
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Med. , 04 March 2025
Sec. Intensive Care Medicine and Anesthesiology
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1561619
Background: Fluid is an essential component of initial resuscitation in sepsis or burns. Meanwhile, the optimal strategy of titrating fluids for both of the two conditions remains uncertain. In this bibliometric analysis, we compared the similarities and differences in fluid resuscitation between sepsis and burns in recent publications.
Methods: Literatures related to fluid resuscitation in either sepsis or burns were searched in the Web of Science database Core Collection from January 1, 1992, to December 31, 2022. CiteSpace and VOSviewer was used for bibliometric analysis.
Results: A total of 1,549 and 468 publications on fluid resuscitation in sepsis and burns were retrieved from 1992 to 2022. Based on the occurrences, 341 and 86 high-frequency keywords were screened out from sepsis and burns publications, respectively, which were similarly categorized into 5 clusters [i.e. “mechanisms of hypovolemia” (cluster 1), “titration of fluid” (cluster 2), “outcomes or complications” (cluster 3), “pathophysiological alternations” (cluster 4), and “fluid types and others” (cluster 5)]. The high-frequency keywords of the top 20 were more concentrated in cluster 3 and cluster 2, with “mortality” ranked the top in both sepsis and burns literature. Significantly, 3 keywords in cluster 2 ranked in the top 5, including “goal directed resuscitation” (the 3rd), fluid responsiveness (the 4th) and fluid balance (the 5th) in sepsis literature, while the keywords of “microvascular exchange” (cluster 1) and “abdominal compartment syndrome” (ACS, cluster 3) ranked at the second and the fifth place in burns publications. Keyword burst analysis demonstrated that the keyword with the highest burst strength (BS) was “formula” (BS = 5.88, 2008–2014), followed by management (BS = 4.79, 2012–2022), ACS (BS = 4.76, 2006–2010), and fluid creep (BS = 4.74, 2011–2016) in burn publications, but they were dobutamine (BS = 12.31, 1992–2008), cardiac output (BS = 9.79, 1993–2001), catecholamine (BS = 9.54, 1993–2006), and consumption (BS = 7.52, 1992–2006) in sepsis literature. Moreover, the most frequently cited article in either sepsis or burns was categorized into cluster 2, that investigated goal-directed fluid therapy for sepsis and formula improvement for burns resuscitation.
Conclusion: It was demonstrated that the research priorities in titrating fluid were mainly concentrated on targeting hemodynamics in sepsis vs. improving formula (which briefly calculates the increased microvascular permeability) in burns, while concerning of “outcomes and complications” in fluid resuscitation similarly after 1992. However, hemodynamics and microvascular permeability have been simultaneously well considered in few previous studies regarding fluid resuscitation in either sepsis or burns.
Administering adequate fluid to improve circulation, perfusion, and oxygen delivery is a common goal of physicians during initial resuscitation in patients with sepsis or burns, both of which share similar pathophysiological mechanisms of hypovolemia (1, 2). However, a growing body of evidence suggests that the potential harms of fluid accumulation are well documented (3, 4). Of note, severe complications of overload such as hypoxia, abdominal compartment syndrome (ACS) and tissue edema could counterbalance the benefits of fluid resuscitation. Therefore, optimizing fluid therapy has been therefore one of the research priorities in sepsis and burns in the past three decades.
Severe burns are usually administered with a large amount of fluids within the first 24 h because of burn shock, characterized by specific microvascular and hemodynamic changes (5). In the past few decades, efforts have been made to promote formulas for estimating fluid requirement based on total burn area (6). In addition, goal-directed fluid therapy has been comprehensively investigated in the initial fluid resuscitation of severe burns since the report of Dries and Waxman in 1991 (7). Meanwhile, there is no consensus on the optimization of initial fluid resuscitation in severe burns. It is worth noting that “fluid creep,” a phenomenon of excessive fluid demand, resulting in a series of harmful effects (8), has attracted increasing attention in acute burn resuscitation recently (9–11).
Initial fluid resuscitation is an essential component of intensive therapies for sepsis (12). The therapeutic goal is to rapidly reverse hypoperfusion (with or without hypotension), administering fluid boluses, continuing fluid replacement and frequently using vasopressors as well (13). This approach was encouraged worldwide due to the results of Rivers's EGDT trial (Early Goal-Directed Therapy) (14) and high recommendation of the “Surviving Sepsis Campaign Guidelines for Management of Severe Sepsis and Septic Shock” (15). However, the recommended goal of fluid resuscitation did not always represent the optimal volume of an individual need, because of interindividual variability resulted from by various biometric factors (16). Accordingly, it was found that overload was common in clinical practices although the cardiac output could be improved large probably by an aggressive fluid resuscitation strategy in the early phase of sepsis (2). Moreover, positive fluid balance during initial resuscitation was associated with higher morbidity and mortality of sepsis (17). Therefore, the latest update of the Surviving Sepsis Campaign (SSC) international guidelines proposed the physiology-based individualized initial fluid resuscitation (18).
In fact, it remains problematic to avoid overload while ensuring adequate plasma volume expansion during fluid resuscitation in both sepsis and burns. Aimed at finding useful information to suggest further research priorities, this bibliometric analysis described the similarities and differences in recent publications on fluid resuscitation between sepsis and burns.
Literature search was performed in the Web of Science (WoS) database Core Collection, which is one of the most comprehensive, systematic and authoritative databases, and has been successfully used for bibliometric analysis (19). The type of literature was limited to original articles and reviews. Publications on fluid resuscitation in burns or sepsis from 1992 to 2022 were retrieved for this bibliometric analysis. The retrieval strategies were as follows: (TS = (burn OR thermal injury) AND TS = (fluid OR liquid OR volume OR colloid OR crystalloid) AND TS = (resuscitation OR therapy OR replacement OR balance OR responsiveness OR challenge)) for burn, and (TS = (sepsis OR septic OR bacteremia OR septicemia OR endotoxemia) AND TS = (fluid OR liquid OR volume OR colloid OR crystalloid) AND TS = (resuscitation OR therapy OR replacement OR balance OR responsiveness OR challenge)) for sepsis, respectively. To avoid changes in publication and citation due to frequent database updates, all searches were performed on a single day, i.e., July 31th, 2023. In addition, all data were obtained from this public database and did not involve any personal information. Therefore, the informed consent for this study was waived by the Ethics Committee of Guiqian International General Hospital. The detailed procedure of literature selection and screening was shown in Figures 1A, B.
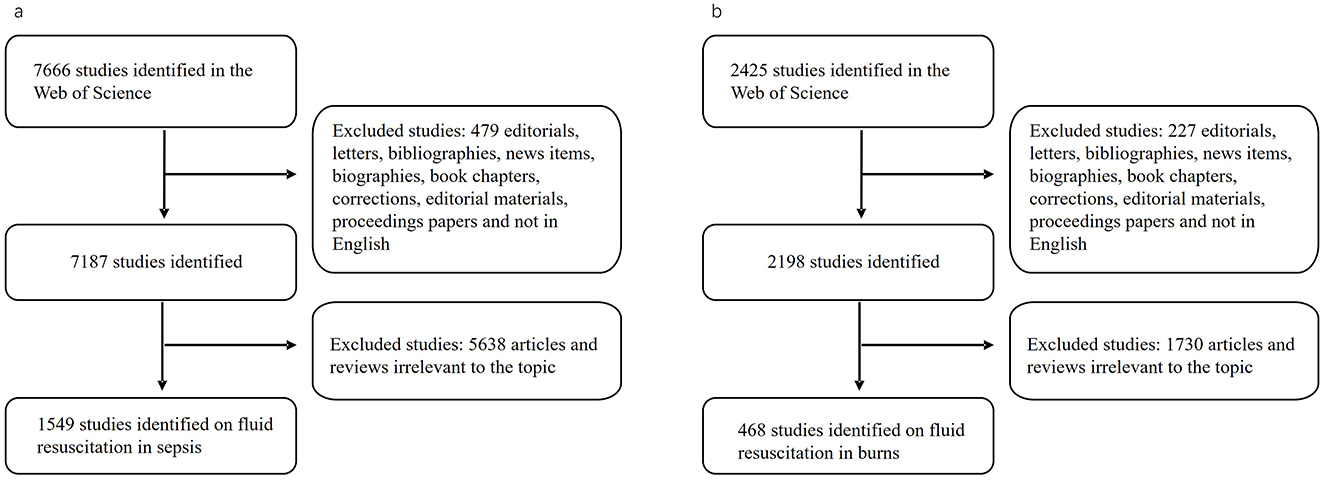
Figure 1. Flowchart for publication selection. The search strategy and process of selecting publications on fluid resuscitation for sepsis (A) and burn (B).
Two researchers (Dongxu Zhou and Lulu He) independently searched the literature. The consistency of the results was 96.8%, which is significant. The title, abstract, authors, countries, institutions, journal, publication year, key words and the total/average citation of the literature were screened and recorded. Reassessment was performed by Dr. Penglin Ma and a three-way coordination was performed immediately if there was any discrepancy in publications screening between the two researchers. The flow chart of publication selection is shown in Figure 1. VOSviewer version 1.6.16, and CiteSpace version 5.8.R1 64 bit, was used to present, analyze, and describe the data.
Keywords represent concise summaries of the core content of the literature. They can reveal the overall characteristics of research results, the inherent connections between research topics, the development trajectory of academic research, and its directions. Therefore, high-frequency keywords can reflect the research hotspots and main research content in the field. In this study, the scientific mapping of keyword co-occurrences and co-cited references in the recruited publications were completed using VOSviewer 1.6.16, a free Java-based software that is mainly oriented to bibliographic data and focuses on the visualization of scientific knowledge and was developed by Nees Jan van Eck and Ludo Waltman in 2009 (20). In the network map, different nodes represent different keywords or citation of publications, and the node size reflects the frequency of occurrence of the keyword or the number of citations of the publication (21). Links between nodes indicate relationships such as co-reference, co-occurrence, and collaboration. Furthermore, VOSviewer can classify keywords into different clusters based on co-occurrence analysis, and simultaneously color them according to the time course. The definition of average appearing year (AAY) was used to quantify the relative novelty of a keyword (22). CiteSpace 5.8.R1, another software developed by professor Chaomei Chen, was used to identify new trends and advances in the scientific literature (23). In our study, it was mainly used for keyword bursts analysis.
There have been 1,549 publications on sepsis fluid resuscitation since 1992 (Figure 2). The number of publications per year rapidly increased overtime, from about 20 articles in 1992, to more than 50 in 2010, and above 100 after 2021. A total number of 468 publications on fluid resuscitation in burn researches met the inclusion criteria for this bibliometric analysis. The annual number of publications never exceeded 50 until 2022 in this field. Meanwhile, it was found that the cumulative proportions were significantly increased in publications on fluid resuscitation among all literatures in both sepsis and burns over years (Supplementary Figure S1).
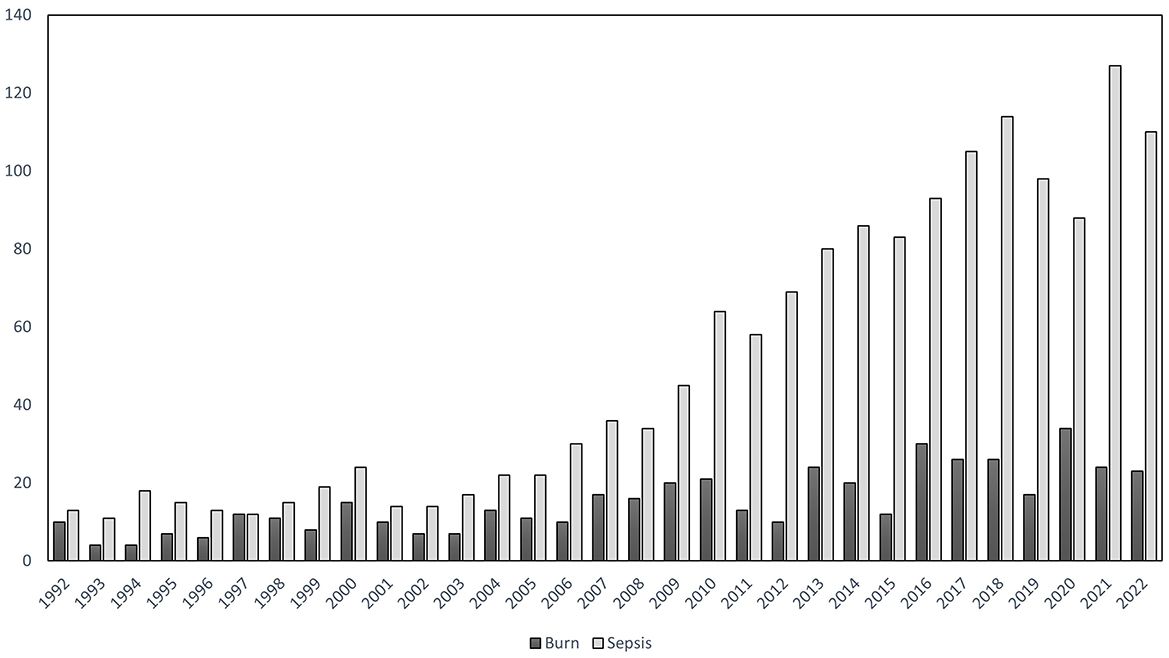
Figure 2. Annual publications from 1992 to 2022. The X-axis represented each year from 1992 to 2022, the Y-axis represented the number of annual publications on fluid resuscitation for burn (dark bar) and sepsis (gray bar).
VOSviewer was used to cluster the keywords of the included literature. Subject terms, synonyms, repetitive words and unrelated terms (sepsis, septic shock, severe sepsis, burn, burns, injury, thermal injury, burn injury, trauma, resuscitation, therapy, fluid therapy, fluid resuscitation, advance, association, critical illness, etc.) were excluded. A mapping analysis was performed for the keywords that occurred equal to or more than 5 times either in sepsis or burns of the literature.
As shown in Figure 3A, 341 keywords from 1,549 publications on fluid resuscitation in sepsis were analyzed (listed in Supplementary Figure S1), resulting in 5 different clusters. Cluster 1 (100 Keywords) was closely related to the mechanisms of sepsis-induced hypovolemia (red), including high-frequency keywords such as vascular dysfunction (76 occurrences), nitric oxide (42 occurrences) and inflammation (33 occurrences). Eighty-two keywords in cluster 2 were mainly related to titration of fluid therapy, as indicated in green, including fluid responsiveness (225 occurrences), cardiac output (107 occurrences) and blood pressure (77 occurrences), etc. In cluster 3, 52 keywords were related to outcomes or complications shown in yellow, that was weighted the highest in occurrences, such as mortality (426 occurrences), management (331 occurrences), and acute kidney injury (AKI; 148 occurrences). Cluster 4 (56 keywords) was related to pathophysiological changes in fluid resuscitation shown in blue, including microcirculatory blood-flow (140 occurrences), norepinephrine therapy (122 occurrences) and hemodynamic (110 occurrences), etc. The remaining 51 out of 341 keywords were categorized into the cluster of fluid types and others (cluster 5), including hydroxyethyl starch (128 occurrences), sodium chloride (77 occurrences) and albumin (70 occurrences, purple circles), etc.
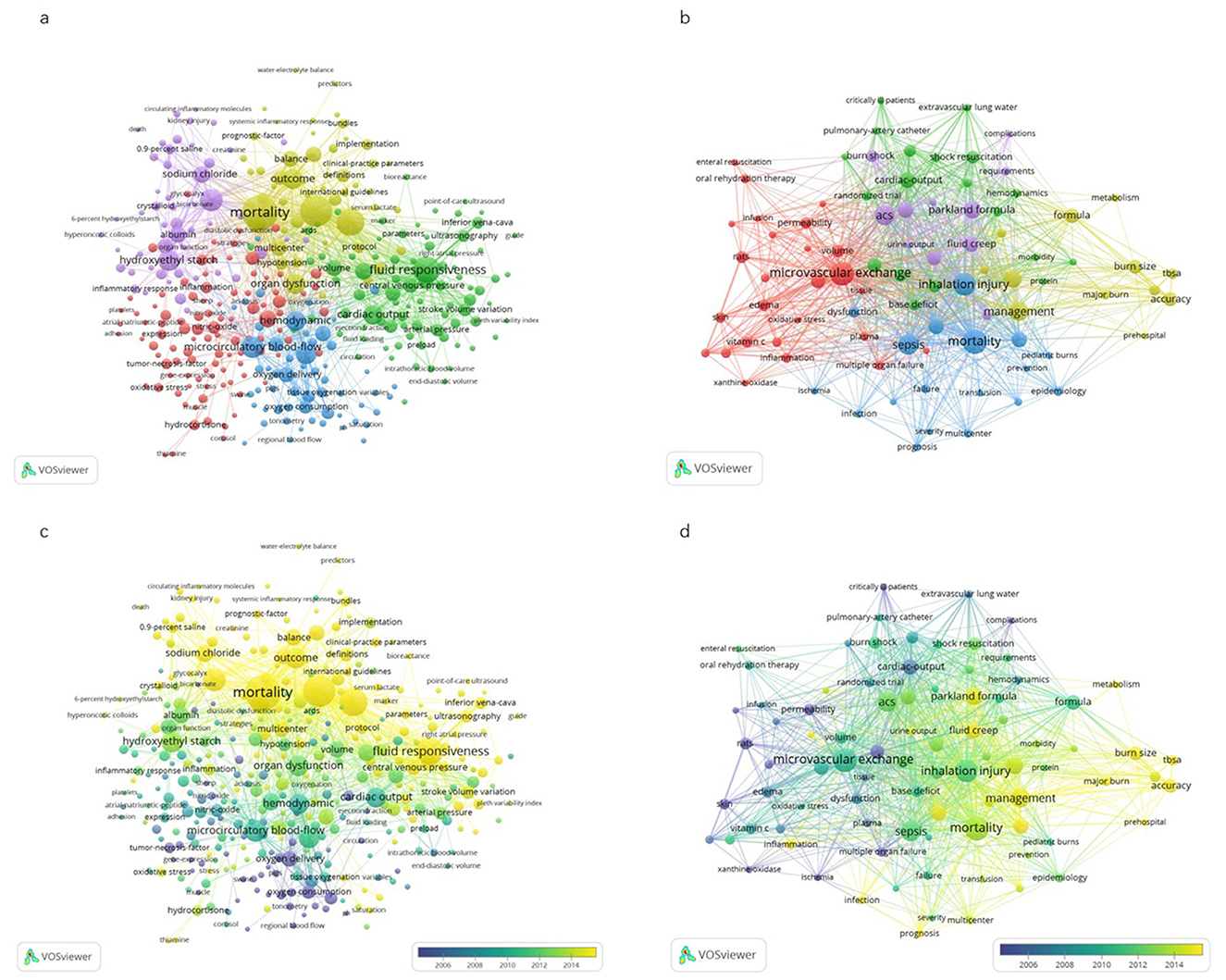
Figure 3. Visualization map of Keywords co-occurrence network in publications. The figure represented the network of keywords with more than 5 occurrences in publications on fluid resuscitation for sepsis (A) and burn (B). The size of the circles indicated the co-occurrence frequency of keywords. The clusters of the keywords (i.e., a set of keywords calculated in the co-occurrence network as a community) were showed in different colors. The connecting lines indicated co-occurrence of the 2 keywords at both ends. The thickness of lines between circles indicated strength of linkage calculated by the frequency of co-occurrence. In addition, VOSviewer colored all keywords in accordance with the average time when the keyword appeared in publications for sepsis (C) and for burn (D). The blue color represented the keywords appeared relatively earlier upon time course, while keywords in yellow for recent appearance.
As show in Figure 3B, a total of 86 keywords extracted in 468 publications on burn fluid resuscitation was also categorized in 5 distinct clusters, which were similar to that in sepsis. Keywords in cluster 1 were largely related to the mechanism of burn shock (26 keywords in red). Cluster 2 was the keywords associated with titration of fluid therapy (19 keywords in green). Keywords in cluster 3 were related to complications and outcomes (19 keywords in blue, with the highest weight in occurrences). Cluster 4 was comprised of the keywords with regard to pathophysiological alternation in fluid resuscitation (12 keywords in yellow). The last cluster was related to the keywords for fluid type and the others (10 keywords in purple).
In addition, as shown in Figures 3C, D, VOSviewer colors all keywords according to their average time of appearance. Blue indicates keywords appearing relatively early in the time course (i.e., earliest, before 2006), and yellow indicates keywords that appear more recently (i.e., latest, after 2014). In the literature of fluid resuscitation in burns, the top 3 high-frequency keywords appeared earliest vs. latest were cardiac-output, oxygen delivery, permeability vs. management, formula and critical care. Meanwhile, the earliest vs. the latest top 3 high-frequency keywords were oxygen delivery, oxygen consumption and dobutamine vs. mortality, management, goal directed resuscitation in the literature in sepsis (Supplementary Table S2).
The top 20 high-frequency keywords in the literature of fluid resuscitation for burns and sepsis were similarly distributed into 5 clusters, as shown in Table 1. Of the top 20, 6 and 5 keywords were clustered into “outcomes or complications” in sepsis literature [mortality (the 1st), AKI (the 6th), outcome (the 9th), organ dysfunction (the 11th) and survival (the 14th)], and in burns literature including mortality (the 1st), sepsis (the 4th), ACS (the 5th), critical care (the 7th), AKI (acute kidney injury, the 10th) and outcomes (the 13th), respectively. Of the top 20, there were 6 keywords in sepsis [goal directed resuscitation (the 3rd), fluid responsiveness (the 4th), fluid balance (the 5th), cardiac output (the 13th), blood pressure (the 15th) and volume (the 20th)], and 4 keywords in burns [Parkland formula (the 8th), cardiac-output (the 9th), formula (the 14th) and blood pressure (the 15th)] in the cluster of “titration of fluid therapy.” There were 1 and 3 out of top 20 keywords clustered into “mechanisms of hypovolemia” and “pathophysiological alternations,” respectively in literature of both sepsis and burns. The other 6 and 5 of top 20 high frequency keywords were classified into “fluid types and others” in burns and sepsis literature. Notably, mortality was the top ranked keyword in either burns or sepsis literature. In addition, it was demonstrated that three keywords in the cluster of “titration of fluid therapy” including goal directed resuscitation (the 3rd), fluid responsiveness (the 4th) and fluid balance (the 5th) were ranked in top five in sepsis literature. Meanwhile, the keywords of “microvascular exchange” and “abdominal compartment syndrome” (ACS) ranked at the second and the fifth place in burns publications.
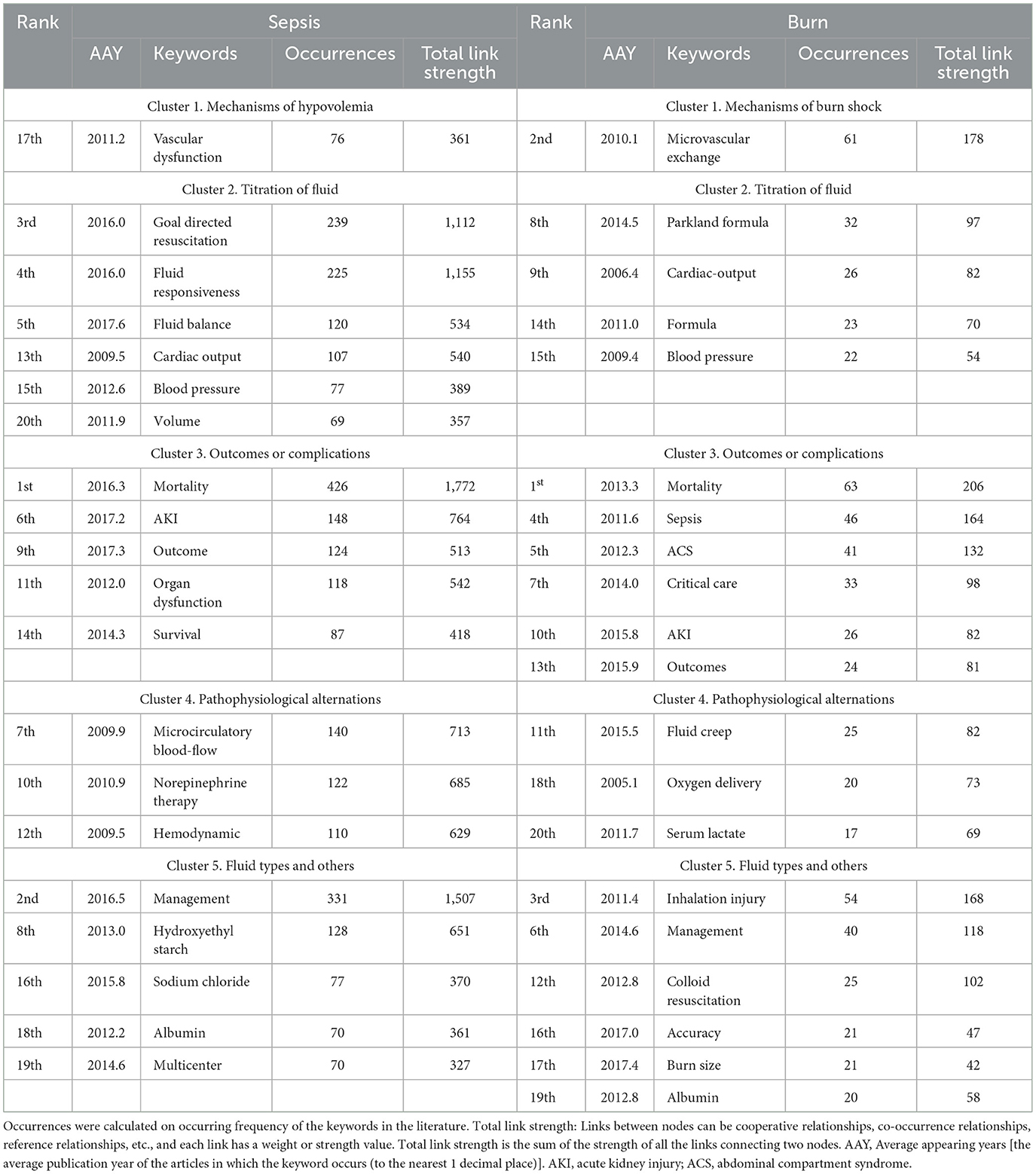
Table 1. Classification of the top 20 high-frequency keywords in publications on fluid resuscitation for sepsis and burns.
Burst detection identified the emerging concepts that caught the attention of peer investigators. Keywords bursts indicated possible hot research topics. The timeline was represented by a blue line divided by year, and the red part of the blue timeline represents the time interval of the burst, indicating the start/end year and duration of a citation burst. Figures 4A, B show the keyword burst analysis in publications related to fluid resuscitation in sepsis and burn.
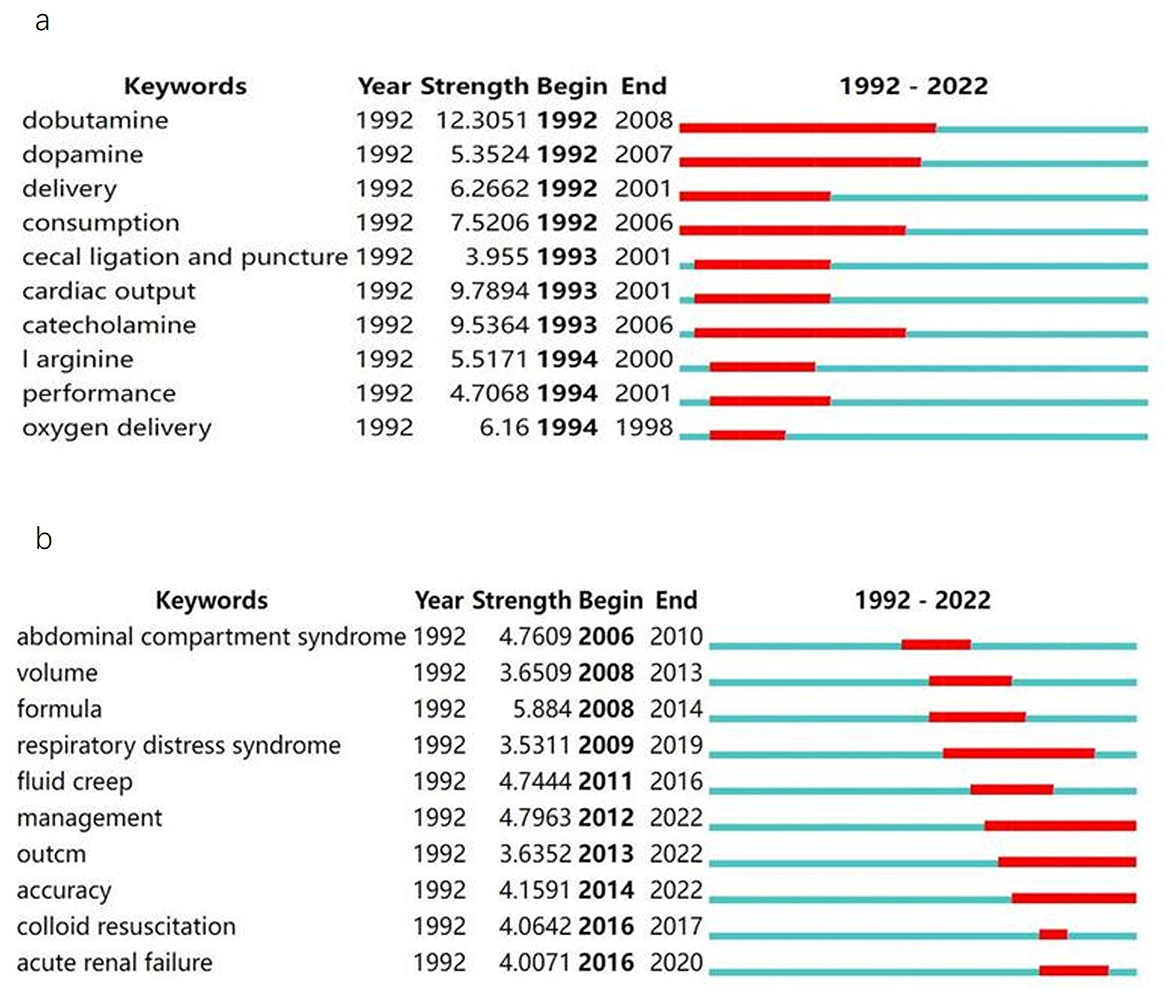
Figure 4. Top 10 keywords with the strongest citation bursts. This represented the keywords with the strongest citation bursts in publications on fluid resuscitation for sepsis (A) and for burn (B) from 1992 to 2022. The time interval of a burst was marked as a red section on the blue timeline to indicate the beginning/ending year and the duration of a citation burst.
Keywords burst analysis was performed in 1,549 articles on sepsis fluid resuscitation in the WoS database from 1992 to 2022. Dobutamine had the highest burst strength (burst strength: 12.3051), and lasted from 1992 to 2008, followed by cardiac output (burst strength: 9.7894, duration: 1993–2001), catecholamine (burst strength: 9.5364, duration: 1993–2006), and consumption (burst strength: 7.5206, duration: 1992–2006).
A total of 468 articles on burn fluid resuscitation from 1992 to 2022 were searched in the WOS database, and an outbreak of keywords was detected. The keyword with the highest burst strength was “formula” (burst strength: 5.884), which occurred from 2008 till 2014, followed by management (burst strength: 4.7963, duration: 2012–2022), abdominal compartment syndrome (burst strength: 4.7609, duration: 2006–2010), and fluid creep (burst strength: 4.7444, duration: 2011–2016).
Highly cited articles are the foundation of a research field and reflect important scientific achievements and academic influence to a certain extent. The co-citation graph of cited references is displayed at Supplementary Figure S2. Table 2 list the top 10 highly cited articles on fluid resuscitation for burn and sepsis, respectively.
There were only 1 randomized controlled trial (RCT) (24) and 2 prospective studies (10, 25), in addition to 3 reviews (8, 26, 27), 3 retrospective cohort studies and 1 clinical practice guideline among the top 10 highly cited articles on burn fluid resuscitation (9, 28–30). The most frequently cited article (with 89 citations) was “Physiological response to crystalloid resuscitation of severe burns” (23). The next was “Protection from Excessive Resuscitation: “Pushing the Pendulum Back”” (26) with 81 citations. It was noted that the latest highly cited article was the updated American Burn Association Practice Guidelines for Burn Shock Resuscitation, which was published in 2008 (30).
Table 2 lists top 10 highly cited articles on sepsis fluid resuscitation researches from 1992 to 2022, including 5 randomized controlled trials, 2 clinical guidelines, 2 reviews (updating sepsis definition), and 1 retrospective cohort studies. The most frequently cited article (with 528 citations) was “Early goal-directed therapy in the treatment of severe sepsis and septic shock” (14). This was followed by “Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock” (31), with 229 citations. The 10 highly citated articles were published from 1992 to 2017.
A total of 4 international practice guidelines for burn care were retrieved in this study (Table 3) (30, 32–34). Two of them were conducted by American Burn Association (30, 32). Of note, the formula of starting acute fluid resuscitation with 2 mL/kg/% TBSA (total body surface area) burn plus considering use of albumin is recommended to reduce the total volume of resuscitation in the recently updated American Burn Association Clinical Practice Guidelines on Burn Shock Resuscitation (32).
We found that the Surviving Sepsis Campaign guidelines for the management of severe sepsis and septic shock have been updated 5 times from 2004 to 2021 (Table 3). The recent updates recommend that at least 30 mL/kg of intravenous (IV) crystalloid fluid be administered within the first 3 h of resuscitation and suggest the use of dynamic measures to guide individualized fluid resuscitation in patients with sepsis-induced hypoperfusion (18).
This bibliometric analysis demonstrated that high-frequency keywords were similarly concentrated in the clusters of “outcomes and complications” as well as “titration of fluid therapy” in publications of fluid resuscitation in patients with either sepsis or burns after 1992. Similarly, mortality ranked the top in the occurrence of the keywords, followed with the keywords about overload associated organ dysfunction or complications, such as AKI, acute respiratory distress syndrome (ARDS), fluid creep, and ACS, etc. in the cluster of “outcomes and complications.” However, our findings suggested that the research priorities were different to the methods of optimizing fluids for sepsis and burns. It was found that the high-frequency keywords and highly cited articles with regard to fluid titration were more tightly linked to targeting hemodynamics improvement in sepsis resuscitation. Meanwhile, the results that “Parkland formula” ranked the 8th of high-frequency keywords, with 4 out of the top 10 frequently cited articles related to “formula” improvement suggested that use of formula to limit resuscitation volume was more emphasized in initial resuscitation for burns. Accordingly, it could be helpful for further researches in titrating fluids for patients with either sepsis or burns to understand the rationales for these diverse research interests.
It has long been recognized that fluid overload leads to worsened organ dysfunction and outcomes in critically ill patients (35). Meanwhile, unnecessary positive fluid balance remained common while resuscitating patients with sepsis (36, 37) or burn shock (9, 38–41). Actually, a great effort has been taken in striking the right fluid balance between adequate and over resuscitation in sepsis for decades, including titration with fluid responsiveness static or dynamic measurements such as central venous pressure (CVP), stroke volume variation (SVV), pulse pressure variation (PPV) and passive leg raising (PLR) (42); or hemodynamic endpoints such as capillary refill time (CRT), lactate clearance, central venous saturation, Pv-a CO2 gap and urinary output (43). Similarly, research priority was given to titrate fluids in initial resuscitation for burn shock, such as investigating use of malperfusion markers (such as lactate, base deficit and urine output), or hemodynamic endpoints (CVP, transpulmonary thermodilution-derived variables, or arterial waveform analysis) (44) or algorithm-based and computer supported decisions to optimize fluid resusciatation (45, 46). However, the optimal strategy of fluid titration for these patients remains uncertain. Researches with regard to maximizing benefits while minimizing adverse effects in fluid resuscitation are urgently needed for patients with sepsis or burn shock.
The strength of this study was that a different priority was found between researches on titrating fluids for sepsis and burn shock. Generally, the research priority was tightly related to the distinctive manifestations of a critical illness, for instance, the increased microvascular permeability in burns and the hemodynamic instability in sepsis. However, it could be a limitation that the diverse pathophysiological alternations of resulting in hypovolemia in a specific critical illness such as sepsis or burns have not been well weighed in previous researches of titrating fluids.
Optimization of hemodynamic endpoint has been the focus of sepsis research since the Chicago conference updated the definition of sepsis (47). For instance, early goal directed therapy (EGDT) ranked first in the fluid optimization among the top 20 keywords (Table 1) and the original article was cited most frequently in the retrieved sepsis publications (Table 2) (14). In addition, fluid responsiveness, restrictive fluid management and individualizing resuscitation strategies have been comprehensively studied in the past two decades (43, 48). Although the ideal strategy remains inconclusive, it was emphasized that the fluid administration should be tailored to the patient's individual needs, either “by time” or “by amount” in sepsis resuscitation (49). Meanwhile, these approaches of titrating fluids for sepsis were largely based on the transient effects on increase of cardiac output or tissue perfusion improvement, despite of a concern about organ dysfunction associated with excessive fluids. Pathophysiological alternations in microvasculature such as the intensity of endothelium injury has been under investigated in fluid titration for sepsis (50). Significantly, dynamic assessments on hemodynamics plus intensity of endothelium injury (or microvascular permeability) would be a novelty in further research, and beneficial to the efficiency and safety in clinical practices of fluid resuscitation for sepsis.
Being the fundamental pathophysiological alternation (51), differently, the increased microvascular permeability was seriously concerned in initial fluids resuscitation for burn shock. As showed in Table 1, the keywords of “microvascular exchange” ranked at the second place in burns publications. “Parkland formula” and “formula” ranked the 8th and the 14th of high-frequency keywords, with 4 out of the top 10 frequently cited articles related to “formula” improvement (Tables 1, 3; Supplementary Table S1) suggested that microvascular permeability involved fluid resuscitation strategy was widely investigated (52, 53), although the severity of microvascular permeability was simply estimated by the percentage of TBSA burn. In addition, assessment of hemodynamic endpoint, such as Pulse index Continuous Cardiac Output (PiCCO) that was demonstrated useful for optimizing initial fluid therapy in sepsis, have been attempted to guide titration of fluid requirement for severe burn too (24, 54, 55). However, the findings were controversial. Importantly, it was reported that equivalent to higher fluid resuscitation volumes was administrated in severe burn patients driven by invasive monitoring device than formulas or standard resuscitation, which is often guided by urine volume. Moreover, administration of albumin in initial fluid resuscitation is a hot spot in the field of fluid type domain in burn literature (Table 1), and aims to reduce the total amount of fluid resuscitation and increase urine output in burn patients while reducing edema-related complications as well. Due to insufficient evidence, no recommendation was made on this issue by the currently updated American Burn Association Clinical Practice Guidelines on Burn Shock Resuscitation (32). These findings indicated that the research interests were more likely concentrated in the intensity of endothelium injury (i.e., microvascular permeability) rather than in circulatory function (i.e., hemodynamical instability) in fluid titration for burns. Meanwhile, hemodynamical instability is the major subsequence of hypovolemia, which should be used as the important goal of fluid therapy in severe burns. Based on our results (i.e., the puzzles regarding resuscitation target on hemodynamics), using hemodynamics as a percentage of TBSA based restrictive goal could be a new attempt in further researches on fluid resuscitation in burns.
Naturally, it is complex to decide how much fluids a critically ill patient including burn or sepsis requires individually. First, the causes of hypovolemia were diverse not only between burns and sepsis, but among individuals. The second, fluid response was not identical among the tested patients. Finally, we could hardly estimate the dynamic depletion of fluid in individuals of either burns or sepsis. Therefore, multidimensional integration of characteristics of a critical illness, such as sepsis or burns (comprising of the severity of circulation failure, microvasculature injury, the physiological responsiveness to fluids, etc.) should logically ensure effective and safe fluid resuscitation in either clinical practices or further trials.
This study has at least three limitations. First, the database used in this study is the Web of Science Core Collection database (WOSCC). Failure to include literature related to fluid resuscitation for burns and sepsis not included by WOSCC, such as literature in Chinese, Japanese or German may have affected the results. Second, the frequency of citation was time dependent (i.e., the latest publications would be less likely citated). Therefore, there was a limitation to evaluate the importance of a publication with the citations. Moreover, among 468 burn publications, 12 keywords with very low-frequency ( ≤ 30) were in the top 20 high-frequency keywords, indicating that the topic concentration of burn fluid resuscitation was not high. Therefore, low-frequency keywords, although ranking in top 20, should be carefully interpreted.
It was demonstrated that the research priorities in titrating fluids were different, while concerning of “outcomes and complications” similarly in fluid resuscitation for patients with burns and sepsis after 1992. Researches were more likely concentrated on targeting hemodynamics in sepsis, but on improving formula to calculate the degree of capillary leakage in burns resuscitation. This difference could be attributable to their specifically important pathophysiological alterations, i.e., hemodynamic instability in sepsis vs. the increased microvascular permeability in burns. However, these pathophysiological alternations have been simultaneously considered in few previous studies, although both of them were important (but with different weight) causes for hypovolemia in either sepsis or burns.
DZ: Methodology, Software, Writing – original draft. LH: Methodology, Software, Writing – original draft. WS: Methodology, Writing – original draft. PM: Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
All authors think professor Rongxia Liao for her contribution to manuscript revision.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1561619/full#supplementary-material
Supplementary Figure S1 | Cumulative proportions of publications on fluid resuscitation for burns and sepsis from 1992 to 2022. The X-axis represented the year from 1992 to 2022, the Y-axis represented the cumulative proportions of publications on fluid resuscitation for burn (dark bar) and sepsis (gray bar). (Cumulative proportions of publications on fluid resuscitation for either burn or sepsis was calculated as the cumulative publications on fluid resuscitation/all publications on either burns or sepsis from 1992 till 2022).
Supplementary Figure S2 | Analysis of the co-citation network of cited references. The node's size indicated the frequency of citations; the larger the node, the higher the number of references cited. In Figure (A, B) showed the mapping of the co-citation in publications on fluid resuscitation for sepsis and burn, respectively.
1. Landry DW, Oliver JA. The pathogenesis of vasodilatory shock. N Engl J Med. (2001) 345:588–95. doi: 10.1056/NEJMra002709
2. Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. (2011) 1:1. doi: 10.1186/2110-5820-1-1
3. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. (2013) 369:840–51. doi: 10.1056/NEJMra1208623
4. Wang N, Jiang L, Zhu B, Wen Y, Xi XM; Beijing Acute Kidney Injury Trial (BAKIT) Workgroup. Fluid balance and mortality in critically ill patients with acute kidney injury: a multicenter prospective epidemiological study. Crit Care. (2015) 19:371. doi: 10.1186/s13054-015-1085-4
5. Guilabert P, Usúa G, Martín N, Abarca L, Barret JP, Colomina MJ. Fluid resuscitation management in patients with burns: update. Br J Anaesth. (2016) 117:284–96. doi: 10.1093/bja/aew266
7. Dries DJ, Waxman K. Adequate resuscitation of burn patients may not be measured by urine output and vital signs. Crit Care Med. (1991) 19:327–9. doi: 10.1097/00003246-199103000-00007
8. Saffle JI. The phenomenon of “fluid creep” in acute burn resuscitation. J Burn Care Res. (2007) 28:382–95. doi: 10.1097/BCR.0B013E318053D3A1
9. Klein MB, Hayden D, Elson C, Nathens AB, Gamelli RL, Gibran NS, et al. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg. (2007) 245:622–8. doi: 10.1097/01.sla.0000252572.50684.49
10. Ivy ME, Atweh NA, Palmer J, Possenti PP, Pineau M, D'Aiuto M. Intra-abdominal hypertension and abdominal compartment syndrome in burn patients. J Trauma. (2000) 49:387–91. doi: 10.1097/00005373-200009000-00001
11. Tejiram S, Tranchina SP, Travis TE, Shupp JW. The first 24 hours: burn shock resuscitation and early complications. Surg Clin North Am. (2023) 103:403–13. doi: 10.1016/j.suc.2023.02.002
12. Practice parameters for hemodynamic support of sepsis in adult patients in sepsis. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. (1999) 27:639–60. doi: 10.1097/00003246-199903000-00049
13. Zampieri FG, Bagshaw SM, Semler MW. Fluid therapy for critically ill adults with sepsis: a review. JAMA. (2023) 329:1967–80. doi: 10.1001/jama.2023.7560
14. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. (2001) 345:1368–77. doi: 10.1056/NEJMoa010307
15. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. (2004) 32:858–73. doi: 10.1097/01.CCM.0000117317.18092.E4
16. Saugel B, Vincent JL, Wagner JY. Personalized hemodynamic management. Curr Opin Crit Care. (2017) 23:334–41. doi: 10.1097/MCC.0000000000000422
17. Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. (2015) 19:251. doi: 10.1186/s13054-015-0970-1
18. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. (2021) 47:1181–247. doi: 10.1007/s00134-021-06506-y
19. Qiang W, Xiao C, Li Z, Yang L, Shen F, Zeng L, et al. Impactful publications of critical care medicine research in China: a bibliometric analysis. Front Med. (2022) 9:974025. doi: 10.3389/fmed.2022.974025
20. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
21. Liang C, Luo A, Zhong Z. Knowledge mapping of medication literacy study: a visualized analysis using CiteSpace. SAGE Open Med. (2018) 6:2050312118800199. doi: 10.1177/2050312118800199
22. Yao RQ, Ren C, Wang JN, Wu GS, Zhu XM, Xia ZF, et al. Publication trends of research on sepsis and host immune response during 1999–2019: a 20-year bibliometric analysis. Int J Biol Sci. (2020) 16:27–37. doi: 10.7150/ijbs.37496
23. Synnestvedt MB, Chen C, Holmes JH. CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu Symp Proc. (2005) 2005:724–8.
24. Holm C, Mayr M, Tegeler J, Hörbrand F, Henckel von Donnersmarck G, Mühlbauer W, et al. A clinical randomized study on the effects of invasive monitoring on burn shock resuscitation. Burns. (2004) 30:798–807. doi: 10.1016/j.burns.2004.06.016
25. Baxter CR, Shires T. Physiological response to crystalloid resuscitation of severe burns. Ann N Y Acad Sci. (1968) 150:874–94. doi: 10.1111/j.1749-6632.1968.tb14738.x
26. Pruitt BA Jr. Protection from excessive resuscitation: “pushing the pendulum back”. J Trauma. (2000) 49:567–8. doi: 10.1097/00005373-200009000-00030
27. Baxter CR. Fluid volume and electrolyte changes of the early postburn period. Clin Plast Surg. (1974) 1:693–703. doi: 10.1016/S0094-1298(20)30126-7
28. Cartotto RC, Innes M, Musgrave MA, Gomez M, Cooper AB. How well does the Parkland formula estimate actual fluid resuscitation volumes? J Burn Care Rehabil. (2002) 23:258–65. doi: 10.1097/00004630-200207000-00006
29. Engrav LH, Colescott PL, Kemalyan N, Heimbach DM, Gibran NS, Solem LD, et al. A biopsy of the use of the Baxter formula to resuscitate burns or do we do it like Charlie did it? J Burn Care Rehabil. (2000) 21:91–5. doi: 10.1097/00004630-200021020-00002
30. Pham TN, Cancio LC, Gibran NS. American Burn Association. American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res. (2008) 29:257–66. doi: 10.1097/BCR.0b013e31815f3876
31. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. (2013) 41:580–637. doi: 10.1097/CCM.0b013e31827e83af
32. Cartotto R, Johnson LS, Savetamal A, Greenhalgh D, Kubasiak JC, Pham TN, et al. American burn association clinical practice guidelines on burn shock resuscitation. J Burn Care Res. (2023) 45:565–89. doi: 10.1093/jbcr/irad125
33. Yoshino Y, Ohtsuka M, Kawaguchi M, Sakai K, Hashimoto A, Hayashi M, et al. The wound/burn guidelines−6: guidelines for the management of burns. J Dermatol. (2016) 43:989–1010. doi: 10.1111/1346-8138.13288
34. ISBI Practice Guidelines Committee; Steering Subcommittee; Advisory Subcommittee. ISBI Practice Guidelines for Burn Care. Burns. (2016) 42:953–102. doi: 10.1016/j.burns.2016.05.013
35. Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med. (2020) 48:1862–70. doi: 10.1097/CCM.0000000000004617
36. Marik PE, Linde-Zwirble WT, Bittner EA, Sahatjian J, Hansell D. Fluid administration in severe sepsis and septic shock, patterns and outcomes: an analysis of a large national database. Intensive Care Med. (2017) 43:625–32. doi: 10.1007/s00134-016-4675-y
37. Messina A, Albini M, Samuelli N, Brunati A, Costantini E, Lionetti G, et al. Fluid boluses and infusions in the early phase of resuscitation from septic shock and sepsis-induced hypotension: a retrospective report and outcome analysis from a tertiary hospital. Ann Intensive Care. (2024) 14:123. doi: 10.1186/s13613-024-01347-6
38. Daniels M, Fuchs PC, Lefering R, Grigutsch D, Seyhan H, Limper U, et al. Is the Parkland formula still the best method for determining the fluid resuscitation volume in adults for the first 24 hours after injury?—A retrospective analysis of burn patients in Germany. Burns. (2021) 47:914–21. doi: 10.1016/j.burns.2020.10.001
39. Kumar P. Fluid resuscitation for burns: a double edge weapon. Burns. (2002) 28:613–4. doi: 10.1016/S0305-4179(02)00056-6
40. Mason SA, Nathens AB, Finnerty CC, Gamelli RL, Gibran NS, Arnoldo BD, et al. Hold the pendulum: rates of acute kidney injury are increased in patients who receive resuscitation volumes less than predicted by the parkland equation. Ann Surg. (2016) 264:1142–7. doi: 10.1097/SLA.0000000000001615
41. Mason SA, Nathens AB, Jeschke MG. “Hold the pendulum: rates of acute kidney injury are increased in patients who receive resuscitation volumes less than predicted by the parkland equation”. Ann Surg. (2017) 266:e108. doi: 10.1097/SLA.0000000000001895
42. Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care. (2016) 6:111. doi: 10.1186/s13613-016-0216-7
43. Bakker J, Kattan E, Annane D, Castro R, Cecconi M, De Backer D, et al. Current practice and evolving concepts in septic shock resuscitation. Intensive Care Med. (2022) 48:148–63. doi: 10.1007/s00134-021-06595-9
44. Paratz JD, Stockton K, Paratz ED, Blot S, Muller M, Lipman J, et al. Burn resuscitation–hourly urine output vs. alternative endpoints: a systematic review. Shock. (2014) 42:295–306. doi: 10.1097/SHK.0000000000000204
45. Hoskins SL, Elgjo GI, Lu J, Ying H, Grady JJ, Herndon DN, et al. Closed-loop resuscitation of burn shock. J Burn Care Res. (2006) 27:377–85. doi: 10.1097/01.BCR.0000216512.30415.78
46. Cancio LC, Salinas J, Kramer GC. Protocolized resuscitation of burn patients. Crit Care Clin. (2016) 32:599–610. doi: 10.1016/j.ccc.2016.06.008
47. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. (1992) 20:864–74. doi: 10.1097/00003246-199206000-00025
48. Marik PE, Byrne L, van Haren F. Fluid resuscitation in sepsis: the great 30 mL per kg hoax. J Thorac Dis. (2020) 12:S37–47. doi: 10.21037/jtd.2019.12.84
49. Vincent JL. Fluid management in the critically ill. Kidney Int. (2019) 96:52–7. doi: 10.1016/j.kint.2018.11.047
50. Uchimido R, Schmidt EP, Shapiro NI. The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care. (2019) 23:16. doi: 10.1186/s13054-018-2292-6
51. Cartotto R, Burmeister DM, Kubasiak JC. Burn shock and resuscitation: review and state of the science. J Burn Care Res. (2022) 26:irac025. doi: 10.1093/jbcr/irac025
52. Tan J, Zhou J, Li N, Yuan L, Luo G, A. New resuscitation formula based on burn index provides more reliable prediction for fluid requirement in adult major burn patients. J Burn Care Res. (2021) 42:962–7. doi: 10.1093/jbcr/irab013
53. Alvarado R, Chung KK, Cancio LC, Wolf SE. Burn resuscitation. Burns. (2009) 35:4–14. doi: 10.1016/j.burns.2008.03.008
54. Aboelatta Y, Abdelsalam A. Volume overload of fluid resuscitation in acutely burned patients using transpulmonary thermodilution technique. J Burn Care Res. (2013) 34:349–54. doi: 10.1097/BCR.0b013e3182642b32
Keywords: burn, sepsis, resuscitation, outcomes, complications, bibliometric analysis
Citation: Zhou D, He L, Shi W and Ma P (2025) Lessons from the similarities and differences in fluid resuscitation between burns and sepsis: a bibliometric analysis. Front. Med. 12:1561619. doi: 10.3389/fmed.2025.1561619
Received: 16 January 2025; Accepted: 13 February 2025;
Published: 04 March 2025.
Edited by:
You Shang, Huazhong University of Science and Technology, ChinaReviewed by:
Zhou Feihu, Chinese PLA General Hospital, ChinaCopyright © 2025 Zhou, He, Shi and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Penglin Ma, bWFwZW5nbGluMUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.