- 1Department of Interventional Radiology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 2Interventional Institute of Zhengzhou University, Zhengzhou, China
- 3Interventional Treatment and Clinical Research Center of Henan Province, Zhengzhou, China
- 4Department of Magnetic Resonance, The First Affiliated Hospital, Zhengzhou University, Zhengzhou, China
- 5Department of Infections Disease, The First Affiliated Hospital, Zhengzhou University, Zhengzhou, China
- 6Department of Radiation Oncology, The Affiliated Cancer Hospital of Zhengzhou University, Zhengzhou, China
- 7First Ward of Spleen, Stomach, Liver and Gall, The First Affiliated Hospital of Henan University of TCM, Zhengzhou, China
- 8Department of Ultrasound, Zhengzhou Sixth People’s Hospital, Henan Infectious Disease Hospital, Zhengzhou, China
- 9Internet Medical and System Applications of National Engineering Laboratory, Zhengzhou, China
- 10Cancer Center, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide and a leading cause of cancer-related deaths. Due to late diagnosis, early intrahepatic metastasis and nonresponse to systemic treatments, surgical resection and/or biopsy specimens remain the gold standard for disease staging, grading and clinical decision-making. Since only a small amount of tissue was obtained in a needle biopsy, the conventional tissue biopsy is unable to represent tumor heterogeneity in HCC. For this reason, it is imperative to find a new non-invasive and easily available diagnostic tool to detect HCC at an early stage and to monitor HCC recurrence. The past decade has witnessed considerable evolution in the development of liquid biopsy technologies with the emergence of next-generation sequencing. As a liquid biopsy approach, molecular analysis of cell-free DNA (cfDNA), characterized by noninvasiveness and real-time analysis, may accurately represent the tumor burden and comprehensively reflect genetic profile of HCC. Therefore, cfDNA may be used clinically as a predictive biomarker in early diagnosis, outcome assessment, and even molecular typing. In this review, we provide an update on the recent advances made in clinical applications of cfDNA in HCC.
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer worldwide and the fourth most frequently reported cause of cancer death by 2018 (Bray et al., 2018). HCC ranks third of cancer-related mortality in China, and the major risk factors for HCC are hepatitis B virus (HBV) or hepatitis C virus (HCV) infection, exposure to aflatoxin B1, alcohol consumption, and metabolic disorders (Chen et al., 2016). Currently, benefiting from liver resection, ablation, liver transplantation, the 5-years survival rate of early HCC (BCLC stage A) can reach 50–75%. Unfortunately, owing to the paucity of specific symptoms and early intra/extrahepatic metastases, most patients have already reached an advanced cancer stage at the time of first HCC diagnosis, giving rise to fewer than 40% of HCC patients eligible for surgical intervention (Forner et al., 2018). Therefore, it is critical to find a robust method to detect patients with HCC at earlier stages, monitor tumor recurrence and even better predict response to treatment in a dynamic and real-time manner.
The diagnosis and surveillance of HCC primarily depends on findings from imaging analysis and alpha-fetoprotein (AFP) levels. Unfortunately, this dynamic imaging has limitations in accuracy and sensitivity when referring to small or hypovascularized lesions. Biopsy is recognized as the standard diagnosis method, while the problem of invasiveness and the false positivity remains to be solved. Lately, circulating free DNA (cfDNA) has emerged as a promising alternative in tumor diagnosis, recurrence surveillance and druggable targets identification (Benesova et al., 2013; Marzese et al., 2013; Diaz and Bardelli, 2014). CfDNA is the fragmented DNA in the blood circulation which can be detected in healthy individuals and patients with cancer, and ctDNA is the fraction of cfDNA specifically derived from primary or metastatic tumors, with the concentration ranging from 0.01 to 90% (Jen et al., 2000). Nowadays, both qualitative and quantitative analysis of cfDNA is utilized in cancer based on underlying genetic predisposition, including detection of genomic changes, mutational analysis, oncogenic pathway determination, prediction/monitoring of treatment response, drug resistance alterations, and identification of mechanisms of malignant/metastatic transformation (Kaseb et al., 2019).
HCC is a highly heterogeneous disease attributing to the accumulation of somatic genomic aberrations in passenger and driver genes as well as epigenetic modifications (Forner et al., 2018). For many years, the recognition of genomic aberrations in HCC mainly relied on liver resection/biopsies. Since invasiveness, traditional fine-needle biopsy does not entirely avoid risks and potential complications, such as pain (84%) (Eisenberg et al., 2003), bleeding (Russo et al., 2018) and needle tract seeding (2.7%) (Silva et al., 2008). In addition, insufficient material for clinical sequencing occurs in 20–25% of needle biopsies (Zill et al., 2015), resulting in the mental and financial pressure of patients to some extent. Intrahepatic metastasis occurs early in the progression of HCC and thus information acquired from a needle biopsy of a single tumor lesion might fail to reflect the tumor burden (Swanton, 2012). In turn, analysis of cfDNA may overcome these limitations and subsequently provide the genomic profiles of all lesions (both primary lesion and metastasis), and this method can be utilized to track genomic evolution systematically and dynamically (Kaseb et al., 2019). With increasing availability and reliability in high-throughput technology, plasma cfDNA may meet the demands of disease surveillance, management of different stages and personal precision medicine for patients with HCC. This review will provide an update on the advances made in the clinical application of cfDNA in HCC in recent years.
cfDNA
Biological Basis
cfDNA is double-stranded DNA measuring approximately 150–200 base pairs which exists in the plasma or serum (Fan et al., 2010). Typically, the concentration of cfDNA is low (10–15 ng/ ml on average) for healthy people, with a short half-life of between 16 min and 2.5 h (Lo et al., 1999; Diehl et al., 2008). While, increasing concentration of cfDNA can be observed under some physical and pathological circumstances, such as exercise, inflammation, surgery, autoimmune disease, and transplantation (Diehl et al., 2008). These characteristics indicate that cfDNA can provide more real-time information regarding the cancer status than routine serum biomarkers, such as AFP, CEA and CA-199.
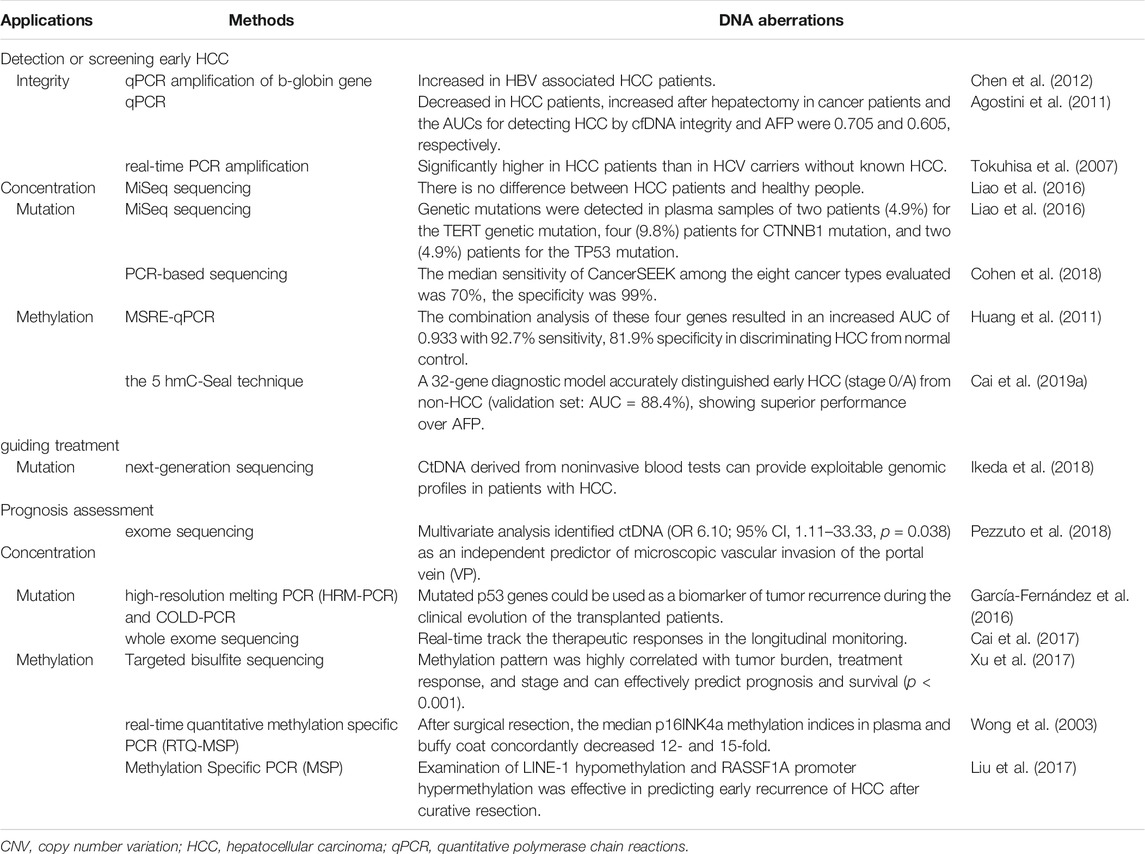
Although the clinical benefits of cfDNA have been increasingly recognized recently, many aspects of the biological characteristics of tumor-derived cfDNA still have not been elucidated clearly. Firstly, the origin of cfDNA has not been definitively clarified with several possible mechanisms proposed (Figure 1). Two possibilities exist for the main origins of cfDNA: cellular breakdown mechanisms (such as apoptosis and necrosis) and active DNA release mechanisms (such as exosomes, virtosomes and argonaute) (Aucamp et al., 2018). Tumor-associated DNA is primarily derived from apoptosis of primary, metastatic and circulating tumor cells (CTCs), as well as active release from proliferative tumor cells, which is known as circulating tumor DNA (ctDNA) (Crowley et al., 2013). In general, ctDNA only accounts for a small fraction of the total cfDNA and there is no way to isolate ctDNA, especially from other cfDNA. Only the emergence of tumor-related molecular alterations in cfDNA indicates the presence of ctDNA (Ye et al., 2019).
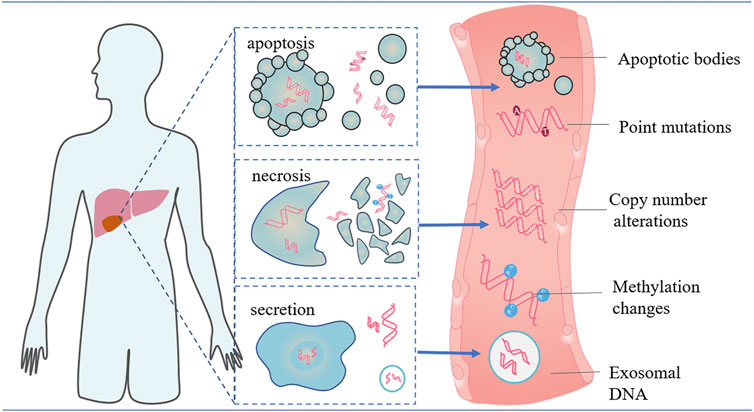
FIGURE 1. Origin and range alterations of cfDNA. Cell-free DNA (cfDNA) is passively released by apoptotic or necrotic tumor cells and actively secreted by exosomes, which are membrane -bound vesicles released by tumor cells. Of these cells, apoptosis serves as the main source of cfDNA in both normal and diseased tissues. Analysis of these molecules can be employed for early tumor detection and may provide a prognostic treatment strategy for HCC patients.
In addition, there are still some different views concerning circulating DNA fragment patterns derived from tumors such as the concentration of total ctDNA and the proportion of tumor-derived ctDNA fragments (Umetani et al., 2006a; Gao et al., 2010; Mouliere et al., 2011). A number of studies reported the finding of increased integrity of tumor-derived plasma DNA (Wang et al., 2003; Jiang et al., 2006). For example, a study reported that the increased DNA integrity in plasma DNA is associated with cancer, and excellent performance was achieved in detecting the cancer group from the nonneoplastic group. On the other hand, there is also seemingly contradictory evidence that plasma DNA molecules released by tumors might be shorter (Diehl et al., 2005; Mouliere et al., 2011). For example, a study performed by massively parallel sequencing suggested that the size of plasma DNA molecules harboring tumor-associated genomic alterations was shorter (Jiang et al., 2015). Overall, cfDNA in the plasma is vulnerable to various assay platforms and physiological state, and thus it is necessary to comprehensively analyze tumor-derived plasma DNA rather than treating without distinction.
Technology Platform for ctDNA
CtDNA accounts for only a small percentage of the total cfDNA in the peripheral blood and is highly variable from patient to patient (0.01–90%), which therefore necessitates the utilization of hypersensitive and highly specific approaches (Corcoran and Chabner, 2018). Typically, alterations of cfDNA in patients with cancers involve quantity and quality (Gao et al., 2017). The former refers to the total concentration and integrity, and the latter means genetic or epigenetic alterations containing single nucleotide mutations, copy number variations and methylation changes and so on. In summary, the techniques for the analysis of cfDNA can be summarized as targeted methods, such as digital PCR, BEAMing digital PCR, and amplification-refractory mutation system (ARMS)-PCR, as well as untargeted methods, such as whole-genome sequencing (WGS) and next-generation sequencing (NGS). Although the former method can screen cfDNA aberrations dynamically and has a very high sensitivity, it detects mutations only in a set of predefined genes based on prior knowledge (Oh et al., 2010). A more comprehensive view of the entire genomic landscape may be exhibited using the latter method, which may provide the potential of identifying drug resistance genes and recognizing novel actionable targets (Slatko et al., 2018). In general, the rational combination of the two techniques would accomplish the purpose, providing a noninvasive approach to guide the clinical management of patients. In the following part, we will detailedly introduce the techniques for detecting aberrant cfDNA in the plasma (Figure 2).
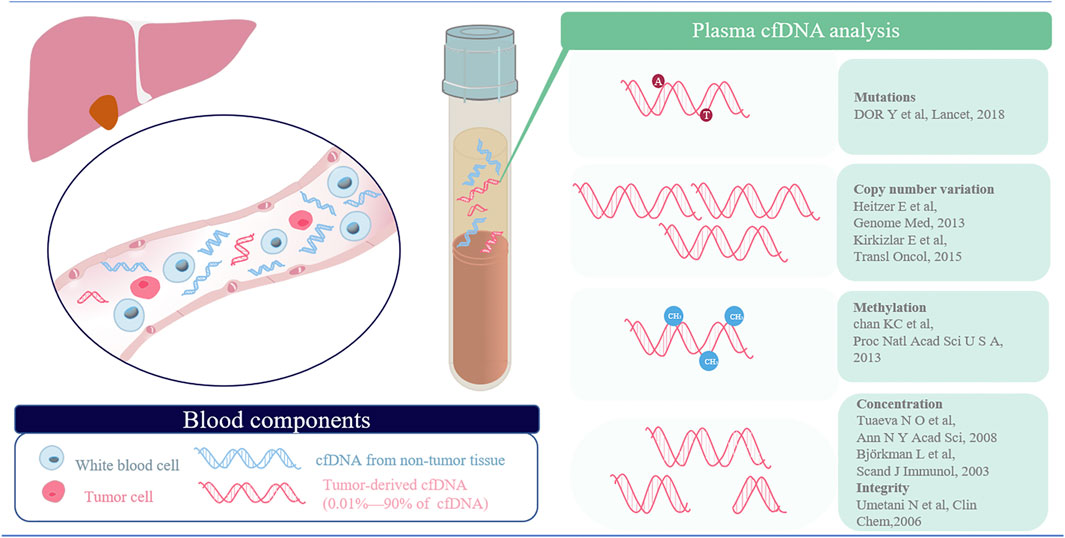
FIGURE 2. Overview of the methods employed in the detection of different cancer-associated alterations. cfDNA in the plasma captures different cancer-associated changes, including mutations, copy number aberrations, alterations in DNA methylation and altered DNA fragmentation patterns (concentration and integrity).
Concentrations
In 1977, for the first time, researchers revealed that cfDNA increased in patients with tumors (Leon et al., 1977). After this seminal work, a significant volume of researches have attempted to detect cancers by quantifying the absolute concentration of cfDNA in the serum/plasma (Mehra et al., 2018; Valpione et al., 2018; Wu et al., 2019). At present, the level of cfDNA in the plasma was estimated by several classical methods, including fluorescence-based quantitative real-time PCR (qPCR), histochemical techniques (such as Hoechst staining and PicoGreen staining) and optical imaging techniques (such as ultraviolet measurement) (Björkman et al., 2003; Tuaeva et al., 2008). It appears that the level of cfDNA in the plasma may reflect the tumor burden (Yang et al., 2011) and may have diagnostic value for HCC (Huang et al., 2012; Yan et al., 2018; Qu et al., 2019). However, an increase in the concentration alone cannot be regarded as an effective and cancer-specific metric for diagnosis and classification because the cfDNA in the plasma is vulnerable to various assay platforms and physiological state like active ongoing hepatitis and hepatic dysfunction (Yan et al., 2018).
Integrity
There is another quantitative characterization of tumors associated with cfDNA: assessment of the integrity index. Currently, the most popular method was published by Umetani. By developed the qPCR method for ALU repeats, this method accomplished the assessment of the integrity without DNA purification and then established the integrity index (Umetani et al., 2006b). In the ALU-qPCR, DNA integrity was determined as the ratio of ALU247 primers to ALU115 primers, and the ALU115 primers represent the absolute amount of DNA. Plasma cfDNA integrity has been applied to many types of cancers, such as breast cancer (Umetani et al., 2006a), colon cancer (Agostini et al., 2011) and liver cancer (Huang et al., 2016a). Compared with concentrations of cfDNA in the plasma, cfDNA integrity is less affected by much influential factors. In previous studies (El-Shazly et al., 2010; Chen et al., 2012; Huang et al., 2016a), changes of integrity in cfDNA is associated with large tumor size and vascular invasion, and it exerted a crucial role in distinguishing cancer from healthy people and surveillance of residual disease after surgery.
Mutations
Studies identifying and characterizing somatic genetic mutations in HCC have been updated annually. There are two types of methods for detecting mutation: targeted methods monitoring interesting gene loci and nontargeted massively parallel sequencing. When the proportion of cfDNA derived from tumor cells accounts for only a small part of the cfDNA in the plasma, abundant errors are expected to be present in the PCR amplification and sequencing procedures. To overcome this problem, unique molecule identifiers (UMIs) have emerged for detecting single nucleotide mutations at a fraction as low as 1 in 1 million molecules (Kinde et al., 2011). In the clinical practice, compared with tumor tissue level mutational heterogeneity, single specific ctDNA alterations do not have sufficiently high sensitivity or specificity as a diagnostic biomarker for HCC. In past literatures, a positive rate of 20–56% for plasma ctDNA was reported (Huang et al., 2016b; Jiao et al., 2018a). Improvement in NGS technology allowed comprehensive analysis of the mutational landscape of ctDNA, expanded the list of mutation biomarker candidates, and promisingly improved the detection rate of tumor-related mutation with the positive rate of 60–80% (Ng et al., 2018; Yang et al., 2019).
Methylation
Epigenetic events play a crucial role in hepatocarcinogenesis. Methylation is a covalent modification pattern that can exist stably in the plasma after the release of defective cells (Dor and Cedar, 2018). Currently, the detection of methylation primarily consists of two types based on the size of the targeted region: target-region methylation detection (methylation-specific PCR) and genome-wide methylation detection (bisulfite sequencing) (Chan et al., 2013). Although concentrated targeted regions are advantageous and inexpensive, the former method cannot precisely show the tumor state because methylation regions (especially CpG islands) are easily affected by gene expression levels. The latter method has wide coverage of the sequenced regions, as well as strong prospects for clinical application. At present, there is ample data to support that DNA methylation changes of specific genes in cfDNA, including hypermethylation of TGR5 (Han et al., 2014), MT1M (Ji et al., 2014) and the RASSF1A promoters (Wong et al., 2000), as well as hypomethylation of LINE-1 elements (Tangkijvanich et al., 2007). Not surprisingly, the combinations of cfDNA methylation in panels can improve the diagnostic performance with high sensitivity and specificity of over 90% (Yang et al., 2019). In summary, the methylation panels appear to be a potential detection marker in the clinical utility accompany with promising application prospects.
Clinical Applications in HCC
CfDNA was originally discovered in 1948 (Mandel and Metais, 1948). With the recent development of genomics and molecular genetics, cfDNA research has significantly increased for a variety of clinical and research purposes (Bettegowda et al., 2014), and cfDNA analysis is increasingly recognized as an effective and noninvasive tool in the diagnosis, personalized treatment, and follow-up of HCC patients (Table 1).
Early Detection
The effective management of patients with HCC relies on the early diagnosis of the disease (Lim et al., 2017), while biomarkers for early detection are still deficient. Most recently, improvement of the next-generation sequencing technology and better understanding of genetic or epigenetic alteration of HCC have allowed comprehensive analysis of the landscape of cfDNA. The non-invasive method was also attached great importance in early detection of HCC.
Increasing concentration of cfDNA was observed in the status of illness, thus quantitative measurement of untargeted cfDNA may have diagnostic value for HCC(Tokuhisa et al., 2007). However, due to factors of various assay platforms and physiological state of different patients, there were wide variations in the concentration of cfDNA even among healthy controls. A recent study enrolled 24 HCC patients and 62 hepatitis B virus-related liver fibrosis patients, and constructed a model including age, cfDNA, and AFP, had an area of 0.98 (95% confidence interval 0.92–1.00) under the ROC for the diagnosis of HCC, with 87.0% sensitivity and 100% specificity. Overall, it would not be recommended for using quantitative measurement independently, whereas the combination of cfDNA with other proteins or genetic biomarkers is expected to be a clinical tool for the early diagnosis of HCC (Liao et al., 2016). Compared with the concentration, detecting the cfDNA integrity index is another approach employed in quantitative analysis, which is considered more stable. A study showed that serum DNA integrity in HCC patients was notably higher than that in HBV carriers or healthy controls (Chen et al., 2012). In another study, found that cfDNA integrity was significantly decreased in HCC patients compared with patients with benign diseases and healthy individuals. Additionally, cfDNA integrity (AUC = 0.705) had a higher diagnostic performance than AFP (AUC = 0.605) (Huang et al., 2016a). Considering the heterogeneity of integrity in different studies, it is necessary to comprehensively analyze aberrantly short and long DNA molecules in the plasma of patients.
Cancer-specific genetic aberrations in cfDNA are detectable by liquid biopsy as biomarkers for the diagnosis and monitoring of HCC. As the high heterogeneity in HCC, single gene variation in cfDNA do not have sufficiently high sensitivity and specificity as a biomarker for HCC(Yang et al., 2017; Jiao et al., 2018b; Marchio et al., 2018). For example, a study showed that there were tumor-associated mutations for HCC in only 8 of 41 patient (19.5%) plasma samples, including mutation to such genes as TP53, hTERT, and CTNNB1 (Liao et al., 2016). To achieve an improved ability to diagnose early HCC, different panels of multigene utilizing NGS technology have broader application in the world. A study of 30 biopsy proven HCC patients were prospectively recruited. Using a panel of 46 genes frequently altered in HCCs, deep sequencing of the DNA from the biopsies, cfDNA, and matched germline was performed and ctDNA was detected in 63% of the patients (Labgaa et al., 2018). Joshua D. Cohen et al. developed a method, termed CancerSeek, which combined the 8 serum protein biomarkers with 16 tumor-associated genes in the cfDNA to detect eight types of early (stage I and II) cancers involving 1,005 patients. Among these cancers, CancerSeek has demonstrated accuracy in the diagnosis of early HCC with a sensitivity of 98% and specificity greater than 99% (Cohen et al., 2018). In summary, large panels of targeted NGS or allele-specific assays targeting hotspot mutations are required for early detection, and ctDNA combined with other biomarkers (AFP or other novel circulating molecular biomarkers) may play a crucial supplementary role as a diagnostic biomarker in HCC.
DNA methylation is a core mechanism of epigenetic regulation of gene expression and cell type-, tissue- and organ-specific methylation signature have been exploited as an HCC marker (Villanueva et al., 2015; Lehmann-Werman et al., 2016; Hlady and Robertson, 2018). A single methylation marker candidate study found that the methylation of RASSF1A was detected in 90% of cfDNA in HCC patients. It showed an accuracy rate of 77.5 and 72.5% as a diagnostic marker of HCC in healthy people and HCV carriers, respectively (Zhong et al., 2003). Similar to mutation in cfDNA, combinations of cfDNA methylation in panels can also improve the diagnostic performance in HCC. A model constructed with four methylation genes (APC, GSTP1, RASSF1A, and SFRP1) had a sensitivity of 92.7% and a specificity of 81.9% for detecting HCC(Huang et al., 2011). Furthermore, a recent study developed a 32-gene diagnostic model that accurately distinguished early HCC (BCL 0/A stage) from non-HCC and 15 AFP-negative patients, exhibiting superior performance over AFP (AUC = 88.4%). The model also exhibited superior ability in diagnosing HCC from high-risk populations, such as those with hepatitis and hepatic cirrhosis (AUC = 84.6%) (Cai et al., 2019a). Overall, ctDNA methylation panels appear to have the strongest potential for clinical utility in the early detection of HCC, and all the biomarkers requires prospective validation for the robust performance.
Medicine Guidance
Another important application of cfDNA is the identification of tumor gene profiling for individualized treatment, which has become a fundamental practice in cancer medicine (Harding et al., 2019). In the recent decade, various advances in treatment bring great promises and new opportunities for HCC therapeutics. Sorafenib and Lenvatinib in first-line showed efficacy, and regorafenib, cabozantinib as well as ramucirumab in second-line provided more chances for sequential systemic therapy in advanced HCC. Recently, immunotherapy has emerged as one of the most promising approaches to extend current options for needed HCC treatment (Liu et al., 2021a). Frustratingly, less than 40% of HCC patients are eligible for potentially curative therapies. Therefore, it is imperative to detect predictive biomarkers including FGFR4, Cdk5, PD-1, PD-L1, and tumor mutation burden (TMB) which may optimize the therapy strategy and forecast the benefit to patients receiving target and immune therapy. The limited applications of molecular classification using biopsy tissue samples may be attributable intra-tumoral or intertumoral heterogeneity in HCC patients; therefore, one piece of tumor tissue failed to present the complete molecular profile of one HCC patient (Liu et al., 2021b; Liu et al., 2021c). In contrast, numerous studies have demonstrated high concordance rates between plasma and tissue samples, particularly for alterations in key genes (Adalsteinsson et al., 2017; Strickler et al., 2018). Therefore, combined with the features of safety, low cost, operability and dynamic monitoring, cfDNA analysis may possess the potential to provide individualized treatment guidance for HCC patients.
Sadakatsu (Ikeda et al., 2018) implemented NGS to identify actionable mutations in 12 HCC patients, and ultimately, 556 exons of 68 genes were sequenced. A total of 79% of patients harbored at least one actionable mutation alteration, and the median of drug target mutation alterations was 2 (0–5), which suggested that performing liquid biopsies and detecting cfDNA may play a key role in guiding therapeutic decision-making. Furthermore, a patient with a CDKN2A-inactivating and a CTNNB1-activating mutation received palbociclib (CDK4/6 inhibitor) and celecoxib (COX-2/Wnt inhibitor); another patient with a PTEN-inactivating and a MET-activating mutation received matched treatment: sirolimus (mechanistic target of rapamycin inhibitor) and cabozantinib (MET inhibitor). Eventually, the treatment outcomes of two patients were described as good. Another study prospectively enrolled 121 patients to identify predictors of primary resistance to systematic therapy using cfDNA. Patients with mutations in the PI3K/MTOR pathway had significantly shorter progression-free survival (PFS) than those without these mutations after tyrosine kinase inhibitors (2.1 vs. 3.7 months, p < 0.001), but not after immune checkpoint inhibition (CPI) (von Felden et al., 2021). Because of the low long-term response to sorafenib in HCC (Méndez-Blanco et al., 2018) and large individual differences in response to immunotherapy (Llovet et al., 2018), few investigations into the use of cfDNA to guide therapy in HCC have been reported.
Prognosis Evaluation
Earlier studies showed that the levels of cfDNA in the plasma were significantly correlated with tumor burden (Cai et al., 2017; Pezzuto et al., 2018) with a high specificity and short half-life periods, meaning that cfDNA has a unique strength of prognostic value. There is evidence that mutations in cfDNA are closely related to vascular invasions, and patients with cfDNA mutations are more frequently reported to have shorter recurrence-free survival (RFS) (Cai et al., 2019b). García-Fernández et al. (2016) found that the presentation of TP53 mutations in cfDNA might be used as a biomarker of tumor recurrence in patients with transplanted HCC. Furthermore, Rui-Hua Xu et al. (2017) constructed a prognostic prediction model based on methylation alterations in cfDNA to effectively predict prognosis and survival (p < 0.001), which was highly correlated with tumor burden, treatment response, and stage. The above findings demonstrated that changes in cfDNA, including concentration, mutation and methylation, may provide references for the prediction of HCC prognosis.
Benefiting from a short half-life, cfDNA exhibits a fast response to changes in tumor burden after treatment, and thus it is possible to improve prognostication with the detection of tumor-specific molecular alterations. One study reported that the level of cfDNA decreased significantly after surgery, indicating that the dynamic monitoring of cfDNA alterations could provide additional information regarding the presence of residual lesions and early relapse after surgery (Corcoran and Chabner, 2018). ZX found that there was a notable decline in the mutation frequency of cfDNA, and during follow-up, the increased frequency of mutations in cfDNA often revealed the presence of residual lesions and, eventually, relapse (Cai et al., 2017). CtDNA methylation of a panel of genes has shown to be an important prognostic factor. The study of Wong IH showed that RTQ-MSP quantitative analysis can detect epigenetic changes (DNA methylation levels) in peripheral blood from patients with HCC. These researchers observed that the p16INK4a sequence of methylation is present in 80% of HCC patients, and a 12-fold decline was observed in the patients after surgery (Wong et al., 2003). Another study indicated that co-evaluation of LINE-1 hypomethylation and RASSF1A promoter hypermethylation was effective in predicting early recurrence of HCC after curative resection (Liu et al., 2017). Furthermore, the level of demethylation was also significantly related to the presence of residual lesions after surgery (Chan et al., 2013). Overall, methylation patterns of the patients after surgery could provide an early warning of residual lesions and early relapse.
Challenges and Perspectives
In general, cfDNA may be an informative, inherently specific and highly sensitive biomarker, and can be performed in clinical and research purposes in many types of cancer. A blood sample from peripheral venous blood is not only convenient and easy to implement, but cfDNA in the plasma is relatively stable and easy to extract. In addition, with the characteristic of short half-life, cfDNA in this context is a more accurate and timely reflection of the tumor staging and recurrence than serum biomarkers. With the accumulation of liquid biopsy data, detection panels involving mutations at multiple loci and multiple methylation patterns using cfDNA may be employed for therapeutic monitoring, prognostic evaluation and early diagnosis in HCC.
The descriptions of molecular aberrations of the cfDNA in this review only focus on HCC, while mutations of the same keeper genes, such as TP53, KRAS, and RAF also occur in many other types of cancers. Besides, the cfDNA in plasma mainly derives from rupture and release of blood cells, and the concentration of plasma cfDNA can be affected by the different physiological and pathological conditions. There is an emerging problem which cannot be neglected: how could cfDNA be cancer-specific? The epigenetic biomarkers of cfDNA may be one of the most promising directions. DNA methylation is favored epigenetic biomarker because of cancer-type-specific and tissue-type-specific for the cancer diagnosis and tracing the tissue origin of cfDNA (Gai and Sun, 2019). Moreover, in combination with machine learning, methylation biomarkers in cfDNA provides a new clue to discriminate specific cancer type. Zhou and colleagues modeled the plasma cfDNA as a mixture of DNA derived from tumor and normal tissues, then they used a probabilistic model to sensitively identify a trace amount of tumor cfDNAs in plasma (Li et al., 2018a). Epigenetic biomarkers in cfDNA provide generalizable solutions for early detection and trace the origin of ctDNA.
Although cfDNA performed as a powerful detection and analysis tool along with promising potential, there are still many challenges for this technology to become clinical reality. First, the experimental data described in this review are diverse and vulnerable, which may attribute to a variety of individual differences, experimental designs and detection methods for cfDNA across different studies. In addition, there is a lack of an effective medical therapy and universal actionable mutations for HCC patients, resulting in rare medical applications of cfDNA in the plasma based on HCC-associated gene mutations (Li et al., 2018b). Altogether, cfDNA is an exciting product of precise medicine, and in the near future it may realize the purpose of real-time surveillance and tailored treatment for patients with HCC.
Author Contributions
YZ and ZAL made conceptualization; YZ and CW consulted and summarized the literature; YZ, ZHL, and KJ prepared original draft, reviewed and edited the manuscript; KJ, ZAL, XC, YL, XH, LM, and XL supervised the study; LL, XC, and ZR contributed to submission. The authors read and approved the final manuscript.
Funding
Project was supported by the National Natural Science Foundation of China (Grant No. U1904143); National Science and Technology Major Project, Prevention and Treatment of Major Infectious Diseases such as AIDS and Viral Hepatitis (2018ZX10303502); The National Natural Science Foundation of China (Grant No. 82002433); Science and Technology Project of Henan Provincial Department of Education (Grant No. 21A320036); Henan Province Medical Science and Technology Research Project Joint Construction Project (Grant No. LHGJ20190003, LHGJ20190055).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AFP, α-fetoprotein; ARMS, amplification-refractory mutation system; AUC, area under the curve; cfDNA, cell-free DNA; CNV, copy number variation; CTCs, circulating tumor cells; ctDNA, circulating tumor DNA; EPIC-Seq, the Epigenetic Profile Inference from the CfDNA Deep Sequencing; HCC, Hepatocellular carcinoma; mmPCR-NGS: massively multiplexed PCR and next-generation sequencing; NGS, next-generation sequencing; qPCR, quantitative real-time PCR; RFS, progression-free survival; ROC, receiver operator characteristic curve; sWGS, shallow WGS; TACE, transplantation or transarterial chemoembolization; TCGA, The Cancer Genome Atlas; UMIs, unique molecule identifiers; WGS, whole-genome sequencing.
References
Adalsteinsson, V. A., Ha, G., Freeman, S. S., Choudhury, A. D., Stover, D. G., Parsons, H. A., et al. (2017). Scalable Whole-Exome Sequencing of Cell-Free DNA Reveals High Concordance with Metastatic Tumors. Nat. Commun. 8 (1), 1324. doi:10.1038/s41467-017-00965-y
Agostini, M., Pucciarelli, S., Enzo, M. V., Del Bianco, P., Briarava, M., Bedin, C., et al. (2011). Circulating Cell-free DNA: A Promising Marker of Pathologic Tumor Response in Rectal Cancer Patients Receiving Preoperative Chemoradiotherapy. Ann. Surg. Oncol. 18 (9), 2461–2468. doi:10.1245/s10434-011-1638-y
Aucamp, J., Bronkhorst, A. J., Badenhorst, C. P. S., and Pretorius, P. J. (2018). The Diverse Origins of Circulating Cell-Free DNA in the Human Body: A Critical Re-Evaluation of the Literature. Biol. Rev. 93 (3), 1649–1683. doi:10.1111/brv.12413
Benesova, L., Belsanova, B., Suchanek, S., Kopeckova, M., Minarikova, P., Lipska, L., et al. (2013). Mutation-Based Detection and Monitoring of Cell-free Tumor DNA in Peripheral Blood of Cancer Patients. Anal. Biochem. 433 (2), 227–234. doi:10.1016/j.ab.2012.06.018
Bettegowda, C., Sausen, M., Leary, R. J., Kinde, I., Wang, Y., Agrawal, N., et al. (2014). Detection of Circulating Tumor DNA in Early- and Late-Stage Human Malignancies. Sci. Translational Med. 6 (224), 224ra24. doi:10.1126/scitranslmed.3007094
Björkman, L., Reich, C. F., and Pisetsky, D. S. (2003). The Use of Fluorometric Assays to Assess the Immune Response to DNA in Murine Systemic Lupus Erythematosus. Scand. J. Immunol. 57 (6), 525–533. doi:10.1046/j.1365-3083.2003.01261.x
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., and Jemal, A. (2018). Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer J. Clinicians 68 (6), 394–424. doi:10.3322/caac.21492
Cai, Z.-X., Chen, G., Zeng, Y.-Y., Dong, X.-Q., Lin, M.-J., Huang, X.-H., et al. (2017). Circulating Tumor DNA Profiling Reveals Clonal Evolution and Real-Time Disease Progression in Advanced Hepatocellular Carcinoma. Int. J. Cancer 141 (5), 977–985. doi:10.1002/ijc.30798
Cai, J., Chen, L., Zhang, Z., Zhang, X., Lu, X., Liu, W., et al. (2019). Genome-wide Mapping of 5-Hydroxymethylcytosines in Circulating Cell-Free DNA as a Non-Invasive Approach for Early Detection of Hepatocellular Carcinoma. Gut 68 (12), 2195–2205. doi:10.1136/gutjnl-2019-318882
Cai, Z., Chen, G., Zeng, Y., Dong, X., Li, Z., Huang, Y., et al. (2019). Comprehensive Liquid Profiling of Circulating Tumor DNA and Protein Biomarkers in Long-Term Follow-Up Patients with Hepatocellular Carcinoma. Clin. Cancer Res. 25 (17), 5284–5294. doi:10.1158/1078-0432.Ccr-18-3477
Chan, K. C. A., Jiang, P., Chan, C. W. M., Sun, K., Wong, J., Hui, E. P., et al. (2013). Noninvasive Detection of Cancer-Associated Genome-Wide Hypomethylation and Copy Number Aberrations by Plasma DNA Bisulfite Sequencing. Proc. Natl. Acad. Sci. 110 (47), 18761–18768. doi:10.1073/pnas.1313995110
Chen, H., Sun, L.-y., Zheng, H.-q., Zhang, Q.-f., and Jin, X.-m. (2012). Total Serum DNA and DNA Integrity: Diagnostic Value in Patients with Hepatitis B Virus-Related Hepatocellular Carcinoma. Pathology 44 (4), 318–324. doi:10.1097/PAT.0b013e328353a24c
Chen, W., Zheng, R., Baade, P. D., Zhang, S., Zeng, H., Bray, F., et al. (2016). Cancer Statistics in China, 2015. CA: A Cancer J. Clinicians 66 (2), 115–132. doi:10.3322/caac.21338
Cohen, J. D., Li, L., Wang, Y., Thoburn, C., Afsari, B., Danilova, L., et al. (2018). Detection and Localization of Surgically Resectable Cancers with a Multi-Analyte Blood Test. Science 359 (6378), 926–930. doi:10.1126/science.aar3247
Corcoran, R. B., and Chabner, B. A. (2018). Application of Cell-Free DNA Analysis to Cancer Treatment. N. Engl. J. Med. 379 (18), 1754–1765. doi:10.1056/NEJMra1706174
Crowley, E., Di Nicolantonio, F., Loupakis, F., and Bardelli, A. (2013). Liquid Biopsy: Monitoring Cancer-Genetics in the Blood. Nat. Rev. Clin. Oncol. 10 (8), 472–484. doi:10.1038/nrclinonc.2013.110
Diaz, L. A., and Bardelli, A. (2014). Liquid Biopsies: Genotyping Circulating Tumor DNA. J. Clin. Oncol. 32 (6), 579–586. doi:10.1200/jco.2012.45.2011
Diehl, F., Li, M., Dressman, D., He, Y., Shen, D., Szabo, S., et al. (2005). Detection and Quantification of Mutations in the Plasma of Patients with Colorectal Tumors. Proc. Natl. Acad. Sci. 102 (45), 16368–16373. doi:10.1073/pnas.0507904102
Diehl, F., Schmidt, K., Choti, M. A., Romans, K., Goodman, S., Li, M., et al. (2008). Circulating Mutant DNA to Assess Tumor Dynamics. Nat. Med. 14 (9), 985–990. doi:10.1038/nm.1789
Dor, Y., and Cedar, H. (2018). Principles of DNA Methylation and Their Implications for Biology and Medicine. The Lancet 392 (10149), 777–786. doi:10.1016/s0140-6736(18)31268-6
Eisenberg, E., Konopniki, M., Veitsman, E., Kramskay, R., Gaitini, D., and Baruch, Y. (2003). Prevalence and Characteristics of Pain Induced by Percutaneous Liver Biopsy. Anesth. Analgesia 96 (5), 1392–1396. table of contents. doi:10.1213/01.ane.0000060453.74744.17
El-Shazly, S. F., Eid, M. A., El-Sourogy, H. A., Attia, G. F., and Ezzat, S. A. (2010). Evaluation of Serum DNA Integrity as a Screening and Prognostic Tool in Patients with Hepatitis C Virus-Related Hepatocellular Carcinoma. Int. J. Biol. Markers 25 (2), 79–86. doi:10.1177/172460081002500204
Fan, H. C., Blumenfeld, Y. J., Chitkara, U., Hudgins, L., and Quake, S. R. (2010). Analysis of the Size Distributions of Fetal and Maternal Cell-free DNA by Paired-End Sequencing. Clin. Chem. 56 (8), 1279–1286. doi:10.1373/clinchem.2010.144188
Forner, A., Reig, M., and Bruix, J. (2018). Hepatocellular Carcinoma. Lancet 391 (10127), 1301–1314. doi:10.1016/s0140-6736(18)30010-2
Gai, W., and Sun, K. (2019). Epigenetic Biomarkers in Cell-free DNA and Applications in Liquid Biopsy. Genes 10 (1), 32. doi:10.3390/genes10010032
Gao, Y.-J., He, Y.-J., Yang, Z.-L., Shao, H.-Y., Zuo, Y., Bai, Y., et al. (2010). Increased Integrity of Circulating Cell-Free DNA in Plasma of Patients with Acute Leukemia. Clin. Chem. Lab. Med. 48 (11), 1651–1656. doi:10.1515/cclm.2010.311
Gao, Y., Zhang, K., Xi, H., Cai, A., Wu, X., Cui, J., et al. (2017). Diagnostic and Prognostic Value of Circulating Tumor DNA in Gastric Cancer: A Meta-Analysis. Oncotarget 8 (4), 6330–6340. doi:10.18632/oncotarget.14064
García-Fernández, N., Macher, H. C., Rubio, A., Jiménez-Arriscado, P., Bernal-Bellido, C., Bellido-Díaz, M. L., et al. (2016). Detection of P53 Mutations in Circulating DNA of Transplanted Hepatocellular Carcinoma Patients as a Biomarker of Tumor Recurrence. Adv. Exp. Med. Biol. 924, 25–28. doi:10.1007/978-3-319-42044-8_5
Han, L.-Y., Fan, Y.-C., Mu, N.-N., Gao, S., Li, F., Ji, X.-F., et al. (2014). Aberrant DNA Methylation of G-Protein-Coupled Bile Acid Receptor Gpbar1 (TGR5) Is a Potential Biomarker for Hepatitis B Virus Associated Hepatocellular Carcinoma. Int. J. Med. Sci. 11 (2), 164–171. doi:10.7150/ijms.6745
Harding, J. J., Nandakumar, S., Armenia, J., Khalil, D. N., Albano, M., Ly, M., et al. (2019). Prospective Genotyping of Hepatocellular Carcinoma: Clinical Implications of Next-Generation Sequencing for Matching Patients to Targeted and Immune Therapies. Clin. Cancer Res. 25 (7), 2116–2126. doi:10.1158/1078-0432.Ccr-18-2293
Hlady, R., and Robertson, K. (2018). Genetic and Epigenetic Heterogeneity in Normal Liver Homeostasis and its Implications for Liver Disease and Hepatocellular Cancer. Semin. Liver Dis. 38 (1), 041–050. doi:10.1055/s-0037-1621712
Huang, Z.-H., Hu, Y., Hua, D., Wu, Y.-Y., Song, M.-X., and Cheng, Z.-H. (2011). Quantitative Analysis of Multiple Methylated Genes in Plasma for the Diagnosis and Prognosis of Hepatocellular Carcinoma. Exp. Mol. Pathol. 91 (3), 702–707. doi:10.1016/j.yexmp.2011.08.004
Huang, Z., Hua, D., Hu, Y., Cheng, Z., Zhou, X., Xie, Q., et al. (2012). Quantitation of Plasma Circulating DNA Using Quantitative PCR for the Detection of Hepatocellular Carcinoma. Pathol. Oncol. Res. 18 (2), 271–276. doi:10.1007/s12253-011-9438-z
Huang, A., Zhang, X., Zhou, S.-L., Cao, Y., Huang, X.-W., Fan, J., et al. (2016). Plasma Circulating Cell-free DNA Integrity as a Promising Biomarker for Diagnosis and Surveillance in Patients with Hepatocellular Carcinoma. J. Cancer 7 (13), 1798–1803. doi:10.7150/jca.15618
Huang, A., Zhang, X., Zhou, S.-L., Cao, Y., Huang, X.-W., Fan, J., et al. (2016). Detecting Circulating Tumor DNA in Hepatocellular Carcinoma Patients Using Droplet Digital PCR Is Feasible and Reflects Intratumoral Heterogeneity. J. Cancer 7 (13), 1907–1914. doi:10.7150/jca.15823
Ikeda, S., Tsigelny, I. F., Skjevik, Å. A., Kono, Y., Mendler, M., Kuo, A., et al. (2018). Next‐Generation Sequencing of Circulating Tumor DNA Reveals Frequent Alterations in Advanced Hepatocellular Carcinoma. Oncol. 23 (5), 586–593. doi:10.1634/theoncologist.2017-0479
Jen, J., Wu, L., and Sidransky, D. (2000). An Overview on the Isolation and Analysis of Circulating Tumor DNA in Plasma and Serum. Ann. N. Y Acad. Sci. 906, 8–12. doi:10.1111/j.1749-6632.2000.tb06581.x
Ji, X.-F., Fan, Y. C., Gao, S., Yang, Y., Zhang, J. J., and Wang, K. (2014). MT1MandMT1Gpromoter Methylation as Biomarkers for Hepatocellular Carcinoma. World J. Gastroenterol. 20 (16), 4723–4729. doi:10.3748/wjg.v20.i16.4723
Jiang, W.-W., Zahurak, M., Goldenberg, D., Milman, Y., Park, H. L., Westra, W. H., et al. (2006). Increased Plasma DNA Integrity index in Head and Neck Cancer Patients. Int. J. Cancer 119 (11), 2673–2676. doi:10.1002/ijc.22250
Jiang, P., Chan, C. W. M., Chan, K. C. A., Cheng, S. H., Wong, J., Wong, V. W.-S., et al. (2015). Lengthening and Shortening of Plasma DNA in Hepatocellular Carcinoma Patients. Proc. Natl. Acad. Sci. USA 112 (11), E1317–E1325. doi:10.1073/pnas.1500076112
Jiao, J., Watt, G. P., Stevenson, H. L., Calderone, T. L., Fisher‐Hoch, S. P., Ye, Y., et al. (2018). Telomerase Reverse Transcriptase Mutations in Plasma DNA in Patients with Hepatocellular Carcinoma or Cirrhosis: Prevalence and Risk Factors. Hepatol. Commun. 2 (6), 718–731. doi:10.1002/hep4.1187
Jiao, J., Niu, W., Wang, Y., Baggerly, K., Ye, Y., Wu, X., et al. (2018). Prevalence of Aflatoxin-Associated TP53R249S Mutation in Hepatocellular Carcinoma in Hispanics in South Texas. Cancer Prev. Res. 11 (2), 103–112. doi:10.1158/1940-6207.CAPR-17-0235
Kaseb, A. O., Sánchez, N. S., Sen, S., Kelley, R. K., Tan, B., Bocobo, A. G., et al. (2019). Molecular Profiling of Hepatocellular Carcinoma Using Circulating Cell-free DNA. Clin. Cancer Res. 25 (20), 6107–6118. doi:10.1158/1078-0432.Ccr-18-3341
Kinde, I., Wu, J., Papadopoulos, N., Kinzler, K. W., and Vogelstein, B. (2011). Detection and Quantification of Rare Mutations with Massively Parallel Sequencing. Proc. Natl. Acad. Sci. 108 (23), 9530–9535. doi:10.1073/pnas.1105422108
Labgaa, I., Villacorta-Martin, C., D’Avola, D., Craig, A. J., von Felden, J., Martins-Filho, S. N., et al. (2018). A Pilot Study of Ultra-Deep Targeted Sequencing of Plasma DNA Identifies Driver Mutations in Hepatocellular Carcinoma. Oncogene 37 (27), 3740–3752. doi:10.1038/s41388-018-0206-3
Lehmann-Werman, R., Neiman, D., Zemmour, H., Moss, J., Magenheim, J., Vaknin-Dembinsky, A., et al. (2016). Identification of Tissue-specific Cell Death Using Methylation Patterns of Circulating DNA. Proc. Natl. Acad. Sci. USA 113 (13), E1826–E1834. doi:10.1073/pnas.1519286113
Leon, S. A., Shapiro, B., Sklaroff, D. M., and Yaros, M. J. (1977). Free DNA in the Serum of Cancer Patients and the Effect of Therapy. Cancer Res. 37 (3), 646–650.
Li, W., Li, Q., Kang, S., Same, M., Zhou, Y., Sun, C., et al. (2018). CancerDetector: Ultrasensitive and Non-invasive Cancer Detection at the Resolution of Individual Reads Using Cell-free DNA Methylation Sequencing Data. Nucleic Acids Res. 46 (15), e89. doi:10.1093/nar/gky423
Li, J., Han, X., Yu, X., Xu, Z., Yang, G., Liu, B., et al. (2018). Clinical Applications of Liquid Biopsy as Prognostic and Predictive Biomarkers in Hepatocellular Carcinoma: Circulating Tumor Cells and Circulating Tumor DNA. J. Exp. Clin. Cancer Res. 37 (1), 213. doi:10.1186/s13046-018-0893-1
Liao, W., Yang, H., Xu, H., Wang, Y., Ge, P., Ren, J., et al. (2016). Noninvasive Detection of Tumor-Associated Mutations from Circulating Cell-free DNA in Hepatocellular Carcinoma Patients by Targeted Deep Sequencing. Oncotarget 7 (26), 40481–40490. doi:10.18632/oncotarget.9629
Lim, C., Bhangui, P., Salloum, C., Gómez-Gavara, C., Lahat, E., Luciani, A., et al. (2017). Impact of Time to Surgery in the Outcome of Patients with Liver Resection for BCLC 0-A Stage Hepatocellular Carcinoma. J. Hepatol. 68, 100–108. doi:10.1016/j.jhep.2017.09.017
Liu, Z. J., Huang, Y., Wei, L., He, J. Y., Liu, Q. Y., Yu, X. Q., et al. (2017). Combination of LINE-1 Hypomethylation and RASSF1A Promoter Hypermethylation in Serum DNA Is a Non-invasion Prognostic Biomarker for Early Recurrence of Hepatocellular Carcinoma after Curative Resection. Neoplasma 64 (5), 795–802. doi:10.4149/neo_2017_519
Liu, Z., Zhang, Y., Shi, C., Zhou, X., Xu, K., Jiao, D., et al. (2021). A Novel Immune Classification Reveals Distinct Immune Escape Mechanism and Genomic Alterations: Implications for Immunotherapy in Hepatocellular Carcinoma. J. Transl Med. 19 (1), 5. doi:10.1186/s12967-020-02697-y
Liu, Z., Liu, L., Lu, T., Wang, L., Li, Z., Jiao, D., et al. (2021). Hypoxia Molecular Characterization in Hepatocellular Carcinoma Identifies One Risk Signature and Two Nomograms for Clinical Management. J. Oncol. 2021, 1–20. doi:10.1155/2021/6664386
Liu, Z., Wang, L., Liu, L., Lu, T., Jiao, D., Sun, Y., et al. (2021). The Identification and Validation of Two Heterogenous Subtypes and a Risk Signature Based on Ferroptosis in Hepatocellular Carcinoma. Front. Oncol. 11, 619242. doi:10.3389/fonc.2021.619242
Llovet, J. M., Montal, R., Sia, D., and Finn, R. S. (2018). Molecular Therapies and Precision Medicine for Hepatocellular Carcinoma. Nat. Rev. Clin. Oncol. 15 (10), 599–616. doi:10.1038/s41571-018-0073-4
Lo, Y. M. D., Zhang, J., Leung, T. N., Lau, T. K., Chang, A. M. Z., and Hjelm, N. M. (1999). Rapid Clearance of Fetal DNA from Maternal Plasma. Am. J. Hum. Genet. 64 (1), 218–224. doi:10.1086/302205
Mandel, P., and Metais, P. (1948). Nuclear Acids in Human Blood Plasma. C R. Seances Soc. Biol. Fil 142 (3-4), 241–243. doi:10.1159/000300537
Marchio, A., Amougou Atsama, M., Béré, A., Komas, N.-P., Noah Noah, D., Atangana, P. J. A., et al. (2018). Droplet Digital PCR Detects High Rate of TP53 R249S Mutants in Cell-free DNA of Middle African Patients with Hepatocellular Carcinoma. Clin. Exp. Med. 18 (3), 421–431. doi:10.1007/s10238-018-0502-9
Marzese, D. M., Hirose, H., and Hoon, D. S. B. (2013). Diagnostic and Prognostic Value of Circulating Tumor-Related DNA in Cancer Patients. Expert Rev. Mol. Diagn. 13 (8), 827–844. doi:10.1586/14737159.2013.845088
Mehra, N., Dolling, D., Sumanasuriya, S., Christova, R., Pope, L., Carreira, S., et al. (2018). Plasma Cell-free DNA Concentration and Outcomes from Taxane Therapy in Metastatic Castration-Resistant Prostate Cancer from Two Phase III Trials (FIRSTANA and PROSELICA). Eur. Urol. 74 (3), 283–291. doi:10.1016/j.eururo.2018.02.013
Méndez-Blanco, C., Fondevila, F., García-Palomo, A., González-Gallego, J., and Mauriz, J. L. (2018). Sorafenib Resistance in Hepatocarcinoma: Role of Hypoxia-Inducible Factors. Exp. Mol. Med. 50 (10), 1–9. doi:10.1038/s12276-018-0159-1
Mouliere, F., Robert, B., Arnau Peyrotte, E., Del Rio, M., Ychou, M., Molina, F., et al. (2011). High Fragmentation Characterizes Tumour-Derived Circulating DNA. PLoS One 6 (9), e23418. doi:10.1371/journal.pone.0023418
Ng, C. K. Y., Di Costanzo, G. G., Tosti, N., Paradiso, V., Coto-Llerena, M., Roscigno, G., et al. (2018). Genetic Profiling Using Plasma-Derived Cell-free DNA in Therapy-Naïve Hepatocellular Carcinoma Patients: a Pilot Study. Ann. Oncol. 29 (5), 1286–1291. doi:10.1093/annonc/mdy083
Oh, J. E., Lim, H. S., An, C. H., Jeong, E. G., Han, J. Y., Lee, S. H., et al. (2010). Detection of Low-Level KRAS Mutations Using PNA-Mediated Asymmetric PCR Clamping and Melting Curve Analysis with Unlabeled Probes. J. Mol. Diagn. 12 (4), 418–424. doi:10.2353/jmoldx.2010.090146
Pezzuto, F., Buonaguro, L., Buonaguro, F., and Tornesello, M. (2018). The Role of Circulating Free DNA and MicroRNA in Non-invasive Diagnosis of HBV- and HCV-Related Hepatocellular Carcinoma. Int. J. Mol. Sci. 19 (4), 1007. doi:10.3390/ijms19041007
Qu, C., Wang, Y., Wang, P., Chen, K., Wang, M., Zeng, H., et al. (2019). Detection of Early-Stage Hepatocellular Carcinoma in Asymptomatic HBsAg-Seropositive Individuals by Liquid Biopsy. Proc. Natl. Acad. Sci. USA 116 (13), 6308–6312. doi:10.1073/pnas.1819799116
Russo, F. P., Imondi, A., Lynch, E. N., and Farinati, F. (2018). When and How Should We Perform a Biopsy for HCC in Patients with Liver Cirrhosis in 2018? A Review. Dig. Liver Dis. 50 (7), 640–646. doi:10.1016/j.dld.2018.03.014
Silva, M. A., Hegab, B., Hyde, C., Guo, B., Buckels, J. A. C., and Mirza, D. F. (2008). Needle Track Seeding Following Biopsy of Liver Lesions in the Diagnosis of Hepatocellular Cancer: a Systematic Review and Meta-Analysis. Gut 57 (11), 1592–1596. doi:10.1136/gut.2008.149062
Slatko, B. E., Gardner, A. F., and Ausubel, F. M. (2018). Overview of Next‐Generation Sequencing Technologies. Curr. Protoc. Mol. Biol. 122 (1), e59. doi:10.1002/cpmb.59
Strickler, J. H., Loree, J. M., Ahronian, L. G., Parikh, A. R., Niedzwiecki, D., Pereira, A. A. L., et al. (2018). Genomic Landscape of Cell-Free DNA in Patients with Colorectal Cancer. Cancer Discov. 8 (2), 164–173. doi:10.1158/2159-8290.Cd-17-1009
Swanton, C. (2012). Intratumor Heterogeneity: Evolution through Space and Time. Cancer Res. 72 (19), 4875–4882. doi:10.1158/0008-5472.Can-12-2217
Tangkijvanich, P., Hourpai, N., Rattanatanyong, P., Wisedopas, N., Mahachai, V., and Mutirangura, A. (2007). Serum LINE-1 Hypomethylation as a Potential Prognostic Marker for Hepatocellular Carcinoma. Clinica Chim. Acta 379 (1-2), 127–133. doi:10.1016/j.cca.2006.12.029
Tokuhisa, Y., Iizuka, N., Sakaida, I., Moribe, T., Fujita, N., Miura, T., et al. (2007). Circulating Cell-free DNA as a Predictive Marker for Distant Metastasis of Hepatitis C Virus-Related Hepatocellular Carcinoma. Br. J. Cancer 97 (10), 1399–1403. doi:10.1038/sj.bjc.6604034
Tuaeva, N. O., Abramova, Z. I., and Sofronov, V. V. (2008). The Origin of Elevated Levels of Circulating DNA in Blood Plasma of Premature Neonates. Ann. N. Y Acad. Sci. 1137, 27–30. doi:10.1196/annals.1448.043
Umetani, N., Giuliano, A. E., Hiramatsu, S. H., Amersi, F., Nakagawa, T., Martino, S., et al. (2006). Prediction of Breast Tumor Progression by Integrity of Free Circulating DNA in Serum. J. Clin. Oncol. 24 (26), 4270–4276. doi:10.1200/jco.2006.05.9493
Umetani, N., Kim, J., Hiramatsu, S., Reber, H. A., Hines, O. J., Bilchik, A. J., et al. (2006). Increased Integrity of Free Circulating DNA in Sera of Patients with Colorectal or Periampullary Cancer: Direct Quantitative PCR for ALU Repeats. Clin. Chem. 52 (6), 1062–1069. doi:10.1373/clinchem.2006.068577
Valpione, S., Gremel, G., Mundra, P., Middlehurst, P., Galvani, E., Girotti, M. R., et al. (2018). Plasma Total Cell-free DNA (cfDNA) Is a Surrogate Biomarker for Tumour burden and a Prognostic Biomarker for Survival in Metastatic Melanoma Patients. Eur. J. Cancer 88, 1–9. doi:10.1016/j.ejca.2017.10.029
Villanueva, A., Portela, A., Sayols, S., Battiston, C., Hoshida, Y., Méndez-González, J., et al. (2015). DNA Methylation-Based Prognosis and Epidrivers in Hepatocellular Carcinoma. Hepatology 61 (6), 1945–1956. doi:10.1002/hep.27732
von Felden, J., Craig, A. J., Garcia-Lezana, T., Labgaa, I., Haber, P. K., D’Avola, D., et al. (2021). Mutations in Circulating Tumor DNA Predict Primary Resistance to Systemic Therapies in Advanced Hepatocellular Carcinoma. Oncogene 40 (1), 140–151. doi:10.1038/s41388-020-01519-1
Wang, B. G., Huang, H. Y., Chen, Y. C., Bristow, R. E., Kassauei, K., Cheng, C. C., et al. (2003). Increased Plasma DNA Integrity in Cancer Patients. Cancer Res. 63 (14), 3966–3968.
Wong, I. H., Lo, Y. M., Yeo, W., Lau, W. Y., and Johnson, P. J. (2000). Frequent P15 Promoter Methylation in Tumor and Peripheral Blood from Hepatocellular Carcinoma Patients. Clin. Cancer Res. 6 (9), 3516–3521.
Wong, I. H., Zhang, J., Lai, P. B., Lau, W. Y., and Lo, Y. M. (2003). Quantitative Analysis of Tumor-Derived Methylated p16INK4a Sequences in Plasma, Serum, and Blood Cells of Hepatocellular Carcinoma Patients. Clin. Cancer Res. 9 (3), 1047–1052.
Wu, J., Tang, W., Huang, L., Hou, N., Wu, J., Cheng, X., et al. (2019). The Analysis of Cell-free DNA Concentrations and Integrity in Serum of Initial and Treated of Lymphoma Patients. Clin. Biochem. 63, 59–65. doi:10.1016/j.clinbiochem.2018.10.002
Xu, R.-h., Wei, W., Krawczyk, M., Wang, W., Luo, H., Flagg, K., et al. (2017). Circulating Tumour DNA Methylation Markers for Diagnosis and Prognosis of Hepatocellular Carcinoma. Nat. Mater 16 (11), 1155–1161. doi:10.1038/nmat4997
Yan, L., Chen, Y., Zhou, J., Zhao, H., Zhang, H., and Wang, G. (2018). Diagnostic Value of Circulating Cell-free DNA Levels for Hepatocellular Carcinoma. Int. J. Infect. Dis. 67, 92–97. doi:10.1016/j.ijid.2017.12.002
Yang, Y.-J., Chen, H., Huang, P., Li, C.-H., Dong, Z.-H., and Hou, Y.-L. (2011). Quantification of Plasma hTERT DNA in Hepatocellular Carcinoma Patients by Quantitative Fluorescent Polymerase Chain Reaction. Clin. Invest. Med. 34 (4), 238. doi:10.25011/cim.v34i4.15366
Yang, J. D., Mohamed, E. A., Aziz, A. O. A., Shousha, H. I., Hashem, M. B., Nabeel, M. M., et al. (2017). Characteristics, Management, and Outcomes of Patients with Hepatocellular Carcinoma in Africa: A Multicountry Observational Study from the Africa Liver Cancer Consortium. Lancet Gastroenterol. Hepatol. 2 (2), 103–111. doi:10.1016/s2468-1253(16)30161-3
Yang, J. D., Liu, M. C., and Kisiel, J. B. (2019). Circulating Tumor DNA and Hepatocellular Carcinoma. Semin. Liver Dis. 39 (4), 452–462. doi:10.1055/s-0039-1688503
Ye, Q., Ling, S., Zheng, S., and Xu, X. (2019). Liquid Biopsy in Hepatocellular Carcinoma: Circulating Tumor Cells and Circulating Tumor DNA. Mol. Cancer 18 (1), 114. doi:10.1186/s12943-019-1043-x
Zhong, S., Yeo, W., Tang, M. W., Wong, N., Lai, P. B., and Johnson, P. J. (2003). Intensive Hypermethylation of the CpG Island of Ras Association Domain Family 1A in Hepatitis B Virus-Associated Hepatocellular Carcinomas. Clin. Cancer Res. 9 (9), 3376–3382.
Keywords: cfDNA, CtDNA, Hepatocellular carcinoma, clinical application, biomarkers
Citation: Zhang Y, Liu Z, Ji K, Li X, Wang C, Ren Z, Liu Y, Chen X, Han X, Meng L, Li L and Li Z (2021) Clinical Application Value of Circulating Cell-free DNA in Hepatocellular Carcinoma. Front. Mol. Biosci. 8:736330. doi: 10.3389/fmolb.2021.736330
Received: 05 July 2021; Accepted: 14 September 2021;
Published: 29 September 2021.
Edited by:
Florence Le Calvez-Kelm, International Agency For Research On Cancer (IARC), FranceReviewed by:
Emmanuelle Gormally, Catholic University of Lyon, FranceKenneth. S Hettie, Stanford University, United States
Copyright © 2021 Zhang, Liu, Ji, Li, Wang, Ren, Liu, Chen, Han, Meng, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lifeng Li, lilifeng0317@163.com; Zhen Li, lzlyct@620.com
†These authors have contributed equally to this work and share senior authorship
 Yuyuan Zhang
Yuyuan Zhang Zaoqu Liu
Zaoqu Liu Kun Ji
Kun Ji Xin Li1,2,3
Xin Li1,2,3 Caihong Wang
Caihong Wang Zhigang Ren
Zhigang Ren Lifeng Li
Lifeng Li Zhen Li
Zhen Li