
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 06 March 2025
Sec. Nephrology
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1558628
Purpose: This study examined the association between the Life’s Crucial 9 (LC9) score and kidney stone prevalence in U.S. adults.
Methods: Using data from the National Health and Nutrition Examination Survey (NHANES) spanning 2007 to 2014, this cross-sectional analysis focused on adult participants with kidney stone onset or recurrence. LC9 scores were divided into four quartiles for analysis. Weighted multivariable logistic regression, restricted cubic spline (RCS) modeling, threshold effect analysis, and subgroup analyses were employed to evaluate the relationship between LC9 scores and kidney stone prevalence.
Results: The study included 24,669 participants with an average age of 46.05 ± 0.34 years and a mean LC9 score of 73.76 ± 0.25. The overall prevalence of kidney stones was 8.45%, while the average recurrence rate stood at 2.96%. Importantly, for each one-point increase in the LC9 score, the incidence of kidney stones dropped by 1.2% (95% CI: 0.979 to 0.997, p = 0.014). Compared to the lowest quartile (Q1), the Q4 group exhibited a 0.305-fold higher recurrence rate (95% CI: 0.159 to 0.586, p < 0.001). Interaction analysis showed that race and gout significantly influenced the relationship between the LC9 score and kidney stone risk. Additionally, curve fitting and threshold effect analysis demonstrated a nonlinear association between LC9 scores and kidney stone recurrence, with a breakpoint identified at 72.777.
Conclusion: An elevated LC9 score correlates with a lower risk of both kidney stone formation and recurrence. Maintaining an optimal LC9 score could be an effective approach for preventing kidney stones.
Kidney stones are a prevalent urological condition, impacting around 10–12% of the global population, with incidence rates steadily increasing in recent decades (1). In the United States, the prevalence has grown from 3.8% in the 1970s to nearly 10% in recent years, disproportionately affecting men and older adults (2). Metabolic factors, including obesity, diabetes, hypertension, and a higher occurrence of cardiovascular events, are closely linked to kidney stone formation (3). Previous research has shown a bidirectional link between kidney stone formation and cardiovascular health (CVH) (4). Life’s Essential 8 (LE8), developed by the American Heart Association, includes eight critical health factors: diet, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, glucose levels, and blood pressure. These factors are widely used to assess CVH (5). Recently, Life’s Crucial 9 (LC9) was introduced as an expansion of the LE8 framework by adding mental health as a crucial component (6). This adjustment recognizes the significant role that mental health, particularly depression, plays in influencing cardiovascular health and overall well-being. The LC9 score, therefore, includes the same eight factors as LE8, along with the addition of depression, making it a more comprehensive measure of overall health.
The link between LC9 and both the incidence and recurrence of kidney stones has yet to be fully explored. To address this, we analyzed data from the extensive National Health and Nutrition Examination Survey (NHANES) to explore how the LC9 score affects the prevalence and recurrence of kidney stones, thereby building on the relationship between cardiovascular health and kidney stones.
NHANES evaluates the health and nutritional status of U.S. children and adults through a stratified, multistage sampling method (7). Conducted by the Centers for Disease Control (CDC), the survey collects vital data on demographics, diet, and health. The studies involving human participants were reviewed and approved by the National Center for Health Statistics (NCHS) Ethics Review Board. Informed consent was obtained from all individual participants enrolled in the study. This study follows Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement.
We initially analyzed NHANES data from 2007 to 2014, which included 40,617 participants. The study excluded several groups: individuals under 20 years old and pregnant participants (n = 17,383), those missing data on kidney stones or LC9 scores (n = 455), and participants with incomplete covariate information (n = 5,555). Ultimately, the final analysis comprised 11,531 participants (Figure 1).
The LC9 score was calculated as the average of the eight LE8 components and the depression score (8). The depression score, derived from the Patient Health Questionnaire-9 (PHQ-9), classifies depressive symptoms into scores of 100, 75, 50, 25, and 0, corresponding to PHQ-9 ranges of 0–4, 5–9, 10–14, 15–19, and 20–27, respectively (9). The LE8 score includes four health behaviors—diet, physical activity, nicotine exposure, and sleep duration—and four health factors: BMI, lipids, blood glucose, and blood pressure. Dietary data were collected through a 24-h diet recall and assessed using the Healthy Eating Index 2015 (HEI-2015) (10). Data on physical activity, nicotine exposure, sleep duration, and diabetes status were obtained from questionnaires, while laboratory and MEC data were used to measure lipids, blood glucose, weight, height, and blood pressure. Supplementary Table S1 provides detailed information on the LE8 scoring algorithms used in the NHANES data.
The diagnosis of nephrolithiasis was determined by asking participants, “Have you/the sample person ever had nephrolithiasis?” Those who answered “yes” were classified as having a history of the condition. Participants who reported experiencing nephrolithiasis two or more times in response to the question, “How many instances of nephrolithiasis did you experience?” were categorized as having recurrent nephrolithiasis. This diagnostic method is consistent with prior research (11).
We gathered data through standardized questionnaires and measurements, adjusting for multiple covariates to enhance the robustness of our analysis. Demographic variables included age, gender, race, education level, marital status, and the poverty-to-income ratio (PIR). Lifestyle factors encompassed smoking and alcohol consumption, categorized as: Never (fewer than 12 lifetime drinks), Ever (12 or more drinks in a single year or lifetime but not in the past year), and Now (currently consuming 12 or more drinks annually). Physical activity was measured by task intensity in metabolic equivalent (MET) minutes and classified as either <500 or ≥ 500 MET minutes per week. Health-related variables included BMI, hypertension, diabetes, cardiovascular diseases (CVD), and self-reported histories of gout and cancer (12).
Following NHANES guidelines, we combined four survey cycles using complex sampling weights (MEC examination weight). Statistical analyses included survey-weighted logistic regression for continuous variables (mean and standard error, SE) and survey-weighted chi-square tests for categorical variables (counts and percentages). To investigate the relationship between LC9 score—analyzed as both a continuous and categorical variable (quartiles)—and kidney stone occurrence and recurrence rates, we applied multinomial logistic regression across three models: Model 1 (unadjusted), Model 2 (adjusted for age, sex, and race), and Model 3 (further adjusted for marital status, PIR, education, smoking, alcohol use, diabetes, BMI, hypertension, CVD, energy intake, physical activity, gout, and cancer). Trend tests were also conducted. We used restricted cubic spline (RCS) regression to explore the relationship between LC9 scores and kidney stone prevalence and recurrence. RCS is a technique that allows us to model complex, non-linear relationships by using multiple curve segments. This method helps us understand how changes in LC9 scores might have varying effects at different levels of the score, rather than assuming a simple straight-line relationship, with nodes placed at the 10th, 50th, and 90th percentiles of the LC9 score distribution. Additionally, we applied piecewise linear regression to investigate whether the effect of LC9 on kidney stone recurrence changes at a certain threshold. This means we tested whether there is a specific point, called the ‘inflection point,’ where the relationship between LC9 scores and kidney stone recurrence shifts significantly. This approach helps to identify potential breaks in the trend that would not be captured by a simple linear model. Interaction tests assessed heterogeneity between subgroups. All statistical analyses were performed using R version 4.3, with a p-value <0.05 considered statistically significant.
Table 1 displays the weighted demographic characteristics of 24,669 participants stratified by LC9 quartiles, with 51.22% male and 48.78% female. The average age was 46.05 ± 0.34 years. Compared to Q1, individuals in the Q4 group were younger, had lower BMI, fewer instances of divorce, separation, or widowhood, higher education levels, and greater financial stability. Although smoking rates were relatively low, alcohol consumption was higher, and the prevalence of underlying diseases was lower. Higher LC9 scores were linked to a reduced risk of kidney stone occurrence and recurrence.
In the fully adjusted model, each one-point increase in LC9 was linked to a 1.2% reduction in kidney stone risk (95% CI: 0.979–0.997, p = 0.014). Quartile analysis revealed that participants in the highest LC9 quartile (Q4) had a 0.636-fold lower risk of kidney stones compared to those in the lowest quartile (Q1). For kidney stone recurrence, model 3 indicated non-significant results when LC9 was treated as a continuous variable, suggesting a potential nonlinear association. However, quartile analysis showed that individuals in Q4 had a 0.305-fold lower recurrence rate than those in Q1 in the fully adjusted model (p for trend = 0.006) (Table 2).
The RCS analysis showed a negative linear relationship between LC9 and kidney stone occurrence (Figure 2A). In contrast, a nonlinear association was identified for kidney stone recurrence (Figure 2B). A comparison of standard and piecewise linear models revealed a significant LC9 effect (p < 0.05) in the likelihood ratio test. Using a piecewise linear model and recursive algorithm, the LC9 inflection point was determined to be 70.556 (Table 3). Beyond this threshold, each unit increase in LC9 corresponded to a 5.6% reduction in kidney stone risk (OR: 0.994, 95% CI: 0.914–0.972).
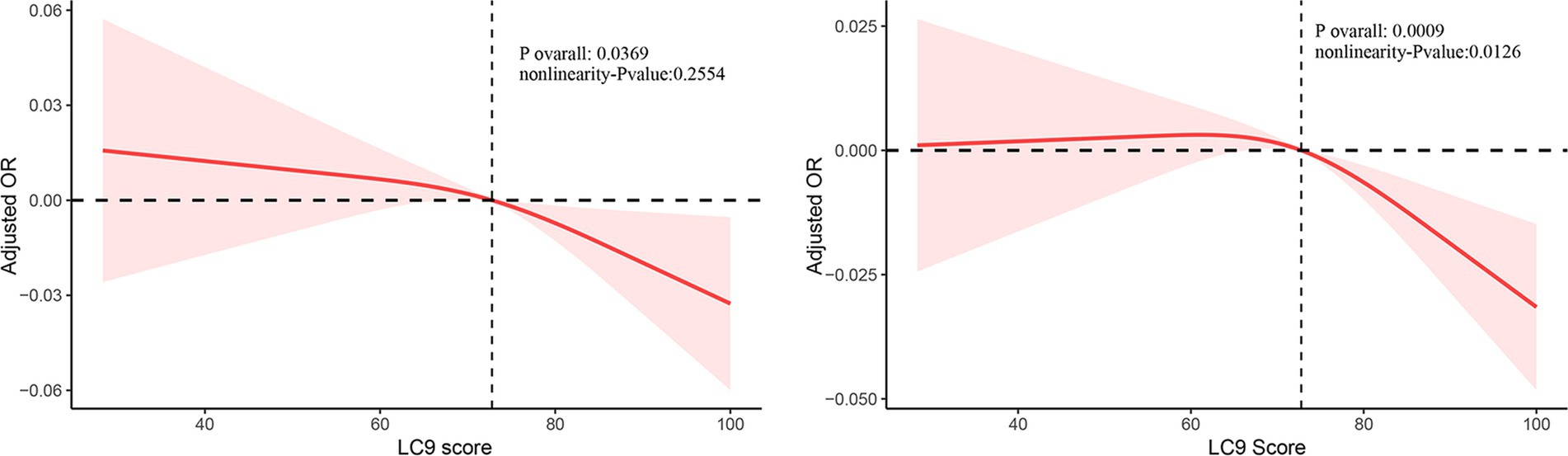
Figure 2. Restricted cubic spline of the association between LC9 score and kidney stone adjusted for all covariates.
Subgroup analyses revealed that race modified the relationship between LC9 and kidney stones after adjusting for other covariates. The odds ratios for the Q4 group compared to Q1 were 0.281 for Mexican Americans, 0.223 for other Hispanics, 0.756 for non-Hispanic whites, 0.558 for non-Hispanic Blacks, and 0.223 for individuals of other races, with a p-value for interaction of 0.044. Additionally, both race and gout were identified as modifiers for kidney stone recurrence, with interaction p-values of 0.003 and 0.012, respectively (Supplementary Table S2).
The LC9 score builds upon the LE8 framework, aiming to improve the development and evaluation of integrated cardiovascular care models that incorporate mental health management. This study investigates the association between the newly developed LC9 score and both the incidence and recurrence of kidney stones in adults. The results demonstrate that higher LC9 scores are inversely related to the risk of kidney stone formation. These findings highlight the potential benefit of further exploring integrated health behaviors and factors that may help prevent kidney stones.
Our study evaluated the predictive value of multidimensional LC9 measures in reducing the risk of kidney stones and highlighted the synergistic impact of depression on cardiovascular health. Previous research has shown that adequate fluid intake (13), a balanced diet (14), low fat (15), moderate physical activity (16), smoking cessation (17), maintaining normal sleep duration (18), and mental well-being are effective strategies to lower the risk of kidney stones (19). Our findings further underscore the importance of comprehensively assessing these behaviors.
Dietary factors significantly influence both the formation and recurrence of kidney stones. Research has shown that high consumption of calcium, oxalate, and animal protein increases the risk of kidney stone development (20). On the other hand, increasing fluid intake appropriately can dilute calcium oxalate, uric acid, and other urinary components, reducing the likelihood of stone formation (21). Physical activity may lower the risk of kidney stones by enhancing urinary metabolism. This effect is likely due to improved calcium metabolism and better bone health, which decrease calcium salt deposition in the urine (22). Depression, recently added as a component of the LC9 score, also merits further exploration in this context. It may indirectly contribute to kidney stone risk through lifestyle factors (e.g., poor diet, physical inactivity) and physiological changes, such as elevated stress hormone levels (19). BMI, blood glucose, non-HDL cholesterol, and blood pressure are also linked to kidney stone formation. Elevated BMI is associated with higher levels of uric acid and oxalate, increasing the risk of stone development. This study found that maintaining a healthy BMI significantly lowers the risk of kidney stones. Additionally, managing blood glucose and blood pressure may reduce the likelihood of stone formation by minimizing renal metabolic stress (23).
Stratified analysis identified an interaction between ethnicity and the LC9 score in relation to both kidney stone occurrence and recurrence. This interaction may result from various factors, including genetic predisposition, physiological differences, mental health, socioeconomic conditions, and cultural practices. Furthermore, an interaction was observed between gout and the LC9 score concerning kidney stone recurrence. Tailored interventions for gout patients, focusing on dietary management and mental health, could help lower the risk of recurrent kidney stones.
Our study underscores the potential of the LC9 score in fostering interdisciplinary collaboration, particularly between urologists and cardiologists (8, 24). By highlighting lifestyle factors associated with cardiovascular disease risk, the LC9 score serves not only as a predictor for cardiovascular conditions but also as a preventive tool for kidney stones. Integrating this score into routine health assessments could improve early detection and intervention. However, the cross-sectional nature of our research limits the ability to draw causal conclusions. Future studies should focus on larger prospective cohorts to validate the relationship between the LC9 score and kidney stone risk and to explore its clinical utility in personalized health management across diverse populations.
While our study demonstrates that higher LC9 scores are associated with a lower risk of kidney stones, further research is needed to clarify the causal relationship between LC9 and kidney stone formation. Prospective cohort studies and randomized controlled trials would provide stronger evidence to support these findings. Additionally, future research could explore how integrating the LC9 score into clinical practice might guide personalized prevention strategies for kidney stones, particularly in individuals at higher cardiovascular risk. These findings could also inform public health recommendations aimed at promoting cardiovascular health and preventing kidney stones through lifestyle modifications.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving humans were reviewed and approved by the NCHS Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
X-rL: Conceptualization, Writing – original draft. H-lL: Writing – original draft, Validation. LW: Writing – original draft, Writing – review & editing. J-wY: Conceptualization, Methodology, Writing – review & editing. K-yW: Data curation, Project administration, Writing – review & editing. S-yC: Resources, Writing – original draft. LY: Project administration, Supervision, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 82160146).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1558628/full#supplementary-material
1. Chewcharat, A, and Curhan, GJU. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis. (2021) 49:27–39. doi: 10.1007/s00240-020-01210-w
2. Scales, CD Jr, Smith, AC, Hanley, JM, and Saigal, CSUrology UDiAPJE. Prevalence of kidney stones in the United States. Eur Urol. (2012) 62:160–5. doi: 10.1016/j.eururo.2012.03.052
3. Ferraro, PM, Taylor, EN, Eisner, BH, Gambaro, G, Rimm, EB, Mukamal, KJ, et al. History of kidney stones and the risk of coronary heart disease. JAMA. (2013) 310:408–15. doi: 10.1001/jama.2013.8780
4. Alexander, RT, Hemmelgarn, BR, Wiebe, N, Bello, A, Samuel, S, Klarenbach, SW, et al. Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol. (2014) 9:506–12. doi: 10.2215/CJN.04960513
5. Lloyd-Jones, DM, Allen, NB, Anderson, CA, Black, T, Brewer, LC, Foraker, RE, et al. Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. (2022) 146:e18–43. doi: 10.1161/CIR.0000000000001078
6. Gaffey, AE, Rollman, BL, and Burg, MMJC. Strengthening the pillars of cardiovascular health: psychological health is a crucial component. Circulation. (2024) 149:641–3. doi: 10.1161/CIRCULATIONAHA.123.066132
7. Control CfD, Prevention. National Health and Nutrition Examination Survey: 2007–2012 Data Documentation, Codebook, and Frequencies. (2018).
8. Ge, J, Peng, W, and Lu, J. Predictive value of Life's crucial 9 for cardiovascular and all-cause mortality: a prospective cohort study from the NHANES 2007 to 2018. J Am Heart Assoc. (2024) 13:e036669. doi: 10.1161/JAHA.124.036669
9. Zhang, Z, Jackson, SL, Gillespie, C, Merritt, R, and Yang, QJJNO. Depressive symptoms and mortality among US adults. JAMA Netw Open. (2023) 6. doi: 10.1001/jamanetworkopen.2023.37011
10. Krebs-Smith, SM, Pannucci, TE, Subar, AF, Kirkpatrick, SI, Lerman, JL, Tooze, JA, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. (2018) 118:1591–602. doi: 10.1016/j.jand.2018.05.021
11. Pan, J, Li, C, Zhang, J, Sun, Z, Yu, X, Wan, Q, et al. Association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and diabetic kidney disease in patients with diabetes in the United States: a cross-sectional study. Lipids Health Dis. (2024) 23:317. doi: 10.1186/s12944-024-02308-5
12. Yin, S, Yang, Z, Zhu, P, Du, Z, Yu, X, Tang, T, et al. Association between added sugars and kidney stones in US adults: data from National Health and nutrition examination survey 2007–2018. Front Nutr. (2023) 10:1226082. doi: 10.3389/fnut.2023.1226082
14. Ferraro, PM, Bargagli, M, Trinchieri, A, and Gambaro, G. Risk of kidney stones: influence of dietary factors, dietary patterns, and vegetarian-vegan diets. Nutrients. (2020) 12. doi: 10.3390/nu12030779
15. Hung, JA, Li, CH, Geng, JH, Wu, DW, and Chen, SC. Dyslipidemia increases the risk of incident kidney stone disease in a large Taiwanese population follow-up study. Nutrients. (2022) 14. doi: 10.3390/nu14071339
16. Feng, X, Wu, W, Zhao, F, Xu, F, Han, D, Guo, X, et al. Association between physical activity and kidney stones based on dose-response analyses using restricted cubic splines. Eur J Pub Health. (2020) 30:1206–11. doi: 10.1093/eurpub/ckaa162
17. Huang, Y, Wang, H, Xu, C, Zhou, F, Su, H, and Zhang, Y. Associations between smoke exposure and kidney stones: results from the NHANES (2007-2018) and Mendelian randomization analysis. Front Med. (2023) 10:1218051. doi: 10.3389/fmed.2023.1218051
18. Yin, S, Wang, J, Bai, Y, Yang, Z, Cui, J, and Wang, J. Association between sleep duration and kidney stones in 34 190 American adults: a cross-sectional analysis of NHANES 2007-2018. Sleep Health. (2022) 8:671–7. doi: 10.1016/j.sleh.2022.08.003
19. Wang, M, Jian, Z, Ma, Y, Jin, X, Li, H, and Wang, K. Depression increases the risk of kidney stone: results from the National Health and nutrition examination survey 2007-2018 and Mendelian randomization analysis. J Affect Disord. (2022) 312:17–21. doi: 10.1016/j.jad.2022.06.008
20. Taylor, EN, Stampfer, MJ, and Curhan, GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. (2004) 15:3225–32. doi: 10.1097/01.ASN.0000146012.44570.20
21. Parivar, F, Low, RK, and MLJTJou, S. The influence of diet on urinary stone disease. J Urol. (1996) 155:432–40. doi: 10.1016/S0022-5347(01)66411-5
22. Aune, D, Mahamat-Saleh, Y, Norat, T, and EJEjoe, R. Body fatness, diabetes, physical activity and risk of kidney stones: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. (2018) 33:1033–47. doi: 10.1007/s10654-018-0426-4
23. Yuan, S, and Larsson, SC. Assessing causal associations of obesity and diabetes with kidney stones using Mendelian randomization analysis. Mol Genet Metab. (2021) 134:212–5. doi: 10.1016/j.ymgme.2021.08.010
Keywords: kidney stone, Life’s crucial 9, NHANSE, cardiovascular health, depression
Citation: Li X-r, Liu H-l, Wang L, Yang J-w, Wang K-y, Chen S-y and Yang L (2025) Association between life’s crucial 9 and kidney stones: a population-based study. Front. Med. 12:1558628. doi: 10.3389/fmed.2025.1558628
Received: 10 January 2025; Accepted: 24 February 2025;
Published: 06 March 2025.
Edited by:
Piergiorgio Messa, University of Milan, ItalyReviewed by:
Hongyang Jiang, Huazhong University of Science and Technology, ChinaCopyright © 2025 Li, Liu, Wang, Yang, Wang, Chen and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Si-yu Chen, MTQzMjk5NjA0MkBxcS5jb20=; Li Yang, ZXJ5X3lhbmdsaUBsenUuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.