
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Aging Neurosci. , 24 December 2024
Sec. Parkinson’s Disease and Aging-related Movement Disorders
Volume 16 - 2024 | https://doi.org/10.3389/fnagi.2024.1411584
This article is part of the Research Topic Pathophysiology, Treatment and Rehabilitation of Neurodegenerative Diseases in Geriatric Population View all 20 articles
 Xu Bin Guo1
Xu Bin Guo1 Lu Tang1,2,3*
Lu Tang1,2,3*Objective: This study aims to compare the effects of Tai Chi, yoga, and resistance training on balance function in healthy elderly individuals and patients with Parkinson’s disease (PD). Given the well-documented benefits of these three exercise types in enhancing balance and motor function, it is crucial to assess their differential impacts.
Methods: A comprehensive search was conducted across PubMed, Web of Science, Scopus, and Cochrane Library databases through December 2023. Articles were selected based on predefined criteria, screened, and evaluated by two independent researchers who also extracted study characteristics. The risk of bias was assessed using the Cochrane risk of bias tool. The primary outcome measures were the Berg Balance Scale and the Timed Up and Go test, while the secondary measure was the Unified Parkinson’s Disease Rating Scale Part III. A random effects model was employed, and heterogeneity was measured using the I2 statistic.
Results: Of the 21 studies reviewed, 9 focused on healthy older adults and 12 targeted individuals with PD. The meta-analysis showed that Tai Chi, yoga, and resistance training significantly improved balance in patients with PD compared to control groups (p < 0.00001). Resistance training was most effective in enhancing dynamic balance in healthy older adults (p = 0.003), while Tai Chi had the most significant impact on balance improvement in PD patients (p < 0.00001). Notably, interventions conducted three to four times per week, each lasting 50–60 min and continued over 12 weeks, yielded the most substantial balance improvements.
Conclusion: Comparative analyses demonstrate that Tai Chi, yoga, and resistance training significantly enhance balance and motor function. Specifically, resistance training markedly improves dynamic balance in healthy elderly individuals, while Tai Chi shows pronounced improvements in motor function and balance for PD patients. Optimal balance improvements are achieved by performing interventions three to four times per week, with each session lasting 50–60 min, over 12 weeks.
Systematic review registration: https://inplasy.com/, identifier INPLASY202470042.
As the elderly population grows, so does the incidence of Parkinson’s disease (PD), a prevalent neurodegenerative condition affecting over 1% of individuals aged 55 years and above globally (Yin et al., 2023). PD originates from the depletion of dopamine neurons within the substantia nigra. As the disease progresses, its pathology extends to neocortical and cortical areas (Parga et al., 2021), impairing cognitive and behavioral functions. Common symptoms include bradykinesia, muscle rigidity, and rest tremor (Perlmutter and Ushe, 2020), resulting in lower limb motor dysfunction, such as diminished balance, gait, and mobility (Mak and Wong-Yu, 2019). Additionally, nearly all patients experience non-motor symptoms alongside basic functional deficits (Kadastik-Eerme et al., 2015). Reports indicate that approximately 70% of PD patients are prone to falls due to reduced motor function and mobility, which may lead to severe consequences like head trauma and fractures (Bloem et al., 2001; Perez-Lloret et al., 2014). Age-related alterations in brain structure and vestibular function, compounded by PD, also affect cognition, walking, and body balance (Xie et al., 2019).
The gradual loss of dopamine neurons in the brain leads to these symptoms. As the disease progresses, motor function deteriorates and can be categorized into distinct stages: Stage 1: mild symptoms appear, typically affecting only one side of the body. Patients may experience slight tremors or bradykinesia. Stage 2: symptoms become more pronounced, involving both sides of the body, but balance remains relatively stable. Stage 3: symptoms further intensify, leading to noticeable balance issues and an increased risk of falls. Stages 4 and 5: motor function is severely compromised, requiring assistance from others for walking (Xiao and Tan, 2023; Debû et al., 2018). The motor symptoms of PD, along with their impact on balance, are complex and multifaceted. As the disease advances, it significantly affects patients’ daily lives and mental health.
The prevalence of PD is projected to exceed 1 million by 2030 due to an aging population (Marras et al., 2018), highlighting the need to optimize the care and management of PD patients. Currently, two treatment approaches exist for PD: conventional and surgical. Pharmacologic interventions involve dopamine replacement therapy or dopamine agonists, Pharmacological interventions, particularly dopamine replacement therapy and dopamine agonists, are essential in managing PD. The most commonly used medications include: 1. Levodopa: as the most widely prescribed drug for PD, levodopa effectively alleviates symptoms by replenishing dopamine levels in the brain. 2. Dopamine agonists: medications such as bromocriptine and ropinirole directly stimulate dopamine receptors. These drugs can be administered in the early stages of the disease or combined with levodopa to enhance therapeutic outcomes.
In recent years, non-pharmacological treatments have gained increasing recognition as valuable adjuncts to the management of PD. Key non-drug interventions include: Physical therapy: this approach helps improve motor function, increase muscle strength, and reduce the risk of falls. Personalized exercise programs can enhance patients’ coordination and flexibility (Witt et al., 2017; Mantovani et al., 2023). Exercise therapy: regular physical activity can improve motor symptoms and help patients maintain their ability to perform daily activities. Common exercises include gait training, balance exercises, and endurance training, in addition to surgical treatments (Obeso et al., 2010; Micó-Amigo et al., 2017). While these treatments offer partial relief from the motor symptoms of the disease (e.g., tremor, bradykinesia, and rigidity), their prolonged use is associated with side effects such as cardiovascular issues and motor instability. Moreover, patients continue to experience a decline in motor function and mobility (Manson et al., 2012; Ashoori et al., 2015; Kim et al., 2019).
The treatment of PD requires a comprehensive approach that integrates both pharmacological and non-pharmacological interventions. By tailoring treatment plans to the needs of individual patients, it is possible to manage symptoms effectively while also enhancing their quality of life (Illman, 2023). As research progresses, the effectiveness of non-pharmacological interventions is increasingly recognized, providing a broader spectrum of treatment options for patients with PD. Exercise therapy, in particular, has demonstrated significant benefits across multiple domains, including physical health, mental wellbeing, and overall quality of life (Gubert and Hannan, 2021). Physical activity is a crucial non-pharmacological intervention with a wide range of benefits. Specifically, aerobic exercise and strength training have been shown to improve muscle strength and endurance, thereby enabling individuals to perform daily activities more effectively (The Lancet, 2016). Furthermore, exercise can stimulate the production of nerve growth factors, which enhance neural connections.
Physical activity represents a crucial non-pharmacologic intervention, specifically exercise therapy, aimed at ameliorating these symptoms in PD patients. For instance, progressive resistance training (PRT) can engage both the mind and body through physical and respiratory exercises, facilitating improvements in motor function among participants (Yu et al., 2013; Vieira and Cavalcante, 2021). Similarly, Tai Chi has shown positive effects, as reported by Hackney and Earhart (2008) and Bubela et al. (2019). Yoga also contributes to these benefits, with findings from Myers et al. (2020) and Elangovan et al. (2020) supporting its effectiveness including gait, balance, functional ability, and flexibility. Tai Chi (Xiao, 2014; Hosseini et al., 2018) and Iyengar Yoga (Tiedemann et al., 2013; Elangovan et al., 2020) have proven effective in enhancing balance, refining body control, and improving daily life quality and functionality in older adults with PD (Lan et al., 2013). Additionally, these practices have demonstrated modest benefits in mitigating mild brain damage (Betker et al., 2007) and mild cognitive impairment (Hemmeter and Ngamsri, 2022).
Various forms of exercise, including resistance training, Tai Chi (Leitão et al., 2022), skiing (Müller et al., 2011; De Vries et al., 2018), and dance (Santos et al., 2020), exert positive effects on older adults and individuals with PD to varying degrees. Long-term exercise regimens significantly contribute to enhancing balance function across three distinct levels: mechanistic, functional, and behavioral. Mechanistically, several studies have demonstrated that exercise training reduces inflammatory cytokines, boosts anti-inflammatory cytokines, and stimulates the production of BDNF and NAA, thereby fostering neural plasticity and functional connectivity within the brain (Tian et al., 2017; Èekanauskaitë et al., 2020). Additionally, research indicates that exercise interventions lead to improved functional connectivity in the frontal lobe (Liu et al., 2020). Functionally, prolonged Tai Chi practice notably enhances brain network function, proprioception, and balance capabilities, while also augmenting neurotransmitter metabolism and conduction, thereby impacting cognition, motor control, and balance (Li and Harmer, 2015). Additional studies have also shown significant changes in energy conduction and neurotransmitter levels, as well as improved physical functioning in PD patients after exercise intervention (Li et al., 2022).
At the behavioral level, participants’ gait, balance, and mobility were significantly improved compared to the control group, and their quality of life was substantially improved. The same study also found that participants’ balance was significantly improved after training (Zhu et al., 2023). Different types of exercise movements have certain effects on different limb parts. On the one hand, exercise can enhance body posture control, proprioception, and visual function. Movement involves the cerebral cortex and subcortical structures, such as the cerebellum, basal ganglia, and brainstem (Takakusaki, 2017; Chen et al., 2023). On the other hand, the process of body posture control requires the synergistic involvement of multiple brain regions (Stuart et al., 2018). The cerebral cortex can modulate the excitability of subcortical structures, spinal columns, and muscles according to the body’s needs to maintain balance and postural stability (Solis-Escalante et al., 2019). Both of these mechanisms are important for improving balance function. Therefore, three different forms of exercise—Tai Chi, yoga, and resistance exercise—may affect the spinal cord, brain functional connectivity, and cortical structures by influencing body posture and breathing rhythm, among other things, to further improve participants’ mobility and motor symptoms. Therefore, the benefits of exercise for the body are profound and comprehensive.
In recent years, there has been a surge in studies investigating the impact of exercise on balance function among older adults and individuals with PD. Prior research (Xiao, 2014; Winser et al., 2018; Leitão et al., 2022) has indicated that Tai Chi, yoga, and resistance exercise can effectively enhance balance function in older adults. These studies underscore the improvement in motor function and balance across various exercise modalities. However, existing literature predominantly focuses on the effects of singular exercise types, lacking comparative analyses between different modalities. Certain reviews (ALJawaee et al., 2021; Hołaj and Chalimoniuk, 2022; Chen et al., 2023; Yu et al., 2021) concentrate solely on specific exercise forms, such as wobble board training, dance, or Tai Chi, without contrasting differences between various exercise types.
Furthermore, current studies have not elucidated the disparities in balance outcomes between healthy older adults and Parkinson’s patients following exercise interventions. Hence, the objective of this review was to compare the effects of Tai Chi, yoga, and resistance exercise on balance function between healthy older adults and individuals with PD. To achieve this, we conducted a systematic review and meta-analysis of relevant studies that evaluated these exercise modalities. By synthesizing and analyzing the data, we aimed to assess the relative effectiveness of each exercise type in improving balance and preventing falls. This analysis aimed to identify the most suitable exercise modality for enhancing balance and averting falls among healthy older adults.
In this study, the reviewer (XG) conducted searches across PubMed, Web of Science, Scopus, and the Cochrane Library databases using keywords, synonyms, and a search strategy employing Boolean logic operators. The search covered literature from inception to December 2023, including four distinct fields with separate search terms (detailed in Table 1). The first search field focused on participants categorized by targeted population criteria, including terms such as “Older adult,” “Older elderly,” “Older,” “Parkinson Disease,” “Primary parkinsonism,” “Parkinsonism,” and “Idiopathic parkinsonism.” The second search field included potential synonyms for various forms of exercise, such as “Tai Ji” (including “Tai chi,” “Chi,” “Tai,” “Tai Ji Quan,” “Tai Chi Chuan,” “Ji Quan,” and “Tai”), “Yoga,” and “Resistance training” (including “Resistance exercise” and “Strength training”). The third search included synonyms related to the balance function, such as “Balance” and “Balance ability.” The fourth search field concentrated on methods and techniques for assessing balance function [e.g., the Berg Balance Scale (BBS), the Timed Up and Go test, and the Balance Assessment System test], commonly employed to evaluate the body’s balance capability, with the BBS being notably user-friendly and swift.
Building on this, we excluded PRT from our review. Although PRT shows a clear correlation with improvements in balance and motor function, we chose to focus primarily on progressive resistance exercise (PRE), yoga, and Tai Chi. These interventions have demonstrated significant effects in the existing literature and are widely applied in clinical practice. All primary search terms were paired with medical subject headings (MeSH) and thoroughly explored. Furthermore, each reference from the included studies underwent scrutiny to ensure the comprehensive coverage of relevant literature. Figure 1 depicts the PRISMA diagram, outlining the literature search strategy and detailing each stage of the research process.
1. Two reviewers (XG and LT) developed the following inclusion and exclusion criteria.
2. The study population comprised healthy older adults aged 50 years and older, as well as patients with mild to moderate PD.
3. In the experimental group, the intervention consisted of various types of exercise interventions or a single type of Tai Chi, resistance training, or yoga. The control group received no exercise intervention, or alternative forms of movement and exercise were utilized.
4. The study incorporated at least one or more of the following assessments: the BBS, Timed Up and Go (TUG) test, movement speed, force plate measurements, and functional balance test.
5. The aim was to investigate the effects of different exercise types (Tai Chi, yoga, and resistance training) on balance function in both healthy older adults and Parkinson’s patients.
6. The outcome indicators were complete and available in full text, and only randomized controlled trials (RCTs) published in the English language were included.
7. Two reviewers, XG and LT, independently assessed the studies based on the above inclusion/exclusion criteria. Initial screening of article titles and abstracts was conducted using NoteExpress 3.9.0.9640 software, with duplicate entries removed. Subsequently, a third reviewer (XYZ) was invited to collaborate in the evaluation of included and uncertain studies.
Two researchers (XG and LT) independently evaluated the risk of bias and study quality using the Cochrane ROB 2.0 risk of bias tool. As depicted in Figure 2. Parameters assessed encompassed random sequence generation (for randomized grouping), allocation concealment (ensuring confidentiality of randomization sequences), double blinding (for participant and researcher blinding), data completeness (addressing missing data issues), and selective reporting (reporting results comprehensively and avoiding the use of multiple evaluation criteria). Any disagreements or discrepancies were resolved through consultation with a third researcher (XYZ).
Two researchers (XG and LT) independently extracted and synthesized information from articles and data, ensuring objectivity and minimizing bias. A data extraction table was then created, which followed the systematic review of characteristics of similar research topics. The extracted information encompassed the first author’s name, average age, year of publication, intervention program details (method, duration, and frequency), testing method, and main conclusions. The synthesized information is presented in Table 2.
We used Comprehensive Meta-Analysis software, RevMan 5.4.1, to analyze key outcomes. The balance function (BBS) was the primary outcome, while motor functions [TUG and Unified Parkinson’s Disease Rating Scale Part III (UPDRS-III)] were secondary outcomes. Given the high variability of UPDRS-III scores between studies, we used the standardized mean difference (SMD) for the combined analysis. For the analysis of TUG and BBS results, the mean difference (MD) was used, and statistical analyses were conducted using weighted average differences within a 95% confidence interval. In cases of significant heterogeneity among the studies (p < 0.05, I2 > 50%), sensitivity analyses and subgroup analyses were conducted to ensure the robustness of the results and identify the sources of heterogeneity.
An initial search across four databases (PubMed, Web of Science, Scopus, and Cochrane Library) based on the search strategy and keywords yielded a total of 5,994 potentially relevant articles. We utilized a different screening process consisting of (removal of duplicates, initial review, systematic evaluation, title screening, and abstract reading). Please refer to Figure 1 for a detailed outline of the process we employed, 21 articles were identified that met the criteria. These comprised 9 studies involving the healthy elderly population and 12 studies involving patients with PD. Among the healthy elderly population, there were four studies on Tai Chi (Penn et al., 2019; Hosseini et al., 2018; Bubela et al., 2019; Xiao, 2014), three studies on resistance training (Leitão et al., 2022; Sañudo et al., 2019; Yu et al., 2013), and two studies on yoga (Patel et al., 2019; Nick et al., 2016). In contrast, within the PD patient population, there were 10 studies on Tai Chi (Li et al., 2022; Gao et al., 2014; Li et al., 2012; Hackney and Earhart, 2008; Choi et al., 2013; Amano et al., 2013; Vergara-Diaz et al., 2018; Huang et al., 2015; Li et al., 2017; Xiao et al., 2021), 1 studies on yoga (Elangovan et al., 2020), and 1 study focused solely on resistance training (Corcos et al., 2013). Notably, the study by (Li et al., 2012) analyzed Tai Chi and resistance training in comparison.
Table 2 presents the main characteristics of the studies, screened using the Hoehn and Yahr scales (Hoehn and Yahr, 2001). A total of 21 studies were included. In the studies involving healthy older adults, interventions using Tai Chi ranged from 2 to 3 times per week for 30–120 min per session over 8 weeks to 12 months, while resistance strength training sessions occurred 2–3 times per week for 60 min each, spanning 5–16 weeks. Yoga training sessions varied from 30 to 60 min, occurring 2–5 times per week, lasting from 4 to 8 weeks. For Parkinson’s patients, Tai Chi interventions lasted 60 min, 2–4 times per week, lasting from 8 weeks to 12 months; yoga interventions involved sessions lasting 60 min, twice weekly for 12 weeks, and resistance training sessions lasted 60 min, twice weekly, lasting for 24 weeks.
Among the 21 studies, 10 utilized the BBS as their outcome measure, reflecting balance function (Leitão et al., 2022; Yu et al., 2013; Nick et al., 2016; Penn et al., 2019; Gao et al., 2014; Hackney and Earhart, 2008; Li et al., 2022; Li et al., 2017; Xiao et al., 2021; Huang et al., 2015), including 6 involving Parkinson’s patients (Li et al., 2022; Hackney and Earhart, 2008; Gao et al., 2014; Li et al., 2017; Xiao et al., 2021; Huang et al., 2015). Twelve studies employed the TUG test (Sañudo et al., 2019; Yu et al., 2013; Patel et al., 2019; Bubela et al., 2019; Xiao, 2014; Hosseini et al., 2018; Penn et al., 2019; Li et al., 2022; Gao et al., 2014; Hackney and Earhart, 2008; Li et al., 2012; Vergara-Diaz et al., 2018), with five including Parkinson’s patients (Li et al., 2022; Gao et al., 2014; Li et al., 2012; Hackney and Earhart, 2008; Vergara-Diaz et al., 2018). Furthermore, outcome indicators for both healthy older adults and Parkinson’s patients included the UPDRS, Modified Falls Efficacy Scale (MFES), Fifty-Foot Walk Test (FFWT), and Activities-Specific Balance Confidence (ABC). Researchers primarily utilized UPDRS-III, BBS, TUG to assess participants’ balance and locomotor ability, with UPDRS-III being the predominant method in clinical and research settings (Siderowf et al., 2002).
Two researchers (XG and LT) performed a literature quality assessment using the Cochrane ROB 2.0 risk of bias tool. The details of each assessment are illustrated in Figure 2. Among the 21 studies reviewed, those exhibiting a higher risk primarily stemmed from the necessity to recruit and group participants from specific sports areas, as evidenced by studies conducted by Yu et al. (2013), Leitão et al. (2022), Bubela et al. (2019), and Patel et al. (2019). Additionally, the implementation of various sports interventions inherently led to participant awareness of intervention content, contributing to some level of risk. However, studies with comparatively lower impact on outcomes were conducted by Nick et al. (2016), Elangovan et al. (2020), Corcos et al. (2013), Sañudo et al. (2019), Xiao (2014), Penn et al. (2019), as well as by Hackney and Earhart (2008), Hosseini et al. (2018), Li et al. (2012), Huang et al. (2015), Li et al. (2017), Xiao et al. (2021), and Vergara-Diaz et al. (2018).
Four studies with healthy elderly participants used the BBS to evaluate the effects of exercise on balance (Leitão et al., 2022; Yu et al., 2013; Nick et al., 2016; Penn et al., 2019). Despite the significant heterogeneity, the analysis indicated no significant differences in static balance between the intervention and control groups (MD = 3.35; 95% CI = 0.62, 7.31; p = 0.10; I2 = 92%; Figure 3). Removing the (Nick et al., 2016; Leitão et al., 2022), study from a sensitivity analysis eliminated heterogeneity (I2 = 0%) and provided consistent results (MD = 0.30; 95% CI = 1.52, 0.93; p = 0.64; I2 = 0%; Figure 3).
Seven studies utilized the TUG test to evaluate functional walking in older adults (Sañudo et al., 2019; Yu et al., 2013; Patel et al., 2019; Bubela et al., 2019; Xiao, 2014; Hosseini et al., 2018; Penn et al., 2019). A high degree of heterogeneity was identified, with an I2 value of 84%. Upon investigation, studies by Xiao (2014) and Hosseini (2018) were identified as sources of heterogeneity. Excluding these studies significantly decreased the heterogeneity to I2 = 0%. Compared to the control group, the three types of exercise significantly improved functional walking (MD = 0.89; 95% CI = 1.30, 0.48; p < 0.0001; I2 = 0%; Figure 4). Further subgroup analysis revealed statistically significant differences in TUG test scores across different exercise interventions. Resistance training showed a more favorable effect than the control group (MD = 0.92; 95% CI = 1.53, 0.30; p = 0.003). However, yoga and Tai Chi did not show statistically significant differences in TUG test scores compared to the control group (yoga: MD = 1.03; 95% CI = 2.26, 0.20; p = 0.10) and (Tai Chi: MD = 0.99; 95% CI = 3.66, 1.69; p = 0.47; Figure 4).
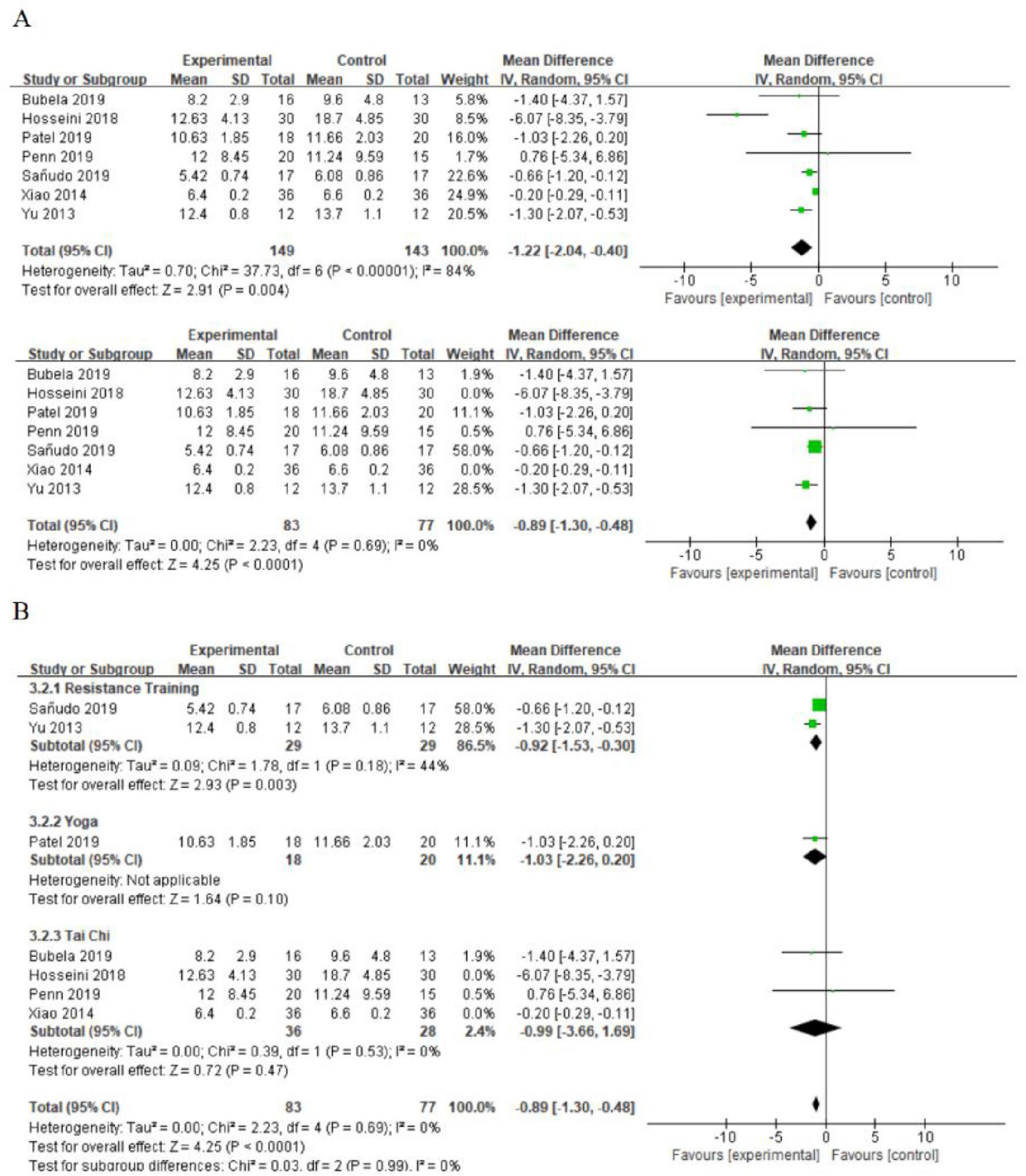
Figure 4. (A) The effect of exercise on functional walking. (B) The effect of different types of exercise on functional walking (subgroup analysis).
In summary, although all three types of exercise interventions significantly improved balance function in older adults, the BBS balance scale showed no significant changes in healthy older adults. Meta-analysis using the TUG measure revealed significant improvements in balance, with resistance training being particularly effective.
In the PD group, 10 studies utilized the UPDRS-III to assess motor function (Corcos et al., 2013; Elangovan et al., 2020; Li et al., 2012; Gao et al., 2014; Hackney and Earhart, 2008; Li et al., 2022; Choi et al., 2013; Amano et al., 2013; Vergara-Diaz et al., 2018; Huang et al., 2015). Results indicated that all three types of exercise improved functional walking compared to the control group (SMD = 0.40; 95% CI = 0.62, 0.18; p = 0.0003; I2 = 14%; Figure 5). Given the different exercise interventions, we conducted subgroup analyses. The meta-analysis revealed varying effectiveness among the exercise types in improving functional walking. Resistance training (SMD = 0.69; 95% CI = 1.35, 0.04; p = 0.04) and Tai Chi (SMD = 0.35; 95% CI = 0.60, 0.09; p = 0.007) had positive effects. However, yoga did not show a statistically significant difference from the control group (SMD = 0.74; 95% CI = 1.71, 0.22; p = 0.13; Figure 5).
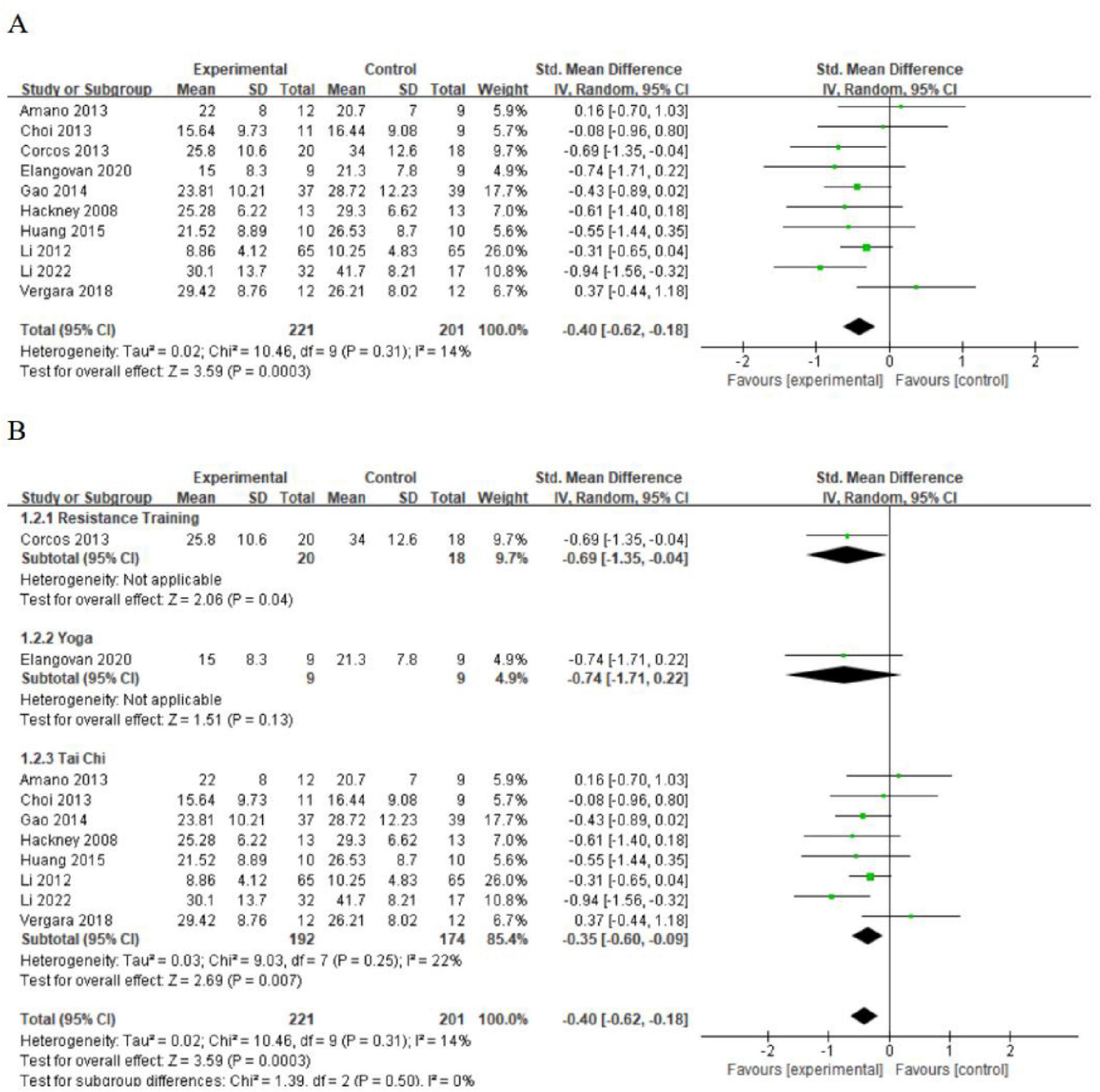
Figure 5. (A) The effect of exercise on motor function. (B) The effect of different types of exercise on motor function (subgroup analysis).
Six studies have employed the BBS to assess balance function in patients with PD (Gao et al., 2014; Li et al., 2022; Hackney and Earhart, 2008; Li et al., 2017; Xiao et al., 2021; Huang et al., 2015). A meta-analysis revealed significant heterogeneity (I2 = 47%) and showed that Tai Chi significantly improved balance function in PD patients compared to the control group (MD = 3.56; 95% CI = 2.24, 4.87; p < 0.00001; Figure 6). Sensitivity analysis, excluding the study by Xiao (2021), resulted in reduced heterogeneity (I2 = 0%) while maintaining the same results (MD = 2.90; 95% CI = 1.76, 4.05; p < 0.00001; Figure 6).
We conducted further subgroup analysis to assess the effects of Tai Chi intervention duration and frequency on balance function in PD patients. The results indicated no significant differences among various intervention durations (MD = 0.79; 95% CI = 0.53, 1.04; p = 0.32, I2 = 0%; Figure 7). Analysis of intervention dosage and exercise frequency showed that engaging in Tai Chi four times per week was most effective (MD = 4.66; 95% CI = 3.54, 5.77; p < 0.00001, I2 = 0%; Figure 8). Conversely, interventions conducted twice and three times per week had p values of 0.02 and 0.006.
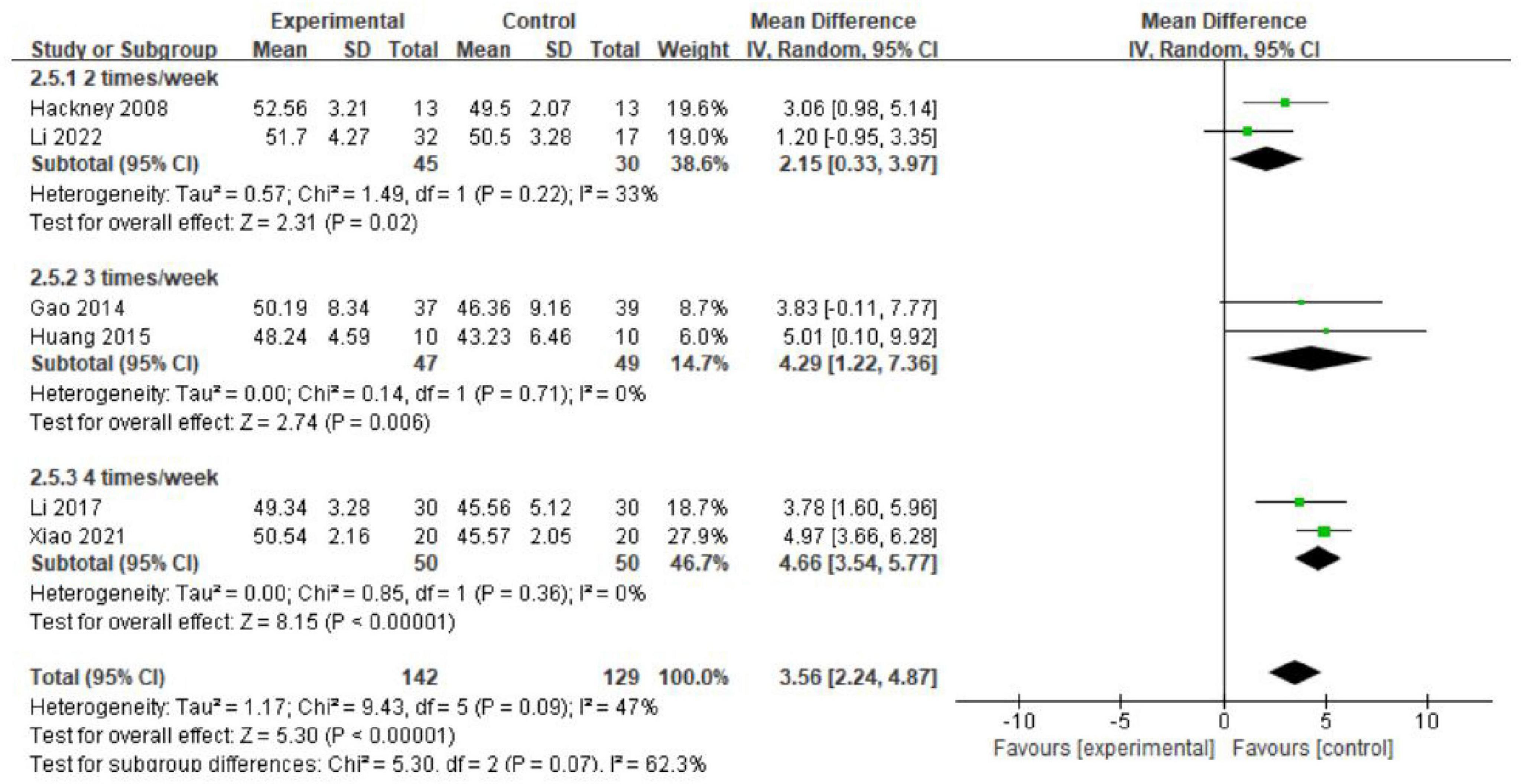
Figure 8. The effects of different intervention frequencies on balance function (subgroup analysis).
In the group of patients with PD, five studies used the TUG test to assess patients’ functional walking (Li et al., 2022; Gao et al., 2014; Hackney and Earhart, 2008; Li et al., 2012; Vergara-Diaz et al., 2018). Compared to the control group, Tai Chi exercises improved functional walking (MD = 0.74; 95% CI = 1.37, 0.11; p = 0.02; I2 = 46%; Figure 9). Sensitivity analysis showed that heterogeneity would significantly decrease only by excluding the study by Gao (2014), but the results remained unchanged (MD = 0.57; 95% CI = 1.01, 0.13; p = 0.01; I2 = 0%). This finding indicates that the study by Gao (2014), was a major contributor to the high heterogeneity.
Overall, these 12 studies evaluated the effects of three types of exercise interventions on patients with PD. First, a meta-analysis assessing balance using the TUG test demonstrated significant improvement in the Tai Chi intervention group compared to the control group. Subgroup analysis by intervention frequency indicated that this improvement did not increase significantly over time. Additionally, a subgroup analysis of the UPDRS-III showed that Tai Chi and resistance training significantly enhanced motor function.
This systematic review and meta-analysis indicate that all three types of exercise interventions can significantly enhance balance and motor functions in older adults. In healthy older adults, resistance training shows the most substantial effect in improving dynamic balance. For PD patients, both resistance training and Tai Chi significantly enhance motor function and balance. Continuous Tai Chi intervention significantly improves the balance of PD patients. The effects become increasingly significant with higher intervention frequency (p < 0.00001). While there is no significant change in effect over time (p = 0.32), interventions conducted 3–4 times per week, for 50–60 min each session, over 12 weeks, yield the most significant improvements in balance. Furthermore, as illustrated in Figure 10, our review synthesized these exercise interventions’ behavioral, functional, and mechanical benefits for healthy older adults and PD patients.
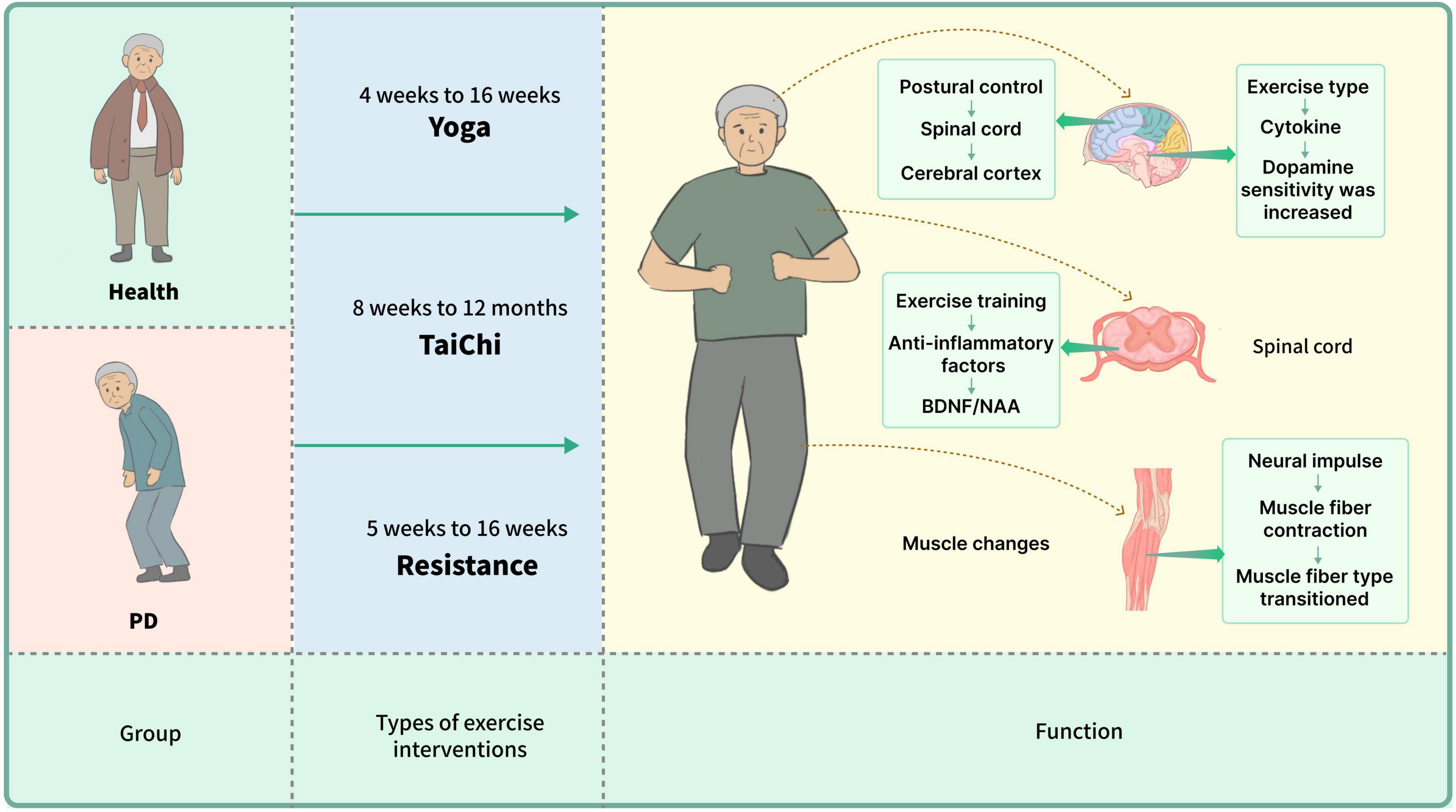
Figure 10. The balance function of healthy elderly individuals and patients with Parkinson’s disease significantly improved after sustained yoga practice for 4–16 weeks, Tai Chi practice for 8–12 months, or resistance training for 5–16 weeks. During these training processes, changes in body posture positively impacted the spinal cord and cerebral cortex; exercise training led to an increase in anti-inflammatory factors, which further influenced the increase in BDNF/NAA and other cytokines, thereby enhancing dopamine plasticity. Long-term practice also resulted in a transformation of muscle fiber contraction types.
In nine studies with healthy older adults, Tai Chi, yoga, and resistance exercise significantly improved gait, flexibility, stability, and tissue-level functioning. Improvements in dopamine levels were also noted.
The BBS, TUG test, and gait measures are commonly used to evaluate balance in Tai Chi studies. These tools have shown significant improvements in lower limb muscles, flexibility, and functional tasks, indicating that Tai Chi may slow motor function decline. These studies provide strong evidence to address key concerns (Hosseini et al., 2018). Tai Chi improves proprioception in the trunk and lower limbs and enhances balance by integrating vestibular and visual inputs (Bubela et al., 2019; Xiao, 2014). Personalized Tai Chi interventions have shown the highest efficacy (Penn et al., 2019). In the yoga intervention group, two studies found that practitioners performed rhythmic stretches with breath control, joint mobilization, and muscle strengthening. Yoga techniques, including posture adjustments and breathing exercises, effectively enhance strength, flexibility, and balance by improving posture control and proprioception (Patel et al., 2019; Nick et al., 2016). Strength training studies assessed overload progression by evaluating maximal repetitions of static balancing and swaying amplitude. Two studies highlighted that different resistance programs varied in effectiveness, with strength training particularly improving daily mobility and quality of life. Leitão et al. (2022) and Yu et al. (2013) found that resistance exercises improved balance, quality of life, and mobility in older adults. Sañudo et al. (2019) also reported improvements in gait, mobility, and static balance, suggesting that resistance training enhances balance, mobility, and muscle strength.
Twelve studies on Parkinson’s patients explored Tai Chi, yoga, and resistance exercise. These interventions showed improvements in behavioral symptoms (e.g., dystonia and motor difficulties), motor functions (e.g., gait and balance), and overall quality of life.
Two studies on Tai Chi showed initial effects were minor, but notable improvements in bradykinesia, muscle tone, posture, and functional activity were observed later, indicating that extended practice may be necessary for significant benefits (Vergara-Diaz et al., 2018; Choi et al., 2013). Li et al. (2012) found Tai Chi outperformed stretching and resistance training in stride length and functional stretching. (Gao et al., 2014) also showed Tai Chi improved gait, postural regulation, body strength, and posture compared to controls. This improvement was linked to Tai Chi’s combination of fluidity and stillness, which enhanced body strength and range of motion (Hackney and Earhart, 2008). Enhanced balance, visual network function, and metrics such as the BBS and reduced interleukin-1 beta levels were observed (Huang et al., 2015; Li et al., 2017). Improvements in UPDRS scores were also related to better visual network function. Tai Chi training significantly improved metabolic pathways, including arginine biosynthesis, the urea cycle, the tricarboxylic acid cycle, and β-oxidation of ultra-long-chain fatty acids (Li et al., 2022). Intensive resistance training significantly improved strength, motor agility, physical function, and quality of life in Parkinson’s patients. Well-structured long-term exercise programs have demonstrated substantial benefits for motor function (Corcos et al., 2013). Yoga interventions, evaluated for gait, postural fluency, UPDRS, cadence, walking speed, and turnaround time, showed improvements in static balance but minimal changes in gait (Elangovan et al., 2020). Corcos et al. (2013) found prolonged exercise effective in reducing Parkinson’s symptoms, while Elangovan et al. (2020) reported that Hatha yoga improved static balance but had little effect on gait. The variability in results across studies, including inconsistent changes in gait (Myers et al., 2020; Patel et al., 2019; Nick et al., 2016; Bartos et al., 2022), maybe due to differences in assessment methods and intervention protocols. Differences in study design, such as intervention duration and frequency, contribute to these discrepancies. Myers et al. (2020) focused on PD patients, whereas other studies targeted general older adults. For instance, Bartos et al. (2022) used a 16-week program with bi-weekly sessions, Patel et al. (2019) a 4-week program with five sessions per week, and Elangovan et al. (2020) a 12-week program with bi-weekly sessions. These variations likely account for the observed differences in outcomes.
Completion rates varied across studies, as shown in Table 2. Most interventions were conducted 2–3 times per week, with durations ranging from a few weeks to 24 months; longer interventions may yield more pronounced effects. Sessions typically lasted around 60 min, though some varied between 30 and 90 min, potentially affecting participant tolerance and outcomes. High completion rates, such as 100% in studies by Sañudo et al. (2019), Yu et al. (2013), and Li et al. (2022), indicate strong participant acceptance and adherence. Conversely, lower completion rates were observed in studies like Leitão et al. (2022), which involved resistance training for healthy older adults (60 min/session, 2 times per week for 16 weeks; 1 of 20 participants dropped out), and Vieira and Cavalcante (2021), which examined Tai Chi for Parkinson’s patients (60 min/session, 2 times per week for 24 weeks; only 12 of 16 participants completed the intervention after 6 months). These lower rates may reflect challenges in intervention implementation or issues with long-term adherence.
It is important to note that the extensive research on Tai Chi and yoga may overshadow the potential benefits of resistance training in improving balance functions. While existing studies suggest that resistance training might have unique effects on PD patients, the limited literature prevents a comprehensive assessment. This imbalance in available research could introduce bias when comparing the overall effects of different physical activities—such as Tai Chi, yoga, and resistance training—on balance function, potentially leading to an overemphasis or underestimation of the effectiveness of Tai Chi or yoga interventions.
Our investigation shows that self-posture changes during movement are primarily controlled by the spinal cord, improving balance post-training (Taube et al., 2007). This regulation involves the cerebral cortex, cerebellum, and brainstem (Takakusaki, 2017; Richer and Lajoie, 2020). Exercise enhances cognitive functions by reducing inflammation, increasing anti-inflammatory cytokines, and boosting BDNF and NAA production, which improve neural plasticity (Tian et al., 2017; Èekanauskaitë et al., 2020). Zhu et al. (2023) linked improved balance to increased vestibular nucleus functionality. PD patients show deviations in the default mode network (DMN) affecting memory regions (Pedersini et al., 2020). Conflicting sensory inputs can impact gait and balance, potentially enhancing overall stability.
Studies by Jarvis (2017), Assländer et al. (2015), and Rogge et al. (2018) indicate that movement increases dopamine and serotonin transporters, altering brain chemistry. Tai Chi training improves brain network function, and neurotransmitter metabolism, and reduces dopaminergic degeneration in PD patients (Su et al., 2018). Additionally, Tai Chi, yoga, and resistance exercises enhance postural control and proprioceptive and visual systems, providing relief from neurodegenerative disorders (Xu, 2004; Peterka, 2002; Koelewijn and Ijspeert, 2020).
Based on this systematic review, Tai Chi, yoga, and resistance exercises have positively impacted balance, visuospatial skills, gait, and stride in both healthy older adults and PD patients.
Despite evidence suggesting that exercise improves motor function and benefits balance, cognitive function, gait, posture control, proprioception, and neurotransmitter metabolism in both patients and healthy individuals, the exact mechanisms remain unclear. Increased brain connectivity is a key theoretical basis for these benefits, but this is supported mainly by indirect evidence. Our review of 21 studies on exercise interventions for balance shows that while Tai Chi, yoga, and resistance exercises can alleviate PD symptoms and enhance motor performance, the generalizability of these findings is limited. Variability in study content, such as differing assessment tools and methods, and the fact that only 12 studies involved PD patients, restrict our comprehensive understanding. Additionally, diverse intervention plans with varying frequency, intensity, duration, and types further complicate the identification of the most effective exercise regimens.
Future research should focus on several key areas to enhance our understanding of exercise interventions. First, standardizing exercise protocols, including frequency, intensity, duration, and type, is crucial for ensuring consistent and comparable assessments across studies. Second, it is important to investigate the underlying mechanisms of exercise benefits using advanced neuroimaging and biomarker analyses to gain clearer insights into the biological effects. Third, accounting for individual variability in physical activities can help tailor intervention strategies to different populations. Finally, addressing knowledge gaps by exploring under-researched areas, such as PRT for PD patients, will contribute to a more comprehensive understanding of exercise effects.
This systematic review and meta-analysis indicate that Tai Chi, yoga, and resistance training significantly enhance brain network function in both healthy older adults and patients with PD. These exercises improve connectivity in subcortical structures, thus enhancing balance and motor function. The study identified resistance training as having the most significant effect on improving balance in healthy older adults, while Tai Chi proved particularly effective for Parkinson’s patients. It is recommended that these exercises be practiced for 50–60 min, three to four times a week, and continued for at least 12 weeks to achieve optimal results.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
XG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LT: Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Fundamental Research Funds for the Central University (PHD2023-02), Aviation Sports Research Institute project of 24CAFUC09034, Sichuan Philosophy and Social Sciences 2022 Planning Project (SC22B001).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ALJawaee, M. A., Jones, M. D., Theobald, P. S., and Williams, J. M. (2021). Does wobble board training improve balance in older adults? A systematic review. Phys. Ther. Rev. 26, 447–456. doi: 10.1080/10833196.2021.1987042
Amano, S., Nocera, J. R., Vallabhajosula, S., Juncos, J. L., Gregor, R. J., Waddell, D. E., et al. (2013). The effect of Tai Chi exercise on gait initiation and gait performance in persons with Parkinson’s disease. Parkins. Relat. Disord. 19, 955–960. doi: 10.1016/j.parkreldis.2013.06.007
Ashoori, A., Eagleman, D. M., and Jankovic, J. (2015). Effects of auditory rhythm and music on gait disturbances in Parkinson’s disease. Front. Neurol. 6:234. doi: 10.3389/fneur.2015.00234
Assländer, L., Hettich, G., and Mergner, T. (2015). Visual contribution to human standing balance during support surface tilts. Hum. Mov. Sci. 41, 147–164. doi: 10.1016/j.humov.2015.02.010
Bartos, L. J., Meek, G. A., and Berger, B. G. (2022). Effectiveness of yoga versus exercise for reducing falling risk in older adults: physical and psychological indices. Percept. Motor Skills 129, 1245–1269. doi: 10.1177/00315125221100820
Betker, A. L., Desai, A., Nett, C., Kapadia, N., and Szturm, T. (2007). Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuries. Phys. Ther. 87, 1389–1398. doi: 10.2522/ptj.20060229
Bloem, B. R., Grimbergen, Y. A. M., Cramer, M., Willemsen, M., and Zwinderman, A. H. (2001). Prospective assessment of falls in Parkinson’s disease. J. Neurol. 248, 950–958. doi: 10.1007/s004150170047
Bubela, D., Sacharko, L., Chan, J., and Brady, M. (2019). Balance and functional outcomes for older community-dwelling adults who practice Tai Chi and those who do not: a comparative study. J. Geriatr. Phys. Ther. 42, 209–215. doi: 10.1519/JPT.0000000000000153
Èekanauskaitë, A., Skurvydas, A., Žlibinaitë, L., Mickevièienë, D., Kilikevièienë, S., Solianik, R., et al. (2020). A 10-week yoga practice has no effect on cognition, but improves balance and motor learning by attenuating brain-derived neurotrophic factor levels in older adults. Exp. Gerontol. 138:110998. doi: 10.1016/j.exger.2020.110998
Chen, W., Li, M., Li, H., Lin, Y., and Feng, Z. (2023). Tai Chi for fall prevention and balance improvement in older adults: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health 11:1236050. doi: 10.3389/fpubh.2023.1236050
Choi, H.-J., Garber, C. E., Jun, T.-W., Jin, Y. S., Chung, S. J., Kang, H. J., et al. (2013). Therapeutic effects of Tai Chi in patients with Parkinson’s disease. ISRN Neurol. 2013, 1–7. doi: 10.1155/2013/548240
Corcos, D. M., Robichaud, J. A., David, F. J., Leurgans, S. E., Vaillancourt, D. E., Poon, C., et al. (2013). A two-year randomized controlled trial of progressive resistance exercise for Parkinson’s disease. Mov. Disord. 28, 1230–1240. doi: 10.1002/mds.25380
De Vries, A. W., Faber, G., Jonkers, I., Van Dieen, J. H., and Verschueren, S. M. P. (2018). Virtual reality balance training for elderly: similar skiing games elicit different challenges in balance training. Gait Posture 59, 111–116. doi: 10.1016/j.gaitpost.2017.10.006
Debû, B., De Oliveira Godeiro, C., Lino, J. C., and Moro, E. (2018). Managing Gait, Balance, and posture in Parkinson’s disease. Curr. Neurol. Neurosci. Rep. 18:23. doi: 10.1007/s11910-018-0828-4
Elangovan, N., Cheung, C., Mahnan, A., Wyman, J. F., Tuite, P., Konczak, J., et al. (2020). Hatha yoga training improves standing balance but not gait in Parkinson’s disease. Sports Med. Health Sci. 2, 80–88. doi: 10.1016/j.smhs.2020.05.005
Gao, Q., Leung, A., Yang, Y., Wei, Q., Guan, M., Jia, C., et al. (2014). Effects of Tai Chi on balance and fall prevention in Parkinson’s disease: a randomized controlled trial. Clin. Rehabil. 28, 748–753. doi: 10.1177/0269215514521044
Gubert, C., and Hannan, A. J. (2021). Exercise mimetics: harnessing the therapeutic effects of physical activity. Nat. Rev. Drug Discov. 20, 862–879. doi: 10.1038/s41573-021-00217-1
Hackney, M. E., and Earhart, G. M. (2008). Tai Chi improves balance and mobility in people with Parkinson disease. Gait Posture 28, 456–460. doi: 10.1016/j.gaitpost.2008.02.005
Hemmeter, U. M., and Ngamsri, T. (2022). Körperliche aktivität und psychische gesundheit: fokus alter. Praxis 111, 193–198. doi: 10.1024/1661-8157/a003853
Hoehn, H., and Yahr, M. D. (2001). Parkinsonism: onset, progression, and mortality. Neurology 17, 427–427. doi: 10.1212/WNL.17.5.427
Hołaj, J., and Chalimoniuk, M. (2022). The impact of dance on balance and posture control in Parkinson’s disease – a systematic review. Physiother. Rev. 26, 5–17. doi: 10.5114/phr.2022.123154
Hosseini, L., Kargozar, E., Sharifi, F., Negarandeh, R., Memari, A. H., Navab, E., et al. (2018). Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: a randomized control trial. J. Exerc. Rehabil. 14, 1024–1031. doi: 10.12965/jer.1836488.244
Huang, H., Zhang, W. Z., Yang, P., and He, Y. X. (2015). Effects of Taijiquan on balance ability and exercise ability in early Parkinson’s disease. Chin. J. Rehabil. Med. 30, 281–282. doi: 10.3969/j.issn.1001-1242.2015.03.016
Illman, J. (2023). Steve Blair: leading expert on the health benefits of exercise. BMJ 383:2496. doi: 10.1136/bmj.p2496
Jarvis, M. (2017). Meditation and yoga associated with changes in brain. Science 358:461. doi: 10.1126/science.358.6362.461
Kadastik-Eerme, L., Rosenthal, M., Paju, T., Muldmaa, M., and Taba, P. (2015). Health-related quality of life in Parkinson’s disease: a cross-sectional study focusing on non-motor symptoms. Health Qual. Life Outcomes 13:83. doi: 10.1186/s12955-015-0281-x
Kim, Y. W., Shin, I.-S., Moon, H. I., Lee, S. C., and Yoon, S. Y. (2019). Effects of non-invasive brain stimulation on freezing of gait in parkinsonism: a systematic review with meta-analysis. Parkins. Related Disord. 64, 82–89. doi: 10.1016/j.parkreldis.2019.02.029
Koelewijn, A. D., and Ijspeert, A. J. (2020). Exploring the contribution of proprioceptive reflexes to balance control in perturbed standing. Front. Bioeng. Biotechnol. 8:866. doi: 10.3389/fbioe.2020.00866
Lan, C., Chen, S.-Y., Lai, J.-S., and Wong, A. M. (2013). Tai Chi Chuan in medicine and health promotion. Evid. Based Complement. Altern. Med. 2013, 1–17. doi: 10.1155/2013/502131
Leitão, L., Venturini, G. R. O., Junior, R. P., Monteiro, E. R., Telles, L. G., Araújo, G., et al. (2022). Impact of different resistance training protocols on balance, quality of life and physical activity level of older women. Int. J. Environ. Res. Public Health 19:11765. doi: 10.3390/ijerph191811765
Li, B., Zhong, Q. L., Yu, H., Wang, D., Huang, Z. Y., and Bi, R. X. (2017). Effects of Tai Chi training on balance function and fear of falling in Parkinson’s patients. China J. Rehabil. Med. 32, 309–312. doi: 10.3969/j.issn.1001-1242.2017.03.013
Li, F., and Harmer, P. (2015). Economic evaluation of a Tai Ji Quan intervention to reduce falls in people with Parkinson disease, Oregon, 2008–2011. Prevent. Chron. Dis. 12:140413. doi: 10.5888/pcd12.140413
Li, F., Harmer, P., Fitzgerald, K., Eckstrom, E., Stock, R., Galver, J., et al. (2012). Tai Chi and postural stability in patients with Parkinson’s disease. N. Engl. J. Med. 366, 511–519. doi: 10.1056/NEJMoa1107911
Li, G., Labandeira-Garcia, J. L., and Sanchez-Lopez, J. (2022). Mechanisms of motor symptom improvement by long-term Tai Chi training in Parkinson’s disease patients. Transl. Neurodegen. 11:6. doi: 10.1186/s40035-022-00280-7
Liu, Z., Li, L., Liu, S., Sun, Y., Li, S., Yi, M., et al. (2020). Reduced feelings of regret and enhanced fronto-striatal connectivity in elders with long-term Tai Chi experience. Soc. Cogn. Affect. Neurosci. 15, 861–873. doi: 10.1093/scan/nsaa111
Mak, M. K. Y., and Wong-Yu, I. S. K. (2019). Exercise for Parkinson’s disease. Int. Rev. Neurobiol. 147, 1–44. doi: 10.1016/bs.irn.2019.06.001
Manson, A., Stirpe, P., and Schrag, A. (2012). Levodopa-induced-dyskinesias clinical features, incidence, risk factors, management and impact on quality of life. J. Parkins. Dis. 2, 189–198. doi: 10.3233/JPD-2012-120103
Mantovani, E., Martini, A., and Tamburin, S. (2023). Pharmacological and non-pharmacological treatments for impulsive-compulsive behaviors in Parkinson’s disease Cochrane Movement Disorders Group. Cochr. Datab. Syst. Rev. 2023:CD015046. doi: 10.1002/14651858.CD015046
Marras, C., Beck, J. C., Bower, J. H., Roberts, E., Ritz, B., Ross, G. W., et al. (2018). Prevalence of Parkinson’s disease across North America. NPJ Parkins. Dis. 4:21. doi: 10.1038/s41531-018-0058-0
Micó-Amigo, M. E., Kingma, I., Faber, G. S., Kunikoshi, A., van Uem, J. M. T., van Lummel, R. C., et al. (2017). Is the assessment of 5 meters of gait with a single body-fixed-sensor enough to recognize idiopathic Parkinson’s disease-associated gait? Ann. Biomed. Eng. 45, 1266–1278. doi: 10.1007/s10439-017-1794-8
Müller, E., Gimpl, M., Poetzelsberger, B., Finkenzeller, T., and Scheiber, P. (2011). Salzburg skiing for the elderly study: study design and intervention – health benefit of alpine skiing for elderly. Scand. J. Med. Sci. Sports 21, 1–8. doi: 10.1111/j.1600-0838.2011.01336.x
Myers, P. S., Harrison, E. C., Rawson, K. S., Horin, A. P., Sutter, E. N., McNeely, M. E., et al. (2020). Yoga improves balance and low-back pain, but not anxiety, in people with Parkinson’s disease. Int. J. Yoga Ther. 30, 41–48. doi: 10.17761/2020-D-18-00028
Nick, N., Petramfar, P., Ghodsbin, F., Keshavarzi, S., and Jahanbin, I. (2016). The effect of yoga on balance and fear of falling in older adults. PMR 8, 145–151. doi: 10.1016/j.pmrj.2015.06.442
Obeso, J. A., Rodriguez-Oroz, M. C., Goetz, C. G., Marin, C., Kordower, J. H., Rodriguez, M., et al. (2010). Missing pieces in the Parkinson’s disease puzzle. Nat. Med. 16, 653–661. doi: 10.1038/nm.2165
Parga, J. A., Rodriguez-Perez, A. I., Garcia-Garrote, M., Rodriguez-Pallares, J., and Labandeira-Garcia, J. L. (2021). NRF2 activation and downstream effects: focus on Parkinson’s disease and brain angiotensin. Antioxidants 10:1649. doi: 10.3390/antiox10111649
Patel, K. K., Deshmukh, M., and Palekar, T. (2019). Effect of Yoga on balance in geriatric population. Int. J. Sci. Res. Sci. Technol. 6, 595–605. doi: 10.32628/IJSRST11962130
Pedersini, C. A., Guàrdia-Olmos, J., Montalà-Flaquer, M., Cardobi, N., Sanchez-Lopez, J., Parisi, G., et al. (2020). Functional interactions in patients with hemianopia: a graph theory-based connectivity study of resting fMRI signal. PLoS One 15:e0226816. doi: 10.1371/journal.pone.0226816
Penn, I.-W., Sung, W.-H., Lin, C.-H., Chuang, E., Chuang, T. Y., Lin, P. H., et al. (2019). Effects of individualized Tai-Chi on balance and lower-limb strength in older adults. BMC Geriatr. 19:235. doi: 10.1186/s12877-019-1250-8
Perez-Lloret, S., Negre-Pages, L., Damier, P., Delval, A., Derkinderen, P., Destée, A., et al. (2014). Prevalence, determinants, and effect on quality of life of freezing of gait in Parkinson disease. JAMA Neurol. 71:884. doi: 10.1001/jamaneurol.2014.753
Perlmutter, J. S., and Ushe, M. (2020). Parkinson’s Disease — What’s the FUS? N. Engl. J. Med. 383, 2582–2584. doi: 10.1056/NEJMe2031151
Peterka, R. J. (2002). Sensorimotor integration in human postural control. J. Neurophysiol. 88, 1097–1118. doi: 10.1152/jn.2002.88.3.1097
Richer, N., and Lajoie, Y. (2020). Automaticity of postural control while dual-tasking revealed in young and older adults. Exp. Aging Res. 46, 1–21. doi: 10.1080/0361073X.2019.1693044
Rogge, A.-K., Röder, B., Zech, A., and Hötting, K. (2018). Exercise-induced neuroplasticity: balance training increases cortical thickness in visual and vestibular cortical regions. Neuroimage 179, 471–479. doi: 10.1016/j.neuroimage.2018.06.065
Santos, D. P. M. A., Queiroz, A. C. C. M., Menezes, R. L., and Bachion, M. M. (2020). Effectiveness of senior dance in the health of adults and elderly people: an integrative literature review. Geriatr. Nurs. 41, 589–599. doi: 10.1016/j.gerinurse.2020.03.013
Sañudo, B., González-Navarrete, Á, Álvarez-Barbosa, F., de Hoyo, M., Del Pozo, J., Rogers, M. E., et al. (2019). Effect of flywheel resistance training on balance performance in older adults. A randomized controlled trial. J. Sports Sci. Med. 18, 344–350.
Siderowf, A., McDermott, M., Kieburtz, K., Blindauer, K., Plumb, S., Shoulson, I., et al. (2002). Test–retest reliability of the unified Parkinson’s disease rating scale in patients with early Parkinson’s disease: results from a multicenter clinical trial. Mov. Disord. 17, 758–763. doi: 10.1002/mds.10011
Solis-Escalante, T., Van Der Cruijsen, J., De Kam, D., van Kordelaar, J., Weerdesteyn, V., Schouten, A. C., et al. (2019). Cortical dynamics during preparation and execution of reactive balance responses with distinct postural demands. Neuroimage 188, 557–571. doi: 10.1016/j.neuroimage.2018.12.045
Stuart, S., Vitorio, R., Morris, R., Martini, D. N., Fino, P. C., Mancini, M., et al. (2018). Cortical activity during walking and balance tasks in older adults and in people with Parkinson’s disease: a structured review. Maturitas 113, 53–72. doi: 10.1016/j.maturitas.2018.04.011
Su, J., Huang, P., Qin, M., Lu, Q., Sang, X., Cai, Y., et al. (2018). Reduction of HIP2 expression causes motor function impairment and increased vulnerability to dopaminergic degeneration in Parkinson’s disease models. Cell Death Dis. 9, 1020. doi: 10.1038/s41419-018-1066-z
Takakusaki, K. (2017). Functional neuroanatomy for posture and gait control. J. Mov. Disord. 10, 1–17. doi: 10.14802/jmd.16062
Taube, W., Gruber, M., Beck, S., Faist, M., Gollhofer, A., Schubert, M., et al. (2007). Cortical and spinal adaptations induced by balance training: correlation between stance stability and corticospinal activation. Acta Physiol. 189, 347–358. doi: 10.1111/j.1748-1716.2007.01665.x
The Lancet (2016). Balancing the benefits and risks of choice. Lancet 388, 1129. doi: 10.1016/S0140-6736(16)31641-5
Tian, Q., Chastan, N., Bair, W.-N., Resnick, S. M., Ferrucci, L., Studenski, S. A., et al. (2017). The brain map of gait variability in aging, cognitive impairment and dementia—A systematic review. Neurosci. Biobehav. Rev. 74, 149–162. doi: 10.1016/j.neubiorev.2017.01.020
Tiedemann, A., O’Rourke, S., Sesto, R., and Sherrington, C. (2013). A 12-week iyengar yoga program improved balance and mobility in older community-dwelling people: a pilot randomized controlled trial. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 68, 1068–1075. doi: 10.1093/gerona/glt087
Vergara-Diaz, G., Osypiuk, K., Hausdorff, J. M., Bonato, P., Gow, B. J., Miranda, J. G., et al. (2018). Tai Chi for reducing dual-task gait variability, a potential mediator of fall risk in Parkinson’s disease: a pilot randomized controlled trial. Glob. Adv. Health Med. 7:216495611877538. doi: 10.1177/2164956118775385
Vieira, A. K. S., and Cavalcante, B. R. (2021). 12 Weeks of progressive resistance training on postural balance and concerns about falling in older adults: randomized controlled trial. Motricidade 17:139. doi: 10.6063/motricidade.24977
Winser, S. J., Tsang, W. W., Krishnamurthy, K., and Kannan, P. (2018). Does Tai Chi improve balance and reduce falls incidence in neurological disorders? A systematic review and meta-analysis. Clin. Rehabil. 32, 1157–1168. doi: 10.1177/0269215518773442
Witt, K., Kalbe, E., Erasmi, R., and Ebersbach, G. (2017). Nichtmedikamentöse Therapieverfahren beim Morbus Parkinson. Der. Nervenarzt. 88, 383–390. doi: 10.1007/s00115-017-0298-y
Xiao, B., and Tan, E.-K. (2023). Thalamic pathways mediating motor and non-motor symptoms in a Parkinson’s disease model. Trends Neurosci. 46, 1–2. doi: 10.1016/j.tins.2022.09.004
Xiao, C. (2014). Effects of long-term Tai Chi ball practice on balance performance in older adults. J. Am. Geriatr. Soc. 62, 984–985. doi: 10.1111/jgs.12805
Xiao, H. L., Hong, A. H., and Ma, X. Z. (2021). Observation on the effect of Taijiquan in improving balance disorder in patients with early Parkinson’s disease. Chin. Manipul. Rehabil. Med. 12, 41–42+44. doi: 10.19787/j.issn.1008-1879.2021.08.017
Xie, H., Zhang, M., Huo, C., Xu, G., Li, Z., Fan, Y., et al. (2019). Tai Chi Chuan exercise related change in brain function as assessed by functional near–infrared spectroscopy. Sci. Rep. 9:13198. doi: 10.1038/s41598-019-49401-9
Xu, D. (2004). Effect of tai chi exercise on proprioception of ankle and knee joints in old people. Br. J. Sports Med. 38, 50–54. doi: 10.1136/bjsm.2002.003335
Yin, J., Liu, Y., Lyu, W., and Fan, Y. (2023). Tai Ji on cognitive function improvement in Parkinson’s disease: a meta-analysis. J. Integr. Neurosci. 22:123. doi: 10.31083/j.jin2205123
Yu, W., An, C., and Kang, H. (2013). Effects of resistance exercise using thera-band on balance of elderly adults: a randomized controlled trial. J. Phys. Ther. Sci. 25, 1471–1473. doi: 10.1589/jpts.25.1471
Yu, X., Wu, X., Hou, G., Han, P., Jiang, L., Guo, Q., et al. (2021). The impact of Tai Chi on motor function, balance, and quality of life in Parkinson’s disease: a systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2021:6637612. doi: 10.1155/2021/6637612
Keywords: Parkinson’s disease, healthy older adults, Tai Chi, yoga, resistance exercise, balance function, exercise intervention
Citation: Guo XB and Tang L (2024) Effects of different exercise types on balance function in healthy older adults and Parkinson’s patients: a systematic review. Front. Aging Neurosci. 16:1411584. doi: 10.3389/fnagi.2024.1411584
Received: 03 April 2024; Accepted: 11 December 2024;
Published: 24 December 2024.
Edited by:
Roger Adams, University of Canberra, AustraliaReviewed by:
Adebimpe Obembe, College of Saint Mary, United StatesCopyright © 2024 Guo and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lu Tang, dGFuZ2x1eXVAYWxpeXVuLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.