
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CORRECTION article
Front. Aging Neurosci. , 16 February 2023
Sec. Neuroinflammation and Neuropathy
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.1120252
This article is a correction to:
Type 2 Diabetes Increases Risk of Unfavorable Survival Outcome for Postoperative Ischemic Stroke in Patients Who Underwent Non-cardiac Surgery: A Retrospective Cohort Study
 Faqiang Zhang1,2
Faqiang Zhang1,2 Yulong Ma2
Yulong Ma2 Yao Yu2
Yao Yu2 Miao Sun2
Miao Sun2 Hao Li2
Hao Li2 Jingsheng Lou2
Jingsheng Lou2 Jiangbei Cao2
Jiangbei Cao2 Yanhong Liu2
Yanhong Liu2 Mu Niu3*†
Mu Niu3*† Long Wang4*†
Long Wang4*† Weidong Mi1,2*†
Weidong Mi1,2*†by Zhang, F., Ma, Y., Yu, Y., Sun, M., Li, H., Lou, J., Cao, J., Liu, Y., Niu, M., Wang, L., and Mi, W. (2022). Front. Aging Neurosci. 13:810050. doi: 10.3389/fnagi.2021.810050
In the original article, there was an error in the section Results, Baseline Characteristics of Patients, Paragraph 1. The number of the patients without follow-up data has an input error. The corresponding N number for “patients without follow-up data” was given as 72, but should be 76. The corrected Paragraph 1 appears below.
From January 1, 2008, to August 31, 2019, at Chinese PLA General Hospital, a total of 2,21,541 patients who underwent non-cardiac surgery were included, of whom 484 (0.22%) patients were diagnosed to have an ischemic stroke within 30 days after surgery. After excluding 76 patients without follow-up data, 408 of 484 (84.3%) eligible patients with postoperative ischemic stroke remained in the cohort, of whom 113 (27.7%) had DM (Figure 1). During a median follow-up of 46.2 months (IQR: 21.1, 84.2), the overall all-cause mortality was 49.0% (200/408).
In the original article, there was an error in Figure 1. The number of the patients without follow-up data has an input error. The corresponding N number for “patients without follow-up data” was given as 72, but should be 76. The corrected Figure 1 appears below.
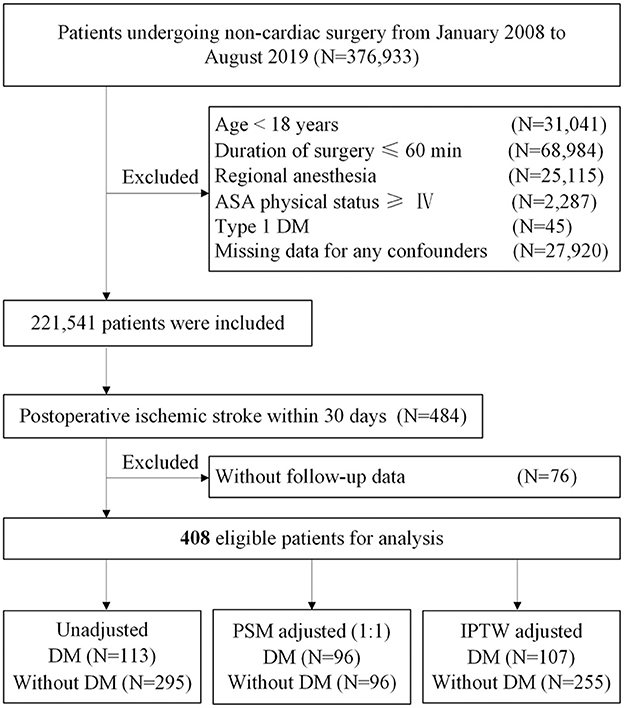
Figure 1. Study flow diagram. ASA, American Society of Anesthesiologists; DM, diabetes mellitus; PSM, propensity score matching; IPTW, inverse probability treatment weighting.
In the original article, there was an error in the section Research Design and Methods, “Exposure of Interest and Covariates,” paragraph 3. The definition of postoperative ischemic stroke was incomplete. The corrected paragraph appears below.
Postoperative ischemic stroke is defined as a brain infarction of ischemic etiology with motor, sensory, or cognitive dysfunction (e.g., hemiplegia, hemiparesis, aphasia, sensory deficit, and impaired memory) 30 days after surgery (Mashour et al., 2011; Sacco et al., 2013; Vlisides and Moore, 2021). Diagnoses of stroke are confirmed by a combination of neuroimaging and clinical evidence of cerebrovascular ischemia during hospital stay. Preoperative MAP was determined on the first blood pressure in the operation room. Stroke laterality, stroke location, and LHI were suggested by CT or MRI. LHI was defined as follow: (1) suffered from >1/3 infarction of the middle cerebral artery (MCA) territory within 6 h after the onset of stroke (or >1/2 MCA territory from 6 h to 7 days after onset) by the assessment of CT scan, (2) exceeded 80 ml within 6 h after the onset of stroke (or 145 ml within 14 h after onset) for infarction volume by appraisal of the MRI), and (3) suffered from >3 cm infarction of cerebellar region on the MRI (Sheth et al., 2016; Vorasayan et al., 2019). In the original article, there was a mistake in the section Discussion, Paragraph 4. Discussion, Paragraph 4 is a duplicate of Discussion, Paragraph 3 and should be deleted.
In the original article, there was a mistake in Figure 4 as published. The death cases of follow-up time >18.5 months subgroup have input errors. The corresponding n number for “Patients without DM and Death cases” was given as 232 (70), but should be 232 (69). In addition, the corresponding n number for “Patients with DM and Death cases” was 81 (39) but should be 81 (42). The revised Figure 4 appears below.
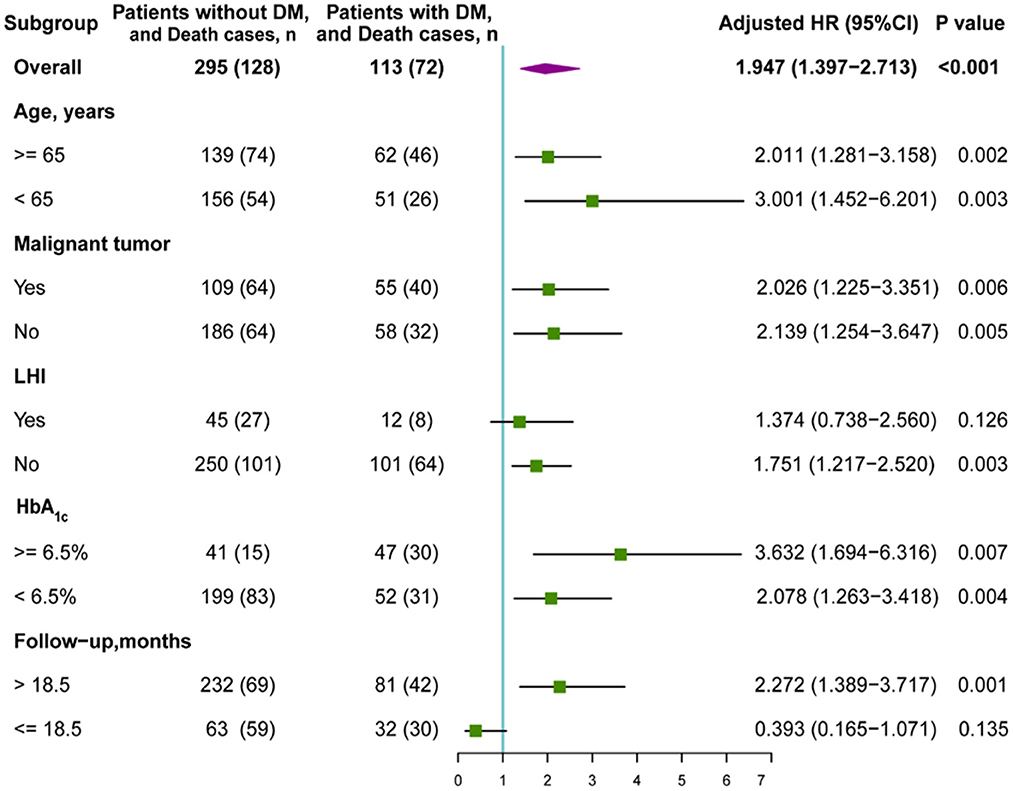
Figure 4. Subgroup analysis of the association between DM and overall survival (OS). HR, hazard ratio; DM, diabetes mellitus; LHI, large hemispheric infarction.
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Mashour, G. A., Shanks, A. M., and Kheterpal, S. (2011). Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology 114, 1289–1296. doi: 10.1097/ALN.0b013e318216e7f4
Sacco, R. L., Kasner, S. E., Broderick, J. P., Caplan, L. R., Connors, J. J., Culebras, A., et al. (2013). An updated definition of stroke for the 21st century: a statement for healthcare professionals from the american heart association/american stroke association. Stroke 44, 2064–2089. doi: 10.1161/STR.0b013e318296aeca
Sheth, K., Elm, J., Molyneaux, B., Hinson, H., Beslow, L., Sze, G., et al. (2016). Safety and efficacy of intravenous glyburide on brain swelling after large hemispheric infarction (GAMES-RP): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 15, 1160–1169. doi: 10.1016/s1474-4422(16)30196-x
Vlisides, P. E., and Moore, L. E. (2021). Stroke in surgical patients. Anesthesiology 134, 480–492. doi: 10.1097/ALN.0000000000003664
Keywords: type 2 diabetes mellitus (type 2 DM), overall survival, perioperative stroke, postoperative complications, large hemispheric infarction (LHI)
Citation: Zhang F, Ma Y, Yu Y, Sun M, Li H, Lou J, Cao J, Liu Y, Niu M, Wang L and Mi W (2023) Corrigendum: Type 2 diabetes increases risk of unfavorable survival outcome for postoperative ischemic stroke in patients who underwent non-cardiac surgery: A retrospective cohort study. Front. Aging Neurosci. 14:1120252. doi: 10.3389/fnagi.2022.1120252
Received: 09 December 2022; Accepted: 30 December 2022;
Published: 16 February 2023.
Edited and reviewed by: Yu-Min Kuo, National Cheng Kung University, Taiwan
Copyright © 2023 Zhang, Ma, Yu, Sun, Li, Lou, Cao, Liu, Niu, Wang and Mi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mu Niu,  eHp5eHlubUAxNjMuY29t; Long Wang,
eHp5eHlubUAxNjMuY29t; Long Wang,  Zmx5bm4ueHVAMTYzLmNvbQ==; Weidong Mi,
Zmx5bm4ueHVAMTYzLmNvbQ==; Weidong Mi,  d3dkZDE5NjJAYWxpeXVuLmNvbQ==
d3dkZDE5NjJAYWxpeXVuLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.