
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med. , 03 February 2025
Sec. Dermatology
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1419922
 Binglin Cui1†
Binglin Cui1† Jing Lin2†
Jing Lin2† Yuanchun Huang3
Yuanchun Huang3 Huachen Zhu4,5,6
Huachen Zhu4,5,6 Jinbo Zou7
Jinbo Zou7 Jiesheng Qin8
Jiesheng Qin8 Hui Pan9,10*
Hui Pan9,10* Jian Chen11*
Jian Chen11*Background: Tumor necrosis factor blockers can suppress immune system and lead to various adverse drug reactions, including deaths. We present a rare case of dysgeusia, strawberry tongue, and psoriasis-like eruptions after simultaneous administration of adalimumab, sulfasalazine, and etoricoxib.
Case description: A 36 year-old male with ankylosing spondylitis presented with progressive loss of taste for 3 months and rashes on his upper trunk for 5 days. He had been receiving adalimumab, sulfasalazine, and etoricoxib for 9 months. After self-discontinuing the medicines, the rashes gradually subsided. On examination, swollen and red strawberry tongue were noticed. Acinetobacter pittii was isolated by sputum culture. The patient refused any treatment. During follow-up, recurrent dispersed papules/macules and desquamation appeared on his upper trunk, with erythema and erosion in umbilical region. Subsequently, generalized scalp erythema, exudates, scabs, hair bundles, redness and desquamation behind ears occurred. The tongue, taste, and skin lesions resolved sequentially and steadily until complete recovery.
Outcome: He remained in remission during 4 years follow-up. The total course of disease was around 10 months.
Discussion: Clinicians should be cautious of the adverse drug reactions/events due to adalimumab, sulfasalazine, and etoricoxib. Rational use of medicines is advocated.
Tumor necrosis factor (TNF) blockers, comprising etanercept, infliximab, adalimumab, certolizumab pegol, and golimumab, have been well-recognized as one of the most promising therapies for various inflammatory diseases, including ankylosing spondylitis. Patients receiving TNF blocker regimen which inhibits immune system are at increased risk of diversified adverse drug reactions or events (including rashes, severe infections, and even deaths), especially when taking concomitant immunosuppressants (1–3). Herein, we report a unique case of dysgeusia, strawberry tongue, and psoriasis-like eruptions after simultaneous administration of adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis.
A 36 year-old Chinese male presented with aggravating loss of taste for 3 months and rashes on his upper trunk for 5 days at Shantou Longhu People’s Hospital in September 2019. He was diagnosed with ankylosing spondylitis for 7 years spinal pain in October 2018 and thereafter was initiated on therapy with subcutaneous injection of adalimumab (40 mg every 3 weeks), oral sulfasalazine (1 g twice per day), and oral etoricoxib (60 mg every 2 days) after careful exclusion of any pre-existent infections. Decreased saliva, dry lips, tongue numbness, and loss of taste appeared in June 2019; blisters occurred on the dorsum of swollen tongue in July 2019 (Figure 1). His tongue became painful and more swollen, and small red maculae and maculopapular scattered around his upper trunk 5 days before the visit (Figure 1). After self-discontinuation of the medicines, the pain and swelling of tongue were alleviated noticeably despite of no apparent change in his taste; the rashes gradually subsided, and his fingers were desquamated bilaterally. From the onset of illness, he occasionally had productive cough of yellow sputum and night sweats without fever/chills. He denied any histories of hepatitis, tuberculosis, sexually transmitted diseases, food/medicine allergies, or recent intake of other medications, but had occasional alcohol consumption and cigarette smoking. His brother had ankylosing spondylitis as well but rejected any treatment. Other family members were generally healthy.

Figure 1. Clinical manifestations of adverse drug events caused by combination therapy with adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis. (A) Strawberry tongue; (B) Small red maculae and maculopapular scattering on the neck; (C) Swollen and red strawberry tongue with visible teeth marks on the edge; (D) Erythema and erosion in umbilical region; (E,F) Dispersed papules/macules and desquamation in armpit and on upper arm; (G) Generalized scalp erythema, exudates, scabs, hair bundles, redness and desquamation behind ears; (H) Scalp pustules, desquamation, and fissures, in addition to dryness and desquamation around ear.
On examination, dry lips, swollen and red strawberry tongue with visible teeth marks on the edge were noticed (Figure 1); submandibular and cervical lymph nodes were enlarged but non-tender to palpation. Other physical examinations were unremarkable.
His main laboratory results are summarized in Supplementary Material 1. Very low titer of antibodies to dust mite (0.43; reference range: < 0.35) was detected in a 19-item screening test for allergens. Cervical ultrasound showed bilateral and multiple hypoechoic nodules, indicating reactive lymphadenopathy. Chest X-ray and ultrasound on heart, liver, gallbladder, pancreas, spleen, and urinary system were basically normal. Acinetobacter pittii was isolated by sputum culture. No pathogenic pathogens (i.e., normal flora) were found through wide-spectrum gene sequencings from tongue coating, sputum, saliva, and urine specimens. Nasopharyngoscopy revealed diffused swellings of tongue root, epiglottis, laryngeal cavity, and aryepiglottic mucosa, adhered by viscous purulent phlegm. The patient refused any treatment for unknown etiology.
During our first follow-up in November 2019, the superficial blisters on his tongue shrank or vanished, along with improvement in taste; however, recurrent dispersed papules/macules and desquamation appeared on/in his face and bilateral armpits/upper arms, accompanied by erythema and erosion in umbilical region (Figure 1). In February 2020, the patient consulted us again for generalized scalp erythema, exudates, scabs, hair bundles, redness and desquamation behind ears without pain/fever in recently 2 weeks, although the tongue and taste mostly recovered and the rashes in/on bilateral armpits/upper arms generally disappeared (Figure 1). Imaging examination of the skin lesions on his head and trunk demonstrated dotted and annular vascular distributions and yellow pustules under red background of skin lesions, with slight fluorescence under Wood’s lamp. The patient refused further skin biopsy and pathogen identification, but accepted skin care and oral vitamins. In March 2020, the scalp exudates decreased, but there were still pustules, scalp desquamation and fissures, in addition to dryness and desquamation around his ears (Figure 1). In April 2020, the skin lesions resolved steadily until complete recovery. He remained in remission during 4 years follow-up. The total course of disease was nearly 10 months (Figure 2). Written informed consent was obtained from the patient. This study was approved by the Ethics Committee of Shantou Longhu People’s Hospital.
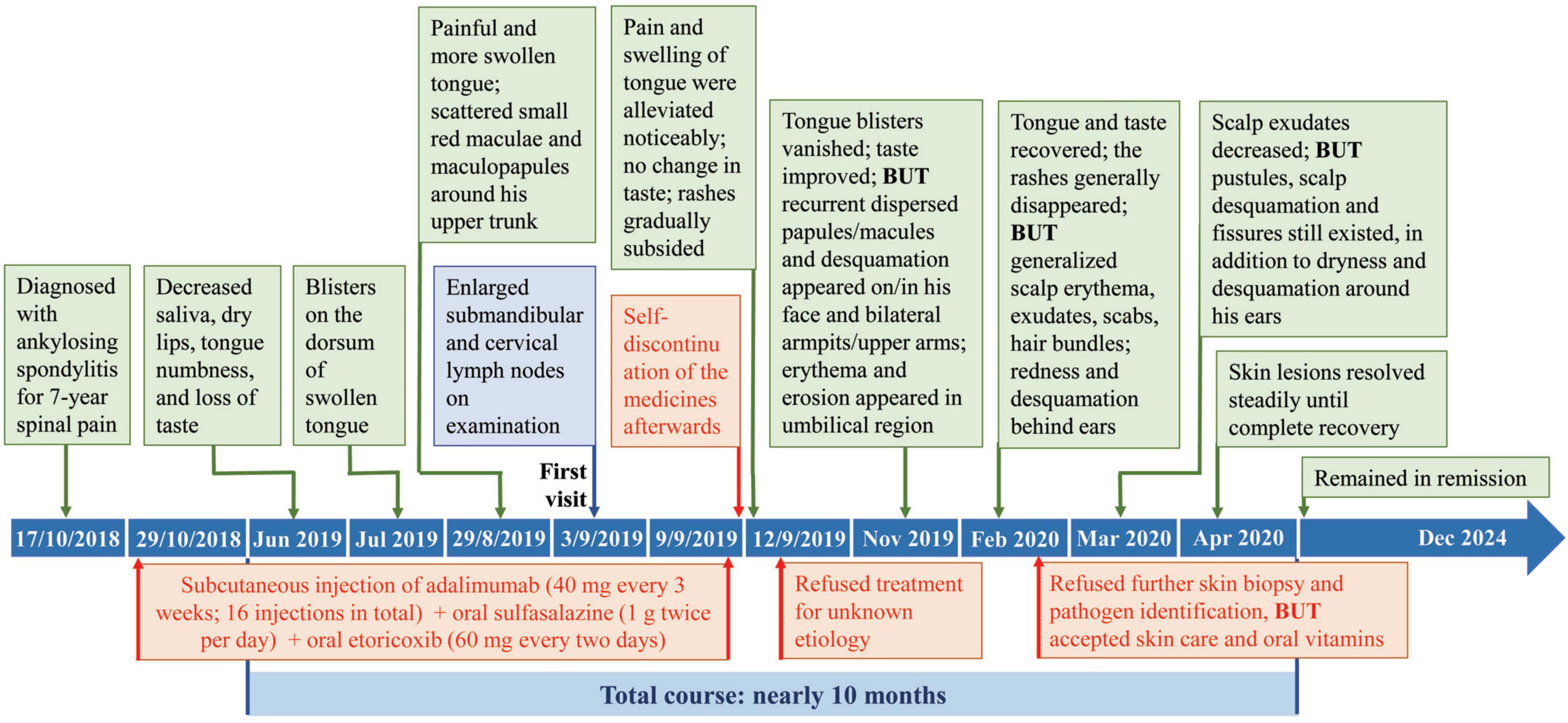
Figure 2. Disease progression after simultaneous use of adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis.
To the best of our knowledge, there is no report of an ensemble of strawberry tongue, dysgeusia, and similar systemic skin lesions in the literature. Therefore, this unusual case needs careful differentiation of a variety of conditions/diseases, including infections, allergy, immune diseases, tumors, and adverse drug reactions.
Strawberry tongue is mostly a result of bacterial toxin-mediated disorders (e.g., scarlet fever, recurrent toxin-mediated perianal erythema, and recalcitrant erythematous desquamating disorder), in addition to viral infection [e.g., yellow fever and coronavirus disease-2019 (COVID-19)] and non-infectious disorders (e.g., Kawasaki disease and food/drug allergies) (4, 5). The manifestations of chronic afebrile generalized papules/macules, pustules, and desquamation (no perianal erythema or desquamation) in our adult patient with no food allergies, normal vital signs and antistreptolysin O titer before the outbreak of COVID-19 do not support a diagnosis of the abovementioned diseases except for adverse drug reaction (differential diagnosis shown in Table 1).
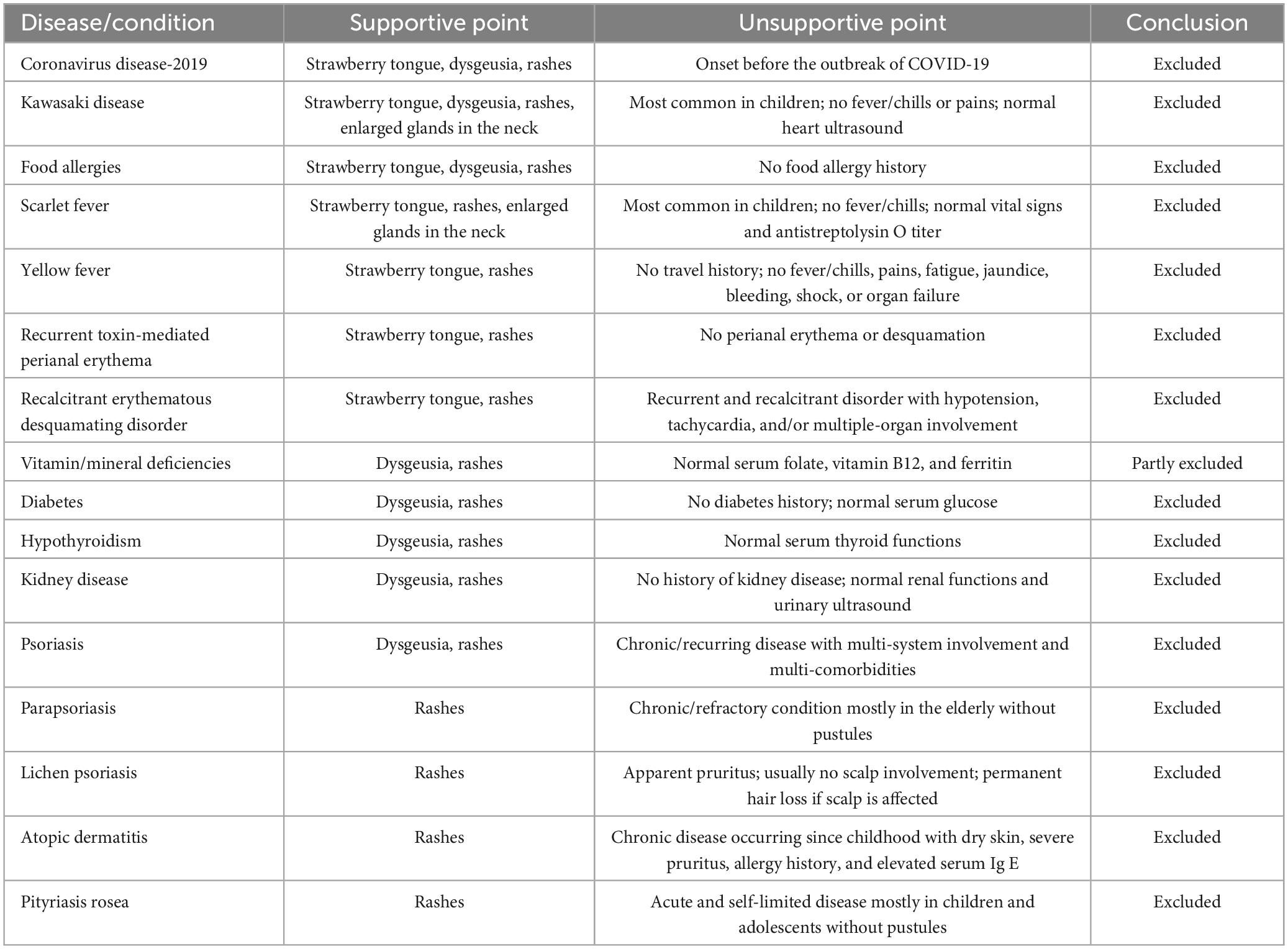
Table 1. Differential diagnosis of adverse drug events caused by simultaneous use of adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis.
Dysgeusia can be caused by various factors, including aging, medications (e.g., immunosuppressants), high alcohol consumption, tobacco use, bacterial/viral/fungal infections (e.g., COVID-19), vitamin/mineral deficiencies, nerve damage, neurologic disorders (e.g., Alzheimer’s disease), diabetes, hypothyroidism, and kidney disease (6, 7). However, certain treatments or medications are usually the predominant cause of dysgeusia (7) and the highly suspected cause of dysgeusia in this case as well, since most of the other causes have been ruled out (Table 1).
Similarly, the skin lesions should be differentiated from varied dermatological diseases. The self-limited feature of generalized rashes with strawberry tongue and dysgeusia in our case is not consistent with psoriasis, parapsoriasis, lichen psoriasis, atopic dermatitis, and pityriasis rosea (Table 1).
Tumor necrosis factor blockers have been reported to induce paradoxically inflammatory psoriasis and/or lichen psoriasis (1, 3). Correspondingly, sulfasalazine as an anti-rheumatic agent and etoricoxib as a cyclooxygenase-2 inhibitor have similar profiles of adverse drug reactions, including rashes, serious infections, and hypersensitivity reactions (e.g., Stevens-Johnson syndrome, vasculitis, and parapsoriasis) (8, 9). Considering their pharmacological mechanisms, the reported similar adverse drug reactions, and gradual recovery and complete remission after cessation of the medicines, the triad-drug therapy might have triggered immunosuppression, opportunistic respiratory infection of Acinetobacter pittii, and the adverse drug events as dysgeusia, strawberry tongue, and psoriatic eruptions. The natural course of the disease without aggressive interventions subject to the willingness of the patient has provided us an invaluable opportunity to understand the dynamic changes of the adverse drug reactions. Administrations of intravenous immunoglobulins and/or topical treatment (corticosteroids, keratolytics, and vitamin D analogs) may help with alleviation of symptoms (1, 10).
This report has illuminated an unusual case of dysgeusia, strawberry tongue, and psoriasis-like eruptions after combination treatment with adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis. Clinicians should be alert to the adverse drug reactions caused by the combination treatment with adalimumab, sulfasalazine, and etoricoxib. Rational use of TNF blockers as well as anti-inflammatory medicines is advocated.
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Ethics Committee of Shantou Longhu People’s Hospital, Shantou, Guangdong, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
BC: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Validation, Writing–original draft, Writing–review and editing. JL: Conceptualization, Data curation, Investigation, Methodology, Resources, Validation, Writing–original draft, Writing–review and editing. YH: Data curation, Investigation, Methodology, Resources, Validation, Writing–original draft, Writing–review and editing, Project administration. HZ: Data curation, Investigation, Resources, Validation, Writing–original draft, Writing–review and editing, Methodology. JZ: Data curation, Investigation, Methodology, Resources, Validation, Writing–original draft, Writing–review and editing. JQ: Data curation, Investigation, Methodology, Resources, Validation, Writing–original draft, Writing–review and editing. HP: Data curation, Investigation, Methodology, Resources, Validation, Writing–original draft, Writing–review and editing, Conceptualization, Funding acquisition, Project administration, Supervision. JC: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing–original draft, Writing–review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the 2020 Guangdong Provincial Funds (grant no. 2020A111129021) and the 2020 Li Ka-Shing Foundation Cross-Disciplinary Research Grant (grant no. 2020LKSFG11C).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1419922/full#supplementary-material
1. Ciccarelli F, De Martinis M, Sirufo M, Ginaldi L. Psoriasis induced by anti-tumor necrosis factor alpha agents: A comprehensive review of the literature. Acta Dermatovenerol Croat. (2016) 24(3):169–74.
2. Solovan C, Chiticariu E. Psoriasis, anti-tumor necrosis factor therapy, and tuberculosis: Report of three challenging cases and literature review. Infect Dis Ther. (2013) 2(1):59–73. doi: 10.1007/s40121-013-0003-9
3. Asarch A, Gottlieb A, Lee J, Masterpol K, Scheinman P, Stadecker M, et al. Lichen planus-like eruptions: An emerging side effect of tumor necrosis factor-alpha antagonists. J Am Acad Dermatol. (2009) 61(1):104–11. doi: 10.1016/j.jaad.2008.09.032
4. Adya K, Inamadar A, Palit A. The strawberry tongue: What, how and where? Indian J Dermatol Venereol Leprol. (2018) 84(4):500–5. doi: 10.4103/ijdvl.IJDVL_57_17
5. Young T, Shaw K, Shah J, Noor A, Alperin R, Ratner A, et al. Mucocutaneous manifestations of multisystem inflammatory syndrome in children during the COVID-19 pandemic. JAMA Dermatol. (2021) 157(2):207–12. doi: 10.1001/jamadermatol.2020.4779
6. Risso D, Drayna D, Morini G. Alteration, reduction and taste loss: Main causes and potential implications on dietary habits. Nutrients. (2020) 12(11):3284. doi: 10.3390/nu12113284
7. Jafari A, Alaee A, Ghods K. The etiologies and considerations of dysgeusia: A review of literature. J Oral Biosci. (2021) 63(4):319–26. doi: 10.1016/j.job.2021.08.006
8. Chen J, Lin S, Liu C. Sulfasalazine for ankylosing spondylitis. Cochrane Database Syst Rev. (2014) 2014(11):CD004800. doi: 10.1002/14651858.CD004800.pub3
9. Edel J, Vered M, Grinstein-Koren O, Porat D, Lukach L, Pettesh J, et al. Oral adverse reactions associated with etoricoxib, a common pain medication. J Am Dental Assoc. (2019) 150(6):556–61. doi: 10.1016/j.adaj.2019.01.028
Keywords: dysgeusia, strawberry tongue, psoriasis-like eruption, adalimumab, adverse drug reaction, case report
Citation: Cui B, Lin J, Huang Y, Zhu H, Zou J, Qin J, Pan H and Chen J (2025) Case report: dysgeusia, strawberry tongue, and psoriatic eruptions after combination treatment with adalimumab, sulfasalazine, and etoricoxib for ankylosing spondylitis. Front. Med. 12:1419922. doi: 10.3389/fmed.2025.1419922
Received: 22 April 2024; Accepted: 16 January 2025;
Published: 03 February 2025.
Edited by:
Takemichi Fukasawa, The University of Tokyo Graduate School of Medicine, Tokyo, JapanReviewed by:
Po Cheng Shih, Changhua Christian Hospital, TaiwanCopyright © 2025 Cui, Lin, Huang, Zhu, Zou, Qin, Pan and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Pan, bWljaGFlbGh1aXBhbkAxNjMuY29t; Jian Chen, ZHJjaGVuQHN0dS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.