
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging Neurosci., 04 December 2020
Sec. Parkinson’s Disease and Aging-related Movement Disorders
Volume 12 - 2020 | https://doi.org/10.3389/fnagi.2020.591640
Depression is a risk factor for subsequent Parkinson's disease (PD). Some patients with depression undergo acupuncture treatment because of other diseases in Taiwan. Therefore, the present study used data from Taiwan's National Health Insurance Research Database (NHIRD) to investigate the incidence of PD in patients having depression with and without acupuncture treatment. We conducted a retrospective study of a matched cohort of 48,981 patients with newly diagnosed depression between 2000 and 2012 who were selected from the NHIRD. The 1:1 propensity score method was utilized to match an equal number of patients (N = 9,189) in the acupuncture and non-acupuncture cohorts. We employed Cox proportional hazard models to evaluate the risk of PD. The cumulative incidence of PD in both cohorts was estimated using the Kaplan–Meier method, and the difference was examined through a log-rank test. Patients with depression who received acupuncture treatment demonstrated a lower risk of PD [adjusted hazard ratio (aHR) = 0.39, 95% confidence interval = 0.31–0.49] than those who did not undergo acupuncture treatment, after adjusting for age, sex, insurance amount, geographic region, urbanization levels, comorbidities, and drugs. The cumulative incidence of PD was significantly lower in the acupuncture cohort than in the non-acupuncture cohort (log-rank test, p < 0.001). The database did not indicate the severity of depression and acupoints. The results suggest that acupuncture treatment significantly reduced the development of PD in patients with depression; however, a future study should be conducted to provide more objective evidence.
According to the World Health Organization's (WHO) estimation, depression had the third highest global socioeconomic burden in 2008, and the ranking is estimated to increase to the first in 2030 (Malhi and Mann, 2018). Depression affected approximately 350 million people of all ages worldwide in 2012 (Marcus et al., 2012). Additionally, WHO estimated a 12-month prevalence of 3.2% for depression in 60 countries in 2003 (Moussavi et al., 2007; Kessler and Bromet, 2013). According to an epidemiological study in Canada, in 2002, the prevalence of depression was 5.0% in women and 2.9% in men, and after 10 years, the prevalence had increased to 5.8 and 3.6%, respectively (Albert, 2015). Several reports have indicated that patients with depression undergoing antidepressant treatment demonstrate increased incidence of Parkinson's disease (PD) (Alonso et al., 2009; Gustafsson et al., 2015). Moreover, studies have highlighted that depression is associated with stroke, cardiovascular disease, hypertension, diabetes (Thomas et al., 2004), and PD (Gustafsson et al., 2015). PD is a common and chronic brain degenerative disease caused by dopaminergic neurodegeneration in the substantia nigra pars compacta (SNpc) in the midbrain, which results in dopamine depletion in the striatum, causing motor symptoms (Kalia and Lang, 2015). Depression is thought to be a causal risk factor for PD (Shen et al., 2013; Leentjens, 2015), and studies have examined the association between depression and PD (Schuurman et al., 2002; Leentjens et al., 2013; Shen et al., 2013; Leentjens, 2015; Wang et al., 2018). A study found that depression may be an early precursor symptom of PD (Gustafsson et al., 2015). A retrospective cohort study indicated a strong relationship between depression and PD, and the hazard ratio (HR) with corresponding 95% confidence interval (CI) was 3.13 (1.95–5.01) for patients with depression compared with patients without depression (Schuurman et al., 2002). Thus, how to reduce the incidence of PD among patients with depression undergoing antidepressant treatment is crucial.
Acupuncture is a traditional and unique medical treatment in Asia. It has been in use for more than 2,500 years and is very popular due to its ease of administration, wide application, and rapid effects. Acupuncture is also an effective and safe treatment for depression, and after antidepressants, it is the second most popular treatment option for depression (Zhang et al., 2010). One study revealed that acupuncture treatment reduces the risk of stroke in patients with depression (Chen et al., 2019).
Since Taiwan's mandatory National Health Insurance (NHI) program was officially implemented in 1995, it has covered more than 98% of the population of Taiwan (Lee et al., 2010). The National Health Insurance Research Database (NHIRD) is a nationwide high-coverage database containing the data of insurants of the single-payer health insurance program in Taiwan. This database comprises medical information, including inpatient and outpatient records and prescriptions of western drugs and Chinese herbal medicines administered to each patient. An increasing number of people opt for Chinese medicine treatment in Taiwan because the treatment is covered by the NHI program (Wu et al., 2018). Because acupuncture treatment has been confirmed to be an alternative treatment option for several diseases, including stroke (Lu et al., 2017), depression (Zhang et al., 2010; MacPherson, 2014), and PD (Rajendran et al., 2001; Tamtaji et al., 2019). Depression affects most of patients with PD. In a clinical trial, acupuncture treatment decreases the depression scores and the Unified Parkinson's Disease Rating Scale (UPDRS) sub-scores among patients with PD (Yeo et al., 2018). Therefore, we'd like to clarify whether acupuncture reduces the risk of PD in depressive cohort. In the present study, we hypothesize that acupuncture treatment in patients with depression reduces the incidence of PD. Therefore, in this large population cohort study, the association between acupuncture treatment and the risk of PD was evaluated in 18,378 patients with depression from 2000 to 2012 identified from the NHIRD.
The present study was conducted using data from the Longitudinal Health Insurance Database (LHID 2000), comprising 1 million patients randomly selected from the NHIRD. The identification details of study subjects were encrypted before the database was released for research. All historical diagnoses in the database were coded according to the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). The study was approved by the Research Ethics Committee of China Medical University and Hospital in Taiwan (CMUH-104-REC2-115-CR4).
This study examined the risk of PD in patients having depression with or without acupuncture treatment, for which patients with depression were identified according to the following diagnostic codes: ICD-9-CM: 296.2, 296.3, 296.82, 300.4, 309.0, 309.1, 309.28, and 311. Depression cases were that were diagnosed by psychiatrists and involved at least two outpatient visits and one recorded hospitalization were included in the study. The case group included patients with depression had undergone acupuncture treatment after being diagnosed with depression. The acupuncture procedure codes were as follows: B41, B42, B45, B46, B80-B84, B90-B94, P27041, P31103, P32103, and P33031, and the following electroacupuncture (EA) codes were used: B43, B44, B86-B89, and P33032. The control group comprised patients having depression without any medical record of receiving traditional Chinese medicines and acupuncture treatment. The date of the first acupuncture treatment was set as the index date. Each case was 1:1 propensity score matched with a control by age, gender, depression diagnosis year, index year, comorbidities, and medications (Figure 1). The comorbidities comprised diabetes (ICD-9-CM: 250), hypertension (ICD-9-CM: 401–405), hyperlipidemia (ICD-9-CM: 272), congestive heart failure (ICD-9-CM: 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, and 428), anxiety (ICD-9-CM: 300.0, 300.2, 300.3, 308.3, and 309.81), alcoholism (ICD-9-CM: 291, 303, 305.00, 305.01, 305.02, 305.03, 790.3, and V11.3), smoking (ICD-9-CM: 305.1), obesity (ICD-9-CM: 278), traumatic brain injury (TBI) (ICD-9-CM: 910, 850–854), and stroke (ICD-9-CM: 430–438), and medications included non-steroidal anti-inflammatory drugs (NSAIDs), oral steroids, statins, and antidepressants. The follow-up period was from the index date to PD diagnosis, withdrawal from the NHI program, or December 31, 2013.
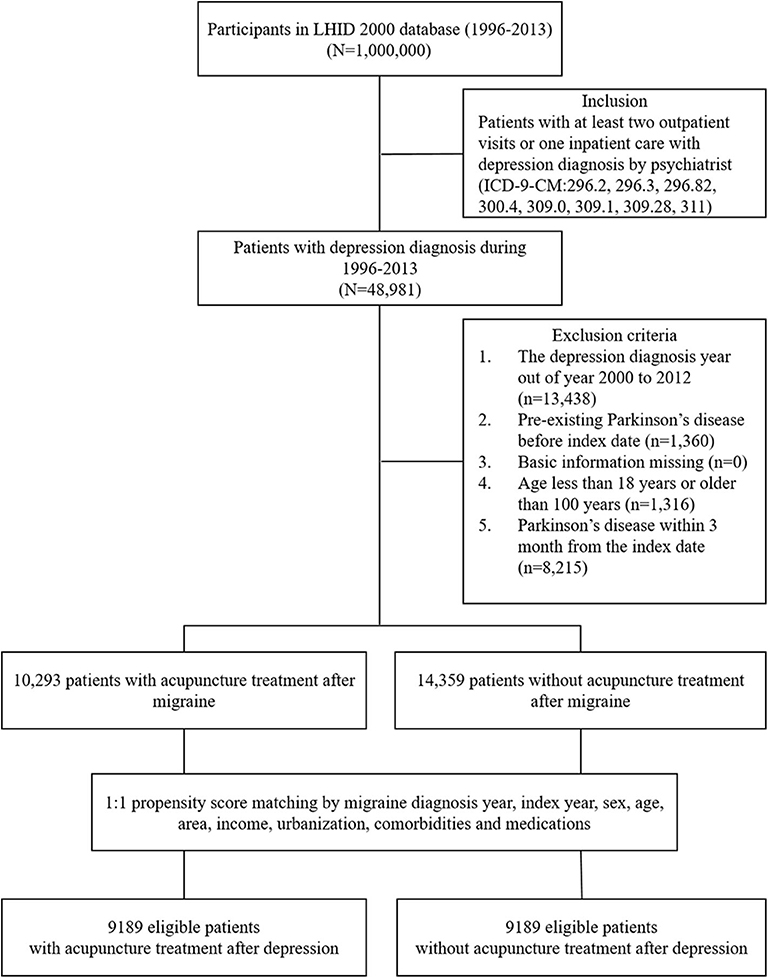
Figure 1. Study population flowchart. We identified 48,981 eligible newly diagnosed depression patients between 1996 and 2013. After using the 1:1 propensity score to match by sex, age, comorbidities, and drugs used, the groups of acupuncture users and acupuncture non-users each contained 9,189 patients. LHID 2000, Longitudinal Health Insurance Database 2000, NHI, National Health Insurance.
Continuous and categorical variables were compared between the two cohorts using the t-test and chi-square test. To determine the risk of PD, Cox proportional hazard models were used to calculate HRs, adjusted hazard ratios (aHRs), and 95% CIs. Multivariate stratification analysis was performed to evaluate the risk of PD in different subgroups. The cumulative incidence of PD in the two cohorts was estimated using the Kaplan–Meier method, and the difference was tested through a log-rank test. All statistical analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC, USA). The cumulative incidence curve was constructed using R software. A two-side p < 0.05 was considered significant.
Among the 18,378 eligible study subjects, 9,189 patients with depression had received acupuncture treatment (acupuncture group), and the remaining 9,189 patients with depression had never received acupuncture treatment (non-acupuncture group) (Table 1). Among all patients, 60% were female, and the mean age was 42.9 years. Gender, age, insurance amount, urbanization levels, comorbidities, and medications demonstrated no significant difference between the two groups after matching (p > 0.05); however, geographic region was statistically significant (p < 0.001). The majority of patients in the acupuncture group were treated with manual acupuncture (87.9%); 3.2% were treated with EA, and 9.0% received both. The mean number of acupuncture visits was 7.2 times during the study period.
Table 2 presents the disease categories/diagnoses of patients who received acupuncture treatment. The most frequent diseases were injury and poisoning (ICD-9-CM: 800–999, 57.6%) and musculoskeletal system and connective tissue (ICD-9-CM: 710–739, 63.0%).
Table 3 presents the number of PD cases and HRs between patients having depression with and without acupuncture treatment. The risk factors for PD comprised increasing age (aHR = 3.19, 95% CI = 2.25–4.54; aHR = 9.79, 95% CI = 6.63–14.44), hypertension (aHR = 1.52, 95% CI = 1.13–2.03), TBI (aHR = 1.60, 95% CI = 1.22–2.10), and other antidepressant drugs (aHR = 1.83, 95% CI = 1.38–2.44). Undergoing acupuncture treatment (aHR = 0.39, 95% CI = 0.31–0.49), higher insurance amount (aHR = 0.45, 95% CI = 0.28–0.72; aHR = 0.42, 95% CI = 0.19–0.89), and use of oral steroids (aHR = 0.56, 95% CI = 0.37–0.85) and statins (aHR = 0.66, 95% CI = 0.48–0.90) were protective factors of PD.
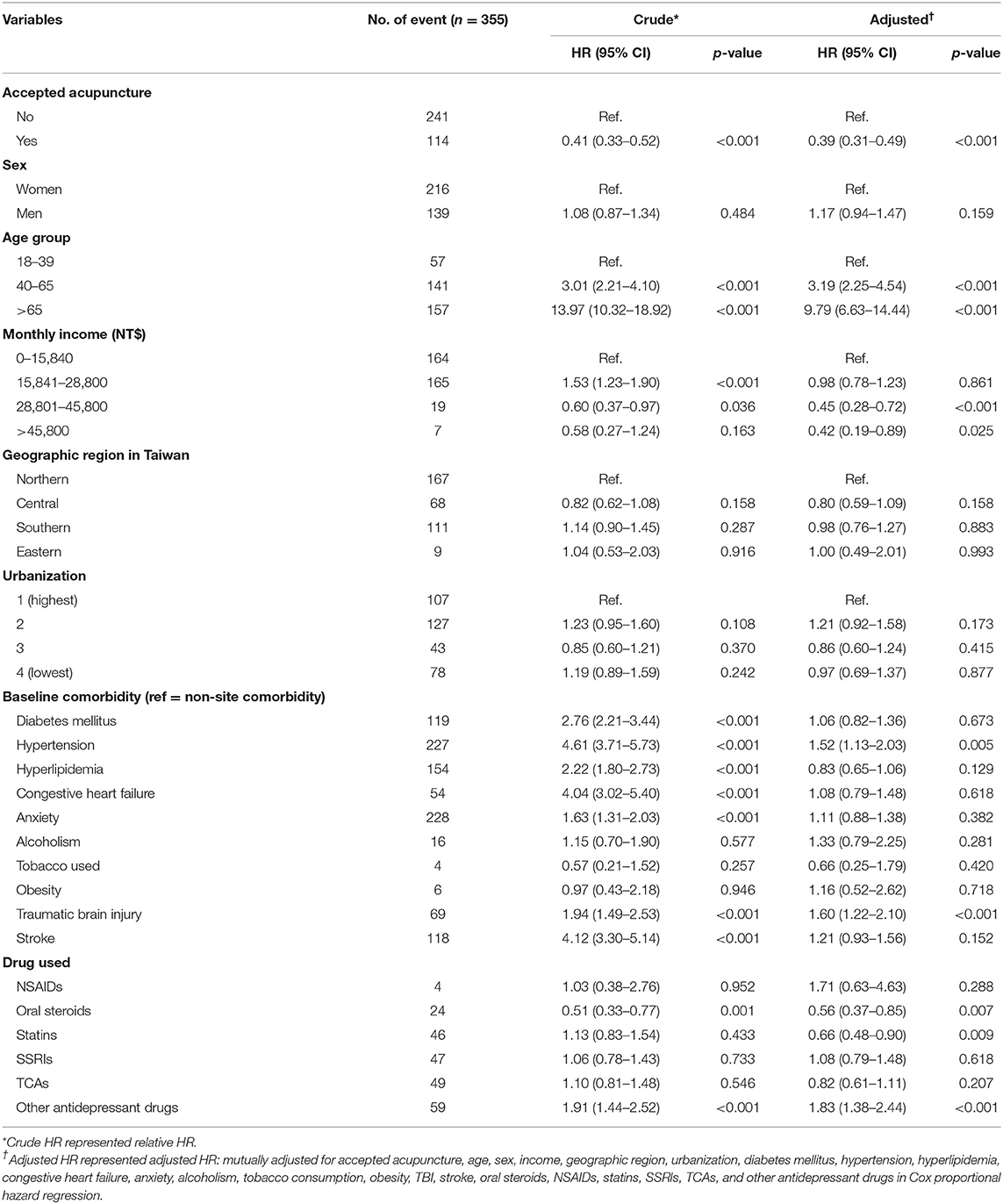
Table 3. Cox proportional hazard models with hazard ratios and 95% confidence intervals of PD associated with acupuncture and covariates among patients with depression.
Multivariate stratification analysis demonstrated decreasing risk of PD in different subgroups (Table 4), comprising female (aHR = 0.42, 95% CI = 0.32–0.56) and male (aHR = 0.38, 95% CI = 0.26–0.54) patients; those aged 18–39 years (aHR = 0.31, 95% CI = 0.17–0.57), 40–65 years (aHR = 0.43, 95% CI = 0.30–0.60), and more than 65 years (aHR = 0.36, 95% CI = 0.26–0.51); those with lower income (aHR = 0.34, 95% CI = 0.25–0.48; aHR = 0.42, 95% CI = 0.31–0.59; aHR = 0.24, 95% CI = 0.07–0.79); those living in northern (aHR = 0.37, 95% CI = 0.27–0.52), central (aHR = 0.39, 95% CI = 0.23–0.65), and southern Taiwan (aHR = 0.42, 95% CI = 0.28–0.64); those with all levels of urbanization (aHR = 0.37, 95% CI = 0.25–0.56; aHR = 0.34, 95% CI = 0.23–0.49; aHR = 0.48, 95% CI = 0.25–0.91; aHR = 0.45, 95% CI = 0.28–0.72); those with diabetes (aHR = 0.38, 95% CI = 0.26–0.56), hypertension (aHR = 0.45, 95% CI = 0.34–0.60), hyperlipidemia (aHR = 0.44, 95% CI = 0.31–0.61), congestive heart failure (aHR = 0.56, 95% CI = 0.32–0.97), anxiety (aHR = 0.41, 95% CI = 0.31–0.54), alcoholism (aHR = 0.17, 95% CI = 0.05-0.64), TBI (aHR = 0.37, 95% CI = 0.22–0.62), and stroke (aHR = 0.55, 95% CI = 0.38–0.80); those using statins (aHR = 0.36, 95% CI = 0.19–0.67), selective serotonin reuptake inhibitors (SSRIs) (aHR = 0.43, 95% CI = 0.23–0.82), and other antidepressant drugs (aHR = 0.46, 95% CI = 0.27–0.79).
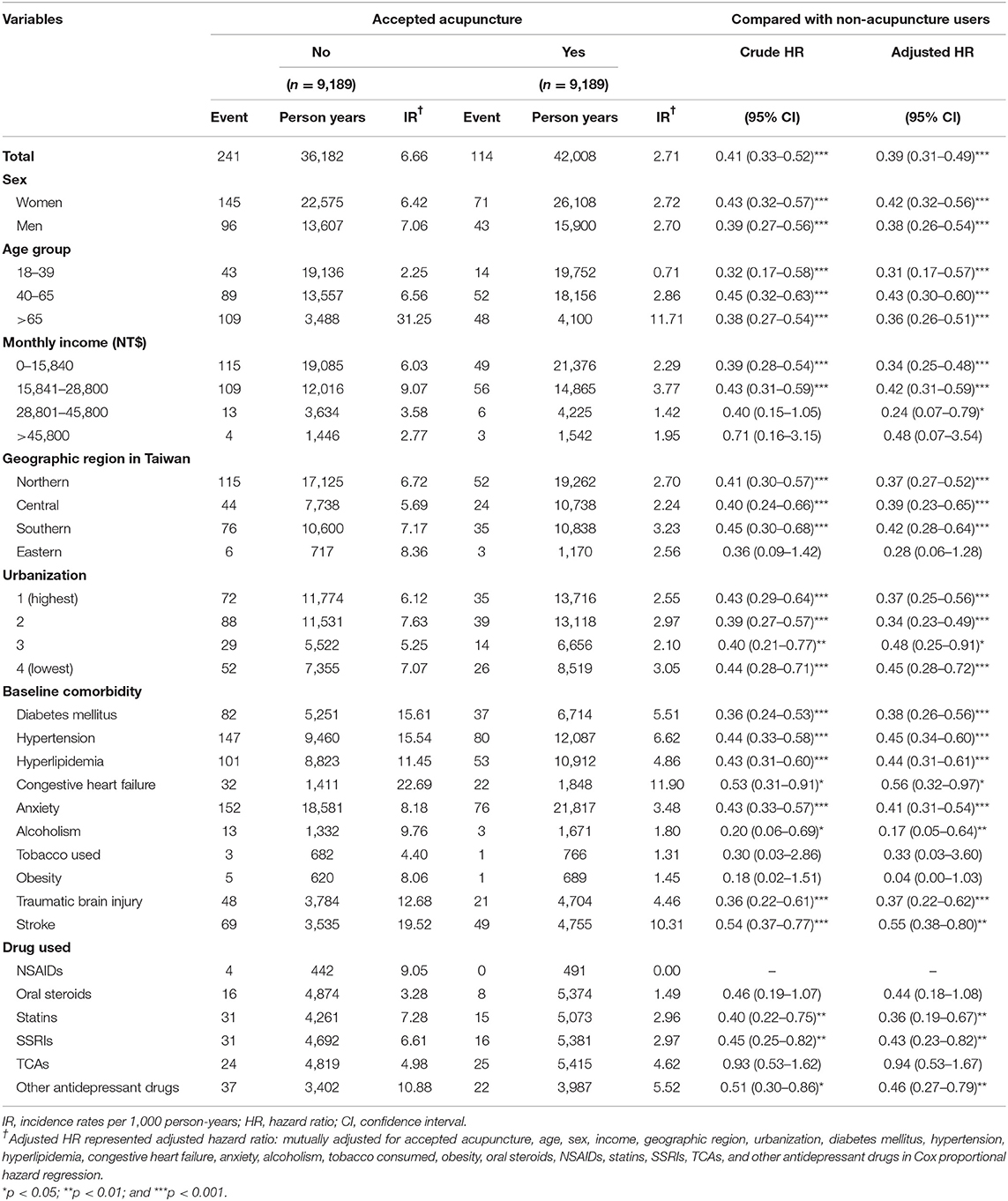
Table 4. Incidence rates, hazard ratios, and confidence intervals of PD for patients with depression with and without acupuncture treatment stratified by sex, age, comorbidities, and drugs.
Figure 2 demonstrates significantly lower cumulative incidence of PD among patients having depression with acupuncture treatment than in those without acupuncture cohort (p < 0.001).
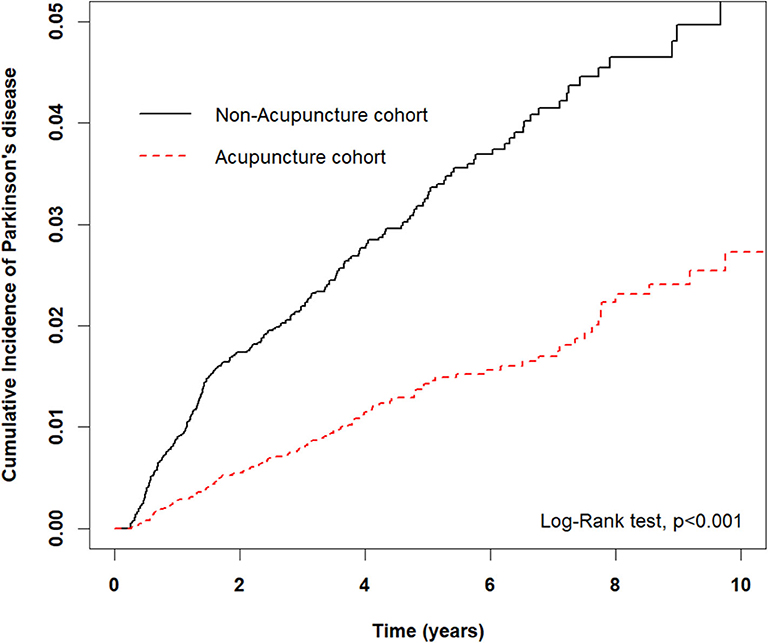
Figure 2. Cumulative incidence of PD between the acupuncture and non-acupuncture cohorts. The cumulative incidence of PD in the acupuncture cohort was significantly lower than that in the non-acupuncture cohort (log-rank test, p < 0.0001).
The results of the present study indicated that the incidence of PD was 61% lower among patients having depression with acupuncture treatment than among those without acupuncture treatment, suggesting acupuncture treatment decreases the risk of PD in patients with depression. After multiple adjustments for sex, age group, monthly income, geographic region, urbanization levels, baseline comorbidities, and drugs, acupuncture treatment was found to play a critical role in PD incidence reduction.
In our study, patients with depression who received acupuncture treatment were divided into two groups: those affected by injury and poisoning (57.6%) and those affected by musculoskeletal system and connective tissue disorders (63.0%). This results of correspondence with patients affected by injury and disease of the musculoskeletal system and connective tissue are the two major populations that undergo acupuncture treatment in Taiwan (Wu et al., 2018). TBI has been confirmed to increase the risk of depressive disorder (Chi et al., 2016), and head injury elevates the risk of depression by 59% (Orlovska et al., 2014).
Depression is the most common mental illness among PD patients. However, depression is also a risk factor for PD. Previous studies showed that acupuncture treatment would induce preventive effects in several disease populations associated with PD, including TBI (Li et al., 2017), stroke (Chen et al., 2019), hypertension (Terenteva et al., 2018), and diabetes mellitus (Shi et al., 2018). Therefore, we infer that acupuncture treatment also prevents from PD. This is the reason we conducted the study associated with the relationship between PD and depression with acupuncture treatment. In addition to affecting mental well-being and quality of life, depression is often associated with chronic musculoskeletal pain in patients. A study identified an elevated prevalence of depression in patients with chronic pain (Magni et al., 1990). Musculoskeletal system problems constitute another common disease found among patients with depression, which were treated with acupuncture in our study. Patients with depression often show symptoms such as muscle tension or soreness, sore bones and joints, headaches, and back pain. A study examined the association between depression and chronic pain in a general population in USA and discovered a high prevalence of depression symptoms among subjects with chronic pain (Magni et al., 1990). Generally, acupuncture is often adopted for treating most musculoskeletal problems of the four limbs, and EA is more effective for shoulder injuries (Cox et al., 2016). Furthermore, acupuncture is beneficial for treating chronic pain, and the relief effects of acupuncture may last up to 1 year (Vickers et al., 2018). A previous study identified the existence of abnormal connectivity in multiple brain regions, including cortical and subcortical areas, among patients with chronic pain (Apkarian et al., 2011), and acupuncture can regulate the activity of the pain matrix in various cortical and subcortical brain regions (Villarreal Santiago et al., 2016). Therefore, acupuncture can not only treat pain symptoms but also improve and activate specific areas of the brain.
PD occurs more commonly among elderly people, and the usual onset age is 50–79 years. PD is primarily a motor disease in which the nervous system gradually degenerates and results in decreased dopamine release in the brain. The present study also indicated that the risk of PD increases with advancing age. Patients aged 40–65 years demonstrated 3.19 times higher risk of PD, whereas the risk elevated to 9.79 times for those aged over 65 years. A study suggested that the incidence of PD in male patients increases till the age of 89 years (Driver et al., 2009). Accordingly, aging is recognized as a critical factor influencing PD incidence (Collier et al., 2017).
Of all baseline comorbidities associated with depression, hypertension significantly increases the risk of PD, except for TBI. Depression is closely related to changes in an individual's physical condition and may cause cardiovascular issues such as hypertension (Joynt et al., 2003). Patients with depression demonstrate a significantly increased risk of hypertension (Markovitz et al., 2001; Meyer et al., 2004). However, a meta-analysis suggested that hypertension is a risk factor for motor-stage PD (Hou et al., 2018), and it may influence PD patients' executive ability and memory (Jones et al., 2014). A previous study highlighted that up to 64.9% of patients with PD are affected by nocturnal hypertension (Tsukamoto et al., 2013). PD is considered to be a movement disorder caused by a massive loss of dopaminergic neurons in the SNpc. Chronic high blood pressure results in hypertensive vascular damage in several brain regions such as the basal ganglia and thalamus. This results in dysfunction and degeneration of dopaminergic neurons in the SN, in turn leading to dopamine transmission in the striatum (Qiu et al., 2011; Hou et al., 2018). However, acupuncture can be utilized as a combined treatment for alleviating hypertension and improving brain circulation and activation to maintain blood pressure and cognition (Sun et al., 2019).
The present study results also indicated that oral steroids and statin can decrease the risk of PD among patients with depression without acupuncture treatment. A study demonstrated that steroids can be used to treat central nervous system (CNS) diseases involving catecholamine by modulating brain activity and dopamine transmission (Sánchez et al., 2010). Steroids can not only protect neurons, glial cells, and blood vessels but also decrease the risks of affective disorders and PD (Garcia-Segura and Balthazart, 2009). In a national population-based study of patients with diabetes, statin users demonstrated a lower risk of PD than statin non-users did (Lin et al., 2016). Moreover, irrespective of whether simvastatin is used alone or in combination with metformin, the risk of PD is more reduced compared with when metformin is used alone (Brakedal et al., 2017). Additionally, a study of the 6-hydroxydopamine (6-OHDA) rat model, in which PD lesions were induced in animals, demonstrated the neuroprotective potential of statins against PD-like symptoms in rats (Kumar et al., 2012). Furthermore, a study showed that simvastatin halted dopaminergic neuronal loss induced by 6-OHDA in parkinsonian rat models and reported that simvastatin has neuroprotective potential against PD (Yan et al., 2011).
Increasing PD risk caused by depression can be attributed to several mechanisms such dopaminergic dysfunction, autonomic dysfunction, inflammation, and antidepressants (Lemke et al., 2004; Lee et al., 2013; Galts et al., 2019). Several studies have identified that dopamine, one of neurotransmitters in the brain, is associated with depression and PD (Lemke, 2008; Picillo et al., 2009). Compared with PD patients without depression, PD patients with depression have more frequent neuronal loss in the midbrain (Picillo et al., 2009). Moreover, lower dopamine levels were found in the brains of patients with TBI or hypertension (Yu et al., 1990; Lan et al., 2019). Acupuncture functions as a neuroprotector because it can increase dopamine levels in the brain and reduce brain atrophy by stimulating the acupoint of Baihui (GV20) in chronic cerebral hypoperfusion and ischemia-reperfusion injured rats (Chuang et al., 2007). Moreover, a study discovered that performing EA at Yanglingquan (GB34) and Taichong (LR3) acupoints could increase striatal dopamine levels in PD rodent models (Lin et al., 2017). Taken together, these results suggest that acupuncture may reduce the risk of PD in patients with depression, possibly by modulating dopamine function.
Except for hypertension, patients with depression are also critically affected by other cardiovascular diseases such as myocardial infarction and congestive heart failure. In other words, emotional problems may affect the autonomic nervous system (ANS) (Sgoifo et al., 2015). Therefore, ANS dysfunction resulting in vagal withdrawal facilitates the reduction of heart rate variability (HRV). Hence, compared with health subjects, reductions in HRV is reported in depression patients (Sgoifo et al., 2015). Autonomic failure in patients increases the risk of PD (Liepelt-Scarfone et al., 2015). Acupuncture not only alleviates autonomic responses by modulating the imbalance between sympathetic and parasympathetic activities but also stabilizes vagal activity in depression (Li et al., 2013; Noda et al., 2015). Several studies have reported that HRV increased significantly in patients with depression after acupuncture or EA (Shi et al., 2013, 2014). Acupuncture can reduce the risk of PD in patients with depression possibly partly from the modulation of acupuncture for ANS dysfunction.
Stress is associated with higher levels of proinflammatory cytokines, such as tumor necrosis factor-α (TNF-α) and interleukin (IL)-6, in patients with depression compared with healthy individuals (Galts et al., 2019). Several studies have shown increased levels of TNF-α, IL-6, and C-reactive protein (CRP) in patients with depression (Chen et al., 2016; Liu et al., 2019). Higher levels of proinflammatory cytokines in patients with depression are closely associated with a higher risk of PD. Both EA and acupuncture can significantly decrease TNF-α and IL-6 expression, which provides antidepressant effects and improves the hippocampal neuroinflammation in animal models of depression (Lu et al., 2016; Yue et al., 2018). In addition to TNF-α and IL-6, acupuncture significantly decreases the serum CRP level in another animal study (Qi et al., 2014). Therefore, acupuncture can reduce the development of PD in patients with depression, by possibly modulating the immune system.
Depression is associated with a decrease in monoamine neurotransmitters, including serotonin, norepinephrine, and dopamine; thus, the main pharmacological effect of antidepressants is that they enhance monoamine neurotransmission (Malhi and Mann, 2018). Several studies have reported that antidepressants increase the risk of PD. Both tricyclic antidepressants and SSRIs administered over 2–3 years may cause PD (Alonso et al., 2009; Zenesini et al., 2019). Several studies have reported that combining acupuncture and antidepressants is more effective than antidepressants alone over a 6-week period (Wang et al., 2014; Chan et al., 2015). A pilot study showed that acupuncture treatment using five acupoints (HT-7, LI-4, ST-36, SP-6, and LR-3) along with EA treatment using two acupoints (GV-20 and GV-24.5) is safe and effective for individuals with depression who are partially responsive or non-response to specific antidepressants (Yeung et al., 2011). To summarize, acupuncture reduces the risk of PD in patients with depression through multiple pathways, including the modulation of dopamine, ANS, immune system, and neurotransmitters.
The present study remains one question need to explanation; the mean number of acupuncture visits was 7.2 times only during the study period that is not enough to prevent the development of PD. We assume that acupuncture improves interest and enjoyment including in activities and increase the physical activity in patients with depression. Because regular physical exercise program can affect neuronal plasticity of the brain, repairing neuronal pathway before the occurrence of PD (Oliveira de Carvalho et al., 2018). The patients with depression are willing to receive another therapy aggressively; moreover, combining acupuncture and antidepressants may improve depressive disorder effectively (Chan et al., 2015) and then. In addition, no more than 15 visits of acupuncture treatment per month are allowed in Taiwan's NHI program. Some patients may receive additional acupuncture by self-pay which is not included in NHIRD database.
The present study had a few limitations. First, regarding data on depression, the NHIRD did not indicate the severity and duration of depression, and these factors possibly affected the incidence of PD. Second, the acupoints used in acupuncture treatments were not recorded in the NHIRD. Therefore, we were unable to clearly identify the acupoints that can treat depression and PD simultaneously. Third, the NHIRD does not contains laboratory data or brain images; therefore, no objective evidence could be found to explain the mechanism through which acupuncture reduces PD incidence in patients with depression, which warrants further study in the future. Fourth, because some PD cases may be late onset, the duration of the current study's follow-up period was insufficient. Double-blind, randomized clinical trials are required in the future.
The present study results indicated that the incidence of PD was lower among patients with depression who received acupuncture treatment than among those patients with depression who did not, suggesting that acupuncture reduces the development of PD. This effect of acupuncture is mediated through multiple pathways, including the modulation of dopamine, ANS, immune system, and neurotransmitters. However, more objective evidence from clinical trials including laboratory data and brain images is required.
The datasets presented in this article are not readily available because due to the legal restrictions imposed by the government of Taiwan in relation to the Personal Information Protection Act, the data used for this study cannot be made publicly available. Request for data can be sent as a formal proposal to the NHIRD. Requests to access the datasets should be directed to http://nhird.nhri.org.tw.
The studies involving human participants were reviewed and approved by the Research Ethics Committee of China Medical University and Hospital in Taiwan (CMUH-104-REC2-115-CR4). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
C-HH conceptualized the study and drafted the manuscript. M-CL performed the statistical analyses. C-HH and C-LH contributed to the interpretation of acupuncture data and finalized the manuscript. M-CL and C-HH contributed to the interpretation of statistical data. All authors contributed to the article and approved the submitted version.
This study was supported in part by China Medical University Hospital (DMR-107-210), the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004), China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-), Tseng-Lien Lin Foundation, Taichung, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. These funders had no role to play in study design, data collection and analysis, data interpretation, writing of the manuscript, or the decision to submit the article for publication. This study was also financially supported by the Chinese Medicine Research Center, China Medical University under the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education in Taiwan (CMRC-CENTER-0).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This study was conducted using data from the NHIRD, which was provided by the National Health Insurance Administration and the Ministry of Health and Welfare, and supervised by National Health Research Institutes. We would like to thank the management office for health data of China Medical University Hospital for collecting and analyzing the data used in this study.
PD, Parkinson's disease; HR, hazard ratio; aHR, adjusted hazard ratio; CI, confidential interval; NHI, National Health Insurance; NHIRD, National Health Insurance Research Database; WHO, World Health Organization; SNpc, substantia nigra pars compacta; UPDRS, the Unified Parkinson's Disease Rating Scale; ICD-9-CM, International Classification of Disease, Ninth Revision, Clinical Modification; TBI, traumatic brain injury; NSAIDs, non-steroidal anti-inflammatory drugs; 6-OHDA, 6-hydroxydopamine; HRV, heart rate variability; CRP, C-reactive protein; TNF-α, tumor necrosis factor-α; SSRIs, selective serotonin reuptake inhibitors; TCAs, tricyclic antidepressants; SNRIs, serotonin–norepinephrine reuptake inhibitors; NDRI, norepinephrine–dopamine reuptake inhibitor; SARI, serotonin antagonist and reuptake inhibitor; NaSSA, noradrenergic and specific serotonergic antidepressant.
Albert, P. R. (2015). Why is depression more prevalent in women? J. Psychiatry Neurosci. 40, 219–221. doi: 10.1503/jpn.150205
Alonso, A., Rodríguez, L. A., Logroscino, G., and Hernán, M. A. (2009). Use of antidepressants and the risk of Parkinson's disease: a prospective study. J. Neurol. Neurosurg. Psychiatr. 80, 671–674. doi: 10.1136/jnnp.2008.152983
Apkarian, A. V., Hashmi, J. A., and Baliki, M. N. (2011). Pain and the brain: specificity and plasticity of the brain in clinical chronic pain. Pain 152, S49–64. doi: 10.1016/j.pain.2010.11.010
Brakedal, B., Haugarvoll, K., and Tzoulis, C. (2017). Simvastatin is associated with decreased risk of Parkinson disease. Ann. Neurol. 81, 329–330. doi: 10.1002/ana.24857
Chan, Y. Y., Lo, W. Y., Yang, S. N., Chen, Y. H., and Lin, J. G. (2015). The benefit of combined acupuncture and antidepressant medication for depression: a systematic review and meta-analysis. J. Affect. Disord. 176, 106–117. doi: 10.1016/j.jad.2015.01.048
Chen, L. Y., Yen, H. R., Sun, M. F., Lin, C. L., Chiang, J. H., and Lee, Y. C. (2019). Acupuncture treatment is associated with a decreased risk of developing stroke in patients with depression: a propensity-score matched cohort study. J. Affect. Disord. 250, 298–306. doi: 10.1016/j.jad.2019.03.020
Chen, W. W., Zhang, X., and Huang, W. J. (2016). Role of neuroinflammation in neurodegenerative diseases (review). Mol. Med. Rep. 13, 3391–3396. doi: 10.3892/mmr.2016.4948
Chi, Y. C., Wu, H. L., Chu, C. P., Huang, M. C., Lee, P. C., and Chen, Y. Y. (2016). Traumatic brain injury and affective disorder: a nationwide cohort study in Taiwan, 2000-2010. J. Affect. Disord. 191, 56–61. doi: 10.1016/j.jad.2015.11.035
Chuang, C. M., Hsieh, C. L., Li, T. C., and Lin, J. G. (2007). Acupuncture stimulation at Baihui acupoint reduced cerebral infarct and increased dopamine levels in chronic cerebral hypoperfusion and ischemia-reperfusion injured sprague-dawley rats. Am. J. Chin. Med. 35, 779–791. doi: 10.1142/S0192415X07005260
Collier, T. J., Kanaan, N. M., and Kordower, J. H. (2017). Aging and Parkinson's disease: different sides of the same coin? Mov. Disord. 32, 983–990. doi: 10.1002/mds.27037
Cox, J., Varatharajan, S., Côté, P., and Optima, C. (2016). Effectiveness of acupuncture therapies to manage musculoskeletal disorders of the extremities: a systematic review. J. Orthop. Sports Phys. Ther. 46, 409–429. doi: 10.2519/jospt.2016.6270
Driver, J. A., Logroscino, G., Gaziano, J. M., and Kurth, T. (2009). Incidence and remaining lifetime risk of Parkinson disease in advanced age. Neurology 72, 432–438. doi: 10.1212/01.wnl.0000341769.50075.bb
Galts, C. P. C., Bettio, L. E. B., Jewett, D. C., Yang, C. C., Brocardo, P. S., Rodrigues, A. L. S., et al. (2019). Depression in neurodegenerative diseases: common mechanisms and current treatment options. Neurosci. Biobehav. Rev. 102, 56–84. doi: 10.1016/j.neubiorev.2019.04.002
Garcia-Segura, L. M., and Balthazart, J. (2009). Steroids and neuroprotection: new advances. Front. Neuroendocrinol. 30, v–ix. doi: 10.1016/j.yfrne.2009.04.006
Gustafsson, H., Nordström, A., and Nordström, P. (2015). Depression and subsequent risk of Parkinson disease: a nationwide cohort study. Neurology 84, 2422–2429. doi: 10.1212/WNL.0000000000001684
Hou, L., Li, Q., Jiang, L., Qiu, H., Geng, C., Hong, J. S., et al. (2018). Hypertension and diagnosis of Parkinson's disease: a meta-analysis of cohort studies. Front. Neurol. 9:162. doi: 10.3389/fneur.2018.00162
Jones, J. D., Jacobson, C., Murphy, M., Price, C., Okun, M. S., and Bowers, D. (2014). Influence of hypertension on neurocognitive domains in nondemented Parkinson's disease patients. Parkinsons. Dis. 2014:507529. doi: 10.1155/2014/507529
Joynt, K. E., Whellan, D. J., and O'Connor, C. M. (2003). Depression and cardiovascular disease: mechanisms of interaction. Biol. Psychiatry 54, 248–261. doi: 10.1016/S0006-3223(03)00568-7
Kalia, L. V., and Lang, A. E. (2015). Parkinson's disease. Lancet 386, 896–912. doi: 10.1016/S0140-6736(14)61393-3
Kessler, R. C., and Bromet, E. J. (2013). The epidemiology of depression across cultures. Annu. Rev. Public Health 34, 119–138. doi: 10.1146/annurev-publhealth-031912-114409
Kumar, A., Sharma, N., Gupta, A., Kalonia, H., and Mishra, J. (2012). Neuroprotective potential of atorvastatin and simvastatin (HMG-CoA reductase inhibitors) against 6-hydroxydopamine (6-OHDA) induced Parkinson-like symptoms. Brain Res. 1471, 13–22. doi: 10.1016/j.brainres.2012.06.050
Lan, Y. L., Li, S., Lou, J. C., Ma, X. C., and Zhang, B. (2019). The potential roles of dopamine in traumatic brain injury: a preclinical and clinical update. Am. J. Transl. Res. 11, 2616–2631. doi: 10.1016/B978-0-12-812344-7.00002-9
Lee, Y., Lin, P. Y., Chang, Y. Y., Chong, M. Y., and Cheng, A. T. (2013). Antidepressant-induced tardive syndrome: a retrospective epidemiological study. Pharmacopsychiatry 46, 281–285. doi: 10.1055/s-0033-1354407
Lee, Y. C., Huang, Y. T., Tsai, Y. W., Huang, S. M., Kuo, K. N., McKee, M., et al. (2010). The impact of universal national health insurance on population health: the experience of Taiwan. BMC Health Serv. Res. 10:225. doi: 10.1186/1472-6963-10-225
Leentjens, A. F. (2015). Parkinson disease: depression-risk factor or early symptom in Parkinson disease? Nat. Rev. Neurol. 11, 432–433. doi: 10.1038/nrneurol.2015.126
Leentjens, A. F., Moonen, A. J., Dujardin, K., Marsh, L., Martinez-Martin, P., Richard, I. H., et al. (2013). Modeling depression in Parkinson disease: disease-specific and nonspecific risk factors. Neurology 81, 1036–1043. doi: 10.1212/WNL.0b013e3182a4a503
Lemke, M. R. (2008). Dopamine agonists in the treatment of non-motor symptoms of Parkinson's disease: depression. Eur. J. Neurol. 15(Suppl. 2), 9–14. doi: 10.1111/j.1468-1331.2008.02213.x
Lemke, M. R., Fuchs, G., Gemende, I., Herting, B., Oehlwein, C., Reichmann, H., et al. (2004). Depression and Parkinson's disease. J. Neurol. 251(Suppl. 6), Vi/24–27. doi: 10.1055/s-2004-833661
Li, Q. Q., Shi, G. X., Xu, Q., Wang, J., Liu, C. Z., and Wang, L. P. (2013). Acupuncture effect and central autonomic regulation. Evid. Based Complement. Alternat. Med. 2013:267959. doi: 10.1155/2013/267959
Li, X., Chen, C., Yang, X., Wang, J., Zhao, M. L., Sun, H., et al. (2017). Acupuncture improved neurological recovery after traumatic brain injury by activating BDNF/TrkB pathway. Evid. Based Complement. Alternat. Med. 2017:8460145. doi: 10.1155/2017/8460145
Liepelt-Scarfone, I., Pilotto, A., Müller, K., Bormann, C., Gauss, K., Wurster, I., et al. (2015). Autonomic dysfunction in subjects at high risk for Parkinson's disease. J. Neurol. 262, 2643–2652. doi: 10.1007/s00415-015-7888-z
Lin, J. G., Chen, C. J., Yang, H. B., Chen, Y. H., and Hung, S. Y. (2017). Electroacupuncture promotes recovery of motor function and reduces dopaminergic neuron degeneration in rodent models of Parkinson's disease. Int. J. Mol. Sci. 18:1846. doi: 10.3390/ijms18091846
Lin, K. D., Yang, C. Y., Lee, M. Y., Ho, S. C., Liu, C. K., and Shin, S. J. (2016). Statin therapy prevents the onset of Parkinson disease in patients with diabetes. Ann. Neurol. 80, 532–540. doi: 10.1002/ana.24751
Liu, C. H., Zhang, G. Z., Li, B., Li, M., Woelfer, M., Walter, M., et al. (2019). Role of inflammation in depression relapse. J. Neuroinflamm. 16:90. doi: 10.1186/s12974-019-1475-7
Lu, C. Y., Huang, H. C., Chang, H. H., Yang, T. H., Chang, C. J., Chang, S. W., et al. (2017). Acupuncture therapy and incidence of depression after stroke. Stroke 48, 1682–1684. doi: 10.1161/STROKEAHA.117.016959
Lu, J., Shao, R. H., Hu, L., Tu, Y., and Guo, J. Y. (2016). Potential antiinflammatory effects of acupuncture in a chronic stress model of depression in rats. Neurosci. Lett. 618, 31–38. doi: 10.1016/j.neulet.2016.02.040
MacPherson, H. (2014). Acupuncture for depression: state of the evidence. Acupunct. Med. 32, 304–305. doi: 10.1136/acupmed-2014-010614
Magni, G., Caldieron, C., Rigatti-Luchini, S., and Merskey, H. (1990). Chronic musculoskeletal pain and depressive symptoms in the general population. An analysis of the 1st national health and nutrition examination survey data. Pain 43, 299–307. doi: 10.1016/0304-3959(90)90027-B
Malhi, G. S., and Mann, J. J. (2018). Depression. Lancet 392, 2299–2312. doi: 10.1016/S0140-6736(18)31948-2
Marcus, M., Yasamy, M. T., Ommeren, M., Chisholm, D., and Saxena, S. (2012). Depression: a global public health concern. World Health Org. Paper Depres. 6–8. doi: 10.1037/e517532013-004
Markovitz, J. H., Jonas, B. S., and Davidson, K. (2001). Psychologic factors as precursors to hypertension. Curr. Hypertens. Rep. 3, 25–32. doi: 10.1007/s11906-001-0074-y
Meyer, C. M., Armenian, H. K., Eaton, W. W., and Ford, D. E. (2004). Incident hypertension associated with depression in the baltimore epidemiologic catchment area follow-up study. J. Affect. Disord. 83, 127–133. doi: 10.1016/j.jad.2004.06.004
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., and Ustun, B. (2007). Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet 370, 851–858. doi: 10.1016/S0140-6736(07)61415-9
Noda, Y., Izuno, T., Tsuchiya, Y., Hayasaka, S., Matsumoto, K., Murakami, H., et al. (2015). Acupuncture-induced changes of vagal function in patients with depression: a preliminary sham-controlled study with press needles. Complement. Ther. Clin. Pract. 21, 193–200. doi: 10.1016/j.ctcp.2015.07.002
Oliveira de Carvalho, A., Filho, A. S. S., Murillo-Rodriguez, E., Rocha, N. B., Carta, M. G., and Machado, S. (2018). Physical exercise for parkinson's disease: clinical and experimental evidence. Clin. Pract. Epidemiol. Ment. Health 14, 89–98. doi: 10.2174/1745017901814010089
Orlovska, S., Pedersen, M. S., Benros, M. E., Mortensen, P. B., Agerbo, E., and Nordentoft, M. (2014). Head injury as risk factor for psychiatric disorders: a nationwide register-based follow-up study of 113,906 persons with head injury. Am. J. Psychiatry 171, 463–469. doi: 10.1176/appi.ajp.2013.13020190
Picillo, M., Rocco, M., and Barone, P. (2009). Dopamine receptor agonists and depression in Parkinson's disease. Parkinsonism Relat. Disord. 15(Suppl. 4), S81–84. doi: 10.1016/S1353-8020(09)70841-7
Qi, Y. C., Xiao, X. J., Duan, R. S., Yue, Y. H., Zhang, X. L., Li, J. T., et al. (2014). Effect of acupuncture on inflammatory cytokines expression of spastic cerebral palsy rats. Asian Pac. J. Trop. Med. 7, 492–495. doi: 10.1016/S1995-7645(14)60081-X
Qiu, C., Hu, G., Kivipelto, M., Laatikainen, T., Antikainen, R., Fratiglioni, L., et al. (2011). Association of blood pressure and hypertension with the risk of Parkinson disease: the national FINRISK study. Hypertension 57, 1094–1100. doi: 10.1161/HYPERTENSIONAHA.111.171249
Rajendran, P. R., Thompson, R. E., and Reich, S. G. (2001). The use of alternative therapies by patients with Parkinson's disease. Neurology 57, 790–794. doi: 10.1212/WNL.57.5.790
Sánchez, M. G., Bourque, M., Morissette, M., and Di Paolo, T. (2010). Steroids-dopamine interactions in the pathophysiology and treatment of CNS disorders. CNS Neurosci. Ther. 16, e43–71. doi: 10.1111/j.1755-5949.2010.00163.x
Schuurman, A. G., van den Akker, M., Ensinck, K. T., Metsemakers, J. F., Knottnerus, J. A., Leentjens, A. F., et al. (2002). Increased risk of Parkinson's disease after depression: a retrospective cohort study. Neurology 58, 1501–1504. doi: 10.1212/WNL.58.10.1501
Sgoifo, A., Carnevali, L., Alfonso Mde, L., and Amore, M. (2015). Autonomic dysfunction and heart rate variability in depression. Stress 18, 343–352. doi: 10.3109/10253890.2015.1045868
Shen, C. C., Tsai, S. J., Perng, C. L., Kuo, B. I., and Yang, A. C. (2013). Risk of parkinson disease after depression: a nationwide population-based study. Neurology 81, 1538–1544. doi: 10.1212/WNL.0b013e3182a956ad
Shi, L., Feng, L., Yang, Y., Li, X., Zhang, M., Zhang, Y., et al. (2018). Prevention of type 2 diabetes mellitus with acupuncture: protocol for a systematic review and meta-analysis. Medicine 97:e13355. doi: 10.1097/MD.0000000000013355
Shi, X., Litscher, G., Wang, H., Wang, L., Zhao, Z., Litscher, D., et al. (2013). Continuous auricular electroacupuncture can significantly improve heart rate variability and clinical scores in patients with depression: first results from a transcontinental study. Evid. Based Complement. Alternat. Med. 2013:894096. doi: 10.1155/2013/894096
Shi, X., Wang, H., Wang, L., Zhao, Z., Litscher, D., Tao, J., et al. (2014). Can tongue acupuncture enhance body acupuncture? First results from heart rate variability and clinical scores in patients with depression. Evid. Based Complement. Alternat. Med. 2014:329746. doi: 10.1155/2014/329746
Sun, J., Ashley, J., and Kellawan, J. M. (2019). Can acupuncture treatment of hypertension improve brain health? A mini review. Front. Aging Neurosci. 11:240. doi: 10.3389/fnagi.2019.00240
Tamtaji, O. R., Naderi Taheri, M., Notghi, F., Alipoor, R., Bouzari, R., and Asemi, Z. (2019). The effects of acupuncture and electroacupuncture on Parkinson's disease: current status and future perspectives for molecular mechanisms. J. Cell. Biochem. 120, 12156–12166. doi: 10.1002/jcb.28654
Terenteva, N., Chernykh, O., Sanchez-Gonzalez, M. A., and Wong, A. (2018). Acupuncture therapy improves vascular hemodynamics and stiffness in middle-age hypertensive individuals. Complement. Ther. Clin. Pract. 30, 14–18. doi: 10.1016/j.ctcp.2017.11.002
Thomas, A. J., Kalaria, R. N., and O'Brien, J. T. (2004). Depression and vascular disease: what is the relationship? J. Affect. Disord. 79, 81–95. doi: 10.1016/S0165-0327(02)00349-X
Tsukamoto, T., Kitano, Y., and Kuno, S. (2013). Blood pressure fluctuation and hypertension in patients with Parkinson's disease. Brain Behav. 3, 710–714. doi: 10.1002/brb3.179
Vickers, A. J., Vertosick, E. A., Lewith, G., MacPherson, H., Foster, N. E., Sherman, K. J., et al. (2018). Acupuncture for chronic pain: update of an individual patient data meta-analysis. J. Pain 19, 455–474. doi: 10.1016/j.jpain.2017.11.005
Villarreal Santiago, M., Tumilty, S., Macznik, A., and Mani, R. (2016). Does acupuncture alter pain-related functional connectivity of the central nervous system? A systematic review. J. Acupunct. Meridian Stud. 9, 167–177. doi: 10.1016/j.jams.2015.11.038
Wang, S., Mao, S., Xiang, D., and Fang, C. (2018). Association between depression and the subsequent risk of Parkinson's disease: a meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 86, 186–192. doi: 10.1016/j.pnpbp.2018.05.025
Wang, T., Wang, L., Tao, W., and Chen, L. (2014). Acupuncture combined with an antidepressant for patients with depression in hospital: a pragmatic randomised controlled trial. Acupunct. Med. 32, 308–312. doi: 10.1136/acupmed-2013-010469
Wu, M. Y., Lee, Y. C., Lin, C. L., Huang, M. C., Sun, M. F., and Yen, H. R. (2018). Trends in use of acupuncture among adults in Taiwan from 2002 to 2011: a nationwide population-based study. PLoS ONE 13:e0195490. doi: 10.1371/journal.pone.0195490
Yan, J., Xu, Y., Zhu, C., Zhang, L., Wu, A., Yang, Y., et al. (2011). Simvastatin prevents dopaminergic neurodegeneration in experimental parkinsonian models: the association with anti-inflammatory responses. PLoS ONE 6:e20945. doi: 10.1371/journal.pone.0020945
Yeo, S., van den Noort, M., Bosch, P., and Lim, S. (2018). A study of the effects of 8-week acupuncture treatment on patients with Parkinson's disease. Medicine 97:e13434. doi: 10.1097/MD.0000000000013434
Yeung, A. S., Ameral, V. E., Chuzi, S. E., Fava, M., and Mischoulon, D. (2011). A pilot study of acupuncture augmentation therapy in antidepressant partial and non-responders with major depressive disorder. J. Affect. Disord. 130, 285–289. doi: 10.1016/j.jad.2010.07.025
Yu, Z. J., Lim, D. K., Hoskins, B., Rockhold, R. W., and Ho, I. K. (1990). Effects of acute and subacute cocaine administration on the CNS dopaminergic system in Wistar-Kyoto and spontaneously hypertensive rats: I. Levels of dopamine and metabolites. Neurochem. Res. 15, 613–619. doi: 10.1007/BF00973752
Yue, N., Li, B., Yang, L., Han, Q. Q., Huang, H. J., Wang, Y. L., et al. (2018). Electro-acupuncture alleviates chronic unpredictable stress-induced depressive- and anxiety-like behavior and hippocampal neuroinflammation in rat model of depression. Front. Mol. Neurosci. 11:149. doi: 10.3389/fnmol.2018.00149
Zenesini, C., Baldin, E., Vignatelli, L., Poluzzi, E., Antonazzo, I., Calandra-Buonaura, G., et al. (2019). Use of antidepressants and the risk of Parkinson's disease in the local health trust of bologna: a historical cohort study. J. Neurol. Sci. 405:116421. doi: 10.1016/j.jns.2019.08.006
Keywords: acupuncture, depression, incidence, Parkinson's disease, National Health Insurance Research Database (NHIRD), cohort study
Citation: Huang C-H, Lin M-C and Hsieh C-L (2020) Acupuncture Treatment Reduces Incidence of Parkinson's Disease in Patients With Depression: A Population-Based Retrospective Cohort Study in Taiwan. Front. Aging Neurosci. 12:591640. doi: 10.3389/fnagi.2020.591640
Received: 05 August 2020; Accepted: 11 November 2020;
Published: 04 December 2020.
Edited by:
Changiz Geula, Northwestern University, United StatesReviewed by:
Hi-Joon Park, Kyung Hee University, South KoreaCopyright © 2020 Huang, Lin and Hsieh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ching-Liang Hsieh, Y2xoc2llaEBtYWlsLmNtdWgub3JnLnR3
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.