- 1Dongzhimen Hospital, The First Affiliated Hospital of Beijing University of Chinese Medicine, Beijing, China
- 2Department of Neurology and Stroke Center, Dongzhimen Hospital, The First Affiliated Hospital of Beijing University of Chinese Medicine, Beijing, China
Objective: This meta-analysis aimed to evaluate the randomized controlled trials (RCTs) of acupuncture for somatosensory deficits after stroke to provide the current best evidence for clinical practice.
Methods: A systematic search was performed for eligible articles on the acupuncture for somatosensory deficits after stroke based on 14 databases. Two reviewers independently screened the RCTs, extracted data, and evaluated the methodological quality. A meta-analysis of RCTs was conducted using STATA 11.0 software.
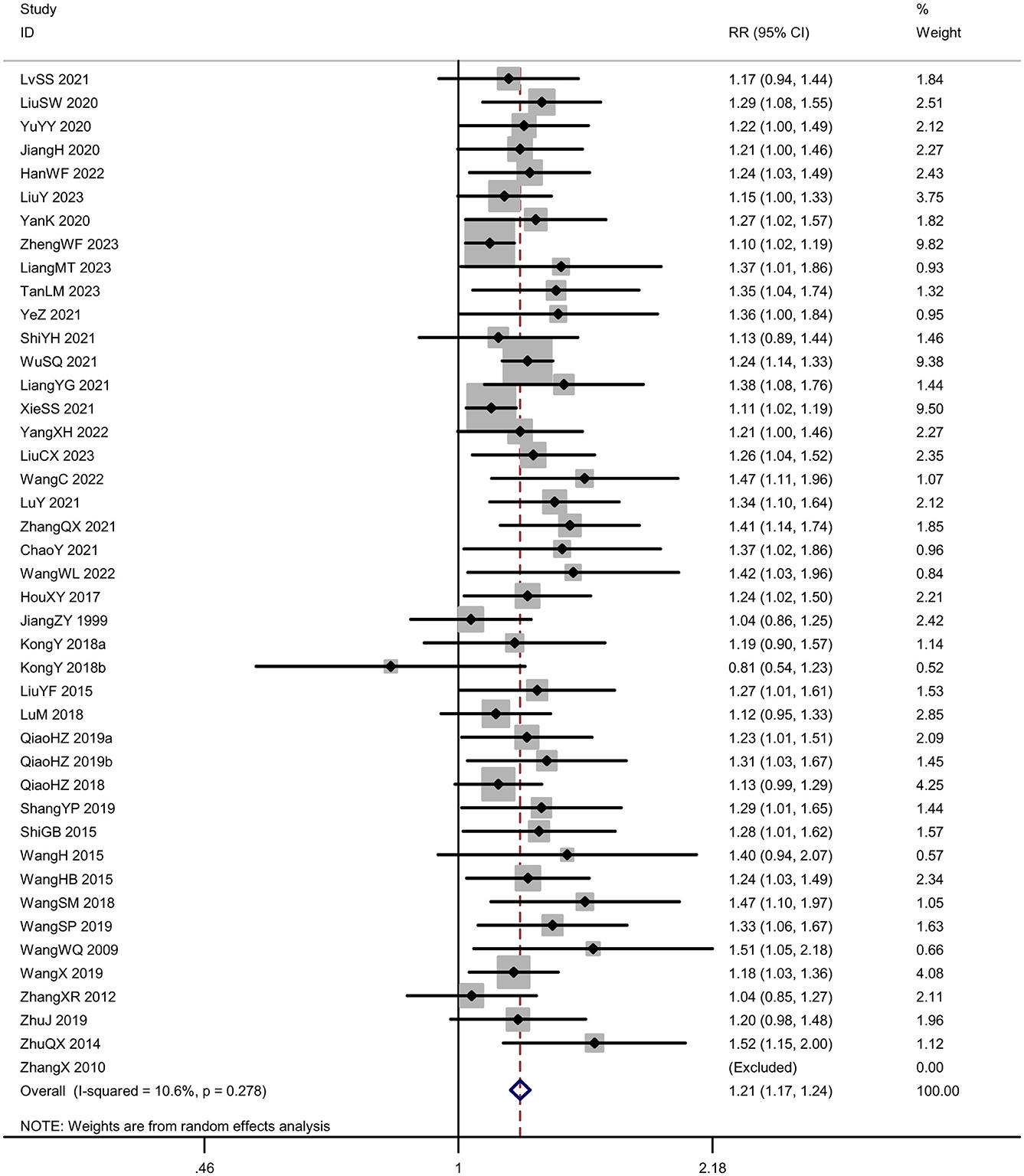
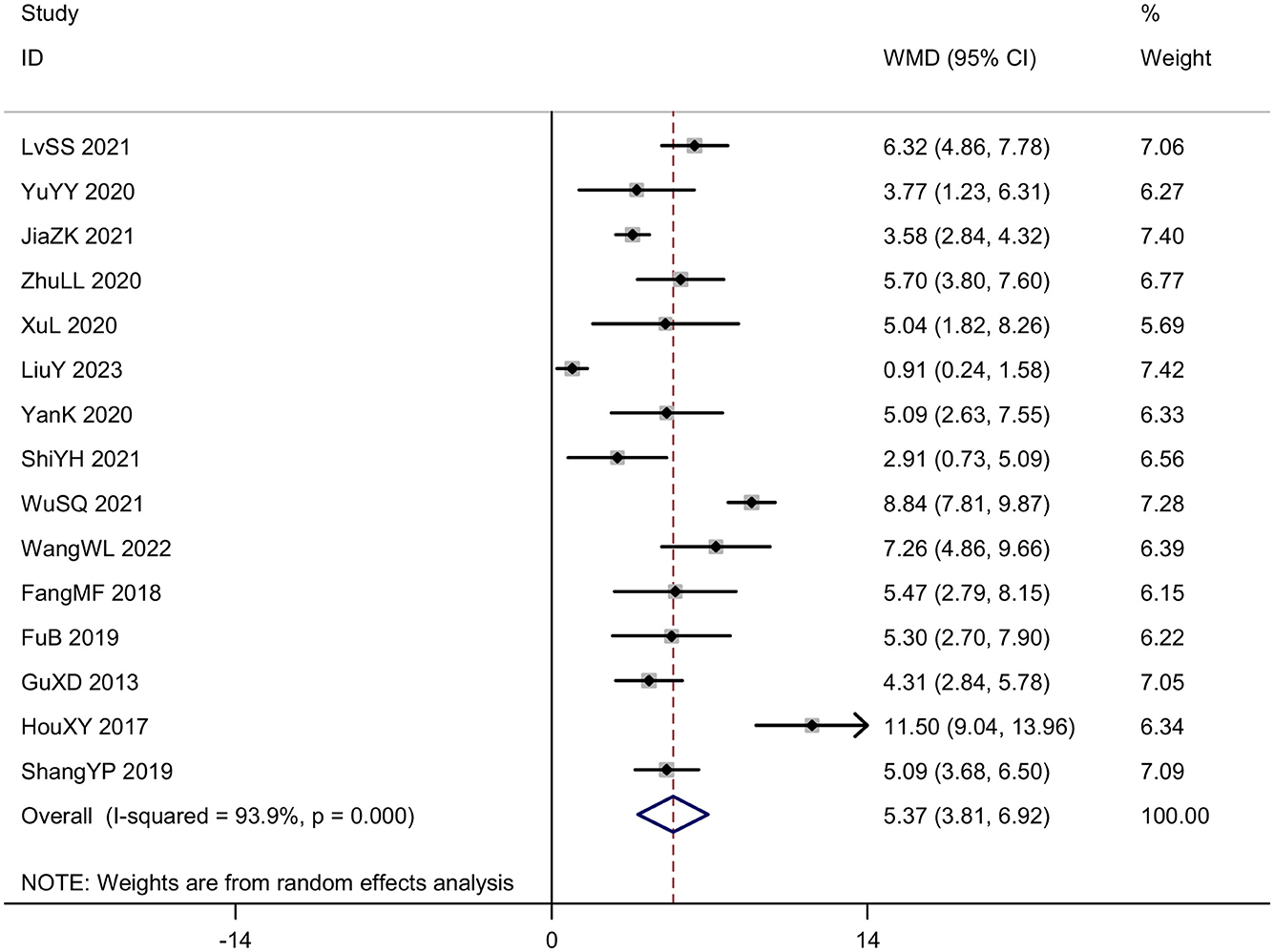
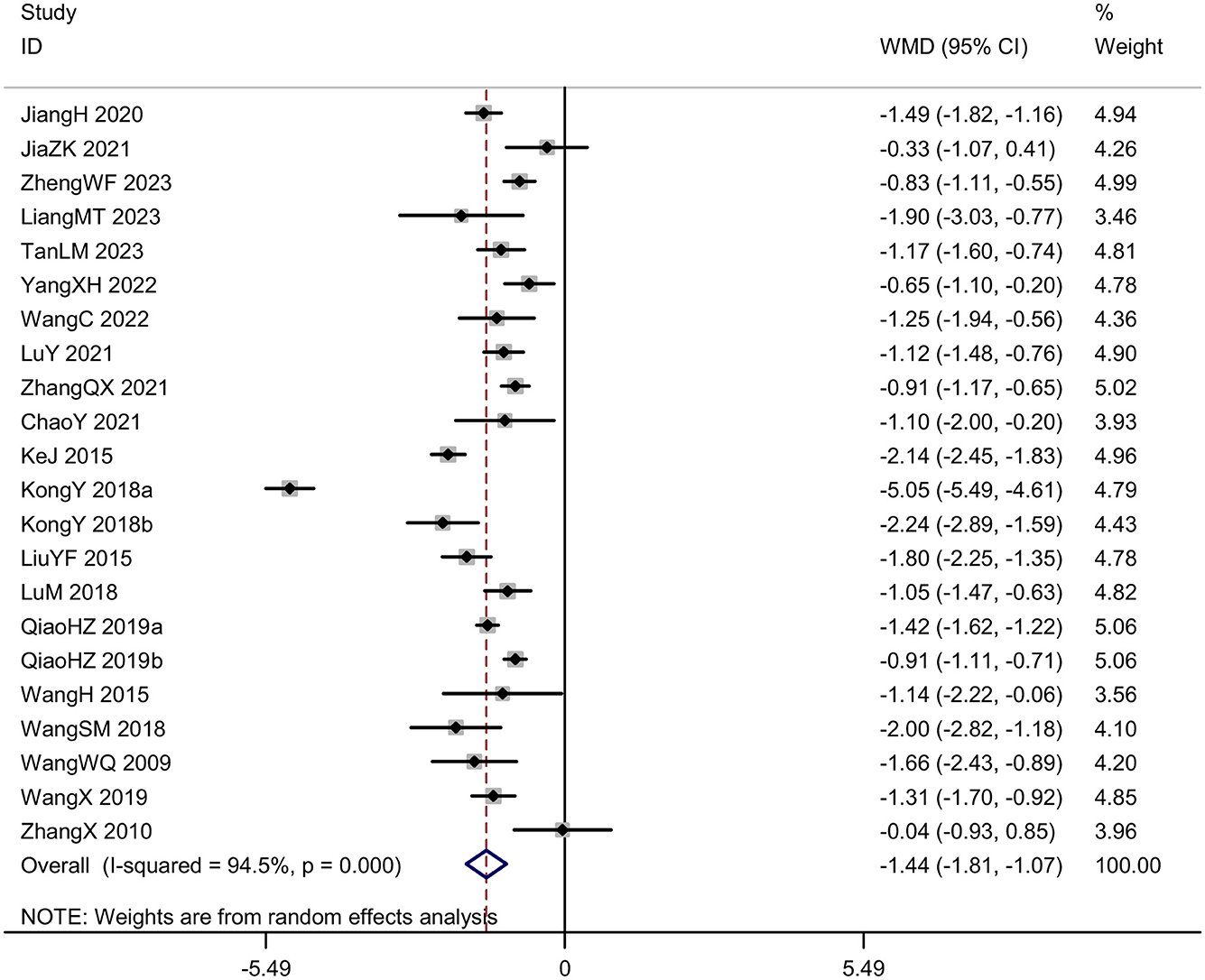
Results: A total of 57 RCTs were included. Meta-analysis results showed that compared with the control group, the acupuncture group had a higher effective rate [risk ratio (RR) = 1.21, 95% CI (1.17, 1.24), I2 = 10.6%, P < 0.001] and a better sensory disturbance score [mean difference (MD) = 5.37, 95%CI (3.81, 6.92), I2 = 93.9%, P < 0.001]. The Visual Analog Scale in the acupuncture group was lower [MD = −1.44, 95%CI (−1.81, −1.07), I2 = 94.5%, P < 0.001]. The acupuncture also showed an improvement in the ability of daily living [MD = 12.19, 95% CI (8.50, 15.87), I2 = 97.2%, P < 0.001] and the symptoms of neurological deficit [Standardized Mean Difference (SMD) = −1.53, 95%CI (−2.04, −1.03), I2 = 89.7%, P < 0.001].
Conclusions: The current best evidence shows that acupuncture has advantages in raising the effective rate, alleviating sensory disturbance, relieving pain, enhancing the ability of daily living, and improving the symptoms of neurological deficits for somatosensory deficits after stroke compared with the control group. And the adverse reactions in acupuncture group were acceptable. However, further well-designed high-quality and multicenter international studies are needed to verify the effectiveness and safety of acupuncture for somatosensory deficits after stroke.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020186040.
Introduction
Stroke, a collective term for a category of diseases caused by cerebrovascular disorders leading to neurological dysfunction, mainly includes ischemic stroke and hemorrhagic stroke (1). It is one of the major diseases causing death and disability in humans, bringing a heavy burden to many patients, families, and society. The incidence of stroke in China continues to rise, with new cases each year accounting for a quarter of the global total. Research from the Global Burden of Disease (GBD) (2) shows that in 2019, there were 3.94 million new stroke cases in our country, with a total of 28.76 million stroke patients and 2.19 million stroke-related deaths.
Following the onset of apoplexy, the five principal symptoms are sudden fainting, hemiplegia, deviation of the mouth and tongue, speech impairment or aphasia, and numbness on one side of the body (3). Sensory disorders are common sequelae subsequent to brain meridian damage, with approximately 50% to 80% of stroke patients presenting varying degrees of sensory disorders (4). The course is frequently protracted and difficult to be cured, severely influencing the recovery of patients' motor functions and other neurological functions, as well as the quality of life. The findings from Lv et al.'s (5) study have demonstrated that the parietal cortex and certain subcortical regions, including the insular cortex and thalamus, contribute to somatosensory symptoms. Current rehabilitation approaches mainly revolve around modern rehabilitation technologies and equipment, which are costly and lack precise individualized rehabilitation plans. Simultaneously, rehabilitation treatment relies on professionals and the environment, and its accessibility is not high (6). Acupuncture, a traditional Chinese medicine technique, was incorporated into the applicable scope of stroke rehabilitation by the World Health Organization in 1998. The possible neural mechanism underlying the modulation of acupuncture is primarily located within the somatosensory cortex (7), in connection with structural neuroplasticity in the primary somatosensory cortex (8) and modulating the neuronal death pathway (9). Additionally, the efficacy and safety of acupuncture for stroke have been a subject of ongoing controversy. Kong et al.'s (10) systematic review did not reveal a positive effect of acupuncture as a treatment for functional recovery after stroke. Park et al.'s (11) systematic review showed that the most methodologically rigorous trials of these included nine studies demonstrated no significant effect of acupuncture. In contrast, Zhang et al.'s (12) overview indicated that acupuncture might be effective in treating post-stroke neurological impairments and dysfunctions, such as dysphagia, but it cannot assist in preventing post-stroke death or disability, nor can it improve other aspects of stroke recovery, such as post-stroke motor dysfunction. In the benchmarks for the practice of acupuncture set by the WHO (13), it is stated that there has been a deficiency of standardized protocols for acupuncture treatment by which the practice can be compared and evaluated. As a result, the efficacy and safety of acupuncture for somatosensory deficits after stroke have remained inconclusive thus far. This study aims to conduct a meta-analysis of published randomized controlled trials (RCTs) on acupuncture treatment for sensory disorders after stroke, to explore the effects of acupuncture intervention on sensory disorders after stroke, and to provide more scientific and reliable evidence for clinical application.
Materials and methods
Registration
The protocol for this systematic review and meta-analysis was registered in PROSPERO (No. CRD42020186040) and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Literature search
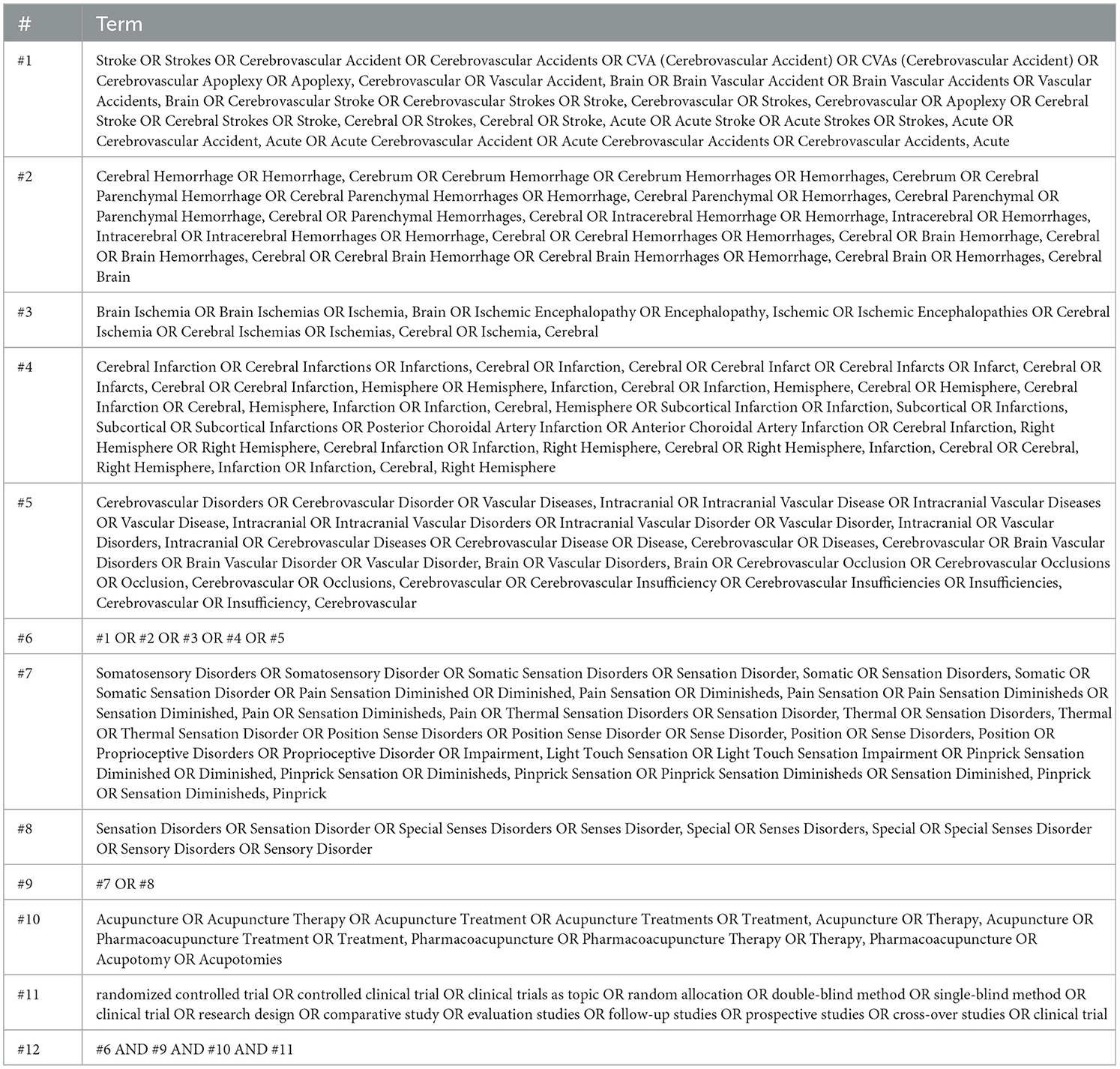
Two researchers (YHC and YL) independently searched PubMed, Cochrane Library, Embase, Web of Science, ClinicalTrials.gov, CINAHL, Wiley, OVID, PROQUES, SCOPUS, Chinese National Knowledge Infrastructure (CNKI), Chinese Science and Technique Journals Database (VIP), Wanfang Database, and SinoMed from study inception to December 1, 2023. There was no restriction on language. The search terms were “stroke,” “somatosensory deficits,” “acupuncture,” “randomized controlled trial,” and related terms. Details of the search strategies are shown in Table 1.
Inclusion criteria
(1) Study types
RCTs of acupuncture for somatosensory deficits after stroke without restriction in language.
(2) Participants
Participants, without gender, age, region, or course restrictions, were diagnosed with stroke by domestic or international relevant diagnostic standards.
(3) Interventions
Acupuncture alone or combined with comparisons. Acupuncture treatments are specified as needle-based acupuncture, including but not limited to manual, electro-acupuncture, fire acupuncture, warm acupuncture, ear (auricular) acupuncture, head acupuncture, and more.
(4) Comparisons
Conventional pharmacotherapy, other non-pharmacotherapy, or invalid groups, including placebo and no treatment.
(5) Outcomes
The included studies reported at least one primary outcome: effective rate and sensory disturbance score. The secondary outcomes included Visual Analog Scale (VAS), daily living ability score, neurological deficit severity score, and incidence of adverse events.
Exclusion criteria
Studies with incomplete data or duplicate publications.
Data extraction
Two researchers (QYL and JP) independently screened the titles, abstracts, and full texts of the retrieved studies for eligibility and independently extracted the data of the final included literature. Disagreements were resolved by mutual negotiation or by consultation with a third researcher (LS). The following information was extracted: authors, publication year, general information, participants' characteristics, details of interventions (type of acupuncture, acupoints, frequency, duration of treatment, retention time of acupuncture), and outcomes.
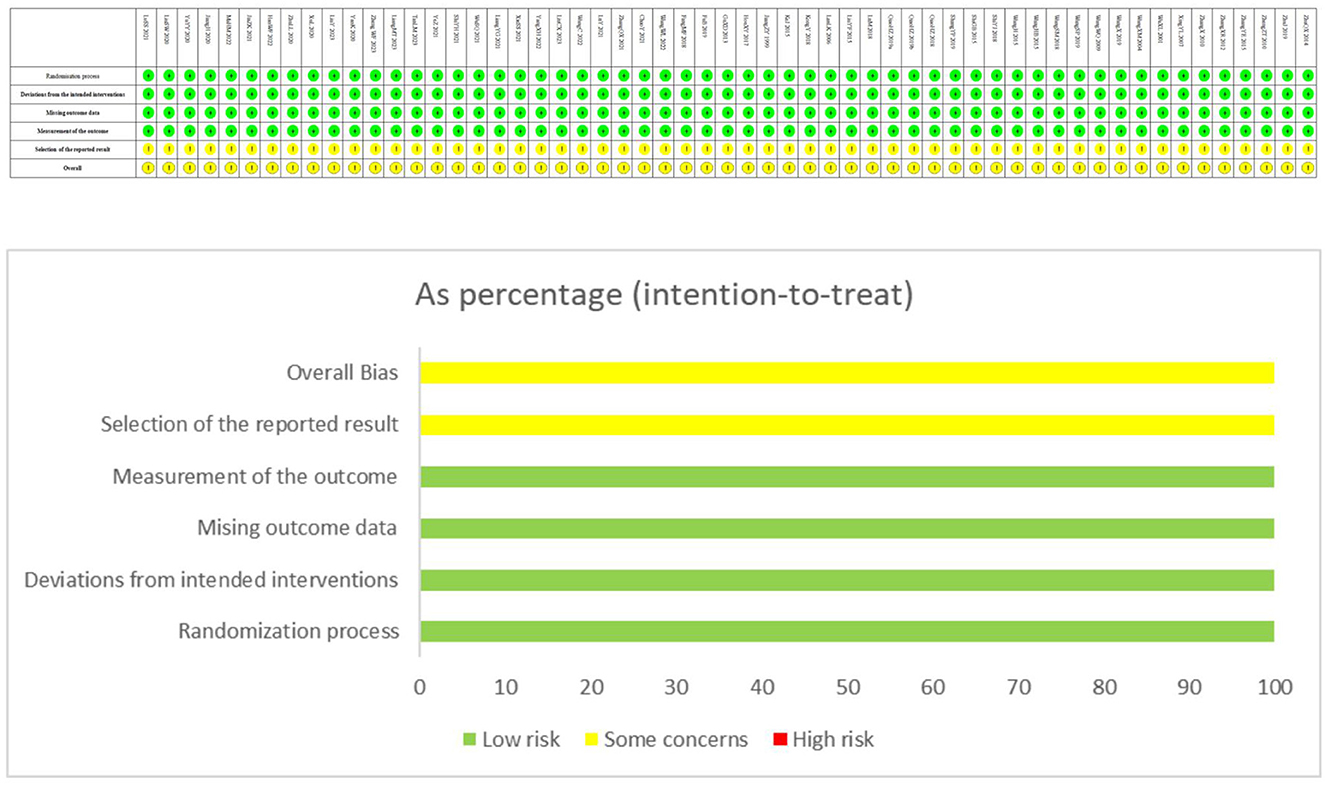
Risk of bias assessment
Two researchers (SMR and XC) independently assessed the methodological quality of the included studies using the Cochrane Risk of Bias Tool 2.0 (RoB 2.0) (14), which contains six aspects: randomization, deviations from the intended interventions, missing outcome data, measurement of the outcome, selective outcome reporting, and overall bias. Each aspect was evaluated as “low risk of bias” “some concerns” or “high risk of bias.” Disagreements were resolved by mutual negotiation or by consultation with other researchers (LS). The appraisal of acupuncture procedures was assessed by Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA).
Assessing certainty of the evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (15) was used to rank the quality of evidence in five downgrading domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The quality of the evidence was classified into four grades: high, moderate, low, or very low.
Statistical analysis
All statistical analyses were performed with STATA Software, version 11.0. We used a random-effects model (DerSimonian and Laird method) to calculate summary effect estimates for primary and secondary outcomes. Heterogeneity was assessed by the χ2 test and the I2 statistic. Dichotomous outcomes were expressed as the risk ratio (RR) with a 95% confidence interval (CI), while continuous outcomes were expressed as the standardized mean difference (MD) with a 95% CI. Standardized mean difference (SMD) was selected when different measures and units were used, or when the difference in means between studies was too large. A funnel plot and Egger's test were applied to evaluate publication bias when the number of included studies was more than 10. A subgroup analysis and a meta-regression were conducted based on the interventions, comparisons, type of disease, course of disease and course of treatment. Sensitivity analysis was conducted to evaluated the stability of the results.
Results
Included studies
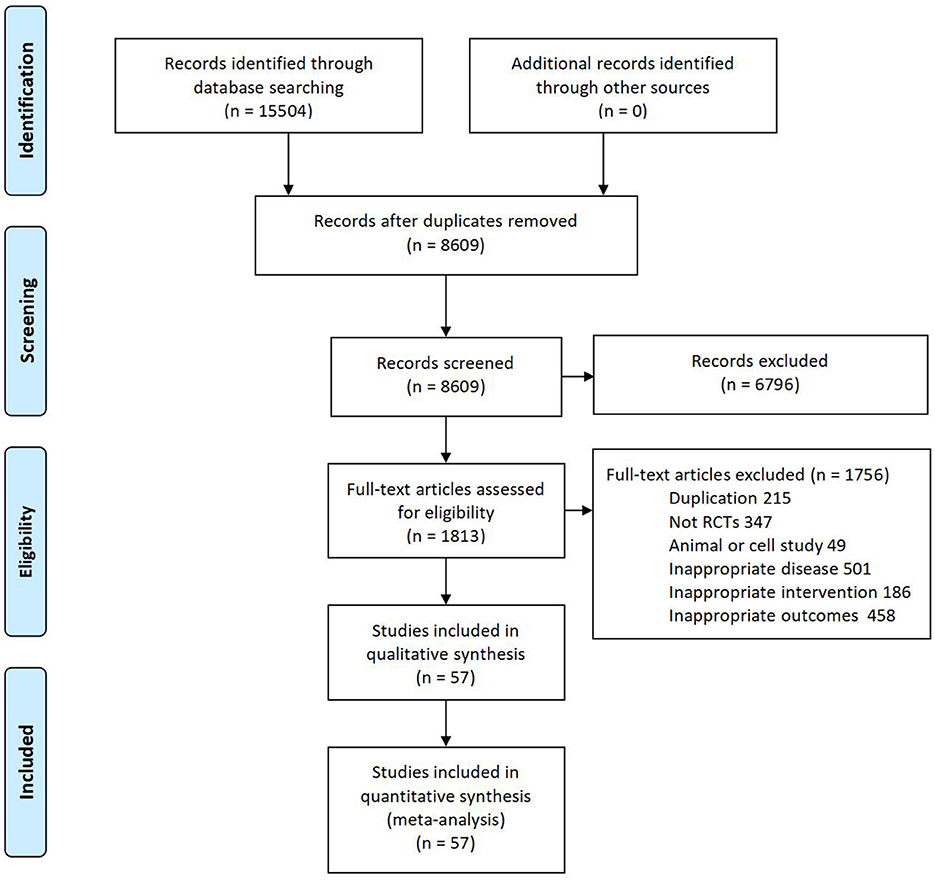
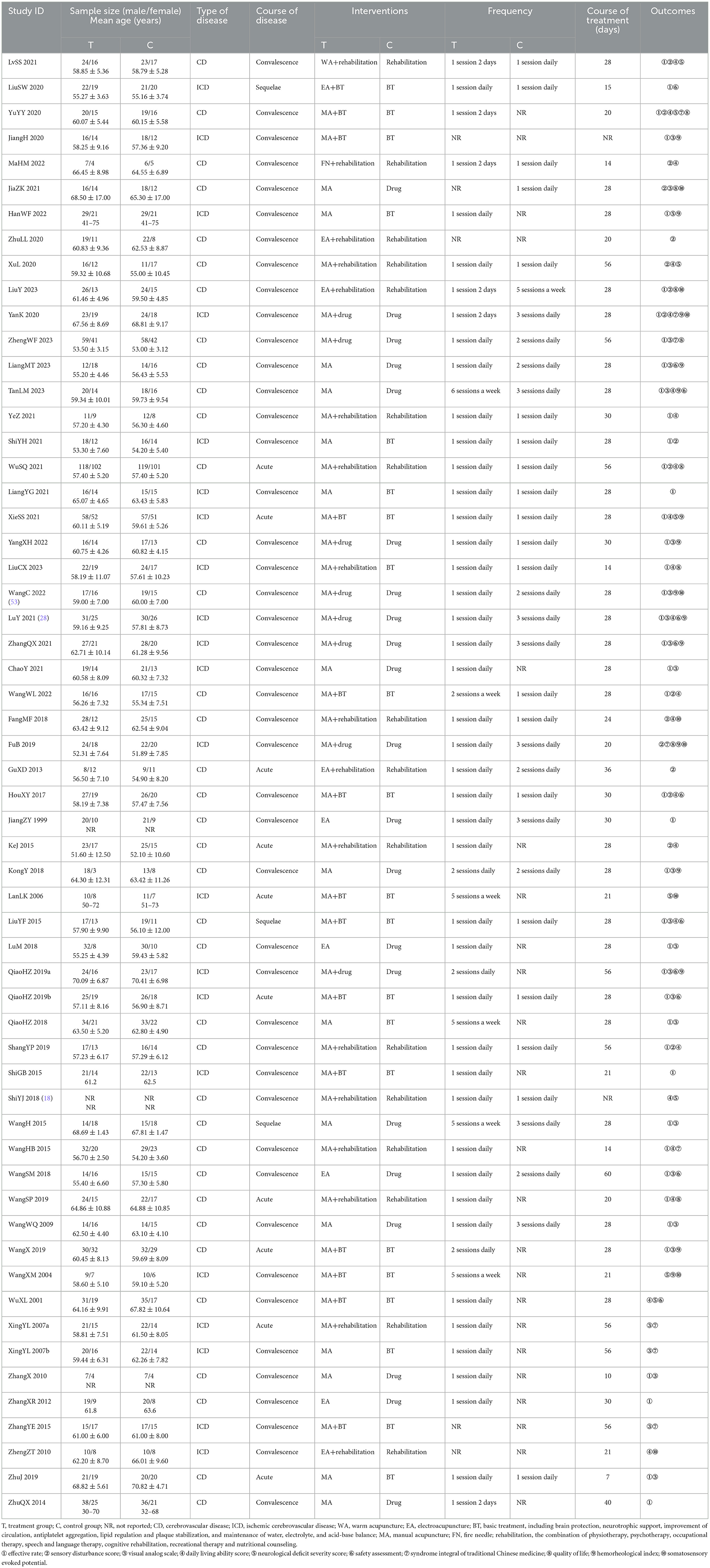
Fifteen thousand five-hundred four articles were yielded by database searching. Eventually, 57 eligible RCTs (with data for 4,794) were included after screening full texts according to the inclusion and exclusion criteria. And a flow diagram for study selection is shown in Figure 1. The 57 articles were all published between 1999 and 2023. Among these articles, 24 articles reported foundation and were all funded by industry. For details of each included trial please see the Table 2.
Participants
All included studies were conducted in China, and 55 studies were published in Chinese and two in English (16, 17). The sample sizes of the 57 trials ranged from 22 to 440. Three trials (16, 18, 19) did not report the mean age of participants, and the age of the rest of the participants ranged from 30 to 79 years. Forty-five trials included more males than females, ranging from 37% to 86% male. One trial (18) did not describe the gender of the participants. Twenty-one trials included only participants with ischemic stroke (20–39). All other trials included participants with ischemic and hemorrhagic strokes (16–18, 40–66). None of the included trials had a definition of severity. There were 10 trials (26, 32, 34, 37, 51, 56, 58, 67–69) involving participants with an interval from stroke onset < 2 weeks (acute phase), 44 trials (21–25, 27–31, 40–50, 52–55, 66) between 2 weeks and 6 months (convalescent phase), and three trials (17, 20, 63) including participants with an interval from stroke onset of more than 6 months (sequelae phase).
Interventions
In 38 studies, acupuncture therapy combined with the same intervention applied in the control group (20, 21, 23, 40–42, 44–47, 50, 51, 66) was compared with the control group; in the remaining 19 trials, acupuncture alone was compared with the control group's treatment (16, 22, 24, 25, 30, 43, 48, 49, 59–61, 63, 65, 66, 70). Among the included trials, there were 3 three-armed trials (37, 38, 59). In this review, the basic treatment included smoking and alcohol cessation, oxygen inhalation, as well as medication for regulating blood glucose, blood pressure, blood lipids, anticoagulation, or antiplatelet aggregation. The drugs included Methylcobalamin, Pregabalin, Amitriptyline, Carbamazepine and Gabapentin. The acupuncture interventions used varied considerably across trials. Forty-seven trials used manual stimulation (21–23, 41–43, 45, 47–50, 66), nine used electroacupuncture (16, 20, 39, 44, 46, 56, 60, 65, 71), and each had a trial using the fire needle (42) and the warm acupuncture (40). Acupuncture point prescriptions were not consistent, with 40 trials only involving body acupoints (20–22, 40–44, 47–50, 66), seven trials involving scalp acupoints (37, 38, 45, 56, 59, 62, 68), five trials involving wrist ankle acupoints (23, 31, 46, 55, 69), one trial involving eye acupoints (24), three trials using both body and scalp acupoints (52, 57, 65), one trial using body and wrist ankle acupoints (30) and one trial using body, scalp and wrist ankle acupoints (33). Through statistical analysis, it has been found that our study mentions a total of 43 acupoints. We discovered that baihui (DU20) appears the most frequently, with a total of 14 occurrences, followed by the sanyinjiao (SP6) with 13 occurrences, and then the zusanli (ST36) with nine occurrences. Fengchi (GB20), hegu (LI4), and yanglingquan (GB34) each appeared six times. Neiguan (PC6), quchi (LI11), and Ah Shi points each appeared five times. Jianyu (LI15), weizhong (BL40), jiquan (HT1), and xuehai (SP10) each appeared four times. Fenglong (ST40), tianzhu (BL10), and shenting (GV24) each appeared three times. Wangu (GB12), taichong (LR3), shousanli (LI10), waiguan (SJ5), huantiao (GB29), fengshi (GB31), chize (LU5), yongquan (KI1), liangqiu (ST34), dicang (ST4) and taiyang each appeared two times. The acupoints that appeared only once include yintang (GV29), taixi (KI3), pishu (BL20), xinshu (BL15), feishu (BL13), shenshu (BL23), ganshu (BL18), yuyao, jianzhen (SI9), xiaguan (ST7), jiache (ST6), chengjiang (ST24), sibai (ST2), yingxiang (LI20), qubin (GB7), and baxie. The needle retention time was 15 min to 8 h in all the included trials. The length of treatment period ranged from 7 to 60 days, with the number of treatment sessions varying from seven to 112 sessions and the frequency of treatment varying from two sessions per week to two sessions per day. The intervention details showed in Appendix 1.
Outcomes
The most commonly reported outcomes were effective rate, visual analog scale and daily living ability score. Forty-three trials evaluated the effective rate of acupuncture. The efficacy criteria for 20 trials were self-defined, and the remaining trials' were derived from the “Guiding Principles for Clinical Research of New Traditional Chinese Medicines,” “Diagnostic Criteria and Therapeutic Effect Standards for Syndromes and Diseases in Traditional Chinese Medicine,” “Criteria for Diagnosis, Cure, and Improvement of Clinical Diseases,” and “Guidelines for Rehabilitation Treatment of Stroke in China” and so on. Twenty-two trials evaluated the effect of acupuncture on activities of daily living. The measures employed included the Barthel Index (BI) or modified Barthel Index (MBI) and the Activities of Daily Living Scale (ADL). Fifteen trials reported sensory disturbance score. Nine trials measured the neurological deficit severity score. The measures employed included the National Institutes of Health Stroke Scale (NIHSS) and the Chinese stroke patient neurological deficit score, also known as the Modified Edinburgh-Scandinavian Stroke Scale (MESSS). Only eleven trials reported information on adverse events. None of the 57 included trials provided any information on death, the proportion of participants requiring institutional care, or extensive family support after acupuncture treatment or at the end of follow-up.
Risk of bias in included studies
The ROB assessment is shown in Figure 2.
(1) Allocation
(1.1) Random sequence generation
Thirty-five trials randomly assigned participants to groups by using random number tables. One trial generated random numbers through SPSS software and one assigned based on the order of consultation. The remaining 20 trials did not report their methods of random sequence generation.
(1.2) Allocation concealment
Of the 57 included trials, only one trial reported adequate allocation concealment by using sealed envelopes (45).
(2) Blinding
Due to the nature of acupuncture manipulations, blinding to participants is not suitable for acupuncture therapy. This makes all included studies have a certain risk of bias. Only one study specified data collectors and outcome assessors were masked to treatment allocation (72).
(3) Incomplete outcome data
Six trials reported withdrawals, but the results were not analyzed on an intention-to-treat basis. None of the remaining 51 trials made any mention of dropouts or withdrawals. For all 51 trials, the count of participants who were randomized matched the count of participants who were subsequently analyzed, indicating that no exclusions took place post-randomization.
(4) Selective reporting
The included trials in this review did not report some clinically important outcomes, such as death, requiring Institutional care, and all-cause mortality. Of the 57 included studies, only 11 studies reported adverse events, therefore we assumed that this may have constituted some degree of reporting bias.
(5) Other potential sources of bias
There was insufficient information reported to determine if there were any other potential sources of bias.
Meta-analysis
Effective rate
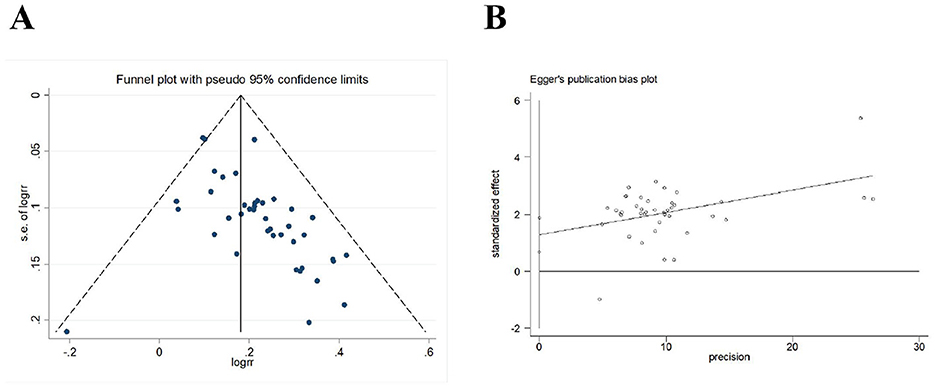
Forty-three trials (N = 3,798 participants) evaluated the effective rate of acupuncture for post-stroke somatosensory deficits. The results of meta-analysis indicated that acupuncture group was significantly higher than the control group [RR = 1.21, 95% CI (1.17, 1.24), I2 = 10.6%, P < 0.001] in improving effective rate (Figure 3). In this analysis there was no significant publication bias on Egger's test (P < 0.001; Figure 4).
Sensory disturbance score
Fifteen trials (N = 1,407) assessed the severity of somatosensory deficits in stroke patients by using the sensory disturbance score. The meta-analysis results showed that acupuncture led to a better sensory disturbance score [MD = 5.37, 95% CI (3.81, 6.92), I2 = 93.9%, P < 0.001] than control group (Figure 5). Funnel plots and Egger's test were done to evaluate publication bias, and results showed no significant publication bias (P = 0.068; Figure 6).
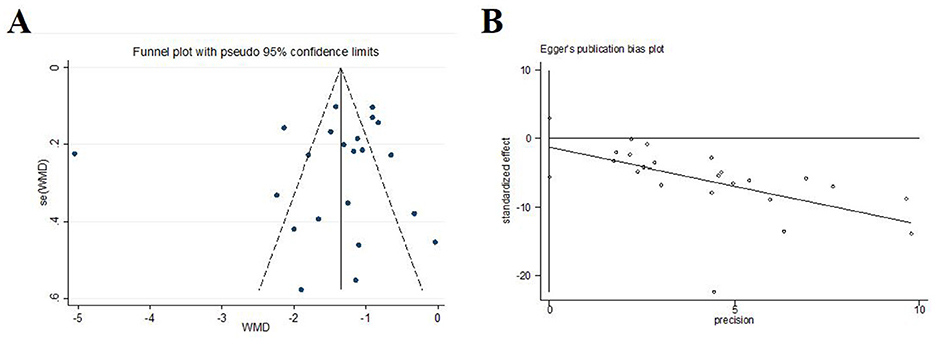
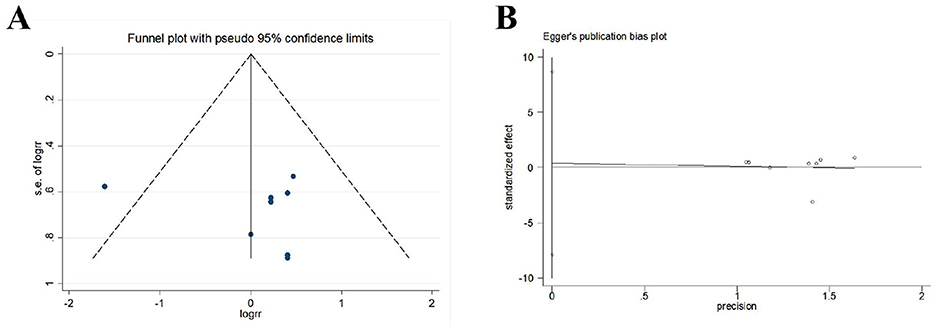
Visual analog scale
We conducted a meta-analysis of the study results based on the visual analog scale. In 22 trials (N = 1,651), acupuncture was statistically superior to control [MD = −1.44, 95%CI (–1.81, –1.07), I2 = 94.5%, P < 0.001; Figure 7]. Funnel plots and Egger's test were done to evaluate publication bias, and results showed no significant publication bias (P = 0.526; Figure 8).
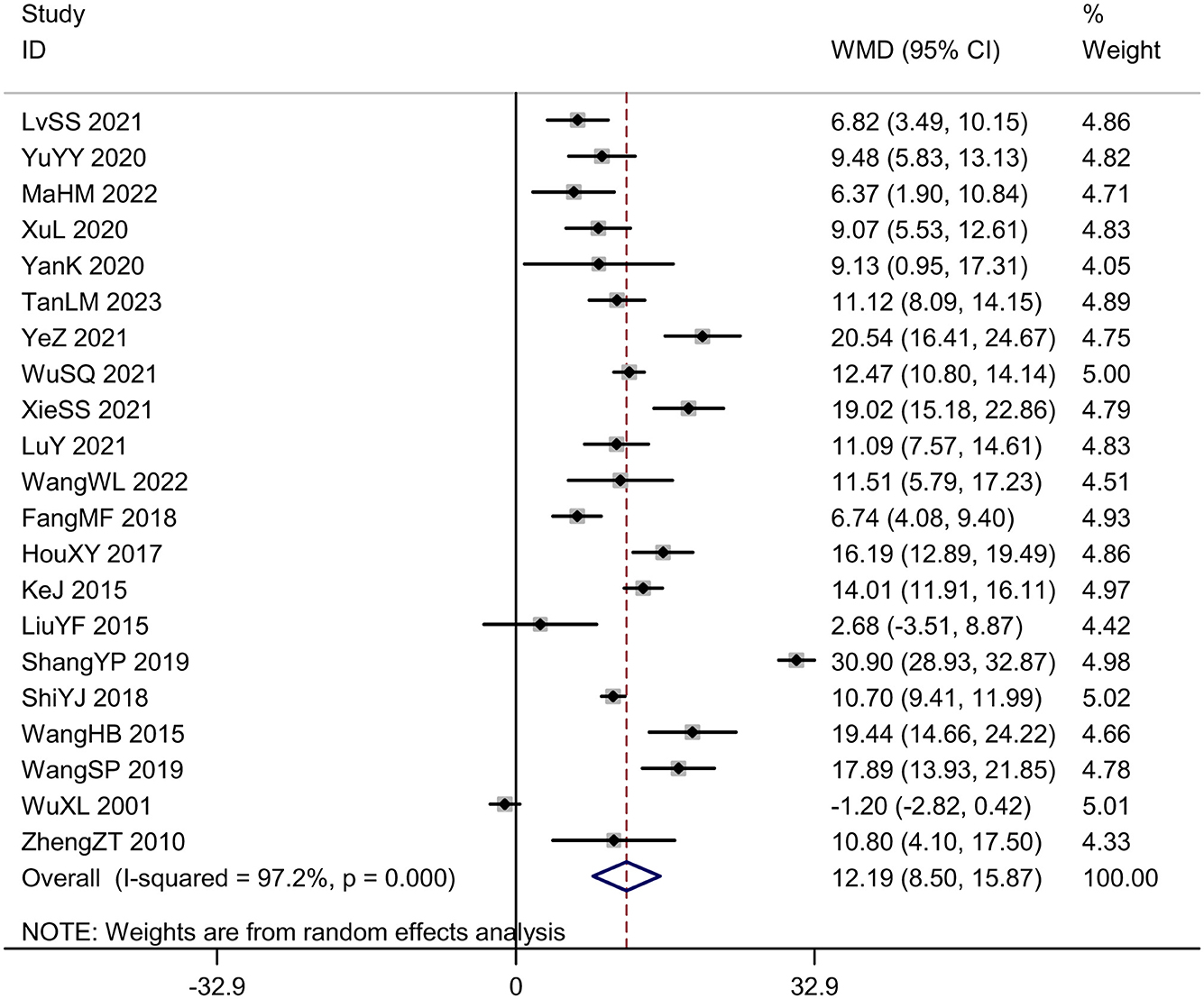
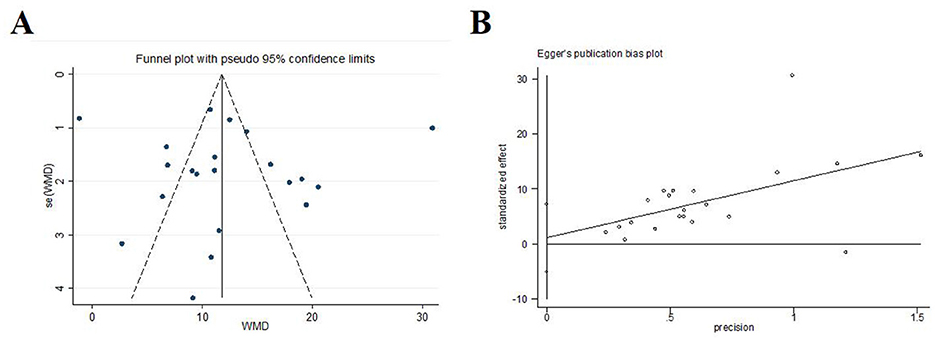
Daily living ability score
Twenty-one trials (N = 2,077) reported daily living ability score. The intervention group exhibited significantly higher daily living ability score compared to the control group [MD = 12.19, 95%CI (8.50, 15.87), I2 = 97.2%, P < 0.001; Figure 9]. The plot on daily living ability score was visibly symmetric and Egger's test revealed no potential publication bias (P = 0.701; Figure 10).
Neurological deficit severity score
A total of nine trials (N = 2,077) scored the severity of neurological deficits before and after treatment. Among them, five trials used the National Institutes of Health Stroke Scale (NIHSS) for scoring, and four trials used the Chinese stroke patient neurological deficit score, also known as the Modified Edinburgh-Scandinavian Stroke Scale (MESSS). Due to the use of different scales for scoring, the SMD was adopted as the indicator for the combined effect. The meta-analysis results showed that the experimental group was superior to the control group in reducing the neurological deficits of the subjects [SMD = –1.53, 95%CI (–2.04, –1.03), I2 = 89.7%, P < 0.001; Figure 11). Funnel plots and Egger's test were done to evaluate publication bias, and results showed no significant publication bias (P = 0.233; Figure 12). Given the limited number of studies included for neurological deficit severity score, we also conducted a trim-and-fill analysis. No trimming performed and data unchanged indicated relatively stable results.
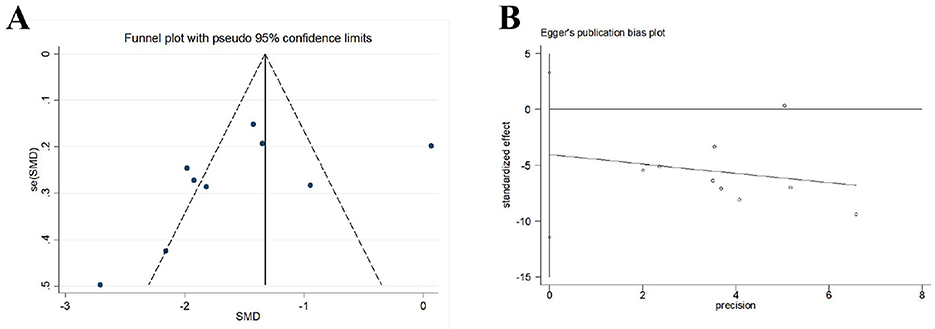
Figure 12. Publication bias in the neurological deficit severity score. (A) Funnel plots. (B) Egger's test.
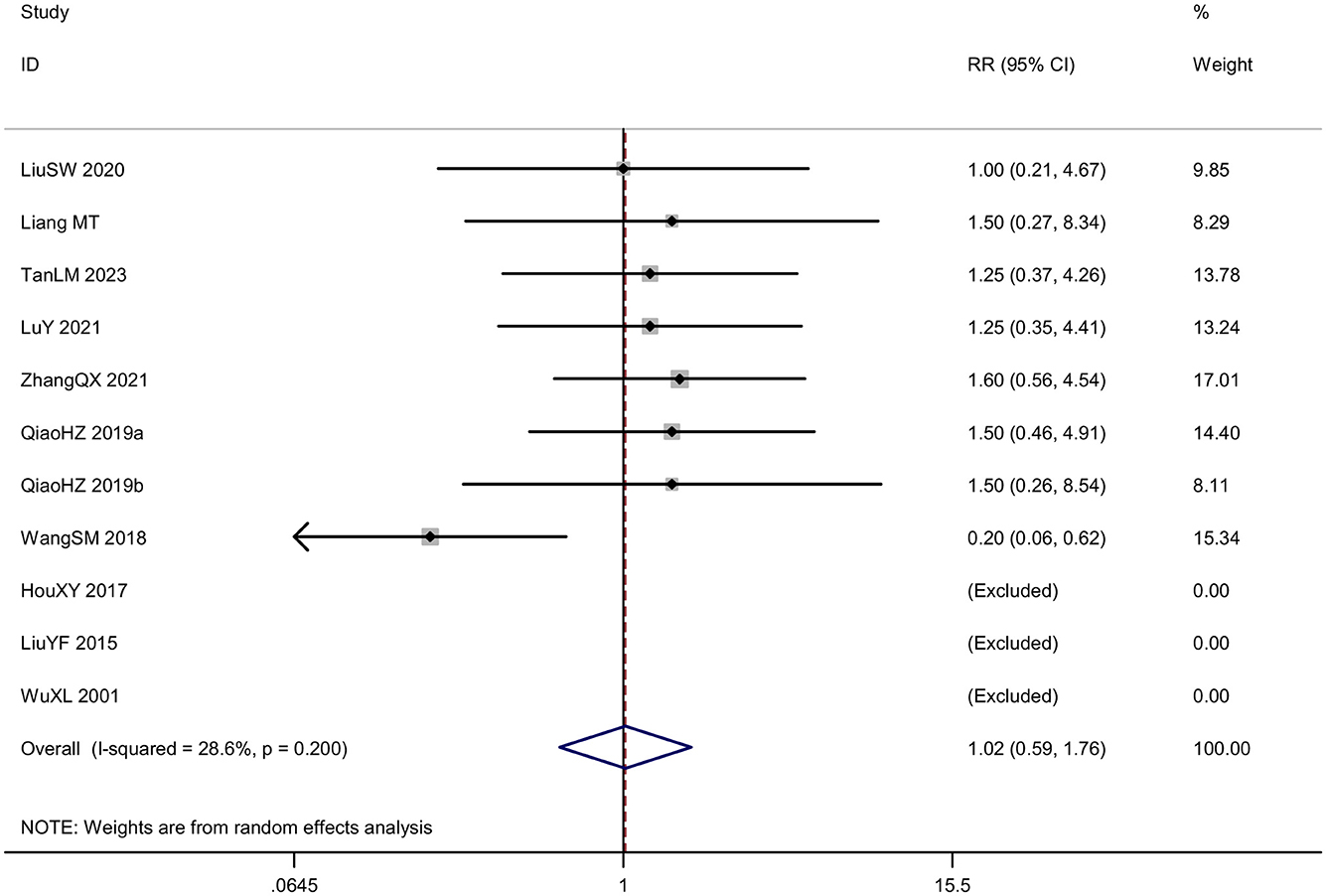
Safety assessment
Eleven RCTs reported the safety of acupuncture. Eight studies reported adverse events, including subcutaneous hemorrhage, dizziness, headache, fatigue, gastrointestinal discomfort, thirst, palpitation, cold sweat, etc. As an invasive treatment method, acupuncture can potentially puncture small blood vessels or veins within the subcutaneous tissue during the treatment process, leading to subcutaneous bleeding or hematoma. This is especially common for thin individuals with little subcutaneous fat, the elderly with increased vascular fragility, as well as areas with abundant capillaries such as the head and face, and areas close to veins. Therefore, doctors should consider the physical condition of the recipients to reduce the risk of subcutaneous bleeding or hematoma. Well, the subcutaneous hemorrhage usually absorbs on their own without requiring special treatment. However, not all subcutaneous bleeding or hematoma should be concealed, as blood-letting through acupuncture is also a traditional Chinese medical treatment method. As for this series of symptoms including dizziness, headache, fatigue, gastrointestinal discomfort, thirst, palpitation, cold sweat etc, they are a phenomenon known as acupuncture-related syncope. It may be related to the patient's weak constitution, mental tension, overexertion, hunger or improper positioning. Methods to handle syncope include immediately stopping the acupuncture, removing all the needles, supporting the patient to lie down flat for a while and providing warm water, after which recovery can occur. And three studies reported no adverse effects related to acupuncture. The incidence rate of adverse events in treatment group was 7.32% and that in control group was 8.04%. Analysis of data from adverse events showed low heterogeneity (P = 0.200, I2 = 28.6%), and the random-effects model showed no significant difference in the RR of acupuncture group compared with control group [RR = 1.02, 95% CI (0.59, 1.76); Figure 13]. A funnel plot was generated to visually assess potential publication bias and Egger test was conducted to assess publication bias. The results of the meta-analysis were not significantly affected by publication bias (P = 0.913; Figure 14).
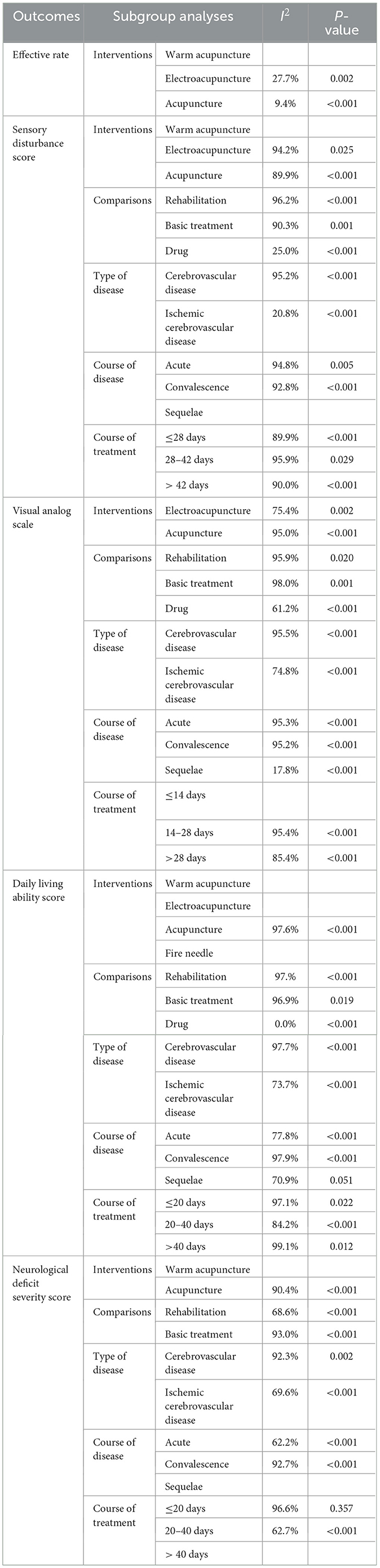
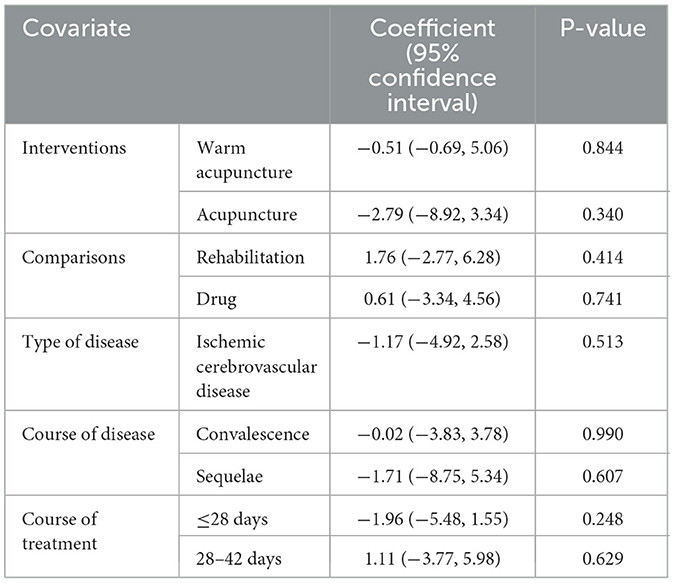
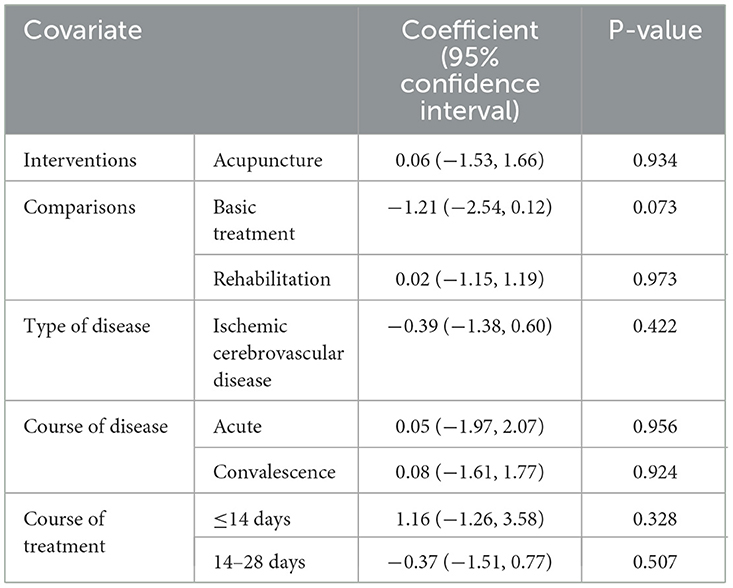
Heterogeneity analysis
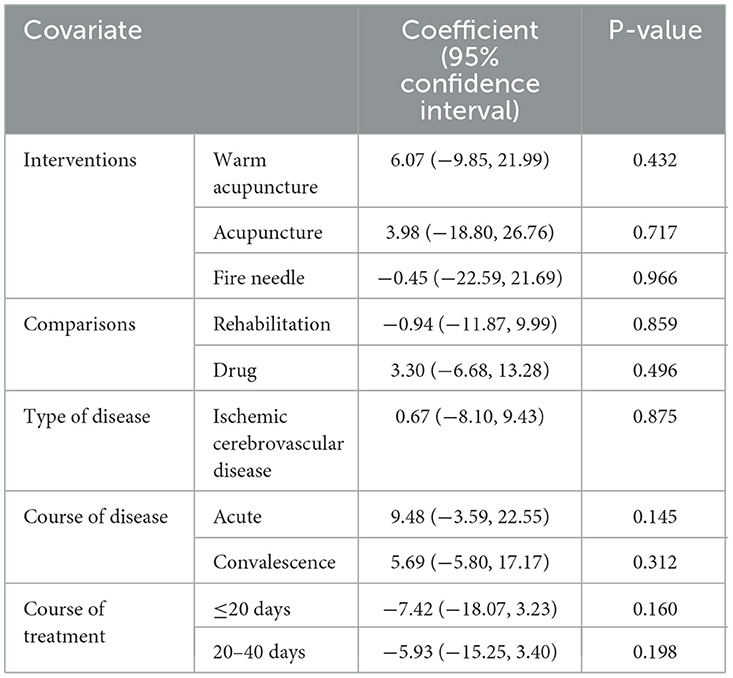
Given the pronounced heterogeneity, the subgroup analysis and meta-regression analysis were further conducted based on the interventions, comparisons, type of disease, course of disease and course of treatment in some outcomes including sensory disturbance score, visual analog scale and daily living ability score. The subgroup analysis and meta-regression analysis indicated no significant association between results and these potential influencing factors (Tables 3–6).
Sensitivity analysis
Further sensitivity analysis was performed to assess the stability of the outcomes of meta-analysis. And the results intuitively showed the robust of the outcomes (Figure 15).

Figure 15. Sensitivity analysis. (A) Effective rate. (B) Sensory disturbance score. (C) Visual analog scale. (D) Daily living ability score. (E) Neurological deficit severity score.
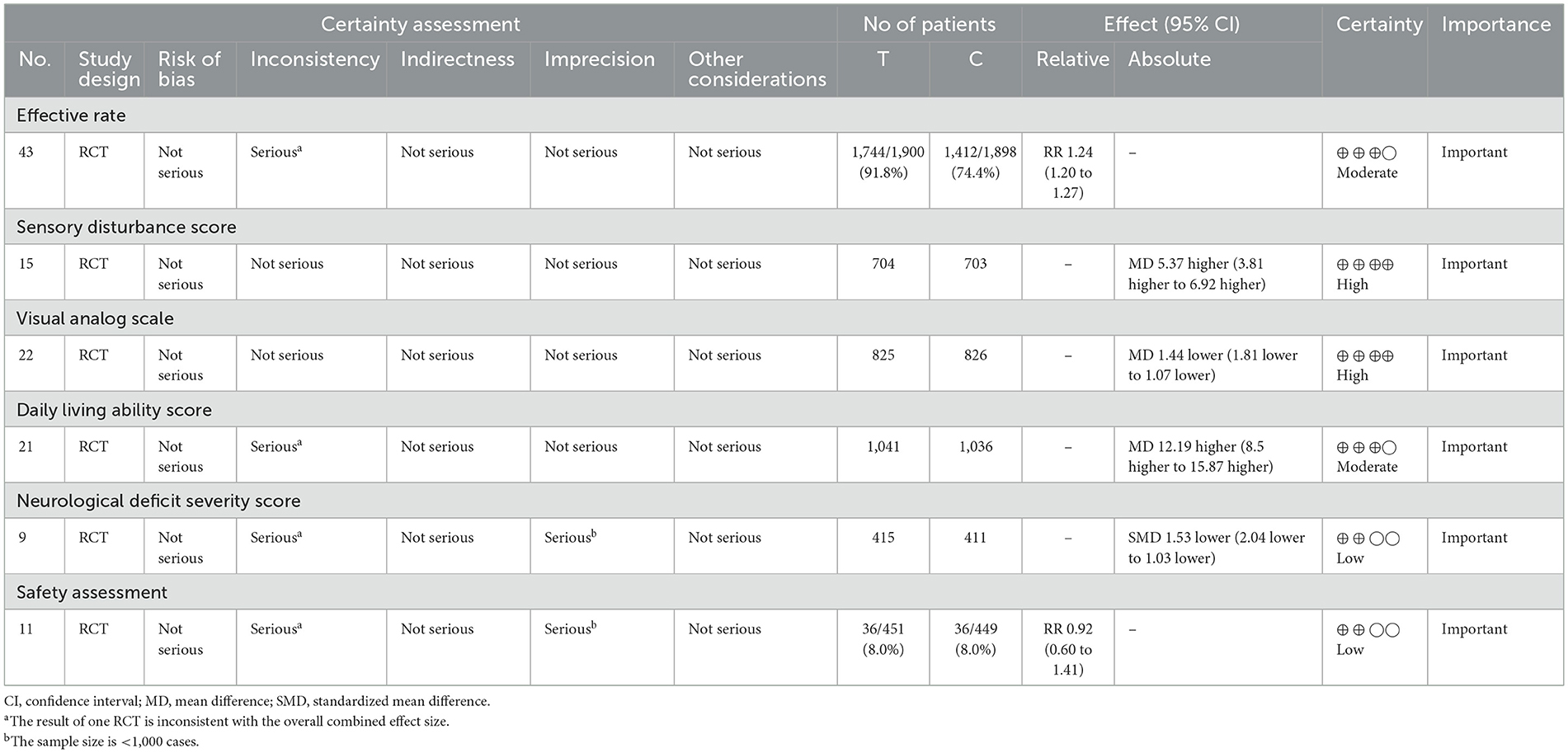
Certainty of evidence
The results of the GRADE analysis showed that sensory disturbance score and VAS were ranked as high-quality, effective rate and daily living ability score were ranked as moderate-quality and other results were ranked as low-quality (Table 7).
Discussion
Summary of main results
This study included a total of 57 randomized controlled trials (RCTs), with 55 in Chinese and two in English. The RoB tool evaluation indicated that the high-risk items in the included literature were mainly due to the lack of specific descriptions of the random sequence concealment method, and the failure to use blinding for patients, intervention implementers, data analysts, data collectors, and outcome evaluators, with only a few documents reporting dropout situations. The GRADE evaluation results showed that the evidence quality for the severity of neurological deficit scores and adverse event occurrence was low.
The results revealed the following.
1. Compared with control group, acupuncture is superior in improving efficiency, alleviating sensory disorders, reducing pain, enhancing daily living abilities, and relieving neurological deficits for sensory disorders after stroke.
2. There was no statistically significant difference in the incidence of adverse events between the treatment group and the control group.
In-depth analysis of meta-analysis results
Funnel plots were drawn for outcome indicators such as efficiency, sensory disorder scores, visual analog scale scores, and daily living abilities, and the symmetry of the funnel plots was tested using the Egger method. The results showed that the funnel plots were basically symmetrical, indicating that the probability of publication bias in the included literature was small.
For outcome indicators with large heterogeneity, including sensory disorder scores, visual analog scale scores, daily living abilities, and the severity of neurological deficit scores, subgroup analysis and meta-regression were conducted to explore the sources of heterogeneity according to different experimental group interventions, control group interventions, disease types, course of disease, and treatment courses. The results showed that these factors were not the reasons for the high heterogeneity. Except for the post-sequelae phase subgroup in the daily living abilities outcome indicator and the treatment course ≤ 20 days subgroup in the neurological deficit severity score outcome indicator, the results of the other outcome indicators' subgroup analyses were statistically significant (P < 0.05), which can indirectly indicate that the meta-analysis results of the above outcome indicators have good robustness. The reasons for the lack of statistical significance in the subgroup results may be the following two points: (1) The number of included RCTs and sample sizes is small, with only two RCTs included in each of the two subgroups, and the sample size of both groups is <200 cases, which led to the appearance of false-negative results; (2) The therapeutic effect of acupuncture may be related to the intervention time and the treatment course. Ruihao's study (73) showed that in the real-world study of comprehensive acupuncture therapy intervention for ischemic stroke, the earlier the intervention of comprehensive acupuncture therapy, the more treatment times, the better the improvement effect on patients' neurological deficits.
To test the robustness of the meta-analysis results, sensitivity analysis was performed by comparing the meta-analysis results under different effect models and the meta-analysis results after removing a single study, and the results showed that the meta-analysis results of each outcome indicator had good robustness.
Overall completeness and applicability of evidence
In this systematic review, all the studies included were undertaken solely in China, with a significant portion of them being published in the Chinese language. However, we acknowledge the possibility that we may have overlooked some pertinent trials, particularly those that were not published in journals indexed by the electronic databases we utilized for our search.
Characteristics of participants
The studies included in this review were primarily conducted in China, limiting the review's generalizability across racial groups. The responsible vessel for cerebrovascular disease, variations in stroke types and severities could potentially modify the effectiveness of acupuncture on stroke patients. Unfortunately, given the constraints, including the scarcity of studies focusing on specific cerebral blood vessel, inconsistent reporting of stroke severity across trials, and ambiguity in defining the timing of treatment initiation post-stroke, it was not feasible to conduct predetermined subgroup analyses comparing patients with varying stroke severities or those who began treatment at different time points after their stroke. Consequently, the findings may not fully capture the nuances of acupuncture's impact across diverse stroke populations and treatment timelines.
The highlights of this study
Currently, no meta-analysis of acupuncture treatment for sensory disorders after stroke has been found to be publicly published. This study is based on clinical needs, formulates rigorous retrieval strategies and inclusion and exclusion criteria, and conducts a comprehensive search in 14 commonly used domestic and international databases and clinical trial registration websites, strictly following the principle of double-blind independent work in literature screening, data extraction, and quality evaluation. Internationally recognized tools, the Jadad scale and the modified RoB tool, are used to comprehensively and objectively evaluate the quality of the included RCTs.
Limitations
This systematic review and meta-analysis also had several limitations. First, this study only included articles conducted in China, which might limit the reliability and global applicability of our findings. When discussing the applicability of acupuncture among non-Chinese populations, the cultural factors or clinical practice variations cannot be overlooked. Acupuncture originated from Traditional Chinese Medicine (TCM), within the framework of the Yin-Yang and Five Elements theory. It may be challenging for non-Chinese populations to comprehend the theories of TCM. Additionally, shortages of skilled personnel and a lack of foundational research pose challenges to the internationalization of acupuncture. On the other hand, eastern and western cultures have distinct characteristics. Asians, especially Chinese people under the traditional Chinese medicine framework, may experience a stronger placebo effect. Experimental designs to exclude acupuncture placebo effects are constantly improving, with methods like fake needles and sham acupoints seeking better forms to minimize placebo effects. Based on studies conducted solely with Chinese participants, we may overestimate the true efficacy and safety of acupuncture. Second, only a small portion of the included literature reported adverse events and the reports lacked detail. The lack of reporting on adverse events may increase patient risks, lead to an underestimation of treatment-related injuries and thereby affect clinical decision-making. Third, the methodological quality of the evidence in this study was not high. Only one included trial reported the implementation of allocation concealment. Moreover, due to the particularity of acupuncture, it is difficult to implement a blind design. The lack of blinding and randomization concealment may lead to selective reporting bias, exaggerating treatment effects or underestimating adverse reactions. No studies included a placebo-controlled group, which significantly impacted the assessment of efficacy and posed a considerable limitation when drawing conclusions about the overall effectiveness of acupuncture. Fourth, there was high heterogeneity in the data, which may limit the generalizability of the findings.
Inspiration and suggestions for future research
First, it is recommended to enhance international communication and develop a unified acupuncture protocol. We suggest that future clinical trials conducting multicenter trials involving diverse populations to improve external validity. Second, we suggest that future clinical trials could systematically collect and report safety outcomes. Third, we suggest that future clinical trials can refer to the corresponding methodological quality evaluation tools for design, and the design in aspects such as random sequence generation, concealment, and blinding should be more scientifically rigorous. Furthermore, the formulation of inclusion criteria should refer to the internationally recognized diagnostic criteria. The baseline data of the included samples should be basically consistent, and the gender, age, course of disease, and severity of the disease of the included patients should be recorded in detail, and the intervention measures and outcome measurement information should be reported as detailed as possible in the registered trial protocol. It is meaningful for future studies to explore innovative methods to simulate the sensation of acupuncture and ensure the effectiveness of blinding. In conclusion, we propose that future research establish a standardized acupuncture protocol to minimize heterogeneity. We hope a scientific and rigorous research paradigm will emerge, promoting practical acupuncture applications both in and outside China, revealing its exact meridian mechanisms.
Conclusion
The best available clinical research evidence indicates that acupuncture for sensory disorders after stroke has certain advantages over the control group in improving efficiency, alleviating sensory disorders, reducing pain, enhancing daily living abilities, and relieving neurological deficits. Additionally, the adverse reactions in acupuncture group were acceptable and the incidence of adverse events is lower than in the control group. However, due to the low quality of the evidence, clinical decision-making should still be made with caution. More high-quality clinical trials are still needed in the future to further verify the clinical efficacy and safety. In order to enhance the universality of acupuncture and promote the dissemination of traditional Chinese medicine worldwide, we look forward to the initiation of more international clinical trials regarding acupuncture treatment for stroke.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SR: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. YC: Data curation, Investigation, Writing – original draft. YL: Data curation, Investigation, Writing – original draft. QL: Data curation, Investigation, Writing – original draft. JP: Data curation, Formal analysis, Investigation, Writing – original draft. LS: Formal analysis, Writing – original draft. YZ: Methodology, Writing – review & editing. HZ: Conceptualization, Supervision, Writing – review & editing. XC: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China, Grant Number: 81904285.
Acknowledgments
We acknowledge Prof. Ying Gao for her assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1504215/full#supplementary-material
References
2. WHO. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
3. Ji'an L, Jinxi Z. Practical New Course of Traditional Chinese Internal Medicine. Beijing: China Press of Traditional Chinese Medicine (2018).
4. Kessner SS, Schlemm E, Cheng B, Bingel U, Fiehler J, Gerloff C, et al. Somatosensory deficits after ischemic stroke. Stroke. (2019) 50:1116–23. doi: 10.1161/STROKEAHA.118.023750
5. Lv Q, Zhang J, Pan Y, Liu X, Miao L, Peng J, et al. Somatosensory deficits after stroke: insights from MRI studies. Front Neurol. (2022) 13:891283. doi: 10.3389/fneur.2022.891283
7. Wei XY, Wang X, Shi GX, Tu JF, Yang JW, Ren MM, et al. Acupuncture modulation of chronic neuropathic pain and its association with brain functional properties. J Pain. (2024) 25:104645. doi: 10.1016/j.jpain.2024.104645
8. Kim H, Mawla I, Lee J, Gerber J, Walker K, Kim J, et al. Reduced tactile acuity in chronic low back pain is linked with structural neuroplasticity in primary somatosensory cortex and is modulated by acupuncture therapy. Neuroimage. (2020) 217:116899. doi: 10.1016/j.neuroimage.2020.116899
9. Lee H, Lee J, Jung D, Oh H, Shin H, Choi B. Neuroprotection of transcranial cortical and peripheral somatosensory electrical stimulation by modulating a common neuronal death pathway in mice with ischemic stroke. Int J Mol Sci. (2024) 25:7546. doi: 10.3390/ijms25147546
10. Kong JC, Lee MS, Shin BC, Song YS, Ernst E. Acupuncture for functional recovery after stroke: a systematic review of sham-controlled randomized clinical trials. CMAJ. (2010) 182:1723–9. doi: 10.1503/cmaj.091113
11. Park J, Hopwood V, White AR, Ernst E. Effectiveness of acupuncture for stroke: a systematic review. J Neurol. (2001) 248:558–63. doi: 10.1007/s004150170132
12. Zhang JH, Wang D, Liu M. Overview of systematic reviews and meta-analyses of acupuncture for stroke. Neuroepidemiology. (2014) 42:50–8. doi: 10.1159/000355435
14. Sterne J, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
15. Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015
16. Zhenya J, Changdu L, Yingkun L. Treatment of postapoplectic thalamic spontaneous pain by electroacupuncture at huatuojiaji points. J Tradit Chin Med. (1999) 3:195–9. doi: 10.19852/j.cnki.jtcm.1999.03.008
17. Yongfeng L, Xiaoming M, Bing Y, Yanhua G, Shaoyun Z, Xiaodan R. Warm needling on the four knee acupoints combined with Chinese herb in the treatment of knee pain after stroke. World J Acupunct-Moxibustion. (2015) 25:21–5. doi: 10.1016/S1003-5257(15)30059-3
18. Youjia S. A rehabilitation effect of acupuncture on stroke. Clin J Chin Med. (2018) 10:22–3. doi: 10.3969/j.issn.1674-7860.2018.01.010
19. Xue Z, Xiaonong F, Ding L, Haitao Z, Lianzhong W, Hairong W. Acupuncture treatment of regulating spirit, acticating blood and relieving pain for thalamic pain. Chin Acupunct. Moxibustion. (2010) 30:367–70. doi: 10.13703/j.0255-2930.2010.05.005
20. Siwei L, Zhilong Z, Chaoqi Y. 41 cases of hemianesthesia in ischemic stroke treated with electroacupuncture combined with western medicine. Tradit Chin Med Res. (2020) 33:53–5. doi: 10.3969/j.issn.1001-6910.2020.09.19
21. Hui J, Hongdu W. Clinical effect of activating blood and dredging collaterals combined with restoring consciousness and opening orifices acupuncture on thalamic pain after cerebral infarction. Chin Arch Tradit Chin Med. (2020) 38:89–91. doi: 10.13193/j.issn.1673-7717.2020.03.02
22. Wenfeng H. Clinical study of Mongolian medical acupuncture therapy for cerebral infarction (SAK disease). China Sci Technol J Database. (2022) 12:0153-5. Available at: https://www.cqvip.com/doc/journal/2436614202
23. Kai Y, Yuan X, Guirong Y. Clinical effect of wrist-ankle acupuncture combined with mecobalamin in the treatment of hemianesthesia in patients with ischemic stroke. Elderly Chin. (2021) 41:3917–20. doi: 10.3969/j.issn.1005-9202.2021.18.010
24. Yanhua S, Peizhong X, Xuerui L. Clinical observation of eye needle therapy combined with Tongbi decoction in treatment of limb numbness during stroke recovery. World Latest Med Inf. (2021) 21:287–8. doi: 10.3969/j.issn.1671-3141.2021.81.144
25. Yueguang L, Shanbin S. Clinical observation on the therapeutic effect of acupuncture combined with external application of traditional Chinese medicine on hemianesthesia in patients with cerebral infarction of qi deficiency and blood stasis type. Pharmacy Weekly. (2021) 30:152–3. Available at: https://d.wanfangdata.com.cn/periodical/Ch9QZXJpb2RpY2FsQ0hJTmV3UzIwMjUwMTE2MTYzNjE0EhpRS0JKQkQyMDIxMjAyMTEyMTAwMDAxNjY5MhoIZnJ3ZWJ2bzg=
26. Shushan X. Clinical observation of acupuncture and moxibusition combined with Tongqiao Huatan Xifeng decoction in the treatment of neurological function and HIF-1 A and HSP70 levels in patients with acute cerebral infarction. Guangming J Chin Med. (2021) 36:4140–2. doi: 10.3969/j.issn.1003-8914.2021.24.012
27. Chunxian L. Effect analysis of acupuncture and moxibustion combined with rehabilitation training in treatment of upper limb numbness after cerebral infarction. Chin Community Doctors. (2023) 39:79–81, 87. doi: 10.3969/j.issn.1007-614x.2023.08.027
28. Ying L, Jingmian Y, Yanxia Y, Qixin Z. Clinical effect of acupuncture and medicine in the treatment of thalamic pain in the recovery period of ischemic stroke. World J Integr Trad West Med. (2021) 16:1353–6 + 1361. doi: 10.13935/j.cnki.sjzx.210736
29. Qixin Z, Ying L. Clinical observation on treatment of thalamic pain in convalescent stage of ischemic stroke with acupuncture and medicine. World J Integr Trad West Med. (2021) 16:1119–22 + 1127. doi: 10.13935/j.cnki.sjzx.210627
30. Yu C, Min W. Observation on the efficacy of acupuncture and medicine treatment for 33 cases of thalamic pain in the recovery period after ischemic stroke. Hunan J Tradit Chin Med. (2021) 37:72–4. doi: 10.16808/j.cnki.issn1003-7705.2021.03.025
31. Biao F, Geng Z, Daliang Z. Observation on the efficacy of wrist-ankle acupuncture combined with mecobalamin in the treatment of partial sensory disorder in ischemic Stroke. World Chin Med. (2019) 14:2492–4. doi: 10.3969/j.issn.1673-7202.2019.09.061
32. Likang L, Zhiping H, Weijuan H. Effect of acupuncture on somatosensory evoked potentials in patients with pontime infarction. Zhejiang J Integr Tradit Chin West Med. (2006) 8:467–8. doi: 10.3969/j.issn.1005-4561.2006.08.003
33. Huizi Q, Jin Y. Neurophysiological pain-suppressing effects of acupuncture combined with repetitive transcranial magnetic stimulation on central neuralgia after cerebral infarction. J Shenyang Med Coll. (2019) 21:505–8 + 513. doi: 10.16753/j.cnki.1008-2344.2019.06.004
34. Huizi Q. Application of point-through-point acupuncture combined with TDP irradiation in patients with central pain after cerebral infarction. J Qiqihar Medi Univ. (2019) 40:2742–5. doi: 10.3969/j.issn.1002-1256.2019.21.043
35. Gaobo S, Hui B. Clinical study of dong's qi points treatment of limb numbness after cerebral infarction. China J Chin Med. (2015) 30:1379–80. doi: 10.16368/j.issn.1674-8999.2015.09.477
36. Xiaoming W, Deben Y, Ke X, Guoyuan Z, Chaoqiong L. Effects of acupuncture on evoked potential, concentration of serum neuron-specific enolase and myelin basic protein in patients with cerebral infarction. Chin J Phys Med Rehabil. (2004) 1:33–5. doi: 10.3760/j:issn:0254-1424.2004.01.009
37. Yanli X, Qiang T, Tiehua W. Study on therapeutic effect of head acupuncture combined with acceleration techniques on stroke patients using the SIAS Appraisal table. Neural Injury Funct Reconstr. (2007) 1:23–25. doi: 10.3870/j.issn.1001-117X.2007.01.007
38. Yue'e Z, Xiaojuan Z, Yiqian H, Lianchen Z, Shuxin Y. The impact of scalp acupuncture, oxygen therapy and acupoint pressing on functional recovery of ischemic stroke. Hebei Med J. (2015) 37:2937–9. doi: 10.3969/j.issn.1002-7386.2015.19.017
39. Zhengtao Z, Ling C, Lei Z, Ziling L. Effect of acupuncture on somatosensory evoked potentials in patients with acute cerebral infarction. J Emerg Tradit Chin Med. (2010) 19:1665–6 + 1689. doi: 10.3969/j.issn.1004-745X.2010.10.009
40. Sunsun L, Xun C, Wenjun Z. Clinical observation of rood technique combined with warm needling therapy for sensory impairment after stroke. Chin J Tradit Med Sci Technol. (2021) 28:793–5.
41. Yuanyuan Y, Xiaozhong L, Chunxiang F. Thirty-five cases of limb numbness in recovery time of apoplexy with rolling needling combined with cupping. Henan Tradit Chin Med. (2020) 40:279–82. doi: 10.16367/j.issn.1003-5028.2020.02.0068
42. Huimin M, Aina Y, Yong L, Wenchao Z, Yinzhu G, Weifeng W. Observation on the therapeutic effect of fire needling acupuncture at Yangming meridian points on hemianesthesia in stroke patients. Health Protect Promot. (2022) 22:595–7. doi: 10.3969/j.issn.1671-0223(x).2022.04.011
43. Zekun J, Yuanfeng P, Ting Z, Liangang Y, Na J, Jing L, et al. Clinical study of elongated needle penetrating governor vessel for treating central post-stroke pain. J Emerg Tradit Chin Med. (2021) 30:1192–5. doi: 10.3969/j.issn.1004-745X.2021.07.016
44. Lingling Z, Wei H, Gang L, Ling Z, Guoqing Z, Shiping Z, et al. Clinical effect of Tongdu Tiaoshen acupuncture combined with electroacupuncture in treatment of hemianesthesia after stroke. J Anhui Univ Chin Med. (2020) 39:38–41. doi: 10.3969/j.issn.2095-7246.2020.01.012
45. Lei X, Yue'e H. Clinical research of scalp retention method combined with sensory training in treatment of patients with unilateral sensory disturbance after stroke. J Guizhou Univ Tradit Chin Med. (2020) 42:34–9. doi: 10.16588/j.cnki.issn2096-8426.2020.05.008
46. Ying L, Ting F, Aishu L, Yang C, Ling Y. Clinical study of wrist - ankle electro - acupuncture combined with rTMS in treatment of post - stroke hemidysesthesia. J Clin Acupunct Moxibustion. (2023) 39:45–9. doi: 10.19917/j.cnki.1005-0779.023096
47. Weifeng Z, Yinglin C. Clinical observation on 100 cases of post stroke thalamic pain treated with consciousness-restoring resuscitation acupuncture combined with pregabalin. J Gansu Univ Chin Med. (2023) 40:68–72. doi: 10.16841/j.issn1003-8450.2023.02.15
48. Miaoting L, Chunmei Y, Yan W, Fang M. Clinical observation on the Xingnao Kaiqiao acupuncture combined with repetitive transcranial magnetic stimulation in the treatment of post-stroke thalamic pain. J Guangzhou Univ Tradit Chin Med. (2023) 40:640–6. doi: 10.13359/j.cnki.gzxbtcm.2023.03.018
49. Langmin T, Cuifang L, Rui F, Zhanqin X. Effect of xingnaokaiqiao acupuncture on thalamic pain after stroke and its influence on the levels of peripheral blood 5-HT, VIP and β-EP. J North Sichuan Med Coll. (2023) 38:178–81. doi: 10.3969/j.issn.1005-3697.2023.02.008
50. Zhong Y, Huihui S, Lu Z, Fanghua X, Ting L, Shaoling C, et al. Clinical analysis of consciousness-restoring and obstruction-clearing acupuncture combined with sensory rehabilitation in the treatment of post-stroke sensory impairment. Mod Pract Med. (2021) 33:41–3. doi: 10.3969/j.issn.1671-0800.2021.01.018
51. Suqing W, Binhong D, Wen M. The impact of early rehabilitation combined with acupuncture and moxibustion massage on sensory function and quality of life in patients with sensory impairment after stroke. Mod J Integr Tradit Chin West Med. (2021) 30:2828–31. doi: 10.3969/j.issn.1008-8849.2021.25.022
52. Xiaohong Y. Effect of acupuncture combined with Shentong Zhuyu decoction on the degree of thalamus pain and hemorheology index in stroke recovery period. J Med Inf. (2022) 35:177–9. doi: 10.3969/j.issn.1006-1959.2022.11.047
53. Cui W, Jinglan Z. Effect of combined acupuncture and medicine on pain sense and sensory threshold in patients with central post-stroke pain. Shanghai J Acupunct Moxibustion. (2022) 41:964–9. doi: 10.13460/j.issn.1005-0957.2022.10.0964
54. Wenlu W, Wanling T. Clinical observation of Zhuang medicine lotus needle cupping blood-letting therapy combined with rehabilitation in the treatment of hemianesthesia after stroke. Yunnan J Tradit Chin Med Mater Med. (2022) 43:55–8. doi: 10.16254/j.cnki.53-1120/r.2022.08.021
55. Meifeng F, Feng T, Xuewen Z. The clinical research of wrist-ankle acupuncture combined with rehabilitation training in the treatment of hemidysesthesia after stroke. J Zhejiang Chin Med Univ. (2018) 42:971–4. doi: 10.16466/j.issn1005-5509.2018.11.021
56. Xudong G, Hua W, Jianming F, Jing W, Qinwei M, Hongwei Z, et al. Electro-acupuncture of the scalp combined with sensory re·education for the functional rehabilitation of stroke patients. Chin J Phys Med Rehabil. (2013) 35:5. doi: 10.3760/cma.j.issn.0254-1424.2013.06.012
57. Xiaoyun H, Zhiyong D, Yanting X. Observation of the efficacy and safety evaluation of acupuncture combined with traditional Chinese medicine in the treatment of patients with hemiplegic sensory impairment after stroke. Hebei Med J. (2017) 39:122–3 + 126. doi: 10.3969/j.issn.1002-7386.2017.01.038
58. Juan K, Junhua W, Cui'e L. 40 cases with limb pain after stroke treated by balance acupuncture. Henan Tradit Chin Med. (2015) 35:539–40. doi: 10.16367/j.issn.1003-5028.2015.03.0228
59. Ying K, Yumengxin W, Di W, Hongchao D. Clinical observation of “Dragon and Tiger Battle” acupuncture therapy for thalamic pain after stroke. Guiding J Tradit Chin Med Pharm. (2018) 24:52–4. doi: 10.13862/j.cnki.cn43-1446/r.2018.14.016
60. Ming L, Lingzhi L, Lu M. Clinical observation on restoring consciousness and opening the orifices needling combined with scalp acupuncture electrical stimulation in treating 40 cases of thalamic pain after stroke. J Tradit Chin Med. (2018) 59:861–5. doi: 10.13288/j.11-2166/r.2018.10.012
61. Huizi Q. A study on the effect of acupuncture treatment for patients with central pain after stroke. Contemp Med Symp. (2018) 16:202–3. doi: 10.3969/j.issn.2095-7629.2018.24.146
62. Yanping S, Lei X, Yue'e H. Clinical study on scalp acupuncture combined with rehabilitation training for the treatment of sensory impairment after stroke. Chin J Trauma Disabil Med. (2019) 27:80–2. doi: 10.13214/j.cnki.cjotadm.2019.06.057
63. Hao W, Wei L, Xiaogang Y. Clinical observation on the treatment of central pain after stroke with scalp acupuncture. Chin J Integr Med Cardio-Cerebrovasc Dis. (2015) 13:966–9. doi: 10.3969/j.issn.1672-1349.2015.08.003
64. Hongbin W, Xiaoping P, Jian X, Yao J, Weifei M, Na B, et al. The impact of acupuncture combined with rehabilitation training on limb motor function and daily living ability of stroke patients with hemiplegia. Shaanxi J Tradit Chin Med. (2015) 36:914–6. doi: 10.3969/j.issn.1000-7369.2015.07.077
65. Shumin W. Clinical observation of row/dot needling cutaneous region of meridian sinew combined with needling stellate ganglion treating post-stroke thalamic pain. Acta Chin Med Pharmacol. (2018) 46:81–4. doi: 10.19664/j.cnki.1002-2392.180122
66. Qingxia Z. Analysis of curative effects of pyonex in treatment of sensory disturbance of the end of limbs after stroke. Chin J Tranma Disabil Med. (2014) 22:29–31. doi: 10.13214/j.cnki.cjotadm.2014.06.284
67. Shuping W. Clinical evaluation of the effectiveness of traditional Chinese medicine acupuncture combined with rehabilitation in the treatment of stroke-induced hemiplegia. Capital Food Med. (2019) 26:199–200. doi: 10.3969/j.issn.1005-8257.2019.23.166
68. Xin W. Effect of acupuncture method of modulating and suppressing pain on recovery of motor dysfunction caused by central pain after stroke and serum levels of IL-6 and TNF-α. Int Med Health Guidance News. (2019) 25:1350–2, 1357. doi: 10.3760/cma.j.issn.1007-1245.2019.09.002
69. Jie Z, Yueqin L. Effective observation on treating limb pain in stroke patients by acupuncture at wrist ankle. Clin J Chin Med. (2019) 11:116–8. doi: 10.3969/j.issn.1674-7860.2019.07.047
70. Weiqiang W, Limei C, Ling W. Observation on the therapeutic effect of plum blossom needle combined with well point bloodletting in the treatment of thalamic pain. J Pract Tradit Chin Med. (2009) 25:821. doi: 10.3969/j.issn.1004-2814.2009.12.034
71. Xiaorui Z, Yongqing Z. Clinical observation on the treatment of thalamic pain after stroke with electroacupuncture. Xinjiang J Tradit Chin Med. (2012) 30:44–5. doi: 10.3969/j.issn.1009-3931.2012.04.023
72. Xiuling W, Qian Z, Dingjun C, Yong T, Zhengyu Z. Clinical observation on rehabilitation of nervous functions in the patient of stroke at acute stage treated with acupuncture. Chin Acupunct Moxibustion. (2002) 11:6–8. doi: 10.3321/j.issn:0255-2930.2002.11.002
Keywords: acupuncture, stroke, somatosensory deficits, systematic review, meta-analysis
Citation: Ren S, Chen Y, Liu Y, Lv Q, Peng J, Song L, Zou Y, Zhang H and Chen X (2025) Acupuncture for somatosensory deficits after stroke: a systematic review and meta-analysis. Front. Med. 12:1504215. doi: 10.3389/fmed.2025.1504215
Received: 01 November 2024; Accepted: 20 January 2025;
Published: 07 February 2025.
Edited by:
Redhwan Ahmed Al-Naggar, National University of Malaysia, MalaysiaReviewed by:
Qinwei Henry Fu, McMaster University, CanadaGuido Knapp, Technical University Dortmund, Germany
Peng Wang, Chengdu Integrated TCM and Western Medical Hospital, China
Arnas Tamasauskas, University of Liverpool, United Kingdom
Copyright © 2025 Ren, Chen, Liu, Lv, Peng, Song, Zou, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xing Chen, eWVhaGNoZW5jeUBzaW5hLmNvbQ==; Hua Zhang, bndremhoc2ZAYWxpeXVuLmNvbQ==
†These authors have contributed equally to this work
 Shumeng Ren
Shumeng Ren Yuhang Chen
Yuhang Chen Yu Liu
Yu Liu Qiuyi Lv
Qiuyi Lv Jing Peng
Jing Peng Lei Song
Lei Song Yihuai Zou
Yihuai Zou Hua Zhang
Hua Zhang Xing Chen
Xing Chen