
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. Technol. , 08 March 2022
Sec. Medtech Data Analytics
Volume 3 - 2021 | https://doi.org/10.3389/fmedt.2021.790956
This article is part of the Research Topic Highlights in Medtech Data Analytics 2021/22 View all 6 articles
Objective: To evaluate the experience of the physician of the technical success in high-intensity focused ultrasound (HIFU) ablation of uterine fibroids with a nonperfused volume ratio (NPVR) of at least 80%.
Methods: Patients from a 20-center prospective study were enrolled in this study. In this study, among the 20 clinical centers, five centers had physician with >3 years of HIFU experience, and the other 15 centers initiated HIFU therapy <3 years, were defined as the experienced group and the inexperienced group, respectively. Technical success was defined as achieving NPVR ≥ 80% of uterine fibroids with no major complications and it was defined as the successful group; otherwise, it was defined as the unsuccessful group.
Results: A total of 1,352 patients were included at the age of 41.32 ± 5.08 years. The mean NPVR (87.48 ± 14.91%) was obtained in the inexperienced group (86.50 ± 15.76%) and in the experienced group (89.21 ± 13.12%), respectively. The multivariate analysis showed that the volume of uterus, location of fibroids, and physician experience were significantly correlated with technical success (p < 0.05). In the experienced group, 82.20% of uterine fibroids obtained NPVR ≥ 80%, compared with 75.32% in the inexperienced group, and the difference was significant (p = 0.003). The technical success rate of the experienced group was 82.00% which was higher than 75.20% of the inexperienced group (p = 0.004).
Conclusion: In technical success of achieving NPVR ≥ 80%, experience of the physician was positively correlated with technical success; NPVR and major complications for the inexperienced group were comparable to those of the experienced group from a clinical perspective; inexperienced physicians could reach NPVR ≥ 80% of sufficient ablation and were trustworthy in efficacy. Smaller uterus and fibroids of anterior wall were correlated with better technical success; experienced physicians still have better technical success when choosing patients with larger uterus, contributing to clinical decision-making and patient referral.
Uterine fibroids are benign lesions or neoplasms of the uterus that can enlarge the uterus and it is estimated that 25% of the patients can develop clinical symptoms (1, 2). There are many therapeutic strategies for uterine fibroids such as hysterectomy, myomectomy, laparoscopic myomectomy, and uterine artery embolization (UAE) therapy (3, 4). However, hysterectomy and myomectomy approaches are associated with a high rate of significant complications and weeks to recover (5, 6). There are also reports of prenatal uterine rupture after laparoscopic myomectomy (7) and major complication rates in UAE were estimated that range from 1 to 17% (8, 9). Every treatment approach should consider the age of the patient, childbearing plans, and the location and size of the leiomyoma (2, 10).
In the recent years, high-intensity focused ultrasound (HIFU) has been used in noninvasive ablation of uterine fibroids, which was a uterus-preserving therapy proved to be safe and effective (11, 12). However, HIFU technology was still in its infancy and it was not commonly used (13, 14). There were some differences in operation outcomes in surgeons according to experience of the physician and the surgical learning curve with increased surgeon experience (15, 16). The degree that impacts technical success in HIFU treatment was not known. In this study, we conducted a multicenter study to compare technical success in physician with different experience, in order to provide a basis for the clinical technical training, choices of physician, patient selection, and expanded application of HIFU technology.
From March 2011 to December 2013, the patients with uterine fibroids were enrolled in 20 clinical centers in China. Data of the patient were selected from the Multicenter Research Information System of Therapy of Uterine Fibroids (www.hifuctr.com) (software copyright certificate number: 2011SR094656). This multicenter study was approved by the Chinese Ethics Committee of Registering Clinical Trials (IRB approval number: ChiECRCT-2011034). Each patient signed a written informed consent before inclusion. The results of clinical efficacy have been reported (17).
Eligibility criteria for patients (17) were as follows: (1) Premenopausal women with completed planned families (and had no recent plan for a further pregnancy), (2) Imaging-confirmed diagnosis of uterine fibroids had any of the following indications for hysterectomy: (a) enlarged uterus (uterine volume ≥10 weeks of gestation); (b) menorrhagia and/or secondary anemia; (c) pelvic pain, urinary frequency, or constipation, (3) For patients with multiple fibroids, no more than three fibroids with minimal diameters of 2 cm based on abdominal ultrasound present, (4) Fibroids clearly imaged by abdominal ultrasound, and (5) For patients with abdominal surgical scars, the width of image blurring due to acoustic attenuation had to be <10 mm.
Exclusion criteria (17) were as follows: (1) Patients with uterine adenomyosis, (2) Previous myomectomy, (3) Concurrent pregnancy, (4) Pedunculated subserous or submucosal fibroids, (5) Any single fibroid >10 cm maximum in diameter, (6) Acute pelvic inflammation or uncontrolled systemic disease, and (7) Patients were unable to communicate with physicians or were unwilling to sign a written informed consent. Patients were provided with written information describing the potential risks and benefits including the potential impact on fertility and the risk of recurrence of symptoms.
A program of HIFU treatment training and qualification certification authorized by the Ministry of Health of China were required for physicians. All the operators were required to complete ablation treatment for 40–60 patients under guidance and supervision before entering the trial, with no major complications among treated patients, and a mean nonperfused volume ratio (NPVR) of treated uterine fibroids (NPVR ≥ 70%) (18).
A single session of HIFU ablation was performed using the Model-JC/JC200 Focused Ultrasound Tumor Therapeutic System (Chongqing Haifu Medical Technology Corporation, Ltd, Chongqing, China). Equipment parameters used in this study were as follows: the frequency of the transducer was 0.8 MHz, the physical focal area was 1.5 × 1.5 × 10 mm, and the therapeutic power was 300–400 W. Standardized clinical program were used for physician training and clinical treatment. Patients placed in prone position on HIFU treatment bed and anterior abdominal wall was fully contact with degassed water. Fentanyl (0.8–1 μg/kg) and midazolam (0.02–0.03 mg/kg) were provided every 30–40 min for conscious sedation; all the patients kept awake or in light sleep with their breath and their breath, oxyhemoglobin saturation, heart rate, and blood pressure were monitored during the procedure. Monitored by real-time ultrasonography, the treatment used massive grayscale changes in the treated area as a measure of treatment effect. Adjust unit time dose according to tolerance of the patient and target grayscale changes. The sonication was terminated when the grayscale enhancement area covered the planned treatment area. Dose reference standard: total dose ≤ 150 kJ and treatment time ≤ 3 h. Post-operative patients were prone to observe 2 h.
All the patients underwent pelvic scans of MRI with 3.0 T MRI System before operation (GE Medical System, Milwaukee, Wisconsin, USA) including the T1-weighted imaging (T1WI), T2-weighted imaging (T2WI), and enhanced T1-weighted gradient-echo imaging contrast enhancement T1-weighted imaging (CE-T1WI) sequence. The three-dimensional diameters of dominant uterine fibroids and uterus were measured based on T2W images. Enhanced MR scans were performed again within 1 week after the treatment and used to measure the diameters of NPV. The fibroid volume and NPV were calculated by using the following equation: V = 0.5233 × D1 × D2 × D3 [longitudinal (D1), anteroposterior (D2), and transverse (D3)] (19). NPVR was the ratio of the volume of the nonperfusion area in the postablation to the volume of the fibroids. The signal intensity of the uterine fibroids was classified into three types according to the pretreatment T2WI: hypointense, isointense, and hyperintense (20).
Technical success was defined as the NPVR of uterine fibroid at least 80% and with no major complications. Complications were recorded and graded using the guidelines of the Society of Interventional Radiology (SIR); classes A and B were considered to be minor complication and classes C to F were considered to be major complication (21, 22).
All the statistical analyses were performed by using the SPSS software version 22.0 (SPSS, IBM Corporation, Chicago, Illinois, USA). Continuous variables that followed the normal distribution were presented as the mean ± SD and the categorical variables were described by the total number. Continuous variables were compared by the independent t-test and categorical variables were compared by the chi-squared test. Binary logistic regression analysis was utilized for multivariate analysis. p < 0.05 was considered as statistically significant.
A total of 1,352 patients were included, with the exception of one patient who was diagnosed as diffuse intravenous leiomyomatosis during follow-up. The age of the patients was 41.32 ± 5.08 years (range: 23–57 years), body mass index (BMI) was 22.68 ± 2.99 kg/m2 (range: 16–43.3 kg/m2), the volume of dominant uterine fibroids was 104.86 ± 81.76 cm3 (range: 4.12–518.07 cm3), uterine volume was 292.32 ± 148.31 cm3 (range: 39.43–1,160.47 cm3), and the mean NPVR was 87.48% (range: 0.2–100%) (Table 1 and Figure 1).
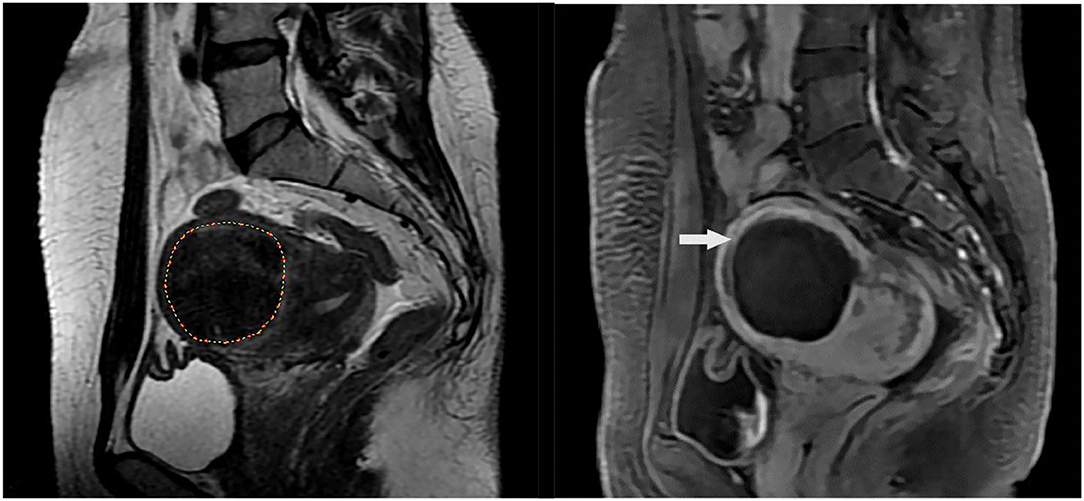
Figure 1. MR images of a 40-year-old woman with uterine fibroid. (A) T2-weighted image shows a single fibroid in the anterior wall of uterine before high-intensity focused ultrasound (HIFU) treatment; (B) Contrast-enhanced MRI shows nonperfused volume (NPV) in the uterine fibroid after HIFU treatment, NPV ratio (NPVR) was 94%. The white arrow indicates the nonperfusion volume (NPV) after treatment.
Among the 20 clinical centers, five centers had five physicians with more than 3 years of HIFU experience as the experienced group and more than 50 cases in each of the five centers; the other 15 centers have 15 physicians <3 years of HIFU as the inexperienced group and only seven centers over 50 cases. In the inexperienced group, 12 hospitals have not carried out HIFU treatment before. A total of 863 patients with fibroids were in the inexperienced group and 489 patients with fibroids were in the experienced group accordingly. The independent sample t-test or the chi-squared test was used to analyze data and we found that no significant difference in age, BMI, position of uterus, number of fibroids, and location of fibroids (p > 0.05). The maximum diameter of fibroids, uterine volume, and uterine fibroid volume of the experienced group were larger than that of the inexperienced group (p < 0.05) and there were significant differences in type of fibroids and classification of T2WI signals intensity between two groups (p < 0.05). The percentage of submucosal fibroids in the experienced group was 14.93%, which was higher than that in the inexperienced group (6.84%) (p = 0.000). There were 430 fibroids with the hyperintense of T2WI, 35.38% in the experienced group, and 29.78% in the inexperienced group, respectively (p = 0.009) (Table 2).
A total of 1,050 patients with NPVR ≥ 80% of uterine fibroids with no major complications were in the successful group, while 302 patients were in the unsuccessful group. Analysis of two groups of characteristics from experience of the patients and physicians, the independent t-test and the chi-squared test were used in the univariate analysis. The volume of uterus, location of fibroids, and physician experience were statistically significant (p < 0.05) (Table 3).
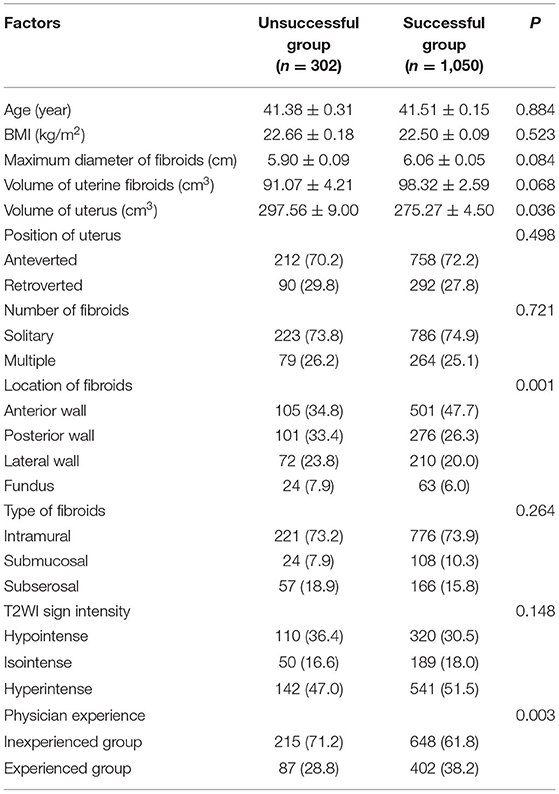
Table 3. The univariate analysis to evaluate the factors between the unsuccessful group and the successful group.
In Table 4, the multivariate logistic regression analysis showed that the volume of uterus, location of fibroids, and physician experience were significantly correlated with technical success. The volume of uterus was negatively correlated with technical success and fibroids of anterior wall and experienced physicians were positively correlated with technical success (p < 0.05).
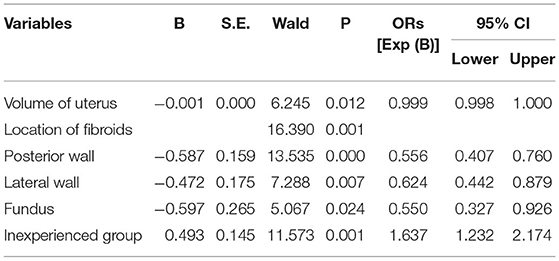
Table 4. The multivariate binary logistic regression analysis to evaluate the correlation of technical success with the significant factors of the univariate analysis.
There was no statistically significant difference in major adverse events between the inexperienced group and the experienced group (p = 1.000). NPVR was 87.48 ± 14.91% in the inexperienced group (86.50 ± 15.76%) and in the experienced group (89.21 ± 13.12%), respectively. In the experienced group, 82.20% of uterine fibroids obtained NPVR ≥ 80%, compared with 75.32% in the inexperienced group, and the difference was significant (p = 0.003). The rate of the technical success accounts for 82.00% in the experienced group higher than the rate of the technical success accounts for 75.20% in the inexperienced group (p = 0.004) (Table 5).
Following the SIR classification as shown in Table 6, a total of 1,068 (78.99%) adverse events were classified as class A and all of these adverse events recovered spontaneously in few days without any treatment. The unsuccessful group and the successful group showed significant difference with vaginal bleeding and discharge (p = 0.028); lower abdominal pain, lumbar and back (sacrum) pain, leg numbness/pain, weakness in lower limb, blurred vision, dizziness and headache, pain, and distension of anus showed no significant differences (p > 0.05). Adverse events classified as class B were 469 (34.69%); lower abdominal pain was significant difference (p = 0.000); sacrum/buttock pain, vaginal bleeding and discharge, leg numbness/pain, weakness in lower limb, fever, nausea and vomiting, hematuria, respiratory tract infection, and urinary retention were no statistical significance in the unsuccessful group and the successful group (p > 0.05). Major adverse events attributable to the intervention occurred in three (0.22%) patients during 30 days follow-up period and were classified as class C; these three patients were in the unsuccessful group and were second-degree skin burns that increased the level of care and did not lead to substantial morbidity and disability; skin burns were significant indigenous statistical difference between the unsuccessful group and the successful group (p = 0.001).
High-intensity focused ultrasound therapy is an uterine-sparing alternative that reported to be safe, effective, and highly acceptable to patients in the treatment of fibroids (11). HIFU treatment has a potential impact on improving the quality of life on patients (12). The United States Food and Drug Administration (FDA) approved the focused ultrasound therapy as entirely a noninvasive approach in treatment of symptomatic uterine fibroids in 2004. HIFU has now become the preferred therapy of fibroids in some centers in China (17, 23). As a new technology for the treatment of uterine fibroids, physician training is the key way to popularize clinical applications and benefit more patients. Understanding the impact of experience of the physicians on technical success is an essential tool to improve safety of the patient and operation training.
Nonperfused volume ratio was directly related to the long-term relief of clinical symptoms, was as large as possible, and was positively associated with symptom control that was ultimately considered as a technical parameter for treatment success in focused ultrasound (17, 24, 25). Early in the application of HIFU technology, NPVR up to 25% can achieve the purpose of clinical symptoms relief. However, it was reported that the reintervention rate was 66.7% when median NPV of 36.4% of all the fibroid tissue volume (26, 27). The regression analysis indicated that when the NPVR directly posttreatment achieved 60%, the probability of undergoing an additional treatment was 10% at a mean 2 years after HIFU treatment of uterine fibroids; the results were comparable to those of myomectomy (14, 28). Two other studies indicated that when NPVR was higher than 70%, the 2-year clinical cumulative recurrence rates after HIFU were lower when compared to myomectomy (29, 30). In earlier studies, the prediction of immediate NPV ratio of more than 60%, which was used as an outcome evaluation index for HIFU treatment of uterine fibroids; on this basis, the technical requirements for operation training were NPVR reached at 70%. Park et al. (31) reported that HIFU ablation of uterine fibroids achievement of an immediate NPVR of at least 80% was safe, with greater tumor volume shrinkage compared with cases with a lower NPVR. Recently, some scholars have set NPVR at least 80% as a measure of sufficient ablation indexes in HIFU treatment of uterine fibroids (32). In addition, some scholars investigated MRI screening parameters for predicting an NPV ratio of at least 90% (33, 34). Among the 20 centers in this study, we aimed to obtain a higher NPVR on the premise of safety, so as to improve the clinical effect of HIFU ablation of uterine fibroids. The standard for HIFU ablation of uterine fibroids was to achieve an average of NPVR ≥ 70% after training and all the centers reached this technical requirement. With the improvement of clinical protocols and more technical experience of physician, the higher NPVR may result in better patient outcomes. Therefore, NPVR ≥ 80% was selected as the technical success criteria of HIFU ablation for uterine fibroids in this study. The results of both the groups had achieved the average NPVR ≥ 80% and NPVR was higher in the experienced center group.
In this study, the major adverse events in the inexperienced group were 0.23% and the major adverse events in the experienced group were 0.20%. There was no statistical significance between the two groups. Adverse events of class A need no therapy and no consequences and adverse events of class B need nominal therapy and no consequence, but need only overnight admission for observation; adverse events of class C require therapy and minor hospitalization (<48 h) (21). The proportion of vaginal bleeding and discharge and lower abdominal pain in the successful group was higher than that in the unsuccessful group in grade class A and class B adverse events, of the three patients in the unsuccessful group, NPVR ≥ 80% in two patients and NPVR <80 % in one patient, indicating that more observation and nursing were needed when the NPVR ≥ 80%. In clinical practice, vaginal bleeding and discharge were related to the location of uterine fibroids and vaginal bleeding and discharge prone to occur in submucosal fibroids after thermal injury; when the NPVR was higher, the boundary was close to the normal tissue, and it was prone to normal tissue thermal damage and stimulation pain of submucosal and subserosal fibroids; this also explained that class B had more lower abdominal pain in the successful group than in the failed group (35, 36). The experienced group was better than the inexperienced group in NPVR, which indicated that the physicians with more experience had better understanding on controlling the boundary in HIFU ablation of uterine fibroids. All the inexperienced group and the experienced group reached NPVR ≥ 80%; the difference between the two groups was only 2.7%, means that the inexperienced group was comparable to those of the experienced group from a clinical perspective in NPVR. On one hand, it shows that HIFU technology is easy to learn and promote and inexperienced physicians can achieve sufficient ablation level. On the other hand, experienced physicians in clinical practice have provided sufficient dose, sufficient ablation level, and remission of clinical symptoms when NPVR reaches 80% and experienced physicians will not blindly improve NPVR considering the safety boundary.
In terms of HIFU ablation technology, previous studies in comparison to the lesions located at the superficial region, lesions located deeper required more energy to achieve the same volume of necrotic tissue (37, 38). HIFU ablation of uterine fibroids was affected by many factors. The signal hypointense on T2WI of uterine fibroids, large size of uterine fibroids, or anteverted uterine could be more easily ablated with high ablation efficiency (37, 39). The technical indication for HIFU ablation of uterine fibroids was that lesions can be localized by ultrasound equipped in HIFU system. However, the selection of clinical cases was still influenced by the experience of the physician and his confidence in the effectiveness of the new technology. In this study, maximum diameter of fibroids, volume of uterine fibroids, and uterine volume in the experienced group were larger; the proportion of submucosal fibroids and fibroids with T2WI hyperintense signal were also higher than that of the inexperienced group; volume of uterus was negatively correlated with technical success. The reason may be that inexperienced physicians lack technical judgment ability. On the other hand, inexperienced physicians have less confidence in HIFU technique than traditional surgery and they were more inclined to recommend traditional surgery for patients with large uterine volume. As a result, inexperienced physicians in the selection of patients were inevitably biased. It was believed that with the accumulation of experience of the physicians, more patients can be selected to receive HIFU treatment. Another notable truth was that with HIFU, most clinical reports of HIFU treatment for fibroids were from China, while many other countries were still considered limit in clinical experience; studying the influence of experience of the physicians on the outcome of HIFU treatment of uterine fibroids could increase the trust in HIFU in centers that lack of HIFU experience (13). The technical success rate of the experienced group was superior to the inexperienced group in technical success rate that also verified the hypothesis of “practice makes perfect” (40). Therefore, with the accumulation of experience, higher NPVR can be obtained on the premise of safety, so as to improve the clinical effect of HIFU ablation of uterine fibroids.
The nature of the hospitals cannot be ignored in analyzing the factors that affect the success of HIFU technology; the influence of the level and nature of the hospitals on technical success can be studied (40, 41). The level and nature of the hospitals reflect the comprehensive level and feature of the hospitals. There may also be differences in the source of patients and the expertise of physicians. Therefore, the influence of HIFU on the technical success needs further study. No study showed the effect of experience of the physicians on the long-term prognosis and reintervention of patients (14, 41). Thus, prospective studies with larger sample sizes were needed to investigate the long-term results including long-term symptom relief, the recurrence rate, and the reintervention rate.
There were some limitations in this study. A total of 20 clinical centers in China were selected, but it was not clear whether consistent results can be obtained in international multicenters. There were many differences in medical education model, medical system, and understanding of diseases of the patient, so whether training programs were applicable and whether standards for technical success were appropriate that still need to be further studied. Adverse events during long-term follow-up were not evaluated, large-scale investigation with long-term follow-up was crucial, and there was a risk of uterine rupture after HIFU treatment (42, 43).
This study has several important implications. The relationship between experience of the physician and patient outcomes was an ancient topic. However, this study proved that HIFU was safe and all the centers in this study could reach the basic requirements of NPVR ≥ 70%; when NPVR set at ≥ 80%, the treatment result was better than that of myomectomy (14, 28, 44, 45). Notably, the inexperienced physicians could reach NPVR ≥ 80% and the experienced group was better than the inexperienced group in NPVR and technical success, indicating that HIFU technology was stable and easy to learn and can tend to be better technical success with better experience, which was worth considering doing HIFU physicians engaged in long-term development. Furthermore, appropriate patient selection was a significant factor in reducing the risk of an unsuccessful outcome of HIFU treatment of uterine fibroids (39, 46); this study discussed characteristic factors of the patient influencing technical success of HIFU ablation for uterine fibroids and whether there were differences in patient selection between the inexperienced physicians and the experienced physicians that provide a certain basis for the choice of patients.
In conclusion, when the treatment standard of HIFU for uterine fibroids is NPVR ≥ 80 %, the two groups of physicians can complete this standard; the inexperienced physicians are also trustworthy in the sufficient ablation for HIFU ablation of uterine fibroids. NPVR ≥ 80% is a standard that is worth being used in HIFU treatment of uterine fibroids. HIFU treatment of uterine fibroids is affected by multiple factors, experienced physicians, smaller volume of uterus, and fibroids of anterior wall that are easier to ablate with higher treatment success. In this study, experienced physicians still achieved better technical success in selecting patients with larger uterus for treatment, providing a basis for physicians with different experience to select patients. In addition, in the selection of indications, with the rich of experience of the physician, more patients with uterine fibroids are suitable for HIFU ablation treatment.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Chinese Ethics Committee of Registering Clinical Trials (IRB approval number: ChiECRCT-2011034). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
XG, XZ, DL, CY, RZ, ZX, WC, and JC provide methods and ideas. XG, XZ, and JC visited and analyzed the data. XG and JC wrote and revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the Chongqing Medical University Intelligent Medicine Project (Grant Number ZHYX2019007).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors wishes to thank the clinical staff from all the clinical centers for their contributions to recruiting patients and providing clinical care.
1. Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers. (2016) 2:16043. doi: 10.1038/nrdp.2016.433
2. Stewart E, Cookson C, Gandolfo R, Schulze-Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG: Int J Obstet Gy. (2017) 124:1501–12. doi: 10.1111/1471-0528.14640
3. Silberzweig JE, Powell DK, Matsumoto AH, Spies JB. Management of uterine fibroids: a focus on uterine-sparing interventional techniques. Radiology. (2016) 280:675–92. doi: 10.1148/radiol.2016141693
4. Faustino F, Martinho M, Reis J, Águas F. Update on medical treatment of uterine fibroids. Eur J Obstet Gynecol Reprod Biol. (2017) 216:61–8. doi: 10.1016/j.ejogrb.2017.06.047
5. Ramdhan RC, Loukas M, Tubbs RS. Anatomical complications of hysterectomy: A review. Clin Anat. (2017) 30:946–52. doi: 10.1002/ca.22962
6. Ciebiera M, Łoziński T, Wojtyła C, Rawski W, Jakiel G. Complications in modern hysteroscopic myomectomy. Ginekol Pol. (2018) 89:398–404. doi: 10.5603/GP.a2018.0068
7. Abbas AM, Michael A, Ali SS, Makhlouf AA, Ali MN, Khalifa MA. Spontaneous prelabour recurrent uterine rupture after laparoscopic myomectomy. J Obstet Gynaecol. (2018) 38:1033–4. doi: 10.1080/01443615.2018.1447913
8. Toor SS, Jaberi A, Macdonald DB, McInnes MDF, Schweitzer ME, Rasuli P. Complication rates and effectiveness of uterine artery embolization in the treatment of symptomatic leiomyomas: a systematic review and meta-analysis. AJR Am J Roentgenol. (2012) 199:1153–63. doi: 10.2214/AJR.11.8362
9. Worthington-Kirsch R, Spies JB, Myers ER, Mulgund J, Mauro M, Pron G, et al. The Fibroid Registry for Outcomes Data (FIBROID) for Uterine Embolization: Short-Term Outcomes. Obstet Gynecol. (2005) 106:52–59. doi: 10.1097/01.ogx.0000183583.44954.17
10. Suomi V, Komar G, Sainio T, Joronen K, Perheentupa A, Blanco Sequeiros R. Comprehensive feature selection for classifying the treatment outcome of high-intensity ultrasound therapy in uterine fibroids. Sci Rep. (2019) 9:10907. doi: 10.1038/s41598-019-47484-y
11. Duc NM, Keserci B. Emerging clinical applications of high-intensity focused ultrasound. Diagn Interv Radiol. (2019) 25:398–409. doi: 10.5152/dir.2019.18556
12. Keserci B, Duc NM, Nadarajan C, Huy HQ, Saizan A, Wan Ahmed WA, et al. Volumetric MRI-guided, high-intensity focused ultrasound ablation of uterine leiomyomas: ASEAN preliminary experience. Diagn Interv Radiol. (2020) 26:207–15. doi: 10.5152/dir.2019.19157
13. Izadifar Z, Izadifar Z, Chapman D, Babyn P. An Introduction to High Intensity Focused Ultrasound: Systematic Review on Principles, Devices, and Clinical Applications. JCM. (2020) 9:460. doi: 10.3390/jcm9020460
14. Verpalen IM, Anneveldt KJ, Nijholt IM, Schutte JM, Dijkstra JR, Franx A, et al. Magnetic resonance-high intensity focused ultrasound (MR-HIFU) therapy of symptomatic uterine fibroids with unrestrictive treatment protocols: A systematic review and meta-analysis. Eur J Radiol. (2019) 120:108700. doi: 10.1016/j.ejrad.2019.108700
15. Gani F, Cerullo M, Zhang X, Canner JK, Conca-Cheng A, Hartzman AE, et al. Effect of surgeon “experience” with laparoscopy on postoperative outcomes after colorectal surgery. Surgery. (2017) 162:880–90. doi: 10.1016/j.surg.2017.06.018
16. Bedri E, Worku A, Redleaf M. The effect of surgeon experience on tympanic membrane closure. Laryngoscope Investig Otolaryngol. (2019) 4:526–31. doi: 10.1002/lio2.296
17. Chen J, Li Y, Wang Z, McCulloch P, Hu L, Chen W, et al. Evaluation of high-intensity focused ultrasound ablation for uterine fibroids: an IDEAL prospective exploration study. BJOG: Int J Obstet Gy. (2018) 125:354–64. doi: 10.1111/1471-0528.14689
18. Keserci B, Duc NM. The role of T1 perfusion-based classification in predicting the outcome of magnetic resonance-guided high-intensity focused ultrasound treatment of adenomyosis. Int J Hyperthermia. (2018) 34:306–14. doi: 10.1080/02656736.2017.1326634
19. Orsini LF, Salardi S, Pilu G, Bovicelli L, Cacciari E. Pelvic organs in premenarcheal girls: real-time ultrasonography. Radiology. (1984) 153:113–6. doi: 10.1148/radiology.153.1.6473771
20. Funaki K, Fukunishi H, Funaki T, Sawada K, Kaji Y, Maruo T. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol. (2007) 196:184.e1–184.e6. doi: 10.1016/j.ajog.2006.08.030
21. Goodwin SC, Bonilla SC, Sacks D, Reed RA, Spies JB, Landow WJ, et al. Reporting standards for uterine artery embolization for the treatment of uterine leiomyomata. J Vasc Interv Radiol. (2003) 14:S467–76. doi: 10.1097/01.RVI.0000094620.61428.9c
22. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided Tumor Ablation: Standardization of Terminology and Reporting Criteria. J Vasc Interv Radiol. (2005) 16:765–78. doi: 10.1097/01.RVI.0000170858.46668.65
23. Zhang L, Zhang W, Orsi F, Chen W, Wang Z. Ultrasound-guided high intensity focused ultrasound for the treatment of gynaecological diseases: A review of safety and efficacy. Int J Hyperthermia. (2015) 31:280–4. doi: 10.3109/02656736.2014.996790
24. Wei C, Fang X, Wang C, Chen Y, Xu X, Dong J. The predictive value of quantitative DCE metrics for immediate therapeutic response of high-intensity focused ultrasound ablation (HIFU) of symptomatic uterine fibroids. Abdom Radiol. (2018) 43:2169–75. doi: 10.1007/s00261-017-1426-7
25. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. (2019) 191:626–9. doi: 10.1055/a-0884-3143
26. Cheung VYT. High-intensity focused ultrasound therapy. Best Practice & Research. J Clin Med. (2018) 46:74–83. doi: 10.1016/j.bpobgyn.2017.09.002
27. Froeling V, Meckelburg K, Schreiter NF, Scheurig-Muenkler C, Kamp J, Maurer MH, et al. Outcome of uterine artery embolization versus MR-guided high-intensity focused ultrasound treatment for uterine fibroids: Long-term results. Eur J Radiol. (2013) 82:2265–9. doi: 10.1016/j.ejrad.2013.08.045
28. Fauconnier A, Chapron C, Babaki-Fard K, Dubuisson JB. Recurrence of leiomyomata after myomectomy. Hum Reprod Update. (2000) 6:595–602. doi: 10.1093/humupd/6.6.595
29. Stewart EA, Gostout B, Rabinovici J, Kim HS, Regan L, Tempany CMC. Sustained relief of leiomyoma symptoms by using focused ultrasound surgery. Obstet Gynecol. (2007) 110:9. doi: 10.1097/01.AOG.0000295980.77822.c1
30. Hanafi M. Predictors of leiomyoma recurrence after myomectomy. Obstet Gynecol. (2005) 105(4):877-881. doi: 10.1097/01.AOG.0000156298.74317.62
31. Park MJ, Kim Y, Rhim H, Lim HK. Safety and therapeutic efficacy of complete or near-complete ablation of symptomatic uterine fibroid tumors by MR imaging–guided high-intensity focused US therapy. J Vasc Interv Radiol. (2014) 25:231–9. doi: 10.1016/j.jvir.2013.11.011
32. Yang M-J, Yu R-Q, Chen W, Chen J-Y, Wang Z-B. A Prediction of NPVR ≥ 80% of ultrasound-guided high-intensity focused ultrasound ablation for uterine fibroids. Front Surg. (2021) 8:663128. doi: 10.3389/fsurg.2021.663128
33. Keserci B, Duc NM. Magnetic resonance imaging parameters in predicting the treatment outcome of high-intensity focused ultrasound ablation of uterine fibroids with an immediate nonperfused volume ratio of at least 90%. Acad Radiol. (2018) 25:1257–69. doi: 10.1016/j.acra.2018.01.022
34. Keserci B, Duc NM. Magnetic resonance imaging features influencing high-intensity focused ultrasound ablation of adenomyosis with a nonperfused volume ratio of ≥90% as a measure of clinical treatment success: retrospective multivariate analysis. Int J Hyperthermia. (2018) 35:626–36. doi: 10.1080/02656736.2018.1516301
35. Baker KG, Robertson VJ, Duck FA. A Review of Therapeutic Ultrasound: Biophysical Effects. Phys Ther. (2001) 81:1351–8. doi: 10.1093/ptj/81.7.1351
36. Yin N, Hu L, Xiao ZB, Liu C, Chen WZ, Roberts N, et al. Factors influencing thermal injury to skin and abdominal wall structures in HIFU ablation of uterine fibroids. Int J Hyperthermia. (2018) 34:1298–303. doi: 10.1080/02656736.2018.1433880
37. Fan HJ, Cun JP, Zhao W, Huang JQ Yi GF, Yao RH, et al. Factors affecting effects of ultrasound guided high intensity focused ultrasound for single uterine fibroids: a retrospective analysis. Int J Hyperthermia. (2018) 35:534–40. doi: 10.1080/02656736.2018.1511837
38. Haar G. ter, Sinnett D, Rivens I. High intensity focused ultrasound-a surgical technique for the treatment of discrete liver tumours. Phys Med Biol. (1989) 34:1743–50. doi: 10.1088/0031-9155/34/11/021
39. Duc NM, Keserci B. Review of influential clinical factors in reducing the risk of unsuccessful MRI-guided HIFU treatment outcome of uterine fibroids. Diagn Interv Radiol. (2018) 24:283–91. doi: 10.5152/dir.2018.18111
40. McAteer JP, LaRiviere CA, Drugas GT, Abdullah F, Oldham KT, Goldin AB. Influence of Surgeon Experience, Hospital Volume, and Specialty Designation on Outcomes in Pediatric Surgery: A Systematic Review. JAMA Pediatr. (2013) 167:468. doi: 10.1001/jamapediatrics.2013.25
41. Machtinger R, Inbar Y, Cohen-Eylon S, Admon D, Alagem-Mizrachi A, Rabinovici J. MR-guided focus ultrasound (MRgFUS) for symptomatic uterine fibroids: predictors of treatment success. Hum Reprod. (2012) 27:3425–31. doi: 10.1093/humrep/des333
42. Minh Duc N, Huy HQ, Keserci B. Adverse events of focused ultrasound surgery for uterine fibroids and adenomyosis. RMI Volume. (2018) 11:15–26. doi: 10.2147/RMI.S166580
43. Qin J, Chen J-Y, Zhao W-P, Hu L, Chen W-Z, Wang Z-B. Outcome of unintended pregnancy after ultrasound-guided high-intensity focused ultrasound ablation of uterine fibroids. Int J Gynaecol Obstet. (2012) 117:273–7. doi: 10.1016/j.ijgo.2012.01.011
44. Wang X, Qin J, Wang L, Chen J, Chen W, Tang L. Effect of high-intensity focused ultrasound on sexual function in the treatment of uterine fibroids: comparison to conventional myomectomy. Arch Gynecol Obstet. (2013) 288:851–8. doi: 10.1007/s00404-013-2775-2
45. Qu K, Mao S, Li J, Wang J, Ouyang G, Wang Z, et al. The impact of ultrasound-guided high-intensity focused ultrasound for uterine fibroids on ovarian reserve. International Journal of Hyperthermia. (2020) 37:399–403. doi: 10.1080/02656736.2020.1754473
Keywords: high-intensity focused ultrasound (HIFU), uterine fibroid, physician experience, training, technical success, non-perfused volume ratio (NPVR)
Citation: Gong X, Zhang X, Liu D, Yang C, Zhang R, Xiao Z, Chen W and Chen J (2022) Physician Experience in Technical Success of Achieving NPVR ≥ 80% of High-Intensity Focused Ultrasound Ablation for Uterine Fibroids: A Multicenter Study. Front. Med. Technol. 3:790956. doi: 10.3389/fmedt.2021.790956
Received: 07 October 2021; Accepted: 05 November 2021;
Published: 08 March 2022.
Edited by:
Minzhong Yu, Case Western Reserve University, United StatesReviewed by:
Nguyen Minh Duc, Pham Ngoc Thach University of Medicine, VietnamCopyright © 2022 Gong, Zhang, Liu, Yang, Zhang, Xiao, Chen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinyun Chen, Y2hlbmp5QGNxbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.