- 1Department of Gynecology, Endocrinology, and Gynecologic Oncology, Pomeranian Medical University, Szczecin, Poland
- 2Institute of Science and Innovation in Mechanical Engineering and Industrial Engineering, Faculty of Engineering, University of Porto, Porto, Portugal
- 3Hôpitaux Universitaires de Genève (HUG), Geneva, Switzerland
Introduction and hypothesis: We aimed to analyze the quality of sexual life of patients with apical vaginal wall prolapse who had undergone laparoscopic lateral suspension (LLS) and laparoscopic sacrocolpopexy (LSC).
Methods: We performed a secondary analysis of sexual outcomes of a previous randomized control trial comparing LLS and LSC in 89 women with symptomatic POP stage ≥ II. We evaluated sexually active (SA) and non-sexually active women (NSA) using the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire-IUGA-Revised (PISQ-IR). Women were reviewed over a period of 1 year post-surgery.
Results: Analysis of the entire PISQ-IR questionnaire indicates that surgical treatment of POP resulted in an improvement of the quality of sexual life in 21 (80.76%) in the group of sexually active women after LSC and in 20 (83.33%) in the group of SA patients after LLS. In both groups of patients, dyspareunia was not observed.
Conclusion: In conclusion, the quality of sexual life in SA group of patients improved significantly after both surgical procedures. The quality of sexual life of surveyed women significantly improved after curing POP symptoms.
1 Introduction
Pelvic Organ Prolapse (POP) primarily affects women of menopausal age and has a detrimental impact on their quality of life. In addition to causing unpleasant symptoms, POP often leads to a deterioration of sexual function (1, 2).
The number of women undergoing surgery for POP increases each year (3, 4). However, studies show that sexual function differs after various surgical procedures (5–7).
Apical suspension procedures can be broadly categorized into transvaginal and abdominal approaches. Abdominal procedures can be performed via laparotomy, conventional laparoscopy, or robotic-assisted laparoscopy. Transvaginal apical suspension methods include native tissue repairs and mesh-based repairs.
1.1 Sacrocolpopexy
Traditionally, sacrocolpopexy has been performed through a laparotomy, known as abdominal sacrocolpopexy (ASCP). However, over the past decade, minimally invasive techniques, including laparoscopic (LSCP) and robotic sacrocolpopexy (RSCP), have become increasingly favored due to their advantages such as shorter recovery times, reduced postoperative pain, and smaller incisions compared to the open abdominal method. Laparoscopic sacrocolpopexy (LSCP) is now regarded as the gold standard for treating apical prolapse, although it requires more advanced surgical expertise. Operating near the sacral region carries potential risks, including neurological, ureteral, or vascular injury, and postoperative bowel issues are frequently reported. Moreover, periostitis, although rare, can occur due to the weak anterior longitudinal ligament at the site of sacral attachment, increasing the risk of periosteal penetration during surgery.
Compared to vaginal procedures, ASCP is associated with higher morbidity, particularly in terms of longer operative times (notably for laparoscopic or robotic approaches), extended hospital stays, delayed return to normal activities, and increased costs. Additionally, sacrocolpopexy may involve mesh-related complications, such as erosion, infection, or pain, although these complications are rare with the use of modern surgical techniques (8–15).
Laparoscopic lateral suspension (LLS) Laparoscopic lateral suspension with mesh has emerged as a promising technique, offering both excellent anatomical and functional outcomes. The uniqueness of LLS lies in the placement of the T-shaped mesh, where the lateral arms are passed through a subperitoneal tunnel along the lateral abdominal wall, exiting just above the iliac crest. This approach minimizes the risk of injury to major blood vessels, nerves, or the bowel and ensures symmetrical, tension-free suspension along the vaginal axis. LLS is primarily indicated for the treatment of anterior pelvic organ prolapse and apical descent. It is particularly useful in cases where access to the sacral promontory is challenging, such as in the presence of dense adhesions, sigmoid megacolon, or when the left common iliac vein is positioned low and partially obstructs the promontory.
Like other mesh-based procedures, LLS carries risks of mesh-related complications, including erosion, infection, and pain. Although the mesh is placed at a distance from the vaginal mucosa, these complications can still occur. While LLS has demonstrated favorable short-to medium-term outcomes, long-term data remain limited when compared to procedures such as sacrocolpopexy. Several studies and reviews have noted a higher risk of recurrence in the anterior compartment after LLS compared to sacrocolpopexy, underscoring the need for further research into its long-term efficacy (16–19).
1.2 Pectopexy
Pectopexy, introduced by Banerjee and Noé in 2010 (20), is a viable alternative to sacrocolpopexy for pelvic organ prolapse repair. Like sacrocolpopexy, pectopexy employs a macroporous, monofilament mesh; however, instead of attaching to the presacral ligament, the mesh is secured to the right and left pectineal ligaments, supporting the anterior and/or posterior vaginal walls. Pectopexy offers several advantages, including a shorter operative time and a lower rate of complications compared to laparoscopic sacrocolpopexy. Additionally, it is particularly beneficial for obese patients, providing a safer and more effective option than traditional sacrocolpopexy in this population. Despite its advantages, pectopexy also has certain drawbacks. One of the primary concerns is the lack of long-term data compared to sacrocolpopexy, limiting our understanding of its durability and effectiveness over time. Additionally, pectopexy may have a higher risk of anterior compartment prolapse recurrence due to its lateral mesh fixation, which may not provide as robust support for the vaginal apex as sacrocolpopexy. There is also the potential for complications such as mesh erosion, infection, and pain, which are risks associated with any mesh-based procedure. Finally, while pectopexy avoids the risks related to sacral nerve and vascular injury seen in sacrocolpopexy, it can still pose a risk to nearby structures, including the obturator nerve and vessels, during fixation to the pectineal ligaments (20–24).
1.3 Sacrospinous ligament fixation
Sacrospinous ligament fixation (SSLF) is a widely recognized and frequently reported transvaginal procedure for addressing apical prolapses using native tissue techniques. This minimally invasive approach offers several advantages, including reduced recovery times, making it an appealing option for women who wish to avoid abdominal surgery or who may not be suitable candidates for sacrocolpopexy. Despite its benefits, SSLF may lead to complications such as vaginal asymmetry, which may impact sexual function. Additionally, during the procedure, there is a risk of injury to critical neurovascular structures located in proximity to the surgical site. When compared to sacrocolpopexy, the recurrence of prolapse is higher (25, 26).
1.4 Ipsilateral uterosacral ligament fixation
Ipsilateral uterosacral ligament fixation (USLS) is a surgical technique that suspends the vaginal apex to the proximal remnants of the uterosacral ligaments via an intraperitoneal approach. This method effectively restores the vaginal axis, thereby mitigating the higher incidence of retroflexion commonly seen with sacrospinous ligament fixation (SSLF). However, patients with more severe prolapse or significant pelvic floor laxity have been noted to experience a higher recurrence rate following this procedure. Additionally, USLS carries the risk of potential injury to adjacent structures, including the ureters and nearby nerves, which necessitates careful surgical technique and consideration during the operation (27–30).
1.5 Transvaginal mesh procedures
Transvaginal mesh procedures involve the insertion of synthetic mesh through the vaginal wall to provide robust and durable support for prolapsed organs. This surgical approach is particularly beneficial in cases where prolapse affects not only the vaginal apex but also the anterior and/or posterior compartments. However, these procedures carry a significant risk of complications, including mesh erosion, infection, pain, and dyspareunia. The use of mesh in vaginal surgeries has also led to numerous legal challenges, prompting restrictions in some countries due to safety concerns. As a result, careful consideration of the risks and benefits is essential when evaluating the use of transvaginal mesh for pelvic organ prolapse repair (31–33).
1.6 McCall culdoplasty
McCall culdoplasty was not initially designed specifically for the treatment of vaginal vault prolapse, it has been shown to effectively prevent recurrence after hysterectomy. Among the various techniques for suspending the vaginal apex during vaginal hysterectomy, McCall culdoplasty is the most commonly performed procedure. This technique involves obliterating the posterior cul-de-sac and plicating the uterosacral ligaments across the midline.
A large study conducted at the Mayo Clinic demonstrated a high success rate in preventing prolapse recurrence among patients who underwent McCall culdoplasty, with the majority expressing satisfaction with their outcomes. Therefore, McCall culdoplasty appears to be an effective method for preventing vaginal vault prolapse following primary repair after hysterectomy, with minimal associated morbidity (34–37).
Obliterative surgery, including total colpocleisis and LeFort partial colpocleisis, is another option for managing apical pelvic organ prolapse (POP). However, these procedures are typically reserved for elderly women, those with significant medical comorbidities, or individuals who are no longer sexually active (38).
Several studies suggest that laparoscopic surgery for POP may confer significant benefits comparing to the vaginal approach (39–44). Unfortunately, there is a lack of consensus regarding the optimal way of surgery to preserve women’s sexual function (45).
Laparoscopic sacrocolpopexy remains the gold standard in the treatment of apical prolapse and it is recommended in sexually active patients (14, 42). Laparoscopic lateral suspension turned out to be an alternative procedure and has proved good anatomical as well as functional outcomes (46–54). However, there are only a few studies that describe the impact of laparoscopic lateral suspension on sexual function using validated questionnaires (55, 56).
Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) is condition—specific measure of sexual function in women with PFD (Pelvic Floor Disorders) (57). Despite the growing demand for validated measures of sexual dysfunction, the PISQ-IR has not been widely used in patients who have undergone laparoscopic urogynaecological procedures. This underutilization highlights a significant gap in our understanding and management of sexual dysfunction in this population.
The aim of this study was to compare sexual function outcomes between laparoscopic lateral suspension and laparoscopic sacrocervicopexy, assessed before surgery and 12 months postoperatively.
2 Materials and methods
This retrospective observational study included 100 women referred to our department and qualified for surgery from January 2018 to December 2021. We performed a secondary analysis of sexual outcomes of a previous randomized control trial comparing LLS and LSC (53).
Preoperative data collected included age, parity, body mass index, and hormonal status.
The study inclusion criteria were: symptomatic apical prolapse stage ≥ II according to the Pelvic Organ Prolapse Quantification (POP-Q) system, sexually active women (SA), sexually not active women (NSA), all women who were able to understand and write in Polish.
The exclusion criteria included: a history of previous urogynecological surgeries, including prolapse/incontinence surgery and hysterectomy; active malignancy; posterior vaginal wall prolapse ≥ II stage.
Stress urinary incontinence was not an exclusion criterion, but patients were informed that only surgical repair of POP would be performed. 43 patients were qualified for laparoscopic sacrocervicopexy, and 46 for laparoscopic lateral suspension. All women underwent concomitant laparoscopic supracervical hysterectomy, which is a standard procedure in our department. All surgical procedures were performed by an experienced surgical team. In our study, we utilized a polypropylene mesh with a pore size of 1 mm and a product weight of 65 g/m2 for LLS and SCP procedures”.
The study was approved by our institutional ethic committee, and patients who met the inclusion criteria signed informed consent prior to participation in the study. Eleven patients were excluded because they did not meet all inclusion criteria or met at least one exclusion criterion.
2.1 The applied questionnaire
The patients completed a validated Polish questionnaire, the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR) before undergoing surgery and 12 months postoperatively. The data were collected through face-to-face interviews conducted by an experienced urogynecologist (EMJ).
PISQ-IR is the disease-specific questionnaire to assess the women’s sexual function in both sexually active (SA) and inactive women (NSA) with PFD (Pelvic Floor Disorders) (57, 58).
PISQ-IR consists of two parts. Part 1, for not SA (NSA) women, and contains four domains – specific subscales (Condition – specific—NSA—CS, Partner-related—NSA—PR, Global Quality—NSA-GQ, Condition Impact—NSA-CI). Part 2, for sexually active (SA) women with six domains – specific subscales (Arousal-Orgasm—AO, Condition-specific—CS, Partner-related—PR, Desire – D, Condition Impact – CI, Global Quality—GQ).
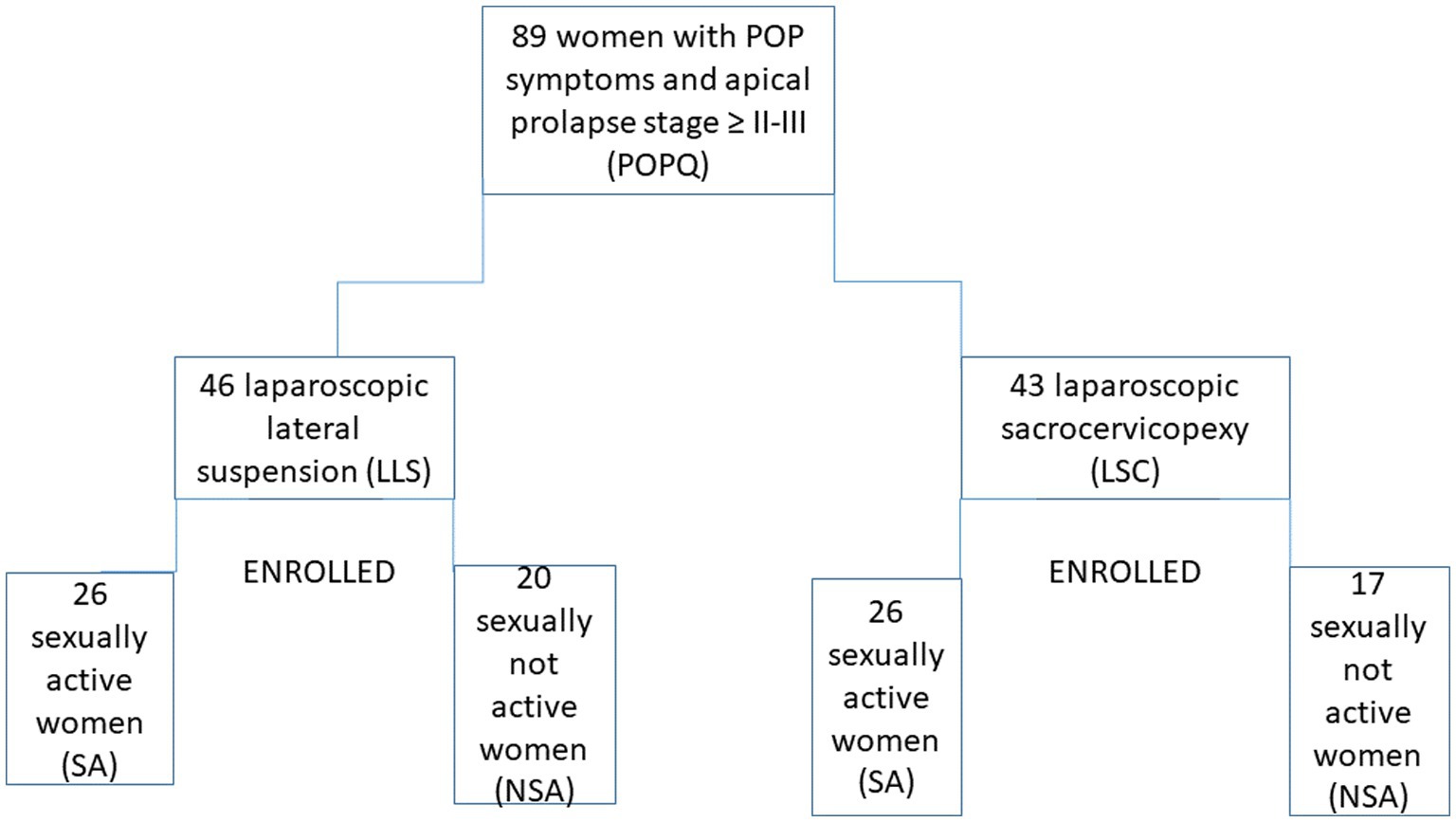
In the PISQ-IR questionnaire, the first question (Q1) describes the engagement in sexual activity and sound: “Which of the following describes you?” According to this, we enrolled patients to two groups SA and not SA. The enrolment process is shown in Figure 1.
Data was collected by face to face interview and from the patient’s medical records. Physical examination was conducted one month after surgery, including POP-Q evaluation. The information collected from patients’ medical records included anamnesis and the patients’ physical examination results. All women underwent post-operative follow-up within 3–6 months postoperatively to assess recurrent prolapse or mesh exposure or other potential complications of the surgery. A personal interview 12 months after surgery was carried out by an experienced urogynaecologist EMJ. In this interview, the patients were requested to answer a PISQ IR questionnaire.
2.2 Statistical analysis
Based on the collected data, a database was created using Microsoft Excel® 2013 (15.0.5589.1000) MSO (15.0.5589.1000) (32-bit), from Microsoft Office Standard 2013, Microsoft Corporation, manufacture code DG7GMGF0D7FX:0002. The data were statistically analyzed using Gretl software version 2017a. Comparisons were made between LLS and LSC preoperatively and 12 months postoperatively; the p value was obtained using a t-test. The significance level was assumed to be p < 0.005.
3 Results
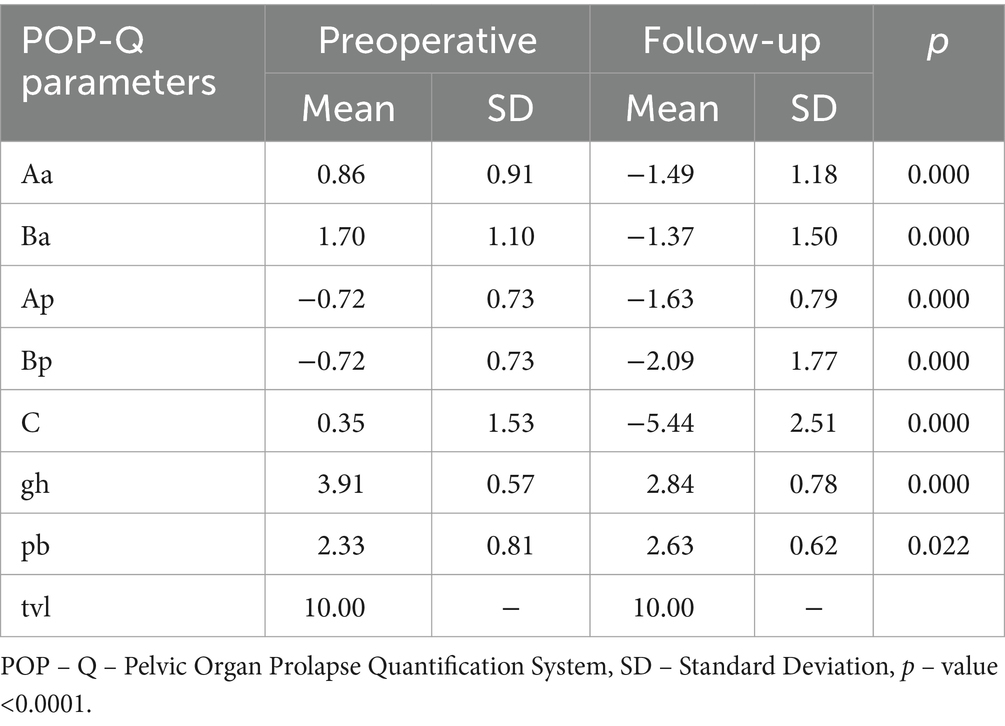
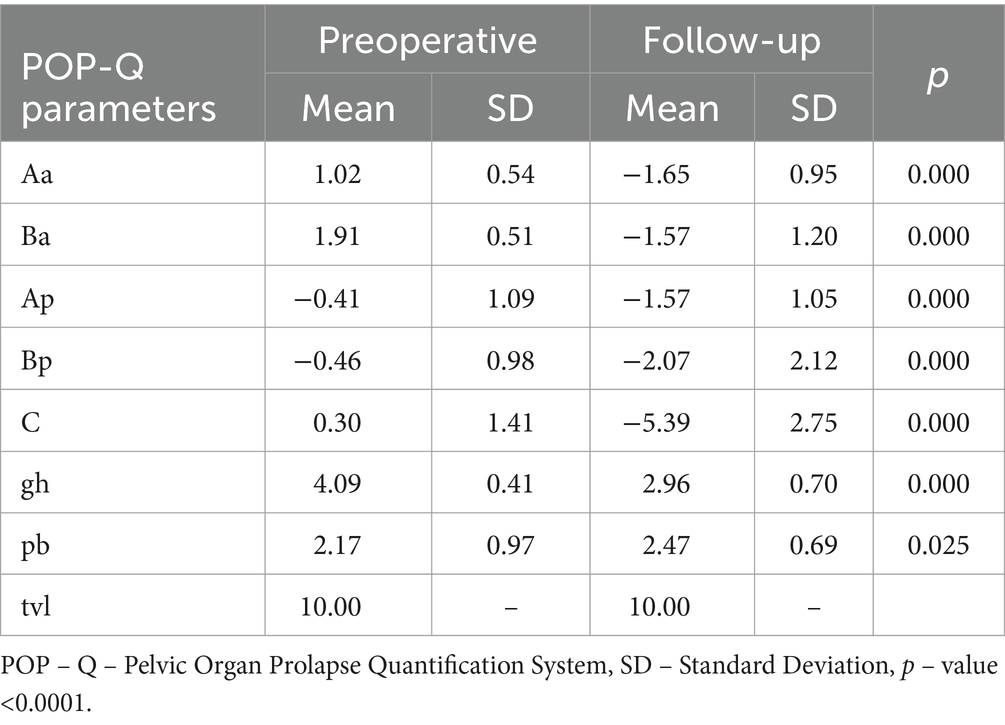
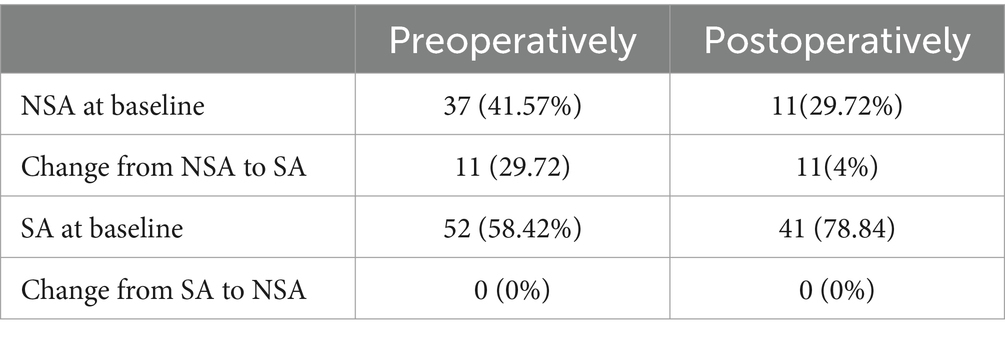
In the analyzed group of 89 female patients, 52 (58.42%) were sexually active (SA) and 37 (41.57%) were inactive (NSA). All of the patients were qualified for surgery because of pelvic organ prolapse (POP). We have observed significant improvement of POP after both procedures. Tables 1, 2 present anatomic outcomes before and after both surgeries.
26 (60.46%) sexually active and 17 (39.53%) inactive patients were qualified for laparoscopic promontofixation surgery, while in the group of patients qualified for laparoscopic lateral suspension surgery, 26 (60.46%) were sexually active and 20 (43.47%) inactive.
In the group of 17 NSA women qualified for laparoscopic promontofixation surgery: 9 (52.94%) women had non-intercourse due to the lack of a partner (NSA-PR), 8 (47.05%) women had non-intercourse due to the lack of intercourse despite having a partner, of which in 2, the lack of desire for intercourse was the result of prolapse (NSA-CS). From the non-intercourse groups due to the surgical reduction of POP, both patients returned to sexual activity.
In a group of 26 SA women scheduled for laparoscopic promontofixation surgery, 17 (65.38%) patients stated that they “significantly” or “very much” avoid sexual activity due to the prolapse of the reproductive organ (SA-CI). The remaining 9 (34.61%) patients replied that the problem of prolapse did not determine their sexual activity. Despite this, a total of 21 (80.76%) women experienced an improvement in the quality of their sexual life after the surgery, due to the reduced feeling of discomfort associated with the improvement of anatomical conditions.
In the group of 20 NSA women qualified for lateral suspension surgery: 4 (20%) women did not have intercourse due to the lack of a partner, 16 (80%) women did not have intercourse due to the lack of willingness to have intercourse, despite having a partner, of which 9 women did not want to have intercourse caused by POP (NSA-PR, NSA-CS). From the group of women who did not have sexual intercourse due to the POP, all patients returned to sexual activity after the surgery.
In a group of 26 SA women qualified for laparoscopic lateral suspension surgery, 15 patients answered that they avoid “significantly” or “very much” sexual activity due to the POP (SA-CI). The remaining 11 patients replied that the problem of POP did not determine their sexual activity. Despite this, 20 (76.92%) women had a significant improvement in their quality of life due to the improvement of depression symptoms.
After both surgeries, no patient in the NSA and SA groups reported dyspareunia or other health problems.
Despite the lack of sexual activity due to reluctance to have intercourse or the lack of a partner, NSA women in both study groups assessed the subjective quality of sexual life (NSA-GQ-) as “sufficient and satisfactory,” both before and after surgical treatment. In response to the questionnaire question “How much does the lack of sexual activity bother you?” answered “Not at all” or “A little”.
In contrast to NSA patients who did not have sexual intercourse due to a POP, who answered the same question “It bothers me a lot” or “It bothers me a lot.” This indicates that the POP was the reason for not having intercourse.
In the group of SA patients, after both procedures, there was no significant improvement in the quality of life in terms of the feeling of orgasm or sexual desire (SA-O, SA-D domain). In the entire SA group operated on, a “positive” or “very positive” influence of the sexual partner on the perceived sexual desire was found, but the surgery did not improve the degree of sexual interest (SA-P domain).
Analyzing the entire questionnaire, surgical treatment to correct the reduction contributed to the improvement of the quality of sexual life in 21 (80.76%) of 26 in the group of sexually active women after promontofixation surgery and in 20 (76.92%) of 26 in the group of SA patients (sexually active) after side suspension surgery (Table 3). Therefore, the quality of sexual life in this group of patients improved significantly after both surgical procedures. The treatment of the symptoms of POP significantly influenced the improvement in the quality of sexual life of the surveyed women (Figure 2).
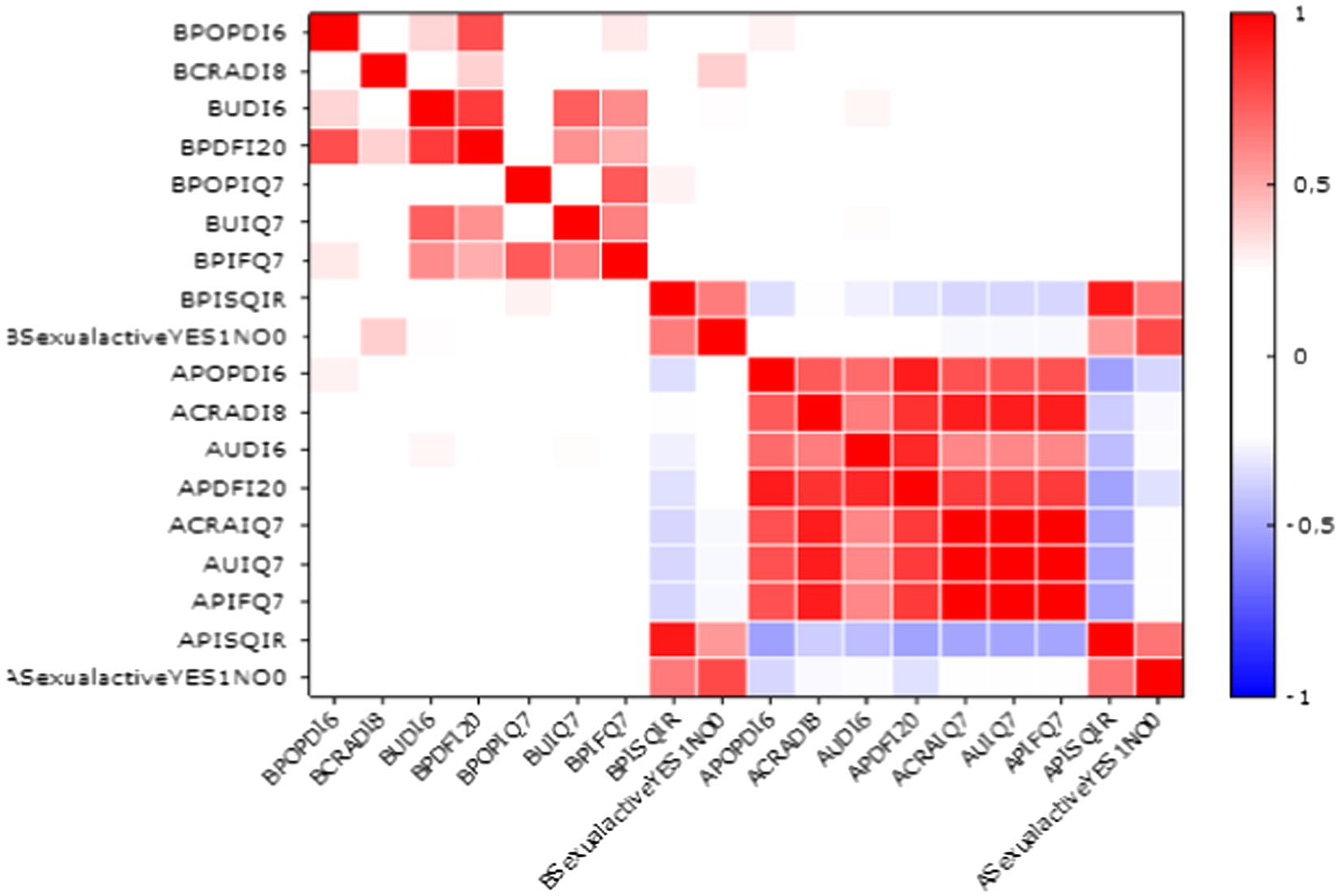
Figure 2. Correlation between sexual activity and symptomatic domains of questionnaire (red colors represent positive correlations, while blue colors denote negative correlations, the darker or more saturated the color—the stronger the relationship).
There was no significant statistical difference between groups in improvement in sexual quality of life after both procedures in NSA women. A total of 11 women in the NSA group returned to sexual activity.
4 Discussion
According to the International Continence Society (ICS) and the International Urogynecological Association (IUGA) Pelvic Organ Prolapse (POP) is defined as „the descent of one or more of the anterior vaginal wall, posterior vaginal wall, the uterus (cervix) or the apex of the vagina, or the perineum (perineal descent)” (59). The symptoms of Pelvic Organ Prolapse (POP) experienced by women can have a significant impact on their biopsychosocial, psychological, and social well-being. According to patient-reported outcome measures (PROMs), women with POP reported moderate levels of pain during sexual intercourse and low levels of bodily pain. Furthermore, POP was found to have a low to moderate impact on sleep quality, energy levels, quality of life, and sexual function domains, while its impact on physical symptoms and general health perception domains was relatively low. The results of PROMs assessing physical functioning varied widely, ranging from low to high impact (60, 61).
Sexual health, as defined by the World Health Organization, is a state of complete physical, mental, and social well-being related to sexuality. It encompasses not just the absence of disease or infirmity, but also emotional health (62). Sexual functioning is defined as “absence of difficulty moving through the stages of sexual desire, arousal, and orgasm, as well as subjective satisfaction with the frequency and outcome of individual and partnered sexual behavior” (63). Patient-reported outcome measures (PROMs) questionnaires provide a valuable patient-centered perspective on the effectiveness of surgical interventions for Pelvic Organ Prolapse (POP). However, it’s crucial to carefully choose a prolapse-specific questionnaire that is both validated and prelevant to the patient’s condition. This ensures an accurate and thorough portrayal of their experiences and outcomes.
To assess female sexual functioning, various questionnaires such as the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire—IUGA Revised (PISQ-IR), Female Sexual Function Index (FSFI), International Consultation on Incontinence Questionnaire–Vaginal Symptoms Module (ICIQ-VS), Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12) can be used. The ICIQ-VS questionnaire may not be the best choice for obtaining a comprehensive understanding of a patient’s condition, as it solely focuses only on vaginal symptoms and is comparatively shorter (4 main questions). The Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ) and its short form version, the PISQ-12, are the only current validated condition-specific female sexual function questionnaires purposively developed to assess sexual function in women with UI and/or POP (64, 65).
PISQ-12 is a shortened version of the PISQ-31 questionnaire presented in 2001. This questionnaire is used to assess sexual function in heterosexual patients with diagnosed POP and/or UI who have been sexually active over the last 6 months. It should not be used for patients who have no partner or are sexually inactive (66). The International Urogynecological Association (IUGA) Sexual Function Working Group undertook a comprehensive re-evaluation of the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire (PISQ), with the primary objectives of refining its psychometric properties, expanding its applicability to women who are not sexually active and those with anal incontinence, and creating a universally applicable instrument for international use (67). These objectives have been successfully achieved with the development of the PISQ-IR, a revised and enhanced version of the original questionnaire.
PISQ-IR includes new ways of evaluating the inherent diversity of women who suffer from pelvic floor disorders (PFDs). Notably, the questionnaire incorporates gender-neutral items to evaluate the impact of a partner on sexual function. Although PISQ-IR enhances the ability to assess outcomes in women who are not sexually active and in women with anal incontinence. Importantly, this questionnaire was designed as an instrument that was directed toward international usage. The PISQ-IR questionnaire has undergone translation and validation in 11 different languages, including Polish (67).
The main focus of our study was the treatment of apical vaginal wall prolapse. There are various surgical techniques for treating apical vaginal prolapse, including open, laparoscopic, and vaginal approaches. These surgical procedures for PFD are associated with a range of side effects, some of which can be successfully avoided by selecting an appropriate method. The gold standard to treat apical prolapse is sacrocolpopexy (SCP) (10, 48). Recent research has confirmed that laparoscopic lateral suspension (LLS) is a valid and effective alternative to sacrocolpopexy (SCP) for apical pelvic organ prolapse (POP) repair. There is no significant difference in apical prolapse cure rates between LLS and SCP, indicating that LLS can achieve comparable outcomes to the SCP. The LLS seems preferable in terms of the Female Sexual Function Index, Pelvic Organ Prolapse Symptom Score, reoperation, and complications (68).
In our study those patients who were sexually active had sexual intercourse regardless of the POP. However, the improvement of anatomical conditions after surgery reduced the feeling of discomfort. Although before surgery, the majority of respondents in the group of SA women reported that POP did not affect their sexual life.
The vast majority associated the quality of sex life with a good relationship with their partner. Like other authors, we did not find any changes in the behavioral-emotional domain after surgical treatment, which assesses sexual desire and arousal, frequency of sexual activity, and the feeling of orgasm. One year after the surgery, the percentage of women with reduced sexual desire before the surgery did not change significantly after the surgery. Patients who did not have sexual intercourse before surgery mentioned age-related decreased sexual drive as the reason for this. The next cause was the POP. Surgical treatment did not improve these feelings, only the patients’ psychological comfort. It is worth emphasizing the fact that in the group of patients who did not have intercourse, some of them returned to sexual activity. This was due to the improvement in the quality of life in the range of experienced symptoms of POP and the return of the desire to have intercourse with a partner.
Numerous studies compare the postoperative results of patients who underwent LSC and anterior vaginal mesh (AVM), including impact on sexual activity or function. For example, vaginal length was greater following LSC-Cx compared to AVM. However, it is essential to note that vaginal length does not have a significant impact on female sexuality either preoperatively or postoperatively, the most important factors were “having a partner” for sexual activity and dyspareunia for sexual function (69). The persistence of dyspareunia was found to be higher after AVM (70, 71). Besides, transvaginal procedures have an increased risk of vaginal erosion, which can occur in up to 20% of patients who undergo transvaginal surgery for POP repair (72). We did not observe any cases of mesh erosion in any of the groups.
According to the available data, surgical management of POP usually results in improved or unchanged scores in sexual function, regardless of the type of procedure used.
None of the patients reported any deterioration in the quality of sexual life after both procedures. We did not observe dyspareunia after both surgeries. There were no women who became sexually inactive due to the surgery.
Our results showed that laparoscopic surgery can improve the quality of women’s sex lives by reducing symptoms associated with POP. The improvement in satisfaction with sexual life resulted from getting rid of the main problem, which was POP and the associated discomfort. Patients who had their uterine corpus removed during urogynecological surgery considered it an element that did not affect their quality of life, including sexual life. This is extremely important in the current discussion on leaving the uterine body during surgery for static disorders.
The data and results collected in this study can serve as a reference for future follow-up on the same cohort with the same tool, namely the PISQ+IR questionnaire. Including the same questionnaire in future studies containing different surgical techniques for POP repair will allow for objective and valid comparison between the operative techniques (73).
This study has several limitations. Considering the potential long-term complications associated with vaginal mesh observed in clinical practice, further investigations are warranted. Factors contributing to these complications include the inherent complexity of pelvic floor disorders, which remain inadequately understood; the biomechanical properties of the mesh, which may not be suitable for pelvic floor applications; variations in surgical techniques and the use of different modifications in operational practices across hospitals; and deficiencies in the regulatory processes for monitoring implantable medical devices. Standardization of surgical procedures is also needed.
The follow-up period is 12 months after the surgery. A longer follow-up is required to evaluate functional status for the long-term results and potential complications such as postoperative incontinence, other voiding dysfunctions, pudendal neuralgia. This study though, as mentioned, can be an initial reference point for any future follow-up. On the other hand, 12 months after surgery is an adequate period to assess POP surgeries efficacy. Our study presents important information regarding the success of laparoscopic lateral suspension pelvic organ prolapse reconstructive surgery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
EM-J: Conceptualization, Investigation, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft. AS: Supervision, Writing – review & editing. MM: Data curation, Resources, Writing – review & editing. DF: Project administration, Writing – review & editing. DO: Project administration, Writing – review & editing. JD: Supervision, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zietarska, M, Cisak, A, Zwierzchowska, A, Barcz, E, and Horosz, E. Sexual function in women with pelvic organ prolapse and surgery influence on their complaints. Ginekol Pol. (2023) 94:1–9. doi: 10.5603/GP.a2023.0029
2. Handa, VL, Harvey, L, Cundiff, GW, Siddique, SA, and Kjerulff, KH. Sexual function among women with urinary incontinence and pelvic organ prolapse. Am J Obstet Gynecol. (2004) 191:751–6. doi: 10.1016/j.ajog.2003.11.017
3. Wang, B, Chen, Y, Zhu, X, Wang, T, Li, M, Huang, Y, et al. Global burden and trends of pelvic organ prolapse associated with aging women: an observational trend study from 1990 to 2019. Front Public Health. (2022) 10:975829. doi: 10.3389/fpubh.2022.975829
4. Wu, JM, Kawasaki, A, Hundley, AF, Dieter, AA, Myers, ER, and Sung, VW. Predicting the number of women who will undergo incontinence and prolapse surgery 2010 to 2050. Am J Obstet Gynecol. (2011) 205:230.e1–5. doi: 10.1016/j.ajog.2011.03.046
5. Rahayu, S, Fakhrizal, E, and Hamidy, MY. Female sexual function following pelvic organ prolapse reconstruction: a case serial study. Curr Womens Health Rev. (2024) 20:442–50. doi: 10.2174/1573404820666230607104422
6. Glavind, K, Larsen, T, and Lindquist, AS. Sexual function in women before and after surgery for pelvic organ prolapse. Acta Obstet Gynecol Scand. (2015) 94:80–5. doi: 10.1111/aogs.12524
7. Chang, OH, Yao, M, Ferrando, CA, Paraiso, MFR, and Propst, K. Changes in sexual function over 12 months after native-tissue vaginal pelvic organ prolapse surgery with and without hysterectomy. Sex Med. (2023) 11:qfad006. doi: 10.1093/sexmed/qfad006
8. Kong, MK, and Bai, SW. Surgical treatments for vaginal apical prolapse. Obstet Gynecol Sci. (2016) 59:253–60. doi: 10.5468/ogs.2016.59.4.253
9. Geoffrion, R, and Larouche, M. Guideline No. 413: surgical Management of Apical Pelvic Organ Prolapse in women. J Obstet Gynaecol Can. (2021) 43:511–523.e1. doi: 10.1016/j.jogc.2021.02.001
10. Maher, C, Yeung, E, Haya, N, Christmann-Schmid, C, Mowat, A, Chen, Z, et al. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. (2023) 2023:CD012376. doi: 10.1002/14651858.CD012376.pub2
11. Intersdyscyplinarne wytyczne Polskiego Towarzystwa Uroginekologicznego odnośnie diagnostyki i leczenia obniżenia narządów miednicy mniejszej. Available at: https://ptug.pl/algorytmy-postepowania/intersdyscyplinarne-wytyczne-polskiego-towarzystwa-uroginekologicznego-odnosnie-diagnostyki-i-leczenia-obnizenia-narzadow-miednicy-mniejszej/ (accessed on 29 May 2024).
12. Maher, C, Feiner, B, Baessler, K, Christmann-Schmid, C, Haya, N, Brown, J, et al. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. (2016) 10:CD012376. doi: 10.1002/14651858.CD012376
13. Nygaard, I, Brubaker, L, Zyczynski, HM, Cundiff, G, Richter, H, Gantz, M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. (2013) 309:2016–24. doi: 10.1001/jama.2013.4919
14. Costantini, E, Brubaker, L, Cervigni, M, Matthews, CA, O'Reilly, BA, Rizk, D, et al. Sacrocolpopexy for pelvic organ prolapse: evidence-based review and recommendations. Eur J Obstet Gynecol Reprod Biol. (2016) 205:60–5. doi: 10.1016/j.ejogrb.2016.07.503
15. Nosti, PA, Andy, UU, Kane, S, White, DE, Harvie, HS, Lowenstein, L, et al. Outcomes of abdominal and minimally invasive sacrocolpopexy: a retrospective cohort study. Female Pelvic Med Reconstr Surg. (2014) 20:33–7. doi: 10.1097/SPV.0000000000000036
16. Dubuisson, JB, Dubuisson, J, and Puigventos, J. Optional treatment of the posterior compartment and techniques of laparoscopic lateral suspension for vaginal vault prolapse In: Laparoscopic anatomy of the pelvic floor. Cham: Springer (2020)
17. Mulayim, B, and Sendag, F. Modified laparoscopic lateral suspension: the Mulayim technique. J Minim Invasive Gynecol. (2019) 26:407–8. doi: 10.1016/j.jmig.2018.07.014
18. Akbaba, E, and Sezgin, B. Modified laparoscopic lateral suspension with a five-arm mesh in pelvic organ prolapse surgery. BMC Womens Health. (2021) 21:244. doi: 10.1186/s12905-021-01388-0
19. Dällenbach, P, De Oliveira, SS, Marras, S, and Boulvain, M. Incidence and risk factors for mesh erosion after laparoscopic repair of pelvic organ prolapse by lateral suspension with mesh. Int Urogynecol J. (2016) 27:1347–55. doi: 10.1007/s00192-016-2974-z
20. Banerjee, C, and Noé, KG. Laparoscopic pectopexy: a new technique of prolapse surgery for obese patients. Arch Gynecol Obstet. (2011) 284:631–5. doi: 10.1007/s00404-010-1687-7
21. Noé, KG, Schiermeier, S, Alkatout, I, and Anapolski, M. Laparoscopic pectopexy: a prospective, randomized, comparative clinical trial of standard laparoscopic sacral colpocervicopexy with the new laparoscopic pectopexy—postoperative results and intermediate-term follow-up in a pilot study. J Endourol. (2015) 29:210–5. doi: 10.1089/end.2014.0413
22. Obut, M, Oğlak, SC, and Akgöl, S. Comparison of the quality of life and female sexual function following laparoscopic pectopexy and laparoscopic sacrohysteropexy in apical prolapse patients. Gynecol Minim Invas Ther. (2021) 10:96–103. doi: 10.4103/GMIT.GMIT_67_20
23. Chuang, FC, Chou, YM, Wu, LY, Yang, TH, Chen, WH, and Huang, KH. Laparoscopic pectopexy: the learning curve and comparison with laparoscopic sacrocolpopexy. Int Urogynecol J. (2022) 33:1949–56. doi: 10.1007/s00192-021-04934-4
24. Peng, J, Li, S, Wang, L, Yang, L, Nai, M, Xu, Q, et al. Comparison of efficacy between laparoscopic pectopexy and laparoscopic high uterosacral ligament suspension in the treatment of apical prolapse—short-term results. Sci Rep. (2023) 13:18519. doi: 10.1038/s41598-023-45871-0
25. Morgan, DM, Rogers, MA, Huebner, M, Wei, JT, and Delancey, JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. (2007) 109:1424–33. doi: 10.1097/01.AOG.0000264066.89094.21
26. Unger, CA, and Walters, MD. Gluteal and posterior thigh pain in the postoperative period and the need for intervention after sacrospinous ligament colpopexy. Female Pelvic Med Reconstr Surg. (2014) 20:208–11. doi: 10.1097/SPV.0000000000000091
27. Briody, C, et al. Uterosacral ligament suspension for the treatment of apical prolapse: a review of the literature. Int Urogynecol J. (2014) 25:293–300.
28. Ghetti, C, et al. Uterosacral ligament suspension for prolapse: a review of the literature. Am J Obstet Gynecol. (2012) 206:298–304.
29. Rardin, CR, et al. Uterosacral ligament suspension for apical prolapse: a comparative effectiveness study. Obstet Gynecol. (2016) 128:821–9.
30. Huang, HF, et al. Comparison of uterosacral ligament suspension and sacrospinous ligament fixation for apical prolapse. Eur J Obstet Gynecol Reprod Biol. (2017) 215:97–102.
31. American Urological Association (AUA) . Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction (SUFU). Guideline for the surgical treatment of female stress urinary incontinence. J Urol. (2017) 197:1575–85.
32. Nager, CW, et al. Transvaginal mesh for pelvic organ prolapse: a review of the literature. Am J Obstet Gynecol. (2012) 206:193–203.
33. FDA Public Health Notification . Urogynecologic surgical mesh: Benefit-risk perspective Food and Drug Administration (2011). Available at: https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/fdas-activities-urogynecologic-surgical-mesh (Accessed 30, January 2024)
34. Barber, MD, and Maher, C. Apical Prolapse. Int Urogynecol J. (2013) 24:1815–33. doi: 10.1007/s00192-013-2172-1
35. McCall, ML . Posterior Culdeplasty: surgical correction of Enterocele during vaginal hysterectomy—a preliminary report. Obstet Gynecol. (1957) 10:595–602. doi: 10.1097/00006250-195712000-00001
36. Karram, MM . Vaginal native tissue suture repair of vaginal vault prolapse In: MS Baggish and MM Karram, editors. Atlas of pelvic anatomy and gynecologic surgery. 4th ed. Philadelphia, PA, USA: Elsevier (2016). 647–77.
37. Webb, MJ, Aronson, MP, Ferguson, LK, and Lee, RA. Posthysterectomy vaginal vault prolapse: primary repair in 693 patients. Obstet Gynecol. (1998) 92:281–5. doi: 10.1016/s0029-7844(98)00201-4
38. Nager, CW, et al. The role of Colpocleisis in the treatment of pelvic organ prolapse. Curr Opin Urol. (2015) 25:407–13.
39. ICS (International Continence Society) . Pelvic Organ Prolapse. Available at: https://www.ics.org/standards (accessed on 31 January 2024) (2024).
40. Dwyer, PL . Choice of pelvic organ prolapse surgery: vaginal or abdominal, native tissue or synthetic grafts, open abdominal versus laparoscopic or robotic. Int Urogynecol J. (2014) 25:1151–2. doi: 10.1007/s00192-014-2481-z
41. Park, YH, Yang, SC, Park, ST, Park, SH, and Kim, HB. Laparoscopic reconstructive surgery is superior to vaginal reconstruction in the pelvic organ prolapse. Int J Med Sci. (2014) 11:1082–8. doi: 10.7150/ijms.9027
42. Maher, CF, Feiner, B, DeCuyper, EM, Nichlos, CJ, Hickey, KV, and O'Rourke, P. Laparoscopic sacral Colpopexy versus Total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol. (2011) 204:e1–7. doi: 10.1016/j.ajog.2010.11.016.
43. Alas, AN, and Anger, JT. Management of Apical Pelvic Organ Prolapse. Curr Urol Rep. (2015) 16:33. doi: 10.1007/s11934-015-0498-6
44. Chan, CYW, Fernandes, RA, Yao, HH, O'Connell, HE, Tse, V, and Gani, J. A systematic review of the surgical management of apical pelvic organ prolapse. Int Urogynecol J. (2023) 34:825–41. doi: 10.1007/s00192-022-05408-x
45. Antosh, DD, Kim-Fine, S, Meriwether, KV, Kanter, G, Dieter, AA, Mamik, MM, et al. Changes in sexual activity and function after pelvic organ prolapse surgery: a systematic review. Obstet Gynecol. (2020) 136:922–31. doi: 10.1097/AOG.0000000000004125
46. Dällenbach, P, Alec, M, Boulvain, M, and Shabanov, S. Outcomes of robotically assisted laparoscopic lateral suspension (RALLS) with mesh for anterior and apical prolapse. J Robot Surg. (2022) 16:287–94. doi: 10.1007/s11701-021-01234-3
47. Dällenbach, P . Laparoscopic lateral suspension (LLS) for the treatment of apical prolapse: a new gold standard? Front Surg. (2022) 9:898392. doi: 10.3389/fsurg.2022.898392
48. Russo, E, Montt Guevara, MM, Sacinti, KG, Misasi, G, Falcone, M, Morganti, R, et al. Minimal invasive abdominal sacral Colpopexy and abdominal lateral suspension: a prospective, open-label, multicenter, non-inferiority trial. J Clin Med. (2023) 12:2926. doi: 10.3390/jcm12082926
49. Mereu, L, Tateo, S, D’Alterio, MN, Russo, E, Giannini, A, Mannella, P, et al. Laparoscopic lateral suspension with mesh for apical and anterior pelvic organ prolapse: a prospective double center study. Eur J Obstet Gynecol Reprod Biol. (2020) 244:16–20. doi: 10.1016/j.ejogrb.2019.10.026
50. Veit-Rubin, N, Dubuisson, JB, Lange, S, Eperon, I, and Dubuisson, J. Uterus-preserving laparoscopic lateral suspension with mesh for pelvic organ prolapse: a patient-Centred outcome report and video of a continuous series of 245 patients. Int Urogynecol J. (2016) 27:491–3. doi: 10.1007/s00192-015-2859-6
51. Dubuisson, J, Eperon, I, Dällenbach, P, and Dubuisson, J-B. Laparoscopic repair of vaginal vault prolapse by lateral suspension with mesh. Arch Gynecol Obstet. (2013) 287:307–12. doi: 10.1007/s00404-012-2574-1
52. Pacquée, S, Nawapun, K, Claerhout, F, Werbrouck, E, Veldman, J, D’hoore, A, et al. Long-term assessment of a prospective cohort of patients undergoing laparoscopic Sacrocolpopexy. Obstet Gynecol. (2019) 134:323–32. doi: 10.1097/AOG.0000000000003380
53. Malanowska-Jarema, E, Starczewski, A, Melnyk, M, Oliveira, D, Balzarro, M, and Rubillota, E. A randomized clinical trial comparing Dubuisson laparoscopic lateral suspension with laparoscopic Sacropexy for pelvic organ prolapse: short-term results. J Clin Med. (2024) 13:1348. doi: 10.3390/jcm13051348
54. Malanowska-Jarema, E, Osnytska, Y, Starczewski, A, Balzarro, M, and Rubilotta, E. A comparative study in learning curves of laparoscopic lateral suspension vs. laparoscopic Sacrocolpopexy: preliminary results. Front Surg. (2023) 10:1274178. doi: 10.3389/fsurg.2023.1274178
55. Najib, B, Rusavy, Z, Abdallah, W, Abdel Khalek, Y, Giraud, N, and Deval, B. Impact of laparoscopic Sacrocolpopexy (LSC) on sexual function in women with advanced stages of pelvic organ prolapse (POP): a five-year prospective study. Eur J Obstet Gynecol Reprod Biol. (2023) 284:12–5. doi: 10.1016/j.ejogrb.2023.02.016
56. Rusavy, Z, Kovarova, V, Tvarozek, S, Smazinka, M, Havir, M, and Kalis, V. A comprehensive evaluation of sexual life in women after laparoscopic Sacrocolpopexy using PISQ-IR. Int Urogynecol J. (2024) 35:873–80. doi: 10.1007/s00192-024-05765-9
57. Rogers, RG, Rockwood, TH, Constantine, ML, Thakar, R, Kammerer-Doak, DN, Pauls, RN, et al. New measure of sexual function in women with pelvic floor disorders (PFD): the pelvic organ prolapse/incontinence sexual questionnaire, IUGA-revised (PISQ-IR). Int Urogynecol J. (2013) 24:1091–103. doi: 10.1007/s00192-012-2020-8
58. Grzybowska, ME, Futyma, K, and Wydra, D. Identification of the pelvic organ prolapse/incontinence sexual questionnaire-IUGA revised (PISQ-IR) cutoff scores for impaired sexual function in women with pelvic floor disorders. J Clin Med. (2019) 9:13. doi: 10.3390/jcm9010013
59. Grzybowska, ME, Piaskowska-Cala, J, and Wydra, DG. Polish translation and validation of the pelvic organ prolapse/urinary incontinence sexual questionnaire, IUGA-revised (PISQ-IR). Int Urogynecol J. (2019) 30:55–64. doi: 10.1007/s00192-017-3539-5
60. Doumouchtsis, SK, de Tayrac, R, Lee, J, Daly, O, Melendez-Munoz, J, Lindo, FM, et al. An international continence society (ICS)/international Urogynecological association (IUGA) joint report on the terminology for the assessment and Management of Obstetric Pelvic Floor Disorders. Int Urogynecol J. (2023) 34:1–42. doi: 10.1007/s00192-022-05397-x
61. Carroll, L, O'Sullivan, C, Perrotta, C, and Fullen, BM. Biopsychosocial profile of women with pelvic organ prolapse: a systematic review. Womens Health. (2023) 19:19. doi: 10.1177/17455057231181012
62. Sexual and Reproductive Health and Research (SRH) , WHO. Available at: https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health (accessed on 29 May 2024).
63. Fielder, R . Sexual Functioning. In: M.D. Gellman and J.R Turner. (eds) Encyclopedia of Behavioral Medicine. Springer, New York, NY, (2013). (Accessed on 29 May 2024).
64. Hoen, LA, Utomo, E, Steensma, AB, Blok, BF, and Korfage, IJ. The pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12): validation of the Dutch version. Int Urogynecol J. (2015) 26:1293–303. doi: 10.1007/s00192-015-2692-y
65. Rogers, RG, Coates, KW, Kammerer-Doak, D, Khalsa, S, and Qualls, C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. (2003) 14:164–8. doi: 10.1007/s00192-003-1063-2
66. Kamińska, A, Skorupska, K, Kubik-Komar, A, Futyma, K, Filipczak, J, and Rechberger, T. Reliability of the polish pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12) and assessment of sexual function before and after pelvic organ prolapse reconstructive surgery—a prospective study. J Clin Med. (2021) 10:1–10. doi: 10.3390/jcm10184167
67. The International Urogynecological Association (IUGA) PISQ-IR: Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire, IUGA-Revised. Available at https://www.iuga.org/resources/pisq-ir (accessed on 29 May, 2024) (2024).
68. Baki Erin, K, Taştan, AŞ, Katırcı, Y, Özdemir, AZ, Güven, D, Önem, K, et al. Comparison of 2-year follow-up outcomes of laparoscopic lateral suspension and sacrospinous fixation in apical compartment prolapse: an observational study. Arch Gynecol Obstet. (2023) 307:1859–65. doi: 10.1007/s00404-023-06958-1
69. Anglès-Acedo, S, Ros-Cerro, C, Escura-Sancho, S, Palau-Pascual, MJ, Bataller-Sánchez, E, Espuña-Pons, M, et al. Female sexuality before and after Sacrocolpopexy or vaginal mesh: is vaginal length one of the key factors? Int Urogynecol J. (2022) 33:143–52. doi: 10.1007/s00192-021-04697-y
70. Antosh, D, Dieter, AA, Balk, EM, Kanter, G, Kim-Fine, S, Meriwether, KV, et al. Sexual function after pelvic organ prolapse surgery: a systematic review comparing different approaches to pelvic floor repair. Am J Obstet Gynecol. (2021) 222:S769. doi: 10.1016/j.ajog.2019.12.036
71. Savary, P, Ferry, X, Deffieux, S, Campagne-Loiseau, S, de Tayrac, R, Blanc, S, et al. Safety of vaginal mesh surgery versus laparoscopic mesh Sacropexy for cystocele repair: results of the prosthetic pelvic floor repair randomized controlled trial. Eur Urol. (2018) 74:167–76. doi: 10.1016/j.eururo.2018.01.044.
72. Deffieux, X, de Tayrac, R, Huel, C, Bottero, J, Gervaise, A, Bonnet, K, et al. Vaginal mesh Erosion after transvaginal repair of cystocele using Gynemesh or Gynemesh-soft in 138 women: a comparative study. Int Urogynecol J. (2006) 18:73–9. doi: 10.1007/s0192-005-0041
Keywords: pelvic organ prolapse, lateral suspension, sacrocervicopexy, sexual function, pelvic organ prolapse/incontinence sexual questionnaire—IUGA revised (PISQ-IR)
Citation: Malanowska-Jarema E, Starczewski A, Melnyk M, Fidalgo D, Oliveira D and Dubuisson J (2024) Comparison of sexual function between laparoscopic lateral suspension and laparoscopic sacrocervicopexy with the use of the PISQ-IR questionnaire. Front. Med. 11:1456073. doi: 10.3389/fmed.2024.1456073
Edited by:
Rafał Watrowski, Helios Hospital Müllheim, GermanyReviewed by:
Laurentiu Cornel Pirtea, Victor Babes University of Medicine and Pharmacy, RomaniaLiu Lubin, The Women and Children Hospital of Chongqing Medical University, China
Copyright © 2024 Malanowska-Jarema, Starczewski, Melnyk, Fidalgo, Oliveira and Dubuisson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ewelina Malanowska-Jarema, ZW1hbGFuMjAxNkBnbWFpbC5jb20=
 Ewelina Malanowska-Jarema
Ewelina Malanowska-Jarema Andrzej Starczewski1
Andrzej Starczewski1 Mariia Melnyk
Mariia Melnyk Daniel Fidalgo
Daniel Fidalgo Dulce Oliveira
Dulce Oliveira Jean Dubuisson
Jean Dubuisson