- 1School of Nursing, Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
- 2School of Biological Sciences, Nanyang Technological University, Singapore, Singapore
- 3Department of Applied Social Sciences, The Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
- 4The Department of Rehabilitation Sciences, Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
- 5Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 6Intensive Care Unit, Shenzhen Traditional Chinese Medicine Hospital, Guangzhou University of Chinese Medicine, Shenzhen, China
Objective: To determine the comparative effects and safety of traditional Chinese medicine (TCM) interventions based on meridian theory for pain relief in patients with primary dysmenorrhea (PD).
Methods: This is a systematic review with network meta-analysis. Randomized controlled trials (RCTs) comparing meridian-based TCM interventions with waitlist, placebo, western medicine, and conventional therapies for PD pain. A SUCRA was used to estimate the probability ranking for the effects of interventions.
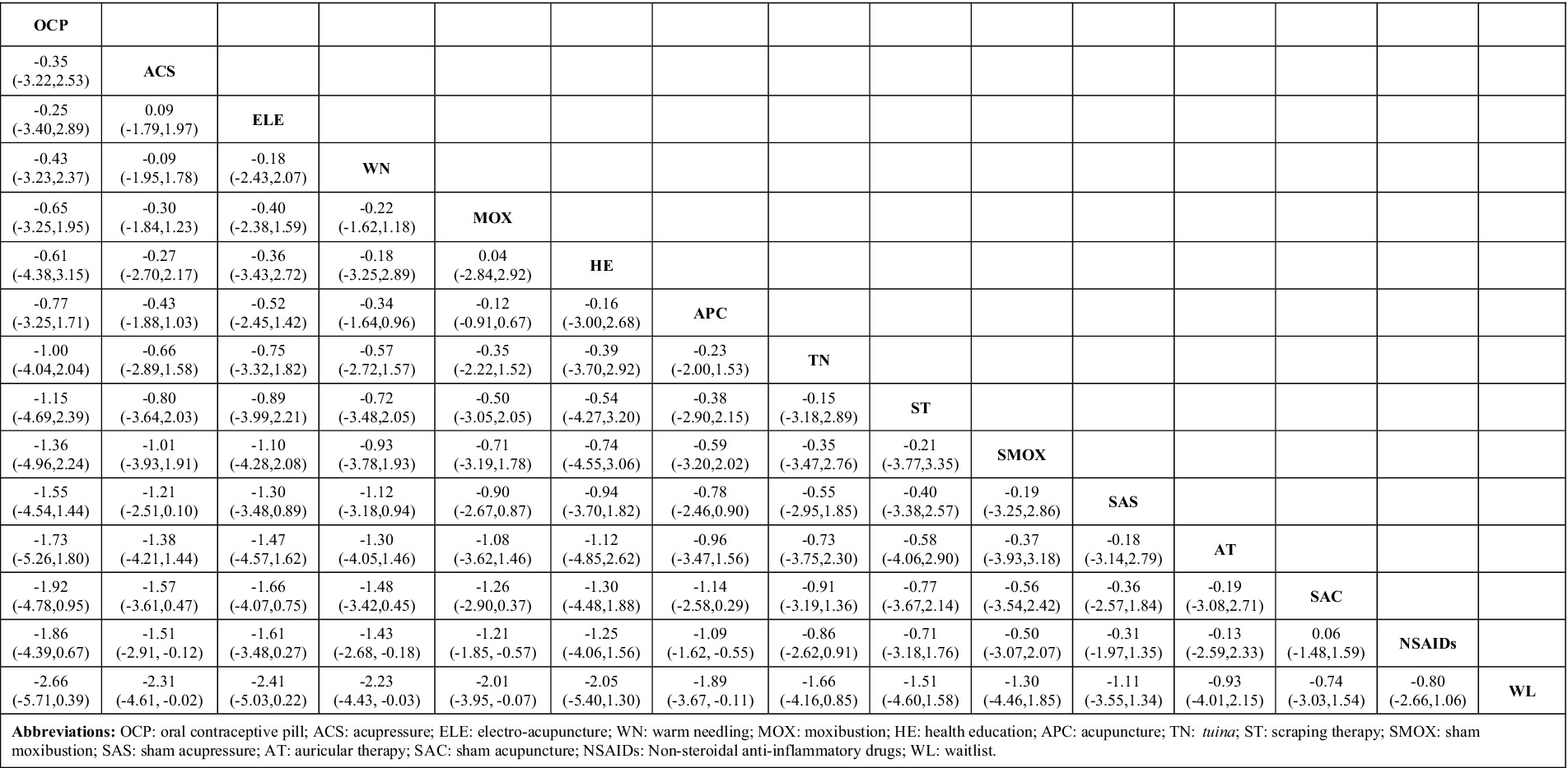
Results: 57 RCTs involving 3,903 participants and 15interventions were included. Thirty-two RCTs were rated as low risk of bias. A network diagram was drawn with 105 pairs of comparisons. Compared with NSAIDs and waitlist, significantly better effects were found in acupressure [SMD = −1.51, 95%CI (−2.91, −0.12)/SMD = −2.31, 95%CI (−4.61, −0.02)], warm needling [SMD = −1.43, 95%CI (−2.68, −0.18)/SMD = −2.23, 95%CI (−4.43, −0.03)], moxibustion [SMD = −1.21, 95%CI (−1.85, −0.57)/SMD = −2.10, 95%CI (−3.95, −0.07)], and acupuncture [SMD = −1.09, 95%CI (−1.62, −0.55)/SMD = −1.89, 95%CI (−3.67, −0.11)]. No adverse events were detected.
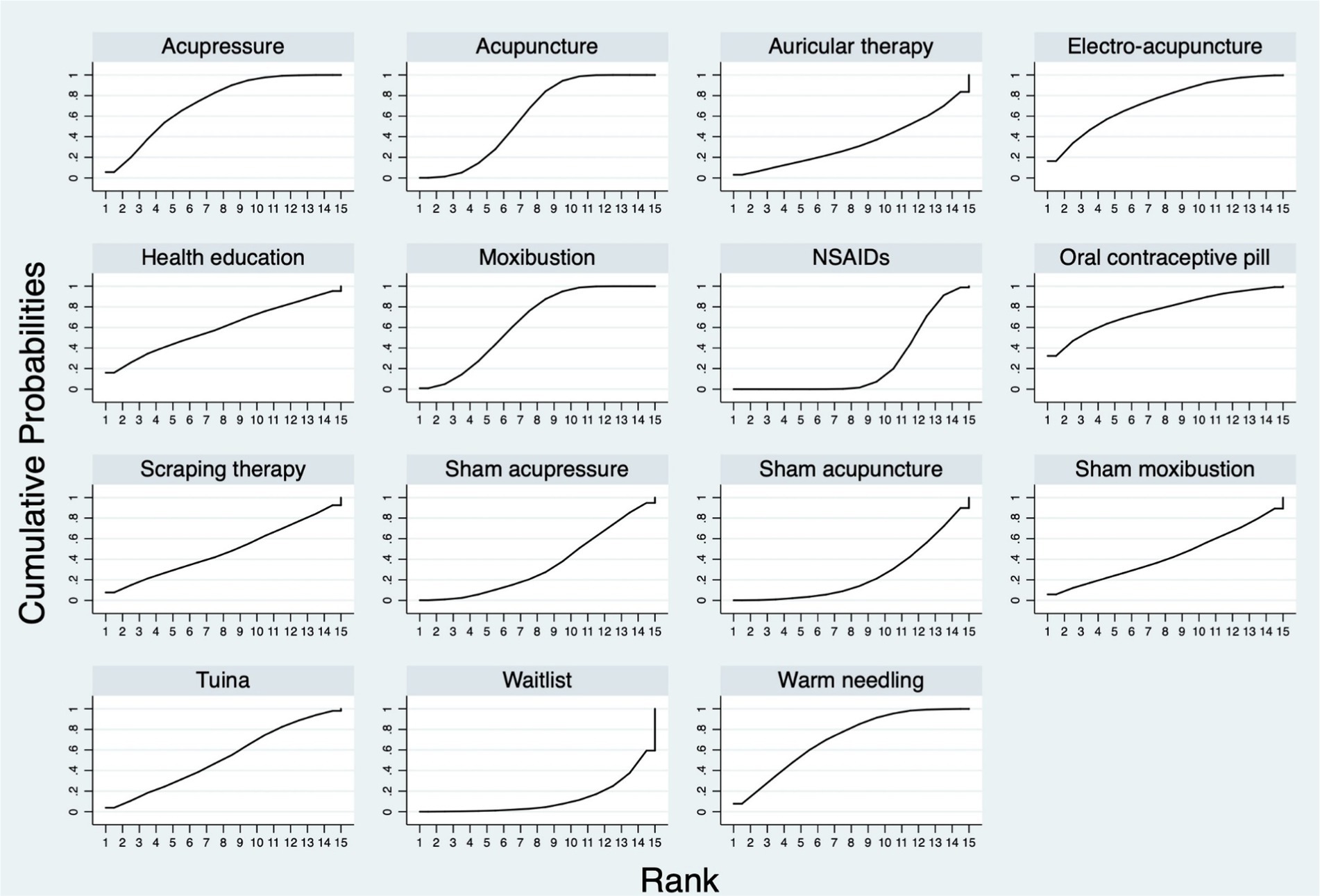
Conclusion: For PD pain, the effects of acupressure, acupuncture, warm needling, and moxibustion were superior to those of NSAIDs and waitlist. Oral contraceptive pill, electro-acupuncture, acupressure, and warm needling demonstrated higher probabilities of being better interventions. More high-quality clinical trials are needed to provide more robust evidence of this network.
Systematic review registration: PROSPERO CRD42022373312.
1 Introduction
Primary dysmenorrhea (PD) refers to the occurrence of menstrual cramps in the lower abdomen, without any identifiable pelvic pathology, with characteristic symptoms such as lower abdominal or pelvic pain, ranging from 8 h to 72 h and typically occurring at the onset of menstrual flow (1). Other associated symptoms include low back pain, headache, diarrhea, fatigue, nausea, or vomiting (2). The prevalence of PD varies from 50 to 90% (3). The exact causes remain unknown, leading to non-targeted treatments. Risk factors for PD include early age at menarche, heavy menstrual flow, nulliparity, family history of dysmenorrhea, and stress (4).
Systematic reviews and randomized controlled trials (RCTs) have shown that non-steroidal anti-inflammatory drugs (NSAIDs) (5, 6) and hormonal regulation through oral contraception (7) are significantly more effective for pain relief than placebo, and they are often used for symptom control (8). However, some women may not always find them effective or acceptable; for example, NSAIDs have undesirable side effects (6). Non-drug, non-surgical treatments for PD include transcutaneous electric nerve stimulation, behavior modification/relaxation, acupressure, acupuncture, spinal manipulation, topical heat, vitamin E, thiamine, fish oil, and herbal medicine (9). Only 26.7% of patients with PD have no experience with complementary and alternative medicine. Diet and homeopathy are the most frequently used methods from complementary and alternative medicine. In spite of the provision of information on efficacy, safety, and costs, patients choose methods based on earlier experience (10). Despite their popularity, evidence on the effectiveness of these nonpharmacologic therapies for PD is limited and inconsistent (11, 12).
Traditional Chinese medicine (TCM) interventions based on meridian theory can be an effective alternative approach for PD. Meridian is a system of conduits through which qi and blood circulate, connecting the bowels, viscera, extremities, superficial, organs, and tissues and making the body an organic whole. The meridian system includes 12 regular meridians, 8 extra meridians, 12 meridian divergence, 12 meridian sinews, 12 cutaneous vessels, and 15 collateral vessels (13). Meridian-based TCM interventions include acupuncture, acupressure, tuina, moxibustion, cupping, auricular therapy, electro-acupuncture, and scraping. These interventions may produce analgesic effects through the regulation of the hypothalamic–pituitary–ovarian axis, modulation of the immune system, and release of endogenous opioid peptides (14). Animal experiments have demonstrated that acupuncture may facilitate the release of central and peripheral neurotransmitters, modulation of immune function, and alleviation of uterine smooth muscle spasm (15, 16). Clinical trials have indicated that acupuncture may elicit analgesia by regulating serum levels of prostaglandins and ovarian hormones, facilitating the release of peripheral β-endorphin, improving the status of uterine artery blood flow, and alleviating uterine smooth muscle spasm (14). Similarly, moxibustion may modulate endocrine hormones, immune function, and nerve factors and enhance uterine microcirculation (17).
Numerous studies have investigated the efficacy of TCM interventions based on meridian theory for dysmenorrhea, including systematic reviews, RCTs, and case series. A systematic review of RCTs on acupuncture for PD reported that acupuncture provides superior pain relief (OR: 4.99; 95% CI: 2.82–8.82; 4 RCTs; I2 = 0%) and has fewer adverse events compared with NSAIDs (OR: 0.10; 95% CI: 0.02–0.44; 4 RCTs; I2 = 15%); however, evidence quality was low, and further research is needed to ascertain the effectiveness of acupuncture and acupressure (18). In an RCT of 152 subjects, moxibustion was found to have sustained and superior pain-relieving effects compared with drugs 3 months post-intervention (effect size: −0.87, 95% CI: −1.32 to −0.42, p < 0.001) measured by the visual analogue scale (VAS) (19). Acupressure on the SP6 meridian was found to be superior to placebo acupressure in relieving PD pain symptoms based on a VAS score (−4.935; 95% CI: [−15.757, 5.887]; p = 0.371) (20), whereas auricular therapy was found to be more effective than analgesics based on VAS scores (OR = 3.28, 95%CI: [1.37, 7.85], p = 0.008) (21). Although numerous studies have examined the effects of meridian-based TCM interventions for PD pain, no comparative analysis of their effectiveness has been conducted. Therefore, a comprehensive comparison of multiple TCM interventions based on meridian theory is required, as well as organization and collection of high-quality evidence.
Network meta-analysis (NMA) yields high-quality evidence, which can be used to evaluate the effects of multiple interventions and rank optimal intervention strategies (22). This study performed an NMA of RCTs on TCM interventions based on meridian theory for relieving pain in patients with PD, comparing the effects among interventions (TCM interventions based on meridian theory and eligible control interventions), and exploring the optimal one. The findings can provide evidence to help clinical workers and researchers understand the optimal protocol for pain management of PD.
2 Methods
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (18), the PRISMA-2020 guidelines (19), and the extension statement for network meta-analysis (PRISMA-NMA) (20). The protocol was registered on PROSPERO (CRD42022373312).
2.1 Selection criteria
Studies had to fulfill the following criteria presented in PICOS tools (population, intervention, comparators, outcomes, and study design): (1) population: patients diagnosed with PD; (2) intervention: meridian-based TCM interventions including acupressure, acupuncture, moxibustion, tuina, electroacupuncture, warm needling, auricular therapy, and scraping therapy (Interventions should be singly used, so that their effects can be detected. Interventions related to Chinese herb, staging acupoint catgut embedment therapy, acupuncture point injection therapy, or combined TCM intervention were excluded.); (3) comparators: control group with waitlist, placebo, western medicine (e.g., NSAIDs and combined oral contraceptives), conventional therapy, or another type of meridian-based TCM interventions (Studies comparing two or more meridian-based TCM interventions were included. Usual care was excluded due to the variety of care content among different interventions and study settings.); (4) outcomes: studies that evaluated pain intensity using VAS or numerical rating scale (NRS); and (5) study design: RCTs.
2.2 Search strategy
We searched Ovid MEDLINE, Embase, Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, Web of Science, Allied and Complementary Medicine, the China National Knowledge Infrastructure, Wanfang Data, PubMed, SinoMed, and CQVIP from database inception until 1 July 2023. The following keywords were used for our search: (massag* OR anmo OR acupress* OR tuina OR acupunct* OR electroacupunct* OR electro-acupunct* OR acupoint* OR meridia* OR auricular OR needl* OR moxibustion OR moxa) AND (dysmenorr* OR menstrua* pain OR period cramp OR period pain* OR menstrua* distress OR period distress OR menstrua* distress). To search the Chinese databases, we used the corresponding Chinese keywords. We did not impose any language restrictions (See Supplementary Appendix 1). We also scanned reference lists of relevant systematic reviews and clinical guidelines. Two authors (SCC and JYR) independently performed the literature search. Disagreements were resolved upon consultation and judgement by a third reviewer (WFY).
2.3 Data extraction
Two authors (SSC and LYP) independently screened the titles and abstracts of the retrieved studies, and the unrelated articles were removed. Thereafter, we reviewed the full texts of potentially relevant studies and extracted the data based on the selection criteria. The following data were extracted from the included RCTs in a predesigned data sheet: the first author’s name, publication year, characteristics of participants, sample size, diagnostic system, details of interventions, details of the control interventions, follow-up period, details of outcomes, and language. Basic information on the excluded studies was also extracted to provide a comprehensive reference to readers, with information on the original title, publication year, and reasons for exclusion. An additional reviewer (WFY) was consulted in the event of discrepancies between authors.
2.4 Quality assessment
Two authors (SCC and LYP) performed the quality evaluation of included studies independently in accordance with Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (21). The risk of bias for trials was assessed using criteria in the Cochrane Risk of Bias version 2 (RoB 2) tool. We assessed potential bias related to five domains, namely, randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each publication was identified as “high risk,” “low risk,” or “some concerns.” If there were any objections, they would be discussed or judged by a third researcher (WFY) to reach a consensus.
The GRADEpro Guideline Development Tool web page was employed to assess the evidence for the quality of outcome indicators including five degrading factors: risk of bias, inconsistency, indirectness, imprecision, and publication bias (23). On the basis of these variables, the software generates a GRADE rating of “high,” “moderate,” “low,” or “very low” to reflect the certainty of the reported effect. A summary of findings (SoF) table was generated for a given comparison of interventions to provide key information concerning the magnitudes of relative and absolute effects of the interventions examined, the amount of available evidence, and the quality of available evidence (21).
2.5 Statistical analysis
Standard mean difference (SMD) with a 95% confidence interval (CI) was used to estimate the effect sizes of NRS or VAS. Variation was expected between the original studies. To make the results more conservative, a random effects model was used rather than a fixed effects model. The statistical heterogeneity in each pairwise comparison was assessed using inconsistency index tests or Chi-square test or I2 statistic test (I2 > 30% or p-value <0.1 indicating inconsistency). Additionally, sensitivity analysis was conducted to verify the robustness of the results and test the source of heterogeneity in each RCT. Three-armed RCTs were transformed into two-armed pairs to clearly present the effects of comparisons. For the studies that reported the mean and standard deviation of effect changes in the interventions, we calculated the data at the endpoint of the intervention period using the current data.
An NMA with a Bayesian framework using Statistics and Data Science (STATA) software was conducted to assess the outcomes of different interventions (24). Network diagrams were used to present the results: (1) each node represents an exercise intervention; (2) the size of the node indicates the sample size of the subjects who performed this intervention; (3) if there are no line segments between each node, then indirect comparisons will be made between the nodes; if there are line segments, then direct comparisons will be made between the nodes; (4) the thickness of the line segments between the nodes indicates the original study sample size; and (5) the size of the nodes and the thickness of the line segments are positively correlated with the number (25). The surface under the cumulative ranking curve (SUCRA) is the probability each intervention has of being among the best of those in the network; the SUCRA values range from 0 to 1, with large values representing high intervention ranking probabilities (26). NMA results were visualized using forest plots. A funnel plot was generated to examine possible publication bias.
3 Results
3.1 Literature search
Our search yielded a total of 3,080 potentially eligible citations, among which 704 remained after the removal of duplicates and irrelevant records. Of the remaining citations, 86 studies were obtained by reading the titles and abstracts. After the full text of these records was screened, 57 studies were included for network analysis. The PRISMA flow diagram describing the inclusion process is presented in Figure 1. Supplementary Appendix 2 shows the details of the excluded studies from full-text screening.
3.2 Description of included studies
As shown in Table 1, the included 57 RCTs were published between 2011 and 2022 and included 3,903 participants. The included participants’ age ranged from 14 years to 39 years. The sample size of the included RCTs was from 20 to 208. Besides the eligibility on age, disease duration, and intervention use records, most RCTs screened and included participants by using pain rating scales (57 studies), including VAS and NRS. Eight types of meridian-based TCM interventions were reported among the included RCTs, namely, acupuncture (n = 865) (31, 32, 35–37, 41, 44, 46, 50–56, 58, 62–65, 68, 70), acupressure (n = 285) (27, 28, 30, 33, 34, 71, 72, 79), auricular therapy (n = 35) (57), electro-acupuncture (n = 66) (34, 47), moxibustion (n = 651) (29, 38–40, 42–44, 48–50, 61, 62, 66, 67, 74, 77), scraping therapy (n = 30) (69), tuina (n = 57) (45, 54), and warm needling (n = 151) (41, 59, 60, 78). The most commonly involved meridians included conception vessel (CV), spleen meridian (SP), stomach meridian (ST), and governor vessel (GV). Four types of control interventions were reported, namely, health education (27), waitlist (35, 81), placebo (sham interventions) (28–30, 32, 33, 56, 72, 82), and conventional medicine (oral contraceptive pill and NSAIDs) (31, 36–40, 42, 43, 45–49, 51–53, 55, 57–61, 63–71, 73–80, 83). Pain outcome measures included VAS and NRS. One RCT used both VAS and NRS (29), 3 used NRS only (36, 59, 69), and the other 53 used VAS only. The treatment period ranged from 30 min to 3 months, and the follow-up period ranged from 3 h to 6 months. Twelve RCTs were published in English and 45 were in Chinese.
3.3 Risk of bias
Figure 2 presents a summary of the methodological quality of the included studies. Thirty-two RCTs were rated as low risk of bias (28, 31, 33, 34, 36, 39–43, 46, 47, 49, 51, 56, 59, 61–66). Nineteen studies were rated as high risk of bias due to the application of inappropriate data analysis methods (27, 29, 30, 32, 45, 48, 50, 54, 55, 57, 58, 60, 68, 71, 72, 81, 83) or unblinding of the outcome assessors (35, 81). The remaining six studies were rated as having certain concerns because of the insufficient information on data analysis methods (37, 38, 44, 52, 53, 77) or the high dropout rate (57, 75).
3.4 Network diagram
A network diagram was drawn based on 15 interventions, including 3,903 participants. A total of 105 pairs of comparisons were formed (including 18 pairs of direct comparisons and 87 pairs of indirect comparisons). Nineteen RCTs reported a comparison between acupuncture and NSAIDs, and 12 RCTs reported the comparison between moxibustion and NSAIDs. Direct comparisons between 9 pairs of comparisons occurred only once. Among these interventions, NSAIDs had the largest sample size (n = 1,426), followed by acupuncture (n = 865), moxibustion (n = 651), and warm needling (n = 151). The data are shown in Figure 3. (Supplementary Appendix 3).
3.5 Heterogeneity and inconsistency test
Conceptual heterogeneity and inconsistency were low across the network given that all the included studies had the same study design, participants, and outcomes. Statistical heterogeneity was high in several pairwise comparisons (Supplementary Appendix 4). Supplementary Appendix 5 shows the detailed information on the local inconsistency test. A node-splitting test was conducted for local inconsistency analysis, and 19 pairs of mixed comparisons (including direct and indirect) were analyzed. The results showed no statistical inconsistency in each pair of direct comparison. Sensitivity analysis indicated that the findings were robust (Supplementary Appendix 6).
3.6 NMA
As shown in Figure 4, the estimated effect of the NMA for each intervention on relieving PD pain was generated. Compared with NSAIDs and waitlist, significantly better effects were found in acupressure [SMD = −1.51, 95% CI (−2.91, −0.12)/SMD = −2.31, 95% CI (−4.61, −0.02)], warm needling [SMD = −1.43, 95% CI (−2.68, −0.18)/SMD = −2.23, 95% CI (−4.43, −0.03)], moxibustion [SMD = −1.21, 95% CI (−1.85, −0.57)/SMD = −2.10, 95% CI (−3.95, −0.07)], and acupuncture [SMD = −1.09, 95% CI (−1.62, −0.55)/SMD = −1.89, 95% CI (−3.67, −0.11)].
3.7 Probability ranking
Figure 5 shows the SUCRA probability ranking for the different treatment effects of all interventions. For the 15 interventions, the SUCRA value predicted the possibility of different interventions as the best treatment on the management of PD pain, and the ranking was as follows: oral contraceptive pill (75.8%), electro-acupuncture (73.0%), acupressure (72.9%), warm needling (70.6%), moxibustion (64.9%), acupuncture (60.0%), health education (59.7%), tuina (52.3%), scarping therapy (48.0%), sham moxibustion (43.1%), sham acupressure (34.8%), auricular therapy (34.1%), sham acupuncture (24.9%), NSAIDs (23.9%), and waitlist (12.1%).
3.8 Safety
Information on the safety of different interventions was collected and assessed based on adverse events reported in RCTs. Nineteen RCTs reported adverse events on acupuncture, warm needling, NSAIDs, and sham acupressure. For acupuncture and warm needling, adverse events included local bleeding or hematoncus (8 RCTs) (36, 37, 51, 53, 58, 60, 68, 73), headache or myalgia (1 RCT) (36), fever (1 RCT) (36), nausea (1 RCT) (46), and nervousness in the first treatment session (1 RCT) (71). Adverse events of NSAIDs incorporated gastrointestinal symptoms (13 RCTs) (36, 37, 46, 48, 51–53, 65, 68, 69, 73, 75, 83), vaginal bleeding (1 RCT) (36), weight gain (1 RCT) (36), breast engorgement (1 RCT) (36), hypermenorrhea (1 RCT) (48), rash (1 RCT) (52), and dizziness and tinnitus (3 RCTs) (68, 73, 83). An RCT also reported that the analgesic effect of medication faded away with repetitive use in some cases (31). An RCT mentioned that 3 participants dropped out from the sham acupressure control group due to severe pain (30, 72), whereas another RCT reported that 2 participants dropped out from the sham acupressure group without providing the specific reasons (30). Details on the adverse events of the interventions are in Supplementary Appendix 7.
3.9 Certainty of evidence
The evidence quality of all 18 comparisons was evaluated by GRADEpro. High-quality evidence was found in two comparisons on PD pain symptoms, namely, acupuncture versus placebo and electroacupuncture versus NSAIDs. The evidence quality was evaluated as moderate in six comparisons: acupressure versus placebo, moxibustion versus NSAIDs, moxibustion versus acupuncture, tunia versus acupuncture, warm needling versus NSAIDs, and scraping therapy versus NSAIDs. The evidence quality of the rest of the 10 comparisons was evaluated as low or very low. The most common reason for downgrading the evidence quality was imprecision, followed by high heterogeneity and high risk of bias. Details of the SoF table are in Supplementary Appendix 8.
3.10 Publication bias
The publication bias is shown in Appendix 9. The results showed that the studies were roughly symmetrical around the center line. Egger’s test (p = 0.162) showed no significant risk of publication bias as well.
4 Discussion
Numerous clinical trials and systematic reviews have investigated the effects of meridian-based TCM interventions for PD pain and suggested that these interventions can reduce PD pain intensity, duration, and related symptoms, with relatively few adverse events. However, this work is the first study to quantitatively summarize and compare the effects of the meridian-based TCM interventions via NMA. In PD pain management, the effects of acupressure, acupuncture, and moxibustion were superior to those of NSAIDs and waitlist; acupressure was more effective than placebo; and warm needling was superior to both NSAIDs and waitlist.
Previous reviews have evaluated the effects of meridian-based TCM interventions for PD pain and found similar results to this study. A systematic review of acupuncture-related therapies (acupuncture, acupoint injection, acupressure, and moxibustion) for PD indicated that acupuncture was significantly more effective than placebo (WMD = −0.57, 95% CI [−0.76, −0.38]) and NSAIDs (WMD = −0.19, 95% CI [−0.37, −0.01]) in PD pain management, and acupressure was more effective than placebo (WMD = −0.91, 95% CI [−1.78, −0.04]). Nevertheless, the reliability of their review may be compromised because it included a combination of randomized and non-randomized trials with fewer interventions, trials, and comparisons. Moreover, most of the studies included were deemed low in methodology (84). Another systematic review on the effects and safety of acupuncture and moxibustion for PD demonstrated that acupuncture (MD = −1.93; 95% CI [−2.80, −1.06]) and moxibustion (MD = −2.67; 95% CI [−4.96, −0.38]) are more effective in managing PD pain than the control via VAS; however, the review combined all control interventions as one for their meta-analysis (85). Similarly, Jiang et al. conducted a systematic review of RCTs on acupressure for PD and reported that acupressure is better at improving pain with VAS compared with placebo or waitlist (MD: −1.41, 95% CI [−1.61, −1.21]), but the study found no difference in pain relief between acupressure and NSAIDs. This discrepancy may be due to the small number of RCTs with modest sample included, which hindered the detection of treatment effects in their systematic review (86). The present study’s findings suggested that electroacupuncture may be an optimal intervention strategy for PD pain; however, direct comparisons among interventions were few based on a limited number of studies.
For safety issues, the current study provided evidence that meridian-based TCM interventions are safe with no severe adverse events for the treatment of PD, and the reported adverse events focused on acupuncture and warm needling. These results were in accordance with previous studies (33, 84, 85). Fainting, hematoma or bleeding, sticking of needle, and needling sensation after acupuncture are common situations during acupuncture treatment in clinics or research (87). These situations might be related to irregular acupressure practice of practitioners, participants’ mental and physical conditions, and participant–practitioner interactions (88). All the abovementioned adverse events are mild and can be handled well under appropriate management. A systematic review examining the adverse events of meridian-based TCM interventions between 2000 and 2011 (117 studies, 25 countries, and 294 cases with adverse events in acupuncture) emphasized the significance of acupuncture practice guidelines (89). Therefore, to minimize adverse events, practitioners should strictly follow the operation guidelines, observe the situation of patients, and communicate with them actively during acupuncture treatment. Standard reporting form can be adopted in future studies to systematically document the occurrence and severity of AE (90).
The good statistical consistency observed in the NMA suggested that the variation in the treatment effects of the meridian-based TCM interventions is predictable and not due to chance (91). However, the statistical heterogeneity in the pairwise comparisons within the NMA is high. Several appropriate statistical methods were applied to identify the sources of heterogeneity. Sensitivity analysis indicated the robustness of the overall results of the meta-analysis (92). Publication bias was suggested from the funnel plot and Egger’s test. Considering that the overall methodological quality of the included studies was high, the high statistical heterogeneity observed in the pairwise comparisons could be attributed to the variability in sample size or the different durations of intervention among various studies (93). The heterogeneity may also arise from differences in demographic characteristic of participants with PD among the study populations (94). Future systematic reviews may limit the age range of the participants, define the optimal information size (for example, 400 as suggested by GRADEpro handbook) (95), and set the treatment duration and frequency. Special attention should be paid to the clinical trials with a large effect size but a small sample size (96, 97).
For the quality of methodology of the included studies, factors that led to high risk of bias included the application of inappropriate data analysis methods, unblinding of the outcome assessors, insufficient information on data analysis methods, and high dropout rate. The factors that rated down the evidence quality of this study by GRADEpro contained imprecision, high heterogeneity, and risk of bias. Further RCTs should give particular emphasis on these several domains, applying the intention-to-treat approach for data analysis to eliminate or reduce bias in treatment effects arising from missing data (98), blinging the outcome assessors to reduce detection bias (99), reporting the results completely to avoid selective reporting bias (e.g., selective outcome reporting, selective analysis reporting, and lack of reporting of adverse events and dropout reasons) (100), and making sure that the sample size has the power to demonstrate the smallest effect of intervention (101).
4.1 Implication
The findings of this study can implicate PD patients, healthcare providers, researchers, and policy makers. The study provides a potential ranking of the effects of multiple interventions (e.g., meridian-based TCM interventions and conventional western medicine) for relieving PD pain, as well as their adverse events. The information could be a reference for PD patients when choosing interventions. Health care providers may use the findings to inform their clinical decisions and improve patient outcomes. Researchers may find some research gaps from the findings. For example, the results indicated that acupressure, moxibustion, and warm needling may also have significant effects on PD pain, but relevant evidence is very limited. More clinical trials can be conducted to examine their effects on PD pain management. Researchers could further explore the effects of meridian-based TCM interventions on other outcomes in patients with PD. Policy makers in the field of women’s health may focus on the safety and potential effects of meridian-based TCM interventions and highlight the importance of integrating these interventions into clinical practice guidelines and health care policies.
4.2 Strength
The present study has several strengths. First, the study strictly defined the inclusion criteria, and the overall methodological quality of the included studies was high. Second, we limited the outcome as PD pain, providing a clear and specific research question that allowed for a focused assessment of the current evidence. Third, evidence of both effects and adverse events was collected, enabling readers to obtain knowledge of meridian-based TCM interventions on PD pain. Additionally, the review included studies published in both English and Chinese, which increased the generalizability of the findings and avoided potential language bias.
4.3 Limitation
Several limitations of this study should be acknowledged. First, as a result of the diversity of intervention types, the number of studies using the same interventions in some direct comparisons was relatively small. Besides, the duration of the interventions varied across the included studies, which may affect the effects of the interventions. These factors may subsequently influence the reliability of the findings. Second, the study only focused on the severity of PD pain as the sole outcome. Evidence on the effects of meridian-related interventions on other associated symptoms such as menstrual blood flow, sleep quality, and mood was not reviewed. Lastly, the statistical heterogeneity observed among different comparisons was high, suggesting the presence of substantial variability in the results and limiting the generalizability of the findings.
5 Conclusion
For the management of PD pain, the effects of acupressure, acupuncture, warm needling, and moxibustion were superior to those of NSAIDs and waitlist. Furthermore, based on probability ranking, oral contraceptive pill, electro-acupuncture, acupressure, and warm needling demonstrated higher probabilities of being better interventions. Meridian-based TCM interventions are safe, and no severe related adverse events were detected. More high-quality clinical trials are needed to provide more robust evidence of this NMA.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
S-CC: Conceptualization, Formal analysis, Methodology, Writing – original draft. J-YR: Methodology, Writing – review & editing. BZ: Formal analysis, Writing – original draft. L-YP: Formal analysis, Writing – original draft. LZ: Writing – review & editing. S-LL: Formal analysis, Writing – original draft. K-PW: Writing – review & editing. H-XO: Writing – review & editing. W-FY: Writing – review & editing. Q-WF: Conceptualization, Writing – review & editing. B-QC: Writing – review & editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1453609/full#supplementary-material
References
1. Dawood, MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstetr Gynecol. (2006) 108:428–41. doi: 10.1097/01.AOG.0000230214.26638.0c
2. Proctor, M, and Farquhar, C. Diagnosis and management of dysmenorrhoea. BMJ. (2006) 332:1134–8. doi: 10.1136/bmj.332.7550.1134
3. Polat, A, Celik, H, Gurates, B, Kaya, D, Nalbant, M, Kavak, E, et al. Prevalence of primary dysmenorrhea in young adult female university students. Arch Gynecol Obstet. (2009) 279:527–32. doi: 10.1007/s00404-008-0750-0
4. Akshatha, K, and Shilpa, D. Dysmenorrhoea. Obst Gynaecol Reprod Med. (2019) 29:286–91. doi: 10.1016/j.ogrm.2019.06.002
5. Daniels, S, Robbins, J, West, CR, and Nemeth, MA. Celecoxib in the treatment of primary dysmenorrhea: results from two randomized, double-blind, active- and placebo-controlled, crossover studies. Clin Ther. (2009) 31:1192–208. doi: 10.1016/j.clinthera.2009.06.003
6. Marjoribanks, J, Proctor, ML, and Farquhar, C. Nonsteroidal anti-inflammatory drugs for primary dysmenorrhoea. Cochrane Database Syst Rev. (2003) 4:CD001751. doi: 10.1002/14651858.CD001751
7. Wong, CL, Farquhar, C, Roberts, H, Proctor, M, and Wong, CL. Oral contraceptive pill for primary dysmenorrhoea. Cochrane Database Syst Rev. (2009) 2010:CD002120–CD20. doi: 10.1002/14651858.CD002120.pub3
8. Vercellini, P, Viganò, P, and Somigliana, E. The role of the levonorgestrel-releasing intrauterine device in the management of symptomatic endometriosis. Curr Opin Obstet Gynecol. (2005) 17:359–65. doi: 10.1097/01.gco.0000175353.03061.7f
9. Khan, KS, Champaneria, R, and Latthe, PM. How effective are non-drug, non-surgical treatments for primary dysmenorrhoea? BMJ. (2012) 344:e3011. doi: 10.1136/bmj.e3011
10. Munstedt, K, and Riepen, T. Patients' decisions regarding the treatment of primary dysmenorrhoea. Complement Ther Med. (2019) 45:1–6. doi: 10.1016/j.ctim.2019.05.016
11. Proctor, ML, Murphy, PA, Pattison, HM, Suckling, J, and Farquhar, CM. Behavioural interventions for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev. (2007) 3:CD002248. doi: 10.1002/14651858.CD002248.pub3
12. Osayande, AS, and Mehulic, S. Diagnosis and initial management of dysmenorrhea. Am Fam Physician. (2014) 89:341–6.
13. World Health Organization. Regional Office for the Western Pacific. WHO international standard terminologies on traditional medicine in the Western Pacific Region WHO Regional Office for the Western Pacific (2007). Available at: https://iris.who.int/handle/10665/206952 (Accessed August, 2024).
14. Song, QY, Zhou, YL, Zhou, B, Chen, XY, Zhang, RY, and Chen, YJ. Study progress on the mechanism of acupuncture for primary dysmenorrhea. World J Acupunct Moxibustion. (2021) 313:227–32. doi: 10.1016/j.wjam.2021.05.016
15. Qin, Y, Guo, MW, Lan, Y, Wang, YF, Wang, S, Ji, MX, et al. Effect of electroacupuncture of "Hegu" (LI4) and "Zusanli" (ST36) on intestinal sensitivity and motility in irritable bowel syndrome rats. Zhen Ci Yan Jiu. (2020) 45:293–8. doi: 10.13702/j.1000-0607.190743
16. Qin, ZY, Ling, H, Xia, XH, Meng, L, and Wu, ZJ. Effects of electroacupuncture of Sanyinjiao (SP 6) on genito-endocrine in patients with perimenopausal syndrome. Zhen Ci Yan Jiu. (2007) 32:255–9.
17. Pan, S, Wang, S, Li, J, Yuan, H, Xue, X, Liu, Y, et al. Moxibustion for primary dysmenorrhea: an adjuvant therapy for pain relief. Evid Based Complement Alternat Med. (2022) 2022:1–14. doi: 10.1155/2022/6864195
18. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DGPRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. Ann Intern Med. (2009) 151:264–69. doi: 10.1136/bmj.b2535
19. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. (2021) 134:103–12. doi: 10.1016/j.jclinepi.2021.02.003
20. Chen, MN, Chien, LW, and Liu, CF. Acupuncture or acupressure at the sanyinjiao (sp6) acupoint for the treatment of primary dysmenorrhea: A meta-analysis. Evid Based Complement Alternat Med. (2013) 2013:493038. doi: 10.1155/2013/493038
21. Kong, X, Fang, H, Li, X, Zhang, Y, and Guo, Y. Effects of auricular acupressure on dysmenorrhea: A systematic review and meta-analysis of randomized controlled trials. Front Endocrinol (Lausanne). (2023) 5:1016222. doi: 10.3389/fendo.2022.1016222
22. Higgins, JPT, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, MJ, et al. (eds.). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). (2023). Available from www.training.cochrane.org/handbook (Accessed August, 2024).
23. Guyatt, GH, Oxman, AD, Kunz, R, Vist, GE, Falck-Ytter, Y, Schünemann, HJ, et al. Rating quality of evidence and strength of recommendations: what is "quality of evidence" and why is it important to clinicians? BMJ. (2008) 336:995–8. doi: 10.1136/bmj.39490.551019.BE
24. van Valkenhoef, G, Lu, G, de Brock, B, Hillege, H, Ades, AE, and Welton, NJ. Automating network meta-analysis. Res Synth Methods. (2012) 3:285–99. doi: 10.1002/jrsm.1054
25. Chaimani, A, Higgins, JPT, Mavridis, D, Spyridonos, P, and Salanti, G. Graphical tools for network meta-analysis in STATA. PLoS One. (2013) 8:e76654. doi: 10.1371/journal.pone.0076654
26. Salanti, G, Ades, A, and Ioannidis, JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
27. Chen, HM, Wang, HH, Chiu, MH, and Hu, HM. Effects of acupressure on menstrual distress and low back pain in dysmenorrheic young adult women: an experimental study. Pain Manag Nurs. (2015) 16:188–97. doi: 10.1016/j.pmn.2014.06.002
28. Dincer, Y, and Oskay, U. The Effect of Acupressure Applied to Sanyinjiao (SP6) on Primary Dysmenorrhea. Altern Ther Health Med. (2023) 29:16–22.
29. Gao, J, Wang, Q, Xian, S, Feng, YM, Cao, WX, Ye, JY, et al. The effect of moxibustion on alleviating menstrual pain in a population of young nursing students: a prospective randomized cross-over pilot study. Complement Ther Med. (2015) 23:773–81. doi: 10.1016/j.ctim.2015.08.005
30. Kashefi, F, Ziyadlou, S, Khajehei, M, Ashraf, AR, Reza Fadaee, A, and Jafari, P. Effect of acupressure at the Sanyinjiao point on primary dysmenorrhea: a randomized controlled trial. Complement Ther Clin Pract. (2010) 16:198–202. doi: 10.1016/j.ctcp.2010.04.003
31. Kiran, G, Gumusalan, Y, Ekerbicer, HC, Kiran, H, Coskun, A, and Arikan, DC. A randomized pilot study of acupuncture treatment for primary dysmenorrhea. Eur J Obstet Gynecol Reprod Biol. (2013) 169:292–5. doi: 10.1016/j.ejogrb.2013.02.016
32. Liu, LY, Li, X, Tian, ZL, Zhang, Q, Shen, ZF, Wei, W, et al. Acupuncture modulates the frequency-specific functional connectivity density in primary dysmenorrhea. Front Neurosci. (2022) 16:1–12. doi: 10.3389/fnins.2022.917721
33. Mirbagher-Ajorpaz, N, Adib-Hajbaghery, M, and Mosaebi, F. The effects of acupressure on primary dysmenorrhea: a randomized controlled trial. Complement Ther Clin Pract. (2011) 17:33–6. doi: 10.1016/j.ctcp.2010.06.005
34. Qorbanalipour, K, Ghaderi, F, and Jafarabadi, MA. Comparison of the effects of acupressure and electroacupuncture in primary dysmenorrhea: a randomized controlled trial. Int J Women’s Health Reprod Sci. (2018) 6:471–6. doi: 10.15296/ijwhr.2018.78
35. Shetty, GB, Shetty, B, and Mooventhan, A. Efficacy of acupuncture in the Management of Primary Dysmenorrhea: a randomized controlled trial. JAMS J Acupuncture Meridian Stud. (2018) 11:153–8. doi: 10.1016/j.jams.2018.04.001
36. Sriprasert, I, Suerungruang, S, Athilarp, P, Matanasarawoot, A, and Teekachunhatean, S. Efficacy of acupuncture versus combined Oral contraceptive pill in treatment of moderate-to-severe dysmenorrhea: a randomized controlled trial. Evidence-based complement Alt Med. (2015) 2015:1–10. doi: 10.1155/2015/735690
37. Wang, H, Cao, Y, Jin, X, Yan, M, Wang, J, Li, R, et al. Effect of an acupuncture technique of penetrating through zhibian (BL54) to shuidao (ST28) with long needle for pain relief in patients with primary dysmenorrhea: a randomized controlled trial. Pain Res Manag. (2019) 2019:7978180. doi: 10.1155/2019/7978180
38. Yang, M, Chen, X, Bo, L, Lao, L, Chen, J, Yu, S, et al. Moxibustion for pain relief in patients with primary dysmenorrhea: a randomized controlled trial. PLoS One. (2017) 12:e0170952. doi: 10.1371/journal.pone.0170952
39. Ding, LP, Liu, H, and Hu, XW. Effect of mixed Moxibustion on pain and serum hormone levels of primary dysmenorrhea of cold coagulation and stasis type (in Chinese). Chin Med Mod Dist Educ China. (2021) 19:59–61. doi: 10.3969/j.issn.1672-2779.2021.07.023
40. Wan, KM, Huang, H, Gen, LL, Tang, LM, Hu, XW, Zhou, GX, et al. Clinical observation of long snake-like moxibustion in treating primary dysmenonrrheal with deficiency of qi and blood (in Chinese). Chinese Medicine Moderen Distance Education of China. (2022) 20:131–33. doi: 10.3969/j.issn.1672-2779.2022.04.051
41. Liu, XP. Observation on treating primary dysmenorrhea of the hanshi ningzhi type by warm acupuncture at bl32 (in Chinese). Clin J Chin Med. (2019) 11:108–10. doi: 10.3969/j.issn.1674-7860.2019.08.042
42. Liu, Y, and Li, Y. Evaluation on clinical efficacy of spaced ginger moxibustion for primary dysmenorrhea with colddamp stagnation (in Chinese). Mod J Integ Trad Chin Western Med. (2018) 27:850–2. doi: 10.3969/j.issn.1008-849.2018.08.015
43. Ye, ZY. Observation of clinical efficacy of heat-sensitive ginger-partitioned moxibustion in the treatment of cold blood stasis type of dysmenorrhea (in Chinese) [master’s thesis]. Jiangxi, China: Jiangxi University of Chinese Medicine. (2022)
44. Wu, F. Clinical observation on ginger-isolated moxibustion treatment with primary dysmenorrhea casued by cold and blood stagnation (in Chinese) [master’s thesis]. Sichuan, China: Chengdu University of Traditional Chinese Medicine. (2009).
45. Tang, N. The clinical observation of immediate analgesic effect of choropractic thearpy to the patients of congestive primary dysmenorrhea (in Chinese) [master’s thesis]. Shandong, China: Shandong University of Traditional Chinese Medicine. (2012).
46. Chang, JY, Long, DH, Yu, X, and Zhang, L. Effect of periodic acupuncture and moxibustion on the pain degree frequency and symptoms of patients with primary dysmenorrhea with cold coagulation and blood stasis (in Chinese). World Journal of Integrated Traditional and Western Medicine (2020) 15:1315–18. doi: 10.13935/j.cnki.sjzx.200731
47. Zhang, Y. Clinical reserach of electro-acupuncture in treatment of primary dysmenorrhea (in chinese). Journal of Hunei University of Chinese Medicine (2017) 19:80–82. doi: 10.3969/j.issn.1008-987x.2017.06.21
48. Zhang, WW, Wang, L, and Qu, L. Clinical observation of moxibustion with immediate effect in treating primary dysmenorrhea (in chinese). Journal of Guangzhou University of Traditional Chinese Medicine. (2020) 37:1091–94. doi: 10.13359/j.cnki.gzxbtcm.2020.06.018
49. Zhang, YH. The study of thunder-fire moxibustion in treating primary dysmenorrhea of cold-coagulation-stasis type (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University of Chinese Medicine. (2019).
50. Zhang, HZ. Clinical study of moxibustion on baliao point in treating primary dysmenorrhea with cold coagulation and blood stasis type (in Chinese) [master’s thesis]. Shandong, China: Shandong University of Traditional Chinese Medicine. (2020).
51. Peng, MH. Clinical observation on treating primary dysmenorrhea by acupuncture xi acupoints of three foot yin meridians (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University of Chinese Medicine. (2012).
52. Cao, Y. Acupuncture clinical analysis of primary dysmenorrhea (in Chinese) [master’s thesis]. Heilongjiang, China: Heilongjiang University of Chinese Medicine. (2011).
53. Cao, YX. The clinical research about primay dysmenorrhea treated by penetrating method from zhibian (b54) to shuidao (st28) (in Chinese) [master’s thesis]. Shanxi, China: Shanxi University of Chinese Medicine. (2014).
54. Zhu, L. Clinical observation on the treatment of dysmenorrhea caused by cold coagulation and blood stasis by wenjing tongluo massage technique (in Chinese) [master thesis]. Yunnan, China: Yunnan University of Chinese Medicine. (2020).
55. Zhu, Y. The clinical effect to primary dysmenorrhoea with adominal acupuncture (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University of Chinese Medicine. (2015).
56. Li, H. To study the functional regions of acupuncture at sanyinjiao(sp6) treatment on primary dysmenorrhea (in Chinese) [master’s thesis]. Henan, China: Henan University of Chinese Medicine. (2014).
57. Li, Z, Qu, JH, Wang, YZ, Ma, XP, Song, XL, Li, JC, et al. Efficacy of press needles to the auricular point in treating primary dysmenorrhea of air force women soldiers (in Chinese). Med J of Air Force (2017) 33:306–07+42.
58. Lin, LX. Clinical obervation on treatment of primary dysmenorrhea of cold coagulation and blood stasis type with filiform-fire needle (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University of Chinese Medicine. (2019).
59. Lin, WM, Wu, JS, and Lin, LX. Observation on the therapeutic effect of warm acupuncture on primary dysmenorrhea (in Chinese). Chinese and Foreign Medical Research. (2020) 18:124–26. doi: 10.14033/j.cnki.cfmr.2020.16.050
60. Lin, GH. Clinical observation on treatment of primary dysmenorrhea of cold congealing and blood stasis type by warming acupuncture and moxibustion on 17 vertebrae (in Chinese) [master’s thesis]. Fujian, China: Fujian Univeristy of Traditional Chinese Medicine. (2020).
61. Liang, RF. Clinical observation and mechanism of treating primary dysmenorrhea with qijiao moxibustion (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University Of Chinese Medicine. (2021).
62. Fan, CH. Ginger moxibustion treatment of blood stasis type of dysmenorrhea haemorrhealogical nature of clinical research (in Chinese) [doctoral thesis]. Guangdong, China: Guangzhou University Of Chinese Medicine. (2014).
63. Tang, XM, and Liu, XC. The acupuncture in the treatment of primary dysmenorrhea for 30 cases. Chin Med Mod Dist Educ China. (2015) 13:83–84. doi: 10.3969/j.issn.1672-2779.2015.22.045
64. Wen, SQ. Clinical observation on the treatment of primary dysmenorrhea with qi stagnation and blood stasis based on the principle of “the liver is the precondition for women” (in Chinese) [master’s thesis]. Liaoning, China: Liaoning University of Traditional Chinese Medicine. (2021).
65. Wang, DF. Clinical study of treatment in primary dysmenorrhea by abdominal acupuncture (in Chinese) [master’s thesis]. Guangxi, China: Guangxi University of Chinese Medicine (2019).
66. Wang, LY, and Chen, HP. Clinical observation of 60 cases of primary dysmenorrhea treated with wheat-grain size cone moxibustion (in Chinese). J Chin Med. (2018) 50:174–76. doi: 10.13457/j.cnki.jncm.2018.07.052
67. Bai, MP, Yang, YF, Lao, JX, Li, ZY, and Chen, SG. Clinical efficacy of heavy moxibustion at the eight acupoints in the treatment of cold-damp stagnation type of moderate to severe primary dysmenorrhea (in Chinese). J Emerg Tradit Chin Med. (2018) 11:2026–28. doi: 10.3969/j.issn.1004-745X.2018.11.043
68. Sheng, ML. Clinical effect of acupuncure on primary dysmenorrhea: A randomized, controlled trial (in Chinese) [master’s thesis]. Heilongjiang, China: Heilongjiang University of Chinese Medicine. (2019).
69. Shi, AD. Clinical study on the treatment of primary dysmenorrhea with cold dampness syndrome by holographic meridian copper-bian scraping method and its influence on prostaglandins (in Chinese) [master’s thesis]. Guangxi, China: Guangxi University of Chinese Medicine. (2022).
70. Shi, ZH, and Guo, YJ. Immediate analgesic effect of warming needle Moxibustion for primary dysmenorrhea (in Chinese). Acta Chin Med. (2017) 32:1343–46. doi: 10.16368/j.issn.1674-8999.2017.07.354
71. Lou, S. A radomized controlled study on the treatment of primary dysmenorrhea od cold coagulation and blood staisi type by wentong chong abdominal massage (in Chinese) [master’s thesis]. Tianjin, China: Tianjin University of Traditional Chinese Medicine. (2020).
72. Zhai, SJ. Immediate analgesic effect of an acupressure wrist-ankle strap simulating wrist-ankle acupuncture stimulation on primary dysmenorrhea in young women: A randomized controlled trial (in Chinese) [master’s thesis]. Shanghai University of Traditional Chinese Medicine. (2020).
73. Xiao, Y. The clinical effect observation on the treatment of primary dysmenorrhea with abdominal meridians acupuncture as the main method (in Chinese) [master’s thesis]. Yunnan, China: Yunnan University of Chinese Medicine. (2016).
74. Fan, CH. Clinical study on the treatment of cold blood stasis type primary dysmenorrhea with thunder fire moxibustion (in Chinese) [master’s thesis]. Guangdong, China: Guangzhou University of Chinese Medicine. (2021).
75. Jia, F. Clinical observation on 120 cases of primary dysmenorrhea treated by acupuncture (in Chinese) [master’s thesis]. Heilongjiang, China: Heilongjiang University of Chinese Medicine. (2017).
76. Hao, CC, and Wang, X. Observation on acupuncture and moxibustion in treatment of primary dysmenorrhea of cold - stagnation and blood - stasis type (in Chinese). Chinese Archives of Traditional Chinese Medicine. (2018) 36:659–62. doi: 10.13193/j.issn.1673-7717.2018.03.034
77. Guo, LM, Zhou, YB, Kong, XJ, Zhou, CH, and Liu, B. Effect of thunder - fire moxibustion therapy for clinical symptoms and serum prostaglandin f2α in patients with primary dysmenorrhea of cold coagulation and blood stasis (in Chinese). Hebei, China: Hebei Journal Traditional Chinese Medicine. (2021) 43:1367–70+74.
78. Zhong, Y, and Wei, YL. Warm needling for primary dysmenorrhea of cold-dampness stagnation syndrome (in Chinese). Chinese Manipulation & Rehabilitation Medicine. (2017) 8:32–33+37. doi: 10.19787/j.issn.1008-1879.2017.21.015
79. Chen, Y, Shang, GD, Fu, GB, and Jin, T. Effect of massage on hemodynamics parameters of uterine artery and serum prostaglandin in treating patients with primary dysmenorrhea (in Chinese). Chin J Integr Med. (2011) 31:1355–58.
80. Chen, CL, and Deng, C. Clinical observation of primary dysmenorrhea treated by acupuncture (in Chinese). J New Chin Med. (2014) 46:161–62. doi: 10.13457/j.cnki.jncm.2014.07.075
81. Chen, L, Guo, XL, Yu, SY, Wei, W, Shen, ZF, Zhao, GL, et al. Effect of acupuncture on brain functional connectivity strength in patients with primary dysmenorrhea (in Chinese). Chinese Acupuncture & Moxibustion. (2022) 42:863–70. doi: 10.13703/j.0255-2930.20210826-k0004
82. Han, Y, Zhou, YL, Guo, XH, Liu, YJ, Li, H, and Chen, XY. Analgesic effect on primary dysmenorrheal treated with conventional and sham acupucture at sanyinjiao (in Chinese). Chinese Acupuncture & Moxibustion. (2015) 35:318–22. doi: 10.13703/j.0255-2930.2015.04.002
83. Wei, YH, Li, WJ, and Fan, HX. Immediate and long-term analgesic effect of baliao points daoqi method in treating primary dysmenorrhea (in Chinese). Acta Chinese Medicine. (2019) 34:2687–91. doi: 10.16368/j.issn.1674-8999.2019.12.616
84. Yang, H, Liu, CZ, Chen, X, Ma, LX, Xie, JP, Guo, NN, et al. Systematic review of clinical trials of acupuncture-related therapies for primary dysmenorrhea. Acta obstetricia et gynecologica Scandinavica. (2008) 87:1114–22. doi: 10.1080/00016340802443798
85. Liu, W, Wang, CC, Lee, KH, Ma, X, and Kang, TL. Efficacy and safety of acupuncture and or Moxibustion for managing primary dysmenorrhea: a systematic review and meta-analysis. Clin Nurs Res. (2022) 31:1362–75. doi: 10.1177/10547738221086984
86. Jiang, HR, Ni, S, Li, JL, Liu, MM, Li, J, Cui, XJ, et al. Systematic review of randomized clinical trials of acupressure therapy for primary dysmenorrhea. Evid Based Complement Alternat Med. (2013) 2013:1–9. doi: 10.1155/2013/169692
87. Zhang, F, Sun, M, Han, S, Shen, X, Luo, Y, Zhong, D, et al. Acupuncture for primary dysmenorrhea: an overview of systematic reviews. Evid Based Complement Alternat Med. (2018) 2018:8791538–11. doi: 10.1155/2018/8791538
88. Chung, KF, Yeung, WF, Kwok, CW, and Yu, YM. Risk factors associated with adverse events of acupuncture: a prospective study. Acupunct Med. (2014) 32:455–62. doi: 10.1136/acupmed-2014-010635
89. Xu, S, Wang, L, Cooper, E, Zhang, M, Manheimer, E, Berman, B, et al. Adverse events of acupuncture: a systematic review of case reports. Evid Based Complement Alternat Med. (2013) 2013:1–15. doi: 10.1155/2013/581203
90. Chung, KF, Yeung, WF, Yu, YM, Kwok, CW, Zhang, SP, and Zhang, ZJ. Adverse events related to acupuncture development and testing of a rating scale. Clin J Pain. (2015) 31:922–8. doi: 10.1097/AJP.0000000000000189
91. White, IR, Barrett, JK, Jackson, D, and Higgins, JPT. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods. (2012) 3:111–25. doi: 10.1002/jrsm.1045
92. Marušić, MF, Fidahić, M, Cepeha, CM, Farcaș, LG, Tseke, A, and Puljak, L. Methodological tools and sensitivity analysis for assessing quality or risk of bias used in systematic reviews published in the high-impact anesthesiology journals. BMC Med Res Methodol. (2020) 20:121. doi: 10.1186/s12874-020-00966-4
93. Higgins, J, Thompson, S, Deeks, J, and Altman, D. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy. (2002) 7:51–61. doi: 10.1258/1355819021927674
94. Viechtbauer, W. Hypothesis tests for population heterogeneity in meta-analysis. Brit J Math Statist Psychol. (2007) 60:29–60. doi: 10.1348/000711005X64042
95. Guyatt, GH, Oxman, AD, Kunz, R, Brozek, J, Alonso-Coello, P, Rind, D, et al. GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol. (2011) 64:1283–93. doi: 10.1016/j.jclinepi.2011.01.012
96. IntHout, J, Ioannidis, JPA, Borm, GF, and Goeman, JJ. Small studies are more heterogeneous than large ones: a meta-meta-analysis. J Clin Epidemiol. (2015) 68:860–9. doi: 10.1016/j.jclinepi.2015.03.017
97. Zhang, Z, Xu, X, and Ni, H. Small studies may overestimate the effect sizes in critical care meta-analyses: a meta-epidemiological study. Crit Care. (2013) 17:R2–2. doi: 10.1186/cc11919
98. Del Re, AC, Maisel, NC, Blodgett, JC, and Finney, JW. Intention-to-treat analyses and missing data approaches in pharmacotherapy trials for alcohol use disorders. BMJ Open. (2013) 3:–e003464. doi: 10.1136/bmjopen-2013-003464
99. Probst, P, Grummich, K, Heger, P, Zaschke, S, Knebel, P, Ulrich, A, et al. Blinding in randomized controlled trials in general and abdominal surgery: protocol for a systematic review and empirical study. Syst Rev. (2016) 5:48–8. doi: 10.1186/s13643-016-0226-4
100. Moher, D, Hopewell, S, Schulz, KF, Montori, V, Gøtzsche, PC, Devereaux, PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. (2010) 63:e1–e37. doi: 10.1016/j.jclinepi.2010.03.004
Keywords: primary dysmenorrhea, TCM, Chinese medicine, acupuncture, acupressure, moxibustion, tuina, warm needling
Citation: Chen S-C, Ruan J-Y, Zhang B, Pang L-Y, Zhong L, Lin S-L, Wong K-P, Ouyang H-X, Yeung W-F, Fu Q-W and Chen B-Q (2024) Traditional Chinese medicine interventions based on meridian theory for pain relief in patients with primary dysmenorrhea: a systematic review and network meta-analysis. Front. Med. 11:1453609. doi: 10.3389/fmed.2024.1453609
Edited by:
Cristina Secosan, Victor Babes University of Medicine and Pharmacy, RomaniaReviewed by:
Coroleuca Catalin, Clinical Hospital of Obstetrics and Gynecology Prof. Dr. Panait Sârbu, RomaniaRazvan Ciortea, County Emergency Hospital Cluj-Napoca, Romania
Copyright © 2024 Chen, Ruan, Zhang, Pang, Zhong, Lin, Wong, Ouyang, Yeung, Fu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo-Qian Chen, MjAxOTMxMTMxNzVAc3R1Lmd6dWNtLmVkdS5jbg==; Qin-Wei Fu, ZnVxaW53ZWl0Y21AMTYzLmNvbQ==
 Shu-Cheng Chen
Shu-Cheng Chen Jia-Yin Ruan
Jia-Yin Ruan Bohan Zhang
Bohan Zhang Lok-Yi Pang1
Lok-Yi Pang1 Linda Zhong
Linda Zhong Ka-Po Wong
Ka-Po Wong Wing-Fai Yeung
Wing-Fai Yeung Qin-Wei Fu
Qin-Wei Fu Bo-Qian Chen
Bo-Qian Chen