- 1School of Acupuncture-Moxibustion and Tuina, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Department of Gastroenterology and Hepatopathy, Xi’an Daxing Hospital, Xi’an, China
- 3Sixth Department of Obstetrics (Foetal Protection Centre), Northwest Women’s and Children’s Hospital, Xi’an, China
Background: Neurodermatitis is a chronic skin condition characterized by intense itching and skin thickening due to neurological dysfunction. Its persistent nature poses a challenge to effective treatment, significantly impacting patients’ quality of life. Wet cupping therapy is increasingly being used in clinics to manage neurodermatitis, so it is imperative to assess the evidence regarding its effectiveness and safety.
Objective: This review aimed to evaluate the efficacy and safety of wet cupping therapy in patients with neurodermatitis.
Methods and analysis: Randomized controlled trials (RCTs) investigating wet cupping for neurodermatitis were identified through searches of eight electronic databases and three clinical trial registration platforms from inception to March 2024, using predefined search terms. Included studies underwent quality appraisal using the Cochrane Collaboration’s Risk of Bias Assessment tool. The quality of evidence was assessed independently by two reviewers using the Grading of Recommendations Assessment, Development, and Evaluation System (GRADE). Meta-analysis and publication bias assessment were conducted using ReviewManager 5.4 and STATA 17.0 software, respectively.
Results: This review encompassed 19 studies, comprising 6 types of comparisons and involving 1,505 participants. The findings revealed no significant difference in the total effective rate between wet cupping alone and high-potency steroids (n = 269, RR = 1.13, 95% CI [0.90, 1.41], p = 0.29, I2 = 83%). However, wet cupping combined with medication or moxibustion exhibited superior efficacy compared to medication alone (n = 272, RR = 1.28, 95% CI [1.16, 1.41], p < 0.00001, I2 = 43%) and (n = 534, RR = 1.22, 95% CI [1.14, 1.30], p < 0.00001, I2 = 0%). Wet cupping groups demonstrated lower recurrence rates (n = 266, RR = 0.31, 95% CI [0.16, 0.60], p = 0.0005, I2 = 0%) and a reduced incidence of adverse events (n = 673, RR = 0.44, 95% CI [0.21, 0.90], p = 0.02, I2 = 36%). Furthermore, wet cupping alone or combined with moxibustion effectively lowered the levels of inflammatory factors compared to medication: TNF-α (n = 120, MD = −6.99, 95% CI [−8.13, −5.85], p < 0.00001, I2 = 0%), IL-1β (n = 120, MD = −5.28, 95% CI [−6.91, −3.65], p < 0.00001, I2 = 48%), and IL-6 (n = 180, MD = −8.61, 95% CI [−13.24, −3.99], p = 0.0003, I2 = 81%).
Conclusion: The efficacy of wet cupping therapy is comparable to that of high-potency steroids. Its combined use with medication or moxibustion appears to enhance effectiveness, reduce recurrence rates, and improve safety. However, due to the overall low grade of evidence for the identified outcomes and poor methodological quality, caution is advised when interpreting and applying these findings in clinical practice.
Systematic review registration:
1 Introduction
Neurodermatitis, a chronic and recurrent skin condition, stems from dysfunctions in the excitatory and inhibitory processes of the cerebral cortex (1). The itch–scratch cycle is a crucial neurophysiological mechanism of its pathogenesis; generally speaking, neurological disorders located in the cerebral cortex can induce endocrine disorders, leading to the release of catecholamines, acetylcholine, histamine, etc., causing itching (2). Chronic itching often triggers the patient’s urge to scratch, which in turn leads to neuronal inflammation, exacerbating and prolonging the itching (3, 4), further prompting the patients to reflexively scratch or rub their skin, exacerbating disruptions in the skin barrier, and leading to excessive corneum thickening, dry skin scaling, and chapping, ultimately resulting in skin lichenoid changes (5), and even to infection or malignant transformation in rare cases (6). With over 10% of the global population affected by neurodermatitis, onset typically occurs between the ages of 30 and 50, with a higher prevalence among women (7, 8). Topical corticosteroids are frequently efficacious as initial treatments for inflammatory dermatoses (6). They exhibit anti-proliferative, immunosuppressive, and hormonal activities. However, prolonged use increases the risk of skin atrophy and secondary infections (9), and a higher number of cases of hypersensitivity reactions have been reported in recent years due to their accessibility as over-the-counter (OTC) medications (10, 11). Another study suggested a potential association between topical corticosteroids and the risk of developing diabetes, which increased with cumulative dose and cumulative duration of use (12). Antihistamines are recommended as the first-line systemic treatment for neurodermatitis in China for anti-inflammatory and pruritus relief (13). Common side effects of first-generation and some second-generation antihistamines are known, such as unwanted sedative effects (fatigue, drowsiness, etc.) and anticholinergic effects (14, 15). They should also be used with caution in people with abnormal liver function. A large cohort study (16) reported that patients with hepatitis B and hepatitis C who took them were at an increased risk of developing liver cancer. For the above reasons, it is indispensable to seek other treatments to meet the management and safety of neurodermatitis.
Cupping, a procedure for physical stimulation of the skin, has been practiced for thousands of years, especially in East Asian and Islamic cultures (17, 18). In traditional Chinese medicine, practitioners make use of the power of flaming heating to create suction inside cups, enabling them to adhere quickly to acupuncture points or specific areas of the body (19). In contrast to dry cupping, wet cupping therapists use a sterile needle or scalpel to make a small incision in the superficial part of the skin and then place a cup over the incision and suck out the air inside, drawing out a small amount of blood or extracellular fluid (20). In recent years, interest in wet cupping has surged. It has not only been recognized as potentially beneficial for dermatological conditions (7, 21, 22), but Chinese scholars have also found that wet cupping is more advantageous than dry cupping in improving lower back pain (23). Despite numerous clinical trials conducted in recent decades to verify the efficacy of wet cupping, there is a lack of meta-analyses focusing on its effectiveness in treating neurodermatitis. Therefore, we aimed to evaluate the efficacy and safety of wet cupping for neurodermatitis through a meta-analysis of randomized controlled trials (RCTs), providing evidence-based support for its management.
2 Methods and analysis
This systematic review was conducted and reported in accordance with the PRISMA 2020 statement, an updated guideline for the reporting of systematic reviews (24), and the recommendations by the Cochrane Collaboration, an updated guideline for trusted systematic reviews—a new edition of the Cochrane Handbook for Systematic Reviews of Interventions (25). The systematic review was registered on the PROSPERO website1 with the registration number: CRD42024524398. The methods were not changed during the review unless otherwise denoted below.
2.1 Inclusion and exclusion criteria
2.1.1 Types of studies
This study included only parallel group-designed RCTs published in English or Chinese. Non-RCTs, such as pre-and post-controlled studies, historically controlled studies, cohort studies, and cross-sectional studies, were excluded. The duplication of studies published elsewhere was also excluded.
2.1.2 Types of participants
The study included adult patients (18 years or above) who met the diagnostic criteria for neurodermatitis issued by the Chinese Medical Association (13) or the European Dermatology Forum (26) or other authoritative academic organizations, regardless of sex, age, or ethnicity.
2.1.3 Types of interventions
Wet cupping therapy. There are no restrictions on the materials of the cups, such as glass, plastic, and bamboo cans. The following needles were considered for bloodletting: plum-blossom needle, fire needle, three-edged needle, skin needle, and other types of acupuncture, regardless of the choice of acupoints or location. Adding any medication to the cups was not allowed. The study involved either wet cupping alone as intervention or wet cupping combined with other treatments in the control group.
2.1.4 Types of outcome measures
2.1.4.1 Primary outcomes
Total effective rate (TER), measured according to two common standards (27, 28), as cure rate + marked effective rate + remission rate. This was judged by calculating the clinical symptom score (including items such as itching, papules, erythema, and pigmentation).
2.1.4.2 Secondary outcomes
Recurrence rate, incidence of adverse events, and levels of inflammatory factors (TNF-α, IL-1β, and IL-6).
2.2 Information sources and search strategies
Two reviewers independently performed a comprehensive search of the following electronic databases: four English databases [PubMed, Embase, Cochrane Central Register of Controlled Trials database (CENTRAL), and Web of Science (WOS)] and four Chinese databases (China National Knowledge Infrastructure (CNKI), SinoMed Database (CBM), VIP Database, and WF Database). In addition, three clinical trial registration platforms were searched: the World Health Organization (WHO) International Clinical Trials Registry Platform,2 the Chinese Clinical Trial Registry,3 and ClinicalTrials.gov4 on wet cupping for neurodermatitis from their inception to March 2024. The following key search terms were imposed: (a) clinical conditions: neurodermatitis, lichen simplex chronicus, etc.; (b) wet cupping therapy-related words: cupping therapy, wet cupping, cupping, bloodletting, bleeding cupping, etc.; and (c) trial type: an RCT. The terms “and” and “or” were combined between the search terms. The search strategies for these sources are shown in the Supplementary Material.
2.3 Selection process and data collection
All investigators received professional, evidence-based medicine training to implement this systematic review. After excluding duplicate articles and uploading potentially eligible studies into Endnote V.20 software, two reviewers (LD and JC) independently screened the titles, abstracts, and keywords of all search items. They identified trials that met the above-mentioned inclusion criteria. Divergences between the two reviewers were resolved through discussion between the two. A third party also assisted in making the final decision. A PRISMA flowchart illustrating the study selection process is included in Figure 1.
Two reviewers (YZ and LD) independently performed the data collection using a standardized tabulation. The extracted elements were as follows: basic information (title, year of publication, first author, language, and country of implementation), participant characteristics at baseline (sample size, age, gender, and course of disease), study design (randomization method, allocation concealment, blinding procedures, diagnostic criteria, intervention frequency and duration, and acupoint composition), and outcomes. In the case of multi-arm RCTs, they were reclassified as dual-arm RCTs to ensure compatibility for result synthesis. The two reviewers conducted data extraction and cross-checking, and any discrepancies were resolved through consultation with the corresponding author.
2.4 Risk of bias assessment
Two independent reviewers (Z-FJ and XT) evaluated the quality of the included studies using the Cochrane Collaboration’s Risk of Bias Assessment tool (25). We evaluated the five items (bias in the randomization process, bias in deviations from the intended intervention, bias in missing outcome data, bias in the measurement of an outcome, and selection bias in the reported results). Each item was assessed and classified as high risk, low risk, or risk of some concern. The corresponding author were asked to resolve any divergences.
2.5 Data synthesis and assessment of heterogeneity
The statistical software ReviewManager V.5.4 was used for data analysis. The mean difference (MD) was used as the effect size for continuous variables, while the risk ratio (RR) was used for dichotomous variables. The 95% confidence interval (CI) was calculated. A significance level of p-value <0.05 was considered statistically significant. Statistical heterogeneity was assessed using the chi-squared tests and the Higgins I2 test. If p-value ≥0.1 and I2 ≤ 50%, indicating a high degree of homogeneity, a fixed-effects model was used for the pooled analysis. Conversely, if p-value <0.1 or I2 > 50%, indicating a significant degree of heterogeneity, a random-effects model was used. If there was significant heterogeneity between studies and the data were available, subgroups of the different cupping therapies and intervention forms were constructed to explore the potential causes of heterogeneity.
2.6 Reporting bias assessment
If more than 10 studies were included in the analysis, the funnel plot method and Egger’s test were used to evaluate publication biases. A p-value of <0.05 was considered indicative of significant publication bias. The analysis for publication bias was performed using STATA V.17.0.
2.7 Confidence in cumulative evidence
The Grading of Recommendations Assessment, Development, and Evaluation System (GRADEpro) evaluation tool5 was independently used by two reviewers (YZ and Z-FJ) to assess the quality of evidence in terms of five dimensions: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The quality of evidence was classified as high, moderate, low, or very low. In the event of any disagreement, a third reviewer was consulted to facilitate consensus.
3 Results
3.1 Study selection
A total of 1,771 studies were initially identified by searching the databases using the keywords mentioned earlier. After stepwise screening, 19 RCTs with 1,505 participants were included in our meta-analysis (29–47). The flowchart of PRISMA is depicted in Figure 1.
3.2 Characteristics of the included trials
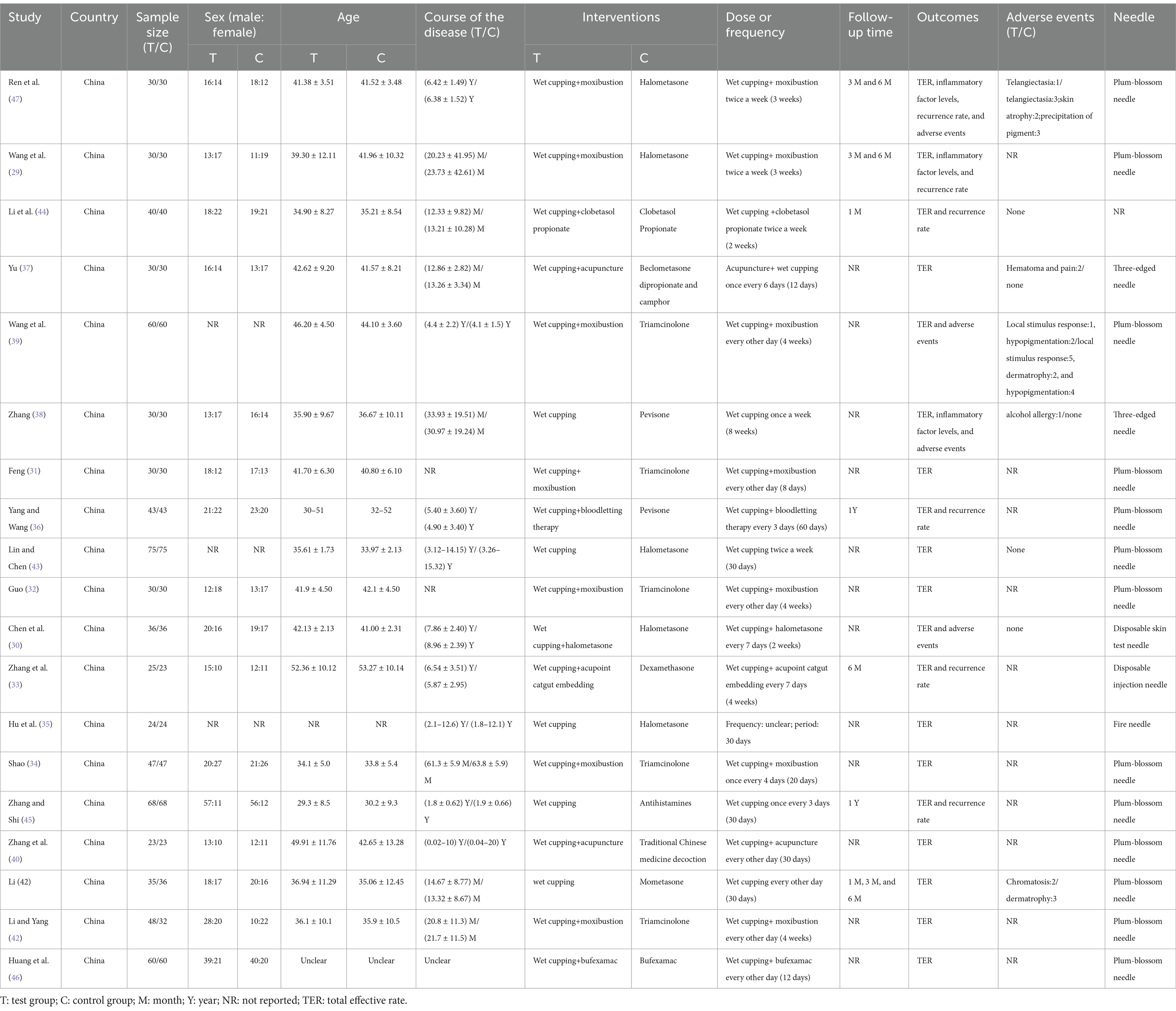
The main characteristics of the included RCTs are shown in Table 1. All studies were conducted in China between 1998 and 2023. Only one study was published in English (34), and the remaining studies were published in Chinese. All included studies were single-center, two-arm RCTs, of which 3 were master’s degree theses (37, 38, 41) and 16 were journal articles. The average age of the 1,505 participants ranged from 29 to 53 years and did not involve any minors or elderly patients. The course of the disease varied from 1 week to 20 years.
3.3 Risk of bias
The risk of bias assessment was conducted for each study, and the results are shown in Figure 2. All the included studies mentioned the term “randomized” or “random” in their methodology; 11 studies used random number tables, 1 study used statistical software to generate random numbers, and 1 study used the method of drawing lots for random allocation, while the other 6 studies did not mention specific randomization methods. Except for two studies (41, 42), none of the other 17 studies explicitly discussed the details of allocation concealment. Due to the nature of cupping therapy, it is unfeasible to blind the operators, so all studies received a “high risk” rating in the third item. Except for two studies (41, 42), the other 17 studies did not assess blinding in their outcomes, leading to “unclear” ratings. The outcome data of all the included studies were complete, and no studies were selectively reported. In terms of other biases, one study neither reported the total time patients received treatment nor assessed the time to treatment outcome (31), and another study had unbalanced baseline data (42), resulting in a high risk of bias.
3.4 Meta-analysis
3.4.1 Total effective rate
3.4.1.1 Wet cupping alone compared to medication alone
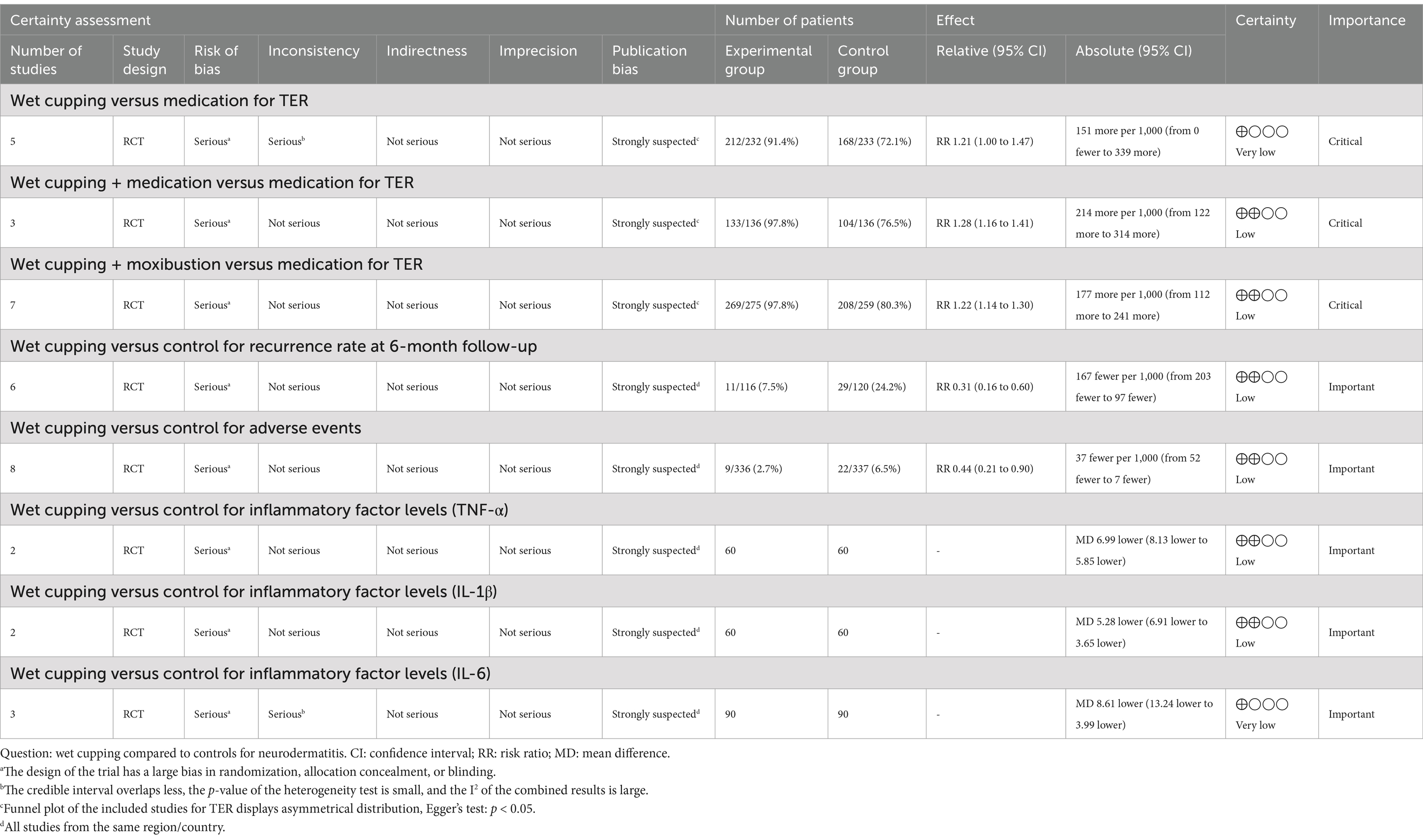
Five studies compared wet cupping alone with medication as an intervention. The pooled data analysis revealed no significant difference in the total effective rate between wet cupping and medication (n = 465, RR = 1.21, 95% CI [1.00, 1.47], p = 0.05, I2 = 83%).
A subgroup analysis was performed based on different control medications; three studies (35, 41, 43) used high-potency steroids as controls, one study (38) used medium-potency steroids, and one (45) used antihistamines as controls (Figure 3). The results indicated that wet cupping was not more effective than high-potency steroids (n = 269, RR = 1.13, 95% CI [0.90, 1.41], p = 0.29, I2 = 83%), and the wet cupping compared to medium-potency steroids study reported no apparent benefit (n = 60, RR = 1.27, 95% CI [1.01, 1.61], p = 0.05). The other study comparing wet cupping with antihistamines showed statistically significant differences (n = 136, RR = 1.45, 95% CI [1.21, 1.75], p < 0.0001). Furthermore, we searched for sources of high heterogeneity in the high-potency steroid subgroup through sensitivity analysis and found that heterogeneity was significantly reduced after excluding the Lin and Chen (43) studies (n = 119, RR = 1.03, 95% CI [0.95, 1.13], p = 0.47, I2 = 0%).
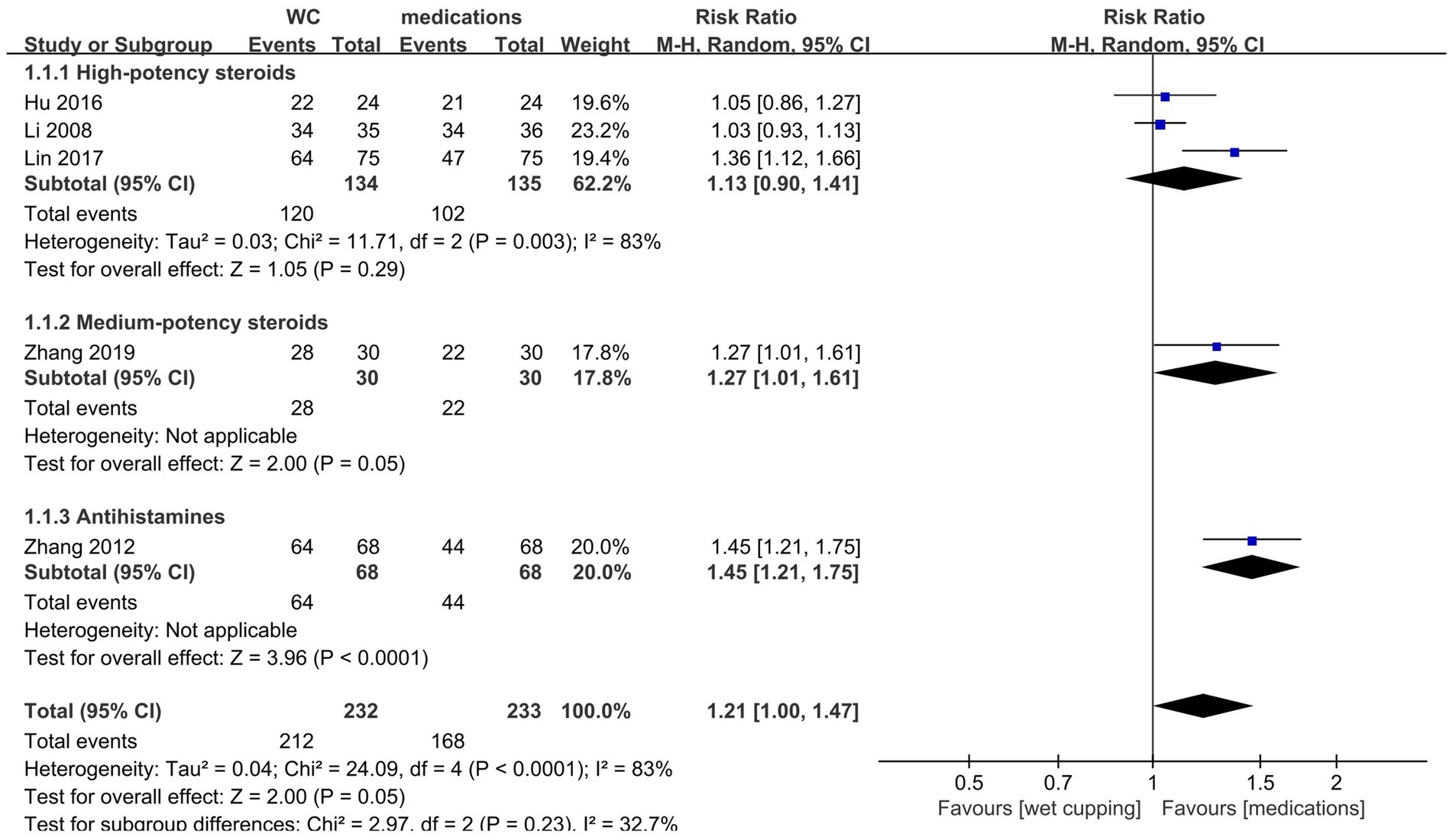
Figure 3. Forest plot of TER. Forest plot showing the effects of wet cupping (WC) compared to medication on the total effective rate in the treatment of neurodermatitis.
3.4.1.2 Wet cupping plus medication compared to medication alone
Three studies had sufficient data to be pooled for meta-analysis; of these, two studies (30, 44) used corticosteroids in the control group, while one (46) used non-steroidal anti-inflammatory drugs. The pooled data analysis indicated that wet cupping and medication were associated with a higher total effective rate than medication alone (n = 272, RR = 1.28, 95% CI [1.16, 1.41], p < 0.00001, I2 = 43%; Figure 4A).
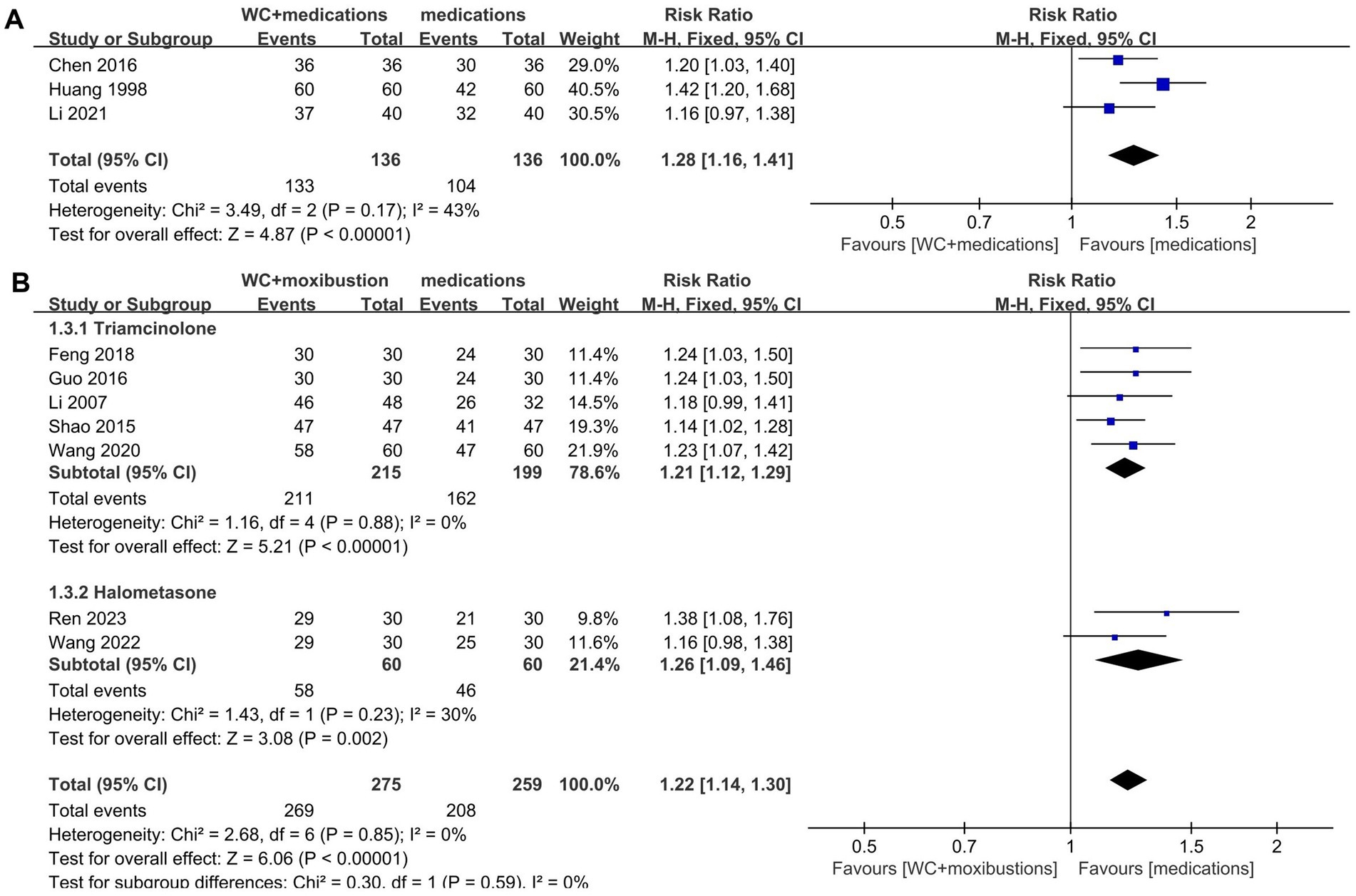
Figure 4. Forest plot of TER. (A) Forest plot showing the effects of wet cupping combined with medication compared to medication alone on the total effective rate in the treatment of neurodermatitis. (B) Forest plot showing the effects of wet cupping combined with moxibustion compared to medication alone on the total effective rate in the treatment of neurodermatitis.
3.4.1.3 Wet cupping plus moxibustion compared to medication
Seven studies reported their total effective rate for the combination of wet cupping with moxibustion compared to medication alone. Two of these studies (29, 47) used high-potency steroids (halometasone), while the other five studies (31, 32, 34, 39, 42) used medium-potency steroids (triamcinolone acetonide). The pooled analysis demonstrated that wet cupping therapy combined with moxibustion was more effective than medication alone (n = 534, RR = 1.22, 95% CI [1.14, 1.30], p < 0.00001, I2 = 0%; Figure 4B).
In the subgroup analysis, wet cupping combined with moxibustion was more effective than triamcinolone (n = 414, RR = 1.21, 95% CI [1.12, 1.29], p < 0.00001, I2 = 0%). Similarly, halometasone was not as effective as wet cupping combined with moxibustion (n = 120, RR = 1.26, 95% CI [1.09, 1.46], p = 0.002, I2 = 30%).
3.4.2 Recurrence rate
A total of four studies reported the recurrence rate at a 6-month follow-up (29, 33, 45, 47). The results of the meta-analysis showed that wet cupping alone or in combination with other treatments had a lower recurrence rate than other treatments (n = 266, RR = 0.31, 95% CI [0.16, 0.60], p = 0.0005, I2 = 0%; Figure 5).
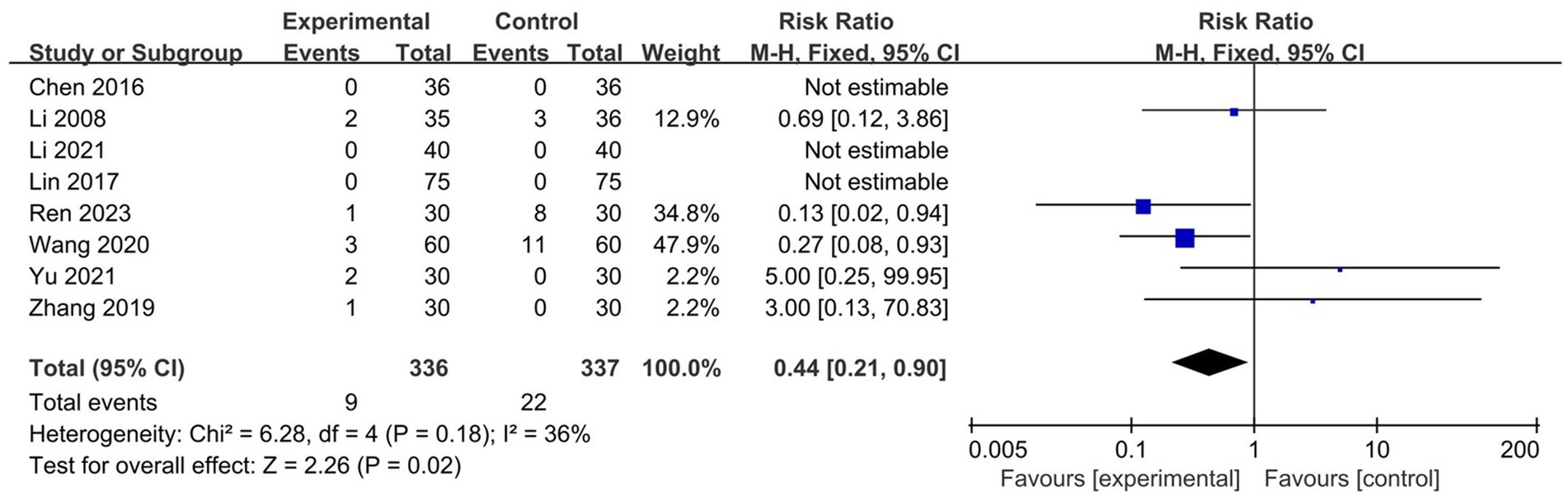
3.4.3 Adverse event incidence
A total of eight studies recorded adverse events, with three studies (30, 43, 44) reporting no adverse events in either the test or control groups. In five studies (37–39, 41, 47), the most common adverse events in the test group included hypopigmentation, subcutaneous hematoma, and pain. The main adverse events in the control group were skin atrophy, pigmentation, and local irritation. No serious adverse events were reported in either group. Interestingly, the results of the meta-analysis showed that wet cupping alone or in combination with other treatments was safer than medication (n = 673, RR = 0.44, 95% CI [0.21, 0.90], p = 0.02, I2 = 36%; Figure 6).
3.4.4 Inflammatory factor levels
Three studies reported the levels of inflammatory factors as an outcome (29, 38, 47). All of these studies reported decreases in the serum levels of interleukin IL-6, and two of the studies also reported decreases in the serum levels of interleukin IL-1β and tumor necrosis factor TNF-α. The meta-analysis of the pooled results indicated that compared to corticosteroids, wet cupping alone or combined with moxibustion had statistically significant differences in reducing the levels of inflammatory factors: TNF-α (n = 120, MD = −6.99, 95% CI [−8.13, −5.85], p < 0.00001, I2 = 0%), IL-1β (n = 120, MD = −5.28, 95% CI [−6.91, −3.65], p < 0.00001, I2 = 48%), and IL-6 (n = 180, MD = −8.61, 95% CI [−13.24, −3.99], p = 0.0003, I2 = 81%) (Figure 7).
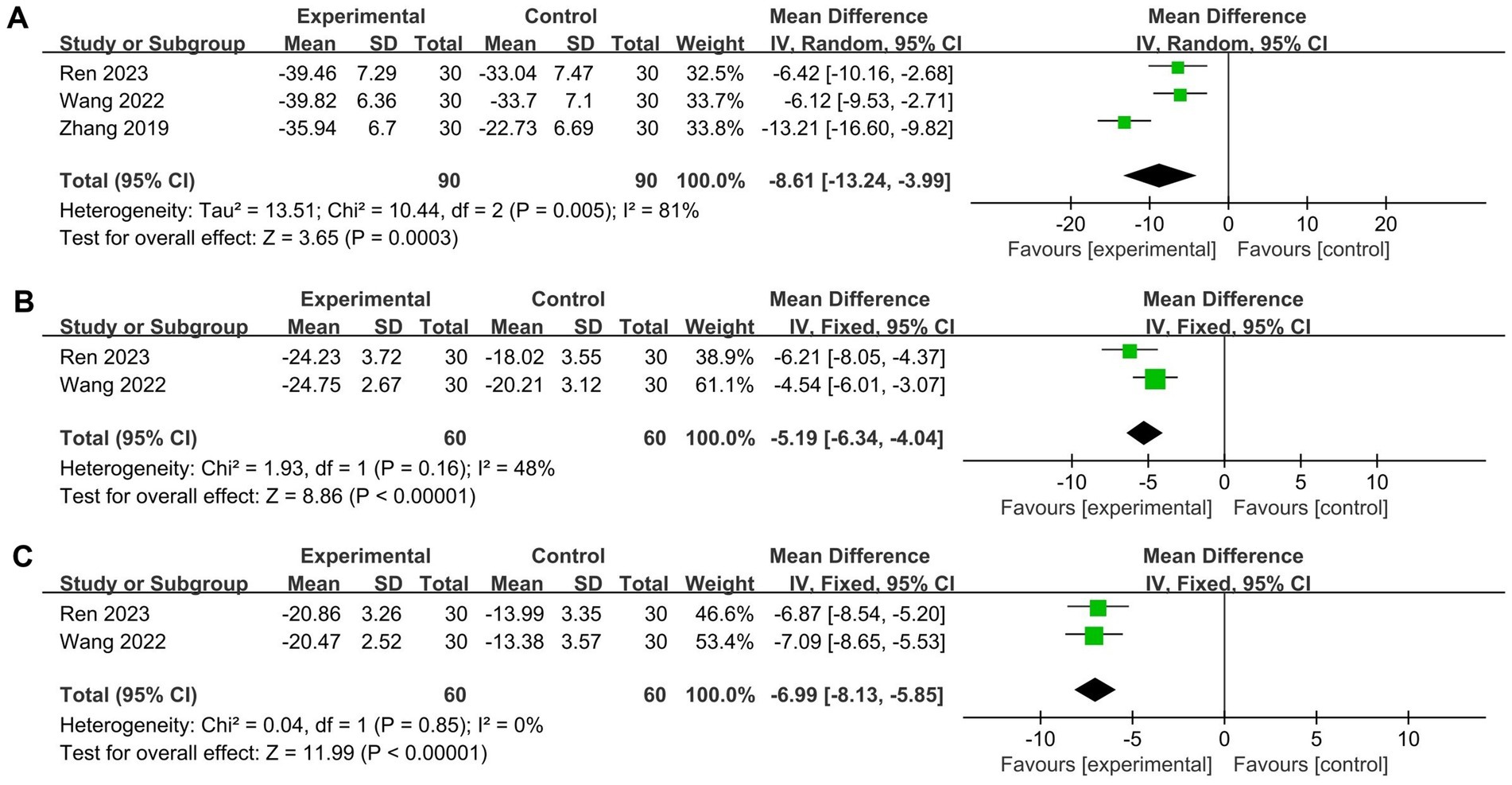
Figure 7. Forest plot of levels of inflammatory factors. (A) interleukin IL-6; (B) interleukin IL-1β; (C) tumor necrosis factor TNF-α.
Given the high heterogeneity of the statistical results for IL-6, a sensitivity analysis revealed a significant reduction after excluding the study by Zhang (38) (n = 120, MD = −6.26, 95% CI [−8.78, −3.74], p < 0.00001, I2 = 0%).
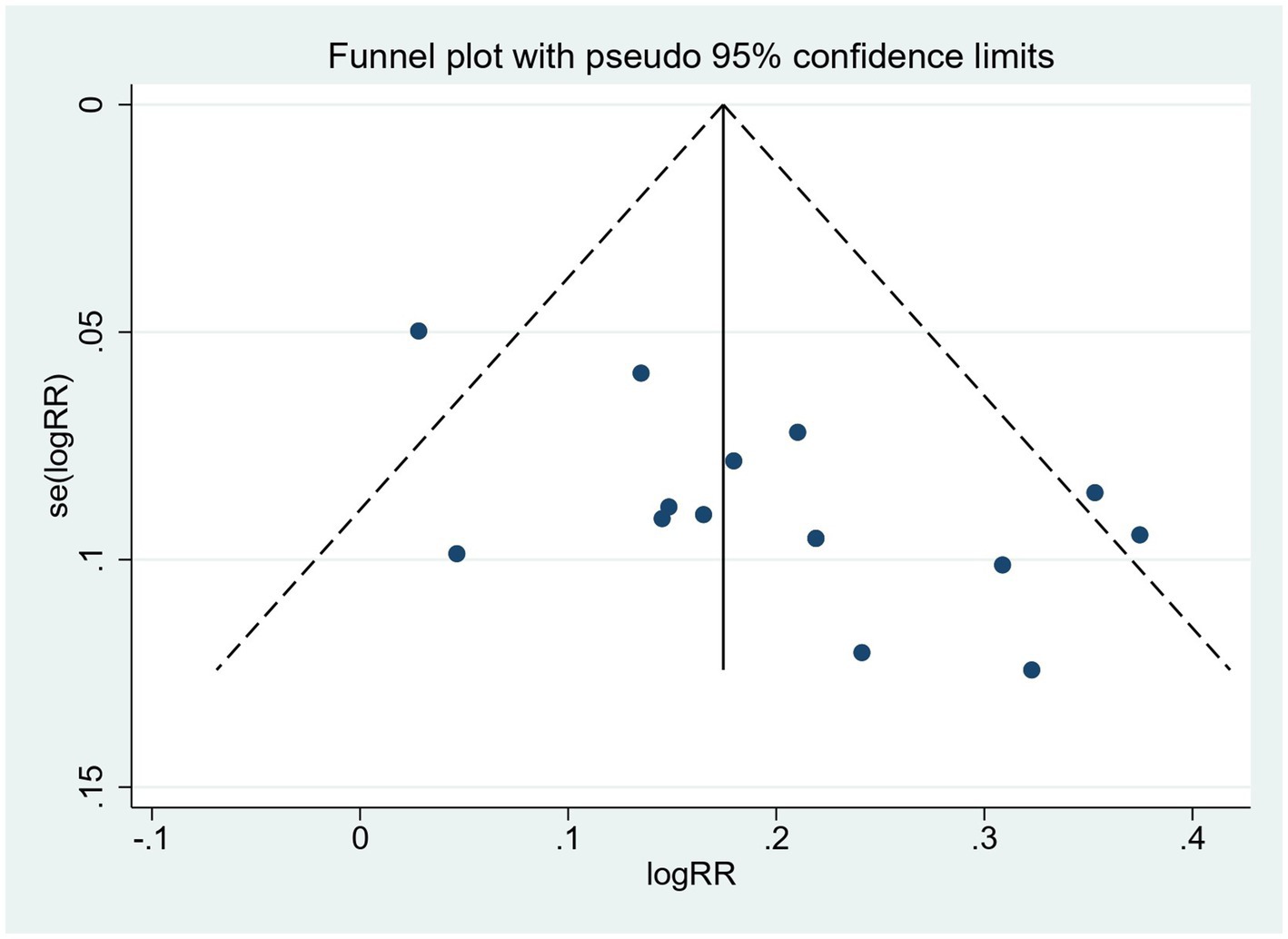
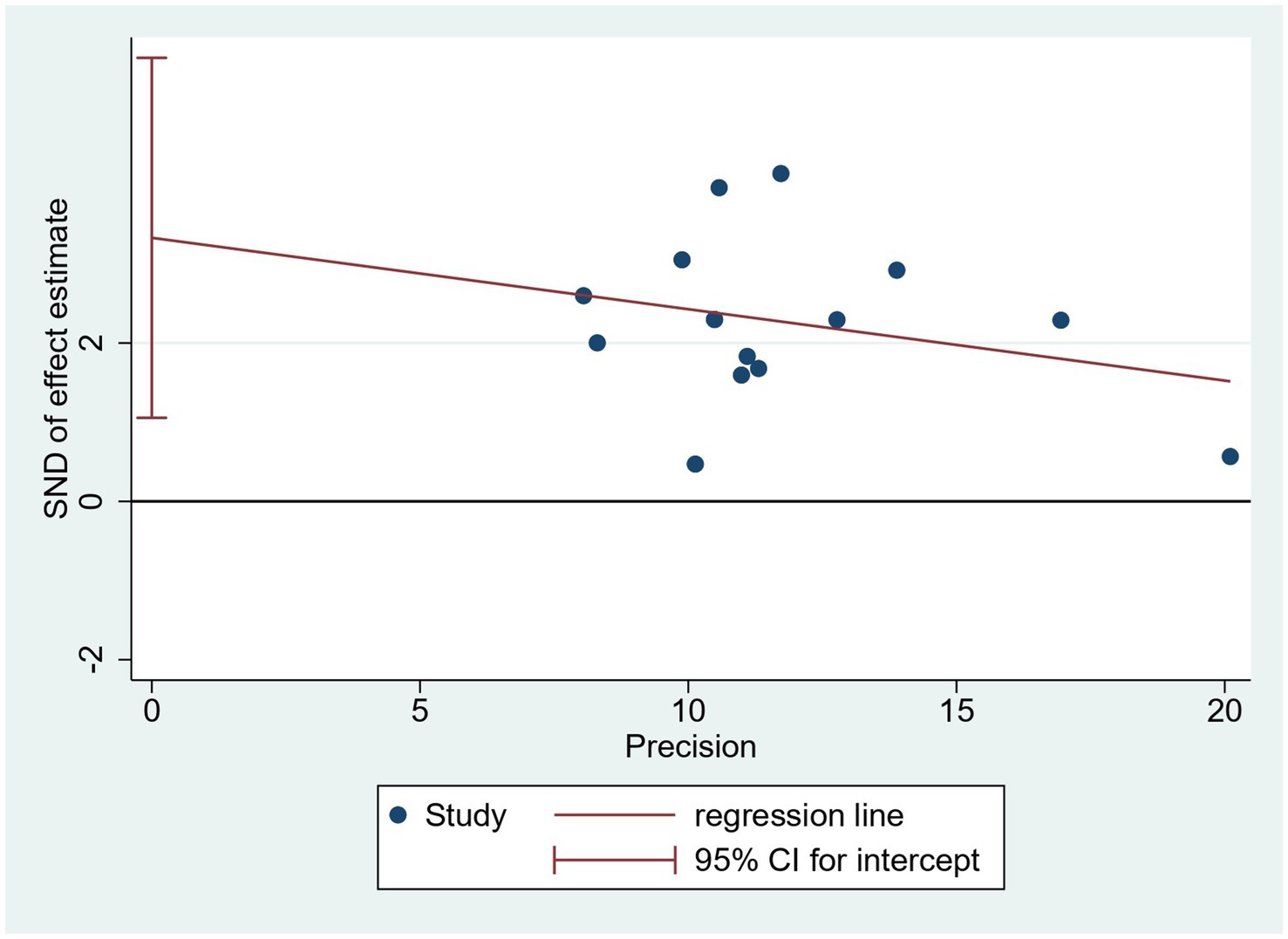
3.5 Publication bias
Since only the TER meets the requirement that the number of studies reporting outcomes be greater than 10, publication bias was tested only for the total effective rate. Visually, the funnel plot showed an asymmetric distribution of included studies, with four studies falling outside the pseudo 95% confidence interval (Figure 8). Furthermore, Egger’s test was conducted (Figure 9), and the results showed a total effective rate with p = 0.007, indicating the existence of significant publication bias. See Figures 8, 9 for details
3.6 Quality assessment of the evidence
Table 2 lists the quality assessment of each outcome of wet cupping and control in the meta-analysis. The GRADEpro system was used to assess the quality of evidence based on different intervention measures and outcomes. The results revealed six studies with low-quality evidence, two with very low-quality evidence, and none with high-quality or moderate-quality evidence. The majority of the studies had limitations in their experimental design, such as inadequate description of random sequence generation, allocation concealment, and blinding. Consequently, they were downgraded. In addition, the presence of publication bias in the majority of the studies contributed to their downgrading.
4 Discussion
4.1 Main results
Neurodermatitis is one of the most prevalent and persistent pruritic dermatoses (8). Nocturnal paroxysmal pruritus, a hallmark of the condition, disrupts sleep and impairs daily functioning, imposing substantial psychological strain on patients (8, 48). Given the limitations of conventional treatments, there is an urgent need for complementary interventions. Our meta-analysis revealed that wet cupping alone did not show a higher TER than high-potency steroids, suggesting that both are equally effective. When used in combination with medication or moxibustion, wet cupping demonstrated superior efficacy compared to medication alone. Regarding secondary outcomes, wet cupping alone or in combination with other therapies can significantly reduce the recurrence rate and the incidence of adverse events.
We conducted an overall search of relevant literature databases and noted the rare use of dry cupping in neurodermatitis. Despite its potential benefits, such as regulating skin immunity and stimulating the release of inflammatory mediators (49), we hypothesized that the non-invasive nature of dry cupping may limit its effectiveness in fully stimulating the deeper layers of hypertrophic lichenified skin. The above reasons influenced our decision to exclude dry cupping from the systematic review. In contrast, wet cupping combines bloodletting and cupping as a physical stimulation procedure. This physical stimulation can cause local tissue congestion and decompression, accelerate blood circulation, and inflammatory exudate discharge (47); it also causes the release of histamine, stimulates phagocytosis, regulates the body’s immune network, and promotes the self-repair of damaged skin tissue (50). Among the studies in our systematic review, 12 used plum-blossom needles, 2 used three-edged needles, and 1 used fire needles, all of which are traditional Chinese acupuncture instruments. On the one hand, acupuncture may alleviate itching by exerting antihistamine effects, reducing itch mediator production, and modulating the brain network involved in the central transmission of itch (7, 51, 52). On the other hand, acupuncture can bolster the body’s stress response, induce denaturation of diseased tissue proteins, and activate macrophages and leukocytes to phagocytose necrotic tissue, thereby ameliorating skin lichenification (53, 54).
As an important effector of the immune system, the release and recruitment of inflammatory factors actively participate in and mediate cellular inflammatory responses (55). IL-6 has been reported to promote the activation and infiltration of inflammatory cells, exacerbating the inflammatory state of the skin and leading to keratinization and desquamation of the skin (56, 57). TNF-α is a tumor necrosis factor that induces the activation of macrophages and T cells, which, in turn, produce pro-inflammatory cytokines, etc. (58). The expression levels of IL-1β, IL-4, IL-6, and TNF-α in peripheral blood positively correlate with the severity of dermatitis (59) and may contribute to disease recurrence (60). Scholars have proposed that wet cupping reduces the aggregation of inflammatory factors by accelerating the metabolism of skin tissues and promoting the skin to repair the damaged tissues and the absorption of inflammatory substances to benefit neurodermatitis patients (50, 61). Our meta-analysis results indicated that, compared to the control group, wet cupping can significantly reduce the levels of inflammatory factors (TNF-α, IL-1β, and IL-6). However, at present, the specific mechanisms of wet cupping to reduce the serum inflammatory factor need to be further confirmed.
4.2 Limitations
Our review has important limitations that should be considered with caution. First, high heterogeneity appeared in the comparison of IL-6 and in the subgroup analysis of wet cupping alone versus high-potency steroids. The variations in study designs, intervention frequencies, outcome measurement intervals, skin lesion sites, or unaccounted confounding factors across comparisons may introduce significant clinical heterogeneity. This may lead to the unreliability of our pooled analysis results. Second, all the studies included in this meta-analysis were completed in China and multicenter trials were lacking, which may affect the quality of evidence in this analysis. Third, due to the nature of cupping therapy, blinding of cupping operators and participants was not feasible, which may have affected the reporting of treatment results in favor of wet cupping. Fourth, 4 studies did not provide information on random sequence generation, 2 used incorrect randomization methods, and 17 studies did not clarify whether allocation concealment was applied. In addition, significant publication bias was evident. Consequently, the overall quality of evidence in these studies may not be sufficient to extrapolate the findings to broader contexts. Fifth, the primary outcome used in the included studies was the total effective rate, which is not an internationally recognized standard. Furthermore, trial details were not comprehensively reported under standard reporting guidelines such as CONSORT. Sixth, the variability in total treatment time and frequency of cupping in each study is often determined by the cupping practitioner’s individual experience, resulting in varying efficacy and outcomes within the same intervention framework.
4.3 Implications for practice and research
Our data show that wet cupping is effective and that patients may gain additional benefits by adding wet cupping to corticosteroid or antihistamine therapy. This finding offers patients more treatment options and aids physicians make informed decisions. For patients who have long relied on medication to manage their condition and suffer from its side effects, wet cupping could be a viable alternative. Our research results suggest that wet cupping is relatively safe; however, it is important to adhere to operating specifications to prevent skin trauma or infection. We recommend the establishment of standardized guidelines for cupping therapy to facilitate its clinical promotion and application, despite being somewhat challenging.
The neuro-anxiety state plays a key role in the pathogenesis of neurodermatitis, with a demonstrated correlation between patients’ anxiety levels and the severity of pruritus (48). However, the included studies failed to incorporate relevant indicators to assess patients’ mental state and improvement. Future studies should consider incorporating the Hamilton Anxiety Scale (HAMA) and the Quality of Life Questionnaire (QOL) as outcomes to evaluate an individual’s mental status and overall quality of life. This would help define the impact of mental state on neurodermatitis patients so that appropriate interventions or research protocols can be prescribed.
Overall, the mechanism of action of wet cupping therapy on neurodermatitis remains unclear, necessitating further basic research to complement the clinical evidence. Given the limited quality of evidence in the studies reviewed, we anticipate more SRs or RCTs with reasonable designs and appropriate methods to validate our findings.
5 Conclusion
This review highlights the efficacy of wet cupping in the treatment of neurodermatitis in terms of total effective rate, recurrence, and safety. The originality of our study lies in comparing the efficacy of wet cupping when used alone, in combination with medication, or alongside moxibustion, against the efficacy of medication to determine its significance in the management of neurodermatitis.
Our findings revealed no difference in the efficacy of wet cupping compared to high-potency steroids. However, wet cupping may improve treatment efficacy when it is used as an adjunctive therapy to corticosteroids or alongside moxibustion, reduce recurrence rates and adverse event incidence, and significantly decrease inflammatory factor levels (TNF-α, IL-1β, and IL-6). Due to the poor methodological quality of allocation concealment and blinding implementation in these studies, along with the overall low grade of evidence, the results should be interpreted and applied in practice with caution.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
YZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Y-yH: Conceptualization, Methodology, Software, Writing – review & editing. Z-fJ: Data curation, Software, Writing – review & editing. LD: Data curation, Formal analysis, Writing – review & editing. JC: Data curation, Writing – review & editing. XT: Writing – review & editing. HaZ: Writing – review & editing. HoZ: Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the “Xinglin Scholars” Subject Talent Research Promotion Plan of Chengdu University of Traditional Chinese Medicine (XKTD2021004) and the State Administration of Traditional Chinese Medicine 2022 National Famous Old Chinese Medicine Expert Inheritance Studio Construction Project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The authors would like to express their gratitude to the “Xinglin Scholars” Subject Talent Research Promotion Plan of Chengdu University of Traditional Chinese Medicine (XKTD2021004) and the State Administration of Traditional Chinese Medicine 2022 National Famous Old Chinese Medicine expert Inheritance Studio construction project for their support.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1478073/full#supplementary-material
Footnotes
1. ^https://www.crd.york.ac.uk/prospero/
2. ^http://www.who.int/ictrp/en/
References
1. Werfel, T, Aberer, W, Augustin, M, Biedermann, T, Fölster-Holst, R, Friedrichs, F, et al. Atopic dermatitis: S2 guidelines. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology: JDDG. (2009) 7:S1–S46. doi: 10.1111/j.1610-0387.2009.06972.x
2. Mack, MR, and Kim, BS. The itch–scratch cycle: a Neuroimmune perspective. Trends Immunol. (2018) 39:980–91. doi: 10.1016/j.it.2018.10.001
3. Yosipovitch, G, Misery, L, Proksch, E, Metz, M, Ständer, S, and Schmelz, M. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. (2019) 99:1201–9. doi: 10.2340/00015555-3296
4. Tang, Y, and Yao, Z. Research and therapy Progress on the mechanisms of pruritus in atopic dermatitis. Med J Peking Union Med College Hospital. (2022) 13:473–9. doi: 10.12290/xhyxzz.2021-0747
5. Ichiki, T, Sugita, K, Furue, M, and Yamamoto, O. An intimate relationship between Intralesional depigmentation and peripheral nervous system in lichen simplex Chronicus. Acta Derm Venereol. (2020) 100:adv00042. doi: 10.2340/00015555-3390
6. Ju, T, Vander Does, A, Mohsin, N, and Yosipovitch, G. Lichen simplex Chronicus itch: an update. Acta Derm Venereol. (2022) 102:adv00796. doi: 10.2340/actadv.v102.4367
7. Xie, Y, Qin, Y, and Du, Y. Research Progress and advantages of acupuncture and Moxibustion in the treatment of lichen simplex Chronicus in recent ten years. Modern Chin Med. (2021) 41:1–6. doi: 10.13424/j.cnki.mtcm.2021.05.001
8. Charifa, A, Badri, T, and Harris, BW. Lichen Simplex Chronicus. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing LLC. (2024).
9. Stacey, SK, and McEleney, M. Topical corticosteroids: choice and application. Am Fam Physician. (2021) 103:337–43.
10. Saraswat, A. Contact allergy to topical corticosteroids and sunscreens. Indian J Dermatol Venereol Leprol. (2012) 78:552–9. doi: 10.4103/0378-6323.100520
11. Vatti, RR, Ali, F, Teuber, S, Chang, C, and Gershwin, ME. Hypersensitivity reactions to corticosteroids. Clin Rev Allergy Immunol. (2014) 47:26–37. doi: 10.1007/s12016-013-8365-z
12. Phan, K, and Smith, SD. Topical corticosteroids and risk of diabetes mellitus: systematic review and meta-analysis. J Dermatolog Treat. (2021) 32:345–9. doi: 10.1080/09546634.2019.1657224
13. Association CM, House CMAP, Dermatology CSo, practice CSoG, association EBoCJoGPoCM, disease EGoGfPCoSaV. Guideline for primary care of neurodermatitis. Chin J Gen Practit. (2023) 3:230–4. doi: 10.3760/cma.j.cn114798-20230116-00060
14. Sidbury, R, Davis, DM, Cohen, DE, Cordoro, KM, Berger, TG, Bergman, JN, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. (2014) 71:327–49. doi: 10.1016/j.jaad.2014.03.030
15. Li, L. Expert consensus on clinical application of antihistamines in the treatment of dermatitis and eczema. Chin J Gen Practit. (2021) 19:709–12.
16. Chan, S-Y, Chang, Y, Polpichai, N, Lee, Y-T, and Ma, KS-K. Treatment with antihistamines and the risk of liver Cancer in patients with viral hepatitis: a multi-center cohort study. Viruses. (2024) 16:940. doi: 10.3390/v16060940
17. Furhad, S, Sina, RE, and Bokhari, AA. Cupping Therapy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2024).
18. Wang, S-z, Lu, Y-h, Wu, M, Chen, K-j, Liu, Y, and Liu, L-t. Cupping therapy for diseases: an overview of scientific evidence from 2009 to 2019. Chin J Integr Med. (2021) 27:394–400. doi: 10.1007/s11655-020-3060-y
19. Hong, S, Wu, F, Lu, X, Cai, Q, and Guo, Y. Discussion on the mechanism of cupping therapy. Chin Acupunct Moxib. (2011) 31:932–4. doi: 10.13703/j.0255-2930.2011.10.028
20. Sajid, MI. Hijama therapy (wet cupping) – its potential use to complement British healthcare in practice, understanding, evidence, and regulation. Complement Ther Clin Pract. (2016) 23:9–13. doi: 10.1016/j.ctcp.2016.01.003
21. Xie, C, Liu, C, and Xuan, G. Traditional Chinese medicine external treatment is an important method to improve the clinical efficacy of dermatological diseases. Dermatology. Bulletin. (2019) 36:183–90+73.
22. Soliman, Y, Hamed, N, and Khachemoune, A. Cupping in dermatology: a critical review and update. Acta Dermatovenerol Alp Pannonica Adriat. (2018) 27:103–7. doi: 10.15570/actaapa.2018.21
23. Shen, W-C, Jan, Y-K, Liau, B-Y, Lin, Q, Wang, S, Tai, C-C, et al. Effectiveness of self-management of dry and wet cupping therapy for low back pain: a systematic review and meta-analysis. Medicine. (2022) 101:e32325. doi: 10.1097/md.0000000000032325
24. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
25. Cumpston, M, Li, T, Page, M, Chandler, J, Welch, V, Higgins, J, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. (2019) 10. doi: 10.1002/14651858.Ed000142
26. Weisshaar, E, Szepietowski, JC, Dalgard, FJ, Garcovich, S, Gieler, U, Giménez-Arnau, AM, et al. European S2k guideline on chronic pruritus. Acta Derm Venereol. (2019) 99:469–506. doi: 10.2340/00015555-3164
27. Zheng, X. Guiding principles for clinical research of new traditional Chinese medicines: Trial implementation. Beijing, China: China Medical Science and Technology Press (2002).
28. Medicine SAoTC. Standards for diagnostic and efficacy of traditional Chinese medicine diseases and syndrome. Nanjing, Jiangsu, China: Nanjing University Press (1994) 1994-01-01.
29. Wang, X, Wang, L, Ruan, J, Zhou, M, and Wu, S. Clinical effect of blood-letting puncture and cupping combined with fume and Moxibustion in treatment of localized Neurodermatitis with blood deficiency and wind dryness. J Anhui Univ Trad Chin Med. (2022) 41:44–8. doi: 10.3969/j.issn.2095-7246.2022.02.011
30. Chen, N, Zhang, L, and Ye, J. Clinical observation of pricking and cupping combined with halomethasone in the treatment of 36 cases of localized neurodermatitis. Zhejiang J Trad Chin Med. (2016) 51:527–8. doi: 10.13633/j.cnki.zjtcm.2016.07.041
31. Feng, Y. Clinical observation of pricking and cupping combined with moxibustion in the treatment of localized neurodermatitis. Med Aesth Beauty. (2018) 27:59.
32. Guo, J. Clinical observation of pricking and cupping combined with moxibustion in the treatment of localized neurodermatitis. Inner Mongolia Trad Chin Med. (2016) 35:135. doi: 10.16040/j.cnki.cn15-1101.2016.11.129
33. Zhang, C, Tian, C, and Tang, D. Clinical observation on 25 cases of Neurodermatitis treated by bloodletting and catgut embedding. China's Naturop. (2016) 24:48–9. doi: 10.19621/j.cnki.11-3555/r.2016.07.039
34. Shao, Y. Clinical observation on collateral-pricking and cupping therapy plus moxibustion for localized neurodermatitis. J Acupunct Tuina Sci. (2015) 4:269–72. doi: 10.1007/s11726-015-0852-8
35. Hu, L, Zhang, W, and Yi, Q. Clinical observation on the combination of fire needle and bleeding cupping in the treatment of neurodermatitis. Med Inf. (2016) 29:208–9. doi: 10.3969/j.issn.1006-1959.2016.33.163
36. Yang, Q, and Wang, C. Clinical observation on the treatment of Neurodermatitis with autobleeding bloodletting therapy and Back walking cupping therapy. Chinese Foreign Med Res. (2017) 15:133–4. doi: 10.14033/j.cnki.cfmr.2017.3.074
37. Yu, H. Clinical observation on treatment of neurodermatitis by acupuncture combined with pricking collaterals and cupping [master's degree]. Wuhan, Hubei, China: Hubei University of Traditional Chinese Medicine (2021).
38. Zhang, S. Clinical study on the treatment of localized neurodermatitis by pricking the collaterals to purge blood [Master's degree]. Beijing, China: Beijing University of Chinese Medicine (2019).
39. Wang, Z, Wang, C, and Tang, Y. Nursing study of pricking and cupping combined with moxibustion in the treatment of localized neurodermatitis. New Chinese Medicine. (2020) 52:164–6. doi: 10.13457/j.cnki.jncm.2020.16.045
40. Zhang, Z, He, H, and Zhang, H. Observation on the clinical efficacy of 23 cases of neurodermatitis of blood deficiency and wind dryness type treated with pricking and cupping combined with acupuncture. Clin Med Eng. (2011) 18:732–4. doi: 10.3936/j.issn.1674-4659.2011.05.0732
41. Li, Y. Observation on the clinical efficacy of pricking and cupping in the treatment of localized neurodermatitis [Master's degree]. Chengdu, Sichuan, China: Chengdu University of Traditional Chinese Medicine (2008).
42. Li, J, and Yang, X. Observation on the efficacy of acupuncture, cupping and mild moxibustion in the treatment of localized neurodermatitis. J Pract Hosp Clin. (2007) 2:94–5.
43. Lin, X, and Chen, Z. Observation on the efficacy of plum blossom needle combined with cupping in the treatment of 75 cases of neurodermatitis. Zhejiang J Trad Chin Med. (2017) 52:289. doi: 10.13633/j.cnki.zjtcm.2017.04.045
44. Li, Z, Wang, Z, Zeng, Y, Ye, X, and Jiao, L. Observation on the efficacy of pricking and cupping therapy combined with compound clobetasol propionate ointment in the treatment of neurodermatitis. World Latest Med Inform. (2021) 21:195–7. doi: 10.3969/j.issn.1671-3141.2021.87.058
45. Zhang, G, and Shi, Y. Randomized controlled clinical study of plum blossom needle combined with cupping in the treatment of localized neurodermatitis. Journal of practical traditional Chinese. Intern Med. (2012) 26:72–3+5. doi: 10.3969/j.issn.1671-7813.2012.10.42
46. Huang, B, Xiao, W, Li, T, Li, Y, and Xiong, W. A report of 60 cases of neurodermatitis treated with three-step method of seven-star needle. J Guiyang Coll Trad Chin Med. (1998) 2:35–6. doi: 10.16588/j.cnki.issn1002-1108.1998.02.027
47. Ren, L, Geng, Q, Wang, J, and Wang, Z. Therapeutic effect of pricking and cupping combined with fumigation and moxibustion on localized neurodermatitis. Chin J Pract Med. (2023) 50:112–5. doi: 10.3760/cma.j.cn115689-20230712-02580
48. Meng, X. Clinical analysis of 182 patients with neurodermatitis and its relationship with nerve anxiety. Chin J Pract Nervous Dis. (2015) 18:49–50.
49. He, B, and Lin, Z. Analysis of the effect of walking cupping method on serum tumor necrosis factor α and vascular endothelial growth factor levels in patients with psoriasis vulgaris and blood stasis syndrome and its clinical efficacy. J Guangzhou Univ Trad Chin Med. (2020) 37:64–8. doi: 10.13359/j.cnki.gzxbtcm.2020.01.012
50. Li, S, Yang, Y, Ze, K, Xu, R, Li, X, and Li, B. Research progress of acupuncture and cupping therapy in the treatment of psoriasis vulgaris. World Clin Drug. (2019) 40:811–5. doi: 10.13683/j.wph.2019.11.012
51. Wang, Y, and Xu, B. Research progress on acupuncture treatment of skin pruritus. J Basic Chin Med. (2014) 20:419–22. doi: 10.19945/j.cnki.issn.1006-3250.2014.03.061
52. Yang, J, Song, K, Liang, F, Zhao, C, and Yang, J. Effects of electroacupuncture on the content of inflammatory mediators in the inflammatory area of rats with adjuvant arthritis. J Chengdu Univ Trad Chin Med. (1999) 1:48–9.
53. Shen, T, Zhang, C, Fu, R, Yang, H, and Li, Z. Effects of fire needle on JNK and p 38 mitogen-activated protein kinase in ankle joints of rats with rheumatoid arthritis. J Nanjing Univ Chin Med. (2016) 32:548–52. doi: 10.14148/j.issn.1672-0482.2016.0548
54. Zhao, A, Li, L, and Cao, Y. Effects of fire acupuncture combined with Halomethasone ointment on symptom score and serum inflammatory factors in patients with Neurodermatitis. Chinese J Aesth Med. (2021) 30:125–8. doi: 10.15909/j.cnki.cn61-1347/r.004363
55. Ergang, P, Vodička, M, Vagnerová, K, Moravec, M, Kvapilová, P, Kment, M, et al. Inflammation regulates 11β-hydroxysteroid dehydrogenase type 1 differentially in specific compartments of the gut mucosal immune system—science direct. Steroids. (2017) 126:66–73. doi: 10.1016/j.steroids.2017.07.007
56. Pondeljak, N, Lugović-Mihić, L, Tomić, L, Parać, E, Pedić, L, and Lazić-Mosler, E. Key factors in the complex and coordinated network of skin keratinization: their significance and involvement in common skin conditions. Int J Mol Sci. (2024) 25:236. doi: 10.3390/ijms25010236
57. Saggini, A, Chimenti, S, and Chiricozzi, A. IL-6 as a Druggable target in psoriasis: focus on pustular variants. J Immunol Res. (2014) 2014:964069:1–10. doi: 10.1155/2014/964069
58. Lee, B-W, and Moon, S-J. Inflammatory cytokines in psoriatic arthritis: understanding pathogenesis and implications for treatment. Int J Mol Sci. (2023) 24:11662. doi: 10.3390/ijms241411662
59. Kee, JY, Jeon, YD, Kim, DS, Han, YH, Park, J, Youn, DH, et al. Korean red ginseng improves atopic dermatitis-like skin lesions by suppressing expression of proinflammatory cytokines and chemokines in vivo and in vitro. J Ginseng Res. (2017) 41:134–43. doi: 10.1016/j.jgr.2016.02.003
60. Long, X, and Yuan, J. Clinical observation of tazarotene gel combined with compound flumetasone ointment in the treatment of 62 patients with local neurodermatitis. Chin J Modern Drug Appl. (2017) 11:9–11. doi: 10.14164/j.cnki.cn11-5581/r.2017.24.004
Keywords: wet cupping, neurodermatitis, lichen simplex chronicus, efficacy, meta-analysis, systematic review
Citation: Zhai Y, Hui Y-y, Jiang Z-f, Ding L, Cheng J, Xing T, Zhai H and Zhang H (2024) Efficacy and safety of wet cupping in the treatment of neurodermatitis: a systematic review and meta-analysis. Front. Med. 11:1478073. doi: 10.3389/fmed.2024.1478073
Edited by:
Dawei Yang, Fudan University, ChinaReviewed by:
Chi-Wen Lung, University of Illinois at Urbana-Champaign, United StatesKamran Ali, Zhejiang University, China
Copyright © 2024 Zhai, Hui, Jiang, Ding, Cheng, Xing, Zhai and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Zhang, aHpoYW5nMDEyM0Bmb3htYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yan Zhai
Yan Zhai You-yi Hui2†
You-yi Hui2† Ze-fei Jiang
Ze-fei Jiang Lin Ding
Lin Ding Tang Xing
Tang Xing