
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Aging Neurosci., 22 December 2022
Sec. Neurocognitive Aging and Behavior
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.1068278
This article is part of the Research TopicPost-Operative Neuropsychiatric DisorderView all 15 articles
Postoperative delirium (POD) is a frequent complication in geriatric patients with hip fractures, which is linked to poorer functional recovery, longer hospital stays, and higher short-and long-term mortality. Patients with increased age, preoperative cognitive impairment, comorbidities, perioperative polypharmacy, and delayed surgery are more prone to develop POD after hip fracture surgery. In this narrative review, we outlined the latest findings on postoperative delirium in geriatric patients with hip fractures, focusing on its pathophysiology, diagnosis, prevention, and treatment. Perioperative risk prediction, avoidance of certain medications, and orthogeriatric comprehensive care are all examples of effective interventions. Choices of anesthesia technique may not be associated with a significant difference in the incidence of postoperative delirium in geriatric patients with hip fractures. There are few pharmaceutical measures available for POD treatment. Dexmedetomidine and multimodal analgesia may be effective for managing postoperative delirium, and adverse complications should be considered when using antipsychotics. In conclusion, perioperative risk intervention based on orthogeriatric comprehensive care is the most effective strategy for preventing postoperative delirium in geriatric patients with hip fractures.
Osteoporotic hip fracture is an important public health concern, with a reported one-year mortality of 12.7% in geriatric patients (Aharonoff et al., 1997). It affects women more frequently than males (Brauer et al., 2009), most likely because post-menopausal women have a higher incidence of osteoporosis (Cummings and Melton, 2002). Hip fracture in geriatric patients is linked to poor functional prognosis and a high frequency of postoperative complications, such as postoperative delirium (POD), pneumonia, urinary tract infections, deep vein thrombosis, and bleeding (Fischer et al., 2021; Schrøder et al., 2022). A third of geriatric patients encounter one or more postoperative complications, and 7.2% of patients experience multiple complications (Merchant et al., 2005). It is reported that compared with senior patients without fractures, those with hip fractures had a higher rate of postoperative mental problems (Kuo et al., 2021).
Postoperative delirium (POD) is one of the most common complications in geriatric patients with hip fractures (Merchant et al., 2005). It is a postoperative cognitive disturbance defined by abrupt and variable impairment in attention and awareness, with reported incidences varying from 4.7 to 74% (Maldonado, 2017; Flikweert et al., 2018; Connolly et al., 2020). POD usually occurs between postoperative days 2–5 (Jin et al., 2020). When patients develop POD, it is usually the most distressing component of the perioperative experience, adding to their personal, medical, and financial burdens (Leslie et al., 2008). POD is associated with increased hospital length of stay (Hecht et al., 2019), poor rehabilitation outcomes, such as impaired functional and cognitive recovery, even the onset of new dementia (Low et al., 2021; Meyer et al., 2021; Pereira et al., 2021), worsened mobility (Ouellet et al., 2019), and a higher risk of both short-term and long-term mortality (Bai et al., 2020; Liu et al., 2021). Additionally, postoperative delirium is a strong indicator for nursing home admission (de Jong et al., 2019). In light of these poor consequences and the high prevalence of POD in geriatric patients with hip fractures, early identification of patients at risk as well as implementation of prophylactic measures to reduce the frequency of POD is extremely desirable (Smith et al., 2017). The underlying pathophysiology of postoperative delirium in geriatric patients with hip fractures is still unclear, most studies focus on the involvement of neuroinflammation, neurotransmitters, and metabolism abnormality. Currently, there are still few effective measures for POD treatment. The most effective approach to preventing POD is to minimize its risk factors, and several risk prediction tools have been developed for risk stratification in geriatric patients with hip fractures. Additionally, avoidance of perioperative benzodiazepine administration and comprehensive multidisciplinary care play a significant role in POD management.
This review aims to describe current research advances on postoperative delirium in geriatric patients with hip fractures and to provide effective and feasible strategies for the prevention and treatment of POD.
Despite that the prevalence of POD in the general surgical population is only 2–3%, it can occur in up to 50–70% of high-risk patient groups (Watne et al., 2016). In particular, hip fracture surgery is associated with up to 70–80% risk of postoperative delirium. There are several reasons for this: a hip fracture is frequently seen in elderly patients who are frail; perioperative pain is a major concern; and the surgery is typically performed in an emergency setting with little chance for preoperative optimization (Jin et al., 2020).
The perioperative risk factors for POD in geriatric patients with hip fractures can be predisposing and precipitating. As is shown in the literature (Smith et al., 2017; Swarbrick and Partridge, 2022; Wittmann et al., 2022), predisposing risk factors include increased age, sensorial deficits, prior cognitive impairment, multimorbidity, malnutrition, and frailty, as well as precipitating risk factors including surgical procedures, ventilation time, and intensive care stay. In addition, there are also several independent predictors for POD in geriatric patients with hip fractures (Koskderelioglu et al., 2017; Mosk et al., 2017; Smith et al., 2017; Yang et al., 2017; Wang et al., 2018; Chen et al., 2020; Tantardini et al., 2020; Xing et al., 2020; Zhou et al., 2021; Table 1).
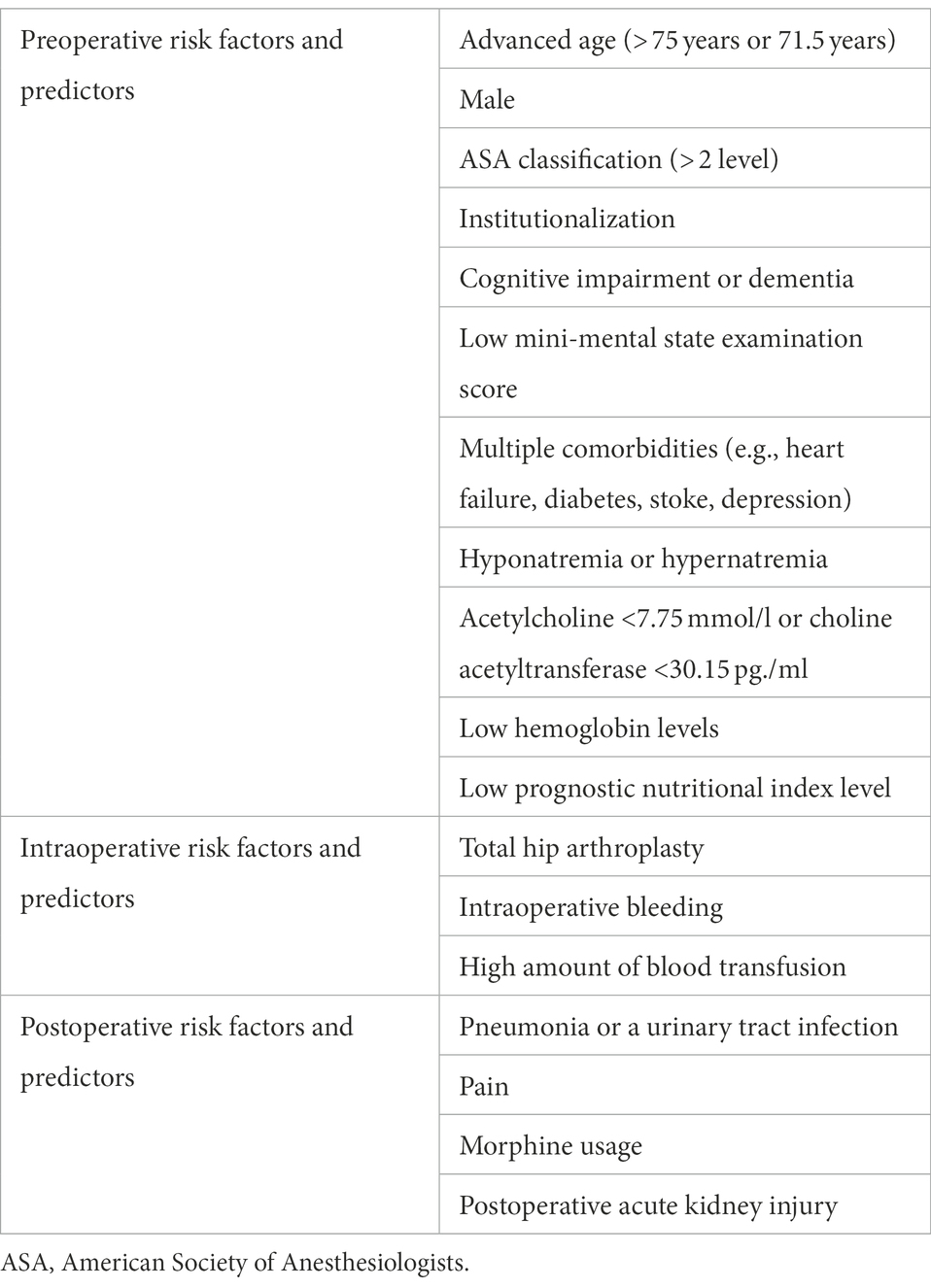
Table 1. Risk factors and predictors for postoperative delirium in geriatric patients with hip fractures.
Increased age is an independent risk factor associated with POD in geriatric patients with hip fractures. Patients older than 71.5 years of age with hip fractures have a more than threefold increased risk of developing postoperative delirium (Xing et al., 2020), and the hypoactive subtype is more likely to develop in people over the age of 80 (Stagno et al., 2004). This may be because the risk of endothelial dysfunction and atherosclerosis increases with age, putting elderly patients at increased risk of cerebral embolism (Rudolph et al., 2009). Additionally, the age-related loss of cholinergic reserve is also a significant contributor. Interestingly, males are more prone to develop delirium after hip fracture surgery (Yang et al., 2017; Haynes et al., 2021), despite women having a larger frequency of hip fractures (Edelstein et al., 2004). A 20–45% risk of postoperative delirium is linked to emergency surgery, which is 1.5–3 times higher than the risk for comparable elective surgery (Ansaloni et al., 2010; Chaiwat et al., 2019). Surgery type may have an influence on POD in geriatric patients with hip fractures. Patients who underwent total hip arthroplasty were more likely to develop POD (OR 2.21; 95% CI 1.16–4.22; Bruce et al., 2007; Yang et al., 2017). The location of the fracture (transcervical fracture, intertrochanteric fracture, and subtrochanteric fracture) seems has no association with the occurrence of POD, according to existing literature (Smith et al., 2017; Xing et al., 2020). Preoperative dementia is also an independent risk factor for POD in elderly patients with hip fractures. Moreover, postoperative delirium plays moderation and mediation effects between preoperative dementia and postoperative adverse events. The effects of preoperative dementia on mortality, readmission, and revision surgery were dramatically enhanced by postoperative delirium (Haynes et al., 2021). ASA physical status classes 2 and 3 and the number of medical comorbidities were significant variables in assessing the risk of POD. The modified Charlson’s Comorbidity Index (CCI) is a commonly used tool for assessment of medical comorbidities (Charlson et al., 1987). It is reported that 94% of hip fracturs patients with POD were associated with at least a medical complication (Mullen and Mullen, 1992). Postoperative infection, such as urinary tract infection and pneumonia, can also increase the POD risk in hip fracture patient. It may cause significant delays in cognitive processing speed, especially when it comes to memory retrieval (Bucks et al., 2008). Additionally, the risk of developing POD is increased by impaired vision or hearing because the elderly person cannot properly perceive the stimuli in the hospital environment (Staus, 2011).
The pathophysiology of postoperative delirium in elderly patients with hip fractures has not been entirely explored yet, and widely accepted hypotheses focus on the involvement of neuroinflammation, neurotransmitters, and metabolic abnormality.
One generally accepted pathophysiological explanation for postoperative delirium in elderly patients with hip fractures is neuroinflammation (Figure 1). Surgical injuries act on Toll-like receptors through damage-associated molecular patterns or pathogen-associated molecular patterns to initiate an intracellular inflammatory response, and inflammatory mediators such as TNF - α are released into the brain, causing aseptic inflammation in the CNS, resulting in POD (Alam et al., 2018). Previous studies have shown that trauma caused by fracture and surgery is associated with increased perioperative systemic inflammatory mediators (Cape et al., 2014; Neerland et al., 2016). These peripheral inflammatory mediators are transported to the brain via three primary pathways: (a) Peripheral inflammation causes the loss of structural and functional integrity of the blood–brain barrier. Thus, inflammatory factors can cross the blood–brain barrier and enter the brain through capillary epithelial cells (Yang et al., 2017); (b) There are transporters in the afferent nerves of the vagus, which can directly transport the peripheral inflammatory substances to the corresponding nerve nuclei; (c) The increased concentration of inflammatory factors in plasma makes it possible for the inflammatory mediators to diffuse to brain tissue through the concentration gradient. The accumulation of central inflammatory mediators leads to the disruption of the large-scale neural networks in the brain, such as suppression of hippocampal plasticity and neurogenesis (Ekdahl et al., 2003; Prieto et al., 2019), neurotoxicity, and neuronal apoptosis (Tian et al., 2018). These damages ultimately result in the occurrence and progress of POD.
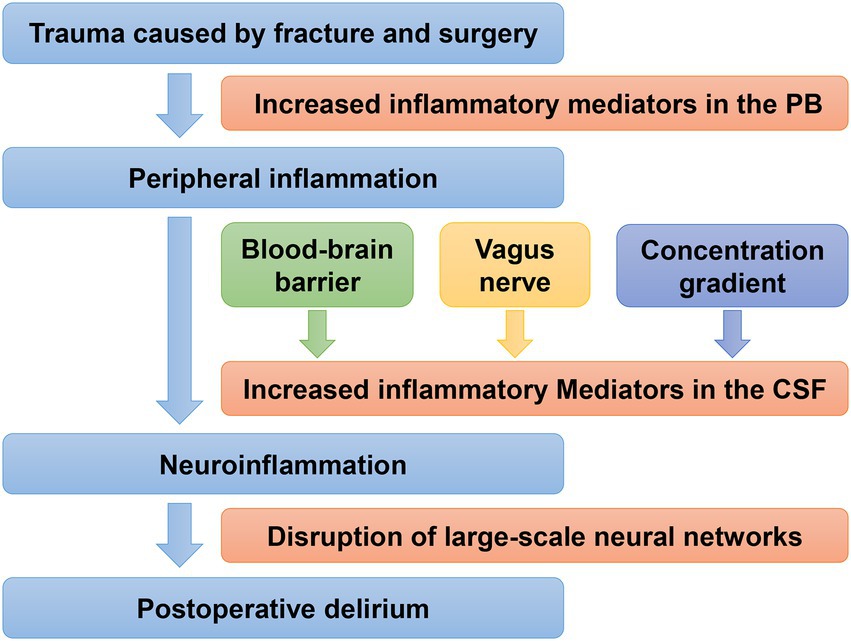
Figure 1. Neuroinflammation mechanism of postoperative delirium in geriatric patients with hip fractures. PB, peripheral blood; CSF, cerebrospinal fluid. Trauma caused by fracture and surgery is associated with increased systemic inflammatory mediators, which are transported from the periphery to the brain via three primary pathways, resulting in neuroinflammation, and finally lead to POD.
The alteration in neurotransmitters is also a possible mechanism for the occurrence and development of POD, among which the most prominent is the deficiency or dysfunction of the cholinergic system (Adam et al., 2020). A prospective observational study demonstrated that the level of acetylcholine in the cerebral spinal fluid was significantly decreased in geriatric patients with postoperative cognitive dysfunction (Chen et al., 2020). Moreover, the cholinergic system interacts significantly with other neurotransmitter systems, and POD is also correlated with the malfunction of these other neurotransmitter systems. Particularly, acetylcholine deficiency is accompanied by an excess of dopamine, which is linked to critical postoperative delirium (Trzepacz, 2000). However, a randomized controlled trial of 261 patients found that postoperative administration of physostigmine did not affect the prevention of POD after liver resection (Spies et al., 2021), which may indicate the underlying mechanisms leading to neurotransmitter alterations still need to be explored to find effective drug targets.
Postoperative delirium is more likely to occur in elderly patients with neurovascular changes. A review explored the association of neurodegenerative and neurovascular changes with the occurrence of POD (Kant et al., 2017), and it found that neurovascular changes, such as white-matter hyperintensities (Hatano et al., 2013; Root et al., 2013), preoperative old cerebral infarct (Otomo et al., 2013; Maekawa et al., 2014) and markers of white matter integrity (Shioiri et al., 2010; Cavallari et al., 2016), appear to be consistently associated with the occurrence of POD. Furthermore, these changes may even help to identify patients at increased risk of POD. Kyeong et al. (2018) developed a prediction model for estimating the probability of POD in geriatric patients with femoral neck fractures, with a correct classification rate of 86%. This model consists of three neural predisposing factors: the neuroticism score, the amplitude of low-frequency fluctuation in the dorsolateral prefrontal cortex, and the density of gray matter in the caudate or suprachiasmatic nucleus. It may accurately predict the likelihood of postoperative delirium by reflecting the fundamental pathophysiology.
Metabolic abnormality is shown to be associated with the occurrence and progression of POD. In a metabonomic study of geriatric hip fracture patients, it was discovered that, while glycolysis products were higher in POD patients after surgery, levels of ω3 and ω6 fatty acids were lower in those both before and after surgery, as well as intermediate levels of the tricarboxylic cycle and the branched-chain amino acid/aromatic amino acid ratio (Guo et al., 2019). These metabolic abnormalities most likely reduce the ability of the brain to provide neuroprotection and take part in neuroinflammatory responses. Another study applied untargeted metabolomics techniques to investigate the change of serum metabolites in POD patients undergoing cardiopulmonary bypass, and found that low serum lipid metabolic phosphatidylinositol was linked to an increased risk of POD in the geriatric patient, which may shed fresh light on the pathophysiology of POD (Huang et al., 2022).
High clinical significance can result from the identification of predictive biomarkers that allow for early risk stratification of hip fracture patients who are vulnerable to POD. The incidence and severity of POD in hip fracture patients were associated with higher levels of white blood cells, neutrophil/lymphocyte ratio, neutrophil percentage, and lower levels of mean platelet volume and basophil percentage (Thisayakorn et al., 2021; Li et al., 2022), which further demonstrated that immune-inflammatory processes are involved in the pathophysiology of POD. Prognostic Nutritional Index (PNI) is a convenient and accurate way to quantify nutritional status, and it was calculated as 10 × albumins (g/dl) + 0.005 × total lymphocyte count (per mm3; Onodera et al., 1984). It is reported that lower preoperative PNI value (cut-off value: 47.45, sensitivity: 86.0%, specificity: 51.9%, OR: 2.88, 95% CI: 1.25–6.64, p = 0.012) was associated with increased POD risk in geriatric patients with hip fractures, and it was a predictor for POD with an area under the curve of 0.686 (95% CI: 0.604–0.767, p < 0.001; Xing et al., 2020). The neuropeptide galanin is a neuromodulator ubiquitously present in the central and peripheral nervous systems as well as nonneural tissues, and its levels are abnormally high in depressive and dementia-like diseases (Counts et al., 2001; Alexandris et al., 2015). It is reported that the increased serum neuropeptide galanin level can predict postoperative cognitive dysfunction in geriatric patients with hip fractures (p = 0.035). However, the association between serum neuropeptide galanin level and POD in geriatric patients with hip fractures has not been investigated yet.
In the current, the diagnosis of postoperative delirium in geriatric patients with hip fractures mainly relies on clinical characteristics. Patients with POD frequently exhibit either hyperactive or hypoactive types, or a mixed type, which alternates between these motor subtypes (Vlisides and Avidan, 2019). The hypoactive type is more prevalent in elderly people, frequently goes undiagnosed, and is linked to higher rates of other postoperative complications and mortality (Oh et al., 2017). Additionally, in the clinical setting, the workload of clinicians is so high that it is difficult to detect POD in time, so the underdiagnosis rate of delirium remains high. Studies found a delirium underdiagnosis rate of 60% in elderly patients with cancer and an even higher rate of 84.6% in elderly patients in the emergency setting (de la Cruz et al., 2015; Boucher et al., 2019).
Delirium has been defined as a disturbance in attention and consciousness based on the following standards in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5; American Psychiatric Association, 2013; European Delirium Association, American Delirium Society, 2014): (A) Disturbance in attention (i.e., reduced ability to focus, sustain, or shift attention) and awareness (reduced orientation to the environment); (B) The disturbance develops over a short period (usually hours to a few days), represents an acute change from baseline attention and awareness, and tends to fluctuate in severity during the course of the day; (C) An additional disturbance in cognition (e.g., memory deficit, disorientation, language, visuospatial ability, or perception); (D) The disturbances in Criteria A and C are not better explained by a pre-existing, established, or evolving neurocognitive disorder and do not occur in the context of a severely reduced level of arousal such as a coma; (E) There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal (i.e., due to a drug of abuse or to a medication), or exposure to a toxin, or is due to multiple etiologies.
Prompt diagnosis of delirium in geriatric patients with hip fractures is the first key step in its appropriate treatment, and the diagnosis approaches in these patients must be convenient and easy to operate. The widely used instrument for POD diagnosis in the clinical setting is the confusion assessment method (CAM) developed in 1990, which is a bedside structured interview with the patient (Inouye et al., 1990). It concentrates on the most notable clinical characteristics of delirium: (1) acute change in mental status with a fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. To make the diagnosis of delirium, (1) and (2) must be present, and the patient must have signs of either (3) or (4). Additionally, in the intensive care unit (ICU) setting, POD is often diagnosed using CAM-ICU, a 2-min version of CAM that is convenient to use and highly accurate (Ely et al., 2001; Heo et al., 2011).
The Mini-mental state examination (MMSE) is also a wildly used instrument for the diagnosis of POD. It is intended to assess abilities related to orientation, memory, attention, object identification, compliance with verbal and written instructions, free writing of sentences, and copying complicated polygons (Folstein et al., 1975). The Organic brain syndrome (OBS) scale mainly assesses two dimensions: disorientation and confusion. A disorientation subscale based on an interview describes the patient’s capacity for time, place, and self-identity orientation; a confusion subscale based on the researcher’s or the nursing staff’s observations that assess a variety of cognitive, perceptual, emotional, and personality alterations, as well as physical and practical impairments, and variations in the clinical condition (Berggren et al., 1987).
There is a study that compared 11 instruments for delirium assessment, and it found that the CAM is the best bedside delirium assessment tool, which takes 5 min to administer, while the MMSE (score < 24) is the least useful for identifying a patient with delirium (Wong et al., 2010). Furthermore, Marcantonio et al. (2014) have developed a 3-min diagnostic interview based on the CAM, called 3D-CAM, which assesses 4 CAM features with cognitive tests, patients question, and interviewer observation. It was demonstrated to have good sensitivity [95% (84, 99%)] and specificity [94% (90, 97%)] in comparison to a reference standard, and was shown to be effective in POD diagnosis in geriatric patients with hip fractures (Neuman et al., 2021).
Increasing evidence indicates that delirium, as well as its severity, is associated with worse outcomes (de Miguel et al., 2018; Sieber et al., 2018). It is vital to measure delirium severity to assess prognosis and to monitor treatment response. The most frequently used instruments to rate the severity of POD include the Confusion Assessment Method-Severity (CAM-S; Inouye et al., 2014), the Delirium Rating Scale-Revised-98 (DRS-R-98; de Rooij et al., 2006), and the Memorial Delirium Assessment Scale (MDAS) (Breitbart et al., 1997). The same fundamental concept of delirium severity is measured by each of these delirium instruments, with a high degree of correlation (Gross et al., 2018).
However, postoperative delirium is characterized by acute onset and recurrent fluctuations. It is difficult for the bedside assessment instruments such as the CAM-S to dynamically grasp the recurrent fluctuations, and the accuracy of these scales in assessing POD depends on the training level of assessors. Furthermore, it is demonstrated that the electrocardiogram (ECG) slowing, such as a composite of generalized theta or delta slowing (OR 10.3, 95% CI, and 5.3–20.1), is associated with delirium severity and poor clinical outcomes (Kimchi et al., 2019). Recently, an automated physiologic process that quantifies the presence and severity of delirium directly has been reported, called the Electroencephalographic Confusion Assessment Method Severity Score (E-CAM-S; van Sleuwen et al., 2022). It is based on a learning-to-rank machine learning model of forehead electroencephalography signals, with a level of performance comparable to conventional interview-based clinical assessment. Tesh et al. (2022) developed the Visual EEG Confusion Assessment Method Severity (VE-CAM-S) for the diagnosis of delirium severity, which was strongly associated with clinically important outcomes. Those ECG-based assessment methods may help close the delirium diagnostic gap and develop more effective delirium treatments and prevention strategies.
Hitherto, there is still no effective strategy to treat POD in geriatric patients with hip fractures, and studies on the management of postoperative delirium mainly concentrate on its precautions. According to a 2020 meta-analysis, 91% of trials about POD focused on prevention and only 9% on its treatment (Pieri et al., 2020). The prevention and treatment measures of POD in geriatric patients with hip fractures can be divided into non-pharmacological and pharmacological interventions.
Early identification of hip fracture patients with POD risk and adoption of effective intervention are important to prevent the occurrence and development of POD. The risk factors and predictors of POD in geriatric patients with hip fractures are listed in Table 1. Clinicians should be vigilant for POD in patients who present with these features during the perioperative period. In recent years, a variety of risk prediction models have been developed to predict POD risk in geriatric patients with hip fractures (Kim et al., 2020; Oberai et al., 2021; Shen et al., 2022; Table 2), which enable delirium risk stratification for hip fracture patients and facilitate the development of strategies for POD. Adapted from the AWOL (Age, WORLD backward, Orientation, illness severity) delirium prediction tool for medical inpatients Douglas et al. (2013), Whitlock et al. (2020) developed a perioperative delirium risk stratification tool called AWOL-S (Age, WORLD backward, Orientation, illness severity, Surgery-specific risk) for elective surgical patients. The AWOL-S tool shows a moderate level of accuracy for delirium prediction in patients undergoing elective surgery, with 75% sensitivity and 59% specificity. According to its procedure-specific delirium risk score, hip fracture surgery belongs to the high-risk level, which needs continuing delirium prevention interventions after discharge from anesthesia care. Bishara et al. (2022) developed a delirium risk prediction model based on machine learning, which demonstrated excellent calibration compared with models developed with traditional logistic regression. It is not limited by time and space and can be repeated and standardized to assess patients. However, the incidence of POD in this study (5.3%) was lower than commonly reported POD rates, which may be owing to the inclusion of a younger population and all procedures, even those considered to have a low risk of delirium, such as gynecologic, urologic and plastics. Future studies could validate the sensitivity and specificity of this model specifically in elderly patients with hip fractures.
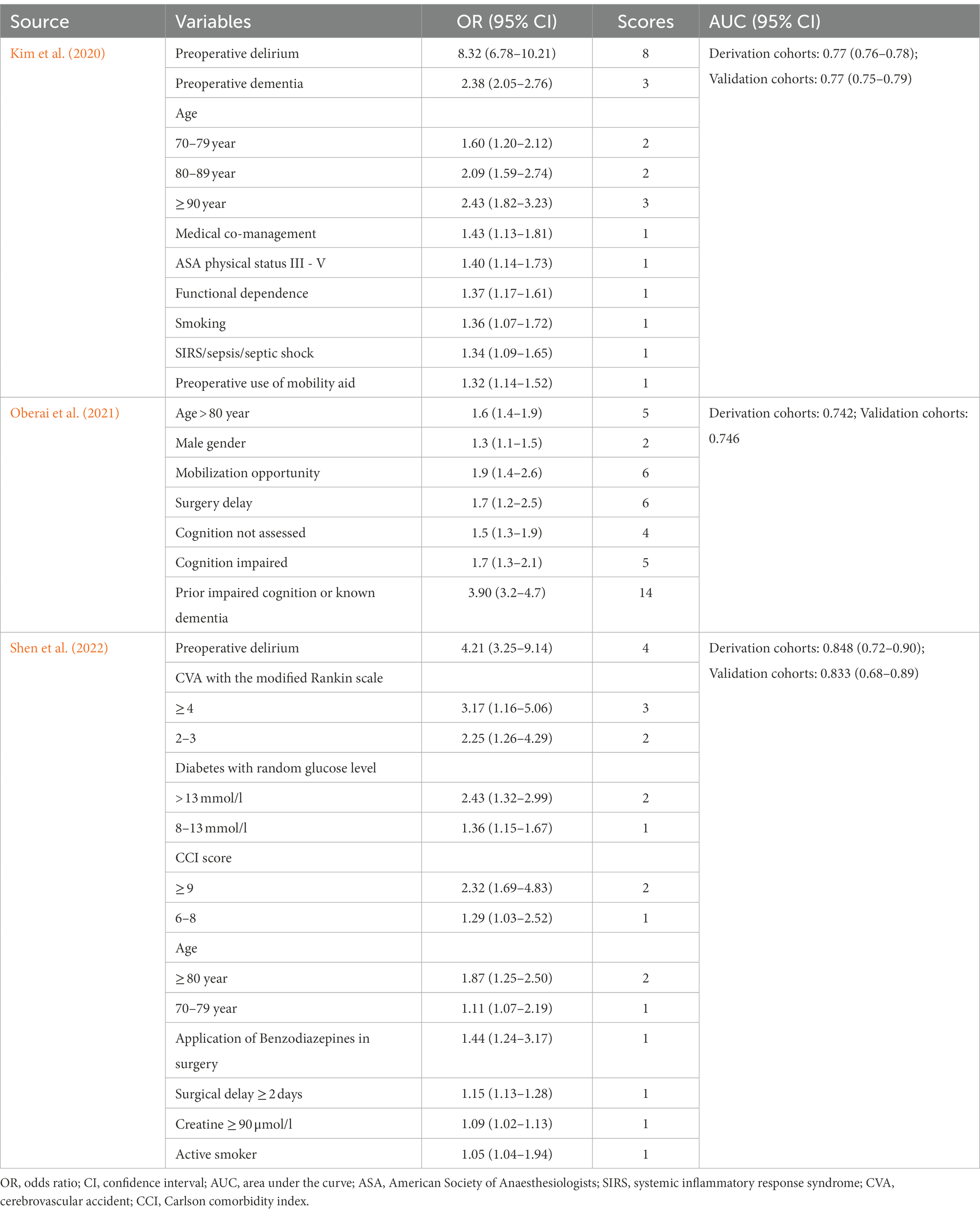
Table 2. Risk prediction models for postoperative delirium in geriatric patients with hip fractures.
Orthogeriatric comprehensive care is a multidisciplinary methodology of systematic assessment and optimization for elderly patients following orthopedic surgery, which plays a significant role in the progress of geriatric patients with hip fractures (Li et al., 2021). The orthogeriatric comprehensive care team usually includes orthopedic surgeons, geriatricians, physiotherapists, occupational therapists, and nurses. The primary responsibility of the team includes the identification of risk factors, optimization of nutrition and bowel function, as well as management of comorbidities, complications, pain, and fluid imbalances for geriatric patients with hip fractures (Figure 2). A 2020 meta-analysis showed that comprehensive interventions, such as education, awareness, and multidisciplinary collaboration around POD prevention and management, significantly reduced the prevalence of POD (Igwe et al., 2020).
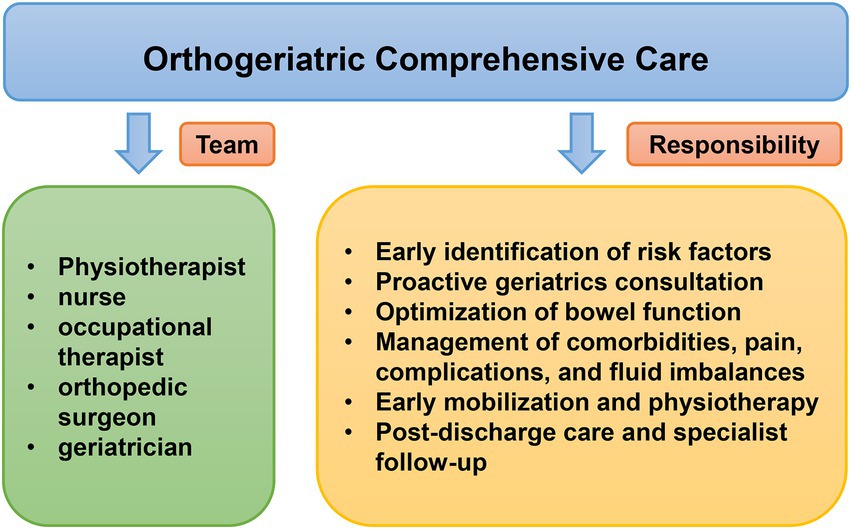
Figure 2. Orthogeriatric comprehensive care in geriatric patients with hip fractures for management of postoperative complication.
A substantially reduced incidence of POD in patients with hip fractures was shown to be associated with proactive geriatrics consultation and orthogeriatric co-management during the perioperative period (Marcantonio et al., 2001; Pollmann et al., 2021). In a meta-analysis of 1840 elderly patients with hip fractures (Wang et al., 2017), the incidence of POD in the comprehensive geriatric care group was significantly reduced compared to the routine orthopedic care group (OR 0.71; 95% CI, 0.57–0.89; p = 0.003). It also revealed that comprehensive geriatric care may accelerate cognitive function recovery after hip fracture surgery. However, these findings should be interpreted cautiously in light of the limitations of this study. For example, the instruments used to diagnose patients with POD are inconsistent, with variable sensitivity and specificity, and the influencing factors such as staff member experience, anesthetic method, and inclusion/exclusion criteria would differ between studies.
Additionally, Enomoto et al. (2021) created a clinical program called the Delirium Team Approach, which included educational sessions, reviews of preprinted doctor orders, and routine delirium screening. They found that implementation of this program could shorten postoperative hospital stays and reduce the incidence of POD in elderly patients after cardiovascular surgery. Furthermore, more multicenter RCTs with excellent methodology are required to gather proof of the effect of comprehensive orthogeriatric care on POD prevention in geriatric patients with hip fractures.
The choice of regional anesthesia or general anesthesia was thought to have an impact on the occurrence of POD previously (Ravi et al., 2019). However, recent results of several multicenter large-scale randomized controlled trials showed that regional anesthesia (spinal, subarachnoid, or both techniques combined with no sedation) did not significantly reduce the risk of POD in geriatric patients with hip fractures compared to general anesthesia (Neuman et al., 2021; Li et al., 2022). These findings indicated that the decision of which anesthetic to use during hip fracture surgery may depend more on patient desire than on predicted variations in clinical results. Additionally, in a randomized controlled trial of 94 geriatric patients with hip fractures (Gu et al., 2021), ultrasound-guided multiple nerve block was shown to be a safe and more effective anesthetic technique than general anesthesia, with reduced intravenous opioid consumption and POD incidence. However, the POD incidence in this study was the secondary outcome, and it was assessed by the delirium index, which is not widely used in clinical practice.
When it comes to general anesthesia, there are contradictory views on the effects of intravenous and inhalation anesthesia on POD. Several studies suggested that inhalation anesthesia, such as sevoflurane anesthesia, may increase the risk of POD by inducing or exacerbating neuroinflammation (Zhang et al., 2013; Saller et al., 2022). On the contrary, a randomized controlled trial of 209 geriatric patients following total hip or knee replacements found that sevoflurane was superior to propofol in the reduction of POD duration (p = 0.049; Mei et al., 2020). However, a growing body of studies has revealed that neither the incidence nor the severity of POD changed significantly between intravenous and inhalation anesthesia (Royse et al., 2011; Lurati Buse et al., 2012; Miller et al., 2018; Jin et al., 2020). Future studies still need to further explore the effects of different anesthesia techniques on the incidence and severity of POD in geriatric patients with hip fractures.
Pharmacologic strategies for the prevention and management of POD in geriatric patients with hip fractures have been studied for many years, while effective candidate drugs with strong evidence have not been found yet (Pluta et al., 2020). Drugs such as steroids (Swarbrick and Partridge, 2022), melatonin (Campbell et al., 2019), and vitamin D (Hung et al., 2022) have all been reported to be associated with POD, but all lack strong evidence. In the current, most studies focus on three medications: dexmedetomidine, antipsychotics, and analgesics.
It is reported that dexmedetomidine is an effective medication in the prevention of POD in hospitalized geriatric patients (León-Salas et al., 2020), but current studies mainly focus on the effect of dexmedetomidine on POD in geriatric patients after cardiovascular surgery. Dexmedetomidine was shown to be the most promising agent able to prevent the occurrence of POD in patients after cardiac surgeries, according to a 2020 meta-analysis of 56 RCTs that examined 38 interventions (Pieri et al., 2020). Two randomized controlled trials compared the effect of dexmedetomidine to midazolam and clonidine respectively, and both found that dexmedetomidine was more effective in the prevention of POD in patients who underwent stomatological or cardiovascular surgeries (Shokri and Ali, 2020; Wang et al., 2020). However, in a 2022 meta-analysis of 30 RCTs comprising 4,090 patients (Patel et al., 2022), perioperative dexmedetomidine administration failed to reduce the incidence of delirium in patients after cardiac surgeries. The possible explanation is that this meta-analysis included an increased number of trials, many of which have been published relatively recently and have not shown a beneficial relationship between dexmedetomidine and POD, and this study excluded trials at high risk of bias.
Whether dexmedetomidine is the most effective candidate for POD still needs further study. Additionally, adverse events such as bradycardia should be considered (Zeng et al., 2019). Future studies should focus on the effects of dexmedetomidine on POD in elderly patients with hip fractures to find effective and feasible dosing methods.
Acute pain in patients who underwent noncardiac surgery strongly mediates the relationship between preoperative cognitive impairment and postoperative delirium (Ma et al., 2022), therefore, adequate analgesia plays an essential role in the rehabilitation of geriatric hip fracture patients (Mears and Kates, 2015). Commonly used perioperative analgesic drugs include nonsteroidal anti-inflammatory drugs and opioids, narcotic and non-narcotic, respectively. Acetaminophen is an efficacious medication for analgesia in geriatric patients with hip fractures (Tsang et al., 2013; Bollinger et al., 2015). There is a retrospective study of 123 geriatric hip fracture patients (Connolly et al., 2020), which showed that intravenous acetaminophen had reduced the incidence of POD from 32.8 to 15.4% (p = 0.024). In a 2021 network meta-analysis (Lee et al., 2021), the combination of propofol and acetaminophen was the most successful pharmaceutical strategy with a minimal incidence of POD.
Although opioid administration can itself be a risk factor for POD (Duprey et al., 2021), pain is probably a stronger POD trigger in geriatric patients with hip fractures (Morrison et al., 2003). Two RCTs compared morphine and oxycodone to sufentanil respectively, and they found that both low-dose morphine intrathecal analgesia and oxycodone patient-controlled intravenous analgesia are superior to sufentanil patient-controlled intravenous analgesia in the prevention of POD in geriatric patients with hip fractures (Gan et al., 2020; Xu et al., 2022). Therefore, multimodal analgesia is recommended for the management of POD in geriatric patients with hip fractures.
Antipsychotics are dopamine D2 receptor antagonists, with varying degrees of affinity to muscarinic, serotonergic, and α2 adrenergic receptors (Farah, 2005). They can be divided into first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs). FGAs are also known as typical antipsychotics and relate to increased risks of psychomotor complications; SGAs are also called atypical antipsychotics and are linked to higher chances of cardiovascular and metabolic complications (Jin et al., 2020). The effect of antipsychotics on POD in geriatric patients with hip fractures is still doubtful, owing to minimal evidence and variable complications of them (Pluta et al., 2020).
Haloperidol, a typical antipsychotic, was studied in multiple trials with inconsistent results (Igwe et al., 2020; Li et al., 2021; Tillemans et al., 2021). According to a meta-analysis of patients admitted to an ICU, haloperidol prophylaxis could lower the incidence of POD compared to the placebo (RR 0.63; p = 0.004; Lin et al., 2020). However, two massive prospective RCTs that compared haloperidol to ketamine or ziprasidone respectively, indicated that none of the three medications could shorten the frequency and duration of postoperative cognitive dysfunction and POD in patients with a critical illness (Girard et al., 2018; Hollinger et al., 2021). Some studies supported the efficacy of SGAs such as aripiprazole, risperidone, and olanzapine in the treatment of POD; nevertheless, the quality of the evidence is poor because of the heterogeneity and bias of the research (Tachi et al., 2021; Sugawara et al., 2022). Moreover, the safety of antipsychotics is more concerning than their efficacy. Boncyk et al. (2021) conducted a trial comparing haloperidol, olanzapine, and quetiapine in the management of delirious patients in the ICU. They reported that all three antipsychotics were associated with noticeably fewer days spent alive and out of the hospital, and similar results were also reported previously (Maust et al., 2015; Agar et al., 2017; Ralph and Espinet, 2018).
In conclusion, antipsychotics are mainly used in the management of POD in critically ill patients in the ICU, and future studies could focus on the effect of antipsychotics on POD in elderly patients with hip fractures.
Perioperative administration of certain medications has been considered an important risk factor for POD in geriatric patients with hip fractures, including antihistamines and scopolamine (Alagiakrishnan and Wiens, 2004; By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, 2019). The most investigated perioperative medications with POD risk are benzodiazepines, antidepressants, and gabapentinoids.
Benzodiazepine receptor agonists (BZDRAs) are commonly used sedatives during the perioperative period, which can lower the consumption of intraoperative anesthetics (Nakagawa et al., 2000). However, numerous studies have demonstrated that perioperative usage of BZDRAs is linked to a higher risk of POD in geriatric patients with hip fractures (Poeran et al., 2020; Hernandez et al., 2021; Duprey et al., 2022; Lertkovit et al., 2022). The concrete mechanisms of benzodiazepine-induced POD vary based on the subtype of BZDRAs: Diazepam may affect the chloride plasticity mediated by Na+ − K+ − 2Cl-cotransporter isoform 1 and result in the gamma-aminobutyric acid α receptor malfunction (Matsumoto et al., 2021); midazolam can alter the expression and activity of acetyl-and butyryl-cholinesterase genes (Rump et al., 2022), and both contribute to benzodiazepine - induced POD. Additionally, a retrospective cohort study of 250 patients who were scheduled for surgery under general anesthesia investigated the relationship between the time course of BZDRAs use and the incidence of POD. It was discovered that the prevalence of POD was highest in the patients who stopped taking BZDRAs after surgery, which indicated that abrupt discontinuation of BZDRAs should be avoided during the perioperative period (Omichi et al., 2021).
Antidepressant administration during the perioperative period is also associated with a high incidence of POD in geriatric patients with hip fractures. In a matched case–control study of geriatric patients after hip or knee surgeries (Kassie et al., 2022), exposures to selective serotonin reuptake inhibitors (SSRIs) such as sertraline, citalopram, escitalopram, and fluvoxamine before surgery in cases were considerably greater than those in controls, which indicated that reduced preoperative use of SSRIs may prevent the occurrence of POD. Additionally, gabapentin and gabapentin combined with midazolam have also been found to be associated with a considerably increased risk of POD, according to several massive observatory studies in patients following major noncardiac surgeries (Athanassoglou et al., 2022; Duprey et al., 2022; Park et al., 2022). However, whether gabapentin can increase the incidence of POD in geriatric patients with hip fractures still needs further study.
Postoperative delirium in geriatric patients with hip fractures is significantly related to high short - and long-term mortality as well as poor functional and cognitive recovery. The concrete mechanism of POD is still elusive, and early identification of patients with POD risks is imperative. In the current, prevention interventions such as risk prediction and orthogeriatric comprehensive care are the most effective measures for POD management. Dexmedetomidine prophylaxis and multimode analgesia may be effective for reducing the prevalence and severity of POD in geriatric patients with hip fractures, which needs more large-scale multicentral RCTs to investigate their safety and efficacy.
YC and JL conceived the idea of this review. YC drafted the manuscript and created the figures. SL, HW, SD, FW, and CL performed the literature search and reviewed the content of this manuscript. All authors read and approved the final manuscript.
This study was financially supported by the National first-class undergraduate professional construction project (clinical medicine) sub-project of Anhui Medical University, Natural Science Foundation of Hefei City (grant number: 2022041 to JL), Clinical Research cultivation Program of the Second Affiliated Hospital of Anhui Medical University (grant number: 2020LCZD20 to JL), and Basic and Clinical Cooperative Research Promotion Plan of Anhui Medical University (grant number: 2020xkjT040 to JL).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Adam, E. H., Haas, V., Lindau, S., Zacharowski, K., and Scheller, B. (2020). Cholinesterase alterations in delirium after cardiosurgery: a German monocentric prospective study. BMJ Open 10:e031212. doi: 10.1136/bmjopen-2019-031212
Agar, M. R., Lawlor, P. G., Quinn, S., Draper, B., Caplan, G. A., Rowett, D., et al. (2017). Efficacy of Oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern. Med. 177, 34–42. doi: 10.1001/jamainternmed.2016.7491
Aharonoff, G. B., Koval, K. J., Skovron, M. L., and Zuckerman, J. D. (1997). Hip fractures in the elderly: predictors of one year mortality. J. Orthop. Trauma 11, 162–165. doi: 10.1097/00005131-199704000-00004
Alagiakrishnan, K., and Wiens, C. A. (2004). An approach to drug induced delirium in the elderly. Postgrad. Med. J. 80, 388–393. doi: 10.1136/pgmj.2003.017236
Alam, A., Hana, Z., Jin, Z., Suen, K. C., and Ma, D. (2018). Surgery, neuroinflammation and cognitive impairment. EBioMedicine 37, 547–556. doi: 10.1016/j.ebiom.2018.10.021
Alexandris, A., Liu, A. K., Chang, R. C., Pearce, R. K., and Gentleman, S. M. (2015). Differential expression of galanin in the cholinergic basal forebrain of patients with Lewy body disorders. Acta Neuropathol. Commun. 3:77. doi: 10.1186/s40478-015-0249-4
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorder: DSM-5. Arlington, VA: American Psychiatric Publishing.
Ansaloni, L., Catena, F., Chattat, R., Fortuna, D., Franceschi, C., Mascitti, P., et al. (2010). Risk factors and incidence of postoperative delirium in elderly patients after elective and emergency surgery. Br. J. Surg. 97, 273–280. doi: 10.1002/bjs.6843
Athanassoglou, V., Cozowicz, C., Zhong, H., Illescas, A., Poeran, J., Liu, J., et al. (2022). Association of perioperative midazolam use and complications: a population-based analysis. Reg. Anesth. Pain Med. 47, 228–233. doi: 10.1136/rapm-2021-102989
Bai, J., Liang, Y., Zhang, P., Liang, X., He, J., Wang, J., et al. (2020). Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos. Int. 31, 317–326. doi: 10.1007/s00198-019-05172-7
Berggren, D., Gustafson, Y., Eriksson, B., Bucht, G., Hansson, L. I., Reiz, S., et al. (1987). Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth. Analg. 66, 497–504.
Bishara, A., Chiu, C., Whitlock, E. L., Douglas, V. C., Lee, S., Butte, A. J., et al. (2022). Postoperative delirium prediction using machine learning models and preoperative electronic health record data. BMC Anesthesiol. 22:8. doi: 10.1186/s12871-021-01543-y
Bollinger, A. J., Butler, P. D., Nies, M. S., Sietsema, D. L., Jones, C. B., and Endres, T. J. (2015). Is scheduled intravenous acetaminophen effective in the pain management protocol of geriatric hip fractures? Geriatr. Orthop. Surg. Rehabil. 6, 202–208. doi: 10.1177/2151458515588560
Boncyk, C. S., Farrin, E., Stollings, J. L., Rumbaugh, K., Wilson, J. E., Marshall, M., et al. (2021). Pharmacologic Management of Intensive Care Unit Delirium: clinical prescribing practices and outcomes in more than 8500 patient encounters. Anesth. Analg. 133, 713–722. doi: 10.1213/ane.0000000000005365
Boucher, V., Lamontagne, M. E., Nadeau, A., Carmichael, P. H., Yadav, K., Voyer, P., et al. (2019). Unrecognized incident delirium in older emergency department patients. J. Emerg. Med. 57, 535–542. doi: 10.1016/j.jemermed.2019.05.024
Brauer, C. A., Coca-Perraillon, M., Cutler, D. M., and Rosen, A. B. (2009). Incidence and mortality of hip fractures in the United States. JAMA 302, 1573–1579. doi: 10.1001/jama.2009.1462
Breitbart, W., Rosenfeld, B., Roth, A., Smith, M. J., Cohen, K., and Passik, S. (1997). The memorial delirium assessment scale. J. Pain Symptom Manag. 13, 128–137. doi: 10.1016/s0885-3924(96)00316-8
Bruce, A. J., Ritchie, C. W., Blizard, R., Lai, R., and Raven, P. (2007). The incidence of delirium associated with orthopedic surgery: a meta-analytic review. Int. Psychogeriatr. 19, 197–214. doi: 10.1017/s104161020600425x
Bucks, R. S., Gidron, Y., Harris, P., Teeling, J., Wesnes, K. A., and Perry, V. H. (2008). Selective effects of upper respiratory tract infection on cognition, mood and emotion processing: a prospective study. Brain Behav. Immun. 22, 399–407. doi: 10.1016/j.bbi.2007.09.005
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel (2019). American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 67, 674–694. doi: 10.1111/jgs.15767
Campbell, A. M., Axon, D. R., Martin, J. R., Slack, M. K., Mollon, L., and Lee, J. K. (2019). Melatonin for the prevention of postoperative delirium in older adults: a systematic review and meta-analysis. BMC Geriatr. 19:272. doi: 10.1186/s12877-019-1297-6
Cape, E., Hall, R. J., van Munster, B. C., de Vries, A., Howie, S. E., Pearson, A., et al. (2014). Cerebrospinal fluid markers of neuroinflammation in delirium: a role for interleukin-1β in delirium after hip fracture. J. Psychosom. Res. 77, 219–225. doi: 10.1016/j.jpsychores.2014.06.014
Cavallari, M., Dai, W., Guttmann, C. R., Meier, D. S., Ngo, L. H., Hshieh, T. T., et al. (2016). Neural substrates of vulnerability to postsurgical delirium as revealed by presurgical diffusion MRI. Brain J. Neurol. 139, 1282–1294. doi: 10.1093/brain/aww010
Chaiwat, O., Chanidnuan, M., Pancharoen, W., Vijitmala, K., Danpornprasert, P., Toadithep, P., et al. (2019). Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. 19:39. doi: 10.1186/s12871-019-0694-x
Charlson, M. E., Pompei, P., Ales, K. L., and Mac Kenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383. doi: 10.1016/0021-9681(87)90171-8
Chen, L., Zhang, S., Tian, W., Huang, L., Jiang, X., Chen, X., et al. (2020). Cerebral spinal fluid cholinergic biomarkers predict postoperative cognitive dysfunction in aged patients – a prospective, observational, single center study. J. Clin. Anesth. 62:109743. doi: 10.1016/j.jclinane.2020.109743
Connolly, K. P., Kleinman, R. S., Stevenson, K. L., Neuman, M. D., and Mehta, S. N. (2020). Delirium reduced with intravenous acetaminophen in geriatric hip fracture patients. J. Am. Acad. Orthop. Surg. 28, 325–331. doi: 10.5435/jaaos-d-17-00925
Counts, S. E., Perez, S. E., Kahl, U., Bartfai, T., Bowser, R. P., Deecher, D. C., et al. (2001). Galanin: neurobiologic mechanisms and therapeutic potential for Alzheimer's disease. CNS Drug Rev. 7, 445–470. doi: 10.1111/j.1527-3458.2001.tb00210.x
Cummings, S. R., and Melton, L. J. (2002). Epidemiology and outcomes of osteoporotic fractures. Lancet 359, 1761–1767. doi: 10.1016/S0140-6736(02)08657-9
de Jong, L., van Rijckevorsel, V., Raats, J. W., Klem, T., Kuijper, T. M., and Roukema, G. R. (2019). Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: risk factors and clinical outcomes. Clin. Interv. Aging 14, 427–435. doi: 10.2147/cia.S189760
de la Cruz, M., Fan, J., Yennu, S., Tanco, K., Shin, S., Wu, J., et al. (2015). The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support. Care Cancer 23, 2427–2433. doi: 10.1007/s00520-015-2610-3
de Miguel, A. M., Roca Chacon, O., Martinez-Alonso, M., Serrano Godoy, M., Mas Atance, J., and Garcia, G. R. (2018). Hip fracture in the elderly patient: prognostic factors for mortality and functional recovery at one year. Rev. Esp. Geriatr. Gerontol. 53, 247–254. doi: 10.1016/j.regg.2018.04.447
de Rooij, S. E., van Munster, B. C., Korevaar, J. C., Casteelen, G., Schuurmans, M. J., van der Mast, R. C., et al. (2006). Delirium subtype identification and the validation of the delirium rating scale--Revised-98 (Dutch version) in hospitalized elderly patients. Int. J. Geriatr. Psychiatry 21, 876–882. doi: 10.1002/gps.1577
Douglas, V. C., Hessler, C. S., Dhaliwal, G., Betjemann, J. P., Fukuda, K. A., Alameddine, L. R., et al. (2013). The AWOL tool: derivation and validation of a delirium prediction rule. J. Hosp. Med. 8, 493–499. doi: 10.1002/jhm.2062
Duprey, M. S., Devlin, J. W., Griffith, J. L., Travison, T. G., Briesacher, B. A., Jones, R., et al. (2022). Association between perioperative medication use and postoperative delirium and cognition in older adults undergoing elective noncardiac surgery. Anesth. Analg. 134, 1154–1163. doi: 10.1213/ane.0000000000005959
Duprey, M. S., Dijkstra-Kersten, S. M. A., Zaal, I. J., Briesacher, B. A., Saczynski, J. S., Griffith, J. L., et al. (2021). Opioid use increases the risk of delirium in critically ill adults independently of pain. Am. J. Respir. Crit. Care Med. 204, 566–572. doi: 10.1164/rccm.202010-3794OC
Edelstein, D. M., Aharonoff, G. B., Karp, A., Capla, E. L., Zuckerman, J. D., and Koval, K. J. (2004). Effect of postoperative delirium on outcome after hip fracture. Clin. Orthop. Relat. Res. 422, 195–200. doi: 10.1097/01.blo.0000128649.59959.0c
Ekdahl, C. T., Claasen, J. H., Bonde, S., Kokaia, Z., and Lindvall, O. (2003). Inflammation is detrimental for neurogenesis in adult brain. Proc. Natl. Acad. Sci. U. S. A. 100, 13632–13637. doi: 10.1073/pnas.2234031100
Ely, E. W., Margolin, R., Francis, J., May, L., Truman, B., Dittus, R., et al. (2001). Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit. Care Med. 29, 1370–1379. doi: 10.1097/00003246-200107000-00012
Enomoto, K., Kosaka, S., Kimura, T., Matsubara, M., Kitada, Y., Mieno, M., et al. (2021). Prevention of postoperative delirium after cardiovascular surgery: a team-based approach. J. Thorac. Cardiovasc. Surg. S0022-5223(21)01126-0. doi: 10.1016/j.jtcvs.2021.07.027 [Epub ahead of print].
European Delirium Association, American Delirium Society (2014). The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer. BMC Med. 12:141. doi: 10.1186/s12916-014-0141-2
Farah, A. (2005). Atypicality of atypical antipsychotics. Prim. Care Companion J. Clin. Psychiatry 7, 268–274. doi: 10.4088/pcc.v07n0602
Fischer, H., Maleitzke, T., Eder, C., Ahmad, S., Stöckle, U., and Braun, K. F. (2021). Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur. J. Med. Res. 26:86. doi: 10.1186/s40001-021-00556-0
Flikweert, E. R., Wendt, K. W., Diercks, R. L., Izaks, G. J., Landsheer, D., Stevens, M., et al. (2018). Complications after hip fracture surgery: are they preventable? Eur. J. Trauma Emerg. Surg. 44, 573–580. doi: 10.1007/s00068-017-0826-2
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). "mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198. doi: 10.1016/0022-3956(75)90026-6
Gan, J., Tu, Q., Miao, S., Lei, T., Cui, X., Yan, J., et al. (2020). Effects of oxycodone applied for patient-controlled analgesia on postoperative cognitive function in elderly patients undergoing total hip arthroplasty: a randomized controlled clinical trial. Aging Clin. Exp. Res. 32, 329–337. doi: 10.1007/s40520-019-01202-w
Girard, T. D., Exline, M. C., Carson, S. S., Hough, C. L., Rock, P., Gong, M. N., et al. (2018). Haloperidol and ziprasidone for treatment of delirium in critical illness. N. Engl. J. Med. 379, 2506–2516. doi: 10.1056/NEJMoa1808217
Gross, A. L., Tommet, D., D’Aquila, M., Schmitt, E., Marcantonio, E. R., Helfand, B., et al. (2018). Harmonization of delirium severity instruments: a comparison of the DRS-R-98, MDAS, and CAM-S using item response theory. BMC Med. Res. Methodol. 18:92. doi: 10.1186/s12874-018-0552-4
Gu, J., Wang, E., Dai, S., Dong, R., Xu, F., Shen, Z., et al. (2021). Ultrasound-guided multiple nerve blocks: a safe and effective anesthetic modality in geriatric hip fracture patients. Clin. J. Pain 37, 881–886. doi: 10.1097/ajp.0000000000000988
Guo, Y., Li, Y., Zhang, Y., Fang, S., Xu, X., Zhao, A., et al. (2019). Post-operative delirium associated with metabolic alterations following hemi-arthroplasty in older patients. Age Ageing 49, 88–95. doi: 10.1093/ageing/afz132
Hatano, Y., Narumoto, J., Shibata, K., Matsuoka, T., Taniguchi, S., Hata, Y., et al. (2013). White-matter hyperintensities predict delirium after cardiac surgery. Am. J. Geriatr. Psychiatry 21, 938–945. doi: 10.1016/j.jagp.2013.01.061
Haynes, M. S., Alder, K. D., Toombs, C., Amakiri, I. C., Rubin, L. E., and Grauer, J. N. (2021). Predictors and sequelae of postoperative delirium in a geriatric patient population with hip fracture. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 5:e20.00221. doi: 10.5435/JAAOSGlobal-D-20-00221
Hecht, G., Slee, C. A., Goodell, P. B., Taylor, S. L., and Wolinsky, P. R. (2019). Predictive modeling for geriatric hip fracture patients: early surgery and delirium have the largest influence on length of stay. J. Am. Acad. Orthop. Surg. 27, e293–e300. doi: 10.5435/jaaos-d-17-00447
Heo, E. Y., Lee, B. J., Hahm, B. J., Song, E. H., Lee, H. A., Yoo, C. G., et al. (2011). Translation and validation of the Korean confusion assessment method for the intensive care unit. BMC Psychiatry 11:94. doi: 10.1186/1471-244x-11-94
Hernandez, N. M., Cunningham, D. J., Hinton, Z. W., Wu, C. J., and Seyler, T. M. (2021). Are patients taking benzodiazepines at increased risk for complications following primary Total knee arthroplasty? J. Arthroplast. 36, 1611–1616. doi: 10.1016/j.arth.2020.12.004
Hollinger, A., Rüst, C. A., Riegger, H., Gysi, B., Tran, F., Brügger, J., et al. (2021). Ketamine vs. haloperidol for prevention of cognitive dysfunction and postoperative delirium: a phase IV multicentre randomised placebo-controlled double-blind clinical trial. J. Clin. Anesth. 68:110099. doi: 10.1016/j.jclinane.2020.110099
Huang, H., Han, J., Li, Y., Yang, Y., Shen, J., Fu, Q., et al. (2022). Early serum metabolism profile of post-operative delirium in elderly patients following cardiac surgery with cardiopulmonary bypass. Front. Aging Neurosci. 14:857902. doi: 10.3389/fnagi.2022.857902
Hung, K. C., Wang, L. K., Lin, Y. T., Yu, C. H., Chang, C. Y., Sun, C. K., et al. (2022). Association of preoperative vitamin D deficiency with the risk of postoperative delirium and cognitive dysfunction: a meta-analysis. J. Clin. Anesth. 79:110681. doi: 10.1016/j.jclinane.2022.110681
Igwe, E. O., Nealon, J., Mohammed, M., Hickey, B., Chou, K. R., Chen, K. H., et al. (2020). Multi-disciplinary and pharmacological interventions to reduce post-operative delirium in elderly patients: a systematic review and meta-analysis. J. Clin. Anesth. 67:110004. doi: 10.1016/j.jclinane.2020.110004
Inouye, S. K., Kosar, C. M., Tommet, D., Schmitt, E. M., Puelle, M. R., Saczynski, J. S., et al. (2014). The CAM-S: development and validation of a new scoring system for delirium severity in 2 cohorts. Ann. Intern. Med. 160, 526–533. doi: 10.7326/m13-1927
Inouye, S. K., van Dyck, C. H., Alessi, C. A., Balkin, S., Siegal, A. P., and Horwitz, R. I. (1990). Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 113, 941–948. doi: 10.7326/0003-4819-113-12-941
Jin, Z., Hu, J., and Ma, D. (2020). Postoperative delirium: perioperative assessment, risk reduction, and management. Br. J. Anaesth. 125, 492–504. doi: 10.1016/j.bja.2020.06.063
Kant, I. M. J., de Bresser, J., van Montfort, S. J. T., Slooter, A. J. C., and Hendrikse, J. (2017). MRI markers of neurodegenerative and neurovascular changes in relation to postoperative delirium and postoperative cognitive decline. Am. J. Geriatr. Psychiatry 25, 1048–1061. doi: 10.1016/j.jagp.2017.06.016
Kassie, G. M., Roughead, E. E., Nguyen, T. A., Pratt, N. L., and Kalisch Ellett, L. M. (2022). The risk of preoperative central nervous system-acting medications on delirium following hip or knee surgery: a matched case-control study. Drug Saf. 45, 75–82. doi: 10.1007/s40264-021-01136-1
Kim, E. M., Li, G., and Kim, M. (2020). Development of a risk score to predict postoperative delirium in patients with hip fracture. Anesth. Analg. 130, 79–86. doi: 10.1213/ane.0000000000004386
Kimchi, E. Y., Neelagiri, A., Whitt, W., Sagi, A. R., Ryan, S. L., Gadbois, G., et al. (2019). Clinical EEG slowing correlates with delirium severity and predicts poor clinical outcomes. Neurology 93, e1260–e1271. doi: 10.1212/WNL.0000000000008164
Koskderelioglu, A., Onder, O., Gucuyener, M., Altay, T., Kayali, C., and Gedizlioglu, M. (2017). Screening for postoperative delirium in patients with acute hip fracture: assessment of predictive factors. Geriatr Gerontol Int 17, 919–924. doi: 10.1111/ggi.12806
Kuo, L. Y., Hsu, P. T., Wu, W. T., Lee, R. P., Wang, J. H., Chen, H. W., et al. (2021). The incidence of mental disorder increases after hip fracture in older people: a nationwide cohort study. BMC Geriatr. 21:249. doi: 10.1186/s12877-021-02195-w
Kyeong, S., Shin, J. E., Yang, K. H., Lee, W. S., Chung, T. S., and Kim, J. J. (2018). Neural predisposing factors of postoperative delirium in elderly patients with femoral neck fracture. Sci. Rep. 8:7602. doi: 10.1038/s41598-018-26030-2
Lee, J. M., Cho, Y. J., Ahn, E. J., Choi, G. J., and Kang, H. (2021). Pharmacological strategies to prevent postoperative delirium: a systematic review and network meta-analysis. Anesth. Pain Med. (Seoul) 16, 28–48. doi: 10.17085/apm.20079
León-Salas, B., Trujillo-Martín, M. M., Del Castillo, L. P. M., García, J. G., Pérez-Ros, P., Ruiz, F. R., et al. (2020). Pharmacologic interventions for prevention of delirium in hospitalized older people: a meta-analysis. Arch. Gerontol. Geriatr. 90:104171. doi: 10.1016/j.archger.2020.104171
Lertkovit, S., Siriussawakul, A., Suraarunsumrit, P., Lertpipopmetha, W., Manomaiwong, N., Wivatdechakul, W., et al. (2022). Polypharmacy in older adults undergoing major surgery: prevalence, association with postoperative cognitive dysfunction and potential associated anesthetic agents. Front. Med. 9:811954. doi: 10.3389/fmed.2022.811954
Leslie, D. L., Marcantonio, E. R., Zhang, Y., Leo-Summers, L., and Inouye, S. K. (2008). One-year health care costs associated with delirium in the elderly population. Arch. Intern. Med. 168, 27–32. doi: 10.1001/archinternmed.2007.4
Li, T., Li, J., Yuan, L., Wu, J., Jiang, C., Daniels, J., et al. (2022). Effect of regional vs general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: the RAGA randomized trial. JAMA 327, 50–58. doi: 10.1001/jama.2021.22647
Li, X., Wang, G., He, Y., Wang, Z., and Zhang, M. (2022). White-cell derived inflammatory biomarkers in prediction of postoperative delirium in elderly patients undergoing surgery for lower limb fracture under non-general Anaesthesia. Clin. Interv. Aging 17, 383–392. doi: 10.2147/CIA.S346954
Li, X., Wang, Y., Liu, J., Xiong, Y., Chen, S., Han, J., et al. (2021). Effects of perioperative interventions for preventing postoperative delirium: a protocol for systematic review and meta-analysis of randomized controlled trials. Medicine 100:e26662. doi: 10.1097/md.0000000000026662
Lin, P., Zhang, J., Shi, F., and Liang, Z. A. (2020). Can haloperidol prophylaxis reduce the incidence of delirium in critically ill patients in intensive care units? A systematic review and meta-analysis. Heart Lung 49, 265–272. doi: 10.1016/j.hrtlng.2020.01.010
Liu, K., Sheng, J., Zhang, H., Liu, L., Tang, Y., Zhu, Z., et al. (2021). Risk factors for mortality after Uncemented bipolar hemiarthroplasty for geriatric displaced femoral neck fracture. Orthopedics 44, e570–e576. doi: 10.3928/01477447-20210618-19
Low, S., Wee, E., and Dorevitch, M. (2021). Impact of place of residence, frailty and other factors on rehabilitation outcomes post hip fracture. Age Ageing 50, 423–430. doi: 10.1093/ageing/afaa131
Lurati Buse, G. A., Schumacher, P., Seeberger, E., Studer, W., Schuman, R. M., Fassl, J., et al. (2012). Randomized comparison of sevoflurane versus propofol to reduce perioperative myocardial ischemia in patients undergoing noncardiac surgery. Circulation 126, 2696–2704. doi: 10.1161/circulationaha.112.126144
Ma, J. H., Liu, Y. F., Hong, H., Li, C. J., Cui, F., Mu, D. L., et al. (2022). Effect of acute pain on the association between preoperative cognitive impairment and postoperative delirium: a secondary analysis of three trials. Br. J. Anaesth. S0007-0912(22)00356-7. doi: 10.1016/j.bja.2022.06.033 [Epub ahead of print].
Maekawa, K., Baba, T., Otomo, S., Morishita, S., and Tamura, N. (2014). Low pre-existing gray matter volume in the medial temporal lobe and white matter lesions are associated with postoperative cognitive dysfunction after cardiac surgery. PLoS One 9:e87375. doi: 10.1371/journal.pone.0087375
Maldonado, J. R. (2017). Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit. Care Clin. 33, 461–519. doi: 10.1016/j.ccc.2017.03.013
Marcantonio, E. R., Flacker, J. M., Wright, R. J., and Resnick, N. M. (2001). Reducing delirium after hip fracture: a randomized trial. J. Am. Geriatr. Soc. 49, 516–522. doi: 10.1046/j.1532-5415.2001.49108.x
Marcantonio, E. R., Ngo, L. H., O'Connor, M., Jones, R. N., Crane, P. K., Metzger, E. D., et al. (2014). 3D-CAM: derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: a cross-sectional diagnostic test study. Ann. Intern. Med. 161, 554–561. doi: 10.7326/M14-0865
Matsumoto, D., Ushio, S., Wada, Y., Noda, Y., Esumi, S., Izushi, Y., et al. (2021). Bumetanide prevents diazepam-modified anxiety-like behavior in lipopolysaccharide-treated mice. Eur. J. Pharmacol. 904:174195. doi: 10.1016/j.ejphar.2021.174195
Maust, D. T., Kim, H. M., Seyfried, L. S., Chiang, C., Kavanagh, J., Schneider, L. S., et al. (2015). Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiat. 72, 438–445. doi: 10.1001/jamapsychiatry.2014.3018
Mears, S. C., and Kates, S. L. (2015). A guide to improving the Care of Patients with fragility fractures, edition 2. Geriatr. Orthop. Surg. Rehabil. 6, 58–120. doi: 10.1177/2151458515572697
Mei, X., Zheng, H. L., Li, C., Ma, X., Zheng, H., Marcantonio, E., et al. (2020). The effects of Propofol and sevoflurane on postoperative delirium in older patients: a randomized clinical trial study. J. Alzheimers Dis. 76, 1627–1636. doi: 10.3233/jad-200322
Merchant, R. A., Lui, K. L., Ismail, N. H., Wong, H. P., and Sitoh, Y. Y. (2005). The relationship between postoperative complications and outcomes after hip fracture surgery. Ann. Acad. Med. Singap. 34, 163–168.
Meyer, M., Gotz, J., Parik, L., Renkawitz, T., Grifka, J., Maderbacher, G., et al. (2021). Postoperative delirium is a risk factor for complications and poor outcome after total hip and knee arthroplasty. Acta Orthop. 92, 695–700. doi: 10.1080/17453674.2021.1980676
Miller, D., Lewis, S. R., Pritchard, M. W., Schofield-Robinson, O. J., Shelton, C. L., Alderson, P., et al. (2018). Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst. Rev. 8:Cd012317. doi: 10.1002/14651858.CD012317.pub2
Morrison, R. S., Magaziner, J., Gilbert, M., Koval, K. J., McLaughlin, M. A., Orosz, G., et al. (2003). Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J. Gerontol. A Biol. Sci. Med. Sci. 58, 76–81. doi: 10.1093/gerona/58.1.m76
Mosk, C. A., Mus, M., Vroemen, J. P., van der Ploeg, T., Vos, D. I., Elmans, L. H., et al. (2017). Dementia and delirium, the outcomes in elderly hip fracture patients. Clin. Interv. Aging 12, 421–430. doi: 10.2147/cia.S115945
Mullen, J. O., and Mullen, N. L. (1992). Hip fracture mortality. A prospective, multifactorial study to predict and minimize death risk. Clin. Orthop. Relat. Res. 280, 214–222.
Nakagawa, M., Mammoto, T., Hazama, A., Kita, T., Akamatsu, T., Kambara, N., et al. (2000). Midazolam premedication reduces propofol requirements for sedation during regional anesthesia. Can. J. Anesth. 47, 47–49. doi: 10.1007/BF03020731
Neerland, B. E., Hall, R. J., Seljeflot, I., Frihagen, F., Mac Lullich, A. M., Raeder, J., et al. (2016). Associations between delirium and preoperative cerebrospinal fluid C-reactive protein, Interleukin-6, and Interleukin-6 receptor in individuals with acute hip fracture. J. Am. Geriatr. Soc. 64, 1456–1463. doi: 10.1111/jgs.14238
Neuman, M. D., Feng, R., Carson, J. L., Gaskins, L. J., Dillane, D., Sessler, D. I., et al. (2021). Spinal anesthesia or general anesthesia for hip surgery in older adults. N. Engl. J. Med. 385, 2025–2035. doi: 10.1056/NEJMoa2113514
Oberai, T., Oosterhoff, J. H. F., Woodman, R., Doornberg, J. N., Kerkhoffs, G., and Jaarsma, R. (2021). Development of a postoperative delirium risk scoring tool using data from the Australian and New Zealand hip fracture registry: an analysis of 6672 patients 2017-2018. Arch. Gerontol. Geriatr. 94:104368. doi: 10.1016/j.archger.2021.104368
Oh, E. S., Fong, T. G., Hshieh, T. T., and Inouye, S. K. (2017). Delirium in older persons: advances in diagnosis and treatment. JAMA 318, 1161–1174. doi: 10.1001/jama.2017.12067
Omichi, C., Ayani, N., Oya, N., Matsumoto, Y., Tanaka, M., Morimoto, T., et al. (2021). Association between discontinuation of benzodiazepine receptor agonists and post-operative delirium among inpatients with liaison intervention: a retrospective cohort study. Compr. Psychiatry 104:152216. doi: 10.1016/j.comppsych.2020.152216
Onodera, T., Goseki, N., and Kosaki, G. (1984). Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85, 1001–1005.
Otomo, S., Maekawa, K., Goto, T., Baba, T., and Yoshitake, A. (2013). Pre-existing cerebral infarcts as a risk factor for delirium after coronary artery bypass graft surgery. Interact. Cardiovasc. Thorac. Surg. 17, 799–804. doi: 10.1093/icvts/ivt304
Ouellet, J. A., Ouellet, G. M., Romegialli, A. M., Hirsch, M., Berardi, L., Ramsey, C. M., et al. (2019). Functional outcomes after hip fracture in independent community-dwelling patients. J. Am. Geriatr. Soc. 67, 1386–1392. doi: 10.1111/jgs.15870
Park, C. M., Inouye, S. K., Marcantonio, E. R., Metzger, E., Bateman, B. T., Lie, J. J., et al. (2022). Perioperative gabapentin use and in-hospital adverse clinical events among older adults after major surgery. JAMA Intern. Med. 182, 1117–1127. doi: 10.1001/jamainternmed.2022.3680
Patel, M., Onwochei, D. N., and Desai, N. (2022). Influence of perioperative dexmedetomidine on the incidence of postoperative delirium in adult patients undergoing cardiac surgery. Br. J. Anaesth. 129, 67–83. doi: 10.1016/j.bja.2021.11.041
Pereira, J. V., Aung Thein, M. Z., Nitchingham, A., and Caplan, G. A. (2021). Delirium in older adults is associated with development of new dementia: a systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 36, 993–1003. doi: 10.1002/gps.5508
Pieri, M., De Simone, A., Rose, S., De Domenico, P., Lembo, R., Denaro, G., et al. (2020). Trials focusing on prevention and treatment of delirium after cardiac surgery: a systematic review of randomized evidence. J. Cardiothorac. Vasc. Anesth. 34, 1641–1654. doi: 10.1053/j.jvca.2019.09.028
Pluta, M. P., Dziech, M., Czempik, P. F., Szczepańska, A. J., and Krzych, Ł. J. (2020). Antipsychotic drugs in prevention of postoperative delirium-what is known in 2020? Int. J. Environ. Res. Public Health 17:6069. doi: 10.3390/ijerph17176069
Poeran, J., Cozowicz, C., Zubizarreta, N., Weinstein, S. M., Deiner, S. G., Leipzig, R. M., et al. (2020). Modifiable factors associated with postoperative delirium after hip fracture repair: An age-stratified retrospective cohort study. Eur. J. Anaesthesiol. 37, 649–658. doi: 10.1097/eja.0000000000001197
Pollmann, C. T., Mellingsæter, M. R., Neerland, B. E., Straume-Næsheim, T., Årøen, A., and Watne, L. O. (2021). Orthogeriatric co-management reduces incidence of delirium in hip fracture patients. Osteopos Int. 32, 2225–2233. doi: 10.1007/s00198-021-05974-8
Prieto, G. A., Tong, L., Smith, E. D., and Cotman, C. W. (2019). TNFα and IL-1β but not IL-18 suppresses hippocampal long-term potentiation directly at the synapse. Neurochem. Res. 44, 49–60. doi: 10.1007/s11064-018-2517-8
Ralph, S. J., and Espinet, A. J. (2018). Increased all-cause mortality by antipsychotic drugs: updated review and meta-analysis in dementia and general mental health care. J Alzheimers Dis. Rep. 2, 1–26. doi: 10.3233/adr-170042
Ravi, B., Pincus, D., Choi, S., Jenkinson, R., Wasserstein, D. N., and Redelmeier, D. A. (2019). Association of Duration of surgery with postoperative delirium among patients receiving hip fracture repair. JAMA Netw. Open 2:e190111. doi: 10.1001/jamanetworkopen.2019.0111
Root, J. C., Pryor, K. O., Downey, R., Alici, Y., Davis, M. L., Holodny, A., et al. (2013). Association of pre-operative brain pathology with post-operative delirium in a cohort of non-small cell lung cancer patients undergoing surgical resection. Psycho-Oncology 22, 2087–2094. doi: 10.1002/pon.3262
Royse, C. F., Andrews, D. T., Newman, S. N., Stygall, J., Williams, Z., Pang, J., et al. (2011). The influence of propofol or desflurane on postoperative cognitive dysfunction in patients undergoing coronary artery bypass surgery. Anaesthesia 66, 455–464. doi: 10.1111/j.1365-2044.2011.06704.x
Rudolph, J. L., Jones, R. N., Levkoff, S. E., Rockett, C., Inouye, S. K., Sellke, F. W., et al. (2009). Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation 119, 229–236. doi: 10.1161/circulationaha.108.795260
Rump, K., Holtkamp, C., Bergmann, L., Nowak, H., Unterberg, M., Orlowski, J., et al. (2022). Midazolam impacts acetyl-and butyrylcholinesterase genes: An epigenetic explanation for postoperative delirium? PLoS One 17:e0271119. doi: 10.1371/journal.pone.0271119
Saller, T., Hubig, L., Seibold, H., Schroeder, Z., Wang, B., Groene, P., et al. (2022). Association between post-operative delirium and use of volatile anesthetics in the elderly: a real-world big data approach. J. Clin. Anesth. 83:110957. doi: 10.1016/j.jclinane.2022.110957
Schrøder, C. K., Hjelholt, T. J., Møller, H., Madsen, M., Pedersen, A. B., and Kristensen, P. K. (2022). Comorbidity and quality of in-hospital care for hip fracture patients. J. Am. Med. Dir. Assoc. 23, 671–677.e4. doi: 10.1016/j.jamda.2022.01.078
Shen, J., An, Y., Jiang, B., and Zhang, P. (2022). Derivation and validation of a prediction score for postoperative delirium in geriatric patients undergoing hip fracture surgery or hip arthroplasty. Front. Surg. 9:919886. doi: 10.3389/fsurg.2022.919886
Shioiri, A., Kurumaji, A., Takeuchi, T., Matsuda, H., Arai, H., and Nishikawa, T. (2010). White matter abnormalities as a risk factor for postoperative delirium revealed by diffusion tensor imaging. Am. J. Geriatr. Psychiatry 18, 743–753. doi: 10.1097/JGP.0b013e3181d145c5
Shokri, H., and Ali, I. (2020). A randomized control trial comparing prophylactic dexmedetomidine versus clonidine on rates and duration of delirium in older adult patients undergoing coronary artery bypass grafting. J. Clin. Anesth. 61:109622. doi: 10.1016/j.jclinane.2019.09.016
Sieber, F. E., Neufeld, K. J., Gottschalk, A., Bigelow, G. E., Oh, E. S., Rosenberg, P. B., et al. (2018). Effect of depth of sedation in older patients undergoing hip fracture repair on postoperative delirium: the STRIDE randomized clinical trial. JAMA Surg. 153, 987–995. doi: 10.1001/jamasurg.2018.2602
Smith, T. O., Cooper, A., Peryer, G., Griffiths, R., Fox, C., and Cross, J. (2017). Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: a systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 32, 386–396. doi: 10.1002/gps.4655
Spies, C. D., Knaak, C., Mertens, M., Brockhaus, W. R., Shadenok, A., Wiebach, J., et al. (2021). Physostigmine for prevention of postoperative delirium and long-term cognitive dysfunction in liver surgery: a double-blinded randomised controlled trial. Eur. J. Anaesthesiol. 38, 943–956. doi: 10.1097/eja.0000000000001456
Stagno, D., Gibson, C., and Breitbart, W. (2004). The delirium subtypes: a review of prevalence, phenomenology, pathophysiology, and treatment response. Palliat. Support. Care 2, 171–179. doi: 10.1017/s1478951504040234
Staus, R. (2011). Delirium in the older adult orthopaedic patient: predisposing, precipitating, and organic factors. Orthop. Nurs. 30, 231–238; quiz 239–240. doi: 10.1097/NOR.0b013e3182247c79
Sugawara, H., Koyama, A., Maruyama, T., Koda, Y., Fukunaga, H., Ishikawa, T., et al. (2022). Prospective clinical intervention study of aripiprazole and risperidone in the management of postoperative delirium in elderly patients after cardiovascular surgery. Psychiatry Clin. Neurosci. 76, 531–533. doi: 10.1111/pcn.13446
Swarbrick, C. J., and Partridge, J. S. L. (2022). Evidence-based strategies to reduce the incidence of postoperative delirium: a narrative review. Anaesthesia 77, 92–101. doi: 10.1111/anae.15607
Tachi, K., Fukuda, T., and Tanaka, M. (2021). Olanzapine attenuates postoperative cognitive dysfunction in adult rats. Heliyon 7:e06218. doi: 10.1016/j.heliyon.2021.e06218
Tantardini, V., Roca, F., Bahri, O., Compere, V., Dujardin, F., and Chassagne, P. (2020). Intraoperative hypotension and delirium in patients with hip fracture. Geriatr. Psychol. Neuropsychiatr. Vieill. 18, 25–33. doi: 10.1684/pnv.2019.0824
Tesh, R. A., Sun, H., Jing, J., Westmeijer, M., Neelagiri, A., Rajan, S., et al. (2022). VE-CAM-S: visual EEG-based grading of delirium severity and associations with clinical outcomes. Crit. Care Explor. 4:e0611. doi: 10.1097/cce.0000000000000611
Thisayakorn, P., Tangwongchai, S., Tantavisut, S., Thipakorn, Y., Sukhanonsawat, S., Wongwarawipat, T., et al. (2021). Immune, blood cell, and blood gas biomarkers of delirium in elderly individuals with hip fracture surgery. Dement. Geriatr. Cogn. Disord. 50, 161–169. doi: 10.1159/000517510
Tian, Y., Chen, K. Y., Liu, L. D., Dong, Y. X., Zhao, P., and Guo, S. B. (2018). Sevoflurane exacerbates cognitive impairment induced by Aβ (1-40) in rats through initiating neurotoxicity, Neuroinflammation, and neuronal apoptosis in rat hippocampus. Mediat. Inflamm. 2018:3802324. doi: 10.1155/2018/3802324
Tillemans, M. P. H., Butterhoff-Terlingen, M. H., Stuffken, R., Vreeswijk, R., Egberts, T. C. G., and Kalisvaart, K. J. (2021). The effect of the anticholinergic burden on duration and severity of delirium in older hip-surgery patients with and without haloperidol prophylaxis: a post hoc analysis. Brain Behav. 11:e2404. doi: 10.1002/brb3.2404
Trzepacz, P. T. (2000). Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin. Clin. Neuropsychiatry 5, 132–148. doi: 10.153/SCNP00500132
Tsang, K. S., Page, J., and Mackenney, P. (2013). Can intravenous paracetamol reduce opioid use in preoperative hip fracture patients? Orthopedics 36, 20–24. doi: 10.3928/01477447-20130122-53
van Sleuwen, M., Sun, H., Eckhardt, C., Neelagiri, A., Tesh, R. A., Westmeijer, M., et al. (2022). Physiological assessment of delirium severity: the electroencephalographic confusion assessment method severity score (E-CAM-S). Crit. Care Med. 50, e11–e19. doi: 10.1097/ccm.0000000000005224
Vlisides, P., and Avidan, M. (2019). Recent advances in preventing and managing postoperative delirium. F1000Res :8. doi: 10.12688/f1000research.16780.1
Wang, C. G., Qin, Y. F., Wan, X., Song, L. C., Li, Z. J., and Li, H. (2018). Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J. Orthop. Surg. Res. 13:186. doi: 10.1186/s13018-018-0897-8
Wang, Y., Tang, J., Zhou, F., Yang, L., and Wu, J. (2017). Comprehensive geriatric care reduces acute perioperative delirium in elderly patients with hip fractures: a meta-analysis. Medicine 96:e7361. doi: 10.1097/md.0000000000007361
Wang, L., Zhang, T., Huang, L., and Peng, W. (2020). Comparison between Dexmedetomidine and midazolam for sedation in patients with intubation after Oral and maxillofacial surgery. Biomed Res. Int. 2020, 7082597–7082596. doi: 10.1155/2020/7082597
Watne, L. O., Idland, A. V., Fekkes, D., Raeder, J., Frihagen, F., Ranhoff, A. H., et al. (2016). Increased CSF levels of aromatic amino acids in hip fracture patients with delirium suggests higher monoaminergic activity. BMC Geriatr. 16:149. doi: 10.1186/s12877-016-0324-0
Whitlock, E. L., Braehler, M. R., Kaplan, J. A., Finlayson, E., Rogers, S. E., Douglas, V., et al. (2020). Derivation, validation, sustained performance, and clinical impact of an electronic medical record-based perioperative delirium risk stratification tool. Anesth. Analg. 131, 1901–1910. doi: 10.1213/ane.0000000000005085
Wittmann, M., Kirfel, A., Jossen, D., Mayr, A., and Menzenbach, J. (2022). The impact of perioperative and predisposing risk factors on the development of postoperative delirium and a possible gender difference. Geriatrics (Basel, Switzerland) 7:65. doi: 10.3390/geriatrics7030065
Wong, C. L., Holroyd-Leduc, J., Simel, D. L., and Straus, S. E. (2010). Does this patient have delirium?: value of bedside instruments. JAMA 304, 779–786. doi: 10.1001/jama.2010.1182
Xing, H., Xiang, D., Li, Y., Ji, X., and Xie, G. (2020). Preoperative prognostic nutritional index predicts postoperative delirium in elderly patients after hip fracture surgery. Psychogeriatrics 20, 487–494. doi: 10.1111/psyg.12511
Xu, Z., Tang, Z., Yao, J., Liang, D., Jin, F., Liu, Y., et al. (2022). Comparison of low-dose morphine intrathecal analgesia and sufentanil PCIA in elderly patients with hip fracture undergoing single spinal anesthesia - a randomized clinical trial. BMC Anesthesiol. 22:124. doi: 10.1186/s12871-022-01677-7
Yang, S., Gu, C., Mandeville, E. T., Dong, Y., Esposito, E., Zhang, Y., et al. (2017). Anesthesia and surgery impair blood-brain barrier and cognitive function in mice. Front. Immunol. 8:902. doi: 10.3389/fimmu.2017.00902
Yang, Y., Zhao, X., Dong, T., Yang, Z., Zhang, Q., and Zhang, Y. (2017). Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin. Exp. Res. 29, 115–126. doi: 10.1007/s40520-016-0541-6
Zeng, H., Li, Z., He, J., and Fu, W. (2019). Dexmedetomidine for the prevention of postoperative delirium in elderly patients undergoing noncardiac surgery: a meta-analysis of randomized controlled trials. PLoS One 14:e0218088. doi: 10.1371/journal.pone.0218088
Zhang, L., Zhang, J., Yang, L., Dong, Y., Zhang, Y., and Xie, Z. (2013). Isoflurane and sevoflurane increase interleukin-6 levels through the nuclear factor-kappa B pathway in neuroglioma cells. Br. J. Anaesth. 110, i82–i91. doi: 10.1093/bja/aet115
Keywords: postoperative delirium, geriatric patients, hip fractures, orthogeriatrics, prevention, treatment
Citation: Chen Y, Liang S, Wu H, Deng S, Wang F, Lunzhu C and Li J (2022) Postoperative delirium in geriatric patients with hip fractures. Front. Aging Neurosci. 14:1068278. doi: 10.3389/fnagi.2022.1068278
Received: 12 October 2022; Accepted: 02 December 2022;
Published: 22 December 2022.
Edited by:
Yiying Zhang, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Nikhil Tondehal, Mount Sinai Beth Israel, United StatesCopyright © 2022 Chen, Liang, Wu, Deng, Wang, Lunzhu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Li, ZWZ5bGlqdW5wYXBlckAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.