- 1Department of Respiratory and Critical Care Medicine, Shanghai Xuhui Central Hospital, Shanghai, China
- 2Nursing Department, Shanghai Xuhui Central Hospital, Shanghai, China
- 3Department of Critical Care Medicine, Shanghai Xuhui Central Hospital, Shanghai, China
- 4Department of Infectious Disease, Shanghai Xuhui Central Hospital, Shanghai, China
Objective: Nurses are key in administering oxygen therapy and managing its potential adverse effects in medical settings. This study aimed to investigate the knowledge, attitudes, and practices (KAP) regarding low-flow oxygen therapy and humidification among nurses.
Methods: This cross-sectional study was conducted from January 2024 to March 2024 at Shanghai Xuhui Central Hospital. Demographic data and KAP scores were collected through questionnaires.
Result: A total of 243 valid questionnaires were collected. Among them, 228 (93.8%) were female, and 93 (38.3%) had been working for more than 10 years. The mean scores for knowledge, attitudes, and practices were 11.11 ± 4.30 (Ranging 0–18), 29.14 ± 3.41 (Ranging 7–35), and 28.07 ± 4.73 (Ranging 7–35), respectively. Multivariate logistic regression confirmed that knowledge (OR = 1.302, 95% CI: [1.167–1.453], p < 0.001) and attitudes (OR = 1.196, 95% CI: [1.080–1.325], p < 0.001) were independently associated with proactive practices. Structural equation modeling (SEM) corroborated the direct influences of training (β = 3.210, p < 0.001) and clinical experience (β = 2.044, p = 0.002) on knowledge, with knowledge (β = 0.379, p < 0.001) and gender (β = −1.642, p = 0.037) directly impacting attitudes. Additionally, knowledge (β = 0.395, p < 0.001), attitudes (β = 0.340, p < 0.001), and equipment utilization (β = 1.098, p < 0.001) directly influenced practices.
Conclusion: Nurses demonstrated inadequate knowledge, positive attitudes, and inactive practices toward low-flow oxygen therapy and humidification. Enhanced training and increased clinical experience are recommended to improve nurses’ knowledge and practice in this area.
Introduction
Oxygen therapy is the primary treatment for hypoxemia, aiming to enhance arterial oxygen pressure. This method is particularly vital in the Department of Respiratory Medicine, where hypoxemia frequently occurs due to inadequate gas exchange in the lungs, caused by factors such as hypoventilation, ventilation/perfusion (V/Q) mismatch, intrapulmonary right-to-left shunting, diffusion impairment, or combinations of these (1). If administered correctly, oxygen therapy can greatly improve treatment outcomes and even save lives. However, its improper use may lead to severe complications (2).
Oxygen is delivered through various systems, categorized into low-flow and high-flow. Low-flow systems provide oxygen at rates below the patient’s inspiratory flow rate, around 30 L/min, whereas high-flow systems exceed the patient’s inspiratory flow in the hope of ensuring adequate oxygenation (3). The devices used in these systems range from face masks and nasal cannulas to more specialized options like Venturi masks, partial and non-re-breather masks, and trans-tracheal catheters (4, 5). Among these, the high-flow nasal cannula (HFNC) has gained prominence for delivering a heated and humidified high-flow air-oxygen mixture. Studies have demonstrated that HFNC outperforms conventional oxygen therapy methods in effectiveness (6–8). Conversely, the routine humidification of oxygen in low-flow systems is not always justifiable. Non-humidified oxygen is particularly advantageous as it reduces bacterial contamination in humidifier bottles, decreases the risk of respiratory infections, and maintains effective oxygen administration times without significant adverse effects on patient comfort or oxygen saturation levels (9).
The Knowledge-Attitude-Practice (KAP) model is crucial in understanding and shaping health behaviors, serving as a foundational component of health literacy. This model posits that knowledge positively influences attitudes, which in turn affect practices (10). It is commonly utilized in conjunction with the KAP questionnaire to thoroughly assess the knowledge, attitudes, and practices of healthcare professionals, as well as to evaluate the demand for and acceptance of relevant interventions within the healthcare sector (11). Nurses play a critical role in administering oxygen therapy and addressing its potential adverse effects in medical centers (12). However, research indicates a substantial knowledge gap among nurses regarding the correct use of oxygen therapy, which has been observed in various international studies (13–15).
Despite the broad application of the KAP model in healthcare research, there is a notable absence of studies specifically exploring low-flow oxygen therapy and humidification among nurses. Addressing this gap is essential for improving the standard of care and minimizing risks associated with oxygen therapy. Consequently, this study aims to investigate the knowledge, attitudes, and practices concerning low-flow oxygen therapy and humidification among nurses, to identify and address these specific educational needs.
Materials and methods
Study design and subjects
This cross-sectional study was conducted from January 2024 to March 2024 at Shanghai Xuhui Central Hospital, focusing on the nursing staff. This study was approved by Shanghai Xuhui Central Hospital Ethics Committee [(2023) Court Review No. (046)], and all participants provided written informed consent.
Nursing staff employed at hospital from January 2024 to March 2024 were included in the study. Exclusion criteria encompassed those who did not submit or selected “No” on the informed consent form, those who had not formally signed a labor contract with hospital, including dispatched personnel and exchange students, and populations deemed unsuitable for inclusion by other researchers.
The electronic questionnaire was created using the Questionnaire Star platform, with a QR code provided to participants. Respondents could access and complete the survey by scanning the QR code via WeChat or by using the provided link. To ensure data integrity and comprehensiveness, submissions were restricted to one per IP address, and all survey items were mandatory. Anonymity was guaranteed for all participants throughout the survey.
Questionnaire introduction
The questionnaire was designed based on established guidelines and literature (9, 16–21) and refined with input from four experts (one respiratory expert and three nursing experts). After incorporating their feedback, a preliminary version of the questionnaire was distributed on a small scale (51 copies), yielding a reliability score of 0.868.
Following ethical approval, the first version of the questionnaire was distributed on a small scale across various departments, including internal medicine and surgery, collecting 2–4 questionnaires per department and resulting in 40 responses. After excluding one respondent who disagreed with the study, three who completed the questionnaire in less than 90 s (22), and eleven who answered trap questions incorrectly, 25 valid questionnaires remained. The initial results showed a Cronbach’s α coefficient of −0.244 for the “knowledge” section, necessitating a redesign. The knowledge section was modified to a popular science format, assessing respondents’ understanding of key points rather than selecting correct answers. Additional validity testing yielded a Kaiser-Meyer-Olkin (KMO) value of 0.897, indicating strong validity of the revised instrument.
The revised questionnaire underwent another round of ethical review and was distributed on a second small scale, receiving 51 responses. After excluding five responses with completion times less than 90 s and nineteen with incorrectly answered trap questions, 27 valid questionnaires remained. This version achieved an overall Cronbach’s α coefficient of 0.868, with coefficients of 0.787, 0.864, and 0.817 for the knowledge, attitude, and practice sections, respectively. Finally, the questionnaire was distributed to all nursing staff, resulting in 399 responses. Exclusions included four responses with completion times less than 60 s, one respondent who disagreed with the study, and 151 respondents who answered trap questions incorrectly, leaving 243 valid responses.
The final questionnaire, written in Chinese, included four dimensions with a total of 33 items. These dimensions were: basic information (9 items), knowledge (10 items, including 10 trap questions to identify invalid responses), attitude (7 items), and practice (7 items). During statistical analysis, scores were assigned based on response options. For the knowledge dimension, scores were 2 points for “very familiar,” 1 point for “heard of,” and 0 points for “unclear,” with a total possible score ranging from 0 to 18. For the attitude dimension, responses ranged from “strongly agree” to “strongly disagree,” scoring from 5 to 1, with a total possible score from 7 to 35. For the practice dimension, responses ranged from “always” to “never,” also scoring from 5 to 1, with a total possible score from 7 to 35.
Sample size calculation
The sample size criterion requires that the minimum sample size be 5–20 times the number of items (23). With 33 items in the questionnaire, the minimum sample size was calculated to be 165. Allowing for a 20% non-response rate, the required sample size was adjusted to 207. This study successfully enrolled a total of 399 participants.
Statistical analysis
Data analysis was conducted using SPSS 27.0 and Amos 26.0 (IBM, Armonk, NY, USA). Questionnaire reliability was assessed with Cronbach’s α. Descriptive analysis of demographic information and KAP scores presented continuous data as Mean ± SD and categorical data as frequency (percentage). Differences in knowledge (K), attitude (A), and practice (P) scores across demographic groups were analyzed. Normally distributed continuous variables were compared using the t-test, while non-normally distributed variables were analyzed using the Mann–Whitney U test or Kruskal-Wallis H test. Spearman correlation analysis evaluated the relationships between K, A, and P, with coefficients ranging from −1 to +1. Logistic regression explored the impact of demographic information, knowledge, and attitude on practice, classifying practice scores at 70% (24). Path analysis examined the relationships between baseline information and KAP dimensions. Statistical significance was set at a p-value of less than 0.05.
Result
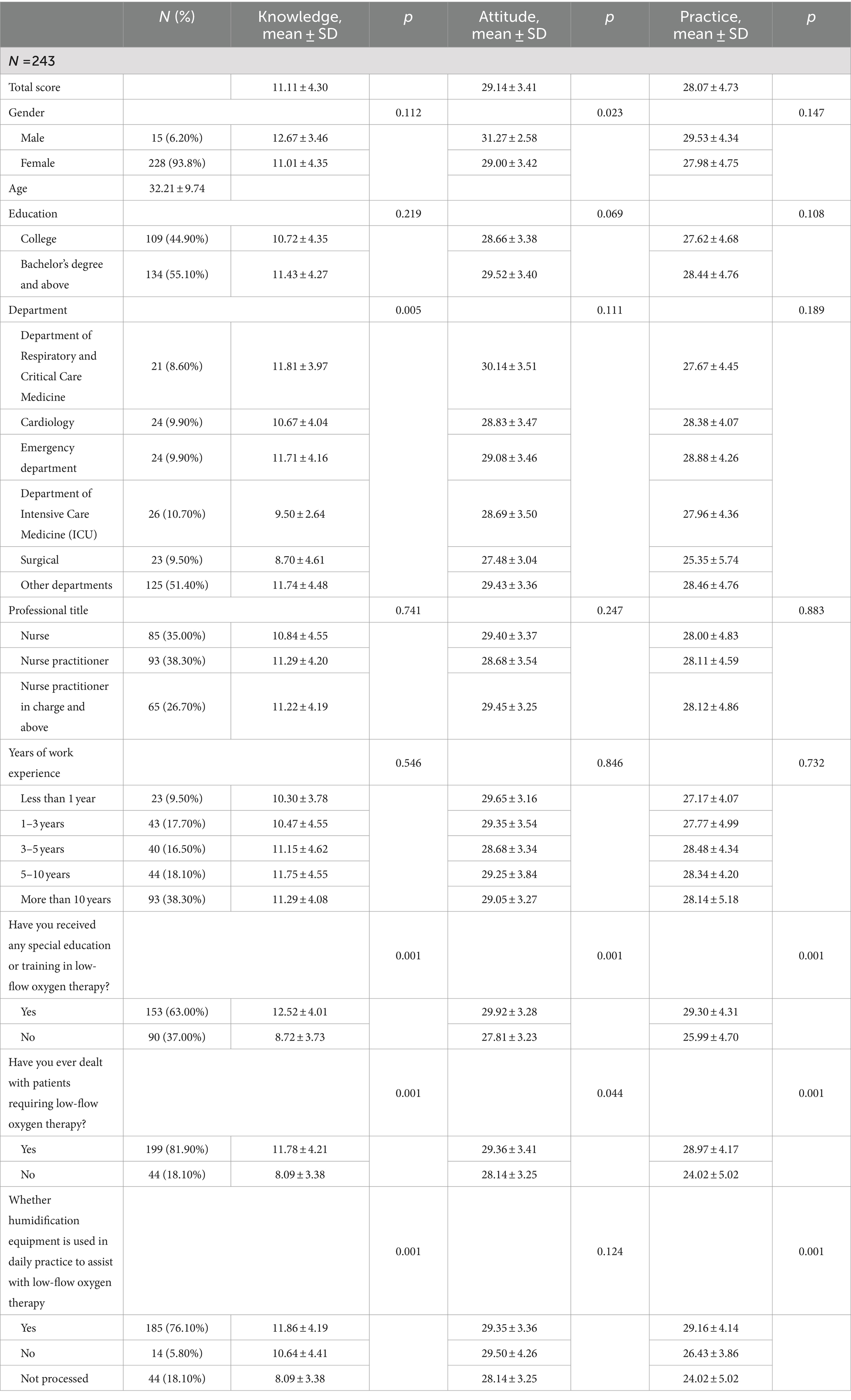
Initially, a total of 399 questionnaires were collected in this study, and data from 4 respondents who completed the questionnaire in less than 60 s, 1 who declined participation, and 151 who incorrectly answered a control question were excluded, resulting in 243 valid responses. The Cronbach’s α coefficient calculated from these 243 responses was 0.905, indicating strong internal consistency. Of the participants, 228 (93.8%) were female, with mean age of 32.21 ± 9.74 years, 134 (55.10%) had a Bachelor’s degree or higher, 93 (38.30%) were nurse practitioners, 93 (38.30%) had been working for more than 10 years, 153 (63.00%) had received specialized education or training in low-flow oxygen therapy, 199 (81.90%) had dealt with patients requiring low-flow oxygen therapy, 185 (76.10%) have used humidification equipment to assist low-flow oxygen therapy in their daily practice. The mean knowledge, attitude, and practice scores were 11.11 ± 4.30, 29.14 ± 3.41, and 28.07 ± 4.73, respectively. The knowledge score varied from participants with different department (p = 0.005), education or training status (p = 0.001), whether dealt with patients requiring low-flow oxygen therapy (p = 0.001), and whether used humidification equipment (p = 0.001). As for the attitude score, there were difference among those with different gender (p = 0.023), education or training status (p = 0.001), and whether dealt with patients requiring low-flow oxygen therapy (p = 0.044). The difference of practice score were found among those with different education or training status (p = 0.001), whether dealt with patients requiring low-flow oxygen therapy (p = 0.001), and whether used humidification equipment (p = 0.001) (as shown in Table 1).
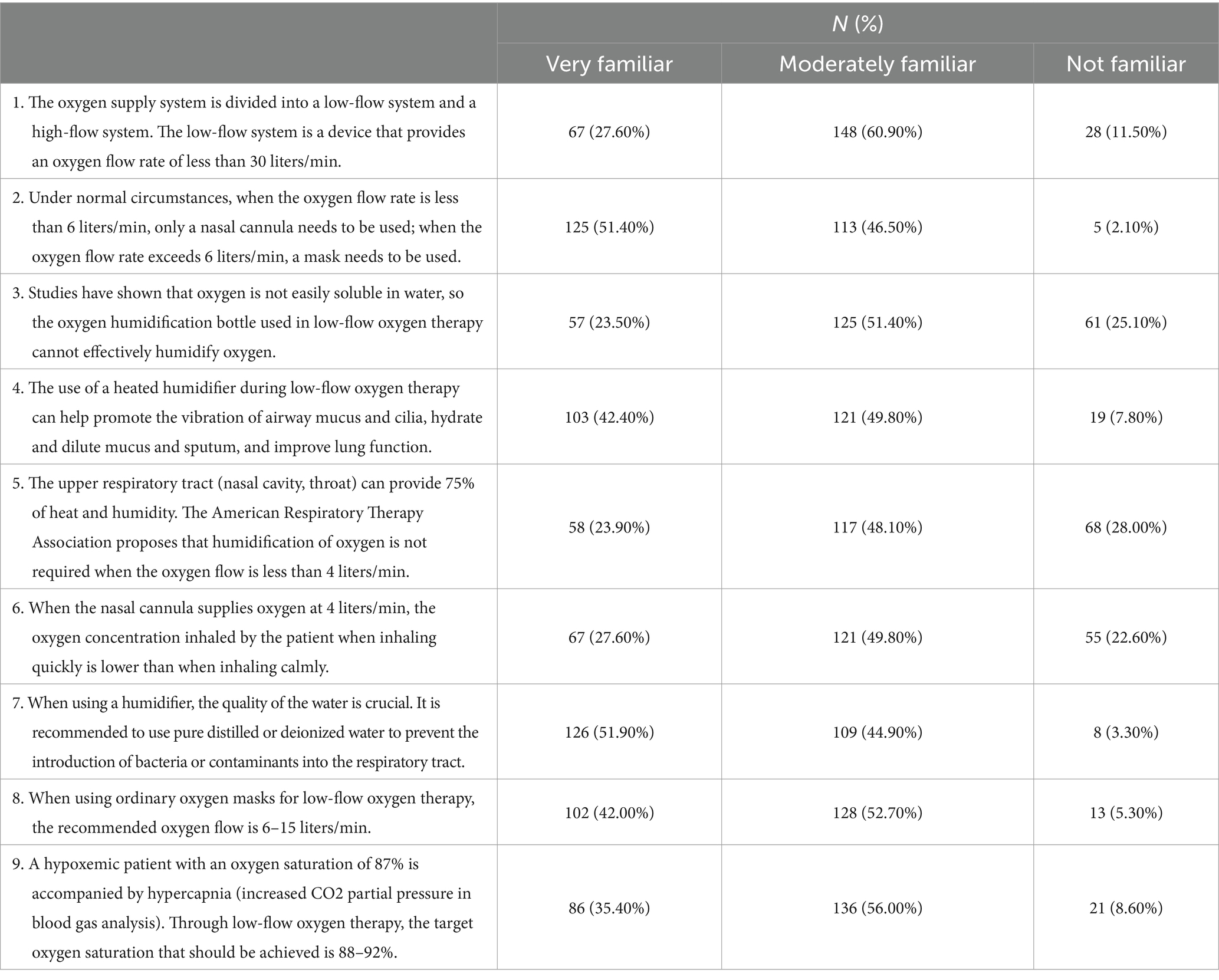
The distribution of knowledge dimension revealed that the question with the highest number of participants choosing the “Very familiar” option was “When using a humidifier, the quality of the water is crucial. It is recommended to use pure distilled or deionized water to prevent the introduction of bacteria or contaminants into the respiratory tract.” (K7), with 51.90%. The question with the highest number of participants choosing the “Moderately familiar” option was “The oxygen supply system is divided into a low-flow system and a high-flow system. The low-flow system is a device that provides an oxygen flow rate of less than 30 liters/min.” (K1), with 60.90%. The question with the highest number of participants choosing the “Not familiar” option was “The upper respiratory tract (nasal cavity, throat) can provide 75% of heat and humidity. The American Respiratory Therapy Association proposes that humidification of oxygen is not required when the oxygen flow is less than 4 liters/min.” (K5), with 28.00% (as shown in Table 2).
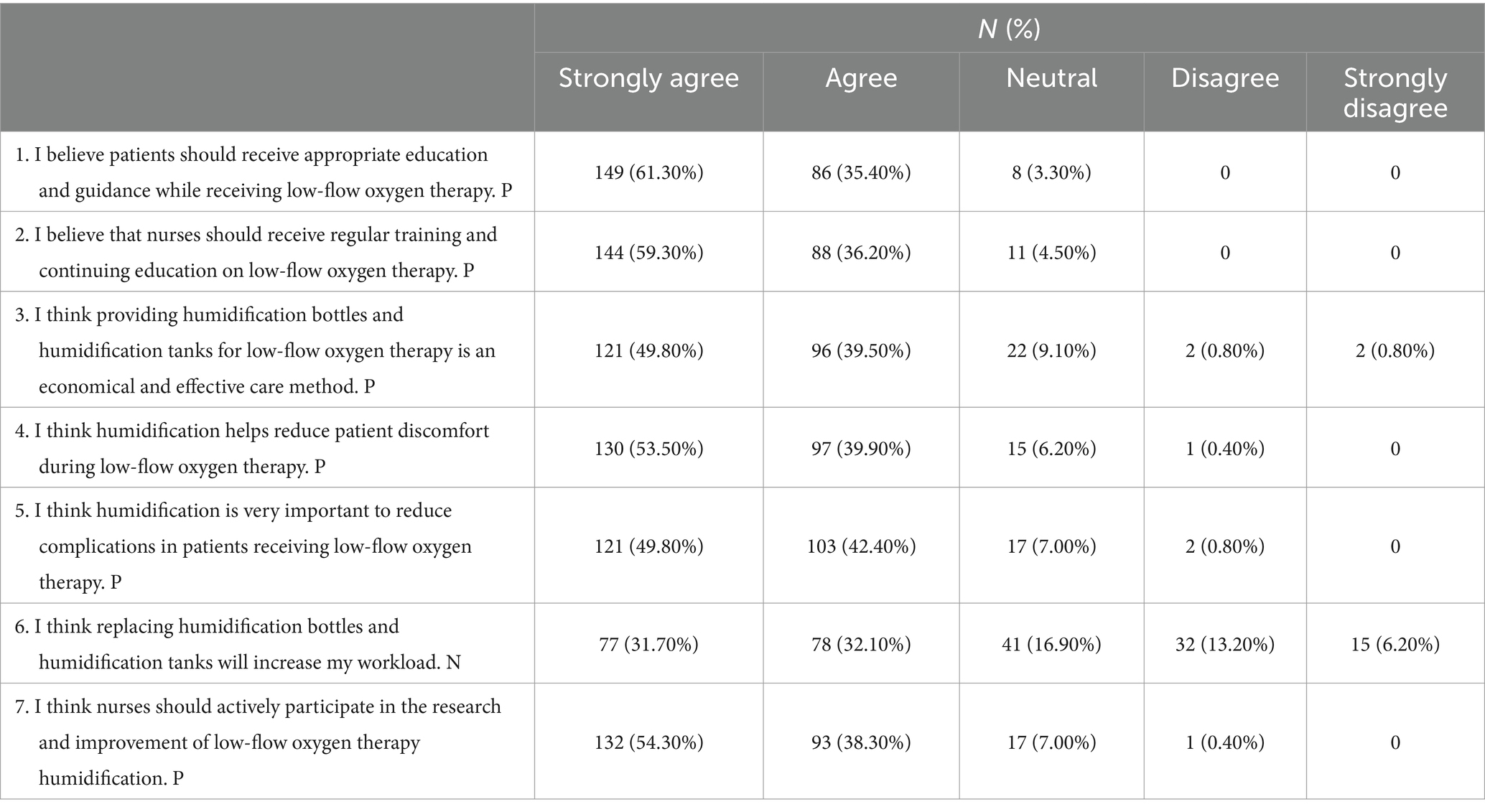
Responses on attitudes showed that patient’s attitudes tended to be positive, with 61.30% strongly agreeing that patients should be properly educated and instructed during low-flow oxygen therapy (A1), 59.30% strongly agreeing that nurses should receive regular training and continuing education on low-flow oxygen therapy (A2), as well as 53.50% strongly agreeing that humidification helps to reduce patients’ discomfort during low-flow oxygen therapy (A4). However, when it comes to whether the replacement of humidifying bottles and canisters would increase their workload (A6), 31.70% strongly agree, 32.10% agree, 16.90% were neutral, and 13.20% were against (as shown in Table 3).
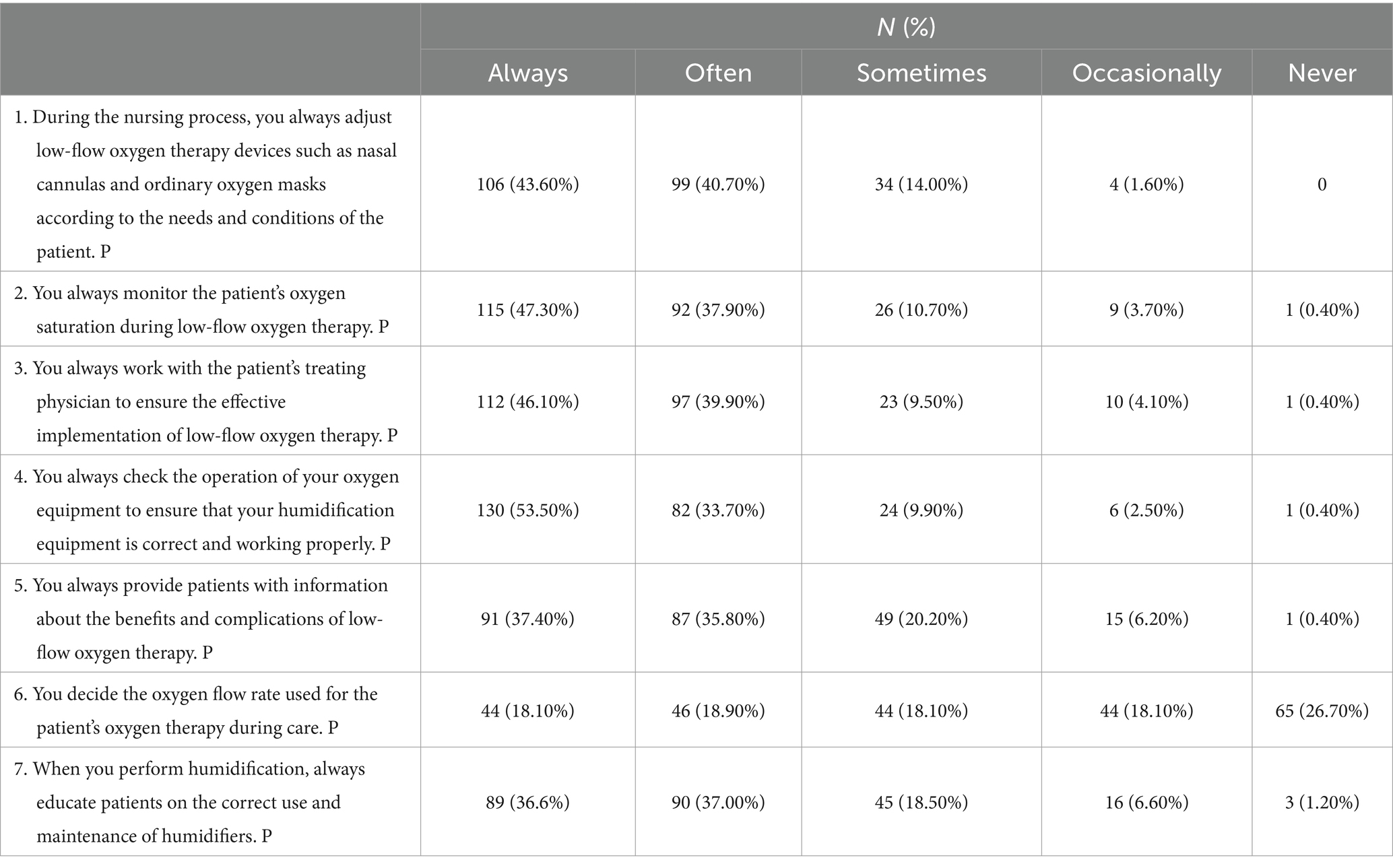
Turning to related practices, 53.50% always checked the operational status of the oxygen equipment (P4), 47.30% always monitored the patient’s oxygen saturation during low-flow oxygen therapy (P2), and 46.10% always collaborated with the patient’s treating physician to ensure that low-flow oxygen therapy was performed effectively (P3). Strikingly, 18.10% occasionally and 26.70% never made their own decisions about the oxygen flow rate to be used for the patient’s oxygen therapy during nursing care (P6) (as shown in Table 4).
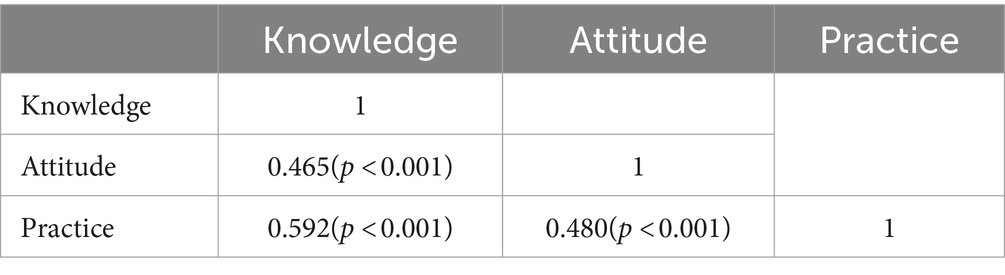
In the correlation analysis, significant positive correlations were found between knowledge and attitude (r = 0.465, p < 0.001), knowledge and practice (r = 0.592, p < 0.001), as well as attitude and practice (r = 0.480, p < 0.001), respectively (as shown in Table 5).
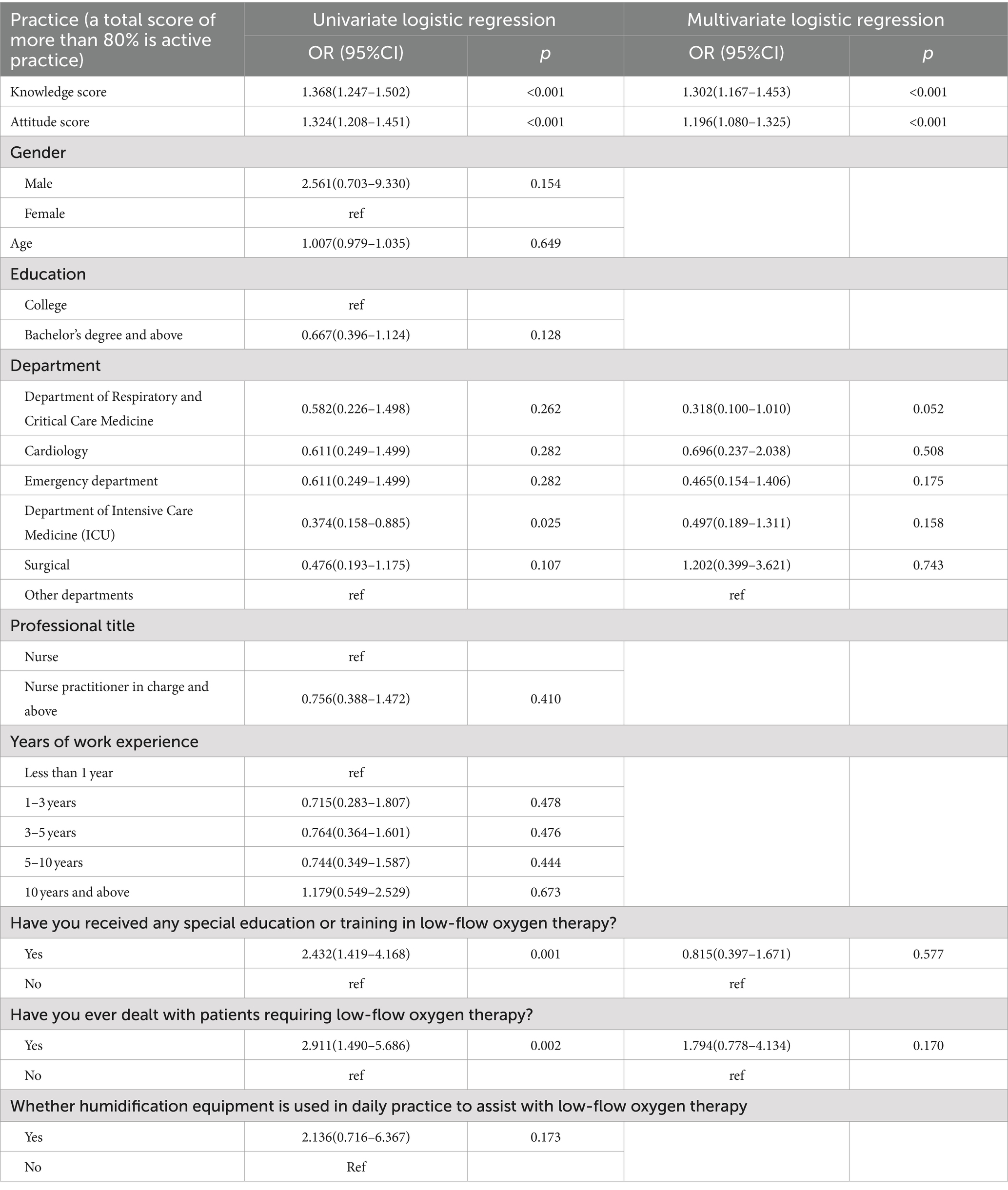
Multivariate logistic regression showed that knowledge score (OR = 1.302, 95% CI: [1.167–1.453], p < 0.001) and attitude score (OR = 1.196, 95% CI: [1.080–1.325], p < 0.001) were independently associated with proactive practice (as shown in Table 6).
The fit indices of the SEM model reached the desired range, indicating good model fit results (as shown in Supplementary Table S1), SEM results show that ‘Trained or not’ (β = 3.210, p < 0.001) and ‘Dealed or not’(β = 2.044, p = 0.002) directly affected knowledge. Meanwhile, knowledge (β = 0.0.379, p < 0.001) and gender (β = −1.642, p = 0.037) directly affected attitude. Further, knowledge (β = 0.395, p < 0.001), attitude (β = 0.340, p < 0.001), and ‘Used or not’ (β = 1.098, p < 0.001) directly affected practice (Figure 1; Supplementary Table S2).
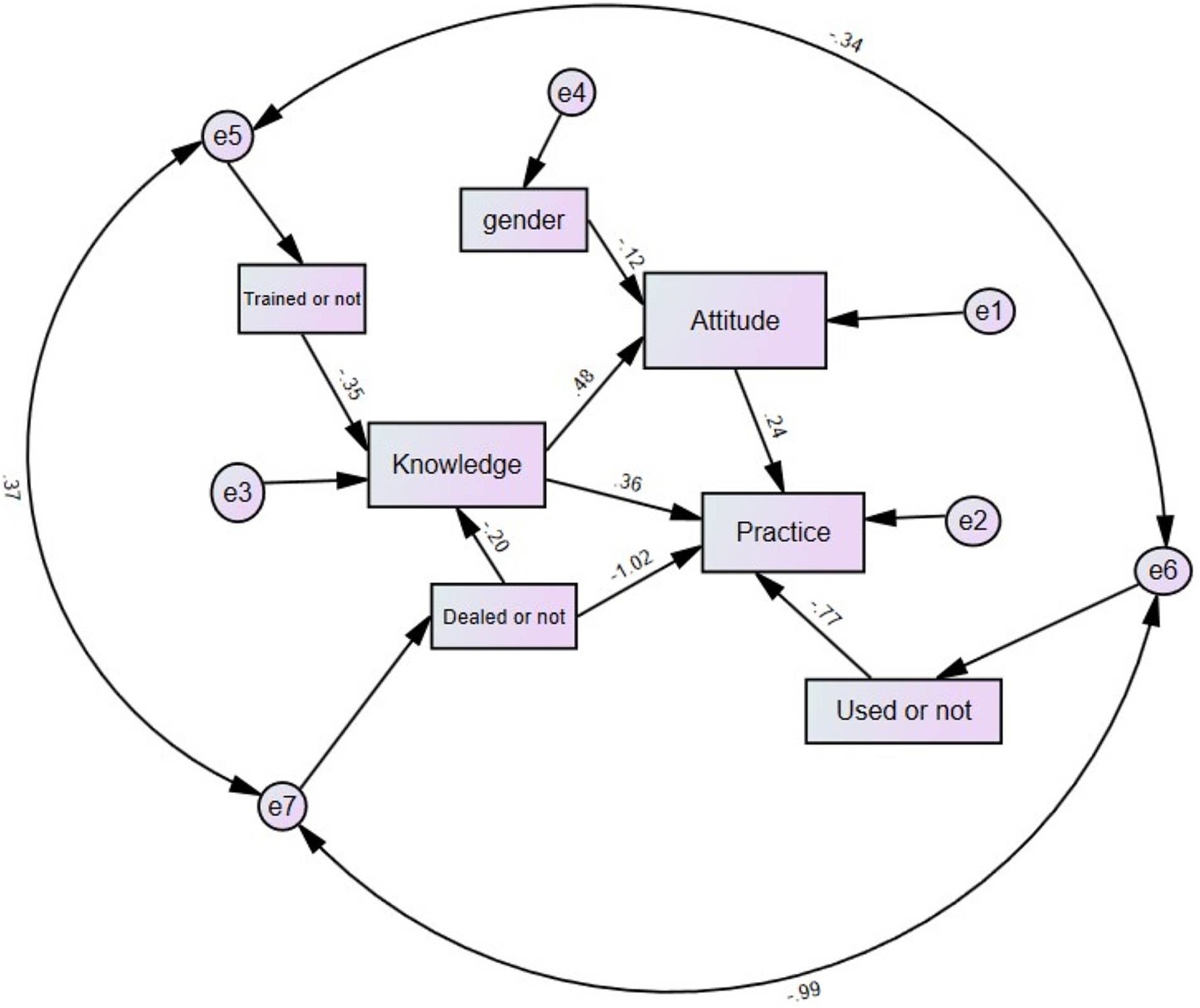
Figure 1. Path analysis results. “Trained or not” refers to the variable in the baseline indicating whether the individual has received specialized education or training on low-flow oxygen therapy. “Dealed or not” refers to the variable in the baseline indicating whether the individual has dealt with patients requiring low-flow oxygen therapy. “Used or not” refers to the variable in the baseline indicating whether the individual has used humidification devices to assist with low-flow oxygen therapy in daily practice. “Gender” refers to the variable in the baseline indicating the individual’s gender. This model illustrates the relationships between gender, training, experience (“dealed or not”), equipment use (“used or not”), and nurses’ knowledge, attitudes, and practices concerning low-flow oxygen therapy. Arrows represent the hypothesized directions of influence. Standardized path coefficients are shown next to each arrow, indicating the strength of these relationships. Error terms (e1 to e7) are associated with the corresponding latent variables, accounting for unexplained variance.
Discussion
Nurses demonstrated inadequate knowledge, positive attitudes, and inactive practices toward low-flow oxygen therapy and humidification. It is essential to implement comprehensive training programs and continuous professional development initiatives to enhance nurses’ knowledge and practices related to low-flow oxygen therapy.
This study highlights that nurses demonstrated inadequate knowledge, positive attitudes, and inactive practices toward low-flow oxygen therapy and humidification. Significant differences in knowledge, attitudes, and practices were observed based on gender, department, special training, clinical experience, and the use of humidification equipment. For instance, gender differences were significant in attitudes, with male nurses scoring higher than female nurses. This finding could be influenced by varying educational backgrounds or different experiences in clinical settings between genders (25, 26). However, no significant gender differences were observed in knowledge and practice scores. Besides, departmental differences significantly influenced knowledge scores. Nurses from the Department of Respiratory and Critical Care Medicine scored the highest, likely due to their frequent exposure to and training in oxygen therapy. Conversely, nurses from the Surgical department had the lowest scores, which might reflect less requirement on oxygen therapy in their daily responsibilities.
Moreover, special education or training in low-flow oxygen therapy significantly improved scores across all KAP categories. Nurses who received training scored higher in knowledge, attitudes, and practices. This underscores the importance of targeted educational interventions, which have been shown to enhance healthcare providers’ competencies in various clinical areas (27). Experience with patients requiring low-flow oxygen therapy was a critical factor in improving nurses’ KAP scores, highlighting the importance of hands-on experience. Nurses with this clinical exposure demonstrated greater knowledge, more positive attitudes, and better practices compared to those with purely theoretical training. Practical experience not only reinforces theoretical concepts but also equips nurses with essential skills for managing respiratory conditions, such as identifying early signs of hypoxia, adjusting oxygen flow rates appropriately, and monitoring patient outcomes effectively. By bridging the gap between theory and practice, this experience enhances nurses’ ability to manage complex cases and adapt swiftly to changing patient needs, ultimately contributing to better patient care. The experiential learning theory posits that direct patient care experiences are essential for effective learning (28, 29). The use of humidification equipment in daily practice was associated with higher knowledge and practice scores, indicating that regular use of relevant tools can reinforce learning and application. This practical engagement likely enhances familiarity and confidence in using the equipment, leading to better clinical practices.
Multivariate logistic regression and SEM results highlighted the independent and direct effects of knowledge and attitudes on proactive practices. Knowledge scores were strongly associated with better practices, corroborating findings from other studies that link higher knowledge levels to improved clinical practices (30). Attitudes also significantly influenced practices, suggesting that positive attitudes toward low-flow oxygen therapy can drive better implementation. The correlation analyses and SEM results further elucidated the relationships between KAP dimensions. Significant positive correlations between knowledge and attitudes, knowledge and practices, and attitudes and practices suggest that these elements are interdependent. Enhancing one aspect, such as knowledge through training, is likely to positively impact attitudes and practices as well (31).
The knowledge dimension revealed a varied familiarity among participants regarding low-flow oxygen therapy. While many respondents showed moderate to high familiarity with concepts such as the oxygen supply system and appropriate oxygen flow rates for nasal cannulas and masks, there were notable gaps in understanding specific details. For instance, a significant portion was not well-versed in the limitations of oxygen humidification bottles, with nearly a quarter being unaware that these bottles cannot effectively humidify oxygen. Moreover, there are different understandings between Eastern and Western countries regarding the necessity of humidification during oxygen therapy. To address these gaps, targeted educational programs and related studies could be implemented. For example, integrating detailed workshops and hands-on training sessions into existing professional development curricula could improve understanding. Leveraging platforms for microlearning modules and interactive quizzes could further reinforce knowledge in an engaging manner (32, 33).
The attitude dimension showed generally positive sentiments toward the importance of education, training, and the use of humidification in low-flow oxygen therapy. However, concerns about workload increase were evident, with 63.8% of nurses agreeing or strongly agreeing that replacing humidification bottles increases workload. This perception of increased workload is consistent with findings from other nursing studies, where the adoption of new equipment or processes was associated with apprehensions about time management and additional tasks (34). To mitigate these concerns, strategies such as streamlining the humidification equipment replacement process and providing adequate staffing could be considered. Additionally, recognizing and rewarding nurses’ efforts in maintaining humidification practices through institutional acknowledgment or incentives could further enhance positive attitudes. Engaging nurses in feedback and decision-making processes about equipment use via online forums or surveys could also improve their investment in these practices (35, 36).
The practice dimension highlighted a strong adherence to best practices in monitoring and adjusting low-flow oxygen therapy, though some areas still require improvement. For example, a notable minority did not consistently educate patients on the correct use and maintenance of humidifiers, nor did they always decide the oxygen flow rate during care. This tendency to defer decision-making on oxygen flow rates may reflect hierarchical dynamics in clinical settings, a pattern seen in other studies where nurses reported limited autonomy in adjusting treatment parameters (37). To address these issues, comprehensive training sessions focusing on the importance of patient education and involvement in care decisions are recommended. Utilizing digital tools to share best practices and practical tips among healthcare professionals could standardize and improve practice. Additionally, implementing regular audits and feedback sessions can ensure adherence to protocols and highlight areas for further improvement (38, 39). This suggests that while nurses are aware of the importance of patient education, barriers such as time constraints or perceived complexity may limit its implementation, as seen in similar clinical studies (40).
It is essential to implement comprehensive training programs and continuous professional development initiatives to enhance nurses’ knowledge and practices related to low-flow oxygen therapy. To address knowledge and practice gaps, implementing simulation-based training and case-based learning could be effective approaches. Simulation-based training, which provides realistic patient care scenarios, has demonstrated significant improvements in clinical skills and decision-making among healthcare providers in intensive care and emergency departments (41). Similarly, case-based learning, involving real-life scenarios and patient cases, has proven effective in enhancing nurses’ critical thinking and practical skills in chronic disease management settings (42). Additionally, e-learning modules, which include interactive quizzes and step-by-step procedures, have been successfully used to improve healthcare workers’ knowledge and adherence to treatment protocols in infectious disease management (43).
This study has some limitations: the use of self-reported questionnaires may introduce response bias, the cross-sectional design limits the ability to infer causality, and the sample was drawn from a single hospital, which may affect the generalizability of the findings. Additionally, the exclusion of a substantial number of participants due to the strict exclusion criteria—trap questions or completion times under 60 s—could introduce selection bias. Moreover, the limited number of male nurses in the current study may influence the representativeness of gender differences in the results. However, it is worth noting that more male nurses have recently joined the nursing workforce, and we plan to conduct a multi-center study to include a greater number of male nurses in the future. Regarding the reviewer’s suggestion to assess the impact of varying levels of nurses’ knowledge and understanding on patients’ clinical outcomes, we acknowledge that this would require a longitudinal study design. The current cross-sectional study primarily aims to describe nurses’ knowledge, attitudes, and practices related to low-flow oxygen therapy. We intend to develop an interventional study design in the future, potentially incorporating longer observation periods to evaluate the effects of training interventions on both nurse competencies and patient outcomes. In addition, while this study recommends training interventions to address gaps in knowledge and practice, the specific type of intervention training is still under preparation. We are considering the use of quasi-experiment designs for future intervention research, which could help enhance training effectiveness and inform more detailed recommendations. Despite these limitations, this study provides valuable insights into the current state of nurses’ knowledge, attitudes, and practices regarding low-flow oxygen therapy and highlights the need for targeted educational interventions.
In conclusion, nurses demonstrated inadequate knowledge, positive attitudes, and inactive practices toward low-flow oxygen therapy and humidification. To improve the clinical application of low-flow oxygen therapy, it is recommended that comprehensive training programs and ongoing professional development be implemented, emphasizing both theoretical knowledge and practical skills. Enhancing these aspects can ensure more effective and consistent use of low-flow oxygen therapy, ultimately improving patient care and outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Shanghai Xuhui Central Hospital Ethics Committee [(2023) Court Review No. (046)]. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. HaL: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. JZ: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. HuL: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. LS: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. HZ: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. QG: Conceptualization, Writing – review & editing. RY: Conceptualization, Formal analysis, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funded project for the construction of peak disciplines in the Xuhui District health system [SHXHZDXK202312].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1460079/full#supplementary-material
References
1. Petersson, J, and Glenny, RW. Gas exchange and ventilation-perfusion relationships in the lung. Eur Respir J. (2014) 44:1023–41. doi: 10.1183/09031936.00037014
2. Kamran, A, Chia, E, and Tobin, C. Acute oxygen therapy: an audit of prescribing and delivery practices in a tertiary hospital in Perth, Western Australia. Intern Med J. (2018) 48:151–7. doi: 10.1111/imj.13612
3. Jha, M, and Gaur, N. Life cycle of medical oxygen from production to consumption. J Family Med Prim Care. (2022) 11:1231–6. doi: 10.4103/jfmpc.jfmpc_956_21
4. Berman, A, Snyder, S, and Frandsen, G. Study guide for Kozier & Erb's fundamentals of nursing: Concepts, process, and practice,[by] Berman. Snyder: Pearson (2016).
5. Ersoy, EO, and Topeli, A. Oxygen therapy systems in respiratory failure. Journal of Critical and Intensive Care. (2016) 7:99–105. doi: 10.5152/dcbybd.2017.1329
6. Chikata, Y, Onodera, M, Oto, J, and Nishimura, M. FIO2 in an adult model simulating high-flow nasal cannula therapy. Respir Care. (2017) 62:193–8. doi: 10.4187/respcare.04963
7. Groves, N, and Tobin, A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. (2007) 20:126–31. doi: 10.1016/j.aucc.2007.08.001
8. Nishimura, M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care. (2015) 3:15. doi: 10.1186/s40560-015-0084-5
9. Wen, Z, Wang, W, Zhang, H, Wu, C, Ding, J, and Shen, M. Is humidified better than non-humidified low-flow oxygen therapy? A systematic review and meta-analysis. J Adv Nurs. (2017) 73:2522–33. doi: 10.1111/jan.13323
10. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about Cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:21501319211063051. doi: 10.1177/21501319211063051
11. Li, L, Zhang, J, Qiao, Q, Wu, L, and Chen, L. Development, reliability, and validity of the"knowledge-attitude-practice" questionnaire of foreigners on traditional Chinese medicine treatment. Evid Based Complement Alternat Med. (2020) 2020:8527320. doi: 10.1155/2020/8527320
12. Nippers, I, and Sutton, A. Oxygen therapy: professional compliance with national guidelines. Br J Nurs. (2014) 23:382–6. doi: 10.12968/bjon.2014.23.7.382
13. Aloushan, AF, Almoaiqel, FA, Alghamdi, RN, Alnahari, FI, Aldosari, AF, Masud, N, et al. Assessment of knowledge, attitude and practice regarding oxygen therapy at emergency departments in Riyadh in 2017: a cross-sectional study. World J Emerg Med. (2019) 10:88–93. doi: 10.5847/wjem.j.1920-8642.2019.02.004
14. Nabwire, J, Namasopo, S, and Hawkes, M. Oxygen availability and nursing capacity for oxygen therapy in Ugandan Paediatric wards. J Trop Pediatr. (2018) 64:97–103. doi: 10.1093/tropej/fmx033
15. Zeleke, S, and Kefale, D. Nurses' supplemental oxygen therapy knowledge and practice in Debre Tabor general hospital: a cross-sectional study. Open Access Emerg Med. (2021) 13:51–6. doi: 10.2147/OAEM.S299139
16. AARC. AARC clinical practice guideline. Oxygen therapy in the home or alternate site health care facility--2007 revision & update. Respir Care. (2007) 52:1063–8.
17. Campbell, EJ, Baker, MD, and Crites-Silver, P. Subjective effects of humidification of oxygen for delivery by nasal cannula. A prospective study. Chest. (1988) 93:289–93.
18. Hardavella, G, Karampinis, I, Frille, A, Sreter, K, and Rousalova, I. Oxygen devices and delivery systems. Breathe (Sheff). (2019) 15:e108–16. doi: 10.1183/20734735.0204-2019
19. Napolitano, N, Berlinski, A, Walsh, BK, Ginier, E, and Strickland, SL. AARC clinical practice guideline: Management of Pediatric Patients with Oxygen in the acute care setting. Respir Care. (2021) 66:1214–23. doi: 10.4187/respcare.09006
20. O'Driscoll, BR, Howard, LS, and Davison, AG. BTS guideline for emergency oxygen use in adult patients. Thorax. (2008) 63:vi68. doi: 10.1136/thx.2008.102947
21. Thirunavukkarasu, A, Al-Hazmi, AH, Dar, UF, Alruwaili, AM, Alsharari, SD, Alazmi, FA, et al. Knowledge, attitude and practice towards bio-medical waste management among healthcare workers: a northern Saudi study. PeerJ. (2022) 10:e13773. doi: 10.7717/peerj.13773
22. Luo, Z, Guo, W, Zhou, H, and Chen, Z. Knowledge, attitude, and practice toward lung cancer risk among offspring of lung cancer patients: a cross-sectional study. Sci Rep. (2024) 14:18003. doi: 10.1038/s41598-024-69142-8
23. Naqvi, AA, Hassali, MA, Rizvi, M, Zehra, A, Nisa, ZU, Islam, MA, et al. Validation of the general medication adherence scale in Pakistani patients with rheumatoid arthritis. Front Pharmacol. (2020) 11:1039. doi: 10.3389/fphar.2020.01039
24. Lee, F, and Suryohusodo, AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: a cross-sectional study. Front Public Health. (2022) 10:957630. doi: 10.3389/fpubh.2022.957630
25. Horne, M, Youell, J, Brown, LJE, Simpson, P, Dickinson, T, and Brown-Wilson, C. A scoping review of education and training resources supporting care home staff in facilitating residents' sexuality, intimacy and relational needs. Age Ageing. (2021) 50:758–71. doi: 10.1093/ageing/afab022
26. Sheffield, V, Hartley, S, Stansfield, RB, Mack, M, Blackburn, S, Vaughn, VM, et al. Gendered expectations: the impact of gender, evaluation language, and clinical setting on resident trainee assessment of faculty performance. J Gen Intern Med. (2022) 37:714–22. doi: 10.1007/s11606-021-07093-w
27. Day, LB, Saunders, S, Steinberg, L, Ginsburg, S, and Soong, C. "get the DNR": residents' perceptions of goals of care conversations before and after an e-learning module. Can Med Educ J. (2022) 13:17–28. doi: 10.36834/cmej.71956
28. Hardie, P, Darley, A, Carroll, L, Redmond, C, Campbell, A, and Jarvis, S. Nursing & Midwifery students' experience of immersive virtual reality storytelling: an evaluative study. BMC Nurs. (2020) 19:78. doi: 10.1186/s12912-020-00471-5
29. Meum, TT, Slettebø, Å, and Fossum, M. Improving the use of simulation in nursing education: protocol for a realist review. JMIR Res Protoc. (2020) 9:e16363. doi: 10.2196/16363
30. Park, H, and Cho, H. Effects of a self-directed clinical practicum on self-confidence and satisfaction with clinical practicum among south Korean nursing students: a mixed-methods study. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19095231
31. Liao, L, Feng, H, Jiao, J, Zhao, Y, and Ning, H. Nursing assistants' knowledge, attitudes and training needs regarding urinary incontinence in nursing homes: a mixed-methods study. BMC Geriatr. (2023) 23:39. doi: 10.1186/s12877-023-03762-z
32. De Sousa, I, Wytenbroek, L, Bailey, E, and Campbell, SH. "they bring the topic [of social justice] but stop there": nursing students' perceptions of teaching practices that develop awareness and engagement with social justice. Nurse Educ Today. (2024) 139:106241. doi: 10.1016/j.nedt.2024.106241
33. Zhang, C, Xu, C, Wang, R, Han, X, Yang, G, and Liu, Y. The learning experiences and career development expectations of Chinese nursing master's degree students: a qualitative investigation. Nurse Educ Pract. (2024) 77:103996. doi: 10.1016/j.nepr.2024.103996
34. Xing, H, Zhu, S, Liu, S, Xia, M, Jing, M, Dong, G, et al. Knowledge, attitudes and practices of ICU nurses regarding subsyndromal delirium among 20 hospitals in China: a descriptive cross-sectional survey. BMJ Open. (2022) 12:e063821. doi: 10.1136/bmjopen-2022-063821
35. Chung, SJ, Lee, H, and Jang, SJ. Factors affecting environmental sustainability attitudes among nurses - focusing on climate change cognition and behaviours: a cross-sectional study. J Adv Nurs. (2024) 1–12. doi: 10.1111/jan.16205
36. Miao, C, Liu, C, Zhou, Y, Zou, X, Song, L, Chung, JWY, et al. Nurses' perspectives on professional self-concept and its influencing factors: a qualitative study. BMC Nurs. (2024) 23:237. doi: 10.1186/s12912-024-01834-y
37. Asl, RG, Taghinejad, R, Parizad, N, and Jasemi, M. The relationship between professional autonomy and job stress among intensive care unit nurses: a descriptive correlational study. Iran J Nurs Midwifery Res. (2022) 27:119–24. doi: 10.4103/ijnmr.ijnmr_375_20
38. Martínez-Arce, A, Rodríguez-Almagro, J, Vélez-Vélez, E, Rodríguez-Gómez, P, Alconero-Camarero, AR, and Hernández-Martínez, A. The impact of incorporating a simulation program into the undergraduate nursing curricula: a cross-sectional descriptive study. Nurse Educ Pract. (2024) 77:103972. doi: 10.1016/j.nepr.2024.103972
39. Xu, HG, Johnston, ANB, and Ray-Barruel, G. Fast-track training in emergency department during the COVID-19 pandemic: evaluation of a hybrid education model. Adv Emerg Nurs J. (2024) 46:169–81. doi: 10.1097/TME.0000000000000516
40. Klankaew, S, Temthup, S, Nilmanat, K, and Fitch, MI. The effect of a nurse-led family involvement program on anxiety and depression in patients with advanced-stage hepatocellular carcinoma. Healthcare. (2023) 11:1–13. doi: 10.3390/healthcare11040460
41. Fouilloux, V, Gran, C, Guervilly, C, Breaud, J, El Louali, F, and Rostini, P. Impact of education and training course for ECMO patients based on high-fidelity simulation: a pilot study dedicated to ICU nurses. Perfusion. (2019) 34:29–34. doi: 10.1177/0267659118789824
42. Chao, CT, Wu, MY, Hung, KY, Wu, MS, and Liang, JC. Interprofessional differences in multidimensional self-efficacy associated with professional performance in nephrology during case-based learning. Kidney Int Rep. (2024) 9:877–87. doi: 10.1016/j.ekir.2024.01.018
Keywords: knowledge, attitude, practice, low-flow oxygen therapy, humidification, nurses
Citation: Tang N, Li H, Zhang J, Ling H, Shi L, Zhang H, Guo Q and Yu R (2024) Nurses’ knowledge, attitude, and practice of low-flow oxygen therapy and humidification. Front. Med. 11:1460079. doi: 10.3389/fmed.2024.1460079
Edited by:
Cheryl E. Hickmann, Haute École provinciale de Hainaut Condorcet, BelgiumReviewed by:
Frédéric Duprez, EpiCURA, BelgiumYogi Prawira, RSUPN Dr. Cipto Mangunkusumo, Indonesia
Copyright © 2024 Tang, Li, Zhang, Ling, Shi, Zhang, Guo and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qi Guo, MTM5MTYzMjE1NjdAMTM5LmNvbQ==; Ronghuan Yu, cHVid29ya3JjQHFxLmNvbQ==
 Naiwang Tang1
Naiwang Tang1 Ronghuan Yu
Ronghuan Yu