- School of Nursing, Jilin University, Changchun, China
Background: Frailty is considered a major public health challenge of the 21st century, characterized by the decline of multiform body functions. Physical activity may be the most effective intervention to delay frailty. This study aims to verify the effect of remotely supervised physical activity on health profile in community-dwelling frail older adults.
Design: This is a multicenter, three-blind, two-arm, and cohort randomized controlled study.
Methods: The intelligent exercise rehabilitation management system (IERMS) is an integrated digital platform that involves evaluation, guidance, monitoring, and feedback. A total of 120 participants aged ≥ 65 years and diagnosed as frailty on the FRAIL scale will be recruited and randomly divided into two groups. Group 1 will receive a 12-week IERMS-based intervention, and Group 2 will receive the usual care. Data will be collected at baseline, 12 and 24 weeks. The primary outcome is the physical function, and secondary outcomes include gait parameters, psychology, and cognition measurements. Analyses will be performed using DSS statistics, version 25. P < 0.05 will be considered statistically significant.
Conclusion: We believe that intervention plays a positive role in delaying the frailty. If our program is effective, we will provide a viable means to promote healthy aging in primary healthcare.
Trial registration number: ChiCTR2100052286; Pre-results.
Introduction
Frailty is a kind of clinical syndrome in older adults who are easily affected by stress. Physical frailty, originally defined by Fried et al. (2001), includes slow gait speed, weakness, self-reported exhaustion, low activity, and weight loss. Due to differences in regions, diagnostic criteria, and other factors, the prevalence of frailty is changed in different parts of the world; previous studies have shown that the prevalence ranged from 4 to 59% and increased with age (Choi et al., 2015; Hoogendijk et al., 2019). It is associated with the development of most chronic diseases, falls, fractures, disabilities, and other adverse outcomes (Theou et al., 2017; Hanlon et al., 2018). Fortunately, frailty is a dynamic reversible process, and measures can be taken to prevent it in advance (Lang et al., 2009).
The health benefits of physical activity have been widely recognized (Cheng et al., 2021). Proper physical activity can improve muscle, heart, and lung function and reduce the risk of high blood pressure, coronary heart disease, stroke, diabetes, cancer, depression, sleep disorders, falls, and fracture (de Labra et al., 2015; Dipietro et al., 2019; Mugueta-Aguinaga and Garcia-Zapirain, 2019). The WHO recommends that adults over 65 years of age engage in at least 150 min of moderate-intensity physical activity per week or at least 75 min of vigorous-intensity physical activity per week, or a combination of moderate and vigorous-intensity physical activity to achieve this amount of physical activity, with at least 10 min of continuous activity each time (van der Ploeg and Bull, 2020).
Recent research has found that physical activity may be the most effective intervention for frailty (Cheng et al., 2021). It is much more accomplished and effective when performed under supervision (Bonnefoy et al., 2012). Home-based supervised training has a better effect on strength and physical function and is more intense (Lacroix et al., 2017; Suikkanen et al., 2021). However, the allocation of health technicians is far from meeting the requirements of the training supervised by physiotherapists at home, so the current focus of primary healthcare is how to maximize the use of existing medical resources and benefit more people. Remote supervision based on wearable devices gradually attracts the attention of researchers (Garcia-Moreno et al., 2020; Zacharaki et al., 2020). This study aims to verify the effect of remotely supervised physical activity on health profile and observe the lingering effect in community-dwelling frail older adults.
Methods
This study was designed and will be conducted and reported in keeping with the Consolidation Standards of Reporting (CONSORT) 2010 statement (Eldridge et al., 2016).
Platform Delivery
The intelligent exercise rehabilitation management system (IERMS) was designed and developed by the research group independently (Xu et al., 2020). It is an integrating evaluation, guidance, monitoring, and feedback of an integrated intelligent motion rehabilitation management system. It consists of three parts: sensing device layer, management data layer, and application layer. The sensing layer collects the health data, including smart insoles, bracelets, and other common terminals; the management layer conducts data processing; and the application layer visualizes the health results, including websites, applications, and applets. Smart insole is a kind of sensing device that contains eight inertial and thin-film pressure sensors (FSR 400) and grants China an invention patent (Publication Patent Number: 201810114305.3).
Study Design
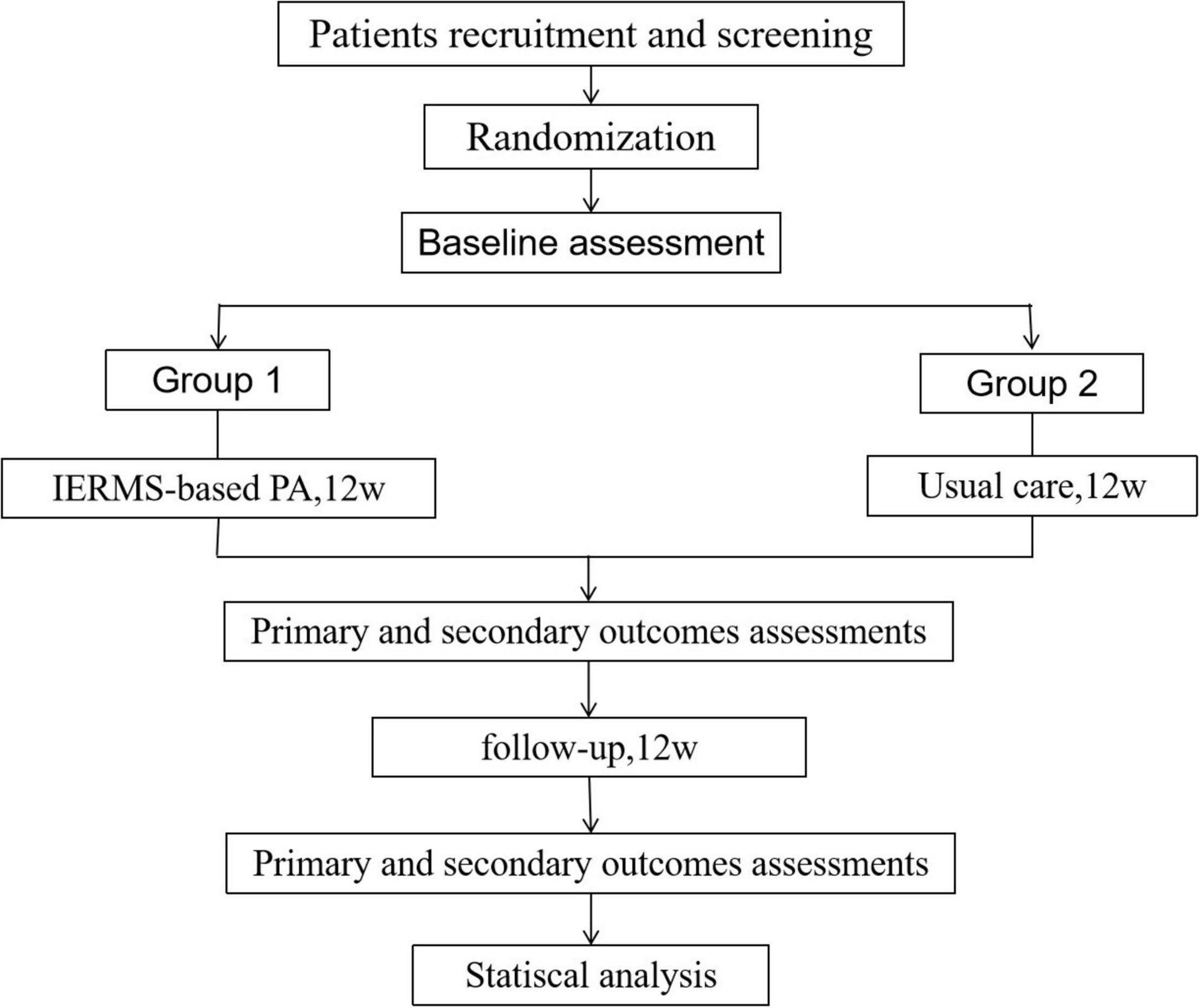
A three-blind, two-arm, cohort randomized controlled trial will be conducted to evaluate the effects of IERMS-based physical activity on health performance in frail older adults (Registration number: ChiCTR2100052286)1. A total of 120 participants will be recruited according to the screening criteria from six community health service centers in Changchun, China, and the participants will be randomly divided into two groups. Participants in the first group will receive a 12-week IERMS-based intervention, and participants in the second group will receive a 12-week conventional care. Then, there will be a 12-week follow-up. Data will be collected at baseline, 12 and 24 weeks. The study design is shown in Figure 1. After the intervention, the same guidance will be given to the second group to ensure that more older adults benefit.
Participants
Ethics Approval
The research protocol was approved by the Human Research Ethics Committee of the School of Nursing, Jilin University (HREC 2020122001). All participants will provide a signed informed consent when entering the study.
Eligibility and Recruitment
Participants will be recruited from six centers at the same time. Once there are 20 samples in a certain community, they will undergo the next step. Inclusion criteria are ≥ 65 years old, meeting the FRAIL scale for frail status, and familiar with the use of smartphones and tablets or computers. Exclusion criteria are nerve dysfunction (stroke, Parkinson’s disease, or lower limbs) with paraplegia, serious cardiovascular disease, cognitive impairment, continuous joint pain, severe muscle bone damage, life expectancy < 6 months of serious illness, serious hearing or visual impairment, severe depression or anxiety, other major diseases affecting training safety, hospitalization, and involvement in other clinical studies during this study.
Calculation of Sample Size
Based on a priori power analysis (G*Power 3.1.9.3) using a power of 0.90 and error probability of 0.05, a sample size of 50 participants will be required for each group to detect an assumed 20% difference in walking speed between the two groups. In addition, with an assumption of 15% dropout rate, a sample size of 120 participants will be initially targeted.
Randomization and Blinding
From each center, 20 participants will be recruited and stratified by gender and age; then, they will be randomly assigned to the first or second group in a 1:1 ratio through a computer-generated randomized list. This task will be performed independently by individuals not involved in the research process. All researchers will be divided into two teams: one team will be responsible for the guidance of group 1, and the other team conduct routine education, they will be ignorant of each other’s content. Throughout the intervention, neither the participants nor the researchers conducting the intervention or the data collection will be aware of the grouping. The study designer and the staff responsible for allocation concealment and data processing will be not permitted to participate in the whole intervention.
Intervention
Training Based on Intelligent Exercise Rehabilitation Management System
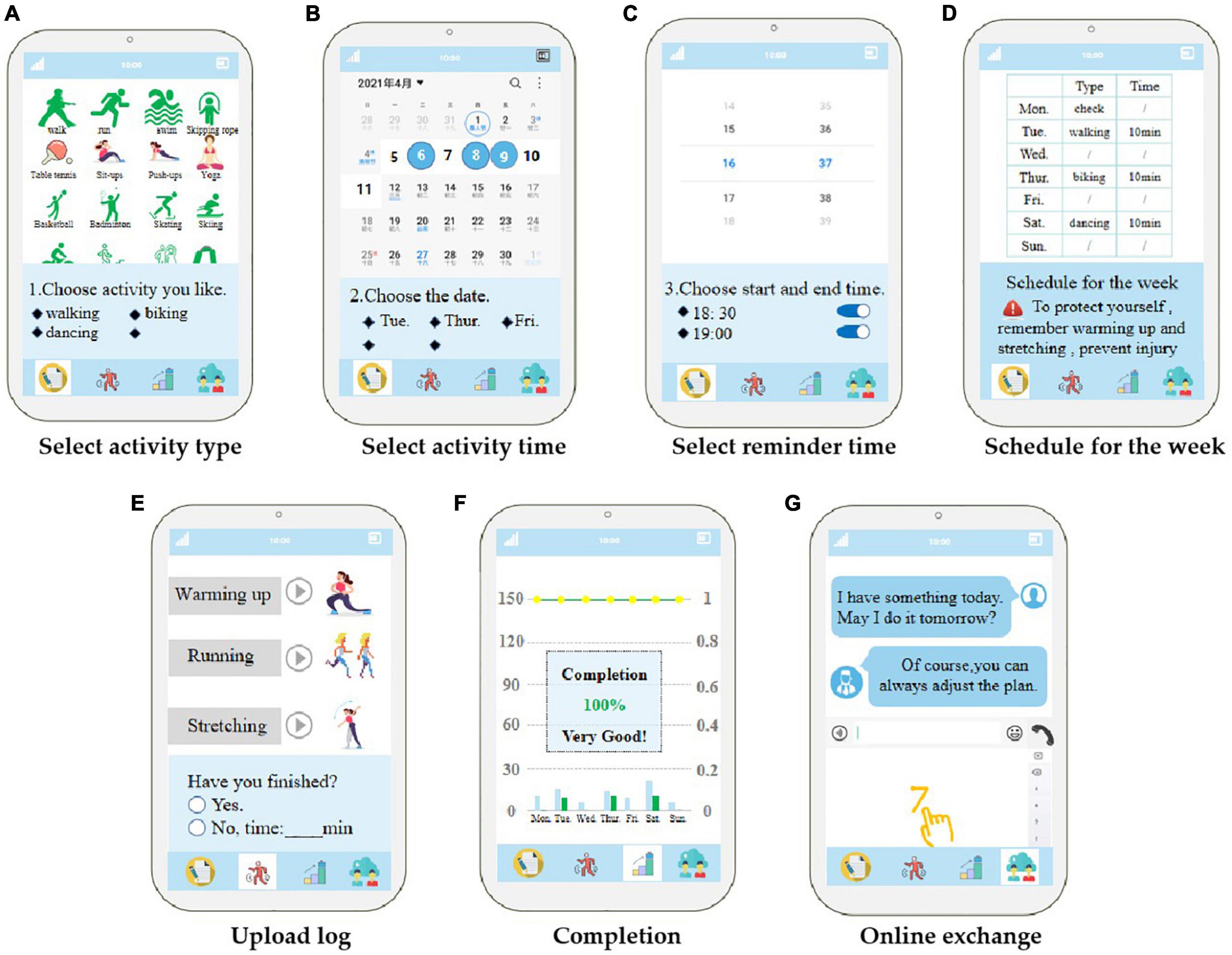
At baseline, all participants will undergo physical function, physical activity, psychology, and cognition assessments. These assessments will be repeated at 12 and 24 weeks. Participants in the first group will receive a pair of smart insoles and a patient-side APP installed on their phone and will learn all the functions of the system. According to the participants’ physical activity level at baseline, professional rehabilitation therapists will select the activity plan from the default scheme (Table 1); upload it to the cloud, which is the management data layer; and send the plan for the next week according to the participants’ weekly completion. If the activity goal of the week is not reached, the plan of the week will be continued. Once the current week’s activities are completed, the plan for the next phase will be carried out. Participants will choose the type of physical activity (Table 2) in the APP according to their preferences and choose the activity day of the week and the training time of each activity according to the target activity days. The system will automatically generate the particular week’s schedule according to participants’ choices and remind them at the time set by participants. At the end of each activity, participants will upload the daily completion of the activity and fill in the specific activity time for unfinished projects. They will have access to view the week’s activity plan at any time and generate the week’s activity schedule every Monday. During the workout, participants will be asked to wear smart insoles that monitor dynamic changes in gait parameters and synchronize them to the cloud in real time. In addition, patients will communicate with professionals through a short messaging service built into the APP and receive feedback within 24 h. The APP interface is shown in Figure 2. Before the start of each training, the user will receive a reminder as follows:
Before activity: Warm-up ≥ 5 min.
After activity: stretch ≥ 5 min.
The time of each successive activity: ≥ 10 min.
The interval between two activities: ≤ 3 days.
Please don’t be nervous if you feel strenuous or the heart rate significantly accelerated in the process of activity, this is a normal phenomenon. But if you feel unwell, please seek medical advice immediately.
Routine Care
All participants will receive a routine nursing care. The rehabilitation therapist will provide health education on frailty and physical activity: manifestation, risk, prevention, screening, and treatment of frailty; benefits of moderate physical activity; and introduction of common forms are listed in Table 2. A registered nurse will conduct a telephonic follow-up for all participants once in a month.
Outcome Measures
In this study, the primary outcome will be the objective changes in physical function. At the same time, other measuring tools will be used to evaluate the multidimensional efficacy of the intervention, and a less number of participants will be selected for semi-structured interviews to gain an in-depth understanding.
Primary Outcome
Physical Function
The physical function will be evaluated by the Timed Up & Go (TUG) test (Mathias et al., 1986), which assesses the basic mobility skill as well as strength, balance, and mobility. In this test, the subjects will stand up from a standard chair (the chair with a height of 46 cm and arms with a height of 65 cm), wear comfortable shoes, walk at a regular speed of 3 m, turn around, walk back to the chair, and sit down in the chair, and then will stop the timer. According to the test results, ≤ 10 s will be considered completely independent, 10–19 s will be considered to be independent, between 20 and 29 s will be considered a “gray area,” and more than 30 s will be considered to be completely dependent. Its reliability and effectiveness have been verified in various populations (Chan et al., 2017; Yuksel et al., 2017).
Secondary Outcomes
Gait Parameters
Gait parameters include walking speed, symmetry, and variability. Participants will wear smart insoles and walk more than 25 m on barrier-free horizontal roads for at least 2 min at their self-selected comfortable pace. The walking process will include four parts, namely, acceleration, deceleration, uniform speed, and turning. The system will complete the gait analysis during this period. Walking speed (m/s) is defined as the walking distance per unit time, and when it is less than 0.6 (Zaccardi et al., 2019), there will be a higher risk of falls. Gait variability is defined as the variable coefficient of all the step-by-step cycles and is used to evaluate the variation of temporal parameters. The normal range is 2–3%, and higher values are regarded as unstable. Gait symmetry is defined as the ratio of the swinging time of biped in the air and is usually around 1.02% for healthy adults.
Frail Score
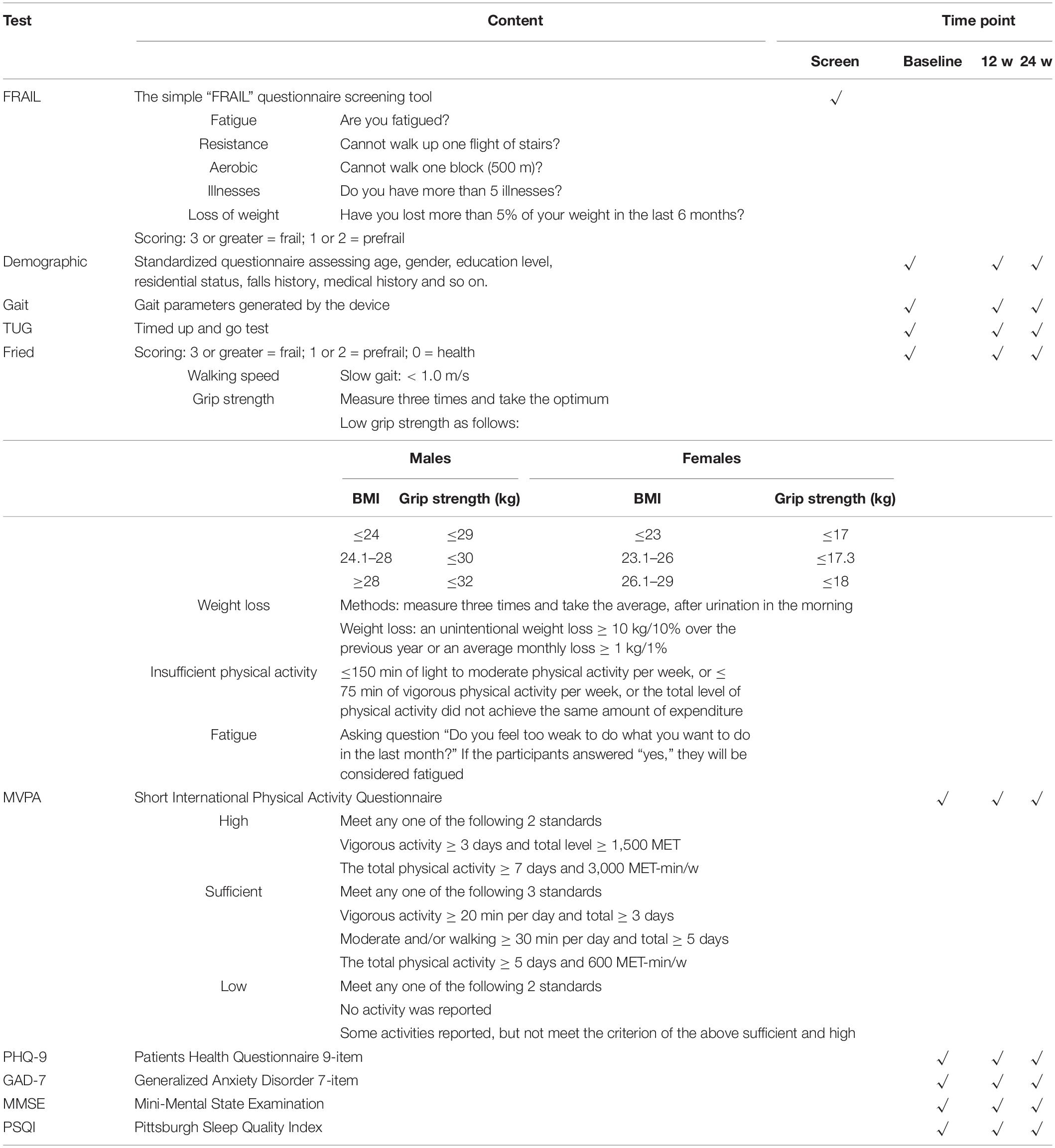
The frailty phenotype represents the most known operational definitions of frailty in older persons (Fried et al., 2001). According to the Fried phenotype: 0 = health; 1–2 = pre-frailty; and ≥ 3 = frailty. Walking speed, grip strength, weight, physical activity, and self-reported fatigue will be measured by the methods as shown in Table 3. One point will be recorded when any items reach the cutoff value.
Moderate-to-Vigorous-Intensity Physical Activity Per Week (MET-Min/Week)
Moderate-to-vigorous-intensity physical activity (MVPA) will be evaluated by the International Physical Activity Questionnaire (IPAQ) (Bassett, 2003). The IPAQ Questionnaire comprises 7 questions about the frequency and duration of vigorous activity (8 MET), moderate activity (4 MET), walking (3.3 MET), and sitting. The total physical activity will be calculated by multiplying the time (minutes per week) by the intensity [metabolic equivalent of task (MET) unit]. Its effectiveness in evaluating the physical activity level has been verified in various populations in China (Hu et al., 2015; Ren et al., 2017). Data processing principle: the cutoff value of the daily time of a certain intensity physical activity is 180 min; if the total daily time of three intensities physical activity is > 960 min (16 h), data will be excluded from the analysis; if the daily time of a certain intensity physical activity is < 10 min, the time and corresponding weekly frequency will be recorded as 0.
Psychological Condition
Patients’ psychological condition will be reflected by anxiety, depression, and sleep quality. Anxiety will be evaluated by the Generalized Anxiety Disorder 7-item (GAD-7) Scale within 7 questions and a total score of 0–21 (Spitzer et al., 2006). Depression will be assessed by the Patients Health Questionnaire 9-item (PHQ-9) within 9 questions and a total score of 0–27 (Kroenke et al., 2001). The Pittsburgh Sleep Quality Index (PSQI) will be used to evaluate the sleep quality in the last month, which consists of 19 self-report items and 5 other-report items; the 19th self-report item and 5 other-report items will not be scored. The total score ranged from 0 to 21; the higher the score, the worse the sleep (Liu et al., 2021).
Cognitive Function
The Mini-Mental State Examination (MMSE) is one of the standardized intelligence examination tools and is widely used in the screening of Alzheimer’s disease (Folstein et al., 1975). Cognitive function will be evaluated by testing their orientation, memory, attention, calculation, recall, and language ability. The total score is related to education level with a range of 0–30.
Adherence and Security
If 9 weeks and more reach to the target activity levels during the entire intervention period, it will be considered as good adherence. The incidence of adverse events, including falls and all-cause hospital admissions, will be assessed by patient self-report.
Other Secondary Outcomes
The difference between the percentage of walking speed < 0.6m/s, gait variability > 3%, frailty score ≥ 3, and low physical activity will also be compared.
Statistical Analysis
Categorical variables will be described by frequency and percentage. Continuous variables will be described by means and standard deviations. Social demographic and clinical data between the groups will be presented using appropriate descriptive statistics and evaluated for homogeneity using independent t-test, Mann-Whitney, chi-square, and Fisher’s exact tests, as appropriate. The differential changes of the primary and secondary outcomes at T1 and T2 concerning T0 between the two groups will be assessed using generalized estimating equations (GEE). The baseline variable will be adjusted, and group effects, time effects, and interaction effects will be observed. DSS statistics 25 will be used for data analysis, and P < 0.05 will be considered statistically significant.
Quality Control
Our research group has established a team of experienced clinical nurses and rehabilitation therapists at a rehabilitation center in Changchun, China. Experienced clinical nurses and researchers from the team will be responsible for recruiting participants. Participants meeting the inclusion criteria will be screened, they will be informed of the study details by the investigator, and if they agree to participate, they will be asked to sign a consent form. If there is a complex clinical problem, our researchers, nursing specialists, and rehabilitation therapists will work together to find a solution.
Discussion
The benefits of physical activity on the frail older adults have been widely recognized (Liu et al., 2018; Trombetti et al., 2018), but which part caused the improvement of health profile is still uncertain. Wearable devices have been widely used in healthcare (Chromik et al., 2022); however, it still needs to be further verified whether the remote evaluation of frailty (Angulo et al., 2020) and obtaining objective feedback can be realized. In this study, the IERMS will be used to intervene the physical activities to evaluate the changes in body performance, which will provide a new method for the remote assessment and supervision of the frail older adults living in the community.
During the COVID-19 pandemic, central-based or home-based face-to-face supervision has been forced to stop, and we need an alternative delivery mode (García Pérez de Sevilla et al., 2021). Remote assessment and guidance become the most feasible way (Liao et al., 2021). Although compared with traditional training, there is no significant difference in remote supervision, but it reached the same benefits at least (Geraedts et al., 2021; Gagnon et al., 2022). We will conduct a randomized controlled trail based on a digital platform, provide the personalized activity plan according to their own condition, and improve the compliance of schedule by increasing the interaction to ensure the intervention efficacy.
Multidimensional objective measurement reduces the subjective bias. Gait has been described as the “sixth vital sign” in recent years (Fritz and Lusardi, 2009). It is an integrative performance of body function with the complication of controlling walking and is associated with frailty (Montero-Odasso et al., 2011; Bortone et al., 2021). However, few wearable devices evaluate gait (Greene et al., 2014), due to the difficulty of obtaining gait parameters, even in today’s exponential development of digital health. Because of the lack of sensitivity and convenience, the existing methods of frail assessment are not suitable for wide-scale popularization. Through the use of smart insoles, we will be able to collect gait parameters continuously and dynamically. Gait analysis may become a new strategy to predict frailty.
However, this study still has certain limitations. First, the sample size is small and the population is limited to five communities in Changchun, so the results may not be fully promoted. Second, the training log is uploaded by the participants themselves, and there is still a certain problem with its authenticity. Finally, the body activity amount is calculated by the self-reported exercise form and metabolic equivalent, so there is a certain deviation in the calculation of exercise amount.
Conclusion and Implications
In general, we designed a personalized remotely supervised physical activity program and expected to add effect by increasing the participation. Based on the evidence, we are convinced that this intervention program will be able to delay or reverse the progress of frailty. If the intervention produces a significant positive effect, the findings will potentially provide valuable evidence and serve as convenient and feasible strategies for primary healthcare to promote healthy aging.
Ethics Statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee of the School of Nursing, Jilin University. The patients/participants will provide their written informed consent to participate in this study.
Author Contributions
XZ and FL: study concept and design. XZ, JL, TZY, XL, and TYY: acquisition of data. XZ, YP, and LZ: analysis and interpretation of data. XZ, FL, and LX: drafting of the manuscript. XS, HX, and YL: critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Innovative Research Plan for Graduate Students at Jilin University (Grant No. 101832020CX322).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank the valuable contribution made by the patients and public representatives during the study design and intervention development.
Footnotes
References
Angulo, J., El Assar, M., Álvarez-Bustos, A., and Rodríguez-Mañas, L. (2020). Physical activity and exercise: strategies to manage frailty. Redox Biol. 35:101513. doi: 10.1016/j.redox.2020.101513
Bassett, D. R. Jr. (2003). International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35:1396.
Bonnefoy, M., Boutitie, F., Mercier, C., Gueyffier, F., Carre, C., Guetemme, G., et al. (2012). Efficacy of a home-based intervention programme on the physical activity level and functional ability of older people using domestic services: a randomised study. J. Nutrition Health Aging 16, 370–377. doi: 10.1007/s12603-011-0352-6
Bortone, I., Sardone, R., Lampignano, L., Castellana, F., Zupo, R., Lozupone, M., et al. (2021). How gait influences frailty models and health-related outcomes in clinical-based and population-based studies: a systematic review. J. Cachexia Sarcopenia Muscle 12, 274–297. doi: 10.1002/jcsm.12667
Chan, P. P., Si Tou, J. I., Tse, M. M., and Ng, S. S. (2017). Reliability and validity of the timed up and go test with a motor task in people with chronic stroke. Arch. Phys. Med. Rehabil. 98, 2213–2220. doi: 10.1016/j.apmr.2017.03.008
Cheng, I. F., Kuo, L. C., Tsai, Y. J., and Su, F. C. (2021). The comparisons of physical functional performances between older adults with and without regular physical activity in two different living settings. Int. J. Environ. Res. Public Health 18:3561. doi: 10.3390/ijerph18073561
Choi, J., Ahn, A., Kim, S., and Won, C. W. (2015). Global prevalence of physical frailty by fried’s criteria in community-dwelling elderly with national population-based surveys. J. Am. Med. Dir. Assoc. 16, 548–550. doi: 10.1016/j.jamda.2015.02.004
Chromik, J., Kirsten, K., Herdick, A., Kappattanavar, A. M., and Arnrich, B. (2022). SensorHub: multimodal sensing in real-life enables home-based studies. Sensors (Basel) 22:408. doi: 10.3390/s22010408
de Labra, C., Guimaraes-Pinheiro, C., Maseda, A., Lorenzo, T., and Millán-Calenti, J. C. (2015). Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatrics 15:154. doi: 10.1186/s12877-015-0155-4
Dipietro, L., Campbell, W. W., Buchner, D. M., Erickson, K. I., Powell, K. E., Bloodgood, B., et al. (2019). Physical activity, injurious falls, and physical function in aging: an umbrella review. Med. Sci. Sports Exerc. 51, 1303–1313. doi: 10.1249/mss.0000000000001942
Eldridge, S. M., Chan, C. L., Campbell, M. J., Bond, C. M., Hopewell, S., Thabane, L., et al. (2016). CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 355:i5239. doi: 10.1136/bmj.i5239
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). Mini-mental state”. a practical method for grading the cognitive state of patients for the clinician. J. Psychiatric Res. 12, 189–198.
Fried, L. P., Tangen, C. M., Walston, J., Newman, A. B., Hirsch, C., and Gottdiener, J. (2001). Frailty in older adults: evidence for a phenotype. J. Gerontol. Med. Sci. 56A, M146–M156.
Fritz, S., and Lusardi, M. (2009). White paper: “walking speed: the sixth vital sign”. J. Geriatric Phys. Therapy 32, 46–49.
Gagnon, M. A., Sèbiyo Batcho, C., Bird, M. L., Labbé, B., and Best, K. L. (2022). Feasibility of a remotely supervised home-based group eHealth fitness and mobility exercise program for stroke: French-Canadian version preliminary study. Top. Stroke Rehabilitation Online ahead of print. doi: 10.1080/10749357.2021.2012008
García Pérez de Sevilla, G., Barceló Guido, O., De la Cruz, M. P., Fernández, A. B., Alejo, L. B., Ramírez Goercke, M. I., et al. (2021). Remotely supervised exercise during the COVID-19 pandemic versus in-person-supervised exercise in achieving long-term adherence to a healthy lifestyle. Int. J. Environ. Res. Public Health 18:12198. doi: 10.3390/ijerph182212198
Garcia-Moreno, F. M., Bermudez-Edo, M., Garrido, J. L., Rodríguez-García, E., Pérez-Mármol, J. M., and Rodríguez-Fórtiz, M. J. (2020). A microservices e-health system for ecological frailty assessment using wearables. Sensors (Basel) 20:3427. doi: 10.3390/s20123427
Geraedts, H. A. E., Dijkstra, H., Zhang, W., Ibarra, F., Far, I. K., Zijlstra, W., et al. (2021). Effectiveness of an individually tailored home-based exercise rogramme for pre-frail older adults, driven by a tablet application and mobility monitoring: a pilot study. Eur. Rev. Aging Phys. Act. 18:10. doi: 10.1186/s11556-021-00264-y
Greene, B. R., Doheny, E. P., O’Halloran, A., and Anne Kenny, R. (2014). Frailty status can be accurately assessed using inertial sensors and the TUG test. Age. Ageing 43, 406–411. doi: 10.1093/ageing/aft176
Hanlon, P., Nicholl, B. I., Jani, B. D., Lee, D., McQueenie, R., and Mair, F. S. (2018). Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health 3, e323–e332. doi: 10.1016/S2468-2667(18)30091-4
Hoogendijk, E. O., Afilalo, J., Ensrud, K. E., Kowal, P., Onder, G., and Fried, L. P. (2019). Frailty: implications for clinical practice and public health. Lancet 394, 1365–1375. doi: 10.1016/s0140-6736(19)31786-6
Hu, B., Lin, L. F., Zhuang, M. Q., Yuan, Z. Y., Li, S. Y., Yang, Y. J., et al. (2015). Reliability and relative validity of three physical activity questionnaires in Taizhou population of China: the Taizhou Longitudinal Study. Public Health 129, 1211–1217. doi: 10.1016/j.puhe.2015.03.024
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lacroix, A., Hortobágyi, T., Beurskens, R., and Granacher, U. (2017). Effects of supervised vs. unsupervised training programs on balance and muscle strength in older adults: a systematic review and meta-analysis. Sports Med. 47, 2341–2361. doi: 10.1007/s40279-017-0747-6
Lang, P. O., Michel, J. P., and Zekry, D. (2009). Frailty syndrome: a transitional state in a dynamic process. Gerontology 55, 539–549. doi: 10.1159/000211949
Liao, Y. Y., Chen, I. H., Hsu, W. C., Tseng, H. Y., and Wang, R. Y. (2021). Effect of exergaming versus combined exercise on cognitive function and brain activation in frail older adults: a randomised controlled trial. Ann. Phys. Rehabilitation Med. 64:101492. doi: 10.1016/j.rehab.2021.101492
Liu, D., Kahathuduwa, C., and Vazsonyi, A. T. (2021). The Pittsburgh Sleep Quality Index (PSQI): psychometric and clinical risk score applications among college students. Psychol. Assess. 33, 816–826. doi: 10.1037/pas0001027
Liu, Z., Hsu, F. C., Trombetti, A., King, A. C., Liu, C. K., Manini, T. M., et al. (2018). Effect of 24-month physical activity on cognitive frailty and the role of inflammation: the LIFE randomized clinical trial. BMC Med. 16:185. doi: 10.1186/s12916-018-1174-8
Mathias, S., Nayak, U. S., and Isaacs, B. (1986). Balance in elderly patients: the “get-up and go” test. Arch. Phys. Med. Rehabil. 67, 387–389.
Montero-Odasso, M., Muir, S. W., Hall, M., Doherty, T. J., Kloseck, M., Beauchet, O., et al. (2011). Gait variability is associated with frailty in community-dwelling older adults. J. Gerontol. Series A: Biol. Sci. Med. Sci. 66, 568–576. doi: 10.1093/gerona/glr007
Mugueta-Aguinaga, I., and Garcia-Zapirain, B. (2019). Frailty level monitoring and analysis after a pilot six-week randomized controlled clinical trial using the FRED exergame including biofeedback supervision in an elderly day care centre. Int. J. Environ. Res. Public Health 16:729. doi: 10.3390/ijerph16050729
Ren, Y. J., Su, M., Liu, Q. M., Tan, Y. Y., Du, Y. K., Li, L. M., et al. (2017). Validation of the simplified chinese-character version of the international physical activity questionnaire-long form in urban community-dwelling adults: a cross-sectional study in Hangzhou. China. Biomed. Environ. Sci. 30, 255–263. doi: 10.3967/bes2017.035
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Suikkanen, S., Soukkio, P., Aartolahti, E., Kaaria, S., Kautiainen, H., Hupli, M. T., et al. (2021). Effect of 12-Month supervised, home-based physical exercise on functioning among persons with signs of frailty: a randomized controlled trial. Arch. Phys. Med. Rehabil. 102, 2283–2290. doi: 10.1016/j.apmr.2021.06.017
Theou, O., Blodgett, J. M., Godin, J., and Rockwood, K. (2017). Association between sedentary time and mortality across levels of frailty. CMAJ: Canadian Med. Assoc. J. 189, E1056–E1064. doi: 10.1503/cmaj.161034
Trombetti, A., Hars, M., Hsu, F. C., Reid, K. F., Church, T. S., Gill, T. M., et al. (2018). Effect of physical activity on frailty: secondary analysis of a randomized controlled trial. Ann. Intern. Med. 168, 309–316. doi: 10.7326/m16-2011
van der Ploeg, H. P., and Bull, F. C. (2020). Invest in physical activity to protect and promote health: the 2020 WHO guidelines on physical activity and sedentary behaviour. Int. J. Behav. Nutrition Phys. Act. 17:145. doi: 10.1186/s12966-020-01051-1
Xu, L., Xiong, W., Li, J., Shi, H., Shen, M., Zhang, X., et al. (2020). Role of the intelligent exercise rehabilitation management system on adherence of cardiac rehabilitation in patients with coronary heart disease: a randomised controlled crossover study protocol. BMJ Open 10:e036720. doi: 10.1136/bmjopen-2019-036720
Yuksel, E., Kalkan, S., Cekmece, S., Unver, B., and Karatosun, V. (2017). Assessing minimal detectable changes and test-retest reliability of the timed up and go test and the 2-minute walk test in patients with total knee arthroplasty. J. Arthroplasty 32, 426–430. doi: 10.1016/j.arth.2016.07.031
Zaccardi, F., Davies, M. J., Khunti, K., and Yates, T. (2019). Comparative relevance of physical fitness and adiposity on life expectancy: a UK biobank observational study. Mayo Clin. Proc. 94, 985–994. doi: 10.1016/j.mayocp.2018.10.029
Keywords: remotely supervised, physical activity, intelligent system, frailty, health profile
Citation: Zhang X, Li J, Sui X, Xu L, Zhu L, Pang Y, Yu T, Lian X, Yu T, Li Y, Xu H and Li F (2022) Effects of Remotely Supervised Physical Activity on Health Profile in Frail Older Adults: A Randomized Controlled Trial Protocol. Front. Aging Neurosci. 14:807082. doi: 10.3389/fnagi.2022.807082
Received: 01 November 2021; Accepted: 09 February 2022;
Published: 31 March 2022.
Edited by:
Mario Bernardo-Filho, Rio de Janeiro State University, BrazilReviewed by:
Eduardo Carballeira, University of A Coruña, SpainAlan Lins Fernandes, University of São Paulo, Brazil
Gülistan Bahat, Istanbul University, Turkey
Copyright © 2022 Zhang, Li, Sui, Xu, Zhu, Pang, Yu, Lian, Yu, Li, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Li, ZmxpQGpsdS5lZHUuY24=
 Xin Zhang
Xin Zhang Jinwei Li
Jinwei Li Feng Li
Feng Li