
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 03 March 2025
Sec. Geriatric Medicine
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1534828
This article is part of the Research Topic Optimizing Medication Management in Older Adults: Addressing Polypharmacy, Deprescribing and Represcribing Challenges View all 3 articles
 Mohammed M. Alsultan1*
Mohammed M. Alsultan1* Solaiman M. Alhawas2
Solaiman M. Alhawas2 Leena H. Alhajri1
Leena H. Alhajri1 Khalid A. Alamer1
Khalid A. Alamer1 Abdullah K. Alahmari3
Abdullah K. Alahmari3 Amani M. AlQarni4
Amani M. AlQarni4 Feras A. Al-Awad5
Feras A. Al-Awad5Objective: To examine the prevalence of potentially inappropriate medications (PIMs) prescribed among older patients diagnosed with psychiatric diseases and to identify associated factors.
Methods: This cross-sectional study was conducted among older patients who visited outpatient clinics in Saudi Arabia between June 1st, 2019, and May 31st, 2023. PIMs use was estimated using the updated 2019 American Geriatric Society (AGS) Beers criteria. Data were analyzed using chi-square or Fisher's exact test for categorical variables and t-test for continuous variables to compare patients with and without PIMs. In addition, the Pearson correlation test was performed between the total number of prescriptions and the number of PIMs. Multivariable logistic regression analysis was used to explore PIMs. Statistical significance was set at p < 0.05.
Results: Our study included 306 patients with psychiatric diseases, with 156 (50.98%) in the PIMs group and 150 (49.02%) in the non-PIMs group. There was a considerable positive correlation between the total number of prescriptions and the number of PIMs (r = 0.76; p < 0.0001). The adjusted logistic regression analysis revealed a significantly higher risk of PIMs use in individuals with psychiatric diseases and comorbid neurological diseases compared to those without [adjusted odds ratio (AOR) = 2.48, 95% CI [1.15–5.32]]. In contrast, the risk of PIMs use was not significantly greater for older individuals with psychiatric diseases and comorbid hypertension {AOR = 1.67, 95% CI [(0.79–3.54)]}, diabetes mellitus {AOR = 1.25, 95% CI [(0.66–2.34)]}, or pulmonary disease {AOR = 2.34, 95% CI [(0.69–7.96)]}.
Conclusion: This study highlighted the elevated number of PIMs in older adults with psychiatric diseases in the outpatient setting, particularly those with comorbid neurological diseases. Therefore, clinical pharmacists may play a crucial role in improving the outcomes of patients diagnosed with psychiatric illnesses. Finally, future studies should examine additional strategies to reduce the use of PIMs in this population.
Rational drug therapy is crucial for older adults to effectively manage their health (1). Worldwide, the percentage of aging individuals is projected to increase to 16% by 2050, with a 6% increase compared to 2022 (2). By 2030, older individuals will comprise ~4.63 million of the anticipated total population of the Kingdom of Saudi Arabia, which is projected to be 39.5 million (3).
Unfortunately, up to 20–30% of hospital admissions for older individuals are because of drug-related problems, which frequently result in greater risks of morbidity, mortality, illness, frailty, and higher healthcare costs (4–6). However, chronic illnesses and alterations in the pharmacokinetics and pharmacodynamics, such as delayed renal elimination of drugs and increased sensitivity to anticholinergic and sedating effects are frequently linked to aging (7–9). Additionally, as the prevalence of multimorbidity among older individuals increases, polypharmacy and the use of potentially inappropriate medications (PIMs) are becoming more prevalent in geriatric populations (10). PIMs are sometimes indispensable, necessitating their use despite associated risks. However, PIMs can be replaced with better-tolerated alternatives whose predicted clinical benefits exceed their risk of adverse drug events when administered to older patients (11).
PIMs are frequently occurring medication-related problems that affect older patients. Common scales and criteria are used to evaluate the usage of PIMs, including the Beers criteria, which are a set of precise standards for identifying PIMs that were developed in 1991 and have since been updated (12, 13). Although the factors associated with inappropriate medication use differ, various studies have linked the risk of PIMs to factors such as age, sex, use of multiple medications, and the number of comorbid conditions (14, 15). One systematic review evaluated factors associated with PIMs use in community-dwelling older adults in the United States. The study reported that taking more drugs, female sex, and higher outpatient and emergency department utilization were the most observed statistically significant factors associated with PIMs use (16). Moreover, older adults with specific chronic diseases such as diabetes, hypertension, depression, osteoporosis, and dementia are more likely to use PIMs than those who do not have these diseases (17, 18).
Multiple studies have been conducted to determine the prevalence of and factors associated with PIMs using Beers Criteria. According to the 2012 Beers Criteria, the prevalence of PIMs in European countries ranged from ~22% to 44% (19–21). Additionally, studies conducted in India, the United States, and Brazil indicated that the prevalence of PIMs among older patients ranged from 29.3% to 59.2% (22–24). In Middle Eastern countries, using the 2015 Beers criteria, 62.5% of patients had at least one prescribed PIMs in Jordan, while the application of the 2019 Beers criteria in the Gulf countries indicated a prevalence of ~34.7% to 62.6% (25–28).
In Saudi Arabia, the prevalence of PIMs was reported to be 19% using the 2012 Beers criteria, whereas it increased to around 60% when utilizing the 2015 Beers criteria (29–31). More recent studies using the 2019 Beers criteria indicated that the prevalence of PIMs among individuals with various chronic diseases ranged from 48.6% to 66.6% (32–36). Although these studies have highlighted a significant risk of PIMs in Saudi Arabia for diseases such as diabetes, dyslipidemia, and anxiety, none specifically examined the issue in the context of comprehensive psychiatric diseases. Therefore, this study aimed to investigate the prevalence of PIMs prescribed to older patients in Saudi Arabia who are diagnosed with psychiatric diseases and to identify the associated factors.
This study was approved by the Institutional Review Board of the Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB-2024-01-200). This study was performed in accordance with the standards of the 1964 Declaration of Helsinki and its later amendments.
This was a retrospective cross-sectional study conducted between 1st June 2019, and 31st May 2023.
Patient data were extracted from the Electronic Medical Records (EMRs) of older patients who visited the outpatient clinic at King Fahad Teaching Hospital, Khobar, Saudi Arabia. The database contains information on patient demographic variables, such as age, and sex. Data regarding medical diagnoses and prescribed drugs, including the date of each diagnosis, and drugs were extracted. The inclusion criteria were individuals aged 65 years and older, who were diagnosed with at least one psychiatric disease, such as mood disorders, anxiety, schizophrenia, or other psychiatric diseases, based on the International Classification of Diseases, Tenth Revision (ICD-10) codes (Appendix-1).
The outcome of our study was to estimate PIMs using the updated 2019 AGS Beers criteria to classify PIMs use. We categorized medications that older adults should avoid or use with caution according to the 2019 Beers criteria. Additionally, we categorized the prevalence of PIMs use into three categories: one PIM, two PIMs, and three or more PIMs. Furthermore, PIMs users were classified into two categories: PIMs users, who were prescribed at least one or more PIMs, and non-PIMs users, who had no prescription for PIMs (13). The covariates included in our study were demographic variables, including age, sex, and comorbidities including neurological diseases, hypertension (HTN), diabetes mellitus (DM), kidney disease, liver disease, dyslipidemia, cancer, and pulmonary disease (Appendix-1). In addition, we evaluated the relationship between the total number of prescriptions and the number of PIMs.
Descriptive data were utilized to examine the baseline characteristics of patients with PIMs and those without. Categorical variables were presented as frequency and percentage and were assessed using the chi-square or Fisher's exact test, as appropriate. Continuous variables were presented as means and standard deviations (SD) and assessed using student t-tests. Pearson correlation (r) test was performed to assess the strength and direction between the total number of prescriptions and the number of PIMs. Furthermore, multivariable logistic regression was used to explore PIMs, and the goodness of fit was checked using the Hosmer-Lemeshow test. The adjusted odds ratio (AOR) along with its confidence interval at 95% (95% CI) were presented. The statistical significance was set at p < 0.05. The SAS software (version 9.4) was used to analyze the data.
The total number of individuals in our study was 306 older adults diagnosed with psychiatric disease, with 156 (50.98%) in the PIMs group and 150 (49.02%) in the non-PIMs group, as shown in Figure 1.
The average age of PIMs users was 73.09 ± 6.55 years, whereas non-PIMs users had an average age of 73.87 ± 7.07 years. Among the participants, there were 197 females (64.38%) and 109 males (35.62%), showing no significant difference between the two groups. In addition, PIMs users had a higher rate of various health comorbidities such as neurological diseases (8.17% vs. 4.25%), hypertension (9.80% vs. 6.54%), diabetes mellitus (11.76% vs. 7.84%), liver diseases (2.29% vs. 1.31%), dyslipidemia (4.90% vs. 4.25%), and pulmonary disease (3.92% vs. 1.31%) compared to non-PIMs users, as detailed in Table 1.
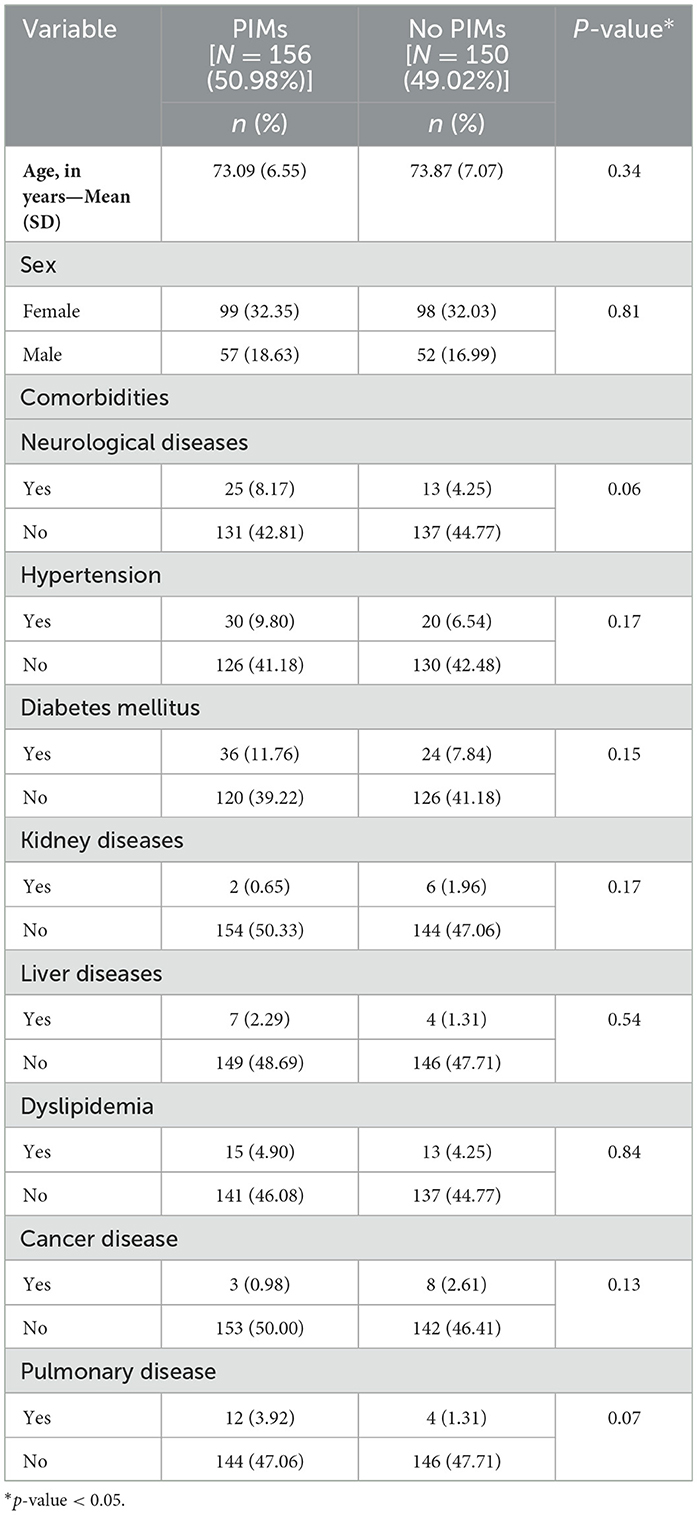
Table 1. Baseline characteristics of older patients with psychiatric disease using PIMs and non-PIMs.
The prevalence of individuals with PIMs that should be avoided in older patients diagnosed with psychiatric disease was (50.98%) whereas the prevalence of individuals with PIMs requiring caution was (84.97%), as shown in Figure 2. Furthermore, the prevalence of medications that should be avoided and used with caution among psychiatric patients was one PIM (51.92% vs. 48.07%), two PIMs (25% vs. 30%), and three or more PIMs (23.08% vs. 21.92%), as displayed in Figure 3. There is a strong positive correlation between the total number of prescriptions and the number of PIMs (r = 0.76; p < 0.0001).
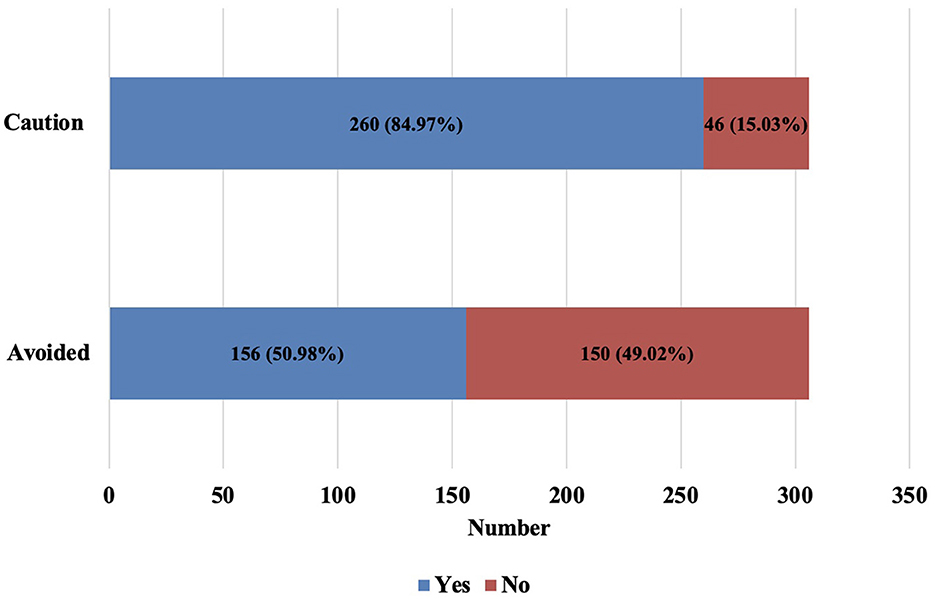
Figure 2. Prevalence of PIMs that should be avoided and used with caution among older with psychiatric diseases.
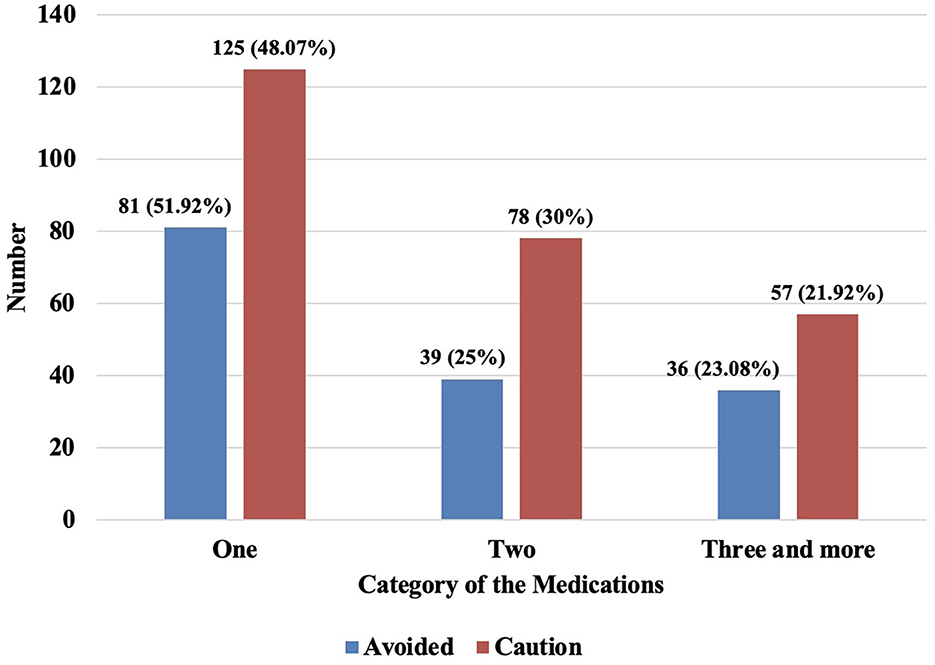
Figure 3. Numbers of PIMs that should be avoided and used with caution among older with psychiatric diseases.
The most frequently prescribed PIMs to avoid were antipsychotics and antidepressants, while the least prescribed were antimanic, skeletal muscle relaxants, and antihypertensives. On the other hand, we observed that antidepressants, were prescribed more frequently followed by antipsychotic drugs than other classes of medications that should be used with caution (see Table 2). In addition, 45.1% of patients were found to have PIMs because of combination of ≥3 Central Nervous System (CNS)-active drugs.
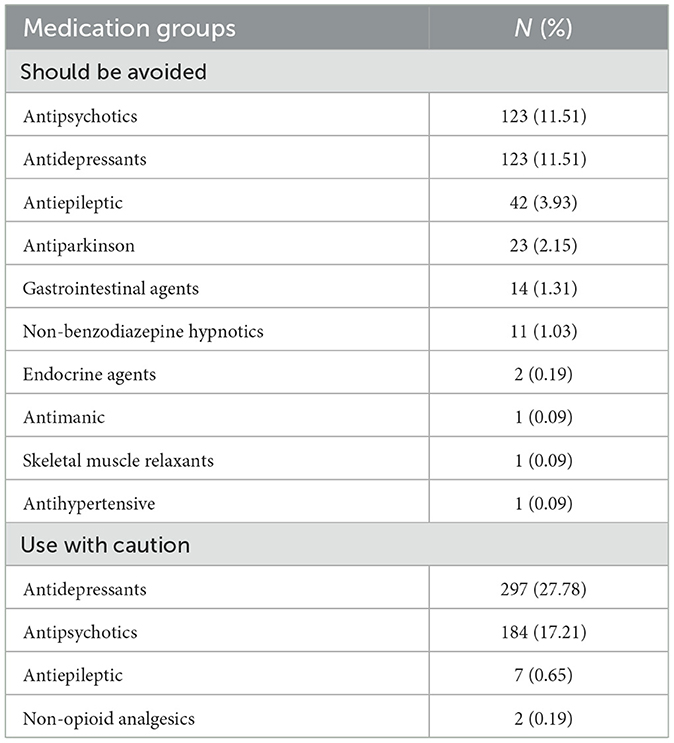
Table 2. Potentially inappropriate medications to be avoided and used with caution among older patients with psychiatric diseases.
The adjusted logistic regression analysis revealed a significantly higher risk of PIMs use in individuals with psychiatric diseases and comorbid neurological disease compared to those without comorbid neurological diseases (AOR = 2.48, 95% CI [1.15–5.32]). However, increased risk of PIMs was not observed for females (AOR = 0.93, 95% CI [0.57–1.52]), patients with hypertension {AOR = 1.67, 95% CI [(0.79–3.54)]}, diabetes mellitus {AOR = 1.25, 95% CI [(0.66–2.34)]}, kidney diseases {AOR = 0.25, 95% CI [(0.05–1.37)]}, liver diseases {AOR = 1.23, 95% CI [(0.31–4.94)]}, dyslipidemia {AOR = 0.79, 95% CI [(0.32–1.96)]}, cancer {AOR = 0.38, 95% CI [(0.10–1.49)]}, and pulmonary diseases {AOR = 2.34, 95% CI [(0.69 −7.96)]} in comparison to those without these diseases (see Table 3).
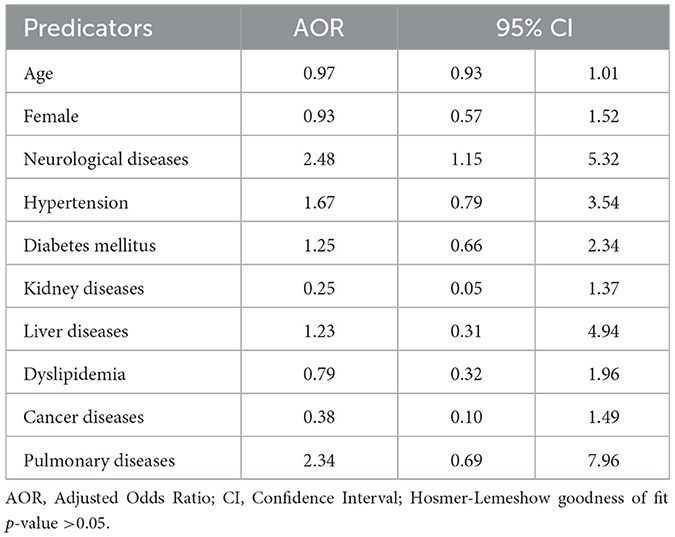
Table 3. Adjusted logistic regression of potentially inappropriate medications among older patients with psychiatric diseases.
In this study, we assessed the prevalence of PIMs prescribed to older patients in Saudi Arabia diagnosed with psychiatric diseases in the outpatient setting. Our findings indicated that the prevalence of PIMs, which include medications that should be avoided or used with caution was notably high. Psychotropic drugs (i.e., antidepressants and antipsychotics) were the most prescribed PIMs. Most patients with PIMs were found to have ≥3 CNS-active drugs. In addition, the risk of PIMs use was higher among patients with psychiatric disease and comorbid neurological disease.
The prevalence of PIMs in our study was 50.98% for those drugs that should be avoided while 84.97% for drugs that should be used with caution. This high prevalence is in line with other studies of older individuals diagnosed with psychiatric diseases; 63% for medications that should be avoided and 81% for medications that should be used with caution (35, 37). Similar to another study among Saudi Arabian individuals with anxiety disorders, the use of one PIM or less was higher than the use of two or more medicines (35). However, our findings are inconsistent with another study that reported a high prevalence of PIMs (>90%) for drugs that should be avoided or those used with caution. This discrepancy might be related to the study setting (inpatient) and/or study population who had schizophrenia and bipolar disorders (38).
In complex situations, the use of PIMs cannot be avoided in older patients with psychiatric diseases. In other cases, PIMs use can be minimized or replaced with better-tolerated alternatives (11). Previous studies reported at least one potentially inappropriate duplicate therapy or PIMs among 43.1%−46.7% of older patients with psychiatric diseases (39, 40). In addition, drug interactions in older patients with psychiatric diseases were found to be frequently encountered (41). Several studies reported that commonly prescribed antidepressants, antipsychotics, and/or CNS-active drugs were classified as PIMs (42–44). In addition, the updated 2019 AGS Beers criteria strongly recommends avoiding a combination of ≥3 CNS-active drugs (13). This may explain the high number of PIMs identified in our study.
This study highlights the need for urgent interventions to improve medication use in older patients with psychiatric diseases who have comorbid neurological diseases requiring multiple CNS-active drugs. The availability of clinical pharmacists in the primary care setting has been reported to reduce medication prescribing including PIMs in older patients with psychiatric diseases (45). In addition, the interdisciplinary medication reviews led by clinical pharmacists may have a potential role in minimizing the number of PIMs that are not indicated, contraindicated, or have significant drug-drug interactions (46, 47). These interventions are crucial for optimizing patient care for the subgroup mentioned earlier. Additionally, literature reported that preventable adverse drug events constitute a large burden on healthcare expenditure and can be minimized with pharmacist-led medication reviews (48–50). Moreover, counseling older patients on medication management during illness may improve appropriate drug use (51). Future studies should examine the effectiveness of other strategies including the implementation of alerts within computerized provider order entry (CPOE), hospital disease management guidelines, and educational activities in this population (52).
To the best of our knowledge, this is the first study in Saudi Arabia to use the 2019 Beers Criteria and comprehensively include psychiatric diseases in older individuals. Second, the study had a long study duration and explored PIMs use predictors. Finally, this study investigated the number of PIMs used per patient, which should be avoided and used cautiously in older patients with psychiatric diseases. Nonetheless, the study does have some limitations. First, the study was limited to a single center in Saudi Arabia and therefore, the study findings cannot be extrapolated to other centers. Second, the study was limited by its retrospective nature. Since ICD-10 classification has limitations with regard to the exact definition of depression and differentiating between bipolar subtypes, we only included codes with confirmed depression and bipolar diagnoses (53, 54). Third, the EMRs did not record patients' usage of over-the-counter medications, which may have had an impact on the prevalence rate of PIMs use. Finally, the missing data in EMRs may have led to bias in our study.
This study highlighted the elevated number of PIMs in older adults with psychiatric diseases in the outpatient setting especially those with comorbid neurological diseases. Therefore, clinical pharmacists may play a significant role in improving the outcomes of patients diagnosed with psychiatric diseases. Finally, future studies should examine other strategies to reduce PIMs in this population.
The datasets presented in this article are not readily available because the data that supports the findings of this study are available from the corresponding author upon reasonable request. Requests to access the datasets should be directed to Mohammed M. Alsultan, bW1hYWxzdWx0YW5AaWF1LmVkdS5zYQ==.
The studies involving humans were approved by the Institutional Review Board of the Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB-2024-01-200). This study was performed in accordance with the standards of the 1964 Declaration of Helsinki and its later amendments. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
MA: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Methodology, Project administration, Software, Supervision, Validation. SA: Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing, Resources, Visualization. LA: Conceptualization, Data curation, Validation, Visualization, Writing – original draft, Writing – review & editing, Investigation. KA: Conceptualization, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing, Resources. AKA: Conceptualization, Resources, Visualization, Writing – original draft, Writing – review & editing, Methodology, Data curation. AMA: Conceptualization, Validation, Visualization, Writing – original draft, Writing – review & editing, Methodology. FA-A: Conceptualization, Validation, Visualization, Writing – original draft, Writing – review & editing, Investigation.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed in this study are those of the author and do not necessarily reflect those of the SFDA or its stakeholders. Guaranteeing the accuracy and validity of the data was the sole responsibility of the research team.
1. H2020 project and WG1b group “Healthy clinical strategies for healthy aging” of the EU COST Action IS 1402. Medication use in older patients and age-blind approach: narrative literature review (insufficient evidence on the efficacy and safety of drugs in older age, frequent use of PIMs and polypharmacy, and underuse of highly beneficial nonpharmacological strategies). Eur J Clin Pharmacol. (2019) 75:451–66. doi: 10.1007/s00228-018-2603-5
2. United Nations. Available online at: https://www.un.org/en/global-issues/ageing (accessed November 20, 2024).
3. Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: kingdom's vision 2030. J Med Life. (2021) 14:347. doi: 10.25122/jml-2021-0070
4. Corsonello A, Pedone C, Lattanzio F, Lucchetti M, Garasto S, Di Muzio M, et al. Potentially inappropriate medications and functional decline in elderly hospitalized patients. J Am Geriatr Soc. (2009) 57:1007–14. doi: 10.1111/j.1532-5415.2009.02266.x
5. Fialová D, Desplenter F. Aging of the population, clinical pharmacy services, and interdisciplinary cooperation in the optimization of pharmacotherapy in older patients. Drugs Aging. (2016) 33:163–7. doi: 10.1007/s40266-016-0361-6
6. Spinewine A, Fialová D, Byrne S. The role of the pharmacist in optimizing pharmacotherapy in older people. Drugs Aging. (2012) 29:495–510. doi: 10.2165/11631720-000000000-00000
7. Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. (2004) 57:6–14. doi: 10.1046/j.1365-2125.2003.02007.x
8. Turnheim K. When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol. (2003) 38:843–53. doi: 10.1016/S0531-5565(03)00133-5
9. Turnheim K. Drug therapy in the elderly. Exp Gerontol. (2004) 39:1731–8. doi: 10.1016/j.exger.2004.05.011
10. Bonfiglio V, Umegaki H, Kuzuya M. Potentially inappropriate medications and polypharmacy: a study of older people with mild cognitive impairment and mild dementia. J Alzheimer's Dis. (2019) 71:889–97. doi: 10.3233/JAD-190284
11. Laroche ML, Charmes JP, Bouthier F, Merle L. Inappropriate medications in the elderly. Clin Pharmacol Therapeut. (2009) 85:94–7. doi: 10.1038/clpt.2008.214
12. American Geriatrics Society 2015 Beers Criteria Update Expert Panel, Fick DM, Semla TP, Beizer J, Brandt N, Dombrowski R, et al. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. (2015) 63:2227–46. doi: 10.1111/jgs.13702
13. American Geriatrics Society Beers Criteria® Update Expert Panel, Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, et al. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. (2019) 67:674–94. doi: 10.1111/jgs.15767
14. Lim YJ, Kim HY, Choi J, Lee JS, Ahn AL, Oh EJ, et al. Potentially inappropriate medications by beers criteria in older outpatients: prevalence and risk factors. Korean J Fam Med. (2016) 37:329. doi: 10.4082/kjfm.2016.37.6.329
15. Shade MY, Berger AM, Chaperon C, Haynatzki G, Sobeski L, Yates B. Factors associated with potentially inappropriate medication use in rural, community-dwelling older adults. J Gerontol Nurs. (2017) 43:21–30. doi: 10.3928/00989134-20170406-01
16. Nothelle SK, Sharma R, Oakes A, Jackson M, Segal JB. Factors associated with potentially inappropriate medication use in community-dwelling older adults in the United States: a systematic review. Int J Pharm Pract. (2019) 27:408–23. doi: 10.1111/ijpp.12541
17. Alhmoud E, Khalifa S, Bahi AA. Prevalence and predictors of potentially inappropriate medications among home care elderly patients in Qatar. Int J Clin Pharm. (2015) 37:815–21. doi: 10.1007/s11096-015-0125-0
18. Zeenny R, Wakim S, Kuyumjian YM. Potentially inappropriate medications use in community-based aged patients: a cross-sectional study using 2012 Beers criteria. Clin Interv Aging. (2017) 12:65–73. doi: 10.2147/CIA.S87564
19. Pasina L, Djade CD, Tettamanti M, Franchi C, Salerno F, Corrao S, et al. Prevalence of potentially inappropriate medications and risk of adverse clinical outcome in a cohort of hospitalized elderly patients: results from the REPOSI Study. J Clin Pharm Ther. (2014) 39:511–15. doi: 10.1111/jcpt.12178
20. Blanco-Reina E, Ariza-Zafra G, Ocaña-Riola R, León-Ortiz M. 2012 American Geriatrics Society Beers Criteria: enhanced applicability for detecting potentially inappropriate medications in European older adults? A comparison with the screening tool of older person's potentially inappropriate prescriptions. J Am Geriatr Soc. (2014) 62:1217–23. doi: 10.1111/jgs.12891
21. Morin L, Fastbom J, Laroche ML, Johnell K. Potentially inappropriate drug use in older people: a nationwide comparison of different explicit criteria for population-based estimates. Br J Clin Pharmacol. (2015) 80:315–24. doi: 10.1111/bcp.12615
22. Davidoff AJ, Miller GE, Sarpong EM, Yang E, Brandt N, Fick DM. Prevalence of potentially inappropriate medication use in older adults using the 2012 Beers criteria. J Am Geriatr Soc. (2015) 63:486–500. doi: 10.1111/jgs.13320
23. Baldoni ADO, Ayres LR, Martinez EZ, Dewulf NLS, Dos Santos V, Pereira LRL. Factors associated with potentially inappropriate medications use by the elderly according to Beers criteria 2003 and 2012. Int J Clin Pharm. (2014) 36:316–24. doi: 10.1007/s11096-013-9880-y
24. Shah KN, Joshi HM, Christian RP, Patel KP, Malhotra SD. Prevalence of potentially inappropriate medications and prescription cost analysis among older cardiac patients in an outpatient department of a tertiary care hospital in India. J Basic Clin Pharm. (2016) 7:110. doi: 10.4103/0976-0105.189434
25. Al-Azayzih A, Alamoori R, Altawalbeh SM. Potentially inappropriate medications prescribing according to Beers criteria among elderly outpatients in Jordan: a cross sectional study. Pharm Pract. (2019) 17:1439. doi: 10.18549/PharmPract.2019.2.1439
26. Alyazeedi A, Fouad Algendy A, Sharabash M, Karawia A. Prevalence, determinants and associated risk of potentially inappropriate prescribing for older adults in Qatar: a national retrospective study. Clin Interv Aging. (2019) 14:1889–99. doi: 10.2147/CIA.S222532
27. Alshammari H, Al-Saeed E, Ahmed Z, Aslanpour Z. Prevalence and predictors of potentially inappropriate medications among patients aged ≥ 65 years on hospital admissions in Kuwait. Clin Interv Aging. (2022) 17:1025–36. doi: 10.2147/CIA.S328693
28. Abdelwahed AA, El-Dahiyat F, Aljawamis D, Al Ajimi J, Bin Rafeea KJ. Potentially inappropriate medications in older adults according to Beers criteria 2019: prevalence and risk factors. Int J Clin Pract. (2021) 75:e14715. doi: 10.1111/ijcp.14715
29. Mekdad SS, Alsayed AA. Quality improvement project to reduce drug-related problems (DRPs) and potentially inappropriate medications (PIMs) in geriatrics cardiac clinic in Saudi Arabia. Can Geriatr J. (2019) 22:49. doi: 10.5770/cgj.22.338
30. Alturki A, Alaama T, Alomran Y, Al-Jedai A, Almudaiheem H, Watfa G. Potentially inappropriate medications in older patients based on Beers criteria: a cross-sectional study of a family medicine practice in Saudi Arabia. BJGP Open. (2020) 4:bjgpopen20X101030. doi: 10.3399/bjgpopen20X101009
31. Alhawassi TM, Alatawi W, Alwhaibi M. Prevalence of potentially inappropriate medications use among older adults and risk factors using the 2015 American Geriatrics Society Beers criteria. BMC Geriatr. (2019) 19:154. doi: 10.1186/s12877-019-1168-1
32. Alsaad SM, AlEraij S, Alsaad AM, AlSaif HI, Bawazeer G. Potentially inappropriate medications among elderly with frailty in a tertiary care academic medical centre in Saudi Arabia. Healthcare. (2022) 10:1440. doi: 10.3390/healthcare10081440
33. Alshehri S, Alshibani M, Magboul G, Albandar A, Nasser R, Yaqoub RM, et al. Adherence to beers criteria in geriatrics: a retrospective study in a Saudi teaching hospital. Geriatrics. (2020) 5:97. doi: 10.3390/geriatrics5040097
34. Alwhaibi M. Potentially inappropriate medications use among older adults with comorbid diabetes and hypertension in an ambulatory care setting. J Diabetes Res. (2022) 2022:1591511. doi: 10.1155/2022/1591511
35. Alwhaibi M. Inappropriate medications use and polypharmacy among older adults with anxiety disorder. J Clin Med. (2023) 12:4195. doi: 10.3390/jcm12134195
36. Alwhaibi M, Alkofide H. Potentially inappropriate medications use among older adults with dyslipidaemia. J Clin Med. (2023) 12:4063. doi: 10.3390/jcm12124063
37. Yaghi G, Chahine B. Potentially inappropriate medications use in a psychiatric elderly care hospital: a cross-sectional study using Beers criteria. Health Sci Rep. (2023) 6:e1247. doi: 10.1002/hsr2.1247
38. Abilmona G, Fekih-Romdhane F, Hallit S. Assessment of potentially inappropriate medications among long-stay older adult patients with serious mental illnesses: findings from a low-resource setting. Middle East Curr Psychiatry. (2024) 31:32. doi: 10.1186/s43045-024-00419-4
39. Schulze Westhoff M, Schröder S, Groh A, Frieling H, Bleich S, Koop F, et al. Sedatives and analgesics are major contributors to potentially inappropriate duplicate prescriptions in geriatric psychiatry. Psychogeriatrics. (2023) 23:354–63. doi: 10.1111/psyg.12940
40. Pfister T, Schröder S, Heck J, Bleich S, Krüger TH, Wedegärtner F, et al. Potentially inappropriate prescriptions of antibiotics in geriatric psychiatry—a retrospective cohort study. Front Psychiatry. (2024) 14:1272695. doi: 10.3389/fpsyt.2023.1272695
41. Heck J, Ihlefeld C, Krause O, Stichtenoth DO, Schulze Westhoff M, Noltemeyer N, et al. Medication-related problems in geriatric psychiatry—a retrospective cohort study. Int J Geriatr Psychiatry. (2022) 37. doi: 10.1002/gps.5800
42. Schulze Westhoff M, Groh A, Schröder S, Proskynitopoulos PJ, Jahn K, Klietz M, et al. Potentially inappropriate medications according to PRISCUS list and FORTA (Fit fOR The Aged) classification in geriatric psychiatry: a cross-sectional study. J Neural Transm. (2022) 129:1367–75. doi: 10.1007/s00702-022-02541-1
43. Sharma R, Bansal P, Sharma A, Chhabra M, Kumar R, Arora M. Prevalence and predictors of potentially inappropriate psychotropic medication in older adults with psychiatric illness. Asian J Psychiatry. (2021) 66:102872. doi: 10.1016/j.ajp.2021.102872
44. Wolff J, Reißner P, Hefner G, Normann C, Kaier K, Binder H, et al. Pharmacotherapy, drug-drug interactions and potentially inappropriate medication in depressive disorders. PLoS ONE. (2021) 16:e0255192. doi: 10.1371/journal.pone.0255192
45. Stuhec M, Nemec A. Clinical pharmacist interventions on potentially inappropriate medications in older primary care patients with mental disorders with polypharmacy: retrospective cohort study. Psychiatry Clin Neurosci. (2023) 77:64–5. doi: 10.1111/pcn.13491
46. Schröder S, Schulze Westhoff M, Pfister T, Bleich S, Wedegärtner F, Krüger TH, et al. Characteristics of clinical-pharmacological recommendations in psychiatry in Germany. Int J Psychiatry Med. (2024) 59:393–405. doi: 10.1177/00912174231177230
47. Werremeyer A, Bostwick J, Cobb C, Moore TD, Park SH, Price C, et al. Impact of pharmacists on outcomes for patients with psychiatric or neurologic disorders. Ment Health Clin. (2020) 10:358–80. doi: 10.9740/mhc.2020.11.358
48. Ayre MJ, Lewis PJ, Keers RN. Understanding the medication safety challenges for patients with mental illness in primary care: a scoping review. BMC Psychiatry. (2023) 23:417. doi: 10.1186/s12888-023-04850-5
49. Elliott RA, Camacho E, Jankovic D, Sculpher MJ, Faria R. Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Qual Saf. (2021) 30:96–105. doi: 10.1136/bmjqs-2019-010206
50. Fernández EV, Warriner CL, David T, Gordon E, Twigg G, Carroll NV. Potential cost savings by prevention of adverse drug events with a novel medication review program. J Am Pharm Assoc. (2020) 60:462–9. doi: 10.1016/j.japh.2019.12.004
51. Krause O, Ziemann CT, Schulze Westhoff M, Schröder S, Krichevsky B, Greten S, et al. What do older patients know about their medication? A cross-sectional, interview-based pilot study. Eur J Clin Pharmacol. (2023) 79:1365–74. doi: 10.1007/s00228-023-03548-7
52. Santos NSD, Marengo LL, Moraes FDS, Barberato Filho S. Interventions to reduce the prescription of inappropriate medicines in older patients. Rev Saude Publica. (2019) 53:7. doi: 10.11606/S1518-8787.2019053000781
53. Damgaard Jakobsen K, Hansen T, Dam H, Bundgaard Larsen E, Gether U, Werge T. Reliability of clinical ICD-10 diagnoses among electroconvulsive therapy patients with chronic affective disorders. Eur J Psychiatry. (2008) 22:161–72. doi: 10.4321/S0213-61632008000300005
54. Gaebel W, Stricker J, Riesbeck M, Zielasek J, Kerst A, Meisenzahl-Lechner E, et al. Accuracy of diagnostic classification and clinical utility assessment of ICD-11 compared to ICD-10 in 10 mental disorders: findings from a web-based field study. Eur Arch Psychiatry Clin Neurosci. (2020) 270:281–9. doi: 10.1007/s00406-019-01076-z
Keywords: potentially inappropriate medication, Beers criteria, older, aging, psychiatric diseases, mental health disease
Citation: Alsultan MM, Alhawas SM, Alhajri LH, Alamer KA, Alahmari AK, AlQarni AM and Al-Awad FA (2025) Potentially inappropriate medications use among the older patients diagnosed with psychiatric diseases in Saudi Arabia: a cross-sectional study. Front. Med. 12:1534828. doi: 10.3389/fmed.2025.1534828
Received: 26 November 2024; Accepted: 17 February 2025;
Published: 03 March 2025.
Edited by:
Ian Scott, Metro South Health, AustraliaReviewed by:
Takahiko Nagamine, Sunlight Brain Research Center, JapanCopyright © 2025 Alsultan, Alhawas, Alhajri, Alamer, Alahmari, AlQarni and Al-Awad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed M. Alsultan, bW1hYWxzdWx0YW5AaWF1LmVkdS5zYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.