- 1Department of Anesthesiology, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, China
- 2Big Data and Artificial Intelligence Center, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, China
- 3Department of Anesthesiology, Shantou Central Hospital, Shantou, Guangdong, China
- 4Department of Neurosurgery, Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, Guangdong, China
- 5Guangzhou AID Cloud Technology Co., Ltd, Guangzhou, Guangdong, China
Introduction: Geriatric postoperative stroke is a rare but serious complication after surgery. The association between hypertriglyceridemia and postoperative stroke remains controversial, especially in older patients undergoing non-cardiac, non-neurological surgery. The study aims to address this clinical dilemma.
Materials and methods: We conducted a nested case-control study among 9601 aged patients undergoing non-cardiac non-neurological surgery from October 2015 to 2021. A total of 22 positive cases were matched for the surgical type and time, to 88 control patients by a ratio of 1:4. The effect of hypertriglyceridemia on the occurrence of postoperative stroke within 30 days after surgery was estimated using conditional logistic regression analysis by adjusting to various potential confounders.
Results: A total of 22 cases developed ischemia stroke after surgery, and compared with the non-stroke group, they had more postoperative ICU admission, longer postoperative hospitalization and higher total cost (all p < 0.05), and more patients were presenting with preoperative hypertriglyceridemia [8 (36.4%) vs. 15 (17.0%), p = 0.045]. There was a significant association between hypertriglyceridemia and postoperative stroke, with adjusted odds ratios of 6.618 (95% CI 1.286, 34.064) (p = 0.024). The above results remained robust in the sensitivity analyses.
Conclusion: Among older patients undergoing non-cardiac and non-neurological surgery, hypertriglyceridemia was associated with significant increased risk of postoperative stroke.
Introduction
Postoperative stroke is a rare but serious postoperative complication associated with high disability and fatality rates. The incidence of postoperative stroke was approximately 0.01–1% in patients undergoing non-cardiac, non-neurological procedures (Mashour et al., 2011, 2014) and even up to 9–10% in patients undergoing difficult heart surgery and neurosurgery (Vlisides and Mashour, 2016; Mrkobrada et al., 2019). However, the 30-day mortality rates in patients who experience postoperative stroke ranged from 21 to 26%, which were 8 times greater than those without postoperative stroke (Mashour et al., 2011; Wang et al., 2019; Benesch et al., 2021). Meanwhile, patients with postoperative stroke also have longer hospital stay and higher risk of being discharged to long-term care facilities (Lindberg and Flexman, 2021). Notably, perioperative covert stroke was reported to occur in up to 7% of the older patients undergoing non-cardiac, non-neurological surgery (Mrkobrada et al., 2019). As the population ages, age of patients undergoing surgery has been increasing, the geriatric stroke after surgery represents a significant public health burden worldwide and early prediction and intervention help to improve the postoperative outcomes of the older patients (Minhas et al., 2020).
Multiple studies have reported the risk factors for postoperative stroke in patients undergoing non-cardiac, non-neurological surgery, including dyslipidemia, overweight and obesity, and metabolic syndrome (Kernan et al., 2014). Whereas, to our knowledge, few study is focusing on the older populations (van Lier et al., 2009; Bahrainwala et al., 2011; Dong et al., 2017; Kwon et al., 2021). Compared with hypercholesterolemia which is tightly associated with stroke (Sacco et al., 2008), hypertriglyceridemia is another type of dyslipidemia that received lesser attention, as its role in stroke remains controversial (Kivioja et al., 2018). On one way, patients with hypertriglyceridemia were also reported to have a significantly increased risk of incident ischemic stroke (Toth et al., 2018; Wang et al., 2018). On the other way, Anxin Wang and his colleague did not observe any significant association between triglycerides variability and ischemic or hemorrhagic stroke (Wang et al., 2020). In another nested case-control study which enrolled 5475 patients with ischemic stroke, 4776 patients with intracerebral hemorrhage, and 6290 control patients, it was demonstrated that hypertriglyceridemia were weakly correlated with ischemic stroke risk (Sun et al., 2019). To our knowledge, whether preoperative hypertriglyceridemia is associated with postoperative stroke in the older patients receiving non-cardiac, non-neurological procedures has not been reported.
To explore the risk factors for postoperative stroke in older patients undergoing non-cardiac, non-neurological surgery, we conducted a nested case-control study using a large retrospective cohort in our center, and found that hypertriglyceridemia is associated with stroke after non-cardiac, non-neurological surgery in the older patients, which enable early intervention to improve their postoperative outcomes.
Materials and methods
Study design
The current study was designed as a nested case-control study in a large retrospective cohort of older patients undergoing non-cardiac and non-neurosurgical surgery. The local hospital ethics committee (The Third Affiliated Hospital of Sun Yat-sen University) approved the study protocol [No. (2019)02-609-02]. No formal informed permission was required because patients were not subjected to investigational actions and unidentifiable patient information was derived from electric health records (EHR).
Study population
All patients over 65 yrs old who underwent inpatient surgical procedures in our center from April 2015 to 2021 were included. Patients with any of the following conditions were excluded: (1) patients undergoing cardiac or neurosurgical procedures, including surgeries of major arteries such as aneurisms of thoracic aorta, (2) patients with preoperative stroke or stroke occurred beyond 30 days after surgery.
Selection of cases and controls
Postoperative stroke is defined as a brain infarction of ischemic or hemorrhagic etiology that occurs within 30 days after surgery (Leary and Varade, 2020). Positive cases were patients with a new focal neurologic impairment of cerebral origin that lasts more than 24 h, or a computed tomography [CT] hemorrhage (Ferrara, 2020). The diagnosis of stroke was made by a neurologist and an anesthesiologist who reviewed all the EHR. Notably, positive cases included diagnoses established solely on clinical grounds (i.e., without CT abnormalities). Cases (with stroke) and controls (without stroke) were matched on type and time of surgery. For every patient with postoperative stroke, four control patients were selected who underwent the same surgery during the same period (as close as possible to the surgical date of the case) but did not experience a postoperative stroke. A ratio of 1:4 is known to yield the best results taking into account the effort to collect the information of the controls (Zhou et al., 2021). When an identical type of surgery was not available, a patient who had the most similar procedure was chosen as a control.
Data collection
Based on previous literature, the clinical data related to demographics, detailed medical histories or perioperative variables associated with postoperative stroke were collected from the EHR system according to our earlier report (Chen et al., 2022). Demographic characteristics related to older patients including age, gender, and body mass index (BMI). Preoperative comorbidity include hypertension, diabetes, cerebrovascular disorders, carotid stenosis, coronary heart disease, atrial fibrillation, renal insufficiency, systemic lupus erythematosus (SLE), chronic obstructive pulmonary disease (COPD), history of drinking and smoking, hemodialysis and intubation before surgery. Preoperative mediations include β blocker, anticoagulant and antiplatelet agents. Preoperative laboratory findings included hemoglobin (HGB), hematocrit (HCT), platelets (PLT), monocyte, neutrophil (NEUT), high sensitivity C reactive protein (hsCRP), creatinine, blood urea nitrogen (BUN), estimated glomerular filtration rate (GFR), uric acid (UA), glucose (GLU), gamma-glutamyl transpeptidase (GGT), alanine transaminase (ALT), aspartate aminotransferase (AST), total bilirubin (TBILI), indirect bilirubin (IBILI), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, thrombin time (TT), activated partial thromboplastin time (APTT), international normalized ratio (INR), and fibrinogen. Intraoperative variables included administration of dexmedetomidine, parecoxib sodium, flurbiprofen axetil, dexamethasone, metylprednisolon, furosemide and mannitol, intraoperative infusion of crystal, colloid and red blood cell (RBC), volume of blood loss and urine output, and duration of surgery. Postoperative outcomes were also collected, including intensive care unit (ICU) admission, postoperative hospitalization, total cost and in-hospital death.
Potential confounders
As the normal range of triglycerides was 0.34–1.92 mmol/L in our hospital, the hypertriglyceridemia was defined as triglycerides concentration >1.92 mmol/L. Variables potentially confounding the association between hypertriglyceridemia and postoperative stroke were predefined based on existing literature, clinical experience and our available EHR system, including age, gender, hypertension, diabetes, concentration of fibrinogen, and duration of surgery.
Statistical analysis
Differences in clinical characteristics between the positive cases and controls were compared using the Student’s t-test for continuous variables which were normally distributed, and the non-parametric Kruskall-Wallis test was used for continuous variables with non-normal distribution. Categorical variables were compared using the Pearson chi-square test or the Fisher exact test. Conditional logistic regression analysis was conducted to estimate association between hypertriglyceridemia and postoperative stroke (Arfè et al., 2016; Glanz et al., 2018). We adjusted for different number of potential confounders in the conditional logistic regression, based on the event per variable (EPV), our experience and the data integrity. The odds ratio (OR) and 95% confidence intervals (CI) were calculated, respectively (Zhang et al., 2019; Zhao et al., 2021).
Several sensitivity analyses were performed to evaluate the robustness of the association between hypertriglyceridemia and postoperative stroke. We analyzed whether the association would change if individuals who underwent liver transplantation were removed. We reanalyzed the association if individuals who underwent carotid endarterectomy were removed. Given the possible impact of anesthesia type on postoperative stroke, we evaluated the association between hypertriglyceridemia and postoperative stroke in those patients with general anesthesia. All analyses were performed using R (release 2.13.1; R Foundation for Statistical Computing, Vienna, Austria).
Results
Of the 9601 initially screened patients in the cohort, 577 patients received cardiac or neurosurgical surgery and 460 patients had stroke before surgery or beyond 30 days after surgery were excluded. Among the 8564 patients, 22 patients (0.26%) were diagnosed as postoperative stroke within 30 days after surgery. After excluding 8454 patients with missing data or did not match the stroke group by surgery and time, a total of 22 eligible cases and 88 successfully matched controls were finally included in the study (Figure 1).
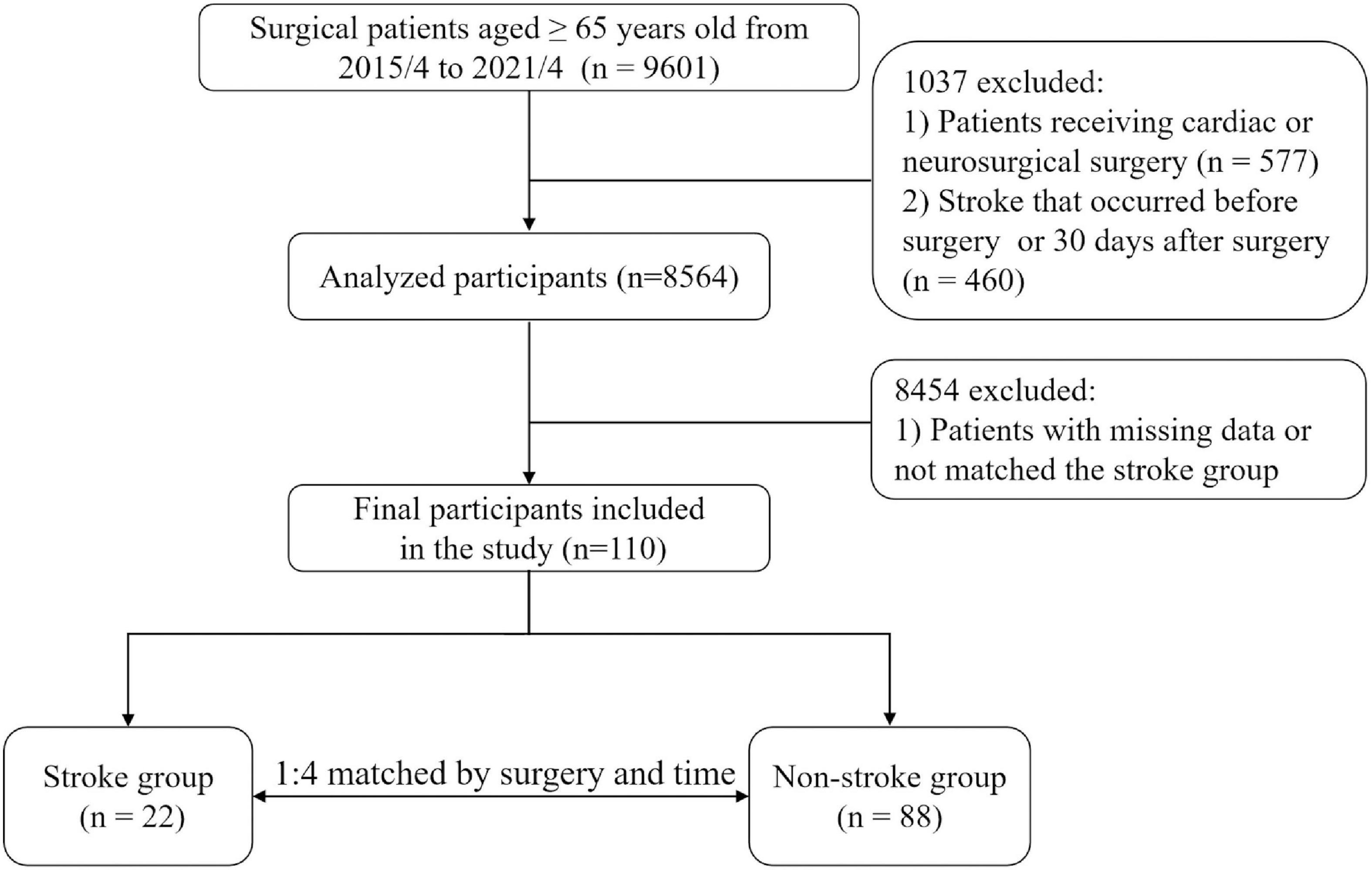
Figure 1. Study flowchart. The stroke diagnosis of each patient, both in the case and control groups, was re-confirmed by a neurologist and an anesthesiologist.
Characteristics of the study population
In the study, we found all the 22 cases were diagnosed as ischemia stroke and all the stroke occurred within 21 days after surgery (Supplementary Table 1). Among the 110 patients (22 cases and 88 controls), the median age was 70 (67–75) years and 68 (61.8%) were men. Patients in the two groups were comparable in age [70 (67–74) vs. 72 (68–76), p = 0.564, Table 1], gender [52 (59.1%) men vs. 16 (72.7%) men, p = 0.239] and BMI [23 (21.1–25.5) vs. 24.8 (22.2–26.7), p = 0.115, Table 1].
Compared with the control group, more patients in the stroke group were presenting with hypertriglyceridemia [8 (36.4%) vs. 15 (17.0%), p = 0.045], while other preoperative variables including the comorbidities (hypertension, diabetes, cerebrovascular disorders, carotid stenosis, coronary heart disease, atrial fibrillation, renal insufficiency, SLE and COPD), administration of β blockers, anticoagulant and antiplatelet agents, other lipid indexes (TC, HDL-C, LDL-C) and other laboratory variables showed no significant differences between groups (all p > 0.05). The intraoperative characteristics of the 110 cases including medication, transfusion and duration of surgery were basically balanced (all p > 0.05, Table 2).
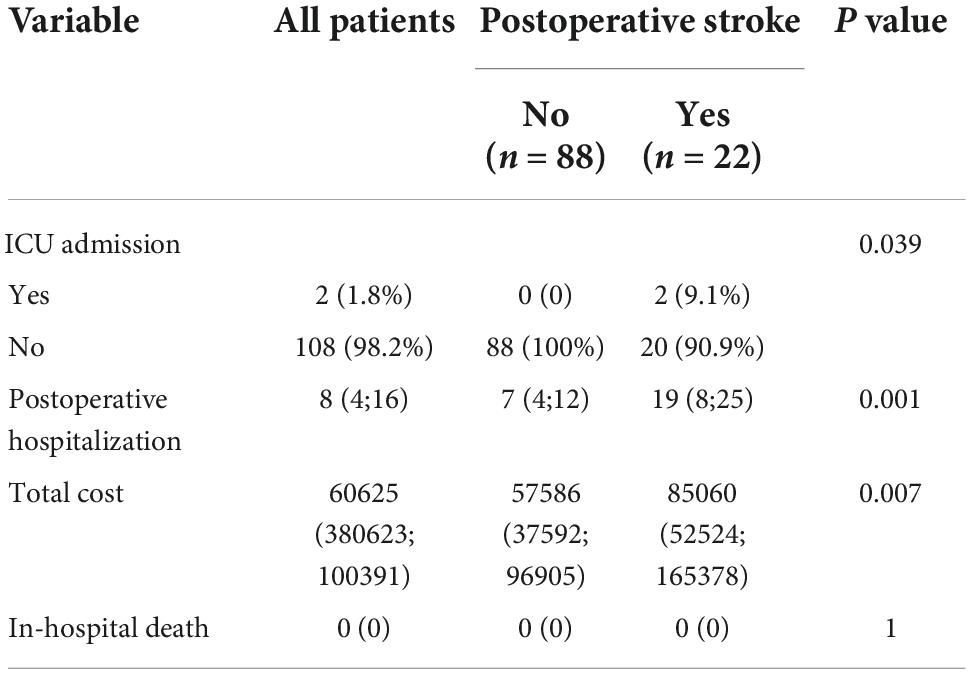
Prognosis of the study population
Compared with the control group, the stroke group had higher incidence of postoperative ICU admission [2 (9.1%) vs. 0 (0), p = 0.039; Table 3], longer postoperative hospitalization [19 (8, 25) vs. 7 (4, 12), p < 0.001; Table 3] and higher total cost [85060 (52524, 165378) yuan vs. 57586 (37592, 96905) yuan, p < 0.001; Table 3]. Meanwhile, the overall mortality was zero in the study.
Risk of stroke after non-cardiac, non-neurological surgery in the older patients
There were 8 (36.4%) and 15 (17.0%) patients had preoperative hypertriglyceridemia in the stroke and the control groups, respectively. The crude analysis showed a 4.71-fold [95% CI (1.13, 19.63), p = 0.0331] increased risk of postoperative stroke in patients with elevated triglycerides. After adjusting only for matched covariates (age, gender, fibrinogen, hypertension, diabetes and duration of surgery), we observed an increased risk of stroke in patients presenting with preoperative hypertriglyceridemia, compared with those who did not [OR 7.46, 95% CI (1.35, 41.22), p = 0.0211; Table 4]. Meanwhile, we found that after adjusting for two to eight confounders like age, gender, fibrinogen, hypertension, diabetes, duration of surgery and medications like β blockers and antiplatelet agents, preoperative hypertriglyceridemia was significantly associated with postoperative stroke (Supplementary Table 2). However, if we increased to 11 confounders and made the EPV to be 2, we found no significant increased risk of stroke between patients presenting with preoperative hypertriglyceridemia and those who did not (P > 0.05).
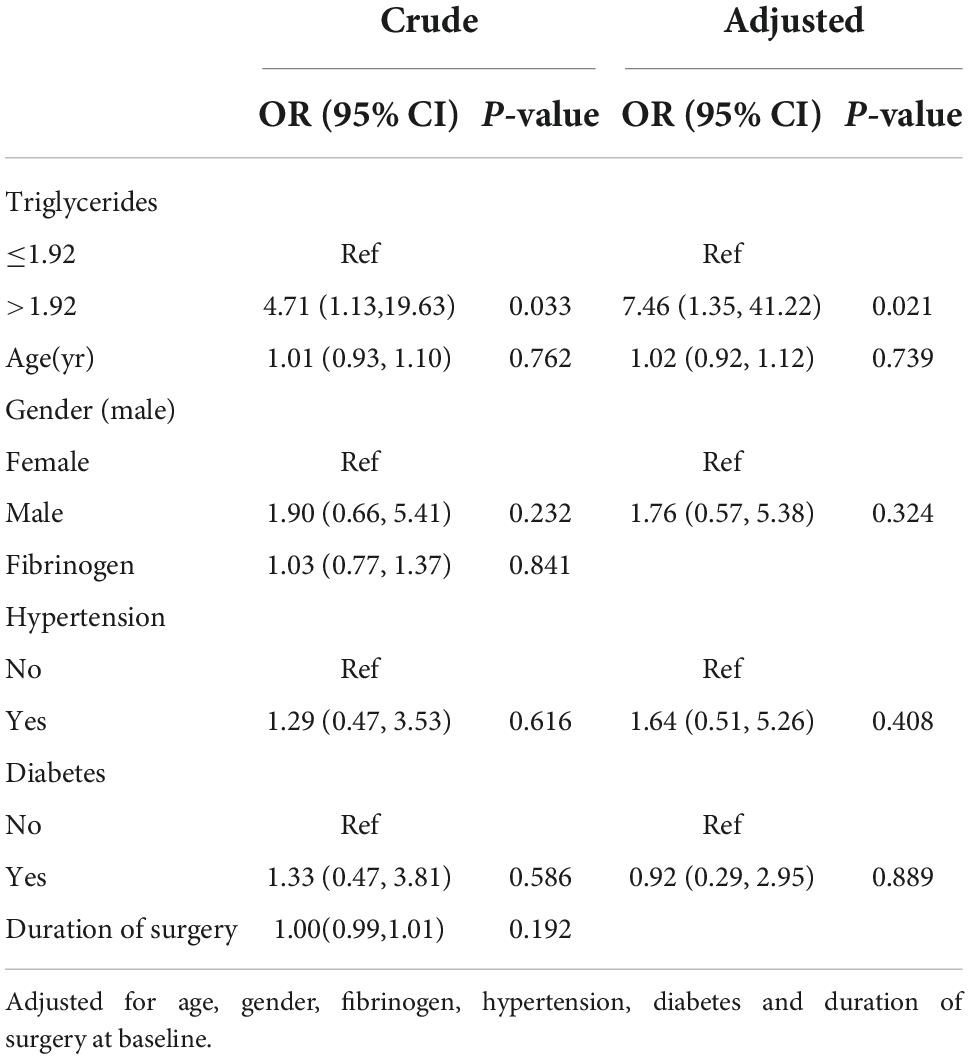
Table 4. Relationship of hypertriglyceridemia with the risk of postoperative stroke in older patients undergoing non-cardiac non-neurosurgery procedures.
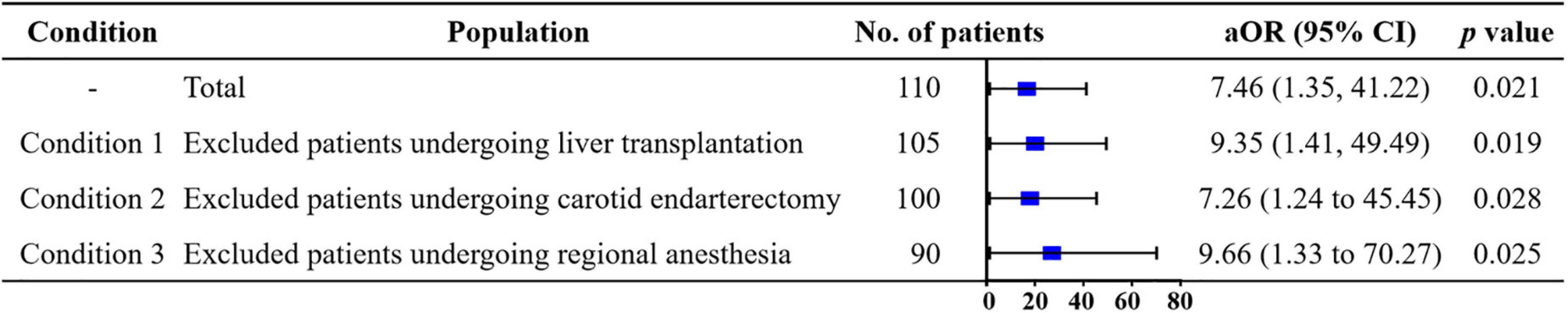
Sensitivity analyses
We conducted three sensitivity analyses to account for observed confounders (Figure 2). First, the result remained robust after excluding patients undergoing liver transplantation whose conditions and operations were much more complicated than others. Compared with patients with triglyceride ≤ 1.92, those with triglyceride > 1.92 had a higher risk of stroke [aOR 9.35, 95% CI (1.41, 49.49), p = 0.019]. In addition, we reanalyzed the data after excluding patients undergoing carotid endarterectomy. The risk of stroke was significantly increased in the multivariable model [aOR 7.26, 95% CI (1.24, 45.45), p = 0.028]. After excluding the patients undergoing regional anesthesia, the hypertriglyceridemia was still associated with increased risk of stroke [aOR 9.66, 95% CI (1.33, 70.27), p = 0.025].
Discussion
In this nested case-control study among the older patients undergoing non-cardiac, non-neurological surgery, we found that 0.257% of the older patients suffered from a perioperative ischemia stroke, which prolonged postoperative hospital stay and increased the total hospitalization charges. Moreover, we found preoperative hypertriglyceridemia was associated with 7.46-fold increased risk of postoperative stroke after adjusting for confounding variables including age, gender, hypertension, diabetes, fibrinogen and duration of surgery.
To our knowledge, the incidence of postoperative stroke in the study was consistent with early reports in patients undergoing non-cardiac, non-neurological procedures (Mashour et al., 2011, 2014). Moreover, this was the first study to show the clinical association between hypertriglyceridemia and the probability of postoperative stroke in older patients receiving non-cardiac, non-neurological surgery. Hypertriglyceridemia is generally caused by defects in triglyceride metabolism in the older population and manifests as increased levels of plasma triglyceride (Bhatt et al., 2019). Although hypertriglyceridemia has been reported to be correlated with the increased risk of ischemic stroke according to large clinical trials (Cui and Naikoo, 2019; Gu et al., 2019), its role in stroke remains controversial and few study focuses on postoperative stroke (Glasser et al., 2016; Holmes et al., 2018). For instance, a longitudinal observational cohort study showed that in patients receiving conventional statin therapy, no significant difference was found in the incidence of non-fatal strokes between the hypertriglyceridemia group and the normal triglyceride group (HR, 1.09; 95% CI, 0.89 to 1.33; p = 0.42) (Nichols et al., 2018). In another population-based cohort study, researchers enrolled 961 patients with ischemic stroke and 1403 patients without ischemic stroke, and found no significant association between hypertriglyceridemia and ischemic stroke (aOR, 1.19; 95% CI, 0.94 to 1.53) (Kivioja et al., 2018). In the current nested case-control study, we included 22 older patients with postoperative stroke and matched them on type and time of surgery by a ratio of 1:4. Finally, the conditional logistic regression analysis showed that hypertriglyceridemia maintained an independent relationship with postoperative stroke in fully adjusted models, and the sensitivity analyses yielded similar results.
Triglyceride molecules are the primary means of storing and transporting fatty acids in the cells and in the plasma. Fatty acids are eliminated by oxidation within the hepatocyte or by secretion into the plasma through triglyceride-rich very low-density lipoproteins (VLDL). It is shown that with the increase of age, the activity of lipoprotein lipase and LDL receptor decrease, the levels of VLDL increase, which further increases the level of triglycerides in the plasma (Alves-Bezerra and Cohen, 2017; Johnson and Stolzing, 2019). We think hypertriglyceridemia may increase the risk of postoperative stroke by promoting atherosclerosis in the older patients (Peng et al., 2017). Firstly, hypertriglyceridemia may theoretically cause subendothelial retention of remnant particles and elicitation of endothelial dysfunction, to establish chronic inflammation in the cerevascular (Liang et al., 2022). Secondly, hypertriglyceridemia may cause hyperviscosity and promote thrombosis through a procoagulant effect involved in the disturbance of both blood coagulation and fibrinolysis, and led to postoperative stroke. Notably, the current results revealed that lipid-lowering and triglyceride reduction measures might help to prevent perioperative ischemic stroke in older patients with preoperative hypertriglyceridemia (Bhatt et al., 2019).
To further confirm the association between preoperative hypertriglyceridemia and postoperative stroke, we tried to enroll more variables potentially confounding the association between hypertriglyceridemia and postoperative stroke, include most of the demographic characteristics, preoperative comorbidity, mediations, laboratory results and intraoperative variables. However, the rule of EPV is taken into consideration in the sample size requirement of logistic regression (Peduzzi et al., 1996). Although EPV values are preferably 10 or greater, there are still several important potential confounders need to be adjusted in the study, including age, gender, hypertension, diabetes, concentration of fibrinogen and duration of surgery. As a result, the current EPV is relaxed as almost 5 samples per predictor (Vittinghoff and McCulloch, 2007). Meanwhile, the current results showed that after adjusting for 11 potentially confounding variables and relaxing the EPV to 2, no significant increased risk of stroke was found between patients presenting with preoperative hypertriglyceridemia and those who did not. The results are interesting and we think this might be attributed to the small sample size and EPV value in this condition.
Limitations of the study
The study has several limitations. First of all, we did not collect the duration of hypertriglyceridemia in the patients and whether the triglyceride concentration level was positively correlated with the severity of stroke need to be further explored. Secondly, due to the retrospective observational design, the results lack information of preoperative and postoperative medications like lipid-lowering agents, blood pressure-lowering agents and glucose-lowering agents etc. In terms of agents for hypertriglyceridemia, lipid-lowering agents like omega 3 PUFA may increase bleeding events, while fibrates may increase thrombotic events. Therefore, the drug information is important to interpret the results and further studies are needed to explore and elucidate the role of preoperative and postoperative medications in the development and prognosis of postoperative stroke. Thirdly, the sample size and the positive cases were small and this limited our subgroup analysis to further explore the association between hypertriglyceridemia and postoperative stroke in different kinds of older patients, as well as the effects between different levels of hypercholesterolemia and hypertriglyceridemia in the current study. Fourthly, we did not explore whether hypertriglyceridemia is also a risk factor for other postoperative vascular events like deep vein thrombosis (DVT) and ischemic heart diseases, and further studies are needed to explore it. Finally, although we considered many confounders, the intraoperative hypotension was not correctly recorded in our database and residual confounders such as different test methods in different years might interfere with our findings.
Conclusion
Among the older patients undergoing non-cardiac, non-neurological surgery, preoperative hypertriglyceridemia is associated with increased risk of postoperative stroke. The study findings are limited by potential confounders due to retrospective observational design and further prospective randomized clinical trials are needed to validate the finding.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
CC, CG, and ZH: conception and design. CC, QW, CM, XL, TH, JK, and CG: acquisition of data. CC, QW, and CM: analysis and interpretation of data. CC, QW, CM, XL, TH, JK, CG, and ZH: writing, review, and/or revision of the manuscript. CC and ZH: study supervision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported partly by the National Natural Science Foundation of China (Grant Nos. 81974296 and 82102297), Natural Science Foundation of Guangdong Province (Grant Nos. 2019A1515110020 and 2022A1515012603), the Fundamental Research Funds for the Central Universities of China (Grant No. 22qntd3401), and Young Talent Support Project of Guangzhou Association for Science and Technology (Grant No. QT20220101257).
Conflict of interest
Author JK was employed by Guangzhou AID Cloud Technology Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.935934/full#supplementary-material
References
Alves-Bezerra, M., and Cohen, D. E. (2017). Triglyceride metabolism in the liver. Compr. Physiol. 8, 1–8. doi: 10.1002/cphy.c170012
Arfè, A., Scotti, L., Varas-Lorenzo, C., Nicotra, F., Zambon, A., Kollhorst, B., et al. (2016). Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: Nested case-control study. BMJ 354:i4857. doi: 10.1136/bmj.i4857
Bahrainwala, Z. S., Grega, M. A., Hogue, C. W., Baumgartner, W. A., Selnes, O. A., McKhann, G. M., et al. (2011). Intraoperative hemoglobin levels and transfusion independently predict stroke after cardiac operations. Ann. Thorac. Surg. 91, 1113–1118. doi: 10.1016/j.athoracsur.2010.12.049
Benesch, C., Glance, L. G., Derdeyn, C. P., Fleisher, L. A., Holloway, R. G., Messe, S. R., et al. (2021). Perioperative neurological evaluation and management to lower the risk of acute stroke in patients undergoing noncardiac, nonneurological surgery: A scientific statement from the american heart association/american stroke association. Circulation 143:e923–e946. doi: 10.1161/CIR.0000000000000968
Bhatt, D. L., Steg, P. G., Miller, M., Brinton, E. A., Jacobson, T. A., Ketchum, S. B., et al. (2019). Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N. Engl. J. Med. 380, 11–22. doi: 10.1056/NEJMoa1812792
Chen, C., Chen, X., Chen, J., Xing, J., Hei, Z., Zhang, Q., et al. (2022). Association between preoperative hs-crp/albumin ratio and postoperative sirs in elderly patients: A retrospective observational cohort study. J. Nutr. Health Aging 26, 352–359. doi: 10.1007/s12603-022-1761-4
Cui, Q., and Naikoo, N. A. (2019). Modifiable and non-modifiable risk factors in ischemic stroke: A meta-analysis. Afr. Health Sci. 19, 2121–2129. doi: 10.4314/ahs.v19i2.36
Dong, Y., Cao, W., Cheng, X., Fang, K., Zhang, X., Gu, Y., et al. (2017). Risk factors and stroke characteristic in patients with postoperative strokes. J. Stroke Cerebrovasc. Dis. 26, 1635–1640. doi: 10.1016/j.jstrokecerebrovasdis.2016.12.017
Ferrara, A. (2020). Computed tomography in stroke diagnosis, assessment, and treatment. Radiol. Technol. 91:447CT–462CT.
Glanz, J. M., Newcomer, S. R., Daley, M. F., DeStefano, F., Groom, H. C., Jackson, M. L., et al. (2018). Association between estimated cumulative vaccine antigen exposure through the first 23 months of life and non-vaccine-targeted infections from 24 through 47 months of age. JAMA 319, 906–913. doi: 10.1001/jama.2018.0708
Glasser, S. P., Mosher, A., Howard, G., and Banach, M. (2016). What is the association of lipid levels and incident stroke? Int. J. Cardiol. 220, 890–894. doi: 10.1016/j.ijcard.2016.06.091
Gu, X., Li, Y., Chen, S., Yang, X., Liu, F., Li, Y., et al. (2019). Association of lipids with ischemic and hemorrhagic stroke: A prospective cohort study among 267 500 Chinese. Stroke 50, 3376–3384. doi: 10.1161/STROKEAHA.119.026402
Holmes, M. V. I., Millwood, Y., Kartsonaki, C., Hill, M. R., Bennett, D. A., Boxall, R., et al. (2018). Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J. Am. Coll. Cardiol. 71, 620–632. doi: 10.1016/j.jacc.2017.12.006
Johnson, A. A., and Stolzing, A. (2019). The role of lipid metabolism in aging, lifespan regulation, and age-related disease. Aging Cell 18:e13048. doi: 10.1111/acel.13048
Kernan, W. N., Ovbiagele, B., Black, H. R., Bravata, D. M., Chimowitz, M. I., Ezekowitz, M. D., et al. (2014). Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke 45, 2160–2236. doi: 10.1161/STR.0000000000000024
Kivioja, R., Pietila, A., Martinez-Majander, N., Gordin, D., Havulinna, A. S., Salomaa, V., et al. (2018). Risk factors for early-onset ischemic stroke: A case-control study. J. Am. Heart Assoc. 7:e009774. doi: 10.1161/JAHA.118.009774
Kwon, S., Kim, T. J., Choi, E. K., Ahn, H. J., Lee, E., Lee, S. R., et al. (2021). Predictors of ischemic stroke for low-risk patients with atrial fibrillation: A matched case-control study. Heart Rhythm 18, 702–708. doi: 10.1016/j.hrthm.2021.01.016
Leary, M. C., and Varade, P. (2020). Perioperative stroke. Curr. Neurol. Neurosci. Rep. 20:12. doi: 10.1007/s11910-020-01033-7
Liang, H. J., Zhang, Q. Y., Hu, Y. T., Liu, G. Q., and Qi, R. (2022). Hypertriglyceridemia: A neglected risk factor for ischemic stroke? J. Stroke 24, 21–40. doi: 10.5853/jos.2021.02831
Lindberg, A. P., and Flexman, A. M. (2021). Perioperative stroke after non-cardiac, non-neurological surgery. BJA Educ. 21, 59–65. doi: 10.1016/j.bjae.2020.09.003
Mashour, G., Moore, L., Lele, A., Robicsek, S., and Gelb, A. (2014). Perioperative care of patients at high risk for stroke during or after non-cardiac, non-neurologic surgery: Consensus statement from the society for neuroscience in anesthesiology and critical care*. J. Neurosurg. Anesthesiol. 26, 273–285. doi: 10.1097/ana.0000000000000087
Mashour, G., Shanks, A., and Kheterpal, S. (2011). Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology 114, 1289–1296. doi: 10.1097/ALN.0b013e318216e7f4
Minhas, J. S., Rook, W., Panerai, R. B., Hoiland, R. L., Ainslie, P. N., Thompson, J. P., et al. (2020). Pathophysiological and clinical considerations in the perioperative care of patients with a previous ischaemic stroke: A multidisciplinary narrative review. Br. J. Anaesth. 124, 183–196. doi: 10.1016/j.bja.2019.10.021
Mrkobrada, M., Chan, M. T. V., Cowan, D., Campbell, D., Wang, C. Y., Torres, D., et al. (2019). Perioperative covert stroke in patients undergoing non-cardiac surgery (NeuroVISION): A prospective cohort study. Lancet 394, 1022–1029. doi: 10.1016/s0140-6736(19)31795-7
Nichols, G. A., Philip, S., Reynolds, K., Granowitz, C. B., and Fazio, S. (2018). Increased cardiovascular risk in hypertriglyceridemic patients with statin-controlled LDL cholesterol. J. Clin. Endocrinol. Metab. 103, 3019–3027. doi: 10.1210/jc.2018-00470
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., and Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49, 1373–1379. doi: 10.1016/s0895-4356(96)00236-3
Peng, J., Luo, F., Ruan, G., Peng, R., and Li, X. (2017). Hypertriglyceridemia and atherosclerosis. Lipids Health Dis. 16:233. doi: 10.1186/s12944-017-0625-0
Sacco, R. L., Diener, H. C., Yusuf, S., Cotton, D., Ounpuu, S., Lawton, W. A., et al. (2008). Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N. Engl. J. Med. 359, 1238–1251. doi: 10.1056/NEJMoa0805002
Sun, L., Clarke, R., Bennett, D., Guo, Y., Walters, R. G., Hill, M., et al. (2019). Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat. Med. 25, 569–574. doi: 10.1038/s41591-019-0366-x
Toth, P., Granowitz, C., Hull, M., Liassou, D., Anderson, A., and Philip, S. (2018). High triglycerides are associated with increased cardiovascular events, medical costs, and resource use: A real-world administrative claims analysis of statin-treated patients with high residual cardiovascular risk. J. Am. Heart Assoc. 7:e008740. doi: 10.1161/jaha.118.008740
van Lier, F., Schouten, O., van Domburg, R. T., van der Geest, P. J., Boersma, E., Fleisher, L. A., et al. (2009). Effect of chronic beta-blocker use on stroke after noncardiac surgery. Am. J. Cardiol. 104, 429–433. doi: 10.1016/j.amjcard.2009.03.062
Vittinghoff, E., and McCulloch, C. E. (2007). Relaxing the rule of ten events per variable in logistic and cox regression. Am. J. Epidemiol. 165, 710–718. doi: 10.1093/aje/kwk052
Vlisides, P., and Mashour, G. A. (2016). Perioperative stroke. Can. J. Anaesth. 63, 193–204. doi: 10.1007/s12630-015-0494-9
Wang, A., Li, H., Yuan, J., Zuo, Y., Zhang, Y., Chen, S., et al. (2020). Visit-to-visit variability of lipids measurements and the risk of stroke and stroke types: A prospective cohort study. J. Stroke 22, 119–129. doi: 10.5853/jos.2019.02075
Wang, H., Li, S., Bai, J., and Wang, D. (2019). Perioperative acute ischemic stroke increases mortality after noncardiac, nonvascular, and non-neurologic surgery: A retrospective case series. J. Cardiothorac. Vasc. Anesth. 33, 2231–2236. doi: 10.1053/j.jvca.2019.02.009
Wang, W., Shen, C., Zhao, H., Tang, W., Yang, S., Li, J., et al. (2018). A prospective study of the hypertriglyceridemic waist phenotype and risk of incident ischemic stroke in a Chinese rural population. Acta Neurol. Scand. 138, 156–162. doi: 10.1111/ane.12925
Zhang, X. P., Gao, Y. Z., Chen, Z. H., Chen, M. S., Li, L. Q., Wen, T. F., et al. (2019). An eastern hepatobiliary surgery hospital/portal vein tumor thrombus scoring system as an aid to decision making on hepatectomy for hepatocellular carcinoma patients with portal vein tumor thrombus: A multicenter study. Hepatology 69, 2076–2090. doi: 10.1002/hep.30490
Zhao, B. C., Lei, S. H., Yang, X., Zhang, Y., Qiu, S. D., Liu, W. F., et al. (2021). Assessment of prognostic value of intraoperative oliguria for postoperative acute kidney injury: A retrospective cohort study. Br. J. Anaesth. 126, 799–807. doi: 10.1016/j.bja.2020.11.018
Keywords: elderly patients, hypertriglyceridemia, postoperative stroke, non-cardiac non-neurological surgery, sensitivity analysis
Citation: Chen C, Wen Q, Ma C, Li X, Huang T, Ke J, Gong C and Hei Z (2022) Hypertriglyceridemia is associated with stroke after non-cardiac, non-neurological surgery in the older patients: A nested case-control study. Front. Aging Neurosci. 14:935934. doi: 10.3389/fnagi.2022.935934
Received: 04 May 2022; Accepted: 27 October 2022;
Published: 14 November 2022.
Edited by:
Li Li, Department of Anesthesiology, Affiliated Beijing Friendship Hospital, Capital Medical University, ChinaReviewed by:
Shun Ishibashi, Jichi Medical University, JapanCheng Ni, Chinese Academy of Medical Sciences and Peking Union Medical College, China
Copyright © 2022 Chen, Wen, Ma, Li, Huang, Ke, Gong and Hei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ziqing Hei, aGVpemlxaW5nQHNpbmEuY29t; Chulian Gong, Z29uZ2NobEBtYWlsLnN5c3UuZWR1LmNu
 Chaojin Chen
Chaojin Chen Qianyu Wen
Qianyu Wen Chuzhou Ma3
Chuzhou Ma3 Jie Ke
Jie Ke