- 1Dental and Periodontal Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
- 2Department of Dental Biomaterials, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
- 3Deputy of Food and Drug Administration, Urmia University of Medical Sciences, Urmia, Iran
- 4Department of Biochemistry, Microbiology and Immunology, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 5Food and Drug Safety Research Center, Faculty of Pharmacy, Tabriz University of Medical Sciences, Tabriz, Iran
As a category of small peptides frequently found in nature, antimicrobial peptides (AMPs) constitute a major part of the innate immune system of various organisms. Antimicrobial peptides feature various inhibitory effects against fungi, bacteria, viruses, and parasites. Due to the increasing concerns of antibiotic resistance among microorganisms, development of antimicrobial peptides is an emerging tool as a favorable applicability prospect in food, medicine, aquaculture, animal husbandry, and agriculture. This review presents the latest research progress made in the field of antimicrobial peptides, such as their mechanism of action, classification, application status, design techniques, and a review on decoration of nanoparticles and polymers with AMPs that are used in treating multidrug resistance. Lastly, we will highlight recent progress in antiviral peptides to treat emerging viral diseases (e.g., anti-coronavirus peptides) and discuss the outlook of AMP applications.
Introduction
Antimicrobial resistance impends the fundamental of modern medicine to the continuing hazard from infectious diseases (World Health Organization, 2001). In fact, advancements in modern medicine, such as many medical and surgical procedures, have been facilitated by developing and using clinical classes of antibiotics. Nowadays, the antibiotic era has been threatened due to the alarming rate of multidrug resistance (MDR; Barra et al., 2020; Tuttobene et al., 2021). Furthermore, secondary infections by MDR in complicated conditions like cancers may increase the mortality (Hota et al., 2009; Yan et al., 2020; Hancock et al., 2021). Hence, to address the persistent global issues associated with MDR-related infectious diseases, there is pressing needs to develop new antimicrobial strategies and agents (Ballus et al., 2015; Faya et al., 2018).
Antimicrobial peptides (AMPs), also called host defense peptides (HDPs), are the biomolecules expressed spontaneously by a large array of species throughout the phylogenetic structure (Mahlapuu et al., 2020; Han et al., 2021). AMPs have the enhanced properties of complex functional features, especially antimicrobial, anti-biofilm and anti-inflammatory abilities (Hancock et al., 2021). They are able to combat microbial infections directly, inhibit bacterial activity, and modulate the host immune responses (Drayton et al., 2020). These peptides can be considered as one of promising strategies to MDR problems since they have broad-spectrum activities, multimodal properties, and minimal resistance generation compared to the conventional antibiotics (Deslouches et al., 2020; Tan et al., 2021). Several key problems however remain challenges in the use of AMPs as clinical drugs, including in vivo liability, toxicity, and high production costs. Although the efforts to reduce the costs are heavily ongoing; application of alternative production methods, such as biotechnological engineering, bacterial expression systems, or fermentation (Moretta et al., 2021). Furthermore, as the length of peptides directly translates into production cost in solid-phase synthesis; hence, the discovery of ultrashort and/or truncated AMPs with amino acids has been chased (Koo and Seo, 2019). Finally, some modifications are also required to improve antimicrobial activity and to increase the therapeutic potential for next-generation antimicrobial agents via chemical or physicochemical alteration of AMPs (Deslouches et al., 2020; Li et al., 2021). Nano delivery systems loaded with AMPs could be promisingly used to enable safe delivery of AMP and decrease their toxic side effects (Tang et al., 2021).
According to its updated version (October 18, 2021), the antimicrobial peptide database (APD3)1 has reported a total of 3,283 AMPs (Wang et al., 2016). The commonalities of various types of AMPs are: all AMPs are almost cationic (with an average net charge of 3.32), and the number of their residues of amino acids ranges between 10 and 60 (with an average of 33.26; Malkoski et al., 2001; Schittek et al., 2001). In this review, we will highlight recent updates regarding the classification, potential applications, and mechanism of action of AMPs and the incorporation of AMPs into Nanoparticles and Polymers which have the potential to enhance AMP activity. In addition, we will summarize the application of the AMPs and the latest research progress of using such reagents to treat emerging viral and bacterial diseases, as well as multidrug resistance from the pathogenic microorganisms. Finally, we will provide our perspectives and discuss the outlook of AMP applications in MDR.
Classification and Mechanism of Action for AMPs
AMPs are made of diversified molecules, which can be classified into four categories on the basis of secondary structural properties: β-sheet, α-helical, loop, and extended peptides (Hancock and Lehrer, 1998; Hamscher et al., 2003), and the common feature among most AMPs is the high content (nearly 50%) of hydrophobic residues and of a net positive charge. Other AMPs belonging to the amphipathic α-helical peptides group include examples, such as LL-37, cecropin, and magainin (Andersson et al., 2003). The β-strand- or β-sheet-like antimicrobial peptides, such as protegrin and the defensin family, include the structural features of two or more disulfide bridges to stabilize their conformations (Nguyen et al., 2011). The highly stable peptides constitute the less frequent group of antimicrobial peptides, which present hairpin-like loop structures interconnected via a minimum of one disulfide bridge (Wu and Hancock, 1999), for example, tachyplesins (Xu et al., 2008) or dodecapeptide (Dings et al., 2013). In addition, the extended AMPs often feature a higher content of tryptophan, proline, histidine, and arginine residues. As a result, these peptides can develop unusual secondary structures, such as the well-studied bactenecins and indolicidin (Frank et al., 1990).
Recently, many attempts have been made to develop and identify the synthetic AMPs as well (Fjell et al., 2012). The logic behind this is to shorten the size and thus optimize for bioavailability, metabolic stability, and the issues related to immunogenicity and safety for clinical trials. In addition, shorter sequences are cost-effective. Strøm et al. (2003) demonstrated the minimal length of cationic AMPs that are critical for antimicrobial activities. They showed that a varied content of charge and of bulk and lipophilicity are necessary to produce an active antibacterial peptide. For instance, a synthetic cationic tripeptide containing of one modified tryptophan edged by two arginine residues showed to eradicate gram-positive bacteria through pore formation with a MIC range of 2–4 μg/ml. As another example, HB1345 is a hexameric lipopeptides is administrated topically for the removal of broad skin infections. The MIC value of HB1345 is reported to be 1–2 μg/ml against Propionibacterium acnes (Koo and Seo, 2019). Subsequent introduction of unnatural amino acids, modification or replacement of peptide bonds within an antimicrobial peptide sequence made it possible to reach higher activity levels (Thaker et al., 2011).
AMPs are a class of antimicrobial agents that are promising to limit the development of antibiotic resistance and act as hopeful new weapons to defend against microbial pathogens. Additionally, since these agents can interact with human cell membranes, AMPs may be applied as delivery routes for various bioactive compounds, as well (Guaní-Guerra et al., 2010). While there is a promising prospect for the applications of antimicrobial peptides, AMPs are associated with these problems. (i) AMPs can disrupt the eukaryotic cell membrane; (ii) AMPs may be technically and costly to produce; (iii) Their enzyme stability or pH-sensitive pattern can vary; and (iv) The presence of specific serum and iron may cause reduction of AMP activities. To address these concerns, an ideal next-generation AMP should have these characteristics: (a) targeted action for greater antimicrobial potency; (b) minimal-to-no toxicity for the cell membranes; (c) good stability against proteases or environmental changes, such as pH or temperature; (d) slight serum binding ability; and (f) easy access and low production cost (Brogden and Brogden, 2011; Li et al., 2017). Hence, there is a need to engineer and design AMPs in order to achieve their preferred effects. The rational strategy of antibacterial peptides will consider these five properties: secondary structure, chain length, hydrophobicity, amphiphilicity, and net charge (Lei et al., 2021).
In addition, functionalized AMPs can be achieved by making peptide conjugates. Using various coupling approaches, it is very common to modify at the N-terminal end of the alpha-amino group with a carboxyl group yielding to an amide bond, an approach that is often done when the peptide is still attached to the solid support by employing standard reagents used in solid-phase peptide synthesis (SPPS). Alternatively, the conjugate can be produced in solution using the free peptide if chemo-selective coupling methods is used. The later exploits the activation by thiol-reactive maleimide groups, or amino reactive N-hydroxysuccinimides (NHS), on top of procedure, such as copper(I)-catalyzed alkyne-azide cycloaddition (CuAAC), among others (Goodge and Frey, 2020; Huan et al., 2020).
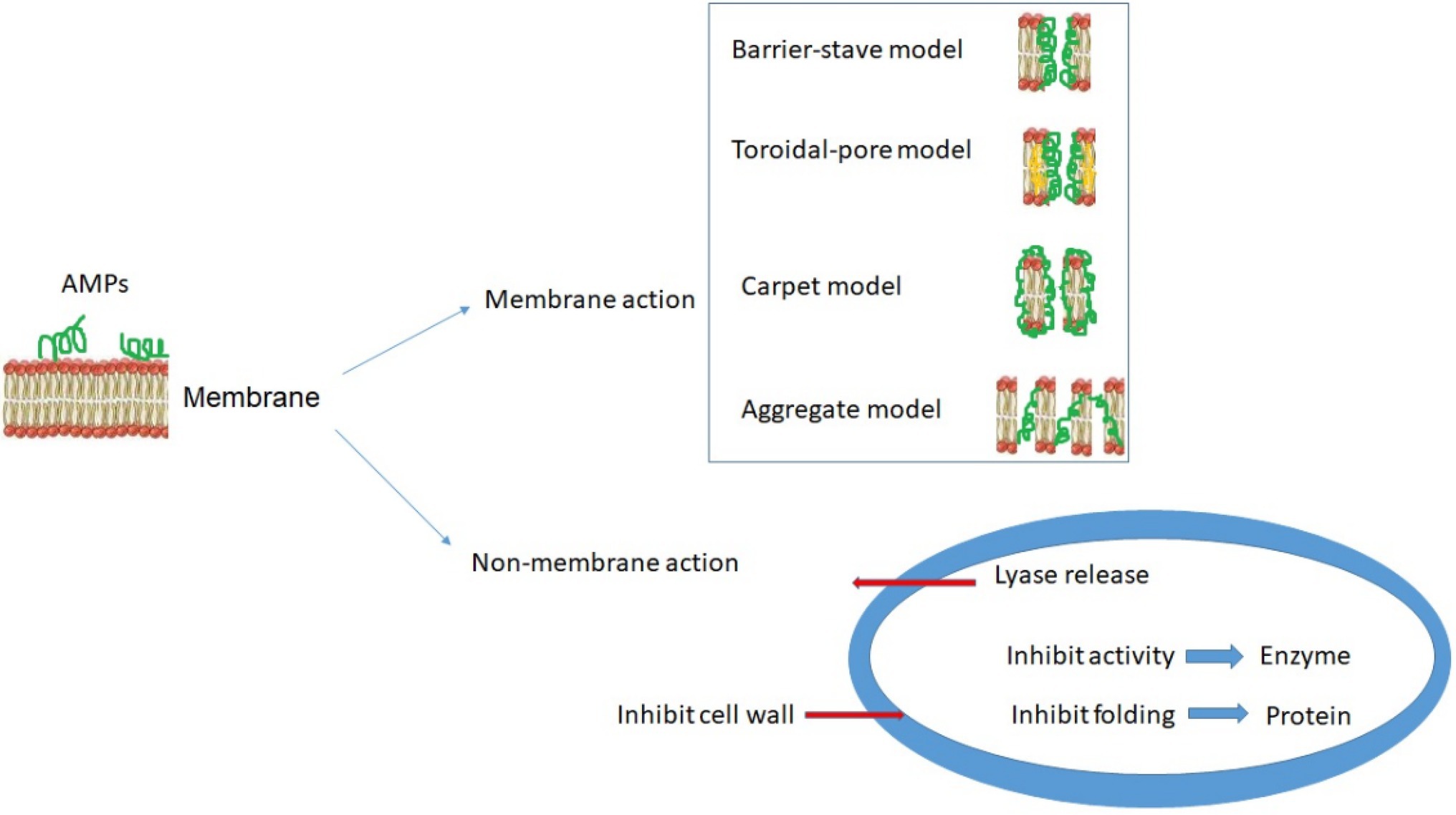
AMPs interact with pathogenic membranes by their surface electrostatic potentials and formation of secondary structures, such that the bacterial membranes can become permeable and eventually destroyed (Da Costa et al., 2015). Understanding the mechanism of AMPs will thus benefit clinical investigations that are needed to understand and evaluate how they work (Schäfer and Wenzel, 2020) and the challenges, such as toxicity of AMPs against host cells (Huang et al., 2010). Due to their cationic and amphiphilic structure, AMPs are believed to interact with negatively charged molecules (such as lipoteichoic acid and lipopolysaccharides) on the microbial outer membrane (Reinhardt and Neundorf, 2016). Hence, the lipid composition of the bacteria has a key role in the sensitivity to the AMPs especially among gram-negative bacteria with significant amounts of both anionic and zwitterionic lipids (Epand and Epand, 2009; Sani and Separovic, 2016). Specific mechanisms that have been observed or proposed include the breakdown of the membrane potential or the leakage of intracellular components, subsequently leading to cell death. So far, as illustrated in Figure 1, the toroidal-pore, the barrel-stave, the carpet-like, and the aggregate models are proposed for membrane-dependent action of AMPs (Brogden, 2005; Schäfer and Wenzel, 2020). The new findings of the toroidal-pore model are showed as an efficient antimicrobial mechanism through the accumulation of peptides on the membrane surface. This aggregation of peptides on the membrane surface and interaction through phospholipid head groups causes the membrane to bend continuously through the pores. Finally, the formation of large diameter pores causes the cell membrane disintegration in microbial pathogens (Matsuzaki et al., 1996; Yang et al., 2001).
The barrel-stave model on the other hand is a two-step process. In this model, the hydrophobic surface of the peptides connected to the microbial membrane and then the peptides enter the hydrophobic region. At the same time, the hydrophilic surface of the peptides tends inward to form a hydrophilic core (Ehrenstein and Lecar, 1977; Di Luca et al., 2014; Kang et al., 2014). Lastly, in the carpet-like model, peptides surround the entire surface area of the bacterial membrane like a carpet. Then, peptides bound to the surface of the bacterial membrane facilitate permeability, and subsequently, the microbial membrane is disrupted by peptides through the mechanism of micelle formation (Pouny et al., 1992; Bechinger, 1999; Fernandez et al., 2012). In addition to membrane permeability processes, AMPs can target microbial pathogenesis through membrane-independent mechanisms (Figure 1, lower panel), including intracellular targets through the inhibition of cell wall synthesis, disruption of DNA, RNA and protein synthesis, and inactivation of relevant enzymes (Brötz et al., 1998; Patrzykat et al., 2002; Kavanagh and Dowd, 2004). Schäfer and Wenzel (2020) recently highlighted several in vivo tools allowing mechanistic investigations of both membrane-active AMPs and AMPs with other targets.
Incorporation of AMPs Into Nanoparticles and Polymers
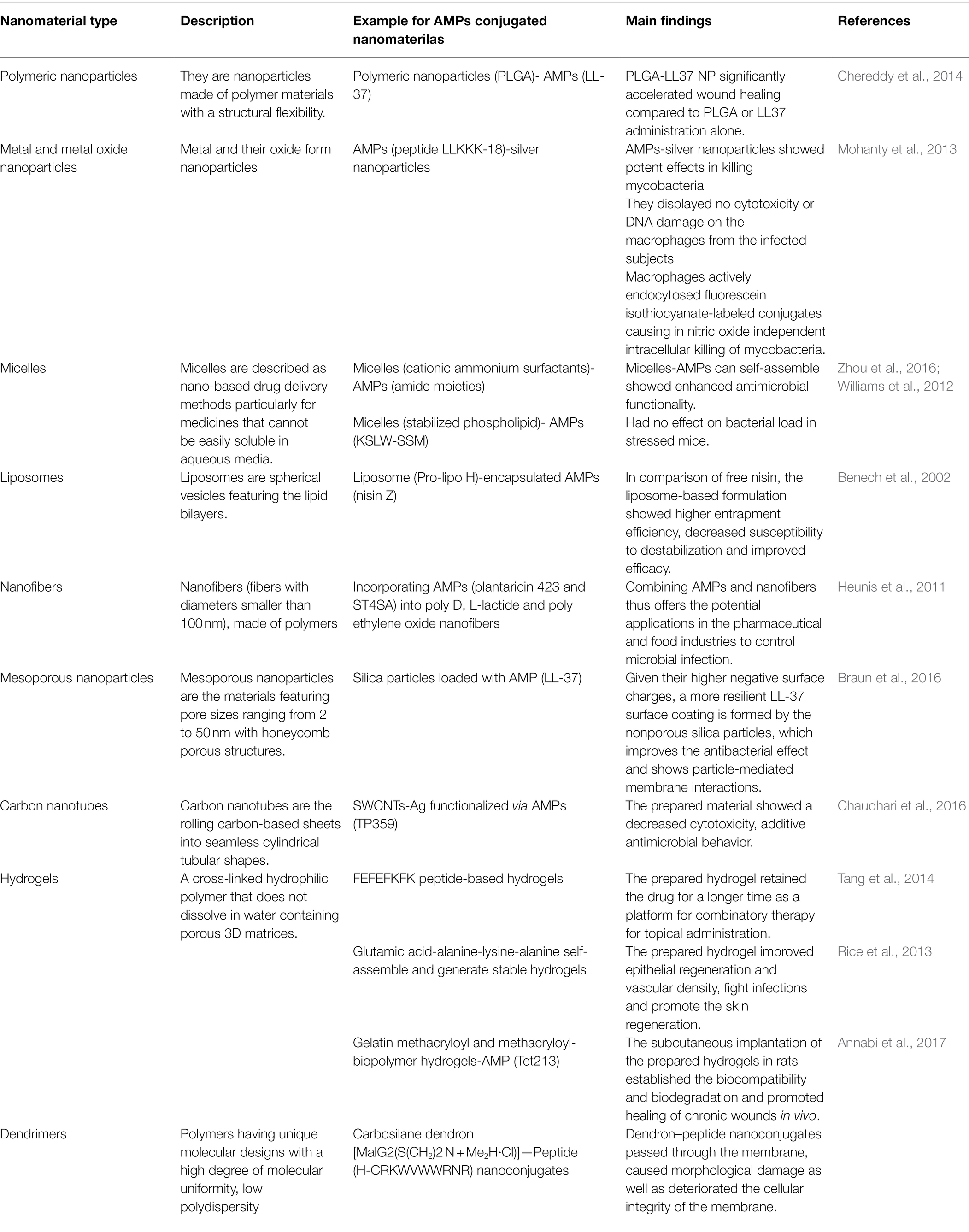
Recent advancement in nanotechnology allows research to minimize the adverse effects of natural or synthetic AMPs. Nanotechnology, an emerging field of science and engineering over the past few decades, studies designing, characterization, production, and applications of the materials, structures, tools, and systems at the nanoscale (Robles-García et al., 2016), and in particular, biomedicine benefits greatly from nanotechnology (Hoyt and Mason, 2008; Rangayasami et al., 2021). One of the major goals of nanotechnology in designing nanocarriers is to promote biomaterial delivery that can increase the effectiveness of treatment, minimize side effects, provide controlled pharmacokinetic properties, and deliver directly to the target organ with, for example, the encapsulated peptides that are protected against degradation and can reduce toxicity. For this, various nanomaterials, such as polymers, liposomes, hydrogels, and self-assembly systems, are consisted of surfactants, block (Co) and (micro) polymers of polar lipid polymers, or inorganic nanoparticles/nanomaterials that each system-specific, have been used as delivery vehicles not only for peptide transport (Weaver et al., 2021) but also for gene therapy (Bai et al., 2019), cancer therapy (Dong et al., 2019) and drug administration (Martin-Serrano et al., 2019). Drug delivery systems like grafting of AMPs into nanoparticles and polymers at the first glance could be probably sound costly or cause the additional complexity of synthesis, cost, and regulatory hurdles, but they cannot be ignored in some cases like topical or oral peptide delivery. On the other hand, by increasing the drug stability and availability, industries are increasingly more convinced to use them (Cheng et al., 2012). Table 1 summarizes some of studies in regard of different types of nanomaterials decoration by AMPs and the main findings.
AMP-Polymer Conjugates
Polymers, including polyethylene glycol (PEG), poly Lactic-co-glycolic acid (PLGA), chitosan, poly-L lysine (PLL), and hyper branched polyglycerol (HPG), are broadly employed in AMP drug delivery, in which they act as the agents carrying drugs across cellular membranes and disintegrate when reaching their specific target inside the cells (Zhang et al., 2019; Zhen et al., 2019). These polymers have also been employed in AMP delivery, protecting these peptides from degradation and allowing effective delivery (Cui et al., 2021). As a result, the peptides or antibiotics are packaged and delivered to the infected sites, ensuring precise loading on targeted pathogens and safeguarding the peptides against degradation by efflux channels and proteases (Mays, 2020).
Currently, polymer conjugates are used to administer AMP in three novel ways. First, PLGA was developed to administer esculentin-1a-derived AMP in patients with cystic fibrosis with Pseudomonas aeruginosa infection and observed improved vehicle transmission and inhibition of bacterial growth inhibition (Casciaro et al., 2019). Secondly, wound healing may be achieved by PLGA conjugates containing covalently-linked growth factors and K4 AMP. This increased sustained release and cell proliferation, and broad-spectrum antimicrobial activity (Vijayan et al., 2019). Lastly, ultrashort AMP was encapsulated in chitosan nanoparticles, which reduced the toxicity compared to free AMP and improved the antibacterial activity compared to chitosan uncharged nanoparticles (Almaaytah et al., 2017).
Polymeric Nanoparticles and Nanoparticles-AMP Conjugates
Polymeric nanoparticles, nanoparticles made of polymer materials, have shown countless potential in the treatment of a variety of diseases, owing to their structural flexibility (Elsabahy and Wooley, 2012). The polymeric nanoparticles can then be characterized through their capability of protecting the drugs against degradation by enzymes to facilitate drug crossing the cell wall barriers in bacteria and to control the rate of drug release (Vauthier and Bouchemal, 2009; Elsabahy and Wooley, 2012). In addition, many polymeric nanoparticles are bio-degradable and cleared through metabolic pathways in the bodies (Chan et al., 2010). Moreover, to facilitate the local administration and the release rate, the polymeric nanoparticles that are conjugated with peptides have been shown to demonstrate near-first-order or near-zero distribution without burst release; as a result, it has emerged as a promising system of drug delivery to treat local infections (Piotrowska et al., 2018). This was further exemplified by the application of multi-polymers, such as a combined use of chitosan and polyethylene glycol, a procedure that has been shown to decrease the propensity to aggregate and make the nanoparticles more stable and biocompatible (Calvo et al., 1997).
Antimicrobial polymeric nanoparticles have been shown as novel antibiotics to combat the rise of infectious diseases (Lam et al., 2018). This is especially illustrated by using peptides as a main element in such novel supramolecular assemblies for polymeric nanoparticles. The peptide-based nanoparticles can also improve drug delivery into the target cells by binding the nanoparticles to the cell membrane, followed by passive diffusion of drugs and/or nanoparticle phagocytosis (Soppimath et al., 2001; Salatin et al., 2015). Together, it is possible to develop more targeted antimicrobial agents against the infectious calls.
Application of AMPs at the clinical settings has been challenging largely due to their vulnerability to proteolysis or the potential toxicity to the host (Wong et al., 2020). Encapsulating AMPs, including their conjugates in appropriate nanocarriers, provides an opportunity to overcome such advert effect when targeting the site infected by bacteria and keep the peptides from fast degradation (Roy et al., 2011). The AMPs encapsulation has been successfully applied for effective delivery by using a variety of nanoparticle materials (see below), including metallic nanoparticles (MNPs), micelles, liposomes, nanofibers, mesoporous nanoparticles, carbon nanotubes, and hydrogels (Faya et al., 2018).
LL37 belongs to antimicrobial peptides of cathelicidin family that was identified in humans. They are part of the innate immune system and represent the first line of defense against many invading pathogens. Chereddy et al. (2014) prepared LL37 encapsulated in PLGA nanoparticles (chemical encapsulation technique) and they declared that treatment with PLGA-LL37 NP significantly accelerated wound healing compared to PLGA or LL37 administration alone. According to their study, PLGA-LL37 NP improved angiogenesis, significantly upregulated IL-6 and VEGFa expression, and modulated the inflammatory wound response. Also, they showed antimicrobial activity PLGA-LL37 NP on Escherichia coli (Roy et al., 2011).
Metal and Metal Oxide Nanoparticles
Gold and silver-derived metallic nanoparticles (MNPs) have been shown to operate as transportation vehicles for AMPs and their conjugates, in which the functionalized nanoparticles are produced by pairing or adhesion of AMPs on the MNP surfaces (Engin and Engin, 2019). These MNPs cause membrane disruption by binding to microbial surfaces through electrostatic interactions due to the large surface area and high surface charges (Burdușel et al., 2018; Alzharani et al., 2021). Considering that most nanoparticles can concentrate in the liver, spleen, and lymph nodes, use of noble metals as resistant compounds to oxidation and erosion is an excellent option for nanoparticle production and toxicity alleviation (Jahangirian et al., 2017). In particular, silver nanoparticles (AgNPs) have shown strong antibiotic properties by disrupting the microbial cell walls and membranes (Yu et al., 2022). It is believed that the silver-based MNPs can attach to the negatively charged microbial membranes, resulting in a greater positive zeta potential and subsequently membrane rupture and permeation (Mi et al., 2018). Interestingly, recent studies by Mohanty et al. (2013) have shown that the synthesized AMPs-silver nanoparticles (synthesized using plant extract and loopful spore methods) are potent in killing mycobacteria, while the conjugates displayed no cytotoxicity or DNA damage on the macrophages from the infected subjects. Macrophages here actively endocytosed fluorescein isothiocyanate-labeled conjugates causing in nitric oxide independent intracellular killing of mycobacteria.
Micelles
Micelles were first described as nano-based drug delivery methods in 1980s, particularly for medicines that cannot be easily soluble in aqueous media (Maghsoudnia et al., 2020). Because of their small sizes, micelles can solubilize hydrophobic medicines that target specific sites (Thassu et al., 2007). Micelles are amphipathic, including hydrophilic and hydrophobic blocks with varying solubility proportions in water (Thassu et al., 2007). Using micelles, some cationic AMPs can self-assemble and have been shown to form a comprehensive range of functions and minimal minimum inhibitory concentration (MIC) rates (Zhou et al., 2016).
Liposomes
Liposomes are spherical vesicles featuring the lipid bilayers broadly used in drug delivery studies. It has been shown that liposomes can extend the drug half-life, biodegradability and/or biocompatibility, and decrease toxicity, making them very attractive solutions for biomedical studies (Fathi and Oyelere, 2016; Allahou et al., 2021). Recent studies, for example, showed that liposomes enhance the bioactive molecules’ delivery by acting as a circulating micro-reservoir for sustained releases (Karimi et al., 2015). In addition, liposomes are able to encapsulate both hydrophobic and hydrophilic substances by nature, which makes them an ideal nanostructure for amphiphilic compounds’ delivery (Pinilla et al., 2021). A critical challenge however is the premature delivery of the payloads before reaching the target sites (Swaminathan and Ehrhardt, 2012), or the encapsulation efficiency for clinical dosage is low, which requires the use of higher liposome volumes (Swaminathan and Ehrhardt, 2012). Benech et al. (2002) prepared and investigated the liposome-encapsulated nisin (molecular self-assembling method) and discovered that the encapsulation provided higher entrapment efficiency along with decreased susceptibility to destabilization. In comparison of free nisin, the liposome-based formulation showed an improved efficacy against Listeria monocytogenes.
Nanofibers
Nanofibers (fibers with diameters smaller than 100 nm), made of polymers specially processed to produce filaments, have shown as another promising vehicles for AMPs or AMP conjugates (Subbiah et al., 2005). To synthesize the nanofibers, scientists utilize electrospinning, a process that the electric stress is used to produce charged strands of polymeric mixture (Subbiah et al., 2005). The polymers can be made of natural or artificial polymers, including chitin, chitosan, polyurethane, poly (L-lactic acid), or polyvinyl alcohol (Hu et al., 2014). Because of the high surface-to-volume proportion and the ability to modify their surfaces, nanofibers are excellent for AMP loading and distribution. Heunis et al. (2011) recently demonstrated incorporating AMPs into nanofibers (using electrospinning method) as a new method for delivering the prepared nanofibers had size ranging from 200 to 450 nm and a loading efficiency of 78 percent. AMPs in wound dressings by making bacteriocins stay active after electrospinning the peptides into nanofiber surfaces. Combining AMPs and nanofibers thus offers the potential applications in the pharmaceutical and food industries to control microbial infection.
Mesoporous Nanoparticles
Mesoporous nanoparticles are the materials featuring pore sizes ranging from 2 to 50 nm with honeycomb porous structures (Antonelli and Ying, 1996). The mechanism of forming the mesoporous pores is unclear, while it is possible to control the morphology and the orientation of the pores (Ciesla and Schüth, 1999). Silica-based mesoporous materials are the main group of this materials with the outstanding advantage of their biocompatibility, uniformly tunable pore sizes, modifiable particle sizes, high pore volume, and high specific surface area (Kwon et al., 2013). Due to their tendency and selectivity to interact with cell membrane, the use of mesoporous nanoparticles as AMP carriers has been instrumental and effective for both free peptide and peptide-loaded nanoparticles. Recent studies by Braun et al. (2016) showed that the porosity of mesoporous nanoparticles could control AMP loading and release, as well as the antimicrobial activity. Such modification makes the loading for various quantities and molecular shapes of drugs possible. The larger are the pore sizes, the greater the release rates will be and therefore the higher and better antimicrobial action can be gained.
The antibacterial capacity can also be affected by the charge of mesoporous materials (Jia et al., 2012). By testing cationic and anionic non-porous and mesoporous silica particles loaded with AMP (LL-37), the proteolytic activity on LL-37 was better prevented by the anionic mesoporous silica particles. Given their higher negative surface charges, a more resilient LL-37 surface coating is formed by the non-porous silica particles (size range of 294 to 306 nm and a slow release pattern of LL-37), which improves the antibacterial effect and shows particle-mediated membrane interactions (Braun et al., 2016). The challenge is however the cytotoxicity on the erythrocytes by the nanoparticles of positively charged mesoporous silica. There are thus needs to improve such mesoporous nanoparticle strategy, despite its promotion of membrane-disrupting activity. Nevertheless, other strategies, such as bonding (capping) of a peptide onto the external surface of mesoporous silica nanoparticles, have been reported to produce new controlled delivery systems (De La Torre et al., 2014). This advancement in the application of multipurpose peptides for surface functionalization of mesoporous materials can achieve cell-specific targeting of antimicrobial agents (Yu et al., 2020).
Carbon Nanotubes
Carbon nanotubes are the rolling carbon-based sheets into seamless cylindrical tubular shapes (Dresselhaus et al., 2000). Besides the improvement of drugs solubility, they can be employed as peptide transporters, near-infrared photothermal agents, vaccine individual gene carriers, or in cancer therapy (Lin et al., 2005). The antibacterial behavior of carbon nanotubes in disinfection of both Gram-negative and Gram-positive bacteria is attributed to the induction of oxidative stress and the physical bactericidal mode of carbon nanotubes that result in damages to their cellular membranes (Niu et al., 2010; Dizaj et al., 2015). Despite their great antimicrobial effects, the problems associated with their use are their low yields, high synthetic energy demands, and high dependency on hydrocarbons predominantly obtained from petroleum (Dizaj et al., 2015). To overcome such technical barriers, functionalization has been shown to resolve these issues. Chaudhari et al. (2016) tested the single-walled carbon nanotubes (SWCNTs) and covalently functionalized via AMPs for antimicrobial activity. Their microscopic results showed the peptide was indeed attached to the SWCNTs-Ag. Besides, the results showed decreased cytotoxicity and additive antimicrobial behavior for the functionalized SWCNTs, a promising step toward novel and biologically compatible nanomaterials.
Hydrogels
A hydrogel is a cross-linked hydrophilic polymer that does not dissolve in water (Borro et al., 2020). Nanohydrogels are the polymers containing porous 3D matrices. Which makes hydrogels good aqueous absorbers, can maintain oxygen penetration, and prolong drug retention when employed in topical administration (Xia et al., 2013). Two types of artificial hydrogels have been developed. One is a nanocomposite hydrogel, in which nanoparticles are embedded in hydrogel networks, whereas the other is a colloidal hydrogel of nanoparticle, in which nanoparticles are directly employed as crosslinkers to create hydrogel networks (Manconi et al., 2018).
Recently, nanohydrogels have been the focus of hydrogel use in the pharmacological applications, due to their good biocompatibility and their ability to carry AMPs against skin infections. According to the findings of Tang et al. (2014) a self-assembling octapeptide method was used to develop a hydrogel model that could be loaded with active peptides and other synergistic drugs for in vitro bioactivity tests. This retained the drug for a longer time (cumulative releases of 68%, 30%, and 39% were observed after 2 h for the 20, 30, and 40 mg L−1 samples, respectively.), a promising way for a combinatory therapy for topical administration. Rice et al. (2013) further showed that once the hydrogels for delivering bioactive molecules known as healing accelerators [e.g., nitric oxide (NO)]; it can improve epithelial regeneration and vascular density, fight infections, and ultimately, promote the skin regeneration. In a recent study, Annabi et al. (2017) designed a new biocompatible hydrogel-AMP conjugate using light-induced crosslinking method and abroad-spectrum antimicrobial activity against Gram-positive or Gram-negative bacteria. The subcutaneous implantation of the prepared hydrogels in rats established their biocompatibility and biodegradation and promoted healing of chronic wounds in vivo.
Dendrimers
Dendrimers signify a class of different polymers having unique molecular designs characterized by their well-defined structure, with a high degree of molecular uniformity, low polydispersity and properties that make them attractive materials for the development of nanomedicines (Samad et al., 2009). The most common dendrimers are polyamidoamine (PAMAM), polypropyleneimine (PPI), poly-l-lysine (PLL), polyglycerol (PG), poly(benzyl ether), carbosilane, or phosphorous dendrimers (Kawano et al., 2020). Nano dendrimers as carriers for AMPs suffer from some basic shortcomings like the limited efficacy, short-lasting bioactivity, and concerns of toxicity as well as high production costs (Kiparissides and Kammona, 2013). Fernandez et al. (2019) recently reported Carbosilane Dendron–Peptide Nanoconjugates with a maleimide group in the focal point that could attach different AMPs containing a cysteine residue in their structure as antimicrobial agents. In this study, the capacity of dendron–peptide nanoconjugates was shown to pass through the membrane, causing morphological damage as well as deteriorating the cellular integrity of the membrane.
Antiviral Peptides
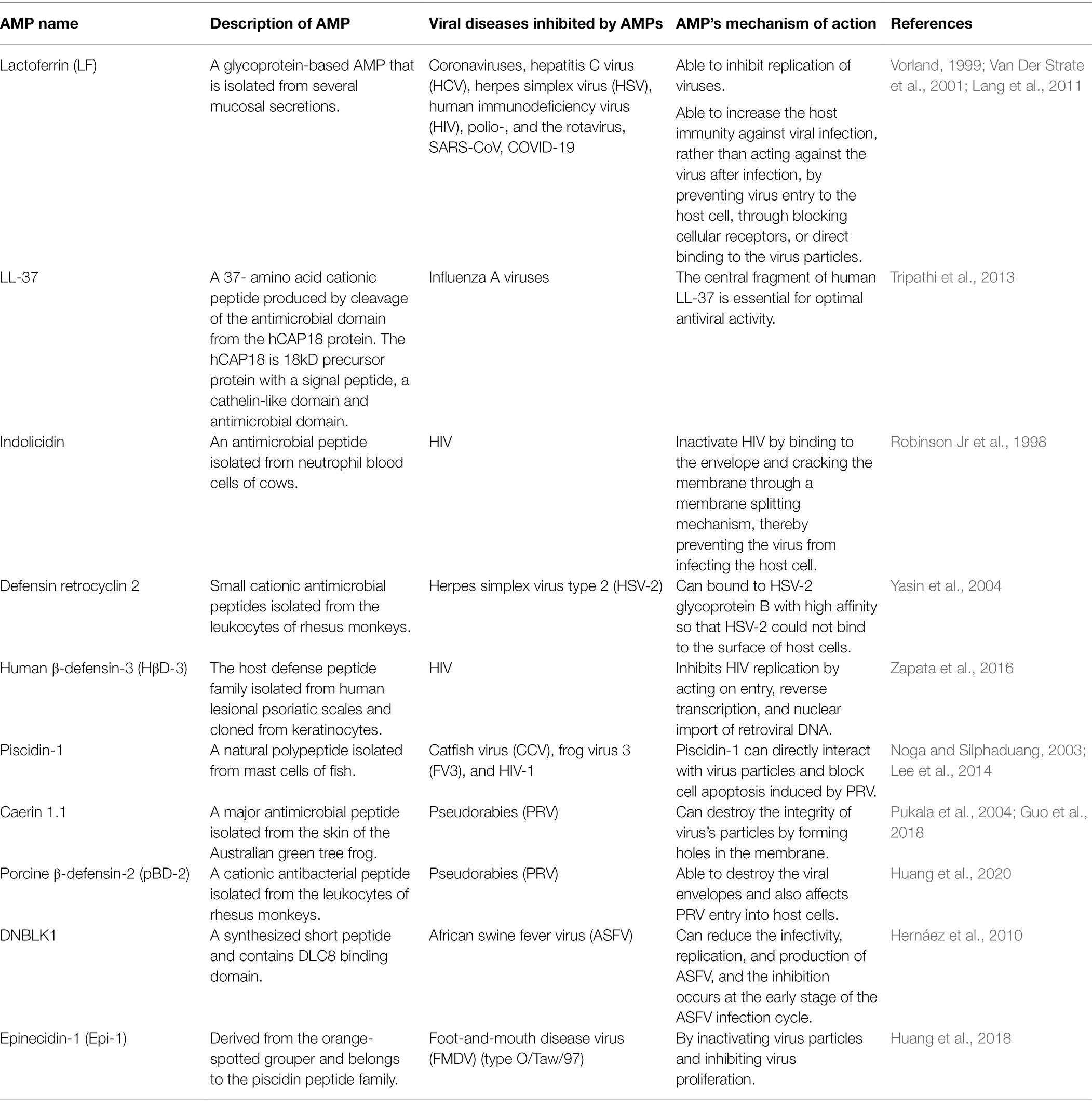
In addition to bacteria-based infectious diseases, viruses are known to cause serious diseases that have a severe impact on economy and public health. Recently, the outbreak of the COVID-19 has led to a dramatic loss of human life worldwide. Other long-term threats to human life include HIV, avian influenza virus (AIV), and foot-and-mouth disease virus. Therefore, there is an urgent need to solve the global problems caused by viruses, and in this case antiviral peptides provide new and promising strategies. Antiviral peptides exhibit inhibitory activity against viruses by (1) impeding viral interaction and membrane fusion, (2) disrupting the integrity of the envelope, and (3) preventing the replication of virus (Eftekhari et al., 2019; Jung et al., 2019). For example, AMP Epi-1 has been shown to exert an excellent anti-foot-and-mouth disease virus effect (Huang et al., 2018). Infectious bronchitis is a viral disease caused by infectious bronchitis virus (IBV), and the mortality of chicken embryos was shown to decrease significantly after they were inoculated with swine intestinal AMP (SIAMP)-IBV solution, compared with the IBV infection group. These results indicated that SIAMP can contribute to an inhibition of this virus (Sun et al., 2010). Nowadays, there is a wide variety of anti-HIV peptides, such as defensins, LL-37, caerin 1, siamycin-I, siamycin-II, dermaseptin-S1, dermaseptin-S4, gramicidin D, maximin 3, magainin 2, and RP 71955. Notably, Fuzeon™ (enfuvirtide) is an approved medication to treat HIV patients (Ashkenazi et al., 2011).
Owing to the rapid outbreak of COVID-19 worldwide, we will focus our discussion on the use of antiviral peptides against the coronaviruses. Morphologically, coronaviruses (CoVs), a group of coronaviridae, are enveloped viruses containing a single strand of positive-sense RNA genome and a helical symmetry (Franks and Galvin, 2014). CoVs, including SARS-CoV (severe acute respiratory syndrome CoV) and MERS-CoV (Middle East respiratory syndrome coronavirus; Mustafa et al., 2018), and SARS-CoV-2 (the new strain causing COVID-19) have resulted in outbreaks with life-threatening respiratory diseases over the past two decades. CoVs consist of the membrane (M), the envelope (E), the spike (S), and the nucleocapsid (N) proteins (Boas et al., 2019), in which S proteins are responsible for the viral infection. Fusion inhibitory peptides in principle can interact with the S protein to block its folding, thereby preventing viral infection. The S protein of SARS-CoV contains two heptad repeats HR1 and HR2 domains in their S2 subunit. Peptide HR2 and its lipid-binding subunit appear to be same or similar to the near-membrane part of S protein ferredoxin, which inhibit refolding into post-fusion fusion-catalyzing domains (FDs; Du et al., 2009; Park and Gallagher, 2017). Overall, AMPs against coronavirus can be derived from (i) HR1, HR2 and RBD domains of the S protein, (ii) non-structural proteins, and (iii) other AMPs (Mustafa et al., 2018).
The EK1-derived lipopeptide (SLDQINVTFLDLEYEMK KLEEAIKKLEESYIDLKEL), has been shown to have the highest inhibitory activity against the S-mediated fusion capacity of COVID-19 (Xia et al., 2020). The results obtained by protein-peptide docking and homology modeling indicated that temporin has good inhibitory effect on MERS-CoV (Marimuthu et al., 2020). It was found that AMPs (K12 and K29) derived from the SARS-CoV-non-structural protein (nsp10), can suppress the replication of SARS-CoV (Ke et al., 2012). Moreover, the mortality induced by SARS-CoV reduced remarkably in animals after treatment with rhesus theta-defensin 1 (RTD-1), by which the airway immunomodulatory was a possible process responsible for its action (Wohlford-Lenane et al., 2009). Molecular docking has demonstrated that peptides are able to prevent the attachment of COVID-19 to ACE2 (angiotensin-converting enzyme 2) and suppress the entry of COVID-19 into host cells (Souza et al., 2020), albeit the studies are currently limited at the preclinical stage. Nevertheless, with the antiviral database (AVPdb2) available and containing collections of antiviral peptides, peptide-based drug administration via the nasal route will exhibit an important area of research for AMPs as potential drugs for the therapy of coronavirus-caused respiratory diseases. Table 2 summarizes some antimicrobial peptides as an antiviral agent.
AMPs and Multidrug Resistance Transporters
The drug resistance process is mediated by various mechanisms leads to the failure of the drug-based treatment of numerous infectious diseases. The expansion of multidrug resistance (MDR) in cancer cells is also another serious risk that many anticancer drugs lose their therapeutic activity. One major cause for MDR is the action of multidrug resistance transporters that block unrelated compounds from retention inside the cells (Bolhuis et al., 1997). The mechanistic understanding of MDR transporters is so far elusive and a main subject of pharmacological/pharmaceutical studies.
Screening for the activity of anticarcinogenic substances led to the isolation of numerous resistant strains, which were then characterized as MDR mutants because they exhibited cross-resistance to multiple distinct medicines (Lomovskaya and Lewis, 1992). In general, the known pharmaceutical transporters throughout eukaryotes and prokaryotes have been classified into two groups based on bioenergetic and morphological standards: (i) ATP-binding cassette (ABC) and (ii) secondary drug transporters (Bolhuis et al., 1997).
ABC transporter family characterized by gene sequence and structural resemblances. This protein superfamily is the main group of cell membrane transporters prearranged into seven subfamilies. Many human ABC proteins, including P-glycoprotein (P-gp/ABCB1/MDR1), breast cancer resistance protein (BCRP/ABCG2/ABCP/MXR; Veitch, 2007), and multidrug resistance protein 1 (MRP1/ABCC1) are efflux transporters, and have been known to have critical role in the development of MDR (Zaman et al., 1994; Hee Choi and Yu, 2014). These membrane transporters have the ability to enhance the efflux of chemotherapeutic drugs to reduce the intracellular concentration of drugs, which is one of the most common reasons of MDR. Human ABCB1 transporter was the first recognized ABC transporter of which its overexpression could induce drug resistance of cancer cells to a series chemotherapeutic drugs like paclitaxel, doxorubicin, and vincristine (Teng et al., 2020).
Recently some antimicrobial peptides are reported to have anticancer activity on cancer MDR cells with less toxicity. Due to the hydrophobic and cationic nature of antimicrobial peptides, they could enable special binding to cancer cells with hydrophobic and negatively charged environments. As well as binding to the cell membrane which cause cell death, antimicrobial peptides can also block the interaction between growth factors and their receptors, activating anti-angiogenic effects; inhibiting specific kinase/protease which promote the growth, invasion, and metastasis of tumor; and inhibiting special functional proteins to stop the development of cancer.
Multidrug resistance during malignancy is often triggered by the overexpression of ATP-binding cassette (ABC) transporters. Upregulation of ABC transporters, which operate as efflux pumps for chemotherapeutic medications throughout cancerous cells, may reduce intracellular drug concentrations compared to their healthy cell counterparts. Novel chemotherapeutic medicines based on antibacterial peptides have been studied, and associations with ABC transporters have been observed in several of these compounds. ABCB1-mediated MDR may be reversed by the peptide of XH-14C, which enhanced the intracellular concentration of paclitaxel, a substrate of ABCB1 (Ma et al., 2015; Robey et al., 2018). Teng et al. (2020) reported that the ATPase function of ABCB1 was stimulated by XH-14C, and they demonstrated by molecular dynamics modeling that the XH-14C-ABCB1 combination was in a sustainable binding position. The therapy with XH-14C did not affect the expression rate or localization of ABCB1.
Current Progress of AMPs in Medical Applications
Many important prospects for the approved AMPs by the US FDA are used in clinical applications, such as ophthalmology, dental, wound healing, and surgical infection (Izadi et al., 2020). Several AMPs have shown tremendous therapeutic potential against various infectious diseases caused by pathogenic bacteria, including peptide ZXR-2 (FKIGGFIKKLWRSLLA) against pathogenic bacteria of dental caries, Porphyromonas gingivalis, Streptococcus sobrinus, Streptococcus mutans, and peptide PAC-113 (Clinical trial identifier: NCT00659971) as effective antimicrobial agents against oral candidiasis (Chen et al., 2017; Sztukowska et al., 2019; Lin et al., 2021). Also, the results of several AMPs studies including in vivo and clinical trials have indicated the good therapeutic potential in treating various surgical infections and wound healing. For example, AMP PXL150 was used as an anti-infective agent in burn wounds in mice. Moreover, results of the third phase of clinical trial studies have reported documents of the pharmacological activities of AMP D2A21 as innovative antimicrobial and wound healing agent in the prevention and treatment of burn wound infections (Björn et al., 2015; Thapa et al., 2020). Regarding the field of ophthalmology, with the popularity of contact lenses and the increasing incidence of eye infections caused by various pathogenic bacteria and fungi (such as Aspergillus spp., S. aureus, P. aeruginosa, Streptococcus pneumoniae, and C. albicans), AMPs, such as Lactoferricin B and Protegrin-1, are able to control the infection effectively (Silva et al., 2013; Khan and Lee, 2020).
Methods to incorporate lipids in medical applications of AMPs have been proposed as part of drug development, including: (1) development of precursors to decrease cytotoxicity and enhance protease stability, (2) the combinational therapy using conventional antibacterial agents and AMPs, (3) designing efficient therapeutic vectors to express AMPs using engineering antimicrobial probiotics, and (4) development of an appropriate expression system using AMPs and more effective drugs. In this regard, we have observed a comprehensive AMP-formulations related to wound healing including nanoparticles, glutinous rice paper capsules, gels, creams, ointments. Moreover, hydrogels in particular demonstrated that loading AMPs in these formulations can now be used therapeutically in the treatment of wound repair (Borro et al., 2020; Thapa et al., 2020). Recent studies by Yang et al. (2001) indicated that the sponges designed with starch, HS-PEG-SH, and AMPs can significantly inhibit the development of bacterial infections (Chu et al., 2019). A variety of techniques have then been developed for improve the targeting mechanism of AMPs. These methods involve graphene, nanotubes, metal nanoparticles, quantum dots, pheromone-labeled AMPs, local environment-triggered AMPs by enzyme precursor drug release system, pH-activated AMPs, etc. (Magana et al., 2020). Various lab-based experimental results showed that fabricating novel hybrid AMPs, such as hybrid peptide PA2 (a P. aeruginosa-targeting peptide)—GNU7 (a broad-spectrum AMP) against the Pseudomonas aeruginosa OprF protein can be a promising template for managing infectious diseases (Kim et al., 2020). In line with these findings, the use of various antibiotics, such as daptomycin (a lipopeptide), lugdunin, and telavancin (a glycopeptide), as potential antimicrobial candidates for the design of AMPs and medical management of the infectious patients (Durand et al., 2019; Lampejo, 2020).
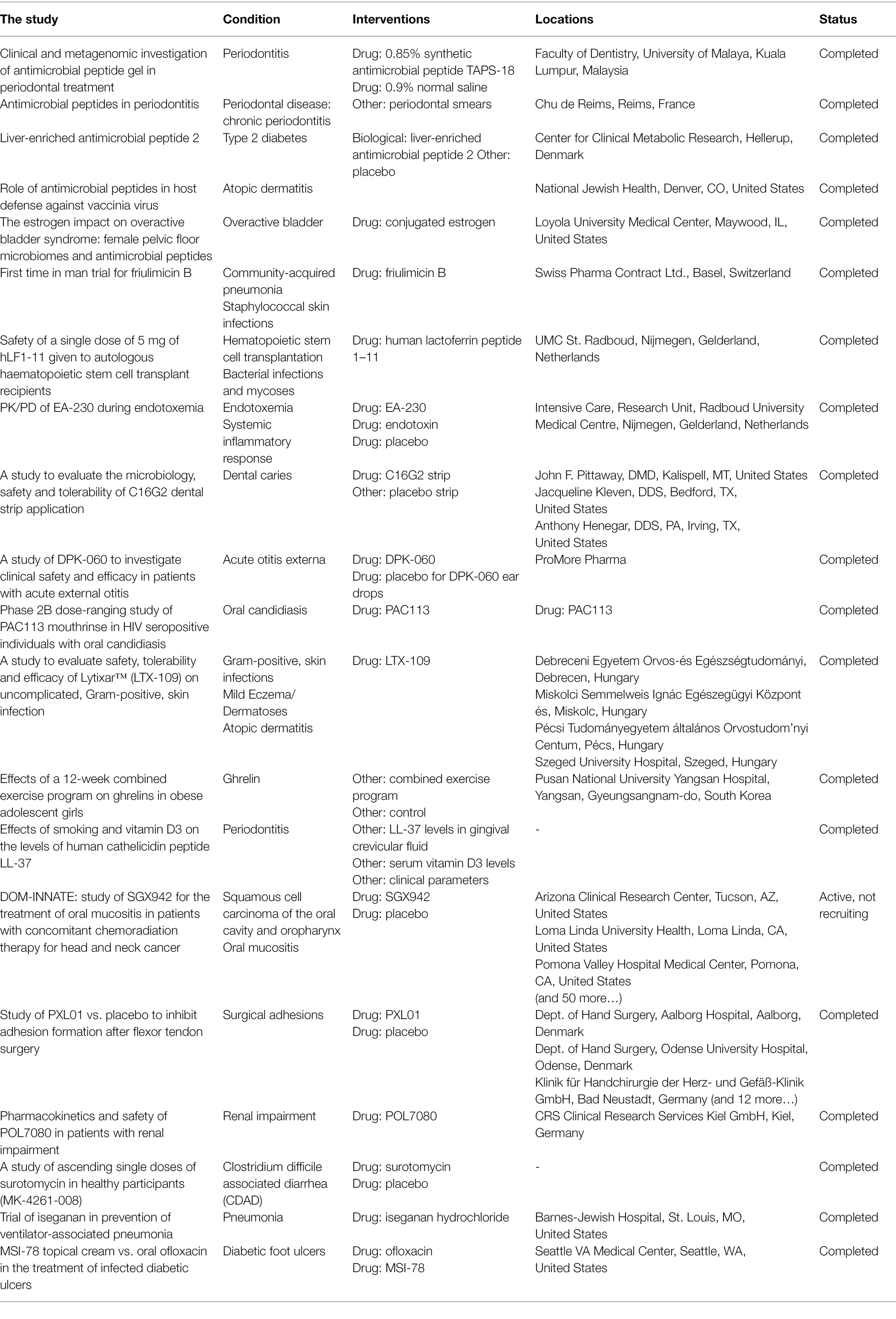
Table 3 summarizes some completed clinical trials (from https://www.clinicaltrials.gov).
AMPs have drawn increased attention due to having high activity among antibiotic-resistant pathogenesis induced by bacteria, fungi, parasites, and various types of cancer, causing disease in animals and plants. But, owing to the coevolution of pathogens and host interaction, bacterial species have developed their resistance mechanisms to sense and create an adaptive response against AMPs as well, which are playing a crucial role in their virulence within the host (Baindara et al., 2020). There are many AMPs being examined for anti-infectives in clinical settings (Costa et al., 2019; Divyashree et al., 2020). So, Understanding the various resistance mechanisms used by gram-negative and gram-positive bacteria to sense and combat AMP activities will help determine new strategies of novel therapeutic strategies to govern MDR pathogens. Furthermore, for host defense AMPs, for example, cathelicidins and defensins, could be utilized as potential compounds for host-targeted therapeutics for treating drug-resistant diseases in humans (Aslam et al., 2018). However, bacteria may even coevolve toward AMP-resistance mechanisms, resulting in low resistance. Some examples are reported so far in the case of AMPs that require specific recognition molecules, such as LPS, Lipid A, Lipid I/II, and LptD, on the membrane surface of bacteria. Nisin and polymyxin resistance are well-studied among bacterial mutants with changes in membrane and cell wall composition which is the target site of AMPs (Tresnak and Hackel, 2020). More research will be needed to understand the behavior of resistance development causing the coevolution of drug-resistant bacteria in humans in healthcare facilities (Dijksteel et al., 2021).
Conclusion and Outlook
Difficulties in the management of resistant microbes are considered as a significant challenge to discover and develop powerful medicines that can be effectively utilized against different resistant microorganisms. Recent years have witnessed a surge in the development of AMPs for antimicrobial therapy. On the other hand, a wide variety of nanoparticles have exhibited outstanding benefits for antimicrobial therapy than that of their corresponding bulk-drug formulations. It is evident from the recent studies that the AMP-decorated nanoparticles and polymers can act as an additively-enhanced combination therapeutic/delivery agent, holding considerable promise for antimicrobial therapy. This success has been obtained in minimizing the side effects and achieving the equal or higher therapeutic effects at a low dose. Nanoparticles not only have effective results on the cellular permeation of antimicrobial agents, but also improve their bioavailability compared with the plain form. Of note, the efficacy of AMP-decorated nanoparticles and polymers against pathogens and drug-resistant pathogens changes according to the physicochemical characteristics of nanoparticles, polymers, and AMPs. However, the majority of these results are from the studies performed at laboratory scale and in animal models. By further studies, the clinical fate of AMP-decorated nanoparticles and polymers should be found. Molecular level understanding of the antimicrobial action of AMP-decorated nanoparticles and polymers can establish a scientific basis to develop novel treatments. It will be assumed that in coming years, we will see great investigations on this field to bring AMP-decorated nanoparticles and polymers into pharmaceutical industry with extensive application in different antimicrobial preparations. AMPs also are appropriate as anti-biofilm agents compared to traditional antibiotics. However, the development of anti-biofilm peptides can be a more delicate process compared to that of AMP inhibitors.
Author Contributions
SM, SS, and KK wrote the different sections of review. J-YL and FL developed the initial plan and correct the final version. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Natural Sciences and Engineering Research Council (NSERC) Discovery Grant (RGPIN 2018-04070) to J-YL.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Allahou, L. W., Madani, S. Y., and Seifalian, A. (2021). Investigating the application of liposomes as drug delivery systems for the diagnosis and treatment of cancer. Int. J. Biomater. 2021:3041969. doi: 10.1155/2021/3041969
Almaaytah, A., Mohammed, G. K., Abualhaijaa, A., and Al-Balas, Q. (2017). Development of novel ultrashort antimicrobial peptide nanoparticles with potent antimicrobial and antibiofilm activities against multidrug-resistant bacteria. Drug Des. Dev. Ther. 11:3159. doi: 10.2147/DDDT.S147450
Alzharani, S., Astudillo-Calderón, S., Pintos, B., Pérez-Urria, E., Manzanera, J. A., Martín, L., et al. (2021). Role of synthetic plant extracts on the production of silver-derived nanoparticles. Plan. Theory 10:1671. doi: 10.3390/plants10081671
Andersson, M., Boman, A., and Boman, H. (2003). Ascaris nematodes from pig and human make three anti-bacterial peptides: isolation of cecropin P1 and two ASABF peptides. Cell. Mol. Life Sci. 60, 599–606. doi: 10.1007/s000180300051
Annabi, N., Rana, D., Sani, E. S., Portillo-Lara, R., Gifford, J. L., Fares, M. M., et al. (2017). Engineering a sprayable and elastic hydrogel adhesive with antimicrobial properties for wound healing. Biomaterials 139, 229–243. doi: 10.1016/j.biomaterials.2017.05.011
Antonelli, D. M., and Ying, J. Y. (1996). Mesoporous materials. Curr. Opin. Colloid Interface Sci. 1, 523–529. doi: 10.1016/S1359-0294(96)80122-1
Ashkenazi, A., Wexler-Cohen, Y., and Shai, Y. (2011). Multifaceted action of Fuzeon as virus–cell membrane fusion inhibitor. Biochim. Biophys. Acta 1808, 2352–2358. doi: 10.1016/j.bbamem.2011.06.020
Aslam, B., Wang, W., Arshad, M. I., Khurshid, M., Muzammil, S., Rasool, M. H., et al. (2018). Antibiotic resistance: a rundown of a global crisis. Infect. Drug Resist. 11, 1645–1658. doi: 10.2147/IDR.S173867
Bai, Z., Wei, J., Yu, C., Han, X., Qin, X., Zhang, C., et al. (2019). Non-viral nanocarriers for intracellular delivery of microRNA therapeutics. J. Mater. Chem. B 7, 1209–1225. doi: 10.1039/C8TB02946F
Baindara, P., Ghosh, A. K., and Mandal, S. M. J. M. D. R. (2020). Coevolution of resistance against antimicrobial peptides. Microb. Drug Resist. 26, 880–899. doi: 10.1089/mdr.2019.0291
Ballus, J., Lopez-Delgado, J. C., Sabater-Riera, J., Perez-Fernandez, X. L., Betbese, A., and Roncal, J. J. B. I. D. (2015). Surgical site infection in critically ill patients with secondary and tertiary peritonitis: epidemiology, microbiology and influence in outcomes. BMC Infect. Dis. 15:304. doi: 10.1186/s12879-015-1050-5
Barra, A. L. C., Dantas, L. D. O. C., Morão, L. G., Gutierrez, R. F., Polikarpov, I., Wrenger, C., et al. (2020). Essential metabolic routes as a way to ESKAPE from antibiotic resistance. Front. Public Health 8:26. doi: 10.3389/fpubh.2020.00026
Bechinger, B. (1999). The structure, dynamics and orientation of antimicrobial peptides in membranes by multidimensional solid-state NMR spectroscopy. Biochim. Biophys. Acta 1462, 157–183. doi: 10.1016/S0005-2736(99)00205-9
Benech, R.-O., Kheadr, E., Laridi, R., Lacroix, C., and Fliss, I. (2002). Inhibition of Listeria innocua in cheddar cheese by addition of nisin Z in liposomes or by in situ production in mixed culture. Appl. Environ. Microbiol. 68, 3683–3690. doi: 10.1128/AEM.68.8.3683-3690.2002
Björn, C., Noppa, L., Salomonsson, E. N., Johansson, A.-L., Nilsson, E., Mahlapuu, M., et al. (2015). Efficacy and safety profile of the novel antimicrobial peptide PXL150 in a mouse model of infected burn wounds. Int. J. Antimicrob. Agents 45, 519–524. doi: 10.1016/j.ijantimicag.2014.12.015
Boas, L. C. P. V., Campos, M. L., Berlanda, R. L. A., De Carvalho Neves, N., and Franco, O. L. (2019). Antiviral peptides as promising therapeutic drugs. Cell. Mol. Life Sci. 76, 3525–3542. doi: 10.1007/s00018-019-03138-w
Bolhuis, H., Van Veen, H. W., Poolman, B., Driessen, A. J., and Konings, W. N. (1997). Mechanisms of multidrug transporters. FEMS Microbiol. Rev. 21, 55–84. doi: 10.1111/j.1574-6976.1997.tb00345.x
Borro, B. C., Nordström, R., and Malmsten, M. (2020). Microgels and hydrogels as delivery systems for antimicrobial peptides. Colloids Surf. B: Biointerfaces 187:110835. doi: 10.1016/j.colsurfb.2020.110835
Braun, K., Pochert, A., Lindén, M., Davoudi, M., Schmidtchen, A., Nordström, R., et al. (2016). Membrane interactions of mesoporous silica nanoparticles as carriers of antimicrobial peptides. J. Colloid Interface Sci. 475, 161–170. doi: 10.1016/j.jcis.2016.05.002
Brogden, K. A. (2005). Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat. Rev. Microbiol. 3, 238–250. doi: 10.1038/nrmicro1098
Brogden, N. K., and Brogden, K. A. (2011). Will new generations of modified antimicrobial peptides improve their potential as pharmaceuticals? Int. J. Antimicrob. Agents 38, 217–225. doi: 10.1016/j.ijantimicag.2011.05.004
Brötz, H., Bierbaum, G., Leopold, K., Reynolds, P. E., and Sahl, H.-G. (1998). The lantibiotic mersacidin inhibits peptidoglycan synthesis by targeting lipid II. Antimicrob. Agents Chemother. 42, 154–160. doi: 10.1128/AAC.42.1.154
Burdușel, A.-C., Gherasim, O., Grumezescu, A. M., Mogoantă, L., Ficai, A., and Andronescu, E. (2018). Biomedical applications of silver nanoparticles: an up-to-date overview. Nano 8:681. doi: 10.3390/nano8090681
Calvo, P., Remunan-Lopez, C., Vila-Jato, J. L., and Alonso, M. (1997). Novel hydrophilic chitosan-polyethylene oxide nanoparticles as protein carriers. J. Appl. Polym. Sci. 63, 125–132. doi: 10.1002/(SICI)1097-4628(19970103)63:1<125::AID-APP13>3.0.CO;2-4
Casciaro, B., D’angelo, I., Zhang, X., Loffredo, M. R., Conte, G., Cappiello, F., et al. (2019). Poly (lactide-co-glycolide) nanoparticles for prolonged therapeutic efficacy of esculentin-1a-derived antimicrobial peptides against Pseudomonas aeruginosa lung infection: in vitro and in vivo studies. Biomacromolecules 20, 1876–1888. doi: 10.1021/acs.biomac.8b01829
Chan, J. M., Valencia, P. M., Zhang, L., Langer, R., and Farokhzad, O. C. (2010). “Polymeric nanoparticles for drug delivery,” in Cancer Nanotechnology (Switzerland: Springer Nature Switzerland), 163–175.
Chaudhari, A. A., Deb Nath, S., Kate, K., Dennis, V., Singh, S. R., Owen, D. R., et al. (2016). A novel covalent approach to bio-conjugate silver coated single walled carbon nanotubes with antimicrobial peptide. J. Nanobiotechnol. 14, 1–15. doi: 10.1186/s12951-016-0211-z
Chen, L., Jia, L., Zhang, Q., Zhou, X., Liu, Z., Li, B., et al. (2017). A novel antimicrobial peptide against dental-caries-associated bacteria. Anaerobe 47, 165–172. doi: 10.1016/j.anaerobe.2017.05.016
Cheng, Z., Al Zaki, A., Hui, J. Z., Muzykantov, V. R., and Tsourkas, A. J. S. (2012). Multifunctional nanoparticles: cost versus benefit of adding targeting and imaging capabilities. Science 338, 903–910. doi: 10.1126/science.1226338
Chereddy, K. K., Her, C.-H., Comune, M., Moia, C., Lopes, A., Porporato, P. E., et al. (2014). PLGA nanoparticles loaded with host defense peptide LL37 promote wound healing. J. Control. Release 194, 138–147. doi: 10.1016/j.jconrel.2014.08.016
Chu, C., Wang, Y., Wang, Y., Yang, R., Liu, L., Rung, S., et al. (2019). Evaluation of epigallocatechin-3-gallate (EGCG) modified collagen in guided bone regeneration (GBR) surgery and modulation of macrophage phenotype. Mater. Sci. Eng. C 99, 73–82. doi: 10.1016/j.msec.2019.01.083
Ciesla, U., and Schüth, F. (1999). Ordered mesoporous materials. Microporous Mesoporous Mater. 27, 131–149. doi: 10.1016/S1387-1811(98)00249-2
Costa, F., Teixeira, C., Gomes, P., and Martins, M. C. L. (2019). Clinical application of AMPs. Adv. Exp. Med. Biol. 1117, 281–298. doi: 10.1007/978-981-13-3588-4_15
Cui, Z., Luo, Q., Bannon, M. S., Gray, V. P., Bloom, T. G., Clore, M. F., et al. (2021). Molecular engineering of antimicrobial peptide (AMP)–polymer conjugates. Biomater. Sci. 9, 5069–5091. doi: 10.1039/D1BM00423A
Da Costa, J. P., Cova, M., Ferreira, R., and Vitorino, R. (2015). Antimicrobial peptides: an alternative for innovative medicines? Appl. Microbiol. Biotechnol. 99, 2023–2040. doi: 10.1007/s00253-015-6375-x
De La Torre, C., Agostini, A., Mondragón, L., Orzáez, M., Sancenón, F., Martínez-Máñez, R., et al. (2014). Temperature-controlled release by changes in the secondary structure of peptides anchored onto mesoporous silica supports. Chem. Commun. 50, 3184–3186. doi: 10.1039/C3CC49421G
Deslouches, B., Montelaro, R. C., Urish, K. L., and Di, Y. P. (2020). Engineered cationic antimicrobial peptides (eCAPs) to combat multidrug-resistant bacteria. Pharmaceutics 12:501. doi: 10.3390/pharmaceutics12060501
Di Luca, M., Maccari, G., and Nifosì, R. (2014). Treatment of microbial biofilms in the post-antibiotic era: prophylactic and therapeutic use of antimicrobial peptides and their design by bioinformatics tools. Pathog. Dis. 70, 257–270. doi: 10.1111/2049-632X.12151
Dijksteel, G. S., Ulrich, M. M., Middelkoop, E., and Boekema, B. K. J. F. I. M. (2021). Lessons learned from clinical trials using antimicrobial peptides (AMPs). Front. Microbiol. 12:616979. doi: 10.3389/fmicb.2021.616979
Dings, R. P., Haseman, J. R., Leslie, D. B., Luong, M., Dunn, D. L., and Mayo, K. H. (2013). Bacterial membrane disrupting dodecapeptide SC4 improves survival of mice challenged with Pseudomonas aeruginosa. Biochim. Biophys. Acta 1830, 3454–3457. doi: 10.1016/j.bbagen.2013.02.002
Divyashree, M., Mani, M. K., Reddy, D., Kumavath, R., Ghosh, P., Azevedo, V., et al. (2020). Clinical applications of antimicrobial peptides (AMPs): where do we stand now? Protein Pept. Lett. 27, 120–134. doi: 10.2174/0929866526666190925152957
Dizaj, S. M., Mennati, A., Jafari, S., Khezri, K., and Adibkia, K. (2015). Antimicrobial activity of carbon-based nanoparticles. Adv. Pharm. Bull. 5:19. doi: 10.5681/apb.2015.003
Dong, P., Rakesh, K., Manukumar, H., Mohammed, Y. H. E., Karthik, C., Sumathi, S., et al. (2019). Innovative nano-carriers in anticancer drug delivery-a comprehensive review. Bioorg. Chem. 85, 325–336. doi: 10.1016/j.bioorg.2019.01.019
Drayton, M., Kizhakkedathu, J. N., and Straus, S. K. (2020). Towards robust delivery of antimicrobial peptides to combat bacterial resistance. Molecules 25:3048. doi: 10.3390/molecules25133048
Dresselhaus, M. S., Dresselhaus, G., Eklund, P., and Rao, A. (2000). “Carbon nanotubes,” in The Physics of Fullerene-Based and Fullerene-Related Materials (Switzerland: Springer Nature Switzerland), 331–379.
Du, L., He, Y., Zhou, Y., Liu, S., Zheng, B.-J., and Jiang, S. (2009). The spike protein of SARS-CoV—a target for vaccine and therapeutic development. Nat. Rev. Microbiol. 7, 226–236. doi: 10.1038/nrmicro2090
Durand, G. A., Raoult, D., and Dubourg, G. (2019). Antibiotic discovery: history, methods and perspectives. Int. J. Antimicrob. Agents 53, 371–382. doi: 10.1016/j.ijantimicag.2018.11.010
Eftekhari, A., Ahmadian, E., Salatin, S., Sharifi, S., Dizaj, S. M., Khalilov, R., et al. (2019). Current analytical approaches in diagnosis of melanoma. TrAC Trends Anal. Chem. 116, 122–135. doi: 10.1016/j.trac.2019.05.004
Ehrenstein, G., and Lecar, H. (1977). Electrically gated ionic channels in lipid bilayers. Q. Rev. Biophys. 10, 1–34. doi: 10.1017/S0033583500000123
Elsabahy, M., and Wooley, K. L. (2012). Design of polymeric nanoparticles for biomedical delivery applications. Chem. Soc. Rev. 41, 2545–2561. doi: 10.1039/c2cs15327k
Engin, A. B., and Engin, A. (2019). Nanoantibiotics: a novel rational approach to antibiotic resistant infections. Curr. Drug Metab. 20, 720–741. doi: 10.2174/1389200220666190806142835
Epand, R. M., and Epand, R. F. (2009). Lipid domains in bacterial membranes and the action of antimicrobial agents. Biochim. Biophys. Acta 1788, 289–294. doi: 10.1016/j.bbamem.2008.08.023
Fathi, S., and Oyelere, A. K. (2016). Liposomal drug delivery systems for targeted cancer therapy: is active targeting the best choice? Future Med. Chem. 8, 2091–2112. doi: 10.4155/fmc-2016-0135
Faya, M., Kalhapure, R. S., Kumalo, H. M., Waddad, A. Y., Omolo, C., and Govender, T. (2018). Conjugates and nano-delivery of antimicrobial peptides for enhancing therapeutic activity. J. Drug Deliv. Sci. Technol. 44, 153–171. doi: 10.1016/j.jddst.2017.12.010
Fernandez, J., Acosta, G., Pulido, D., Maly, M., Copa-Patiño, J. L., Soliveri, J., et al. (2019). Carbosilane dendron–peptide nanoconjugates as antimicrobial agents. Mol. Pharm. 16, 2661–2674. doi: 10.1021/acs.molpharmaceut.9b00222
Fernandez, D. I., Le Brun, A. P., Whitwell, T. C., Sani, M.-A., James, M., and Separovic, F. (2012). The antimicrobial peptide aurein 1.2 disrupts model membranes via the carpet mechanism. Phys. Chem. Chem. Phys. 14, 15739–15751. doi: 10.1039/c2cp43099a
Fjell, C. D., Hiss, J. A., Hancock, R. E., and Schneider, G. (2012). Designing antimicrobial peptides: form follows function. Nat. Rev. Drug Discov. 11, 37–51. doi: 10.1038/nrd3591
Frank, R. W., Gennaro, R., Schneider, K., Przybylski, M., and Romeo, D. (1990). Amino acid sequences of two proline-rich bactenecins. Antimicrobial peptides of bovine neutrophils. J. Biol. Chem. 265, 18871–18874. doi: 10.1016/S0021-9258(17)30595-1
Franks, T. J., and Galvin, J. R. (2014). “Coronavirus,” in Viruses and the Lung (Switzerland: Springer Nature Switzerland), 109–116.
Goodge, K., and Frey, M. (2020). Biotin-conjugated cellulose nanofibers prepared via copper-catalyzed alkyne-azide cycloaddition (CuAAC)“click” chemistry. Nano 10:1172. doi: 10.3390/nano10061172
Guaní-Guerra, E., Santos-Mendoza, T., Lugo-Reyes, S. O., and Terán, L. M. (2010). Antimicrobial peptides: general overview and clinical implications in human health and disease. Clin. Immunol. 135, 1–11. doi: 10.1016/j.clim.2009.12.004
Guo, N., Zhang, B., Hu, H., Ye, S., Chen, F., Li, Z., et al. (2018). Caerin1. 1 suppresses the growth of porcine epidemic diarrhea virus in vitro via direct binding to the virus. Viruses 10:507. doi: 10.3390/v10090507
Hamscher, G., Pawelzick, H. T., Sczesny, S., Nau, H., and Hartung, J. (2003). Antibiotics in dust originating from a pig-fattening farm: a new source of health hazard for farmers? Environ. Health Perspect. 111, 1590–1594. doi: 10.1289/ehp.6288
Han, Y., Zhang, M., Lai, R., and Zhang, Z. (2021). Chemical modifications to increase the therapeutic potential of antimicrobial peptides. Peptides 146:170666. doi: 10.1016/j.peptides.2021.170666
Hancock, R. E., Alford, M. A., and Haney, E. F. (2021). Antibiofilm activity of host defence peptides: complexity provides opportunities. Nat. Rev. Microbiol. 19, 786–797. doi: 10.1038/s41579-021-00585-w
Hancock, R. E., and Lehrer, R. (1998). Cationic peptides: a new source of antibiotics. Trends Biotechnol. 16, 82–88. doi: 10.1016/S0167-7799(97)01156-6
Hee Choi, Y., and Yu, A.-M. J. C. P. D. (2014). ABC transporters in multidrug resistance and pharmacokinetics, and strategies for drug development. Curr. Pharm. Des. 20, 793–807. doi: 10.2174/138161282005140214165212
Hernáez, B., Tarragó, T., Giralt, E., Escribano, J. M., and Alonso, C. J. J. O. V. (2010). Small peptide inhibitors disrupt a high-affinity interaction between cytoplasmic dynein and a viral cargo protein. J. Virol. 84, 10792–10801. doi: 10.1128/JVI.01168-10
Heunis, T., Bshena, O., Klumperman, B., and Dicks, L. (2011). Release of bacteriocins from nanofibers prepared with combinations of poly (D, L-lactide)(PDLLA) and poly (ethylene oxide)(PEO). Int. J. Mol. Sci. 12, 2158–2173. doi: 10.3390/ijms12042158
Hota, S., Hirji, Z., Stockton, K., Lemieux, C., Dedier, H., Wolfaardt, G., et al. (2009). Outbreak of multidrug-resistant Pseudomonas aeruginosa colonization and infection secondary to imperfect intensive care unit room design. Infect. Control Hosp. Epidemiol. 30, 25–33. doi: 10.1086/592700
Hoyt, V. W., and Mason, E. (2008). Nanotechnology: emerging health issues. J. Chem. Health Saf. 15, 10–15. doi: 10.1016/j.jchas.2007.07.015
Hu, X., Liu, S., Zhou, G., Huang, Y., Xie, Z., and Jing, X. (2014). Electrospinning of polymeric nanofibers for drug delivery applications. J. Control. Release 185, 12–21. doi: 10.1016/j.jconrel.2014.04.018
Huan, Y., Kong, Q., Mou, H., and Yi, H. (2020). Antimicrobial peptides: classification, design, application and research progress in multiple fields. Front. Microbiol. 11:2559. doi: 10.3389/fmicb.2020.582779
Huang, H.-N., Pan, C.-Y., and Chen, J.-Y. (2018). Grouper (Epinephelus coioides) antimicrobial peptide epinecidin-1 exhibits antiviral activity against foot-and-mouth disease virus in vitro. Peptides 106, 91–95. doi: 10.1016/j.peptides.2018.07.003
Huang, J., Qi, Y., Wang, A., Huang, C., Liu, X., Yang, X., et al. (2020). Porcine β-defensin 2 inhibits proliferation of pseudorabies virus in vitro and in transgenic mice. Virol. J. 17:18. doi: 10.1186/s12985-020-1288-4
Huang, J.-F., Xu, Y.-M., Hao, D.-M., Huang, Y.-B., Liu, Y., and Chen, Y. (2010). Structure-guided de novo design of α-helical antimicrobial peptide with enhanced specificity. Pure Appl. Chem. 82, 243–257. doi: 10.1351/PAC-CON-09-01-12
Izadi, N., Keikha, M., Ghazvini, K., and Karbalaei, M. (2020). Oral antimicrobial peptides and new therapeutic strategies for plaque-mediated diseases. Gene Rep. 21:100811. doi: 10.1016/j.genrep.2020.100811
Jahangirian, H., Lemraski, E. G., Webster, T. J., Rafiee-Moghaddam, R., and Abdollahi, Y. (2017). A review of drug delivery systems based on nanotechnology and green chemistry: green nanomedicine. Int. J. Nanomedicine 12:2957. doi: 10.2147/IJN.S127683
Jia, L., Shen, J., Li, Z., Zhang, D., Zhang, Q., Duan, C., et al. (2012). Successfully tailoring the pore size of mesoporous silica nanoparticles: exploitation of delivery systems for poorly water-soluble drugs. Int. J. Pharm. 439, 81–91. doi: 10.1016/j.ijpharm.2012.10.011
Jung, Y., Kong, B., Moon, S., Yu, S.-H., Chung, J., Ban, C., et al. (2019). Envelope-deforming antiviral peptide derived from influenza virus M2 protein. Biochem. Biophys. Res. Commun. 517, 507–512. doi: 10.1016/j.bbrc.2019.07.088
Kang, S.-J., Park, S. J., Mishig-Ochir, T., and Lee, B.-J. (2014). Antimicrobial peptides: therapeutic potentials. Expert Rev. Anti-Infect. Ther. 12, 1477–1486. doi: 10.1586/14787210.2014.976613
Karimi, N., Ghanbarzadeh, B., Hamishehkar, H., Keyvani, F., Pezeshki, A., and Gholian, M.M. (2015). Phytosome and liposome: the beneficial encapsulation systems in drug delivery and food application. Appl. Food Biotechnol. 2, 17–27.
Kavanagh, K., and Dowd, S. (2004). Histatins: antimicrobial peptides with therapeutic potential. J. Pharm. Pharmacol. 56, 285–289. doi: 10.1211/0022357022971
Kawano, Y., Jordan, O., Hanawa, T., Borchard, G., and Patrulea, V. (2020). Are antimicrobial peptide dendrimers an escape from ESKAPE? Adv. Wound Care 9, 378–395. doi: 10.1089/wound.2019.1113
Ke, M., Chen, Y., Wu, A., Sun, Y., Su, C., Wu, H., et al. (2012). Short peptides derived from the interaction domain of SARS coronavirus nonstructural protein nsp10 can suppress the 2′-O-methyltransferase activity of nsp10/nsp16 complex. Virus Res. 167, 322–328. doi: 10.1016/j.virusres.2012.05.017
Khan, S. A., and Lee, C.-S. (2020). Recent progress and strategies to develop antimicrobial contact lenses and lens cases for different types of microbial keratitis. Acta Biomater. 113, 101–118. doi: 10.1016/j.actbio.2020.06.039
Kim, H., Jang, J. H., Kim, S. C., and Cho, J. H. (2020). Development of a novel hybrid antimicrobial peptide for targeted killing of Pseudomonas aeruginosa. Eur. J. Med. Chem. 185:111814. doi: 10.1016/j.ejmech.2019.111814
Kiparissides, C., and Kammona, O. (2013). Nanoscale carriers for targeted delivery of drugs and therapeutic biomolecules. Can. J. Chem. Eng. 91, 638–651. doi: 10.1002/cjce.21685
Koo, H. B., and Seo, J. J. P. S. (2019). Antimicrobial peptides under clinical investigation. Pept. Sci. 111:e24122. doi: 10.1002/pep2.24122
Kwon, S., Singh, R. K., Perez, R. A., Abou Neel, E. A., Kim, H.-W., and Chrzanowski, W. (2013). Silica-based mesoporous nanoparticles for controlled drug delivery. J. Tissue Eng. 4:204173141350335. doi: 10.1177/2041731413503357
Lam, S. J., Wong, E. H., Boyer, C., and Qiao, G. G. (2018). Antimicrobial polymeric nanoparticles. Prog. Polym. Sci. 76, 40–64. doi: 10.1016/j.progpolymsci.2017.07.007
Lampejo, T. (2020). Dalbavancin and telavancin in the treatment of infective endocarditis: a literature review. Int. J. Antimicrob. Agents 56:106072. doi: 10.1016/j.ijantimicag.2020.106072
Lang, J., Yang, N., Deng, J., Liu, K., Yang, P., Zhang, G., et al. (2011). Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLoS One 6:e23710. doi: 10.1371/journal.pone.0023710
Lee, E., Shin, A., Jeong, K.-W., Jin, B., Jnawali, H. N., Shin, S., et al. (2014). Role of phenylalanine and valine10 residues in the antimicrobial activity and cytotoxicity of piscidin-1. PLoS One 9:e114453. doi: 10.1371/journal.pone.0114453
Lei, M., Jayaraman, A., Van Deventer, J. A., and Lee, K. (2021). Engineering selectively targeting antimicrobial peptides. Annu. Rev. Biomed. Eng. 23, 339–357. doi: 10.1146/annurev-bioeng-010220-095711
Li, J., Koh, J.-J., Liu, S., Lakshminarayanan, R., Verma, C. S., and Beuerman, R. W. (2017). Membrane active antimicrobial peptides: translating mechanistic insights to design. Front. Neurosci. 11:73. doi: 10.3389/fnins.2017.00073
Li, W., Separovic, F., O'Brien-Simpson, N. M., and Wade, J. D. (2021). Chemically modified and conjugated antimicrobial peptides against superbugs. Chem. Soc. Rev. 50, 4932–4973. doi: 10.1039/D0CS01026J
Lin, B., Li, R., Handley, T. N., Wade, J. D., Li, W., and O’Brien-Simpson, N. M. (2021). Cationic antimicrobial peptides are leading the way to combat oropathogenic infections. ACS Infect. Dis. 7, 2959–2970. doi: 10.1021/acsinfecdis.1c00424
Lin, Y., Yantasee, W., and Wang, J. (2005). Carbon nanotubes (CNTs) for the development of electrochemical biosensors. Front. Biosci. 10:492. doi: 10.2741/1545
Lomovskaya, O., and Lewis, K. (1992). Emr, an Escherichia coli locus for multidrug resistance. Proc. Natl. Acad. Sci. 89, 8938–8942. doi: 10.1073/pnas.89.19.8938
Ma, W., Feng, S., Yao, X., Yuan, Z., Liu, L., and Xie, Y. (2015). Nobiletin enhances the efficacy of chemotherapeutic agents in ABCB1 overexpression cancer cells. Sci. Rep. 5:18789. doi: 10.1038/srep18789
Magana, M., Pushpanathan, M., Santos, A. L., Leanse, L., Fernandez, M., Ioannidis, A., et al. (2020). The value of antimicrobial peptides in the age of resistance. Lancet Infect. Dis. 20, e216–e230. doi: 10.1016/S1473-3099(20)30327-3
Maghsoudnia, N., Eftekhari, R. B., Sohi, A. N., Zamzami, A., and Dorkoosh, F. A. (2020). Application of nano-based systems for drug delivery and targeting: a review. J. Nanopart. Res. 22, 1–41.
Mahlapuu, M., Björn, C., and Ekblom, J. J. C. R. I. B. (2020). Antimicrobial peptides as therapeutic agents: opportunities and challenges. Crit. Rev. Biotechnol. 40, 978–992. doi: 10.1080/07388551.2020.1796576
Malkoski, M., Dashper, S. G., O'Brien-Simpson, N. M., Talbo, G. H., Macris, M., Cross, K. J., et al. (2001). Kappacin, a novel antibacterial peptide from bovine milk. Antimicrob. Agents Chemother. 45, 2309–2315. doi: 10.1128/AAC.45.8.2309-2315.2001
Manconi, M., Manca, M. L., Caddeo, C., Cencetti, C., Di Meo, C., Zoratto, N., et al. (2018). Preparation of gellan-cholesterol nanohydrogels embedding baicalin and evaluation of their wound healing activity. Eur. J. Pharm. Biopharm. 127, 244–249. doi: 10.1016/j.ejpb.2018.02.015
Marimuthu, S. K., Nagarajan, K., Perumal, S. K., Palanisamy, S., and Subbiah, L. (2020). Insilico alpha-helical structural recognition of temporin antimicrobial peptides and its interactions with Middle East respiratory syndrome-coronavirus. Int. J. Pept. Res. Ther. 26, 1473–1483. doi: 10.1007/s10989-019-09951-y
Martin-Serrano, Á., Gómez, R., Ortega, P., and De La Mata, F. J. (2019). Nanosystems as vehicles for the delivery of antimicrobial peptides (AMPs). Pharmaceutics 11:448. doi: 10.3390/pharmaceutics11090448
Matsuzaki, K., Murase, O., Fujii, N., and Miyajima, K. (1996). An antimicrobial peptide, magainin 2, induced rapid flip-flop of phospholipids coupled with pore formation and peptide translocation. Biochemistry 35, 11361–11368. doi: 10.1021/bi960016v
Mays, Z.J.S. (2020). Engineering Microbes for the Treatment of Phenylketonuria. dissertation/master’s thesis. Tufts University.
Mi, G., Shi, D., Wang, M., and Webster, T. J. (2018). Reducing bacterial infections and biofilm formation using nanoparticles and nanostructured antibacterial surfaces. Adv. Healthc. Mater. 7:1800103. doi: 10.1002/adhm.201800103
Mohanty, S., Jena, P., Mehta, R., Pati, R., Banerjee, B., Patil, S., et al. (2013). Cationic antimicrobial peptides and biogenic silver nanoparticles kill mycobacteria without eliciting DNA damage and cytotoxicity in mouse macrophages. Antimicrob. Agents Chemother. 57, 3688–3698. doi: 10.1128/AAC.02475-12
Moretta, A., Scieuzo, C., Petrone, A. M., Salvia, R., Manniello, M. D., Franco, A., et al. (2021). Antimicrobial peptides: a new hope in biomedical and pharmaceutical fields. Front. Cell. Infect. Microbiol. 11:668632. doi: 10.3389/fcimb.2021.668632
Mustafa, S., Balkhy, H., and Gabere, M. N. (2018). Current treatment options and the role of peptides as potential therapeutic components for Middle East respiratory syndrome (MERS): a review. J. Infect. Public Health 11, 9–17. doi: 10.1016/j.jiph.2017.08.009
Nguyen, L. T., Haney, E. F., and Vogel, H. J. (2011). The expanding scope of antimicrobial peptide structures and their modes of action. Trends Biotechnol. 29, 464–472. doi: 10.1016/j.tibtech.2011.05.001
Niu, A., Han, Y., Wu, J., Yu, N., and Xu, Q. (2010). Synthesis of one-dimensional carbon nanomaterials wrapped by silver nanoparticles and their antibacterial behavior. J. Phys. Chem. C 114, 12728–12735. doi: 10.1021/jp104720w
Noga, E. J., and Silphaduang, U. J. D. N. P. (2003). Piscidins: a novel family of peptide antibiotics from fish. Drug News Perspect. 16, 87–92. doi: 10.1358/dnp.2003.16.2.829325
Park, J.-E., and Gallagher, T. (2017). Lipidation increases antiviral activities of coronavirus fusion-inhibiting peptides. Virology 511, 9–18. doi: 10.1016/j.virol.2017.07.033
Patrzykat, A., Friedrich, C. L., Zhang, L., Mendoza, V., and Hancock, R. E. (2002). Sublethal concentrations of pleurocidin-derived antimicrobial peptides inhibit macromolecular synthesis in Escherichia coli. Antimicrob. Agents Chemother. 46, 605–614. doi: 10.1128/AAC.46.3.605-614.2002
Pinilla, C. M. B., Lopes, N. A., and Brandelli, A. (2021). Lipid-based nanostructures for the delivery of natural antimicrobials. Molecules 26:3587. doi: 10.3390/molecules26123587
Piotrowska, U., Oledzka, E., Kamysz, W., Białek, S., and Sobczak, M. (2018). The effect of polymer microstructure on encapsulation efficiency and release kinetics of Citropin 1.1 from the poly (ε-caprolactone) microparticles. Nano 8:482. doi: 10.3390/nano8070482
Pouny, Y., Rapaport, D., Mor, A., Nicolas, P., and Shai, Y. (1992). Interaction of antimicrobial dermaseptin and its fluorescently labeled analogs with phospholipid membranes. Biochemistry 31, 12416–12423. doi: 10.1021/bi00164a017
Pukala, T. L., Brinkworth, C. S., Carver, J. A., and Bowie, J. H. J. B. (2004). Investigating the importance of the flexible hinge in caerin 1.1: solution structures and activity of two synthetically modified caerin peptides. Biochemistry 43, 937–944. doi: 10.1021/bi035760b
Rangayasami, A., Kannan, K., Murugesan, S., Radhika, D., Sadasivuni, K. K., Reddy, K. R., et al. (2021). Influence of nanotechnology to combat against COVID-19 for global health emergency: a review. Sens. Int. 2:100079. doi: 10.1016/j.sintl.2020.100079
Reinhardt, A., and Neundorf, I. (2016). Design and application of antimicrobial peptide conjugates. Int. J. Mol. Sci. 17:701. doi: 10.3390/ijms17050701
Rice, J. J., Martino, M. M., De Laporte, L., Tortelli, F., Briquez, P. S., and Hubbell, J. A. (2013). Engineering the regenerative microenvironment with biomaterials. Adv. Healthc. Mater. 2, 57–71. doi: 10.1002/adhm.201200197
Robey, R. W., Pluchino, K. M., Hall, M. D., Fojo, A. T., Bates, S. E., and Gottesman, M. M. J. N. R. C. (2018). Revisiting the role of efflux pumps in multidrug-resistant cancer. Nat. Rev. Cancer 18:452. doi: 10.1038/s41568-018-0005-8
Robinson, W. E. Jr., Mcdougall, B., Tran, D., and Selsted, M. E. J. J. O. L. B. (1998). Anti-HIV-1 activity of indolicidin, an antimicrobial peptide from neutrophils. J. Leukoc. Biol. 63, 94–100. doi: 10.1002/jlb.63.1.94
Robles-García, M. A., Rodriguez-Felix, F., Marquez-Rios, E., Aguilar, J. A., Barrera-Rodriguez, A., Aguilar, J., et al. (2016). Applications of nanotechnology in the agriculture, food, and pharmaceuticals. J. Nanosci. Nanotechnol. 16, 8188–8207. doi: 10.1166/jnn.2016.12925
Roy, V., Adams, B. L., and Bentley, W. E. (2011). Developing next generation antimicrobials by intercepting AI-2 mediated quorum sensing. Enzym. Microb. Technol. 49, 113–123. doi: 10.1016/j.enzmictec.2011.06.001
Salatin, S., Maleki Dizaj, S., and Yari Khosroushahi, A. (2015). Effect of the surface modification, size, and shape on cellular uptake of nanoparticles. Cell Biol. Int. 39, 881–890. doi: 10.1002/cbin.10459
Samad, A., Alam, M. I., and Saxena, K. (2009). Dendrimers: a class of polymers in the nanotechnology for the delivery of active pharmaceuticals. Curr. Pharm. Des. 15, 2958–2969. doi: 10.2174/138161209789058200
Sani, M.-A., and Separovic, F. J. (2016). How membrane-active peptides get into lipid membranes. Acc. Chem. Res. 49, 1130–1138. doi: 10.1021/acs.accounts.6b00074
Schäfer, A.-B., and Wenzel, M. (2020). A how-to guide for mode of action analysis of antimicrobial peptides. Front. Cell. Infect. Microbiol. 10:540898. doi: 10.3389/fcimb.2020.540898
Schittek, B., Hipfel, R., Sauer, B., Bauer, J., Kalbacher, H., Stevanovic, S., et al. (2001). Dermcidin: a novel human antibiotic peptide secreted by sweat glands. Nat. Immunol. 2, 1133–1137. doi: 10.1038/ni732
Silva, N. C., Sarmento, B., and Pintado, M. (2013). The importance of antimicrobial peptides and their potential for therapeutic use in ophthalmology. Int. J. Antimicrob. Agents 41, 5–10. doi: 10.1016/j.ijantimicag.2012.07.020
Soppimath, K. S., Aminabhavi, T. M., Kulkarni, A. R., and Rudzinski, W. E. (2001). Biodegradable polymeric nanoparticles as drug delivery devices. J. Control. Release 70, 1–20. doi: 10.1016/S0168-3659(00)00339-4
Souza, P. F., Lopes, F. E., Amaral, J. L., Freitas, C. D., and Oliveira, J. T. (2020). A molecular docking study revealed that synthetic peptides induced conformational changes in the structure of SARS-CoV-2 spike glycoprotein, disrupting the interaction with human ACE2 receptor. Int. J. Biol. Macromol. 164, 66–76. doi: 10.1016/j.ijbiomac.2020.07.174
Strøm, M. B., Haug, B. E., Skar, M. L., Stensen, W., Stiberg, T., and Svendsen, J. S. (2003). The pharmacophore of short cationic antibacterial peptides. J. Med. Chem. 46, 1567–1570. doi: 10.1021/jm0340039
Subbiah, T., Bhat, G. S., Tock, R. W., Parameswaran, S., and Ramkumar, S. S. (2005). Electrospinning of nanofibers. J. Appl. Polym. Sci. 96, 557–569. doi: 10.1002/app.21481
Sun, Q., Wang, K., She, R., Ma, W., Peng, F., and Jin, H. (2010). Swine intestine antimicrobial peptides inhibit infectious bronchitis virus infectivity in chick embryos. Poult. Sci. 89, 464–469. doi: 10.3382/ps.2009-00461
Swaminathan, J., and Ehrhardt, C. (2012). Liposomal delivery of proteins and peptides. Expert Opin. Drug Deliv. 9, 1489–1503. doi: 10.1517/17425247.2012.735658
Sztukowska, M. N., Roky, M., and Demuth, D. R. (2019). Peptide and non-peptide mimetics as potential therapeutics targeting oral bacteria and oral biofilms. Mol Oral Microbiol 34, 169–182. doi: 10.1111/omi.12267
Tan, P., Fu, H., and Ma, X. J. N. T. (2021). Design, optimization, and nanotechnology of antimicrobial peptides: from exploration to applications. Nano Today 39:101229. doi: 10.1016/j.nantod.2021.101229
Tang, Z., Ma, Q., Chen, X., Chen, T., Ying, Y., Xi, X., et al. (2021). Recent advances and challenges in nanodelivery systems for antimicrobial peptides (AMPs). Antibiotics 10:990. doi: 10.3390/antibiotics10080990
Tang, C., Miller, A. F., and Saiani, A. (2014). Peptide hydrogels as mucoadhesives for local drug delivery. Int. J. Pharm. 465, 427–435. doi: 10.1016/j.ijpharm.2014.02.039
Teng, Q.-X., Luo, X., Lei, Z.-N., Wang, J.-Q., Wurpel, J., Qin, Z., et al. (2020). The multidrug resistance-reversing activity of a novel antimicrobial peptide. Cancer 12:1963. doi: 10.3390/cancers12071963
Thaker, H. D., Sgolastra, F., Clements, D., Scott, R. W., and Tew, G. N. (2011). Synthetic mimics of antimicrobial peptides from triaryl scaffolds. J. Med. Chem. 54, 2241–2254. doi: 10.1021/jm101410t
Thapa, R. K., Diep, D. B., and Tønnesen, H. H. (2020). Topical antimicrobial peptide formulations for wound healing: current developments and future prospects. Acta Biomater. 103, 52–67. doi: 10.1016/j.actbio.2019.12.025
Thassu, D., Pathak, Y., and Deleers, M. (2007). Nanoparticulate Drug-Delivery Systems: An Overview. United States: CRC Press.
Tresnak, D. T., and Hackel, B. J. J. A. (2020). Mining and statistical modeling of natural and variant class IIa Bacteriocins elucidate activity and selectivity profiles across species. Appl. Environ. Microbiol. 86, e01646–e01620. doi: 10.1128/AEM.01646-20
Tripathi, S., Tecle, T., Verma, A., Crouch, E., White, M., and Hartshorn, K. L. J. T. J. O. G. V. (2013). The human cathelicidin LL-37 inhibits influenza A viruses through a mechanism distinct from that of surfactant protein D or defensins. J. Gen. Virol. 94, 40–49. doi: 10.1099/vir.0.045013-0
Tuttobene, M., Pérez, J., Pavesi, E., Perez Mora, B., Biancotti, D., Cribb, P., et al. (2021). Light modulates important pathogenic determinants and virulence in ESKAPE pathogens Acinetobacter baumannii, Pseudomonas aeruginosa, and Staphylococcus aureus. J. Bacteriol. 203, e00566–e00620.
Van Der Strate, B., Beljaars, L., Molema, G., Harmsen, M., and Meijer, D. J. (2001). Antiviral activities of lactoferrin. Antivir. Res. 52, 225–239. doi: 10.1016/S0166-3542(01)00195-4
Vauthier, C., and Bouchemal, K. (2009). Methods for the preparation and manufacture of polymeric nanoparticles. Pharm. Res. 26, 1025–1058. doi: 10.1007/s11095-008-9800-3
Veitch, Z. W. N. (2007). The genomic response of MCF-7 breast cancer cells in the selection of resistance to taxane and anthracycline chemotherapeutics. Thesis. Ottawa, Canada: Library and Archives Canada.
Vijayan, A., James, P. P., Nanditha, C., and Kumar, G. V. (2019). Multiple cargo deliveries of growth factors and antimicrobial peptide using biodegradable nanopolymer as a potential wound healing system. Int. J. Nanomedicine 14, 2253–2263. doi: 10.2147/IJN.S190321
Vorland, L. H. J. A. (1999). Lactoferrin: a multifunctional glycoprotein. APMIS 107, 971–981. doi: 10.1111/j.1699-0463.1999.tb01499.x
Wang, G., Li, X., and Wang, Z. J. (2016). APD3: the antimicrobial peptide database as a tool for research and education. Nucleic Acids Res. 44, D1087–D1093. doi: 10.1093/nar/gkv1278
Weaver, E., Uddin, S., Cole, D. K., Hooker, A., and Lamprou, D. A. (2021). The present and future role of microfluidics for protein and peptide-based therapeutics and diagnostics. Appl. Sci. 11:4109. doi: 10.3390/app11094109
Williams, R. L., Lim, S. B., Onyuksel, H., and Marucha, P. T. J. I. J. O. P. R. (2012). Sterically stabilized phospholipid micelles reduce activity of a candidate antimicrobial wound healing adjunct. Int. J. Pept. Res. Ther. 18, 195–203. doi: 10.1007/s10989-012-9292-1
Wohlford-Lenane, C. L., Meyerholz, D. K., Perlman, S., Zhou, H., Tran, D., Selsted, M. E., et al. (2009). Rhesus theta-defensin prevents death in a mouse model of severe acute respiratory syndrome coronavirus pulmonary disease. J. Virol. 83, 11385–11390. doi: 10.1128/JVI.01363-09
Wong, X. Y., Sena-Torralba, A., Alvarez-Diduk, R., Muthoosamy, K., and Merkoçi, A. (2020). Nanomaterials for nanotheranostics: tuning their properties according to disease needs. ACS Nano 14, 2585–2627. doi: 10.1021/acsnano.9b08133
World Health Organization (2001). WHO Global Strategy for Containment of Antimicrobial Resistance. United States: World Health Organization.
Wu, M., and Hancock, R. E. (1999). Interaction of the cyclic antimicrobial cationic peptide bactenecin with the outer and cytoplasmic membrane. J. Biol. Chem. 274, 29–35. doi: 10.1074/jbc.274.1.29
Xia, S., Liu, M., Wang, C., Xu, W., Lan, Q., Feng, S., et al. (2020). Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 30, 343–355. doi: 10.1038/s41422-020-0305-x
Xia, L.-W., Xie, R., Ju, X.-J., Wang, W., Chen, Q., and Chu, L.-Y. (2013). Nano-structured smart hydrogels with rapid response and high elasticity. Nat. Commun. 4, 1–11. doi: 10.1038/ncomms3226
Xu, F., Meng, K., Wang, Y.-R., Luo, H.-Y., Yang, P.-L., Wu, N.-F., et al. (2008). Eukaryotic expression and antimicrobial spectrum determination of the peptide tachyplesin II. Protein Expr. Purif. 58, 175–183. doi: 10.1016/j.pep.2007.12.007
Yan, Y., Shin, W. I., Pang, Y. X., Meng, Y., Lai, J., You, C., et al. (2020). The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: recent advances, prevention. Int. J. Environ. Res. Public Health 17:2323. doi: 10.3390/ijerph17072323
Yang, L., Harroun, T. A., Weiss, T. M., Ding, L., and Huang, H. W. (2001). Barrel-stave model or toroidal model? A case study on melittin pores. Biophys. J. 81, 1475–1485. doi: 10.1016/S0006-3495(01)75802-X
Yasin, B., Wang, W., Pang, M., Cheshenko, N., Hong, T., Waring, A. J., et al. (2004). Theta defensins protect cells from infection by herpes simplex virus by inhibiting viral adhesion and entry. J. Virol. 78, 5147–5156. doi: 10.1128/JVI.78.10.5147-5156.2004
Yu, J., Cheng, L., Jia, A., Han, X., Xu, H., and Jiang, J. (2022). Injectable methylcellulose and hyaluronic acid hydrogel containing silver nanoparticles for their effective anti-microbial and wound healing activity after fracture surgery. J. Polymers Environ. 30, 1330–1343.
Yu, Q., Deng, T., Lin, F.-C., Zhang, B., and Zink, J. I. (2020). Supramolecular assemblies of heterogeneous mesoporous silica nanoparticles to co-deliver antimicrobial peptides and antibiotics for synergistic eradication of pathogenic biofilms. ACS Nano 14, 5926–5937. doi: 10.1021/acsnano.0c01336
Zaman, G., Flens, M., Van Leusden, M., De Haas, M., Mülder, H., Lankelma, J., et al. (1994). The human multidrug resistance-associated protein MRP is a plasma membrane drug-efflux pump. Proc. Natl. Acad. Sci. 91, 8822–8826. doi: 10.1073/pnas.91.19.8822
Zapata, W., Aguilar-Jiménez, W., Feng, Z., Weinberg, A., Russo, A., Potenza, N., et al. (2016). Identification of innate immune antiretroviral factors during in vivo and in vitro exposure to HIV-1. Microbes Infect. 18, 211–219. doi: 10.1016/j.micinf.2015.10.009
Zhang, X., Zhao, L., Zhai, G., Ji, J., and Liu, A. (2019). Multifunctional polyethylene glycol (PEG)-poly (lactic-co-glycolic acid)(PLGA)-based nanoparticles loading doxorubicin and tetrahydrocurcumin for combined chemoradiotherapy of glioma. Med. Sci. Monit. 25:9737. doi: 10.12659/MSM.918899
Zhen, J.-B., Kang, P.-W., Zhao, M.-H., and Yang, K.-W. (2019). Silver nanoparticle conjugated star PCL-b-AMPs copolymer as nanocomposite exhibits efficient antibacterial properties. Bioconjug. Chem. 31, 51–63. doi: 10.1021/acs.bioconjchem.9b00739
Keywords: antimicrobial peptides, multidrug resistance, nanoparticles, polymer, peptide
Citation: Maleki Dizaj S, Salatin S, Khezri K, Lee J-Y and Lotfipour F (2022) Targeting Multidrug Resistance With Antimicrobial Peptide-Decorated Nanoparticles and Polymers. Front. Microbiol. 13:831655. doi: 10.3389/fmicb.2022.831655
Edited by:
Alexey S. Vasilchenko, Tyumen State University, RussiaReviewed by:
Wenyi Li, The University of Melbourne, AustraliaMarc-Antoine Sani, The University of Melbourne, Australia
Giuseppe Maccari, The Pirbright Institute, United Kingdom
Copyright © 2022 Maleki Dizaj, Salatin, Khezri, Lee and Lotfipour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jyh-Yeuan Lee, anloLXlldWFuLmxlZUB1b3R0YXdhLmNh; Farzaneh Lotfipour, bG90Zmlwb29yQHRiem1lZC5hYy5pcg==
 Solmaz Maleki Dizaj1,2
Solmaz Maleki Dizaj1,2 Sara Salatin
Sara Salatin Jyh-Yeuan Lee
Jyh-Yeuan Lee Farzaneh Lotfipour
Farzaneh Lotfipour