
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. Technol. , 28 April 2023
Sec. Regenerative Technologies
Volume 5 - 2023 | https://doi.org/10.3389/fmedt.2023.1198612
This case report discusses an elderly male patient (86 years old), suffering from limb pain related to ulcers in the lower limbs resulting from peripheral arterial disease (PAD). Clinically evaluated with the aid of infrared thermal imaging before, during and after treatment, he was submitted to treatment with neuromodulation protocols with REAC Technology, Neuro Postural Optimization (NPO) and Neuropsychophysical Optimization (NPPO) in association with traditional treatments for PAD. It was followed clinically with the aid of infrared thermal imaging of the lower limbs before, during and after treatment. He had a clinical result with a significant reduction in pain and infrared thermal images with complete revascularization of both feet. Evidencing that the treatment of dysfunctional adaptive responses by managing psychological factors often associated with anxiety, depression and stress performed by the REAC NPO and NPPO protocols can be a useful intervention to improve symptoms of patients with lower limb pain and circulatory disturbances.
Peripheral arterial disease (PAD) is a common disorder that affects the blood vessels in the lower limbs, causing reduced blood flow to the muscles and tissues. Vasospasm (1), a sudden constriction of the blood vessels, is a potential complication of PAD that can exacerbate symptoms and increase the risk of tissue damage and limb loss. While the pathophysiology of vasospasm is not fully understood, recent research suggests that psychological factors, such as depression, anxiety and stress, may play a role in its development (2, 3).
Anxiety and stress are known to activate the sympathetic nervous system, which regulates blood vessel tone and can cause vasoconstriction (4, 5). In individuals with PAD, this may lead to an increased risk of vasospasm and worsened symptoms (1).
Understanding the link between depression, anxiety and stress and vasospasm in PAD has important implications for the management of this condition (6). If depression, anxiety and stress are found to be significant risk factors for vasospasm (7), interventions targeting these factors may be a useful adjunct to traditional treatments for PAD, such as medication and lifestyle modifications.
In the present study, we report a case where Radio Electric Asymmetric Conveyer (REAC) technology was used to administer two treatments—Neuro Postural (NPO) and Neuro Psycho Physical Optimization (NPPO)—aimed at improving adaptive response, and consequently, mitigating depression, anxiety, and stress. The effectiveness of these treatments was evaluated in a patient with peripheral vasospasm of the lower limbs, a condition that had persisted for approximately four years.
The results demonstrated the effectiveness of NPO and NPPO in improving peripheral vasospasm of the lower limbs.
This case report presents the clinical findings of an 86-year-old male. Written informed consent was obtained from the patient.
The patient presented to our observation with chronic pain in bilateral wounds located in the medial perimalleolar region, which had not responded to previous wound dressings. The patient's pain was initially assessed using a 0–10 visual analog scale, and the reported pain level was between 8 and 9.
The patient reported two previous operations: cardiac pacemaker implantation in 2014 for heart rhythm disturbances and coronary stent implantation surgery in 2016.
During the initial assessment, we aimed to analyze the vascular perfusion in the perimalleolar area. To accomplish this, we employed a FLIR thermal imaging camera with a sensitivity range set between 27 and 37 degrees Celsius. The image obtained from the diagnostic examination revealed a distinctive and concerning circulatory amputation pattern, which appeared to originate from the lower third of the legs (see Figure 1).

Figure 1. The thermal image obtained during the first visit shows the state of vasospasm in the lower third of the legs and feet, which results in a lack of thermal visualization of the affected areas.
This visual representation highlights the severity and complexity of the circulatory issue, which may potentially lead to further complications if left untreated.
In order to improve the thermal imaging camera analysis and the patient's symptomatic picture, a single REAC NPO treatment session was administered. This treatment produced an immediate and sustained response, resulting in the resolution of functional dysmetria and the initiation of a cascade of neurovegetative events that could contribute to the amelioration of vasospasm (Figure 2).
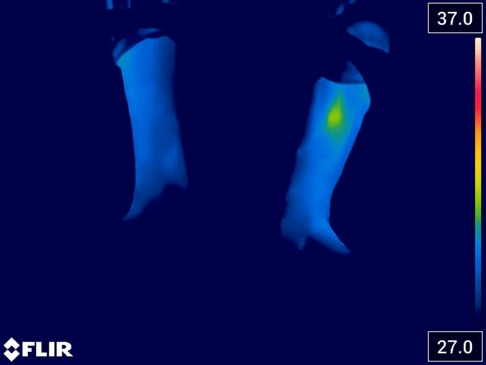
Figure 2. The thermal image acquired after the administration of REAC NPO treatment shows an initial reduction in the vasospasm state of the lower third of the legs and the left foot.
The acquisition of a thermal image immediately after administering the REAC NPO treatment indicates an initial improvement, characterized by the reappearance of vascularization in the left perimalleolar area. This finding suggests the presence of a dysfunctional component in the thermo-vascular amputation and highlights the potential of the REAC NPO treatment to stimulate the initial restoration of blood flow and tissue oxygenation, a crucial factor in wound healing.
After undergoing REAC NPO treatment, a follow-up pain assessment was conducted, which revealed an improvement from the initial score of 8–9 to a score of 7, which was recorded.
One week after undergoing the REAC NPO treatment, the patient underwent a follow-up check-up and a new thermal imaging was acquired, demonstrating further improvement compared to the initial images (Figure 3).

Figure 3. Thermal image acquired one week after administration of REAC NPO treatment. The image highlights a further improvement of the bilateral vasospasm in the two limbs.
In addition, pain assessment was conducted during the follow-up, and it was observed that the pain score had improved from 7 to 5–6.
After observing the positive outcomes resulting from the initial neurovegetative modulation induced by the REAC NPO treatment, we recommended that the patient continue with the NPPO treatment. The NPPO treatment is specifically designed to enhance mood and alleviate behavioral disorders including depression, anxiety, and stress related disorders.
The REAC NPPO is a neurobiological modulation treatment aimed at improving the ability to respond to environmental interaction from a neurological, psychological, and physical point of view (8–12). Each treatment cycle consists of 18 sessions, to be administered from one to a maximum of four sessions per day. Each treatment session lasts approximately three seconds. In this scenario, the patient underwent two weekly treatments of REAC NPPO spaced one hour apart.
The REAC treatment parameters are predetermined by the manufacturer and cannot be altered by the operator. To administer REAC treatments, a BENE 110 device (ASMED, Florence, Italy), was used.
After completing 18 sessions of REAC NPPO, the patient underwent a follow-up assessment the following week. Thermal imaging was performed and revealed complete revascularization of both feet (Figure 4).

Figure 4. Thermal image acquired the week after the end of 18 sessions of REAC NPPO, which reveals complete revascularization of both feet.
In the final follow-up, a new evaluation of the patient's perceived pain was conducted, revealing that while the pain had not completely disappeared, it was rated between 1 and 2 on the evaluation scale.
There is a growing body of scientific evidence indicating that depression, anxiety, and stress can contribute to the development and exacerbation of vasospasm and pain (2, 13). Vasospasm is a condition characterized by the sudden constriction of blood vessels, which can cause reduced blood flow to vital organs and tissues. Pain is often associated with vasospasm, as the reduced blood flow can cause tissue damage and inflammation (14, 15).
Depression, anxiety, and stress are known to increase the levels of stress hormones such as cortisol, which can promote inflammation and blood vessel constriction (16). These changes can lead to the development of vasospasm and pain (17). Additionally, depression and anxiety are associated with alterations in pain perception and processing in the brain, which can lead to increased pain sensitivity and intensity (18, 19).
Also, stress can trigger vasospasm and increase pain sensitivity through a variety of mechanisms, including activation of the sympathetic nervous system and release of pro-inflammatory cytokines.
In summary, depression, anxiety, and stress can contribute to the development and exacerbation of vasospasm and pain through various mechanisms.
Drawing on these considerations, it is possible to appreciate how the REAC NPO and NPPO neuromodulation treatments, which target dysfunctional adaptive responses frequently associated with depression, anxiety, and stress, have demonstrated efficacy in reducing vasospasm and restoring distal circulation in the lower extremities.
After analyzing the obtained results, it can be concluded that the patient's chances of maintaining restoration of distal circulation in the lower limbs are positive, particularly if the patient continues to manage depression, anxiety, and stress on a regular basis. Additionally, the patient may benefit from REAC neuromodulation treatments in their management of these psychological factors.
In conclusion, the lack of improvement in pain and distal circulation of the lower limbs with conventional physiotherapy treatments underscores the importance of addressing the neurovegetative dysfunctional component related to depression, anxiety and stress in patients. Current scientific evidence supports the use of neuromodulation treatments, such as REAC NPO and NPPO, as useful interventions for improving such symptomatology in patients with lower limb pain and circulatory disturbances.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
The author confirms being the sole contributor of this work and has approved it for publication.
Open access funding provided by the International Scientific Society of Neuro Psycho Physical Optimization with REAC Technology.
I thank the scientific team of the Rinaldi Fontani Institute and Foundation for the support received.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sasaki S, Yasuda K. Vasospastic syndrome. In: Chang JB, editors. Textbook of angiology. New York, NY: Springer New York (2000). p. 979–86.
2. Aragao JA, de Andrade LGR, Neves OMG, Aragao ICS, Aragao FMS, Reis FP. Anxiety and depression in patients with peripheral arterial disease admitted to a tertiary hospital. J Vasc Bras. (2019) 18:e20190002. doi: 10.1590/1677-5449.190002
3. Bouzinova EV, Wiborg O, Aalkjaer C, Matchkov VV. Role of peripheral vascular resistance for the association between Major depression and cardiovascular disease. J Cardiovasc Pharmacol. (2015) 65(4):299–307. doi: 10.1097/FJC.0000000000000187
4. Shah P, Khaleel M, Thuptimdang W, Sunwoo J, Veluswamy S, Chalacheva P, et al. Mental stress causes vasoconstriction in subjects with sickle cell disease and in normal controls. Haematologica. (2020) 105(1):83–90. doi: 10.3324/haematol.2018.211391
5. Ayada C, Toru Ü, Korkut Y. The relationship of stress and blood pressure effectors. Hippokratia. (2015) 19(2):99–108. PMCID: PMC4938117; PMID: 27418756.27418756
6. Ercan S, Unal A, Altunbas G, Kaya H, Davutoglu V, Yuce M, et al. Anxiety score as a risk factor for radial artery vasospasm during radial interventions: a pilot study. Angiology. (2014) 65(1):67–70. doi: 10.1177/0003319713488931
7. Kim JH, Almuwaqqat Z, Hammadah M, Liu C, Ko YA, Lima B, et al. Peripheral vasoconstriction during mental stress and adverse cardiovascular outcomes in patients with coronary artery disease. Circ Res. (2019) 125(10):874–83. doi: 10.1161/CIRCRESAHA.119.315005
8. Rinaldi S, Fontani V, Aravagli L, Margotti ML. Psychological and symptomatic stress-related disorders with radio-electric treatment: psychometric evaluation. Stress Health. (2010) 26(5):350–8. doi: 10.1002/smi.1298
9. Rinaldi S, Fontani V, Aravagli L, Mannu P, Castagna A, Margotti ML, et al. Stress-Related psycho-physiological disorders: randomized single blind placebo controlled naturalistic study of psychometric evaluation using a radio electric asymmetric treatment. Health Qual Life Outcomes. (2011) 9:54. doi: 10.1186/1477-7525-9-54
10. Rinaldi A, Rinaldi C, Coelho Pereira JA, Lotti Margotti M, Bittencourt MN, Barcessat ARP, et al. Radio electric asymmetric conveyer neuromodulation in depression, anxiety, and stress. Neuropsychiatr Dis Treat. (2019) 15:469–80. doi: 10.2147/NDT.S195466
11. Pinheiro Barcessat AR, Nolli Bittencourt M, Duarte Ferreira L, de Souza Neri E, Coelho Pereira JA, Bechelli F, et al. Reac cervicobrachial neuromodulation treatment of depression, anxiety, and stress during the COVID-19 pandemic. Psychol Res Behav Manag. (2020) 13(13):929–37. doi: 10.2147/PRBM.S275730
12. Rinaldi A, Maioli M, Marins Martins MC, de Castro PCF, de Oliveira Silva NAP, de Mattos JAV, et al. Reac non-invasive neurobiological stimulation for mitigating the impact of internalizing disorders in autism Spectrum disorder. Advances in Neurodevelopmental Disorders. (2021) 5(4):446–56. doi: 10.1007/s41252-021-00217-7
13. Kim S, Lee J, Boone D. Protective and risk factors at the intersection of chronic pain, depression, anxiety, and somatic amplification: a latent profile approach. J Pain Res. (2022) 15:1107–21. doi: 10.2147/JPR.S340382
14. Nakabayashi K, Ando H. Hand vasospasm, mimicking acute upper limb ischaemia. BMJ Case Rep. (2020) 13(7):1. doi: 10.1136/bcr-2020-235462
15. Kuchynkova S, Chochola M, Varejka P, Kautznerova D, Prochazka P, Rucka D, et al. A rare cause of acute limb ischemia of both upper and lower limbs caused by prolonged vasospasm. Cor Vasa. (2017) 59(5):e503–6. doi: 10.1016/j.crvasa.2017.01.005
16. Yang S, Zhang L. Glucocorticoids and vascular reactivity. Curr Vasc Pharmacol. (2004) 2(1):1–12. doi: 10.2174/1570161043476483
17. Hinterdobler J, Schott S, Jin H, Meesmann A, Steinsiek AL, Zimmermann AS, et al. Acute mental stress drives vascular inflammation and promotes plaque destabilization in mouse atherosclerosis. Eur Heart J. (2021) 42(39):4077–88. doi: 10.1093/eurheartj/ehab371
18. Hermesdorf M, Berger K, Baune BT, Wellmann J, Ruscheweyh R, Wersching H. Pain sensitivity in patients with Major depression: differential effect of pain sensitivity measures, somatic cofactors, and disease characteristics. J Pain. (2016) 17(5):606–16. doi: 10.1016/j.jpain.2016.01.474
Keywords: peripheral vasospasm, depression, anxiety, stress, neuromodulation, neurostimulation, radio electric asymmetric conveyer, case report
Citation: Bechelli F (2023) Effectiveness of REAC neuro postural and neuro psycho physical optimization in improving peripheral vasospasm dysfunction: a case report. Front. Med. Technol. 5:1198612. doi: 10.3389/fmedt.2023.1198612
Received: 1 April 2023; Accepted: 10 April 2023;
Published: 28 April 2023.
Edited by:
Salvatore Rinaldi, Rinaldi Fontani Institute, ItalyReviewed by:
Alessandro Castagna,Rinaldi Fontani Institute, Italy© 2023 Bechelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabio Bechelli ZmFiaW9AaW5vdml0dGEuY29tLmJy
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.