- 1Center of Infectious Diseases, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Gastroenterology, West China Hospital, Sichuan University, Chengdu, China
- 3Department of Radiology, West China Hospital, Sichuan University, Chengdu, China
Bacterial liver abscesses commonly occur in patients with immune deficiencies such as diabetes, post-chemotherapy, or post-immunosuppressive therapy. The recommended treatment for liver abscesses exceeding 5 cm in a diameter is anti-infection therapy combined with percutaneous catheter drainage. Complications may include local spread to adjacent tissues or organs and thrombosis of the liver and portal veins. Rare hematogenous spread to distant sites, such as endophthalmitis and central nervous system embolism, have been reported, though such complications are uncommon post-drainage. This case report details a patient who suffered a brain infarction shortly after percutaneous drainage of a large liver abscess.
Introduction
Liver abscess refers to purulent lesions of liver tissue, which are caused by infection by various purulent microorganisms. It is clinically categorized into three types: bacterial, fungal, and amoebic, with bacterial liver abscesses being the most common. The disease occurs mainly due to the invasion of the liver by purulent bacteria, which can adversely affect some organs, with necrosis of the liver and liquefaction of abscesses—a potentially life-threatening disease characterized by the formation of a space-occupying lesion in the liver parenchyma. With the rapid development of the economy and the aging of the population, the incidence of metabolic diseases has been rising, resulting in an increase in the number of patients with PLA in combination with underlying diseases, corresponding to which the etiology, diagnosis, and treatment of PLA have undergone significant changes. The clinic is faced with new challenges. If PLA is not diagnosed in time and treated appropriately, it will lead to severe complications such as sepsis and infectious shock, and the mortality rate is as high as 10% ~ 30% (1). Traditional open treatment methods are usually used as insurance treatment options, and the preferred surgical option for patients is minimally invasive techniques. Ultrasound-guided puncture therapy is a relatively standard treatment measure, and the advantages of ultrasound intervention are more significant, with minimally invasive, shorter procedure times, milder patient stress, and a high degree of safety, which promotes postoperative recovery and ensures patient outcomes. Despite the current advances in diagnostic imaging and antibiotic therapy, the common complications of ultrasound-guided percutaneous drainage include poor catheter drainage, bleeding, infection, biliary fistula, extravasation of injected medication, and liver rupture, etc. (2). There may be a greater surgical risk for immunodeficient patients who are comorbid with a variety of underlying diseases. In this paper, we report a case of a large liver abscess that caused a brain infarction shortly after percutaneous drainage.
Case presentation
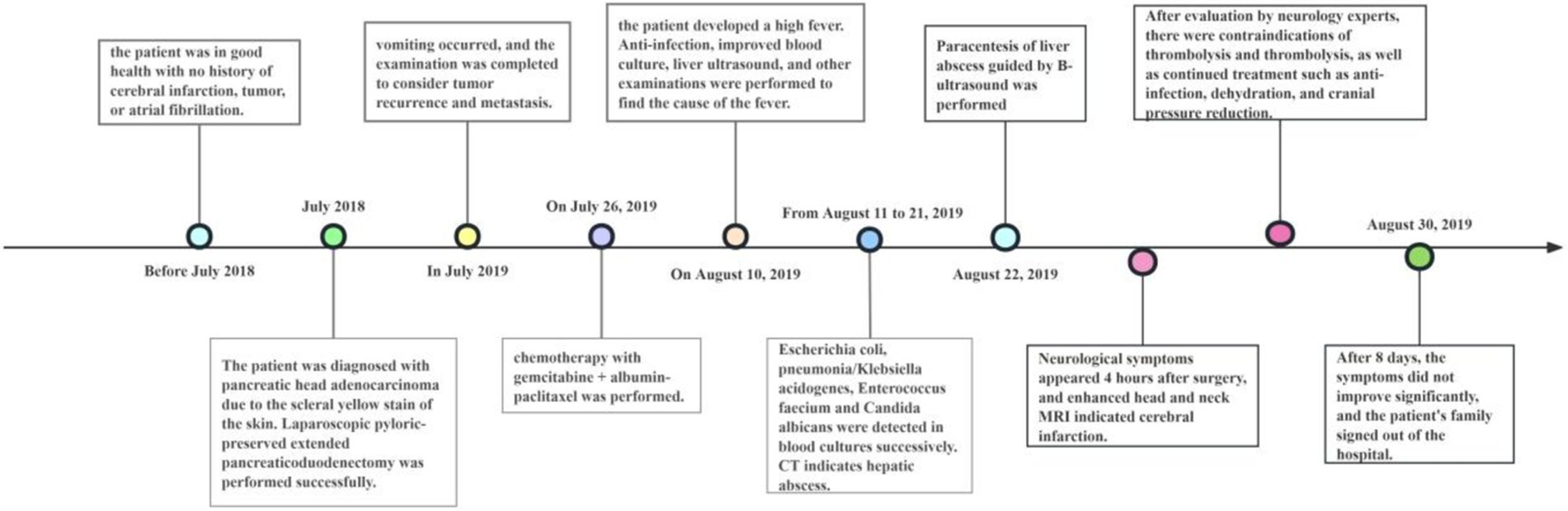
The patient, a 50-year-old woman, was diagnosed with adenocarcinoma of the pancreatic head one year prior and underwent laparoscopic pylorus-preserving pancreaticoduodenectomy. Twenty days before admission, she presented with vomiting. Past medical history: the patient has not had a brain infarction and denies a history of atrial fibrillation or hyperlipidemia. Family history: no family history of tumor, brain infarction, coronary heart disease, etc., and nothing special in the rest. The patient has a physical examination every 3–5 years with no significant abnormal findings. A follow-up abdominal CT suggested tumor recurrence and metastasis near the portal vein main trunk, pancreatic head, and mesentery. She was treated with a chemotherapy regimen including Gemcitabine and albumin-bound paclitaxel. Post-chemotherapy, she developed bleeding, fever, and chills. Laboratory tests revealed anemia, thrombocytopenia, leukopenia, elevated C-reactive protein, and interleukin-6 levels. Blood cultures identified multiple pathogens, and a CT scan indicated a liver abscess (14 × 10 cm), as shown in Figure 1. The patient received various antibiotics and underwent ultrasound-guided liver abscess drainage, yielding over 1,000 mL of pus infected with Escherichia coli. Shortly after, she experienced respiratory distress and was treated with oxygen therapy, methylprednisolone, and aminophylline. She then developed right-side limb weakness and left-upper limb fatigue. A head and neck MRI indicated acute brain infarction, as shown in Figure 2. Due to contraindications for thrombolysis or thrombectomy, she continued to receive anti-infection, diuretic, and mannitol treatment. Her condition worsened, resulting in incontinence, mixed aphasia, and decreased right-side sensation. Despite treatment, her symptoms did not improve, and she was discharged at the family’s request. The timeline of the episode of care is showed in Figure 3.

Figure 1. Upper abdominal enhanced CT. (A) Plain scan, large low-density shadows in the right and left inner lobes of the liver, Size about 14x10cm; there is separation and gas accumulation inside; (B,C) the lesion wall and septum were enhanced, which was considered liver abscess.
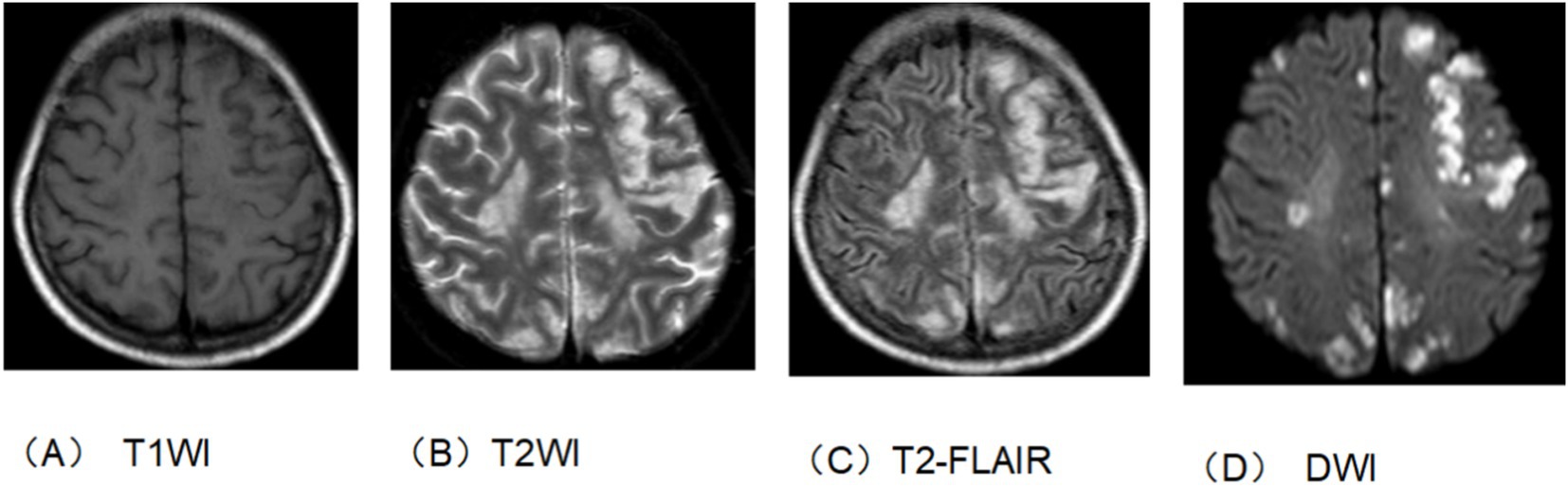
Figure 2. Head and neck enhanced MRI. (A) T1 sequence. (B) T2 sequence. (C) T2-flair sequence. (D) DWI sequence. The bilateral rated lobes scattered in multiple patchy and nodular slightly longer T1 and long T2 signal shadow. T2-flair showed hypertension and DWI showed high signal intensity. This suggests brain infarction.
Discussion
Studies (3) have reported that Klebsiella pneumoniae and Escherichia coli are the primary pathogens causing pyogenic liver abscess (PLA). PLA is often caused by biliary system obstruction, portal vein reflux obstruction, or systemic bacteremia, and its onset is rapid and typically accompanied by fever and chills. It easily affects organs outside the liver and, in severe cases, can lead to septic shock and multiple organ failure. The incidence of PLA is higher in Asian countries, with about 12–18 cases per 100,000 people (4), and recent studies in developed countries report a mortality rate of 2.6 to 9.6% (5–7). Patients with compromised immune function have a significantly higher poor prognosis rate than those with normal immune function, as they tend to have more severe infections and worse nutritional status when PLA occurs, thus requiring more aggressive treatment strategies. In this case, the patient had a malignant tumor and experienced rapid infection progression due to immunosuppression following chemotherapy, leading to leukopenia and anemia (8). Early blood cultures during the fever indicated infections by multiple pathogens, including Escherichia coli, Klebsiella pneumoniae, Enterococcus faecium, and Candida albicans, and a CT scan suggested a liver abscess, which was confirmed by pus culture from the drainage fluid. Anti-infection measures and early aggressive drainage are the primary treatment methods for bacterial liver abscesses. Abscesses smaller than 5 cm are recommended to be treated with aspiration, which can be repeated if necessary (9). In contrast, catheter drainage is recommended for abscesses larger than 5 cm, as it provides continuous drainage, removes thick pus due to its wider diameter, and prevents re-accumulation. Regarding treatment efficacy, ultrasound-guided catheter drainage is safe, has fewer complications, a higher success rate, and reduces the time needed to achieve clinical relief compared to pus aspiration, making it a preferable method (10, 11).
Complications of liver abscess drainage include abscess rupture and intraperitoneal dissemination, but short-term pulmonary or cerebral embolism post-drainage has not been reported. The patient had no history of brain infarction and no high-risk factors such as atrial fibrillation and hyperlipidemia. Therefore, we analyzed the possible causes of this acute brain infarction: bacterial emboli may enter the bloodstream and spread to cerebral vessels, causing cerebral infarction; the patient’s previous diagnosis of pancreatic head adenocarcinoma and abdominal CT findings suggested the possibility of multiple metastases within the liver, and the abscess drainage might have caused cancer emboli to disseminate through the bloodstream to cerebral vessels, leading to cerebral infarction. Additionally, the rapid drainage of a large volume from the patient’s substantial liver abscess could have caused a swift reduction in intracavitary pressure and volume, potentially leading to the collapse of the abscess wall, causing localized damage, and resulting in distant dissemination through blood-borne pus emboli, thereby causing pulmonary embolism and cerebral embolism.
Conclusion
In summary, we report a rare case of cerebral embolism caused by the drainage of a bacterial liver abscess, highlighting the potential for hematogenous spread and distant organ embolism due to rapid drainage of a large liver abscess.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
W-qD: Conceptualization, Data curation, Writing – original draft. BW: Data curation, Writing – review & editing. Z-yL: Data curation, Visualization, Writing – review & editing. KL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1453533/full#supplementary-material
References
1. Song, H, Wang, X, Lian, Y, and Wan, T. Analysis of the clinical characteristics of 202 patients with liver abscess associated with diabetes mellitus and biliary tract disease. J Int Med Res. (2020) 48:300060520949404. doi: 10.1177/0300060520949404.32865074
2. Alasso, AAO, Ibrahim, IG, Ali, IA, and Ahmed, MR. A case report and treatment considerations for pyogenic liver abscess with biliary fistula. Int J Surg Case Rep. (2024) 116:109343. doi: 10.1016/j.ijscr.2024.109343
3. Hui-an, Y, Jin-jin, Y, and Xiao-ling, Y. Clinical characteristics and influencing fractors for prognosis of patients with pyogenic liver abscess under different immunne status. China J Infect Control. (2023) 22:52–8. doi: 10.12138/j.issn.1671-9638.20233399
4. Chen, YC, Lin, CH, Chang, SN, and Shi, ZY. Epidemiology and clinical outcome of pyogenic liver abscess: an analysis from the National Health Insurance Research Database of Taiwan, 2000-2011. J Microbiol Immunol Infect. (2016) 49:646–53. doi: 10.1016/j.jmii.2014.08.028
5. Yoo, JJ, Lee, TK, Kyoung, DS, Park, MA, Kim, SG, and Kim, YS. A population-based study of pyogenic liver abscess in Korea: incidence, mortality and temporal trends during 2007-2017. Liver Int. (2021) 41:2747–58. doi: 10.1111/liv.15034
6. Zimmermann, L, Wendt, S, Lübbert, C, and Karlas, T. Epidemiology of pyogenic liver abscesses in Germany: analysis of incidence, risk factors and mortality rate based on routine data from statutory health insurance. United European Gastroenterol J. (2021) 9:1039–47. doi: 10.1002/ueg2.12132.PMID: 34329537
7. Mukthinuthalapati, VVPK, Attar, BM, Parra-Rodriguez, L, Cabrera, NL, Araujo, T, and Gandhi, S. Risk factors, management, and outcomes of pyogenic liver abscess in a US safety net hospital. Dig Dis Sci. (2020) 65:1529–38. doi: 10.1007/s10620-019-05851-9
8. Yin, D, Ji, C, Zhang, S, Wang, J, Lu, Z, Song, X, et al. Clinical characteristics and management of 1572 patients with pyogenic liver abscess: a 12-year retrospective study. Liver Int. (2021) 41:810–8. doi: 10.1111/liv.14760
9. Zerem, E, and Hadzic, A. Sonographically guided percutaneous catheter drainage versus needle aspiration in the management of pyogenic liver abscess. AJR Am J Roentgenol. (2007) 189:W138–42. doi: 10.2214/AJR.07.2173.17715080
10. SMR, S, Bakhshi, G, and Muley, GA. Needle aspiration versus catheter drainage in medium-sized (5-10 cm) liver abscesses: a comparative study in Mumbai, India. Cureus. (2023) 15:e38240. doi: 10.7759/cureus.38240
Keywords: chemotherapy, liver abscess, percutaneous drainage, brain infarction, pancreatic head cancer
Citation: Deng W-q, Wei B, Li Z-y and Liu K (2024) Case report: Brain infarction following percutaneous drainage of a liver abscess post-chemotherapy for pancreatic head cancer. Front. Med. 11:1453533. doi: 10.3389/fmed.2024.1453533
Edited by:
Sara Lorente, Hospital Clinico Universitario Lozano Blesa, SpainReviewed by:
Cuiling Zheng, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaLintao Liu, Houston Methodist Research Institute, United States
Copyright © 2024 Deng, Wei, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai Liu, bGl1YnVzaW5lc3NAMTYzLmNvbQ==; Bo Wei, YWxseW9va2luZ0AxNjMuY29t
 Wan-qiu Deng
Wan-qiu Deng Bo Wei
Bo Wei Zheng-yan Li3
Zheng-yan Li3 Kai Liu
Kai Liu