
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Med. Technol. , 09 June 2023
Sec. Medtech Data Analytics
Volume 5 - 2023 | https://doi.org/10.3389/fmedt.2023.1206969
This article is part of the Research Topic Artificial Intelligence: Applications in Clinical Medicine View all 5 articles
Editorial on the Research Topic
Artificial intelligence: applications in clinical medicine
Exciting opportunities abound for exploring the potential of artificial intelligence (AI) technologies in medicine. The interest in AI has grown substantially across all industries, including healthcare, in part owing to the advent of popular and highly publicized AI technologies. For instance, the emergence of ChatGPT has enabled rapid access to knowledge and information in a highly digestible format (despite its tendency to generate nonsensical responses) (1). The rise of these new technologies has created a lot of enthusiasm and anticipation about the potential of AI to revolutionize healthcare by functioning as an unbiased observer capable of efficiently processing large, intricate datasets. This eagerness can sometimes overshadow practical considerations for the translation of AI from development into clinical implementation. While it is tempting to apply AI to every clinical problem, it should be noted that not every problem can be solved more efficiently with AI technologies. In comparison to ChatGPT, which has already provided users with a series of useful “productivity hacks”, medical AI technologies have not yet delivered on their promises to transform healthcare. This has led to a growing viewpoint that these technologies are in a “trough of disillusionment”—initial excitement and expectations have not yet been met, giving way to increasing skepticism.
To move from the “trough of disillusionment” to the “plateau of productivity” in medical AI technology (Figure 1), it is important to address practical considerations for development and implementation before investing in multicenter clinical trials. This requires a broader set of tools to understand the suitability of technologies for clinical trials and identify barriers to adoption. Implementation science frameworks, such as the Consolidated Framework for Implementation Research (CFIR), can promote the adoption of evidence-based practices and consider additional context beyond the intervention's effectiveness (2–4). Transdisciplinary teams are essential to realizing the potential of medical AI technologies, as not all computer science experts are implementation scientists or clinicians.
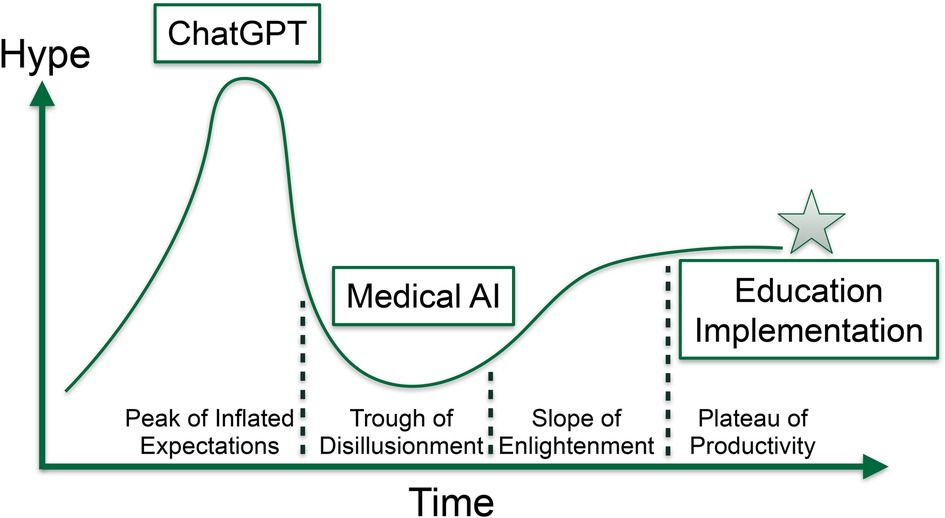
Figure 1. Illustration of the hype curve for emerging medical AI technologies, demonstrating the importance of implementation, education, and training in progressing from the trough of disillusionment to the plateau of productivity.
The development of AI technologies can lead to bias if not approached with a blend of perspectives, values, experiences, and viewpoints. This bias can result in algorithmic behavior that negatively impacts historically underserved groups and can lead to higher under-diagnosis and misdiagnosis rates in these populations. For example, skin cancer image prediction algorithms have been found to be less accurate for underprivileged demographics (5). As AI algorithms become more widely used in clinical care, it is crucial to broaden participation in their development to be more representative of varied populations.
Previous research has shown that highly diverse research groups outperform homogenous groups (6), making it essential to involve practitioners and participants from underserved populations in AI development. Remote learning frameworks present an opportunity to expose students from underrepresented groups to AI research and STEM career pathways where transportation and access to opportunities is limited. Still, there is a need to develop a deeper understanding of the instructional, curricular, and infrastructure adaptations required to successfully implement fully remote research experiences for students of underserved backgrounds (7, 8). This includes providing access to mentors as role models to help them find and leverage resources that can advance career prospects.
We requested articles that adhered to implementation and educational principles for designing, validating, and implementing emerging medical AI technologies. The articles featured include two reviews, an education curriculum design article, and an original research article that broadly covers advances in orthopedics, drug delivery and design, radiology, and margin assessment.
Farhadi et al. summarized current advances and applications of machine learning algorithms across five key orthopedic disciplines, namely, joint reconstruction, spine, orthopedic oncology, trauma, and sports medicine. They noted the lack of adoption of these technologies for clinical use and suggested metrics such as reduction in interpretation time, lower misinterpretation rates, patient outcomes, and complications to communicate the scope and impact of these technologies. The authors also highlighted the importance of utilizing interpretable models capable of recapitulating diagnostic uncertainty and exploring procedures for facilitating rapid data acquisition across multiple institutional partners.
Kaushik et al. explored areas where AI technologies could be used to facilitate treatment planning for cancer patients by mining genomics data to measure and optimize material properties of the therapeutic and selecting optimal therapies based on interactions with the immune system (Das and Chandra). Reinforcement learning, a machine learning approach that operates on feedback from the environment or system of interaction given the selection of a potential solution (i.e., drug design and delivery space), was discussed as a potential tool to predict a sequence of future actions to take based on the patient's state and expected rewards. While there are only sparse applications of reinforcement learning in the biomedical space, real-time feedback on drug discovery/delivery is one domain where these algorithms are being applied for future pharmacogenomic research.
Chen et al. explored the application of machine learning methods to a radiomics-based margin assessment of fluorescence-based paired-agent imaging. Paired-agent images improve the discrimination of tumors based on EGFR targets by the presurgical administration of ABY-029, offering significant advantages beyond standard histological assessment. Complementing improved imaging modalities with image analysis workflows can improve the accuracy, efficiency, and completeness of real-time intraoperative tumor margin assessment. Technologies that enhance the efficiency of the surgical pathology workflow have high likelihood for adoption.
Medical students and residents are entering a rapidly changing healthcare landscape where technology and data will play a crucial role. It will be essential for practicing professionals to gain familiarity with machine learning tools and how to operate them. Having a quantitative skillset paired with clinical domain expertise is crucial for developing technologies germane to work in the clinic. Lindqwister et al. epitomized these aspirations through a longitudinal education curriculum for radiology residents and demonstrated high satisfaction and perceived understanding of AI concepts from a 7-month course and workshop offerings. Considering how AI and medical informatics can be seamlessly integrated into the medical student/resident curriculum is an ongoing debate as trainees are highly pressed for time with competing demands.
In summary, addressing practical considerations for medical AI technology development and implementation, involving diverse perspectives in the development process, and providing access to mentorship and resources for students from underserved backgrounds are crucial steps to move towards the “plateau of productivity” and realize the potential of medical AI technology.
Beyond Hype: The Key Role of Implementation and Education in Realizing the Promise of Emerging Medical AI Technologies. Disclosure: During the preparation of this work the authors applied large language models to perform minor edits to originally drafted content to improve readability and language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
All authors participated in drafting and editing the manuscript. All authors contributed to the article and approved the submitted version.
JL is supported by NIH subawards P20GM104416 and P20GM130454. LV is supported by NIH award K08CA267096.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kung TH, Cheatham M, Medenilla A, Sillos C, De Leon L, Elepaño C, et al. Performance of ChatGPT on USMLE: potential for AI-assisted medical education using large language models. PLoS Digit Health. (2023) 2:e0000198. doi: 10.1371/journal.pdig.0000198
2. Li RC, Asch SM, Shah NH. Developing a delivery science for artificial intelligence in healthcare. NPJ Digit Med. (2020) 3:1–3. doi: 10.1038/s41746-019-0211-0
3. Fujimori R, Liu K, Soeno S, Naraba H, Ogura K, Hara K, et al. Acceptance, barriers, and facilitators to implementing artificial intelligence–based decision support systems in emergency departments: quantitative and qualitative evaluation. JMIR Form Res. (2022) 6:e36501. doi: 10.2196/36501
4. Car J, Sheikh A, Wicks P, Williams M. Beyond the hype of big data and artificial intelligence: building foundations for knowledge and wisdom. BMC Med. (2019) 17:143. doi: 10.1186/s12916-019-1382-x
5. Daneshjou R, Vodrahalli K, Novoa RA, Jenkins M, Liang W, Rotemberg V, et al. Disparities in dermatology AI performance on a diverse, curated clinical image set. Sci Adv. (2022) 8:eabq6147. doi: 10.1126/sciadv.abq6147
6. Smith-Doerr L, Alegria SN, Sacco T. How diversity matters in the US science and engineering workforce: a critical review considering integration in teams, fields, and organizational contexts. Engag Sci Technol Soc. (2017) 3:139–53. doi: 10.17351/ests2017.142
7. Morgan H. Best practices for implementing remote learning during a pandemic. Clear House J Educ Strateg Issues Ideas. (2020) 93:135–41. doi: 10.1080/00098655.2020.1751480
Keywords: implementation, education, machine learning, medicine, artificial intelligence, stakeholder
Citation: Levy J, Madrigal E and Vaickus L (2023) Editorial: Artificial intelligence: applications in clinical medicine. Front. Med. Technol. 5:1206969. doi: 10.3389/fmedt.2023.1206969
Received: 16 April 2023; Accepted: 22 May 2023;
Published: 9 June 2023.
Edited by:
Alicia Jennifer El Haj, University of Birmingham, United Kingdom© 2023 Levy, Madrigal and Vaickus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joshua Levy am9zaHVhLmoubGV2eUBkYXJ0bW91dGguZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.