- Intensive Care Unit, Zhongshan City People's Hospital, Zhongshan City, China
Background: Electrical impedance tomography (EIT) evaluates lung function by providing continuous, real-time monitoring of regional lung ventilation distribution to guide the restoration of lung ventilation. Patients with obesity who are dependent on mechanical ventilation often struggle with weaning. This case report highlights the potential of EIT to guide the weaning of ventilator-dependent patients in an obese patient with severe pneumonia.
Case summary: A 23-year-old male obese patient was admitted to Zhongshan People’s Hospital in November 2023 due to progressive dyspnea. He suffered from recurrent fever and worsening oxygenation and had a 20+ year history of syringomyelia. Combined with abnormal computed tomography imaging, the discovery of a viral infection in the bronchoalveolar lavage fluid, and next-generation sequencing results, he was diagnosed with severe pneumonia. In addition to conventional treatment, EIT was used to guide him through postural changes and ventilation recovery. EIT-informed prone positioning improved ventilation distribution and facilitated successful ventilator weaning on day 26. The patient was discharged after recovering spontaneous respiratory function.
Conclusion: EIT may help ventilator-dependent obese patients achieve tailored targets to improve ventilatory outcomes.
Introduction
Obesity is at epidemic levels in the majority of countries in the world, significantly impacting respiratory mechanics and predisposing individuals to atelectasis and prolonged mechanical ventilation (1). Unfortunately, authorities’ guidelines lack specific recommendations for weaning obese patients from ventilation (2). One of the greatest challenges in critically ill patients with obesity is the optimization of mechanical ventilation, and the controversy surrounding weaning revolves around the utilization of PEEP/CPAP during spontaneous breathing trials (SBTs). Severe pneumonia often leads to respiratory failure because lung damage caused by infection reduces the efficiency of oxygen exchange. Patients with respiratory failure are unable to maintain normal breathing on their own and often rely on mechanical ventilation to support respiratory function (3). Electrical impedance tomography (EIT) is a non-invasive, radiation-free bedside imaging technique that enables real-time monitoring of ventilation dynamics, thereby facilitating precise adjustment of mechanical ventilation settings (4). It has been suggested that EIT has the potential to mitigate lung injury in patients with respiratory distress and, when combined with esophageal manometry, can reduce the mortality rate by approximately 50% in obese patients with respiratory failure (5). In this case report, we present a rare case of severe pneumonia in an obese patient with a long history of syringomyelia who received EIT guidance to assist with ventilator weaning under conventional anti-infective therapy.
Case presentation
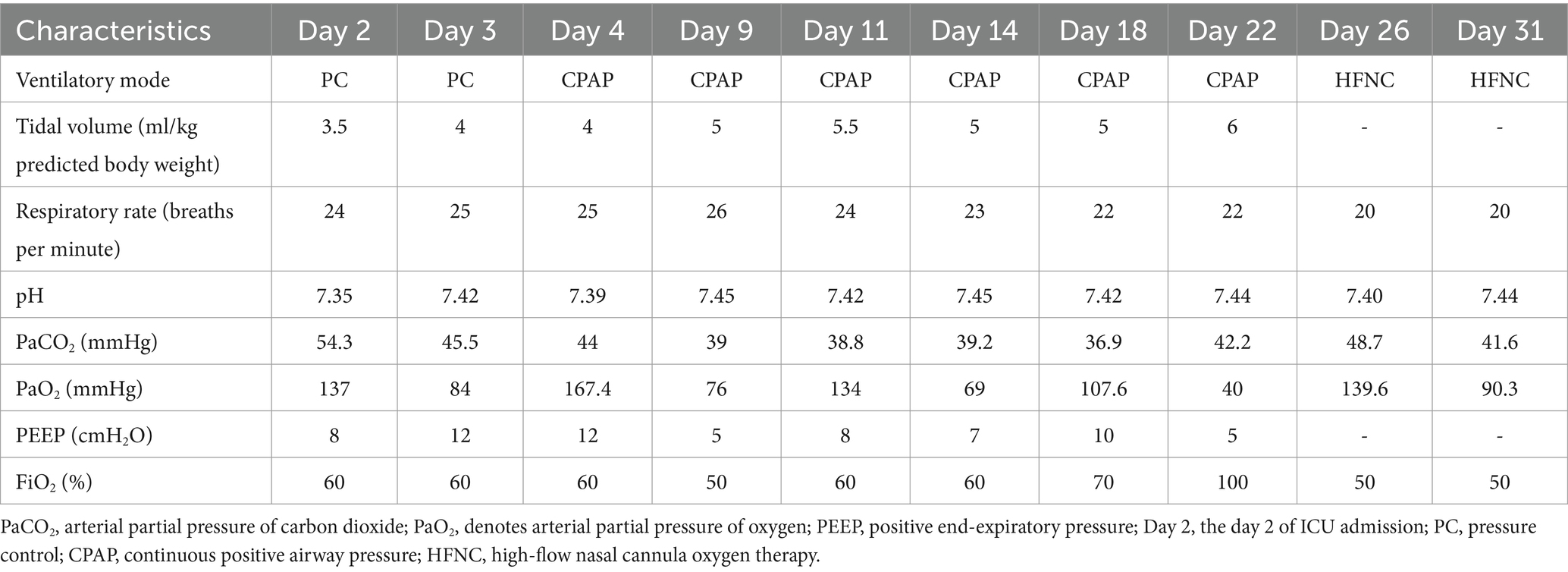
A 23-year-old man with a body mass index (BMI) of 42.9 kg/m2 was transferred to Zhongshan People’s Hospital in November 2023 due to progressive dyspnea of 1 week with cough and fever. The patient had self-administered cold medication for an unprovoked cough and phlegm 1 week before admission, followed by the onset of fever 3 days before admission. The patient also had a 20+ year history of syringomyelia. On admission, the patient was conscious and sedated, with pupils having a diameter of approximately 3 mm and sensitive to light reflexes, coarse lung sounds, minimal wet rales, regular cardiac rhythm, absent abdominal tenderness, diminished bowel sounds, non-edematous lower limbs, and intermittent tremors. Vital signs revealed tachycardia (137/min), hypertension (166/76 mmHg), tachypnea (42/min), hyperthermia (40.2°C), and maintained oxygen saturation at 95% under mechanical ventilation. Next-generation sequencing (NGS) results of bronchoalveolar lavage fluid suggested Acinetobacter baumannii, Morganella, and influenza B virus infection. There were multiple abnormalities in the patient’s blood gas analysis and laboratory test indicators at the time of admission (Supplementary Table S1). A chest computed tomography (CT) showed severe pneumonia mainly in the inferior lung lobes (Figure 1). He was then diagnosed with severe pneumonia.
The patient subsequently underwent routine lung protective ventilation and anti-infection therapy. In addition, EIT (PulmoVista 500 system by Dräger Medical, Lübeck, Germany) was conducted to guide the position. The measurement revealed suboptimal ventilation in the dorsal regions (Figure 2A). On day 3, a chest X-ray showed increased bilateral lung exudation and consolidation in the lower lobes. As the oxygenation further declined, we utilized a prone position with the head up and feet down at 30° for 16 h daily as EIT showed the most even ventilation distribution across all four regions in this configuration (Figure 2B). Starting on day 4, the parameters of the ventilator were gradually lowered to prepare for weaning. On day 7, optimal ventilation in an upright position according to EIT (Figure 2C) prompted sitting respiratory training. On day 8, the prone position was discontinued as EIT showed nearly normalized ventilation distribution. On day 9, the patient had weaning attempts that failed with obvious shortness of breath. Starting on day 11, the patient had recurrent fevers, which made weaning more difficult at this time, and began to use EIT to assist with pulmonary rehabilitation training. On day 26, the patient performed a successful SBT when 5 cm H2O PEEP during SBTs and was extubated to 5 cm H2O mask CPAP. The tracheal intubation was safely removed, and subsequently, the patient transitioned to nasal high-flow oxygen therapy. On day 28, EIT showed increased ventilation with uniform distribution (Figure 2D). With the help of an electric lift-off shift weighing machine, the patient independently completed the transfer from the bedside to the wheelchair (Figure 3). In addition, the respiratory parameters gradually normalized from day 2 to day 31 (Table 1). Meropenem was continued for anti-infection treatment, along with expectoration assistance, nutritional support, and rehabilitation exercises. On day 39, he was discharged from the hospital.
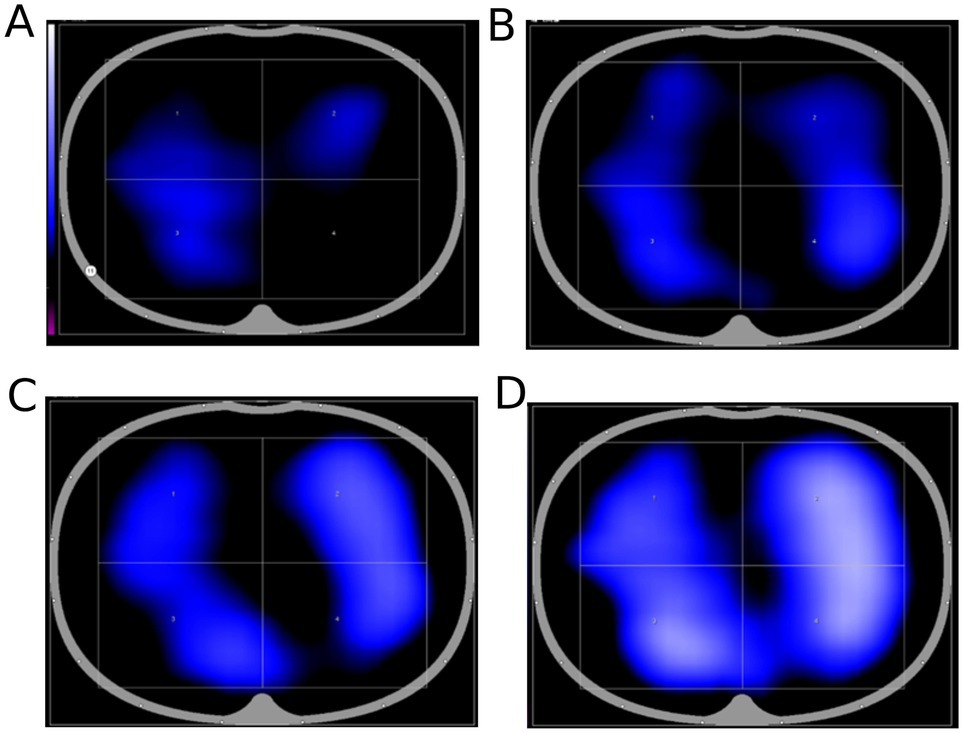
Figure 2. EIT measurements show ventilation in the dorsal area. (A) EIT assessment of ventilation function in the 45° lateral decubitus position; (B) EIT assessment of ventilation function in the prone position on day 3; (C) EIT assessment of ventilation function in the prone position on day 7; and (D) EIT assessment of ventilation function in successful weaning on day 28.
Discussion
This case highlights the role of EIT in guiding the routine treatment of obese patients with severe pneumonia to achieve ventilator weaning. Guided by EIT, we meticulously optimized the patient’s ventilation position and actively facilitated early mobilization. At the outset, EIT measurements found poor ventilation in dependent regions, especially in the lower right lobe in the lateral decubitus position and in the dorsal regions in the supine position.
Therefore, we started in the early prone position and enhanced vibratory stimulation of the lower right lung to facilitate the expectoration of phlegm until it alleviated inhomogeneous ventilation distribution and improved dependent region ventilation. Since the dependent regions’ ventilation had improved, especially the lower right region, the percentage of ventilation increased from 1 to 18% on day 7, and the prone position was terminated on day 8. After the failure of weaning on day 9, considering the continuous mechanical ventilation of the patient after admission and the reduction of respiratory muscle work, along with the resulting atrophy, we intensified pulmonary rehabilitation training, including abdominal breathing, diaphragmatic breathing, vibration expectoration, and upper limb resistance training. In the orthostatic position, the EIT-monitored ventilation area was the largest and the ventilation distribution was the most homogenous. Thus, the patient received early mobilization, starting with sitting up in bed and gradually progressing to sitting at the bedside and in a wheelchair. Combined with anti-infective therapy, the obese patient underwent a successful extubation procedure and made a full recovery.
The present case report aligns with existing medical literature that has highlighted the challenges faced by obese patients with pneumonia during mechanical ventilation and the benefits of using advanced technologies to optimize their care. EIT can dynamically evaluate the changes in regional pulmonary ventilation in patients with mechanical ventilation during weaning, which is helpful in predicting the outcome of weaning. Kacmarek et al. have indicated that EIT is an essential tool to systematically assess respiratory system mechanics, to safely adjust relatively high levels of positive end-expiratory pressure (PEEP), and to improve the chances of successful weaning of obese patients (6). When compared with the use of a decremental best compliance PEEP and esophageal manometry, EIT has been shown to result in the same PEEP setting when performed in a sequential manner (7). Rubin et al. have demonstrated that incorporating EIT into a multimodal approach to individualizing ventilator management can improve outcomes, particularly in obese patients (8). EIT found that early activity and physical therapy in severe patients could improve dorsal ventilation, promote lung re-expansion, and slowly increase end-respiratory lung volume (9).
The primary strength of EIT lies in its real-time, non-invasive, and radiation-free capability to assess regional ventilation distribution, allowing for precise and individualized positioning strategies to optimize oxygenation and facilitate weaning from mechanical ventilation (10). In this case, EIT guided the adoption of prone positioning with a 30° head-up tilt, significantly improving ventilation distribution and facilitating the patient’s successful weaning from the ventilator on day 26. This tailored approach addresses the patient’s unique physiological challenges associated with severe pneumonia, emphasizing the clinical value of EIT in enhancing ventilator management. In addition, an early activity program under the guidance of EIT is also essential to the patient’s recovery. The implementation of early mobilization and rehabilitation programs in critically ill patients has been shown to reduce ICU-acquired weakness, improve functional outcomes, and potentially shorten the duration of mechanical ventilation (11).
Conclusion
In conclusion, this study suggests that EIT may improve ventilation outcomes in obese patients with pneumonia through tailored positioning, and early mobilization and rehabilitation based on EIT findings may accelerate recovery. EIT in the care plan facilitates ventilation management in obese patients who underwent mechanical ventilation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Zhongshan City People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YL: Project administration, Writing – original draft. RL: Data curation, Supervision, Writing – original draft, Writing – review & editing. BL: Data curation, Writing – review & editing. LC: Methodology, Writing – review & editing. JH: Writing – review & editing. WZ: Data curation, Methodology, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1505114/full#supplementary-material
References
1. Syed, MKH, Selickman, J, Evans, MD, Dries, D, and Marini, JJ. Elastic power of mechanical ventilation in morbid obesity and severe hypoxemia. Respir Care. (2021) 66:626–34. doi: 10.4187/respcare.08234
2. Windisch, W, Geiseler, J, Simon, K, Walterspacher, S, and Dreher, M. German National Guideline for treating chronic respiratory failure with invasive and non-invasive ventilation–revised edition 2017: part 2. Respiration. (2018) 96:171–203. doi: 10.1159/000488667
3. Lin, X, Chen, C, Liu, Y, Peng, Y, Chen, Z, Huang, H, et al. Peripheral nerve conduction and sympathetic skin response are reliable methods to detect diabetic cardiac autonomic neuropathy. Front Endocrinol (Lausanne). (2021) 12:709114. doi: 10.3389/fendo.2021.709114
4. He, H, Chi, Y, Yang, Y, Yuan, S, Long, Y, Zhao, P, et al. Early individualized positive end-expiratory pressure guided by electrical impedance tomography in acute respiratory distress syndrome: a randomized controlled clinical trial. Crit Care. (2021) 25:230. doi: 10.1186/s13054-021-03645-y
5. Florio, G, Ferrari, M, Bittner, EA, De Santis, SR, Pirrone, M, Fumagalli, J, et al. A lung rescue team improves survival in obesity with acute respiratory distress syndrome. Crit Care. (2020) 24:4. doi: 10.1186/s13054-019-2709-x
6. Kacmarek, RM, Wanderley, HV, Villar, J, and Berra, L. Weaning patients with obesity from Ventilatory support. Curr Opin Crit Care. (2021) 27:311–9. doi: 10.1097/MCC.0000000000000823
7. de, R, Teggia, M, Fumagalli, J, Marrazzo, F, Florio, G, Grassi, L, et al. High pleural pressure prevents alveolar Overdistension and hemodynamic collapse in acute respiratory distress syndrome with class III obesity. A clinical trial. Am J Respir Crit Care Med. (2021) 203:575–84. doi: 10.1164/rccm.201909-1687OC
8. Rubin, J, and Berra, L. Electrical impedance tomography in the adult intensive care unit: clinical applications and future directions. Curr Opin Crit Care. (2022) 28:292–301. doi: 10.1097/MCC.0000000000000936
9. Eimer, C, Freier, K, Weiler, N, Frerichs, I, and Becher, T. The effect of physical therapy on regional lung function in critically ill patients. Front Physiol. (2021) 12:749542. doi: 10.3389/fphys.2021.749542
10. Wang, Q, Su, L, Jiang, J, Wang, N, He, H, and Long, Y. Incorporating electrical impedance tomography to Transpulmonary pressure-guided Peep in severe Ards with pneumothorax and multiple cavitations: a case report. Front Med. (2023) 10:1240321. doi: 10.3389/fmed.2023.1240321
Keywords: electrical impedance tomography, ventilator weaning, pneumonia, respiratory failure, case report
Citation: Liu Y, Liu R, Li B, Cai L, Hou J and Zhao W (2025) Case report: Electrical impedance tomography-guided ventilator weaning in an obese patient with severe pneumonia. Front. Med. 11:1505114. doi: 10.3389/fmed.2024.1505114
Edited by:
Themba Nyirenda, Hackensack Meridian School of Medicine, United StatesReviewed by:
Filippo Binda, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, ItalyZhanqi Zhao, Guangzhou Medical University, China
Copyright © 2025 Liu, Liu, Li, Cai, Hou and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rui Liu, bGl1cnVpbHljeEAxNjMuY29t
 Yuxia Liu
Yuxia Liu Rui Liu
Rui Liu