.
In recent years, numerous studies have shown the need for increased attention to mental health (Pan et al., 2021). Deaths caused by mental disorders account for 14.3% of global mortality (Walker et al., 2015), and depression is one of the most common mental disorders. Depression is characterized by loss of pleasure, fatigue, and worthlessness, as well as cognitive impairment and neurotrophic symptoms including anorexia, memory alterations, and sleep disturbances (Ribeiro et al., 2018). To date, little is known about the etiology of depression. A sequence of stressful events leads to negative physical and psychological effects, and such changes are tightly linked with the depression (Yang et al., 2015). Depression is often insidious and unpredictable (Malhi and Mann, 2018). One reason is that some depressed patients choose to conceal their mental symptoms to avoid being stigmatized (Dubovsky et al., 2021). Patients with other frequently occurring diseases are at high risk of depression (Read et al., 2017); however, there is the possibility of focusing on the underlying disease and ignoring depressive symptoms. The elderly are at risk of frequently occurring diseases due to reduced physical activity and worsening health status (Reynolds et al., 2019). In addition, bereavement, living alone, lack of social attention, lack of sleep (Casey, 2017), and aging have been identified as independent risk factors for depression. Depression in older adults often accompanies cognitive impairment, making it more difficult to identify (Linnemann and Lang, 2020). Depression increases the risk of obesity, coronary artery disease, and inflammation (Aksay et al., 2016; Biffi et al., 2017; Leonard, 2018). At present, western medicine antidepressants mainly include the following categories: monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants (TCAs), and serotonin reuptake inhibitors (SSRIs). However, chemical drugs are often accompanied by clinical problems such as adverse reactions and drug resistance (Willner et al., 2014). There were nearly half of the patients still failed to respond after receiving multiple antidepressant treatments, or relapse again due to trivial matters, which is not conducive to recovery of the patients and increases the possibility of developing refractory depression (Belzung, 2014; Dodd et al., 2021).
Traditional Chinese medicine prescriptions composed of multiple herbs can act on different targets at the same time and have long been found to be effective in health care and disease treatment (Zhang et al., 2013). Kaixinsan (KXS), recorded in Sun Simiao’s “Prescriptions for Emergencies” in the Tang Dynasty, was used to treat dementia and amnesia; other herbs include Ginseng Radix Rhizoma (GR; root and rhizome of Panax ginseng C. A. Mey.), Polygalae Radix (PR; root of Polygala tenuifolia Wild.), Acori Tatarinowii Rhizoma (ATR; rhizome of Acorus tatarinowii Schott), and Poria [PO; sclerotium of Poriacocos (Schw.) Wolf]. The ratio of the four herbs in the prescription is 1:1:25:50. Modern clinical studies have shown that KXS has significant efficacy in the treatment of depression associated with multiple causes (Fu et al., 2019; Hu et al., 2021a,b).
Although KXS has been proven to be a classical Chinese medicine compound with a positive effect on depression, the underlying mechanism of its effect has not been fully elucidated. A meta-analysis, combined with network pharmacology, was used in this study to systematically evaluate the efficacy and pharmacological mechanism of KXS for depression. The results will promote further research on the treatment of depression.
The reports on experiments on the use of KXS in the treatment of depression were systematically collected from PubMed, Web of Science, Embase, China National Knowledge Infrastructure (CNKI), Chongqing VIP (CQVIP), and Wanfang Data from the establishment to July 2022, the searched keywords were kaixinsan, kai-xin-san, depression, mood disorders. As depression is one of the main psychiatric symptoms of AD, AD models with depressive symptoms were also included in the analysis. See Supplementary material for the search strategy.
Studies on animal models of depression were included in the analysis, and there were no restrictions on animal species, sex, age, and weight. KXS is only used as an intervention drug, and there is no limit to its dosage. Other positive therapeutic drugs and Chinese herbal medicine prescriptions were not added; the control group was treated with non-therapeutic liquid (normal saline or distilled water); the evaluation of the outcome after treatment was based on the index level of depressive function or mechanism.
Reviews, conference abstracts, non-animal studies, studies incorporating other traditional Chinese medicine prescriptions, and duplicate articles were excluded.
All articles were screened and included by two independent researchers. Relevant information was extracted from the included studies, including authors, year of publication, sex, age, weight, number, dose of KXS, and data on outcome assessment of experimental animals. Getdate software was used to extract the data for graphical representation.
Review Manager 5.3 was used for the meta-analysis. Two independent researchers used the SYRCLE Animal experimental bias risk assessment tool to evaluate the included articles, and any disagreements were resolved through consultation. The SYRCLE animal experiment bias risk assessment tool was for animal experiment assessment, which was established on the basis of the Cochrane bias risk assessment tool. It included 10 items in total, among which baseline characteristics, randomization of animal placement, and assessment of random results were new items. In the results, data such as the sucrose preference index in the sucrose preference test, and 5-HT levels were treated as continuous data. Standard mean difference (SMD) and 95% confidence interval (CI) were determined using Review Manager 5.3. A random effects model was also used on the data to estimate combined effect sizes, the Q statistic was used to assess heterogeneity, and the I2 statistic was used to quantify the magnitude of heterogeneity.
The traditional Chinese medicine system pharmacological analysis platform (TCMSP)1 was used to collect the traditional Chinese medicine ingredients of GR, PO, and ATR, and the oral bioavailability (OB) was set to be ≥ 30%. The drug-likeness (DL) was ≥ 0.18 (Pang et al., 2018) and the active ingredients of traditional Chinese medicine were obtained. The active ingredients of PR were obtai ned at the herb station.
The compounds of KXS obtained from the TCMSP database were used to obtain the action targets of GR, PO, and ATR according to MOL ID. The effective components of PR were imported into the Pubchem database,2 and the components SMILES (simplified molecular input line entry system) and the chemical structural formula were obtained. In the same line, the structural formula was imported into the database, swisstargetprediction3 to predict the target. The UniProt4 database was used to download the compound data table. The “TRIM” function is used to optimize the data, the “VLOOKUP” function was used to match the target gene name. We supplemented the unmatched gene names by consulting the literature. The relevant target proteins of the chemical components obtained by the above methods were annotated using UniProt.
GeneCards,5 online Mendelian inheritance in man (OMIM),6 and Disgenet7 platforms were used to obtain disease-related targets. “Depression” was used as the keyword to search for depression-related targets. Setting the disease object as “human,” the “VLOOKUP” function was used to match the target gene names and screen out the intersection genes of drugs and diseases.
The Venny8 software was used to obtain the intersection targets of the active compounds of herbs and depression as potential targets for the treatment of depression in traditional Chinese medicine.
The four traditional Chinese herbs, their drug-related active chemical components, and the predicted target gene were imported into Cytoscape (V3. 7. 2) software. Using the degree of analysis of the imported data, the protein interaction network diagram of traditional Chinese medicine, active ingredients, and predicted targets were formed.
The intersection genes were input to the String9 platform, setting the object as “homo sapiens,” the highest confidence score was 0.9, and the free gene nodes were hidden to obtain the protein-protein interaction (PPI) relationship. The results were imported into Cytoscape 3.7.2, and “network analyze” was selected to obtain the network topology parameters.
Degree referred to the interconnection between proteins. Betweenness centrality (BC) reflects the number of times the shortest path passes through a single node. Closeness centrality (CC) means the ease of communication between nodes.
Gene ontology (GO) enrichment and KEGG (Kyoto encyclopedia of genes and genomes) helped explain the biological process of the target and its role in metabolism and signal transduction. Drug-disease targets were input into the String database and DAVID database10 to obtain the GO enrichment and KEGG pathway. The species was restricted to Homo sapiens, and only the items with a p-value < 0.05 were displayed. The bubble diagram was drawn using R software.
After screening, 10 out of 225 studies (Table 1) were included in the analysis (Dang et al., 2009; Zhou et al., 2012; Zhu et al., 2012, 2016; Dong et al., 2013, 2016, 2017; Jiang et al., 2021; Qu et al., 2021; Yu et al., 2021; Figure 1). As one of the indexes of depression function, eight studies measured sucrose preference in depression model rats. Four studies analyzed the outcome of sucrose consumption after treatment with KXS (Zhu et al., 2012; Dong et al., 2013, 2016; Qu et al., 2021). The results show that both low-dose KXS (P < 0.00001, SMD = 19.66, 95% confidence interval [14.82, 24.50], heterogeneity: x2 = 5.16, I2 = 42%, Figure 2A) and high-dose KXS (P < 0.00001, SMD = 23.84, 95% confidence interval [18.32, 29.36], heterogeneity: x2 = 3.45, I2 = 13%, Figure 2B) could increase sucrose consumption of depression models. In the same line, four studies evaluated sucrose preference in depression models before and after KXS treatments (Zhu et al., 2016; Dong et al., 2017; Jiang et al., 2021; Yu et al., 2021), both low-dose KXS (P = 0.003, SMD = 19.31, 95% confidence interval [6.49,23.13], heterogeneity: x2 = 18.37, I2 = 84%, Figure 2C) and high-dose KXS (P = 0.0004, SMD = 24.55, 95% confidence interval [10.88, 38.2], heterogeneity: x2 = 20.24, I2 = 85%, Figure 2D) showed positive effects. Four studies reported levels of 5-hydroxytryptamine (5-HT) (Dang et al., 2009; Zhou et al., 2012; Zhu et al., 2012; Dong et al., 2013). The data showed that after using low-dose KXS (P = 0.003, SMD = 10.91, 95% confidence interval [3.67, 18.16], heterogeneity: x2 = 4.03, I2 = 50%, Figure 2E) 5-HT levels recovered to normal level, but when high-dose KXS was used to assess the level of 5-HT in the depression models, there was no significant difference between the treatment group and the control group (P = 0.21, SMD = 45.55, 95% confidence interval [−25.22, 116.32], heterogeneity: x2 = 5.41, I2 = 63%, Figure 2F). The low risk rate was 42%, the medium risk rate was 52%, and the high risk rate was 6% in all items of animal experiment evaluation. All studies provided brief study details, the number and total of animals in each group were listed, and randomization was used for grouping, but no further method was specified. In terms of animal experiments, nine studies have described the animal species, only one study has provided age, but all studies have provided the animal weight and gender. During the experiment, each study recorded the experimental method and time, but lacked a specific description of the principle (Table 2).
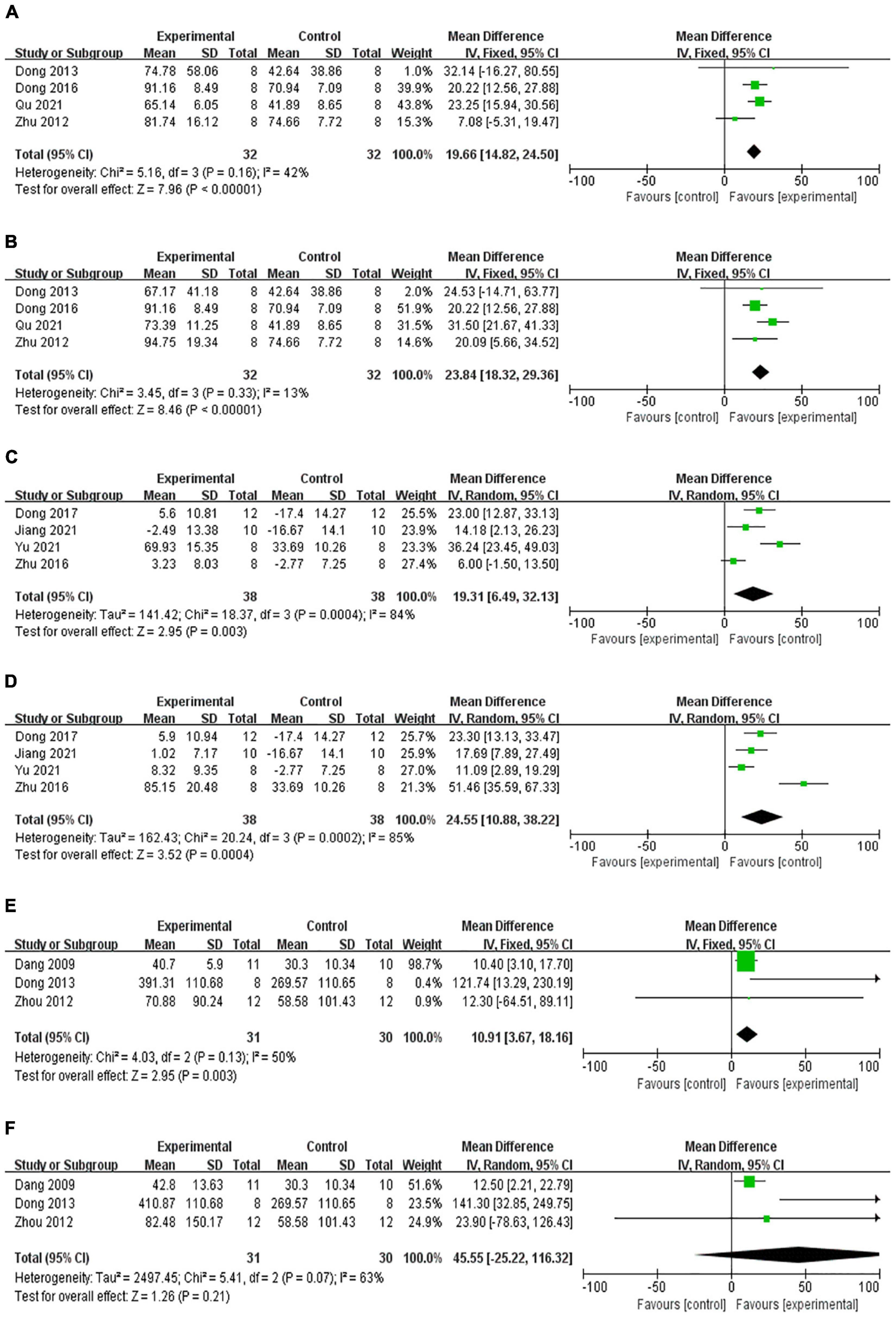
Figure 2. Forest plot shows that low-dose (A) and high-dose (B) KXS increased the sucrose consumption in the depression model, compared with sucrose consumption before and after treatment with KXS, which shows a statistically significant increase in sucrose preference at both low-dose (C) and high-dose (D). Low-dose KXS could increase the 5-HT levels (E), not statistically significant in the 5-HT level following high-dose KXS (F).
Pharmacokinetics is the process of studying the absorption, distribution, metabolism, and excretion (ADME) of drugs in the body. Based on the ADME index (OB ≥ 30%, DL ≥ 0.18), 60 compounds of KXS were selected, including 22 species of GR, 15 species of PO, 4 species of ATR (Table 3), and 19 species of PR (Table 4). After removing non-targeted compounds, 46 active compounds were finally included in the analysis.
The relationship between each herb and the predicted target in KXS (Figure 3). The inverted triangle represented the constituent drugs of the compound KXS, the regular hexagon represented the active ingredient of each drug, and the diamond represented the predicted target of each active ingredient.

Figure 3. The inverted triangle represented the constituent drugs of the compound KXS, the regular hexagon represented the active ingredient of each drug, and the diamond represented the predicted target of each active ingredient. RS, Ginseng Radix Rhizoma (GR; root and rhizome of Panax ginseng C. A. Mey.); FL, Poria [PO; sclerotium of Poriacocos (Schw.) Wolf]; YZ, Polygalae Radix (PR; root of Polygala tenuifolia Wild.); SCP, Acori Tatarinowii Rhizoma (ATR; rhizome of Acorus tatarinowii Schott).
After deduplication, 3878 depression-related targets were obtained in the GeneCards, OMIM, and Disgenet databases. Six hundred and fifty-seven targets of the KXS were predicted to be related to depression. Finally, 376 targets were the same as drugs and diseases (Figure 4), which were the final predicted targets for treating depression with KXS.
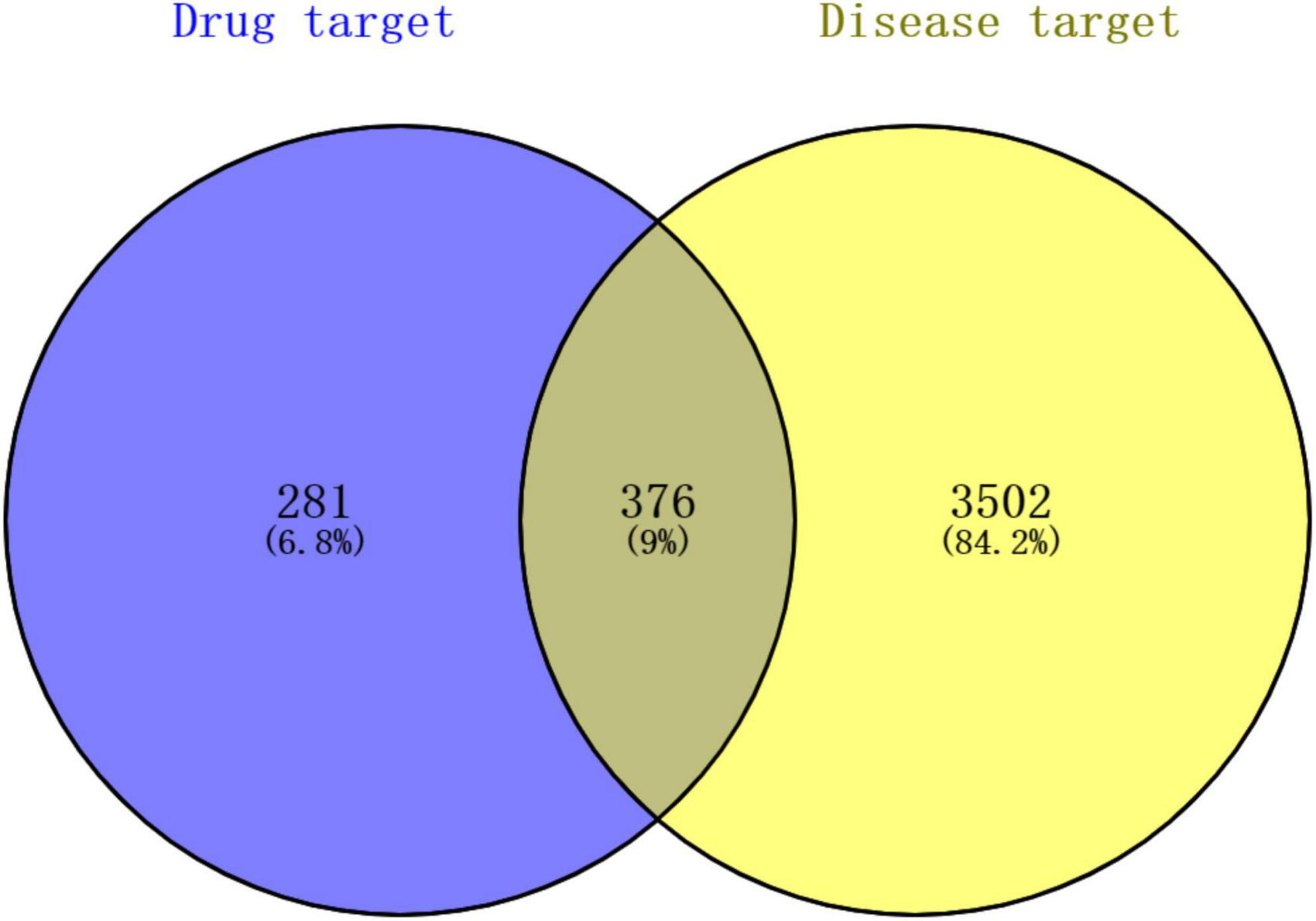
Figure 4. Venn diagram of the targets of the active ingredients of KXS and the depression-related targets. Blue bubble shows the potential targets of KXS, the yellow bubble represents the targets of depression. The overlapping part of the circles represents potential herbs target for depression therapy.
The intersection genes were imported into the protein interaction analysis platform String, the episomal node was hidden, and the PPI relationship diagram was obtained (Figure 5). The larger and darker circles in the center (AKT1, GAPDH, ALB, TNF, TP53, EGFR, SRC, VEGFA, and MAPK3) indicated that these genes were more critical in the treatment of depression with KXS.
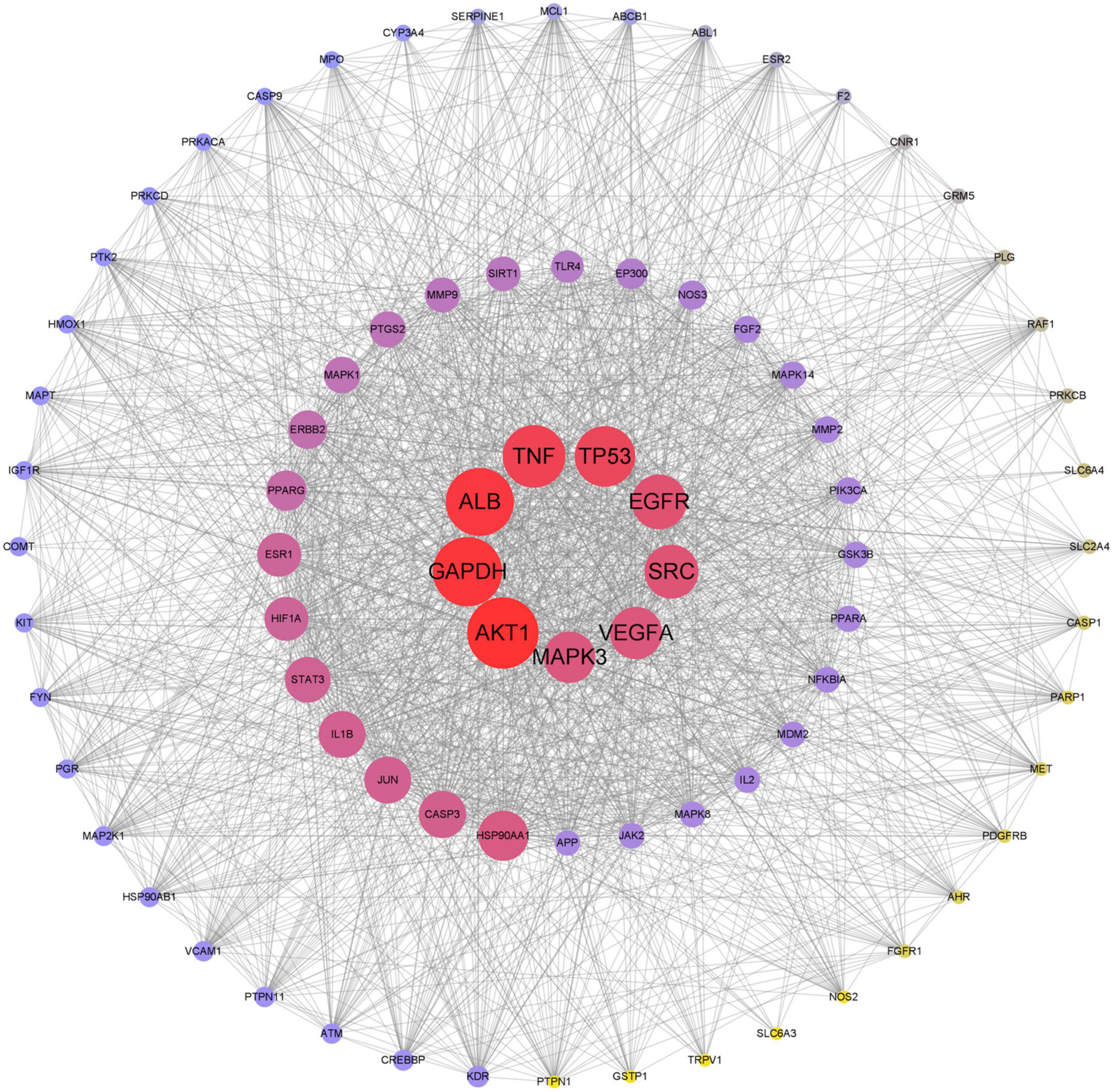
Figure 5. Protein-protein interaction (PPI). The larger and darker circle in the center indicated that these genes were more critical in the treatment of depression with KXS.
Gene ontology function and KEGG enrichment analysis were performed on 376 intersecting targets, and the enrichment condition was P < 0.05. The GO function includes three parts: molecular function (MF), biological process (BP), and cellular component (CC). Target genes in MF were mainly enriched in drug binding (GO: 0008144), neurotransmitter receptor activity (GO: 00.30594), nuclear receptor activity (GO: 0004878), and ligand-activated transcription factor activity (GO: 0098531) (Figure 6A). The top five terms in the biological processes were: response to drug (GO: 0042493), cellular calcium ion homeostasis (GO: 0006874), positive regulation of protein serine/threonine kinase activity (GO: 0071902), calcium ion transport (GO: 0006816), and vascular process in the circulatory system (GO: 0003018) (Figure 6B). The most common cellular components of target genes were the membrane raft (GO: 0045121), the membrane microdomain (GO: 0098857), and the membrane region (GO: 0098589) (Figure 6C). KEGG enrichment analysis showed that KXS in the treatment of depression mainly exerted its effects through lipid and atherosclerosis, neuroactive ligand-receptor interaction, calcium signaling pathway, and chemical carcinogenesis-receptor activation (Figure 7).
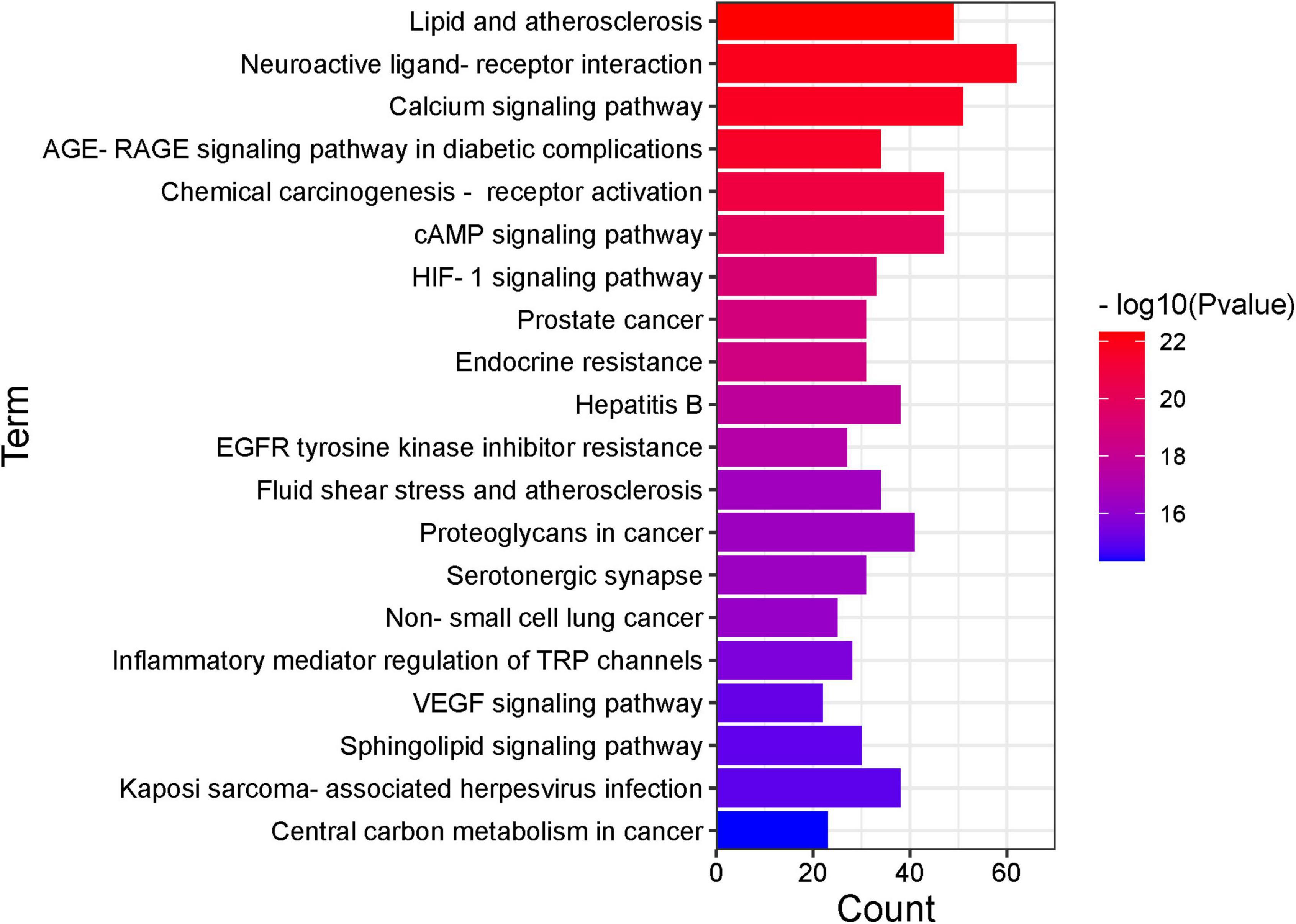
Figure 7. Kyoto encyclopedia of genes and genomes (KEGG) pathway (top 20). The x-axis represents the number of target genes in each pathway and the ordinate represents each entry.
Using the research method of network pharmacology to analyze traditional Chinese prescription, the single corresponding relationship of “one disease-one drug-one gene” has been broken, and the efficient utilization of multiple targets and effects between drugs and disease has been identified (Shen et al., 2020).
The efficacy of KXS in the treatment of depression was assessed in a meta-analysis using sucrose consumption and 5-HT level in a depression model as indicators. Seventy mice were included in eight studies for sucrose preference analysis, four studies evaluated 5-HT levels, and 38 animals were included. The results of the study showed a positive effect in the treatment of depression with KXS. Nevertheless, this study also had some shortcomings. One concern was that the number of animals included was relatively limited.
The PPI network shows that the core targets of KXS in treating depression were AKT1, GAPDH, ALB, TNF, TP53, EGFR, SRC, VEGFA, and MAPK3. AKT1 is one of the serine/threonine kinases, which participates in monoamine neurotransmission (Machado-Vieira et al., 2015). Additionally, there was a significant correlation between the severity of depression and the AKT1 gene polymorphisms. One theory was that AKT1 was closely related to bipolar disorder (BD), a mental genetic disease characterized by depression and mania. AKT1 was a first-line target for treatment of BD (Beaulieu, 2012). Although a recent cohort study contradicted the relationship between AKT1 and BD (Millischer et al., 2020), the correlation with the occurrence of depression was certain. AKT1 participates in the myelination of the peripheral nervous system and neurotrophic protein signaling pathway: the AKT/mTOR pathway may be the common core target of psychoactive drugs (Musashe et al., 2016; Liu et al., 2018). GAPDH, tumor necrosis factor (TNF), and TP53 were closely related to apoptosis. The GAPDH level in blood was positively correlated with Alzheimer’s disease (AD; Tsai et al., 2020). TNF induce low-grade inflammation, and inflammatory cytokines were the receptor regulators of 5-HT, which were related to the pathogenesis of anxiety and major depression (Schmidt et al., 2019; Karadag et al., 2021). TP53 was involved in astrocyte autophagy and neuronal apoptosis, which was the antidepressant mechanism of fluoxetine (Shu et al., 2019).
The lipid and atherosclerosis pathway in KEGG analysis was one of the key pathways in the treatment of depression with KXS. Omega-3 polyunsaturated fatty acids in lipids, including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), play an important role in antidepression and neuroprotection (Borsini et al., 2021). The lack of DHA may cause depression (Hsu et al., 2018). Furthermore, some studies showed that plasma lipoprotein was potentially related to the aggravation of depressive symptoms (Hui et al., 2021).
Patients with AD have an increased social burden due to cognitive and emotional disorders. As the second most common mental symptom of AD, depression increases the disability rate of AD patients. Prior studies have demonstrated the usefulness of KXS for AD (Yi et al., 2020), indeed, KXS reduced oxidative stress through acetylcholine, leading to improved cognitive function (Xu et al., 2019). This study explored the positive effects and mechanisms of KXS on emotions from the perspective of mental health. The research results helped promote the recovery of AD patients in many aspects. The majority of network pharmacological research about antidepression drugs focused on safety because of their diverse reactions (Cipriani et al., 2018; Cortese et al., 2018; Zhou et al., 2020), but KXS, as a Chinese medicine prescription with higher safety, is more focused on the exploration of the promotion mechanism.
This study was mainly based on big data analytics. Further pharmacological experimental evidence is needed to investigate the antidepressant effect of KXS. Moreover, the evaluation of the efficacy of KXS in this study was limited to animal models. Although an accurate animal model can reproduce the pathophysiological changes of human diseases, the uncertainty and repeatability of depression increase the difficulty to cure the disease, and more clinical studies should be actively carried out to the premise of ensuring safety.
We explored the treatment of depression with the traditional Chinese prescription, KXS, by integrating meta-analysis and network pharmacology. Our study proved that KXS is capable of systematically improving depression symptoms through multi-target and multi-pathway systems. Elucidation of the components of the pathway and core targets with a high likelihood for translation into therapies for depression. Multi-pathways will not only greatly increase the multitarget effect, but overcome resistance and adverse effects. Therefore, the present findings may have important implications for clinical studies.
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
ZL and GW designed the research. HZ and XJ did the proofreading. JX performed the image production and editing. MB and HJZ collected and analyzed the data and wrote the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the National Natural Science Foundation of China (grant no. 81973803) and the Science and Technology Innovation Cultivation Program of Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (grant nos. YD202210 and YD202219).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnbeh.2022.1061877/full#supplementary-material
AD, Alzheimer’s disease; ADME, absorption, distribution, metabolism, and excretion; ATR, Acori Tatarinowii Rhizoma; BC, betweenness centrality; BD, bipolar disorder; BP, biological process; CC, cellular component; CC, closeness centrality; CI, confidence interval; CNKI, China national knowledge infrastructure; CQVIP, Chongqing VIP; DHA, docosahexaenoic acid; DL, drug-likeness; EPA, eicosapentaenoic acid; GR, Ginseng Radix Rhizoma; KXS, Kaixinsan; MF, molecular function; OB, oral bioavailability; OMIM, online Mendelian inheritance in man; PO, Poria; PPI, protein-protein interaction; PR, Polygalae Radix; SMD, standard mean difference; SMILES, simplified molecular input line entry system; TCMSP, traditional Chinese medicine system pharmacological analysis platform; TNF, tumor necrosis factor.
Aksay, S. S., Bumb, J. M., Janke, C., Biemann, R., Borucki, K., Lederbogen, F., et al. (2016). Serum lipid profile changes after successful treatment with electroconvulsive therapy in major depression: A prospective pilot trial. J. Affect. Disord. 189, 85–88. doi: 10.1016/j.jad.2015.09.037
Beaulieu, J. M. (2012). A role for Akt and glycogen synthase kinase-3 as integrators of dopamine and serotonin neurotransmission in mental health. J. Psychiatry Neurosci. 37, 7–16. doi: 10.1503/jpn.110011
Belzung, C. (2014). Innovative drugs to treat depression: Did animal models fail to be predictive or did clinical trials fail to detect effects? Neuropsychopharmacology 39, 1041–1051. doi: 10.1038/npp.2013.342
Biffi, A., Scotti, L., and Corrao, G. (2017). Use of antidepressants and the risk of cardiovascular and cerebrovascular disease: A meta-analysis of observational studies. Eur. J. Clin. Pharmacol. 73, 487–497. doi: 10.1007/s00228-016-2187-x
Borsini, A., Nicolaou, A., Camacho-Munoz, D., Kendall, A. C., Di Benedetto, M. G., Giacobbe, J., et al. (2021). Omega-3 polyunsaturated fatty acids protect against inflammation through production of LOX and CYP450 lipid mediators: Relevance for major depression and for human hippocampal neurogenesis. Mol. Psychiatry 26, 6773–6788. doi: 10.1038/s41380-021-01160-8
Casey, D. A. (2017). Depression in Older Adults: A Treatable Medical Condition. Prim. Care 44, 499–510. doi: 10.1016/j.pop.2017.04.007
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., et al. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet 391, 1357–1366. doi: 10.1016/s0140-6736(17)32802-7
Cortese, S., Adamo, N., Del Giovane, C., Mohr-Jensen, C., Hayes, A. J., Carucci, S., et al. (2018). Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. Lancet Psychiatry 5, 727–738. doi: 10.1016/s2215-0366(18)30269-4
Dang, H., Sun, L., Liu, X., Peng, B., Wang, Q., Jia, W., et al. (2009). Preventive action of Kai Xin San aqueous extract on depressive-like symptoms and cognition deficit induced by chronic mild stress. Exp. Biol. Med. 234, 785–793. doi: 10.3181/0812-RM-354
Dodd, S., Bauer, M., Carvalho, A. F., Eyre, H., Fava, M., Kasper, S., et al. (2021). A clinical approach to treatment resistance in depressed patients: What to do when the usual treatments don’t work well enough? World J. Biol. Psychiatry 22, 483–494. doi: 10.1080/15622975.2020.1851052
Dong, X. Z., Li, Z. L., Zheng, X. L., Mu, L. H., Zhang, G. Q., and Liu, P. (2013). A representative prescription for emotional disease, Ding-Zhi-Xiao-Wan restores 5-HT system deficit through interfering the synthesis and transshipment in chronic mild stress-induced depressive rats. J. Ethnopharmacol. 150, 1053–1061. doi: 10.1016/j.jep.2013.10.018
Dong, X. Z., Wang, D. X., Lu, Y. P., Yuan, S., Liu, P., and Hu, Y. (2017). Antidepressant effects of Kai-Xin-San in fluoxetine-resistant depression rats. Braz. J. Med. Biol. Res. 50:e6161. doi: 10.1590/1414-431X20176161
Dong, X. Z., Wang, D. X., Yu, B. Y., Liu, P., and Hu, Y. (2016). Kai-Xin-San, a traditional Chinese medicine formulation, exerts antidepressive and neuroprotective effects by promoting pCREB upstream pathways. Exp. Ther. Med. 12, 3308–3314. doi: 10.3892/etm.2016.3773
Dubovsky, S. L., Ghosh, B. M., Serotte, J. C., and Cranwell, V. (2021). Psychotic Depression: Diagnosis, Differential Diagnosis, and Treatment. Psychother. Psychosom. 90, 160–177. doi: 10.1159/000511348
Fu, H., Xu, Z., Zhang, X. L., and Zheng, G. Q. (2019). Kaixinsan, a Well-Known Chinese Herbal Prescription, for Alzheimer’s Disease and Depression: A Preclinical Systematic Review. Front. Neurosci. 13:1421. doi: 10.3389/fnins.2019.01421
Hsu, M. C., Tung, C. Y., and Chen, H. E. (2018). Omega-3 polyunsaturated fatty acid supplementation in prevention and treatment of maternal depression: Putative mechanism and recommendation. J. Affect. Disord. 238, 47–61. doi: 10.1016/j.jad.2018.05.018
Hu, Y., Chen, C., Wang, Y., Yang, W., Wang, Y., Zhu, W., et al. (2021a). The effects of KaiXinSan on depression and its association with lipid profiles: A randomized, double-blinded, placebo-controlled trial. Phytomedicine 83:153467. doi: 10.1016/j.phymed.2021.153467
Hu, Y., Wang, Y., Chen, C., Yang, W., Zhu, W., Wang, Y., et al. (2021b). A randomized, placebo-controlled, double-blind study on the effects of SZL on patients with mild to moderate depressive disorder with comparison to fluoxetine. J. Ethnopharmacol. 281:114549. doi: 10.1016/j.jep.2021.114549
Hui, N., Morris, M. J., Allison, M. A., Tsai, M. Y., Rye, K. A., Tabet, F., et al. (2021). Lipoprotein (a) and the risk of elevated depressive symptoms: The Multi-Ethnic Study of Atherosclerosis. J. Psychiatr. Res. 133, 119–124. doi: 10.1016/j.jpsychires.2020.12.022
Jiang, N., Wang, H., Li, C., Zeng, G., Lv, J., Wang, Q., et al. (2021). The antidepressant-like effects of the water extract of Panax ginseng and Polygala tenuifolia are mediated via the BDNF-TrkB signaling pathway and neurogenesis in the hippocampus. J. Ethnopharmacol. 267:113625. doi: 10.1016/j.jep.2020.113625
Karadag, H., Saygili, G., Yuksel, R., Usta, M. B., Topcuoglu, C., and Erzin, G. (2021). Serum TNF- Related Weak Inducer of Apoptosis (TWEAK), TNF- Related Apoptosis-Inducing Ligand (TRAIL) Levels in Patients with Bipolar Depression, Major Depression and a Healthy Control Group. Psychiatr. Danub. 33, 314–319. doi: 10.24869/psyd.2021.314
Leonard, B. E. (2018). Inflammation and depression: A causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 30, 1–16. doi: 10.1017/neu.2016.69
Linnemann, C., and Lang, U. E. (2020). Pathways Connecting Late-Life Depression and Dementia. Front. Pharmacol. 11:279. doi: 10.3389/fphar.2020.00279
Liu, W., Xue, X., Xia, J., Liu, J., and Qi, Z. (2018). Swimming exercise reverses CUMS-induced changes in depression-like behaviors and hippocampal plasticity-related proteins. J. Affect. Disord. 227, 126–135. doi: 10.1016/j.jad.2017.10.019
Machado-Vieira, R., Zanetti, M. V., Teixeira, A. L., Uno, M., Valiengo, L. L., Soeiro-de-Souza, M. G., et al. (2015). Decreased AKT1/mTOR pathway mRNA expression in short-term bipolar disorder. Eur. Neuropsychopharmacol. 25, 468–473. doi: 10.1016/j.euroneuro.2015.02.002
Malhi, G. S., and Mann, J. J. (2018). Depression. Lancet 392, 2299–2312. doi: 10.1016/s0140-6736(18)31948-2
Millischer, V., Matheson, G. J., Martinsson, L., Romer Ek, I., Schalling, M., Lavebratt, C., et al. (2020). AKT1 and genetic vulnerability to bipolar disorder. Psychiatry Res. 284:112677. doi: 10.1016/j.psychres.2019.112677
Musashe, D. T., Purice, M. D., Speese, S. D., Doherty, J., and Logan, M. A. (2016). Insulin-like Signaling Promotes Glial Phagocytic Clearance of Degenerating Axons through Regulation of Draper. Cell Rep. 16, 1838–1850. doi: 10.1016/j.celrep.2016.07.022
Pan, K.-Y., Kok, A. A. L., Eikelenboom, M., Horsfall, M., Jörg, F., Luteijn, R. A., et al. (2021). The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 8, 121–129. doi: 10.1016/s2215-0366(20)30491-0
Pang, X.-C., Kang, D., Fang, J.-S., Zhao, Y., Xu, L.-J., Lian, W.-W., et al. (2018). Network pharmacology-based analysis of Chinese herbal Naodesheng formula for application to Alzheimer’s disease. Chin. J. Nat. Med. 16, 53–62. doi: 10.1016/s1875-5364(18)30029-3
Qu, S., Liu, M., Cao, C., Wei, C., Meng, X. E., Lou, Q., et al. (2021). Chinese Medicine Formula Kai-Xin-San Ameliorates Neuronal Inflammation of CUMS-Induced Depression-like Mice and Reduces the Expressions of Inflammatory Factors via Inhibiting TLR4/IKK/NF-kappaB Pathways on BV2 Cells. Front. Pharmacol. 12:626949. doi: 10.3389/fphar.2021.626949
Read, J. R., Sharpe, L., Modini, M., and Dear, B. F. (2017). Multimorbidity and depression: A systematic review and meta-analysis. J. Affect. Disord. 221, 36–46. doi: 10.1016/j.jad.2017.06.009
Reynolds, C. F. III, Lenze, E., and Mulsant, B. H. (2019). Assessment and treatment of major depression in older adults. Handb. Clin. Neurol. 167, 429–435. doi: 10.1016/B978-0-12-804766-8.00023-6
Ribeiro, A., Ribeiro, J. P., and von Doellinger, O. (2018). Depression and psychodynamic psychotherapy. Braz. J. Psychiatry 40, 105–109. doi: 10.1590/1516-4446-2016-2107
Schmidt, F. M., Koch, J., Nowak, C., Holdt, L. M., Teupser, D., Hegerl, U., et al. (2019). Ligands and receptors of the TNF superfamily are decreased in major depression and during early antidepressant therapy. J. Psychiatr. Res. 119, 116–121. doi: 10.1016/j.jpsychires.2019.09.010
Shen, Y., Zhang, B., Pang, X., Yang, R., Chen, M., Zhao, J., et al. (2020). Network Pharmacology-Based Analysis of Xiao-Xu-Ming Decoction on the Treatment of Alzheimer’s Disease. Front. Pharmacol. 11:595254. doi: 10.3389/fphar.2020.595254
Shu, X., Sun, Y., Sun, X., Zhou, Y., Bian, Y., Shu, Z., et al. (2019). The effect of fluoxetine on astrocyte autophagy flux and injured mitochondria clearance in a mouse model of depression. Cell Death Dis. 10:577. doi: 10.1038/s41419-019-1813-9
Tsai, C. W., Tsai, C. F., Lin, K. H., Chen, W. J., Lin, M. S., Hsieh, C. C., et al. (2020). An investigation of the correlation between the S-glutathionylated GAPDH levels in blood and Alzheimer’s disease progression. PLoS One 15:e0233289. doi: 10.1371/journal.pone.0233289
Walker, E. R., McGee, R. E., and Druss, B. G. (2015). Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 72, 334–341. doi: 10.1001/jamapsychiatry.2014.2502
Willner, P., Scheel-Kruger, J., and Belzung, C. (2014). Resistance to antidepressant drugs: The case for a more predisposition-based and less hippocampocentric research paradigm. Behav. Pharmacol. 25, 352–371. doi: 10.1097/FBP.0000000000000066
Xu, Y. M., Wang, X. C., Xu, T. T., Li, H. Y., Hei, S. Y., Luo, N. C., et al. (2019). Kai Xin San ameliorates scopolamine-induced cognitive dysfunction. Neural Regen. Res. 14, 794–804. doi: 10.4103/1673-5374.249227
Yang, L. F., Zhao, Y. H., Wang, Y. C., Liu, L., Zhang, X. Y., Li, B. J., et al. (2015). The Effects of Psychological Stress on Depression. Curr. Neuropharmacol. 13, 494–504. doi: 10.2174/1570159x1304150831150507
Yi, P., Zhang, Z., Huang, S., Huang, J., Peng, W., and Yang, J. (2020). Integrated meta-analysis, network pharmacology, and molecular docking to investigate the efficacy and potential pharmacological mechanism of Kai-Xin-San on Alzheimer’s disease. Pharm. Biol. 58, 932–943. doi: 10.1080/13880209.2020.1817103
Yu, S., Liu, S., Wang, N., Yu, D., Qin, M., Wu, J., et al. (2021). Novel insights into antidepressant mechanism of Kai Xin San formula: Inhibiting NLRP3 inflammasome activation by promoting autophagy. Phytomedicine 93:153792. doi: 10.1016/j.phymed.2021.153792
Zhang, A., Sun, H., Qiu, S., and Wang, X. (2013). Advancing drug discovery and development from active constituents of yinchenhao tang, a famous traditional chinese medicine formula. Evid Based Complement. Alternat. Med. 2013:257909. doi: 10.1155/2013/257909
Zhou, X., Teng, T., Zhang, Y., Del Giovane, C., Furukawa, T. A., Weisz, J. R., et al. (2020). Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: A systematic review and network meta-analysis. Lancet Psychiatry 7, 581–601. doi: 10.1016/s2215-0366(20)30137-1
Zhou, X. J., Liu, M., Yan, J. J., Cao, Y., and Liu, P. (2012). Antidepressant-like effect of the extracted of Kai Xin San, a traditional Chinese herbal prescription, is explained by modulation of the central monoaminergic neurotransmitter system in mouse. J. Ethnopharmacol. 139, 422–428. doi: 10.1016/j.jep.2011.11.027
Zhu, K. Y., Mao, Q. Q., Ip, S. P., Choi, R. C., Dong, T. T., Lau, D. T., et al. (2012). A standardized chinese herbal decoction, kai-xin-san, restores decreased levels of neurotransmitters and neurotrophic factors in the brain of chronic stress-induced depressive rats. Evid Based Complement. Alternat. Med. 2012:149256. doi: 10.1155/2012/149256
Zhu, Y., Duan, X., Cheng, X., Cheng, X., Li, X., Zhang, L., et al. (2016). Kai-Xin-San, a standardized traditional Chinese medicine formula, up-regulates the expressions of synaptic proteins on hippocampus of chronic mild stress induced depressive rats and primary cultured rat hippocampal neuron. J. Ethnopharmacol. 193, 423–432. doi: 10.1016/j.jep.2016.09.037
Keywords: Kaixinsan, depression, traditional Chinese medicine prescription, network pharmacology, efficacy
Citation: Bo M, Zhang H, Xu J, Zhao H, Jia X, Wang G and Lu Z (2022) Systematic review of Kaixinsan in treating depression: Efficacy and pharmacological mechanisms. Front. Behav. Neurosci. 16:1061877. doi: 10.3389/fnbeh.2022.1061877
Received: 05 October 2022; Accepted: 18 November 2022;
Published: 06 December 2022.
Edited by:
Mu Li, Huazhong University of Science and Technology, ChinaReviewed by:
Gaurav Kandoi, Invaio Sciences, United StatesCopyright © 2022 Bo, Zhang, Xu, Zhao, Jia, Wang and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhengyu Lu, bHUuemhlbmd5dUBzaHV0Y20uZWR1LmNu; Guangdong Wang, ZHJnZHdhbmdAc2h1dGNtLmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.