- 1Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 2Key Laboratory of Ocular Fundus Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 3Eight-Year Medical Doctor Program, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Ophthalmology education is increasingly influenced by non-technical factors. This paper examines the multifaceted influences on ophthalmology education, focusing on direct and indirect factors that have shaped the training and wellbeing of ophthalmology students and residents. A systematic search of PubMed and Embase was carried out, searching date was from inception to 01/07/2024. A total of 8,232 articles were screened, of which 7,976 were excluded following abstract review. After reading the remaining 256 articles in full, a further 228 were excluded. A total of 28 original articles were included in this systematic review. The non-technical factors that influenced ophthalmology education included various crisis, inadequate curricular time, training resources, lack of training standardization and shortage of financial support and teaching resources. The review summarizes the influences on ophthalmology education of various non-technical factors, thereby helping educators improve the training methods.
1 Introduction
Ophthalmology education, traditionally centered around technical skills and clinical expertise, is increasingly influenced by a myriad of non-technical factors. These factors, encompassing mental health, economic conditions, gender dynamics, intrinsic motivation, and communication skills, play a crucial role in shaping the educational landscape for future ophthalmologists. Understanding these influences is essential for developing comprehensive training programs that address not only the technical competencies but also the holistic development of medical professionals.
Recent global events, such as the COVID-19 pandemic, have underscored the importance of considering non-technical influences in medical education. The pandemic has brought to light the significant psychological toll on students and residents, disrupting traditional educational pathways and necessitating a shift to virtual learning environments. Concurrently, economic crises and other societal disruptions have further strained educational resources and opportunities, highlighting the need for resilient and adaptable educational frameworks.
Gender dynamics within ophthalmology education also warrant attention. Studies indicate that gender-related factors influence career choices, mentorship opportunities, and educational experiences, thereby impacting the overall diversity and inclusivity within the field. Additionally, intrinsic motivation and self-determination are pivotal in fostering effective learning environments. The creation of supportive educational settings that meet students’ psychological needs can enhance their engagement and professional growth.
Effective communication skills are equally vital in medical training, influencing patient interactions and clinical outcomes. As such, the development of these skills should be integral to ophthalmology education, ensuring that graduates are not only technically proficient but also adept at building rapport with patients.
This research aims to explore the diverse non-technical factors impacting ophthalmology education, drawing on recent studies and surveys to provide a comprehensive understanding of their implications. By examining these influences, we seek to inform the development of more holistic and adaptive educational strategies that can better prepare future ophthalmologists for the complexities of their profession.
2 Materials and methods
2.1 Eligibility criteria
All original studies were evaluated if they described development in ophthalmic training. Studies were included: (1) study participants were ophthalmologists or medical students who were accepting their ophthalmology training; (2) studies related to non-technical factors. Studies were excluded: (1) if they did not provide original data; (2) articles not specific to ophthalmology; (3) studies not related to training or education. We included papers written in English.
2.2 Search methods
A systematic search of PubMed and Embase was carried out, using the terms “(train* OR education OR learning) AND ophthalm*”. Search date was from inception to 01/07/2024. Reference lists from included articles and relevant reviews were hand searched for eligible studies.
2.3 Study selection
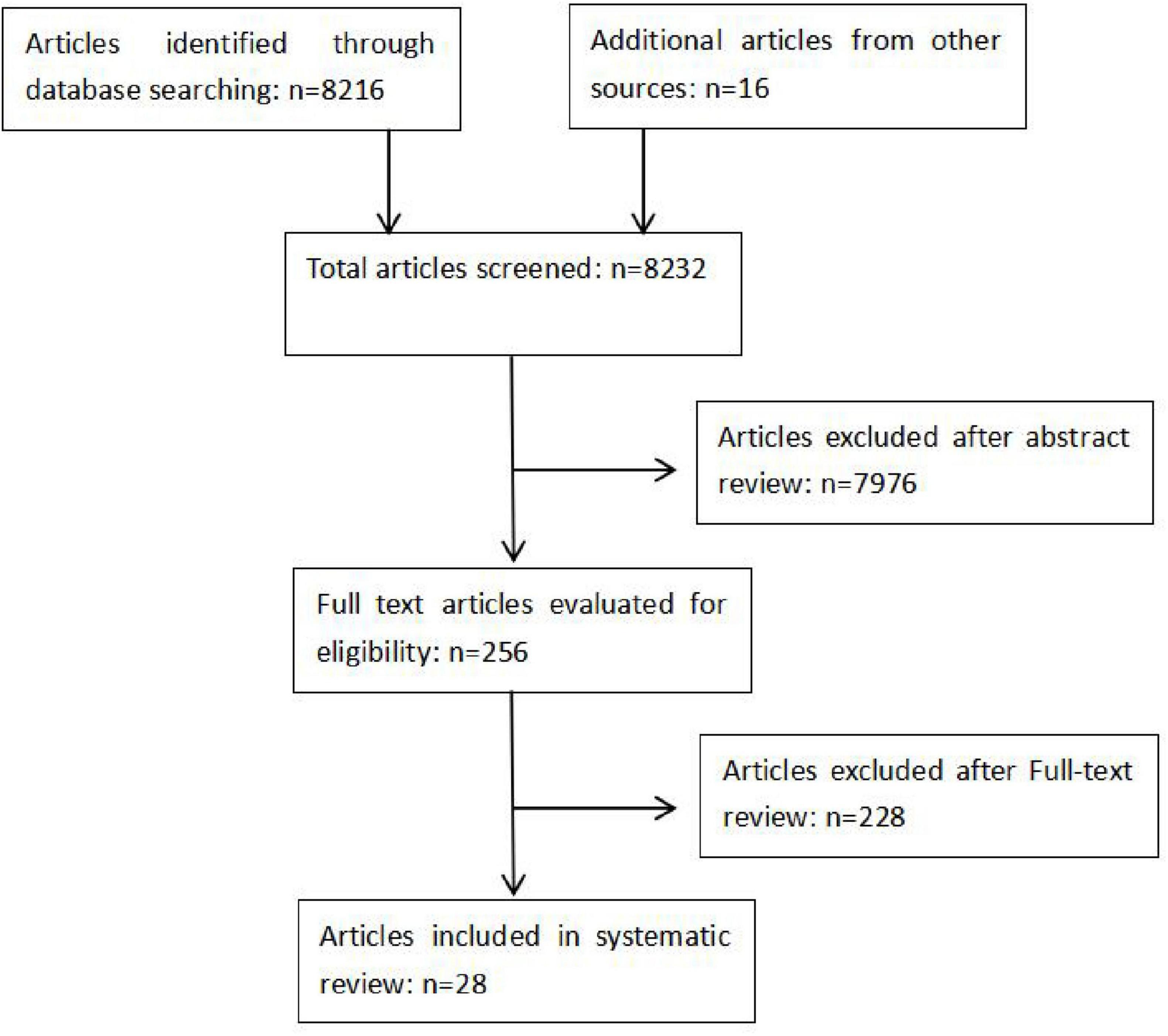
Two authors, YJ and HJ, carried out independent, duplicate searches. All abstracts were reviewed and articles that were potentially eligible were read in full. A final list of studies meeting the eligibility criteria was compared and disagreements resolved by discussion (Figure 1).
2.4 Data collection
The same two authors extracted data for each study separately and differences were resolved through discussion. Data collected included details of the observation subject, sample size, methods and evaluation results.
3 Results
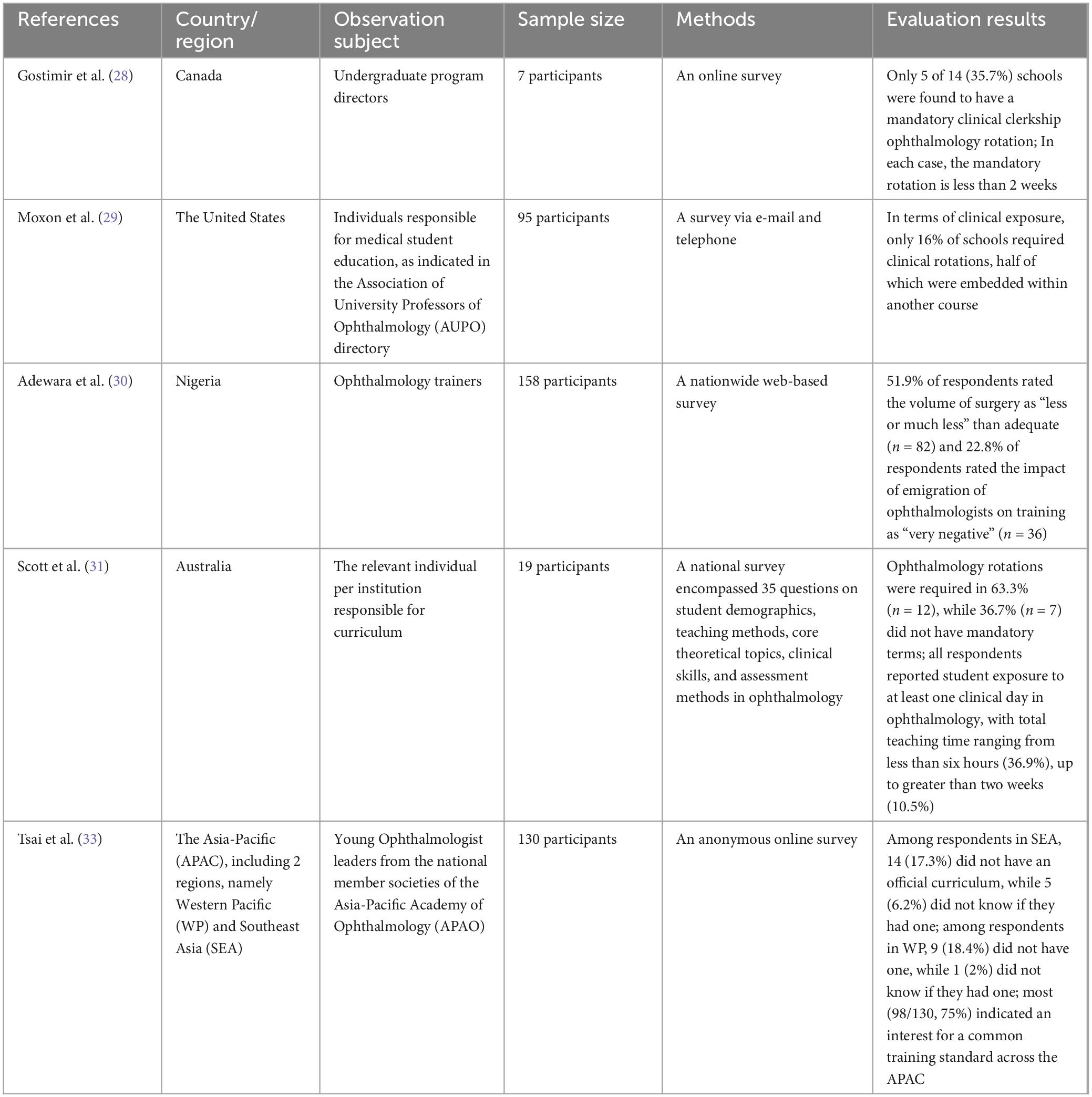
A total of 8,232 articles were screened, of which 7,976 were excluded following abstract review. After reading the remaining 256 articles in full, a further 228 were excluded. A total of 28 original articles were included in this systematic review (Figure 1). Details of findings are summarized in Tables 1–4 according to the different non-technical factors on ophthalmology education.
3.1 Direct factors
3.1.1 Coronavirus disease 2019
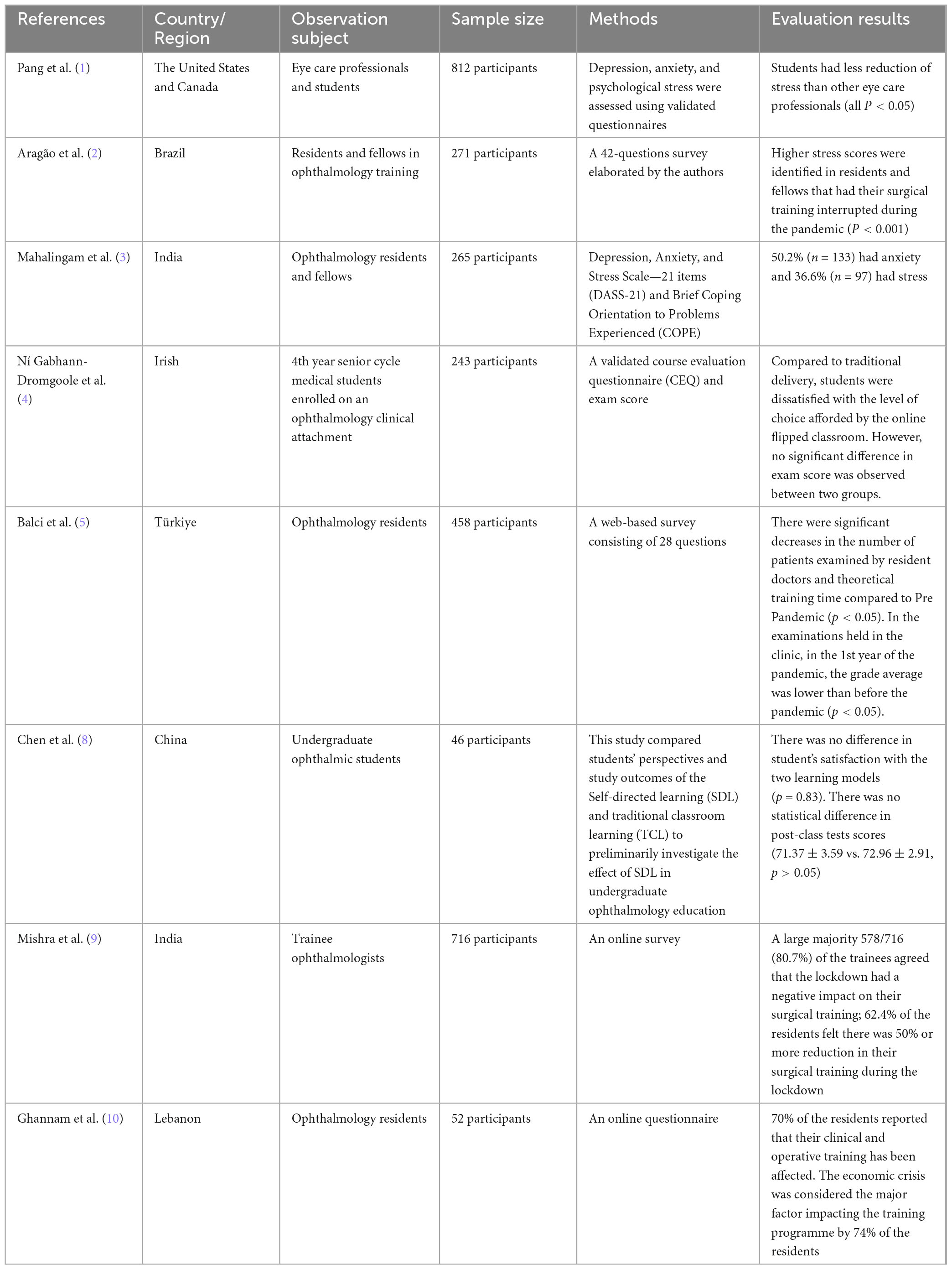
Pang et al. (1) conducted a longitudinal study to evaluate the mental health impact of the COVID-19 pandemic on ophthalmic personnel and students. The study identified students experiencing high stress levels. Aragão et al. (2) evaluated the impact of the COVID-19 pandemic on the mental health of ophthalmology residents and fellows in Brazil. Using a 42-question survey that included the Perceived Stress Scale (PSS-10), the study found that both residents and fellows experienced similar stress levels during the pandemic, but those who had their surgical training interrupted reported significantly higher stress levels. Mahalingam et al. (3) conducted a survey to evaluate the long-term impact of the COVID-19 pandemic on the training and mental health of ophthalmology residents and fellows in India. The study, which involved 265 participants, found a significant reduction in clinical exposure and surgical cases, with participants handling only 29.6–46.6% of the pre-pandemic volume. The study revealed high levels of depression, anxiety, and stress among participants, with 55.8% experiencing depression and 50.2% reporting anxiety. It has been demonstrated that COVID-19 pandemic had negative impact on mental health of ophthalmology residents.
Ní Gabhann-Dromgoole et al. (4) evaluated the shift to online learning for ophthalmology education during the COVID-19 pandemic. The study compared traditional delivery (TD) and online flipped classroom (OFC) approaches among 243 fourth-year medical students. Results indicated that OFC students reported reduced satisfaction with staff motivation, feedback, and clarity of work standards. They also found the OFC less beneficial for developing problem-solving skills. Balci et al. (5) examined the impact of the COVID-19 pandemic on ophthalmology residency education in Turkey. The study surveyed 37 educators across 35 centers, highlighting significant reductions in patient examinations, theoretical training, and surgical procedures during the pandemic compared to the pre-pandemic period. Most residents (53.71%) worked on COVID-19 duties, averaging 69.57 days away from their own clinics. Theoretical training shifted largely online, with many hospitals implementing physical distancing measures for in-person sessions. The study noted declines in academic publications and congress participation, alongside increased stress and resignations among residents. These findings underscore the pandemic’s severe disruptions to ophthalmology education and training. It has been demonstrated that COVID-19 pandemic had influenced the conventional ophthalmology education.
Martins et al. (6) addressed the challenges of teaching ophthalmology during the COVID-19 pandemic by developing a new methodology for teaching direct ophthalmoscopy and red reflex testing. The approach involved online theoretical classes using platforms like YouTube to provide tutorials and enable students to construct teaching dummies, thereby enhancing their understanding of the examination’s fundamental principles. Practical sessions used these dummies and portable handheld fundus cameras, allowing real-time supervision and reducing in-person class time without compromising teaching quality.
Patel et al. (7) explored the adaptations in medical education and ophthalmology residency interviews due to the COVID-19 pandemic. The study highlighted the shift to virtual platforms for residency interviews and educational activities. Social media usage by ophthalmology programs increased significantly, with Instagram and Twitter being the most popular. The study found that virtual tools like open houses and simulated internships helped maintain educational standards. Chen et al. (8) explored the efficacy of self-directed learning (SDL) as an alternative to traditional classroom learning (TCL) in undergraduate ophthalmic education during the COVID-19 pandemic in China. The findings revealed no significant difference in learning outcomes or student satisfaction between the two models. However, students with a high interest in ophthalmology found SDL more effective in enhancing self-study ability and learning efficiency, whereas TCL was preferred for developing problem-solving skills. Mishra et al. (9) reported that a large majority 578/716 (80.7%) of the trainees agreed that the lockdown had a negative impact on their surgical training, 62.4% of the residents felt there was 50% or more reduction in their surgical training during the lockdown. It has been demonstrated that COVID-19 pandemic had reduce the training opportunity for ophthalmology trainees.
3.1.2 Economic crisis
Ghannam et al. (10) investigated the effects of the economic crisis, and the Beirut explosion on ophthalmology training in Lebanon. This observational cohort survey included 52 participants, revealing that the majority experienced significant disruptions in training and mental health challenges, including increased stress, anxiety, and depression. The study highlighted financial burdens, reduced patient loads, and a decrease in surgical and educational activities as primary issues.
3.2 Indirect factors
3.2.1 Gender
Aljuhani et al. (11) authored the research, published in Cureus in 2023. This cross-sectional study investigates the influence of gender on the decision to pursue ophthalmology as a career among medical students and interns in Madinah, Saudi Arabia. Data from 449 participants revealed that while fewer working hours attracted males to ophthalmology, females were more interested in the anatomy and physiology of the eye. Huh et al. (12) authored the study published in JAMA Ophthalmology in 2023. The retrospective cross-sectional study examines gender differences in ACGME Milestone ratings among ophthalmology residents. Analyzing data from 452 residents, the study found no significant gender differences in patient care ratings at midyear or year-end. However, female residents had lower midyear medical knowledge ratings compared to male residents. The findings suggest the need for ongoing examination of potential biases in resident evaluations to ensure fair educational and career opportunities. Paul et al. (13) authored the research, published in the American Journal of Ophthalmology in 2022. The study evaluates attitudes toward mentorship of female medical students among ophthalmology educators. Using a cross-sectional survey, the research found that while both male and female respondents mentored a similar percentage of female students, female respondents placed higher importance on gender-specific mentorship. The study suggests that expanding female mentorship in ophthalmology could promote equity in training and address the lack of female representation in leadership roles.
3.2.2 Intrinsic motivation
Dutt et al. (14) examined the factors influencing medical students’ autonomy, competence, and relatedness in ophthalmology education through the lens of Self-Determination Theory (SDT). The study, conducted at the University of Western Australia, identified that intrinsic motivation is crucial for effective learning and student contentment. The researchers highlighted the importance of creating environments that satisfy students’ basic psychological needs to foster intrinsic motivation, which in turn enhances learning outcomes and promotes continuous professional development.
3.2.3 Communication skills
Li et al. (15) examined the willingness of outpatients in China to undergo fundus examinations conducted by ophthalmology residents as part of the National Standardized Training for Resident Doctors (STRD). The study, involving 261 valid responses, identified that patient cooperation was influenced by the demeanor of the residents, and the quality of doctor-patient communication. These findings suggest that improving communication skills among residents could significantly increase patient cooperation, thereby improving the effectiveness of ophthalmology training programs in China.
3.3 Non-technical factors in advanced ophthalmic training
In recent years, a large number of new techniques have emerged in ophthalmology education, including: virtual reality and physical models (e.g., three-dimensional 3D technology). Novel techniques can drastically improve the trainees’ clinical competence (16–26). However, among the novel training techniques, there were still non-technical factors that could affect ophthalmology education.
3.3.1 Fatigued training could reduce learning effectiveness
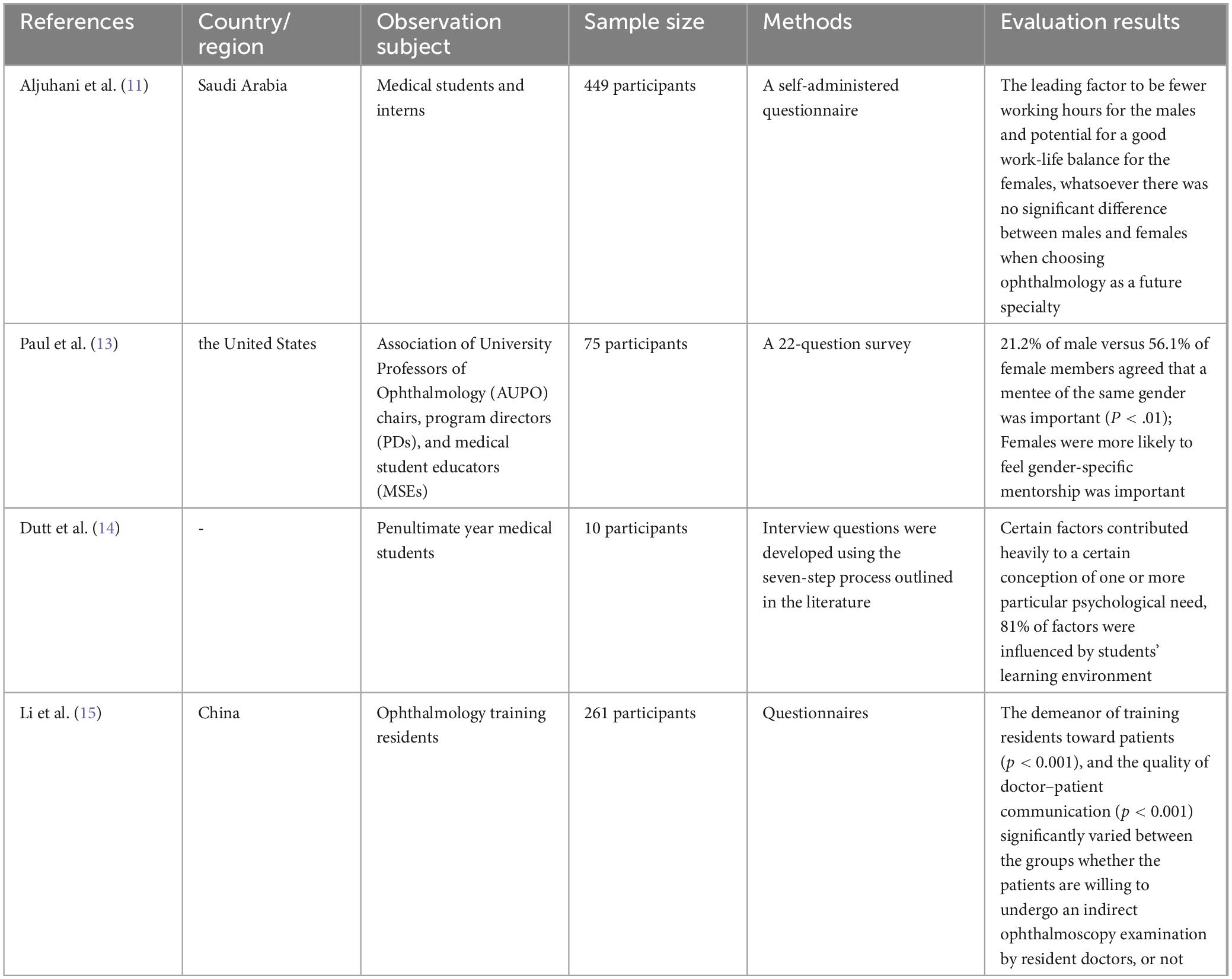
Feudner et al. (16) reported that for students and residents taken together, subjects with a low number of attempts on training had a higher probability to perform well than the group with a higher number of attempts. Cissé et al. (17) reported that fatigue and loss of concentration over time may have affected residents’ performance, as demonstrated by the lower scores of the last tasks. They suggests that several short sessions are probably more effective than a single longer one.
3.3.2 The high expense of the advanced training equipment posed a great barrier for their application in ophthalmology education
Despite evidence that novel technologies like virtual reality simulator-based surgical training yields positive outcomes, not all fellowship programs can afford to include simulator training in their curriculum owing to the high expense of the equipment and the need for periodic upgradation (19). According to La Cour et al. (27), this poses a great barrier to establishing a simulated training curriculum.
3.3.3 Other non-technical limits
Mondal et al. (19) reported that the main reasons limiting the utilization of the simulators to their full capacity were the unavailability of the simulator beyond their working hours (54.8%), the lack of a structured training program (19.3%), and the scarcity of a dedicated supervisor (16.1%).
To sum up, the influence of various non-technical factors on the new technology of ophthalmology teaching clearly exists. Combining the non-technical factors discussed above, it is suggested that short sessions of training is recommended to the trainees, sufficient financial support and strong teaching resources are necessary to provide efficient ophthalmic training for the trainees.
3.4 Problems and shortcomings
3.4.1 Lack of curricular and clinical rotation time
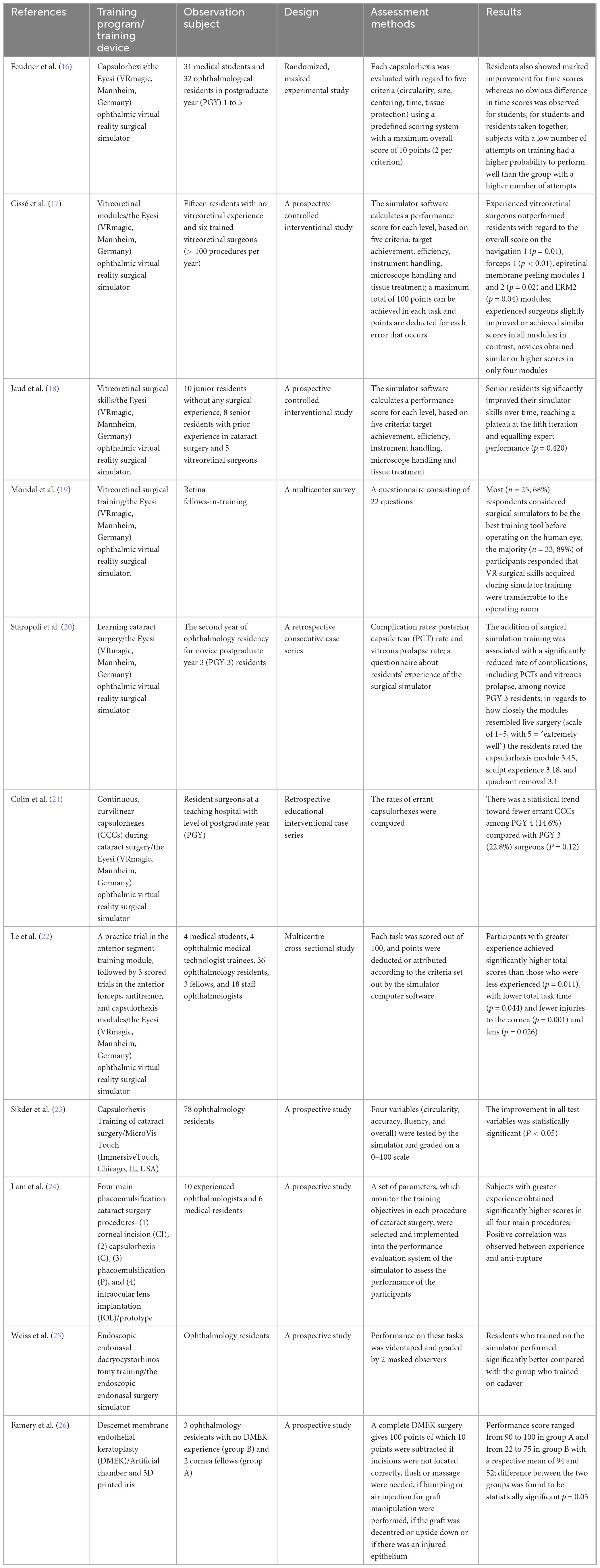
Gostimir et al. (28) assessed the state of undergraduate ophthalmology education in Canadian medical schools through a survey of program directors. The study found that only 35.7% of schools required a mandatory clinical rotation in ophthalmology, typically lasting less than two weeks. Moxon et al. (29) analyze the state of ophthalmology education for medical students in the United States. Their survey of 117 institutions reveals a decline in curricular time dedicated to ophthalmology, now often confined to preclinical years with supplemental extracurricular activities. The study highlights the importance of continuous adaptation in medical education to maintain ophthalmic training quality.
3.4.2 Lack of training resources
Adewara et al. (30) conducted a web-based survey of ophthalmology trainers in Nigeria to assess the ophthalmology residency training. With a response rate of 71.2%, the survey highlighted that while the overall quality of training was rated as good, significant inadequacies were noted in surgical volume and resources. Trainers recommended improvements in funding, training resources, and examination practices.
3.4.3 Lack of training standardization
Scott et al. (31) conducted a national survey on ophthalmology education in Australian medical schools. The survey, which included responses from 19 of 21 medical schools, found that 63.3% required ophthalmology rotations, while 36.7% did not. Chinese ophthalmology residency training is continuously evolving with an emphasis on standardization. Wang et al. (32) assesses the current status of ophthalmology residency training in China compared with that in the United States. It reveals significant regional differences among training programs due to the lack of a national standard, resulting in varying competencies of graduating Chinese ophthalmology residents. A survey of ophthalmology training experiences (33) among young ophthalmologists in the Asia-Pacific region highlights the diversity in training experiences across different countries. The study compares experiences between trainees from Southeast Asia and Western Pacific countries, revealing differences in training quality, exposure to various subspecialties, and satisfaction levels. The findings emphasize the need for standardized training curricula to ensure consistent competency among ophthalmologists in the region.
3.4.4 The decline of ophthalmology education
Liao et al. (34) explores the current challenges and potential solutions in ophthalmology education within US and Canadian medical schools. Utilizing a systematic review of 66 articles, the study identifies four main themes: challenges in curriculum standardization, inadequate clinical exposure, the role of technology, and innovative teaching methods. Spencer et al. (35) conducted a systematic review to analyze trends in ophthalmology education in medical schools worldwide. This study reviewed 52 publications from 19 countries, highlighting a significant decline in course lengths over the past two decades, with averages dropping from 92.9 h in the 2000s to 52.9 h in the 2020s. Students reported low confidence in their ophthalmic knowledge and skills, with only 26.4% feeling confident in their knowledge and 34.5% in their skills.
3.4.5 The future of ophthalmology education
Maling et al. (36) propose the need for global standards in ophthalmology training, citing significant variations in curricula, learning outcomes, and procedural requirements across different countries. They emphasize the importance of modern training tools such as AI, simulation, and virtual reality. The authors propose that establishing international standards could enhance the quality and consistency of ophthalmological education, ensuring better preparedness and skill proficiency among trainees.
4 Discussion
Vision has an enormous impact on quality of life. Blindness is ranked by the public to be the worst disease or ailment possible (37). Misdiagnosis and delayed diagnosis lead to demonstrated poor patient outcomes, including permanent vision loss, severe pain (38), and potentially loss of life. Thus, the ability to assess, interpret, and manage ophthalmic signs and ocular disease is essential to the training of safe medical practitioners. Understanding and surgical skills garnered in ophthalmic education is essential to the clinical competence.
The comprehensive analysis of various non-technical factors influencing ophthalmology education underscores the multifaceted challenges and opportunities within this field.
The COVID-19 pandemic has notably disrupted traditional educational practices, leading to heightened stress, anxiety, and depression among ophthalmic personnel and students. The shift to online learning and virtual platforms, while necessary, has yielded mixed results, highlighting the need for more effective and engaging educational methodologies. Economic crises, such as the Beirut explosion, have further compounded these challenges, exacerbating financial burdens and reducing clinical and surgical training opportunities. Significant heterogeneity in ophthalmology training exist in different regions. Major differences exist in surgical and medical competencies of doctors between Southeast Asia (SEA) and Western Pacific (WP). There were significant differences in the types of cataract surgeries performed between WP and SEA trainees. WP trainees performed more phacoemulsification surgeries (76, 0–500 vs. 19, 0–275, P = 0.004), extracapsular cataract extraction (34, 0–200 vs. 9, 0–50, P = 0.001), and intracapsular cataract extraction (1.5, 0–50 vs. 0.8, 0–15, P = 0.47) cases than their counterparts in SEA during their training. Gender dynamics play a crucial role in shaping career choices and educational experiences in ophthalmology, necessitating targeted mentorship programs to ensure equitable opportunities for all genders. Intrinsic motivation, driven by supportive educational environments that fulfill students’ psychological needs, is essential for effective learning and professional growth. Enhancing communication skills among residents can significantly improve patient cooperation and overall training effectiveness.
Persistent issues such as the lack of curricular and clinical rotation time, inadequate training resources, and the absence of standardized training curricula highlight the need for continuous adaptation and improvement in ophthalmology education. The decline in ophthalmology course lengths and the resultant low confidence among students in their ophthalmic knowledge and skills call for innovative teaching methods and increased clinical exposure. Looking forward, the establishment of global standards in ophthalmology training, coupled with the integration of modern training tools such as AI, simulation, and virtual reality, is imperative.
In recent years, a large number of novel techniques have emerged in ophthalmology. Among theses ophthalmic training, there were still non-technical factors that would influence ophthalmology education. Fatigue and loss of concentration over time may have affected residents’ performance (26). Insufficient financial support would pose a great barrier to establishing an advanced training curriculum (36). Lack of human resources in teaching could limit the utilization of the advanced training techniques to their full capacity (28). Therefore, multiple short sessions of training is suggested to the trainees, sufficient financial support and strong teaching resources are recommended to provide efficient ophthalmic training by the use of the novel techniques.
5 Conclusion
The non-technical factors that influenced ophthalmology education included various crisis, inadequate curricular time, training resources, lack of training standardization and shortage of financial support and teaching resources. The review summarizes the influences on ophthalmology education of various non-technical factors, thereby helping educators improve the training methods.
Author contributions
YJ: Writing – original draft. HJ: Writing – original draft. ZY: Writing – review and editing. YL: Writing – review and editing. YC: Writing – review and editing.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Beijing Health Achievements in Technology and Effective Technology Transfer Foundation (BHATET2024-03).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pang Y, Robbs C, Wang J. A longitudinal study of the COVID-19 pandemic impact on mental health in ophthalmic personnel and students. PLoS One. (2024) 19(3):e0300144. doi: 10.1371/journal.pone.0300144
2. Aragão IO, Alencar TGC, Soares AKA, da Rocha CS, Ventura CV. Effects of COVID-19 pandemic on stress level of residents and fellows during ophthalmology training. Indian J Ophthalmol. (2022) 70:2170–3. doi: 10.4103/ijo.IJO_401_22
3. Mahalingam K, Sharma N, Ganesh R, Panigrahi A, Patil V, Saxena R. The impact of COVID-19 pandemic on training and mental health of ophthalmology residents and fellows in India: A survey. Indian J Ophthalmol. (2023) 71(9):3262–3. doi: 10.4103/IJO.IJO_1776_23
4. Ní Gabhann-Dromgoole J, Murphy CC, Boland F, Doyle AJ, Pawlikowska T. How has medical student learning changed with the pivot to online delivery of ophthalmology in the pandemic? PLoS One. (2023) 18(3):e0282829. doi: 10.1371/journal.pone.0282829
5. Balci AS, Altan C, Taskapili M. The impact of COVID-19 pandemic on ophthalmology residency education. Beyoglu Eye J. (2022) 7(3):213–22. doi: 10.14744/bej.2022.58234
6. Martins TG, Benchimol GL, Gameiro GR, Schor P. Learning and teaching ophthalmology in the pandemic. einstein (São Paulo). (2022) 20:eCE6988. doi: 10.31744/einstein_journal/2022CE6988
7. Patel OU, Bonner A, Sisk M, Grant MB. Dynamic changes in medical education amidst the COVID-19 pandemic: Adapting to virtual ophthalmology residency interviews. Ann Med Surg. (2022) 76:103417. doi: 10.1016/j.amsu.2022.103417
8. Chen L, Tang X-J, Liu Q, Zhang X. Self-directed learning: Alternative for traditional classroom learning in undergraduate ophthalmic education during the COVID-19 pandemic in China. Heliyon. (2023) 9(5):e15632. doi: 10.1016/j.heliyon.2023.e15632
9. Mishra D, Nair AG, Gandhi RA, Gogate PJ, Mathur S, Bhushan P, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India - Outcomes of a survey. Indian J Ophthalmol. (2020) 68:999–1004. doi: 10.4103/ijo.IJO_1067_20
10. Ghannam AB, Ibrahim HA, Hammoud B, Hamam R. Impact of the economic crisis, COVID-19 and the Beirut explosion on ophthalmology training in Lebanon: An observational cohort survey-based study. BMJ Open. (2024) 14:e075321. doi: 10.1136/bmjopen-2023-075321
11. Aljuhani GA, Abdulaziz M, Alharbi AS. The influence of gender on choosing ophthalmology as a career among medical students and interns in Madinah. Saudi Arabia. Cureus. (2023) 15(9):e44936. doi: 10.7759/cureus.44936
12. Huh DD, Yamazaki K, Holmboe E, Bartley GB, Schnabel SD, Levine RB, et al. Gender bias and ophthalmology accreditation council for graduate medical education milestones evaluations. JAMA Ophthalmol. (2023) 141(10):982–8. doi: 10.1001/jamaophthalmol.2023.4138
13. Paul M, Dweck M, Chadha N. Ophthalmology education leadership attitudes toward mentorship of female medical students. Am J Ophthalmol. (2022) 243:149–57. doi: 10.1016/j.ajo.2022.07.026
14. Dutt DDCS, Razavi H, Carr SE. Self-determination theory in ophthalmology education: Factors influencing autonomy, competence and relatedness in medical students. Med Educ. Online (2023) 28(1):2258633. doi: 10.1080/10872981.2023.2258633
15. Li H, Li T, Fan Y, Zheng B, Zhao Y. A survey on the willingness of outpatients to participate in fundus examination procedures conducted by ophthalmology training residents in China: A cross-sectional study. Health Sci Rep. (2024) 7:e1870. doi: 10.1002/hsr2.1870
16. Feudner EM, Engel C, Neuhann IM, Petermeier K, Bartz-Schmidt K, Szurman P. Virtual reality training improves wet-lab performance of capsulorhexis: Results of a randomized, controlled study. Graefes Arch Clin Exp Ophthalmol. (2009) 247(7):955–63. doi: 10.1007/s00417-008-1029-7
17. Cissé C, Angioi K, Luc A, Berrod J, Conart J. EYESI surgical simulator: Validity evidence of the vitreoretinal modules. Acta Ophthalmol. (2019) 97(2):e277–82. doi: 10.1111/aos.13910
18. Jaud C, Salleron J, Cisse C, Angioi-Duprez K, Berrod J, Conart J. EyeSi Surgical Simulator: Validation of a proficiency-based test for assessment of vitreoretinal surgical skills. Acta Ophthalmol. (2021) 99(4):390–6. doi: 10.1111/aos.14628
19. Mondal S, Kelkar AS, Singh R, Jayadev C, Saravanan VR, Kelkar JA. What do retina fellows-in-training think about the vitreoretinal surgical simulator: A multicenter survey. Indian J Ophthalmol. (2023) 71(8):3064–8. doi: 10.4103/IJO.IJO_381_23
20. Staropoli PC, Gregori NZ, Junk AK, Galor A, Goldhardt R, Goldhagen BE, et al. Surgical simulation training reduces intraoperative cataract surgery complications among residents. Simul Healthc. (2018) 13(1):11–5. doi: 10.1097/SIH.0000000000000255
21. Colin A, McCannel, David C, Reed, Darin R, Goldman. Ophthalmic surgery simulator training improves resident performance of capsulorhexis in the operating room. Ophthalmology. (2013) 120(12):2456–61. doi: 10.1016/j.ophtha.2013.05.003
22. Le TBD, Adatia FA, Lam W. Virtual reality ophthalmic surgical simulation as a feasible training and assessment tool: Results of a multicentre study. Can J Ophthalmol. (2011) 46(1):56–60. doi: 10.3129/i10-051
23. Sikder S, Luo J, Banerjee P, Luciano C, Kania P, Song JC, et al. The use of a virtual reality surgical simulator for cataract surgical skill assessment with 6 months of intervening operating room experience. Clin Ophthalmol. (2015) 20(9):141–9. doi: 10.2147/OPTH.S69970
24. Lam CK, Sundaraj K, Sulaiman MN, Qamarruddin FA. Virtual phacoemulsification surgical simulation using visual guidance and performance parameters as a feasible proficiency assessment tool. BMC Ophthalmol. (2016) 16:88. doi: 10.1186/s12886-016-0269-2
25. Weiss M, Lauer SA, Fried MP, Uribe J, Sadoughi B. Endoscopic endonasal surgery simulator as a training tool for ophthalmology residents. Ophthalmic Plast Reconstr Surg. (2008) 24(6):460–4. doi: 10.1097/IOP.0b013e31818aaf80
26. Famery N, Abdelmassih Y, El-Khoury S, Guindolet D, Cochereau I, Gabison EE. Artificial chamber and 3D printed iris: A new wet lab model for teaching Descemet’s membrane endothelial keratoplasty. Acta Ophthalmol. (2019) 97(2):e179–83. doi: 10.1111/aos.13852
27. La Cour M, Thomsen ASS, Alberti M, Konge L. Simulators in the training of surgeons: Is it worth the investment in money and time? 2018 Jules Gonin lecture of the retina research foundation. Graefes Arch Clin Exp Ophthalmol. (2019) 257:877–81. doi: 10.1007/s00417-019-04244-y
28. Gostimir M, Sharma RA, Bhatti A. Status of Canadian undergraduate medical education in ophthalmology. Can J Ophthalmol. (2018) 53(5):474–9. doi: 10.1016/j.jcjo.2017.11.015
29. Moxon NR, Goyal A, Giaconi JA, Rosenberg JB, Graubart EB, Waxman EL, et al. The state of ophthalmology medical student education in the United States: An update. Ophthalmology. (2020) 127(11):1451–3. doi: 10.1016/j.ophtha.2020.05.001
30. Adewara BA, Adeoye AO, Awe OO, Oyedun TO, Akinde MO. Ophthalmology residency training in Nigeria: The trainers’ perspective. Nigerian Postgraduate Med J. (2023) 30(1):61–9. doi: 10.4103/npmj.npmj_272_22
31. Scott TM, Succar T, Petsoglou C. Ophthalmology teaching in Australian medical schools: A national survey. Med Teach. (2022) 44(10):1173–8. doi: 10.1080/0142159X.2022.2072283
32. Wang YE, Zhang C, Chen AC, Pineles A, Hou J. Current status of ophthalmology residency training in China: The experience from well-structured centers around the country. Asia Pac J Ophthalmol. (2020) 9(2020):369–73. doi: 10.1097/APO.0000000000000284
33. Tsai ASH, Yeo BSY, Alaminos RA, Wong CW, Tham CC, Fang SK. Survey of Ophthalmology training experiences among young ophthalmologists in the Asia-Pacific. Asia Pac J Ophthalmol. (2022) 11(2022):434–40. doi: 10.1097/APO.0000000000000556
34. Liao J, Wright RR, Vora GK. The decline of basic ophthalmology in general medical education: A scoping review and recommended potential solutions. J Med Educ Curricular Dev. (2024) 11:1–22. doi: 10.1177/23821205241245635
35. Spencer SKR, Ireland PA, Braden J, Hepschke JL, Lin M, Zhang H. A systematic review of ophthalmology education in medical schools. Ophthalmology. (2024) 131:855–63. doi: 10.1016/j.ophtha.2024.01.005
36. Maling S, Kaur K, Gurnani B. Should there be global standards in ophthalmology training? Eye. (2023) 37:3710–1. doi: 10.1038/s41433-023-02582-0
37. Scott AW, Bressler NM, Ffolkes S. Public attitudes about eye and vision health. JAMA Ophthalmol. (2016) 134(10):1111–8.
Keywords: ophthalmology education, non-technical factors, training, educators, trainees
Citation: Jiang Y, Jiang H, Yang Z, Li Y and Chen Y (2024) Non-technical factors on ophthalmology education: a narrative review. Front. Med. 11:1468631. doi: 10.3389/fmed.2024.1468631
Received: 22 July 2024; Accepted: 29 October 2024;
Published: 15 November 2024.
Edited by:
Jinhai Huang, Fudan University, ChinaReviewed by:
Lijun Zhang, Dalian No.3 People’s Hospital, ChinaZhao Shaozhen, Tianjin Medical University Eye Hospital, China
Copyright © 2024 Jiang, Jiang, Yang, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhikun Yang, eWFuZ3poaWt1bkBwdW1jaC5jbg==; Ying Li, bGl5aW5nNjAwN0BwdW1jaC5jbg==; Youxin Chen, Y2hlbnlvdXhpbnB1bWNoQDE2My5jb20=
†These authors have contributed equally to this work
 Yang Jiang
Yang Jiang Hanyu Jiang1,2,3†
Hanyu Jiang1,2,3† Zhikun Yang
Zhikun Yang Youxin Chen
Youxin Chen