- Clinical Laboratory Department, The Affiliated Hospital of Liaoning University of Traditional Chinese Medicine, Shenyang, Liaoning, China
The recent article by Wen et al., published in PLOS ONE, titled “Effects of neuraxial anesthesia in sitting and lateral positions on maternal hemodynamics in cesarean section: A systematic review and meta-analysis,” caught my attention. In their study, the authors observed the effects of neuraxial anesthesia in sitting and lateral positions on maternal hemodynamics during cesarean section. Given the anatomical differences between the left and right sides of the body, which could result in differences in maternal hemodynamics and vasopressor requirements during neuraxial anesthesia for cesarean delivery, I was intrigued by the idea of further dividing the lateral position data from Wen et al.'s study into three subgroups: “left lateral position,” “right lateral position,” and “not mentioned” (where the included original study did not mention the lateral position) for a subgroup analysis. It seems to be more rigorous, the subgroup analysis revealed that the usage rate of ephedrine support was 1.42 times higher for parturients in the right lateral position compared to those in the sitting position. This finding supports our recommendation to distinguish between left and right lateral decubitus positioning in neuraxial anesthesia for cesarean delivery. But in contrast, no significant difference was observed between the sitting and lateral positions in terms of the number of parturients requiring ephedrine in Wen et al.'s. Given the limited research on the right-lateral position and its hemodynamic effects, further studies are needed to explore its clinical applications. Future research should also focus on conducting larger trials with greater sample sizes to evaluate the long-term neonatal outcomes associated with varying maternal positions. Additionally, researchers should conduct subgroup analyses that separate the left- and right-lateral positions to provide clearer guidance for anesthesiologists.
1 Introduction
Cesarean section is a common mode of delivery, and the choice of anesthesia plays a critical role in ensuring the safety and comfort of both mother and baby. Neuraxial anesthesia is widely used in cesarean sections due to its effective analgesic properties and maternal-fetal safety (2). Patient positioning is an important factor in anesthesia management, as it can significantly affect the anesthesia's effectiveness and the patient's hemodynamic status (3). Neuraxial anesthesia can be administered in a sitting, lateral, or rarely prone posture. Each position has its advantages and disadvantages.
The advantage of the sitting position is that midline structures can be easily identified, even in obese patients, and it prevents compression of the aorta and the inferior vena cava, thereby avoiding supine hypotension syndrome caused by sympathetic blockade. However, maintaining the sitting position is difficult in cases of multiple pregnancies, umbilical cord prolapse, and emergency situations, where the lateral position may be more suitable for the patient. Sympathectomy caused by neuraxial anesthesia, combined with peripheral blood pooling due to gravity, makes hypotension more pronounced in the sitting position than in the lateral position (4). The lateral position, which has a lower risk of postural hypotension, is better suited for patients in a weakened condition and provides superior local anesthetic spread, leading to better sensory blockade. However, the lateral position may cause compression of the axillary artery, axillary vein, and brachial plexus in the armpit area (5).
Cesarean section under spinal anesthesia often results in maternal hypotension and fetal acidosis. The hypotension experienced by mothers after neuraxial anesthesia is mainly due to the spread of local anesthetics in the subarachnoid space and compression of the abdominal aorta by the uterus (6). Although current practice suggests a 15° left-lateral tilt for cesarean sections under neuraxial anesthesia, some early studies reported the use of a right-lateral tilt in actual patients. The effects of left-lateral and right-lateral tilt on the aortic and inferior vena cava volumes in pregnant women remain unclear. To address this, Fujita et al. used magnetic resonance imaging (MRI) and found no significant difference in aortic volume between the left-lateral and right-lateral tilt positions under neuraxial anesthesia. However, the mean inferior vena cava volume in the 30° left-lateral tilt was significantly greater than that in the 15° and 30° right-lateral tilt positions. Interestingly, for some patients, the 30° right-lateral tilt yielded the optimal inferior vena cava volume (7).
These findings suggest that the hemodynamic effects of left-lateral or right-lateral tilt following neuraxial anesthesia differ among individuals and are directly related to the selection and dosage of vasopressors used in treatment.
2 Statistical methods
First, we verified that the extracted data from Wen et al. (1) matched the original data in the included studies. All data were analyzed using RevMan version 5.3 software. Continuous variables such as the lowest systolic blood pressure and ephedrine dose were expressed as mean difference (MD) with a 95% confidence interval (CI). Relative risk (RR) with 95% CI was used for dichotomous variables such as the incidence of hypotension, the usage rate of ephedrine, and the incidence of nausea and vomiting. The I2 value indicated the heterogeneity among included original studies; I2 values of over 25%, 50%, and 75% are commonly defined as low, medium, and high heterogeneity, respectively. When I2 ≥ 50%, the heterogeneity is significant, this degree of variability required sensitivity analysis or subgroup analysis to identify plausible sources of heterogeneity, and the random effect model is applied. When I2 <50%, the heterogeneity among included studies is considered small, and the fixed effects model is selected.
3 Subgroup analysis results
3.1 Incidence of hypotension
Hypotension was observed in the sitting and lateral decubitus groups across seven trials, with the lateral decubitus group divided into right lateral and left lateral decubitus subgroups (8–14). Subgroup analysis showed no difference between the sitting and right lateral decubitus groups (RR, 1.05; 95% CI, 0.26–4.19; P = 0.95; I2 = 86%), and no difference between the sitting and left lateral decubitus groups (RR, 0.73; 95% CI, 0.54–1.00; P = 0.05; I2 = 53%) (Supplementary Figure S1).
3.2 Lowest systolic blood pressure
Comparing the lowest systolic blood pressure in women after neuraxial anesthesia in the two positions across 5 trials (8–11, 13), subgroup analysis showed no difference between the sitting and right lateral decubitus groups (MD, −2.10; 95% CI, −22.67–18.46; P = 0.84; I2 = 92%), and no difference between the sitting and left lateral decubitus groups (MD, 1.11; 95% CI, −5.15–7.38; P = 0.73; I2 = 84%) (Supplementary Figure S2).
3.3 Dose of ephedrine
The comparison of ephedrine dosages in nine RCTs after neuraxial anesthesia in parturients in two positions (8–12, 15–18). In Yun et al.'s study (18), it was not mentioned whether the parturients adopted the left or right lateral decubitus position after neuraxial anesthesia, so this study was separately defined as the “not mentioned” subgroup. Subgroup analysis showed that there was no difference between the sitting and right lateral decubitus position groups (MD, 1.73; 95% CI, −3.87–7.33; P = 0.55; I2 = 78%), and there was no difference between the sitting and left lateral decubitus position groups (MD, −1.00; 95% CI, −5.85–3.84; P = 0.68; I2 = 78%) (Supplementary Figure S3).
3.4 Usage rate of ephedrine
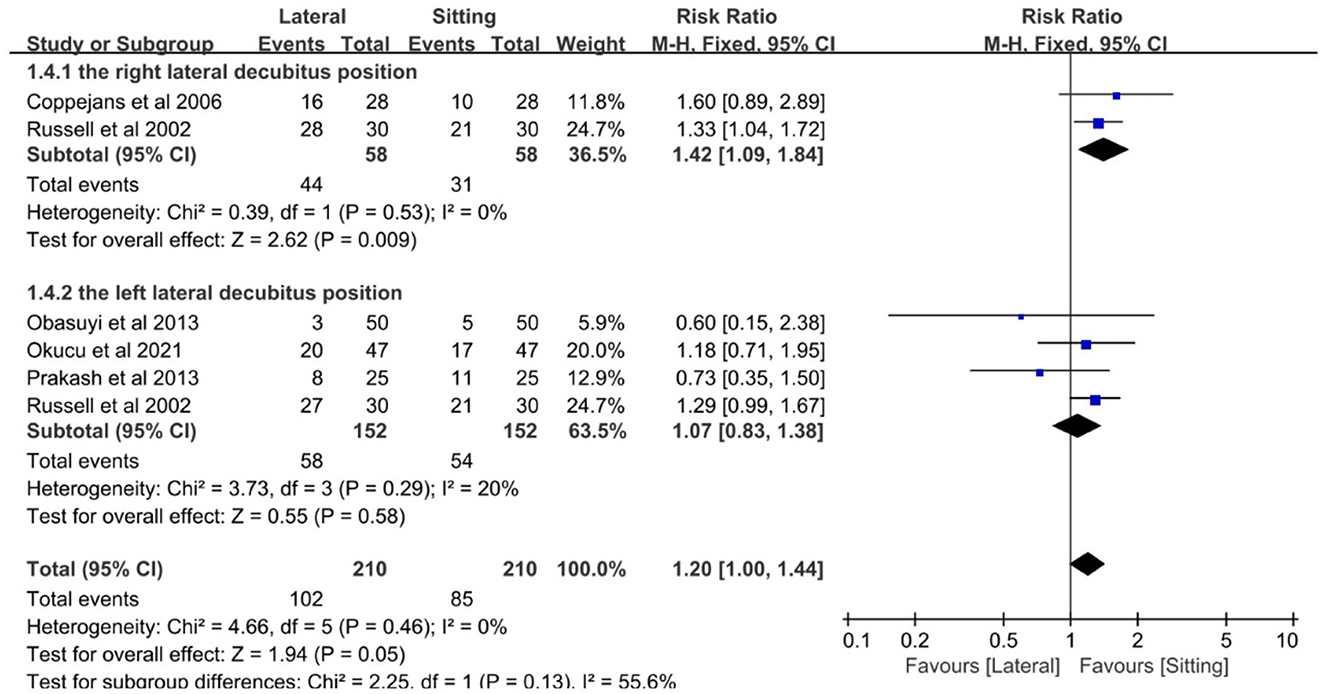
The number of parturients who needed ephedrine support following spinal anesthesia in the sitting and lateral positions was recorded in five trials (9, 11, 14, 16, 17). Xu et al.'s study (13) was excluded because it did not contain information on the number of parturients using ephedrine after neuraxial anesthesia. Subgroup analysis showed that the likelihood of needing ephedrine support was 1.42 times higher in parturients in the right lateral position compared to those in the sitting position (RR, 1.42; 95% CI, 1.09–1.84; P = 0.009; I2 = 0%), and there was no difference between the sitting and left lateral position groups (RR, 1.07; 95% CI, 0.83–1.38; P = 0.58; I2 = 20%) (Figure 1).
3.5 Incidence of nausea and vomiting
Comparing the incidence of nausea and vomiting in women after neuraxial anesthesia in the sitting and lateral decubitus positions across nine trials (8, 9, 11–13, 16–19). In Yun et al.'s study (18), it was not mentioned whether the parturients adopted the left or right lateral decubitus position after neuraxial anesthesia, so this study was separately defined as the “not mentioned” subgroup. Subgroup analysis showed no difference between the sitting and right lateral decubitus groups (RR, 1.30; 95% CI, 0.51–3.33; P = 0.58; I2 = 69%), and no difference between the sitting and left lateral decubitus groups (RR, 0.75; 95% CI, 0.27–2.12; P = 0.59; I2 = 70%) (Supplementary Figure S4).
4 Discussion
The subgroup analysis results showed that the usage rate of women needing ephedrine support was 1.42 times higher in the right lateral decubitus group compared to the sitting group. There was no significant difference in the incidence of hypotension, nausea, and vomiting, lowest systolic blood pressure, ephedrine dose, and probability of needing ephedrine support during cesarean section among the sitting, right and left lateral decubitus groups. The usage rate of ephedrine was higher in the right lateral decubitus group compared to the sitting group, but there was no significant difference between the left lateral decubitus and sitting groups, indicating that the left lateral decubitus position and sitting position can effectively reduce the usage rate of ephedrine than the right lateral decubitus position. However, further large-scale studies are needed to confirm this conclusion due to the limitations of this study, including a small number of included studies and a small sample size.
If hypotension is not corrected promptly with vasopressors, it can lead to nausea, vomiting, decreased uteroplacental blood flow, fetal acidosis, and in rare cases, severe consequences such as cardiovascular collapse. Although ephedrine can effectively treat maternal hypotension, it has higher transplacental transfer than phenylephrine due to its high lipid solubility, leading to fetal sympathetic metabolism stimulation as the dose increases. This results in neonatal acidemia, increased umbilical arterial and venous concentrations of lactate, glucose, epinephrine, and norepinephrine, and increased umbilical venous PCO2 (20). A systematic review reported that the risk of fetal acidosis with ephedrine use after neuraxial anesthesia in cesarean section is 5.29 times higher compared to phenylephrine (21). The right lateral decubitus position often requires more vasopressors to maintain blood pressure, increasing the risk of drug-related side effects (22). Given the above situation, studies on the lateral position for cesarean section under neuraxial anesthesia should be divided into the left lateral and the right lateral decubitus subgroups to ensure scientific rigor.
Further research should focus on larger, multicenter RCTs that examine the hemodynamic differences between the left-lateral and right-lateral positions during neuraxial anesthesia. Additionally, studies should explore the long-term outcomes for neonates exposed to different vasopressor regimens, particularly with regard to the risks of neonatal acidosis associated with ephedrine vs. phenylephrine. By advancing our understanding of the relationship between maternal positioning and anesthesia outcomes, we can improve maternal and neonatal safety during cesarean-sections.
Author contributions
SW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1454681/full#supplementary-material
References
1. Wen C, Xiang Y-Y, Pang Q-Y, Liu H-L. Effects of neuraxial anesthesia in sitting and lateral positions on maternal hemodynamics in cesarean section: a systematic review and meta-analysis. PLoS ONE. (2024) 19:e0303256. doi: 10.1371/journal.pone.0303256
2. Jaafarpour M, Taghizadeh Z, Shafiei E, Vasigh A, Sayehmiri K. The effect of intrathecal meperidine on maternal and newborn outcomes after cesarean section: a systematic review and meta-analysis study. Anesth Pain Med. (2020) 10:375. doi: 10.5812/aapm.100375
3. Kundra P, Arunsekar G, Vasudevan A, Vinayagam S, Habeebullah S, Ramesh A. Effect of postural changes on inferior vena cava dimensions and its influence on haemodynamics during caesarean section under spinal anaesthesia. J Obstet Gynaecol. (2015) 35:667–71. doi: 10.3109/01443615.2014.991291
4. Kelly JD, McCoy D, Rosenbaum SH, Brull SJ. Haemodynamic changes induced by hyperbaric bupivacaine during lateral decubitus or supine spinal anaesthesia. Eur J Anaesthesiol. (2005) 22:717–22. doi: 10.1017/s0265021505001183
5. Shahzad K, Afshan G. Induction position for spinal anaesthesia: sitting versus lateral position. J Pak Med Assoc. (2013) 63:11–5. doi: 10.3122/jabfm.2013.01.120304
6. Rajabi M, Razavizade M-R, Hamidi-Shad M, Tabasi Z, Akbari H, Hajian A. Magnesium sulfate and clonidine; effects on hemodynamic factors and depth of general anesthesia in Cesarean section. Anesth Pain Med. (2020) 10:e100563. doi: 10.5812/aapm.100563
7. Fujita N, Higuchi H, Sakuma S, Takagi S, Latif MAHM, Ozaki M. Effect of right-lateral versus left-lateral tilt position on compression of the inferior vena cava in pregnant women determined by magnetic resonance imaging. Anesth Analg. (2019) 128:1217–22. doi: 10.1213/ANE.0000000000004166
8. Simin A, Naghipour B, Farzin H, Maddahi S. Effect of position during induction of spinal anaesthesia for Caesarean section on maternal haemodynamic: randomised clinical trial. J Clin Diagn Res. (2018) 12:UC05–8. doi: 10.7860/JCDR/2018/27753.11184
9. Coppejans HC, Hendrickx E, Goossens J, Vercauteren MP. The sitting versus right lateral position during combined spinal-epidural anesthesia for cesarean delivery: block characteristics and severity of hypotension. Anesth Analgesia. (2006) 102:243–47. doi: 10.1213/01.ane.0000189049.11005.26
10. Manouchehrian NA-O, Moradi A, Torkashvand L. Comparative study of effect of spinal anesthesia in sitting and lateral positions on the onset time of sensory block and hemodynamic condition in cesarean section: a randomized clinical trial. Anesth Pain Med. (2021) 11:e111483. doi: 10.5812/aapm.111483
11. Obasuyi BI, Fyneface-Ogan S, Mato CN. A comparison of the haemodynamic effects of lateral and sitting positions during induction of spinal anaesthesia for caesarean section. Int J Obstet Anesth. (2013) 22:124–8. doi: 10.1016/j.ijoa.2012.12.005
12. Patel M, Samsoon G, Swami A, Morgan B. Posture and the spread of hyperbaric bupivacaine in parturients using the combined spinal epidural technique. Can J Anaesth. (1993) 40:943–6. doi: 10.1007/BF03010097
13. Xu Z, Shen F, Zhang Y, Tao Y, Chen X, Liu Z. Combined spinal-epidural anesthesia with hypobaric ropivacaine in sitting position significantly increases the incidence of hypotension in parturients undergoing cesarean section. J Obstet Gynaecol Res. (2016) 43:669–75. doi: 10.1111/jog.13253
14. Prakash S, Chaudhary K, Gogia AR, Chellani H, Salhan S, Singh R. A prospective, randomized controlled trial comparing the left lateral, modified lateral and sitting positions for spinal block characteristics for cesarean delivery. Minerva Anestesiol. (2013) 79:652–60.
15. Inglis A, Daniel M, McGrady E, McGrady E. Maternal position during induction of spinal anaesthesia for caesarean section A comparison of right lateral and sitting positions. Anaesthesia. (1995) 50:363–5. doi: 10.1111/j.1365-2044.1995.tb04620.x
16. Russell R, Popat M, Richards E, Burry J. Combined spinal epidural anaesthesia for caesarean section: a randomised comparison of Oxford, lateral and sitting positions. Int J Obstet Anesth. (2002) 11:190–5. doi: 10.1054/ijoa.2002.0964
17. Okucu F, Aksoy M, Ince I, Aksoy AN, Dostbil A, Ozmen O. Combined spinal epidural anesthesia in obese parturients undergoing cesarean surgery: a single-blinded randomized comparison of lateral decubitus and sitting positions. Anaesthesist. (2021) 70:30–7. doi: 10.1007/s00101-021-00995-8
18. Yun EM, Marx GF, Santos AC. The effects of maternal position during induction of combined spinal-epidural anesthesia for cesarean delivery. Anesth Analg. (1998) 87:614–8. doi: 10.1097/00000539-199809000-00023
19. Tan ED, Günaydin B. Comparison of maternal and neonatal effects of combined spinal epidural anaesthesia in either the sitting or lateral position during elective cesarean section. Turk J Anaesthesiol Reanim. (2014) 42:23–32. doi: 10.5152/TJAR.2013.55
20. Ngan Kee WD, Khaw KS, Tan PE, Ng FF, Karmakar M. Placental transfer and fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery. Anesthesiology. (2009) 111:506–12. doi: 10.1097/ALN.0b013e3181b160a3
21. Veeser M, Hofmann T, Roth R, Klöhr S, Rossaint R, Heesen M. Vasopressors for the management of hypotension after spinal anesthesia for elective caesarean section Systematic review and cumulative meta-analysis. Acta Anaesthesiol Scand. (2012) 56:810–6. doi: 10.1111/j.1399-6576.2011.02646.x
Keywords: cesarean delivery, neuraxial anesthesia, hemodynamics, vasopressor, lateral decubitus positioning
Citation: Wu S (2024) Potential differences in ephedrine requirements between left lateral and right lateral decubitus positions during neuraxial anesthesia for cesarean delivery. Front. Med. 11:1454681. doi: 10.3389/fmed.2024.1454681
Received: 25 June 2024; Accepted: 23 September 2024;
Published: 10 October 2024.
Edited by:
Jessian Munoz, Texas Children's Hospital, United StatesReviewed by:
Nishant Kumar, University of Delhi, IndiaCopyright © 2024 Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shanshan Wu, d3VtYTE5ODExOTgyQDE2My5jb20=
 Shanshan Wu
Shanshan Wu