- 1Department of Emergency Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 2Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan
- 3Department of Information Management, Southern Taiwan University of Science and Technology, Tainan, Taiwan
- 4Division of Geriatrics and Gerontology, Department of Internal Medicine, Chi Mei Medical Center, Tainan, Taiwan
- 5Department of Senior Services, Southern Taiwan University of Science and Technology, Tainan, Taiwan
- 6Department of Nursing, Chi Mei Medical Center, Tainan, Taiwan
- 7School of Nursing, China Medical University, Taichung City, Taiwan
- 8School of Medicine, College of Medicine, National Sun Yat-sen University, Kaohsiung, Taiwan
- 9Department of Emergency Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 10Department of Environmental and Occupational Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Aim: Transitional care in the emergency department (ED) has the potential to improve outcomes for older patients, but the specific population benefits from it and impact in Taiwan remain unclear. Therefore, we conducted this study.
Methods: An interdisciplinary team comprising emergency physicians, dedicated transitional care nurse (TCN), nurse practitioners, nurses, geriatricians, and social workers was established at a tertiary medical center. TCN conducted screenings of ED patients (≥75 years) awaiting hospitalization to identify those in need of social or care support and aid as required. The team held regular meetings to address transitional care challenges. A retrospective analysis was conducted, comparing patients who received transitional care with those who did not, between February 1, 2022, and October 31, 2022, followed by a three-month outcome assessment.
Results: We successfully implemented a novel ED transitional care model, involving 183 patients with TCN assistance and 374 patients without. Compared to patients without TCN, those with TCN were older, had more underlying comorbidities, required more nasogastric feeding and Foley indwelling, and had higher rates of hospice and palliative care. The common needs for TCN included providing home care instructions to a foreign caregiver (38.4%), long-term care referral (30.0%), care instructions for family members of older adults in long-term care facilities (26.3%), social worker referral (3.2%), and home healthcare referral (2.1%). Follow-up analysis showed no significant outcome differences between the two cohorts.
Conclusion: The model we implemented identified the population benefiting from this service. Despite the frailty of patients receiving TCN, their outcomes were not inferior, suggesting the potential benefits of TCN for this population. Further research is warranted.
1 Introduction
The global aging issue is a major concern, with the proportion of the world’s population aged 60 years and above projected to nearly double from 12 to 22% between 2015 and 2050 (1). Taiwan is experiencing rapid population aging, with the percentage of older individuals already reaching 18.3% in 2023 (2). Projections indicate that this figure is expected to surpass 20% by 2025 (2). Older individuals typically experience a higher prevalence of chronic and complex diseases compared to younger populations (3). Ensuring continuous care for older adults can enhance care quality while reducing the burden on their family members, caregivers, and society (3).
The emergency department (ED) serves as a crossroad connecting various healthcare settings such as home, long term care facilities, outpatient care, and hospitalization (4). It also serves as the primary entry point for older patients with urgent medical needs, making the management of the ED crucial to the outcomes of this population (4). The American College of Emergency Physicians recommends the implementation of effective transitional care (TC) to facilitate outpatient care following an ED evaluation (4).
In Taiwan, TC is typically provided through discharge planning after hospitalization, with little emphasis placed on initiating such care within the ED. Numerous models for ED TC have been proposed, including the GEDI WISE (Geriatric Emergency Department Innovations in Care through Workforce, Informatics, and Structural Enhancements) program in the United States (5, 6). The GEDI WISE program was designed to meet the complex needs of older adults in emergency settings (5, 6). At its core, GEDI WISE incorporates ED-based Transitional Care Nurse (TCN) interventions, which specifically target the needs of geriatric patients by assessing and addressing their cognitive, functional, and social support requirements (5, 6). TCNs act as dedicated care coordinators, working to avoid unnecessary hospital admissions and facilitating safe, effective discharges (5, 6). Evidence from studies has shown that TCN involvement reduces 30-day readmission rates, lowers immediate hospitalization risk, and brings considerable healthcare cost savings, highlighting their critical role in enhancing care quality and efficiency for aging populations (5, 6). However, it is important to consider the cultural and insurance differences between Western nations and Taiwan, as the applicability of Western models may be limited. In Taiwan, the family-centric culture places strong responsibility for elder care on families, with significant reliance on live-in foreign caregivers, unlike Western models that often depend on professional providers. Additionally, Taiwan’s National Health Insurance offers near-universal coverage, reducing financial barriers but necessitating more education and support for navigating long-term care services. Transitional care models must address these cultural and systemic differences to be effective. Therefore, our study aimed to implement a model for ED TC specifically tailored to the Taiwanese context, adapted from the existing evidence-based United States model (i.e., GEDI WISE). We sought to investigate the targeted population and evaluate the outcomes of this new model. Our primary objective was to bridge the existing knowledge gap and make a meaningful contribution to the development of effective and culturally appropriate TC strategies within Taiwan’s ED setting. Additionally, our findings may serve as a valuable reference for other nations seeking to enhance their TC practices.
2 Materials and methods
2.1 Study hospital
This study was conducted at the Chi Mei Medical Center (CMMC), a Southern Taiwan tertiary medical center with over 60 full-time attending physicians and residents who served >121,000 ED patients in 2019 (7). In 2016, the CMMC ED established a Chi Mei Integrated Geriatric Emergency Team, and subsequently launched Taiwan’s first Geriatric ED in 2019, with the objective of leading and enhancing geriatric care for the rapidly growing older population (8). The Geriatric ED at CMMC employed various studies and approaches to generate local data and formulate solutions targeted toward the older population in Taiwan, including emergency medical services in the older population (9), geriatric syndromes and hospice care needs (10), a novel comprehensive screening tool (Emergency Geriatric Assessment) (11), computer-based and pharmacist-assisted medication review (12), hospice and palliative care (13), computer-assisted home care referral (14), and computerized tool and interdisciplinary care for older patients with delirium (15).
2.2 Establishment of interdisciplinary team and ED TC model
First, an interdisciplinary team consisting of emergency physicians, a dedicated TCN, nurse practitioners, nurses, geriatricians, and social workers was established in Feb 2022 to initiate TC in the ED. The dedicated TCN was an ED nurse with 6 years of working experience in the study hospital. Before initiating the protocol, she received 1 month of training in geriatric emergency medicine and home healthcare.
Second, following a consensus among the interdisciplinary team, a flowchart outlining the protocol for ED TC was developed (Figure 1). A TCN screened patients who were aged 75 years or older and waiting for hospitalization in the ED to assess their need for social or care support. The TCN’s working hours were from 8:00 am to 5:00 pm on weekdays, Monday through Friday. Patients who met the screening criteria were randomly visited by the TCN, and those in need of social or care support were classified as the cohort with TCN assistance. Conversely, those who did not require such support were classified as the cohort without TCN assistance. The TCN evaluated patients for social or care support needs across five different aspects. The first aspect focused on providing home care instructions to foreign caregivers, including assessing their abilities and guiding them on nursing skills. The second aspect pertained to providing care instructions to family members of older adults residing in long-term facilities, which involved assessing their abilities and providing nursing skill guidance. The third aspect of the TCN’s assistance involved assessing the patient’s daily activities and long-term care needs. If necessary, the TCN referred the patient to a long-term care institution or nursing home. Additionally, the TCN provided information and assistance with applications for long-term care services, including transportation services, assistive device rental or purchase, home nursing, respite care services, day care centers, and other related services. The fourth aspect of the TCN’s role was to consult with a social worker to assist patients with financial, emotional, and social support issues. However, it should be noted that financial assistance was only considered successful when patients met the conditions for social welfare subsidies. The fifth aspect involved evaluating and arranging for home healthcare of the patient after hospital discharge if appropriate. Telephone follow-up was conducted with all patients after their hospital discharge.
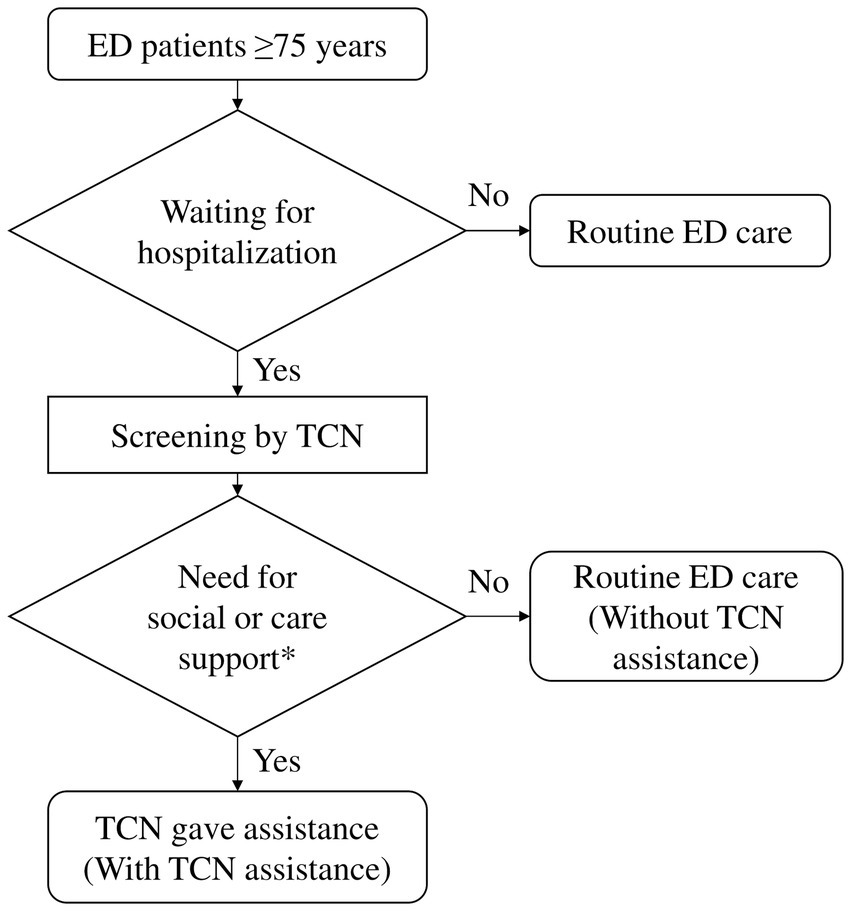
Figure 1. Flowchart of the protocol for ED transitional care. ED, emergency department; TCN, transitional care nurse.
Thirdly, a computer-assisted case management system was developed for ED TC, which integrated patients’ medical information, electronic assessment forms, and the aspects of social and care needs that were addressed by the TCN.
Fourth, all ED staff members were trained on the ED TC protocol, and the implementation of this protocol was officially announced on March 1, 2022.
2.3 Data collection: retrospective cohort study
Retrospective data of patients who were screened by TCN from March to October 2022 were collected. Patients who received with the five aspects of social or care need support by TCN were classified as the cohort with TCN assistance, while those who did not were classified as the cohort without TCN assistance (Figure 2). Data was collected by an experienced ED TCN, who was blinded to patient outcomes.
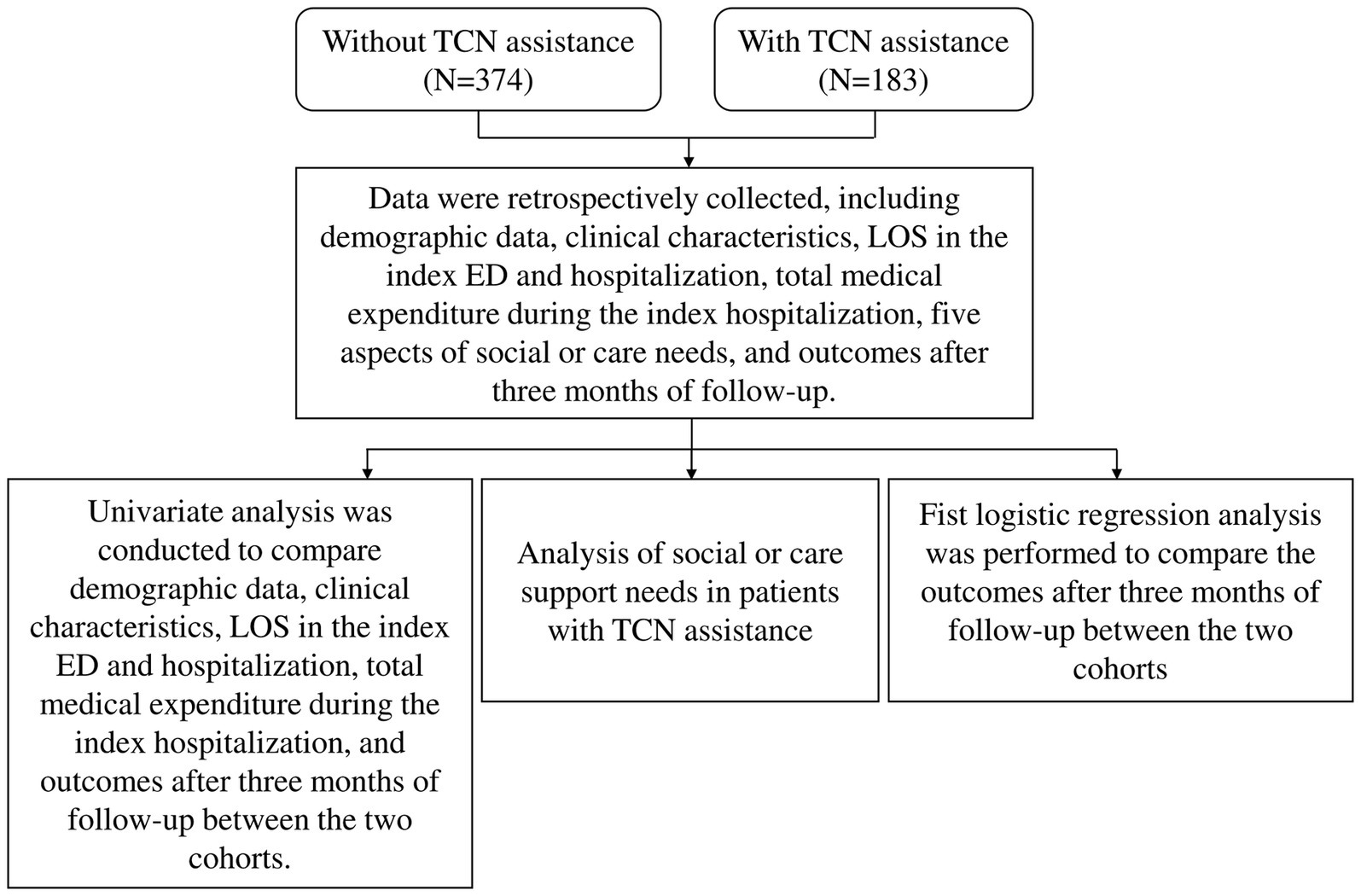
Figure 2. Flowchart of the study design. TCN, transitional care nurse; LOS, length of stay; ED, emergency department.
2.4 Characteristics and outcome comparisons between two cohorts
To investigate the characteristics of the population requiring social or care support (referred to as the cohort with TCN), we conducted a comparison between two cohorts. The comparison focused on clinical characteristics, length of stay (LOS) in the index ED and hospitalization, and total medical expenditure during the index hospitalization. The ED triage was conducted using the Taiwan Triage and Acuity Scale (TTAS), a modification of the Canadian Emergency Department Triage and Acuity Scale (16), with the following categories: (1) Category 1: critical conditions requiring immediate life-saving interventions, (2) Category 2: emergent conditions requiring prompt medical attention to prevent serious outcomes, (3) Category 3: urgent conditions that are not life-threatening but require timely evaluation and treatment, (4) Category 4: less urgent conditions where delays in care would unlikely cause harm, and (5) Category 5: non-urgent conditions suitable for outpatient management. Additionally, an analysis was performed on five aspects of social or care needs in patients with TCN. Both cohorts were followed up for 3 months to compare outcomes, which included total medical expenditure within 3 months after hospital discharge, ED visit within 3 days after hospital discharge, re-hospitalization within 14 days after hospital discharge, and death within 1 month after hospital discharge.
2.5 Ethical statements
Following approval from the institutional review board of the study hospital, this retrospective study was conducted using anonymized patient data in accordance with the principles outlined in the Declaration of Helsinki. Informed consent was waived due to the study’s retrospective design, which posed no risk to patient welfare.
2.6 Statistics
In the univariate analysis, categorical variable analysis was conducted using the Chi-Squared Test or Fisher’s exact test, while continuous variable analysis utilized the Mann–Whitney U Test. Fist logistic regression analysis was performed to compare the outcomes between the two cohorts. Statistical analyses were carried out using Statistical Analysis System 9.4 (SAS Institute Inc., Cary, NC, United States). A significance level of 0.05 (two-tailed) was employed.
3 Results
We successfully implemented an ED TC model, screening a total of 557 older ED patients. Of these, 183 patients received TCN assistance, while 374 patients did not (Table 1). Compared to patients without TCN, those with TCN assistance were older (84.0 years vs. 81.0 years, p < 0.001), had a higher percentage of individuals aged ≥85 (47.0% vs. 28.3%, p < 0.001), a lower body mass index (22.5 vs. 23.5, p = 0.034), and a lower Glasgow Coma Scale (13.4 vs. 14.4, p < 0.001). Most patients in both cohorts were triaged as either category 2 or 3, but the TCN cohort had a higher proportion of patients triaged as category 1 (7.7% vs. 6.2%) and category 2 (48.6% vs. 31.3%), along with a lower proportion of patients triaged as category 3 (43.7% vs. 62.6%) compared to the cohort without TCN (p < 0.001). No patients in either cohort were triaged as category 4 or 5. Most patients presented to the ED for non-traumatic reasons, and there was no difference between the two cohorts in this regard. The TCN cohort had a higher proportion of underlying comorbidities and iatrogenesis compared to the cohort without TCN assistance. These included congestive heart failure (26.8% vs. 17.7%, p = 0.012), cerebrovascular disease (51.4% vs. 34.8%, p < 0.001), dementia (41.5% vs. 14.7%, p < 0.001), diabetes (33.9% vs. 23.3%, p = 0.008), nasogastric feeding (26.8% vs. 5.9%, p < 0.001), Foley indwelling (37.2% vs. 18.7%, p < 0.001), bedridden status (87.4% vs. 59.1%, p < 0.001), and receiving hospice and palliative care (37.7% vs. 17.7%, p < 0.001). In terms of ED diagnosis or symptoms/signs, the TCN cohort had a higher proportion of urinary tract infections (18.6% vs. 10.4%, p = 0.007) and pneumonia (16.9% vs. 9.4%, p = 0.009) compared to the cohort without TCN. Additionally, the TCN cohort had a longer LOS in the index ED visit (median: 24.8 h vs. 31.0 h, p < 0.001), longer LOS in the index hospitalization (median: 10 days vs. 7 days, p < 0.001), and higher total medical expenditure during index hospitalization (median: 76,532.0 New Taiwan Dollars [NTD] vs. 58,678.5 NTD, p = 0.001) compared to the cohort without TCN.

Table 1. Comparison of demographic data and clinical characteristics between older ED patients without and with TCN assistance.
Among patients with TCN assistance (Table 2), the most common social or care need aspect was “providing home care instructions to a foreign caregiver (38.4%),” followed by “long-term care referral (30.0%),” “providing care instructions to a family member of an older adult living in a long-term care facility (26.3%),” “social worker referral (3.2%),” and “home healthcare referral (2.1%)”.
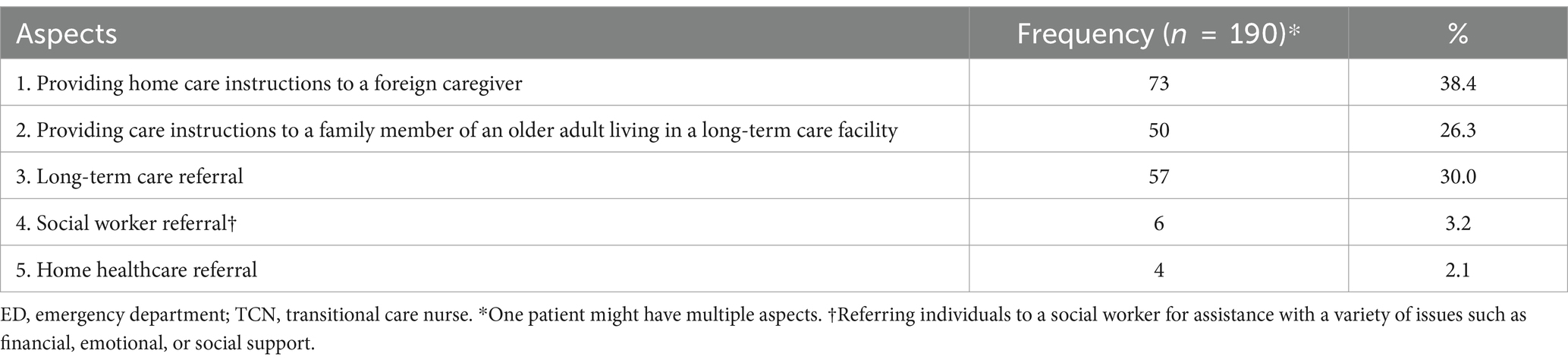
Table 2. Aspects for need of social or care support in the older ED patients who received TCN assistance.
In the univariate analysis, the cohort with TCN assistance had a higher total medical expenditure <3 months after hospital discharge (median: 126,427.0 NTD vs. 89,093.5 NTD, p = 0.004) compared to the cohort without TCN (Table 3). However, when utilizing Fist logistic regression analysis with adjustment for confounding factors (Table 4), there was no significant difference found in total medical expenditure <3 months after hospital discharge, ED visit ≤3 days after hospital discharge, re-hospitalization ≤14 days after hospital discharge, and death <1 month after hospital discharge between the two cohorts.
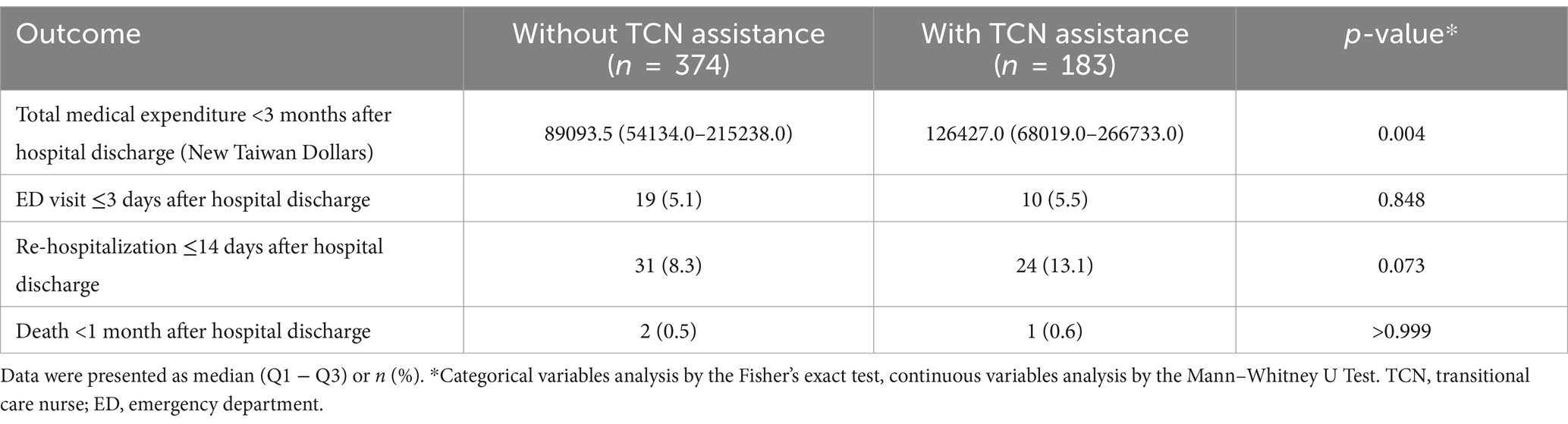
Table 3. Outcomes in older emergency department patients after hospital discharge: a univariate analysis comparing patients with and without TCN assistance.
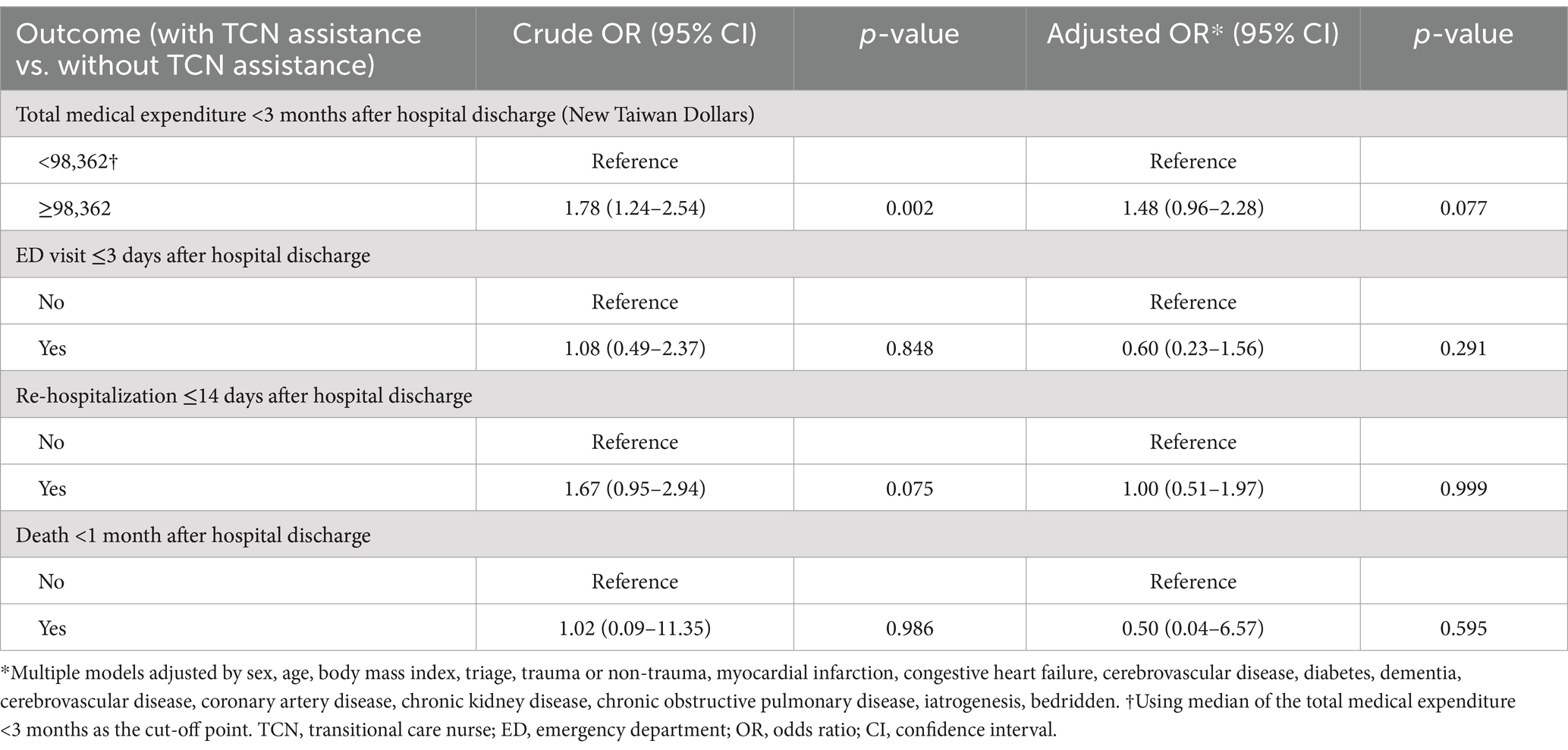
Table 4. Comparison of outcomes in older emergency department patients after hospital discharge: first logistic regression analysis comparing patients with and without TCN assistance.
4 Discussion
We successfully implemented an ED TC model for older patients through collaboration among an interdisciplinary team and a dedicated TCN. Our findings revealed that patients who received TCN assistance exhibited greater frailty, as indicated by older age, higher acuity, a higher proportion of underlying comorbidities and receiving hospice and palliative care, longer LOS in the index ED visit and hospitalization, and higher total medical expenditure during the index hospitalization (Table 1). The most common aspect requiring social, or care support was “providing home care instructions to a foreign caregiver,” followed by “long-term care referral” and “providing care instructions to a family member of an older adult living in a long-term care facility (Table 2)”. However, despite these factors, the cohort with TCN did not demonstrate inferior outcomes compared to the cohort without TCN (Table 4).
The success of this model relies on a dedicated TCN and effective collaboration among interdisciplinary team members. Having a dedicated healthcare professional for TC in the ED is considered a beneficial geriatric care model (17). A systematic review has demonstrated that dedicated healthcare professionals have two primary functions: conducting individual needs assessments of ED patients and coordinating discharge planning and services (17). Implementing a structured individual needs assessment has been associated with a significant decrease in hospital admissions, hospital readmissions, and ED revisits (17). Additionally, developing individualized discharge plans from the ED has shown a significant decrease in ED revisits and hospital readmissions (17). Our model essentially embodies a structured individual needs assessment. Given the complex nature of issues faced by older patients, geriatric integrated care necessitates interdisciplinary or multidisciplinary teamwork (17). The specific components of the structured individual needs assessment and the composition of the interdisciplinary team depend on the objectives of the hospital, the needs of the patient/caregiver, and the available local resources (4, 17).
This study examined the characteristics of patients who received TCN assistance, aiming to identify the target population in need of social and care support in the future (Tables 1, 2). The screening and inclusion criteria for TCN assistance depend on the hospital’s objectives, available local resources, and the population likely to experience better outcomes (4, 5, 18). The first implementation of the TCN model was carried out through the program called “GEDI WISE” in the United States (5). In the GEDI WISE program, TCN was used to screen ED patients aged 65 and above and assess their cognitive function, delirium, functional status, falls risk, care transitions, and caregiver strain (5). The choice of assessments used in the GEDI WISE program was based on preexisting hospital programs or staff preferences in the anticipated three hospitals (5). In a randomized controlled trial, ED patients aged 65 and above who revisited the ED within 30 days were included to evaluate the effects of an ED-to-home TC program on outcomes (18). This study classified the patients into six classes and observed differences in outcomes among these classes (18).
Our model assessed five aspects of the services provided by the TCN and revealed that the most common social or care support was the “providing home care instructions to foreign caregivers” (Table 2). In 2022, approximately 30% of foreign workers in Taiwan were employed as caregivers, with over 90% providing round-the-clock live-in care services (19), highlighting the high demand for foreign caregivers in Taiwan. However, foreign caregivers often face language barriers and lack medical care education, necessitating the providing home care instructions by the TCN, as demonstrated in this study. The second most prevalent social or care need identified in this study was long-term care referral. Since 2017, the Taiwanese government has expanded the scope of long-term care services and allocated increased funds to promote Long-term Care 2.0 (20). Nevertheless, most people lack knowledge about long-term care services and the application process, prompting the TCN program to assist patients and their families in understanding and applying for such services. In 2021, approximately 52,000 individuals aged 65 or above resided in long-term care facilities in Taiwan, representing around 1.3% of the older population (21). This option provides an alternative to informal care by family members or foreign caregivers. However, even when older adults live in long-term care facilities, their family members may still require coordination with the facility staff, thus highlighting their need for social or care support. The proportions of social worker referrals and home healthcare referrals were notably low. The low proportion of social worker referrals primarily resulted from most patients failing to meet the government’s social welfare subsidy requirements, leading to unsuccessful referrals. The low rate of home healthcare referrals may be attributed to the shortage of home healthcare professionals in the study hospital. Since 2020, the hospital has initiated ED referrals for home healthcare, which have shown lower median total medical expenditure within 3 months compared to home healthcare initiated after hospitalization (14). In the future, our aim is to expand the service by recruiting more healthcare professionals to meet the needs of this population.
The univariate analysis revealed higher medical expenditures within 3 months of hospital discharge among patients with TCN assistance compared to those without, likely due to their inferior underlying condition (Table 3). However, after adjusting for confounding factors, the difference was not statistically significant (Table 4). These findings demonstrate a promising result for TCN assistance in our model.
One major strength of our study is the successful implementation of a novel TCN model in Taiwan, which can serve as an important reference for the future promotion of TCN in the ED. However, the study has several limitations. Firstly, the retrospective design and small sample size limit the generalizability of the findings. To address this limitation, a prospective randomized study with a larger sample size should be conducted in the future to provide further clarification on the topic. Another limitation is that the applicability of this model may be limited to the specific context of our hospital and may not fully generalize to other hospitals or nations. This is due to variations in hospital objectives and available local resources. Therefore, modifications would be necessary if implementing this model in other healthcare settings.
5 Conclusion
Our study successfully implemented a TC model for older patients in the ED. We observed that the population requiring TCN assistance tended to be older and had a more compromised condition compared to those who did not require TCN assistance. The most common needs for TCN assistance were providing home care instructions to foreign caregivers, facilitating long-term care referrals, and offering care instructions to family members of older adults residing in long-term care facilities. Upon adjusting for confounding factors, we found that patients receiving TCN assistance did not exhibit inferior outcomes compared to those without TCN, indicating the potential benefits of TCN assistance. This study has effectively identified the target population in need of TCN assistance, and our novel TC model can serve as a valuable reference for future implementation of TC in ED settings. However, it is important to note that further research using a prospective randomized design and larger sample sizes is necessary to explore the full impact of the TCN program. This future research should aim to assess the potential of TCN in reducing healthcare costs and improving outcomes for older ED patients.
Data availability statement
The datasets presented in this article are not readily available because the data that support the findings of this study are not publicly available due to privacy and institutional policies. Requests to access the datasets should be directed to amFzb25odWFuZzA4MDNAZ21haWwuY29t.
Author contributions
H-LH: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. C-HH: Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing. Y-JL: Data curation, Formal analysis, Validation, Writing – review & editing. K-TT: Investigation, Methodology, Project administration, Supervision, Writing – review & editing. P-CY: Investigation, Project administration, Resources, Software, Validation, Writing – review & editing. S-LH: Investigation, Project administration, Supervision, Writing – review & editing. A-CP: Writing – review & editing, Supervision, Project administration, Investigation. C-CHs: Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. SY-CH: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. C-CHu: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Grant CMFHR112095 and Grant physician-scientist 11001 from Chi Mei Medical Center.
Acknowledgments
We express our gratitude to Yi-Chun Lin (transitional care nurse), I-Chi Lin (social worker), Chao-Hsueh Wang (case manager), Yu-Pao Chen (registered nurse), Zi-Hui Chao (registered nurse), Hsiu-Yuan Chan (nurse practitioner) and all the ED staff for their valuable collaborations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ED, emergency department; TC, transitional care; GEDI WISE, Geriatric Emergency Department Innovations in Care through Workforce, Informatics, and Structural Enhancements; TCN, transitional care nurse; CMMC, Chi Mei Medical Center; LOS, length of stay; NTD, New Taiwan Dollars.
References
1. Ageing and Health. (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (Accessed May 15, 2023).
2. Ministry of the Interior, Taiwan. (2023). Available at: https://www.moi.gov.tw/english/Default.aspx (Accessed Novemember 15, 2024).
3. Conneely, M, Leahy, S, Dore, L, Trepel, D, Robinson, K, Jordan, F, et al. The effectiveness of interventions to reduce adverse outcomes among older adults following emergency department discharge: umbrella review. BMC Geriatr. (2022) 22:462. doi: 10.1186/s12877-022-03007-5
4. American College of Emergency Physicians. American geriatrics S, emergency nurses a, Society for Academic Emergency M, geriatric emergency department guidelines task F: geriatric emergency department guidelines. Ann Emerg Med. (2014) 63:e7–e25. doi: 10.1016/j.annemergmed.2014.02.008
5. Hwang, U, Dresden, SM, Rosenberg, MS, Garrido, MM, Loo, G, Sze, J, et al. Geriatric emergency department innovations: transitional care nurses and hospital use. J Am Geriatr Soc. (2018) 66:459–66. doi: 10.1111/jgs.15235
6. Dresden, SM, Hwang, U, Garrido, MM, Sze, J, Kang, R, Vargas-Torres, C, et al. Geriatric emergency department innovations: the impact of transitional care nurses on 30-day readmissions for older adults. Acad Emerg Med. (2020) 27:43–53. doi: 10.1111/acem.13880
7. Introduction of Chi Mei Medical Center. (2023). Available at: http://www.chimei.org.tw/newindex/assets/img/about/about_chimei/english.pdf (Accessed May 12, 2023).
8. Introduction for Geriatric Emergency Department. (2023). Available at: http://sub.chimei.org.tw/57900/index.php/specially/specially3 (Accessed May 15, 2023).
9. Huang, CC, Chen, WL, Hsu, CC, Lin, HJ, Su, SB, Guo, HR, et al. Elderly and nonelderly use of a dedicated ambulance Corps' emergency medical Services in Taiwan. Biomed Res Int. (2016) 2016:1–7. doi: 10.1155/2016/1506436
10. Ke, YT, Peng, AC, Shu, YM, Chung, MH, Tsai, KT, Chen, PJ, et al. Prevalence of geriatric syndromes and the need for hospice Care in Older Patients of the emergency department: a study in an Asian medical center. Emerg Med Int. (2020) 2020:1–9. doi: 10.1155/2020/7174695
11. Ke, YT, Peng, AC, Shu, YM, Chung, MH, Tsai, KT, Chen, PJ, et al. Emergency geriatric assessment: a novel comprehensive screen tool for geriatric patients in the emergency department. Am J Emerg Med. (2018) 36:143–6. doi: 10.1016/j.ajem.2017.07.008
12. Liu, YL, Chu, LL, Su, HC, Tsai, KT, Kao, PH, Chen, JF, et al. Impact of computer-based and pharmacist-assisted medication review initiated in the emergency department. J Am Geriatr Soc. (2019) 67:2298–304. doi: 10.1111/jgs.16078
13. Weng, TC, Yang, YC, Chen, PJ, Kuo, WF, Wang, WL, Ke, YT, et al. Implementing a novel model for hospice and palliative care in the emergency department: an experience from a tertiary medical center in Taiwan. Medicine (Baltimore). (2017) 96:e6943. doi: 10.1097/MD.0000000000006943
14. Hsu, SL, Tsai, KT, Tan, TH, Ho, CH, Yang, PC, Hsu, CC, et al. Interdisciplinary collaboration and computer-assisted home healthcare referral in the emergency department: a retrospective cohort study. Aging Clin Exp Res. (2022) 34:1939–46. doi: 10.1007/s40520-022-02109-9
15. Tan, TH, Yang, TY, Chen, YM, Chung, SY, Liu, HH, Yang, PC, et al. Computerized tool and interdisciplinary care for older patients with delirium in the emergency department: a novel model in Taiwan. Aging Clin Exp Res. (2022) 34:3137–44. doi: 10.1007/s40520-022-02240-7
16. Ng, CJ, Chien, CY, Seak, JC, Tsai, SL, Weng, YM, Chaou, CH, et al. Validation of the five-tier Taiwan triage and acuity scale for prehospital use by emergency medical technicians. Emerg Med J. (2019) 36:472–8. doi: 10.1136/emermed-2018-207509
17. van den Broek, S, Westert, GP, Hesselink, G, and Schoon, Y. Effect of ED-based transitional care interventions by healthcare professionals providing transitional care in the emergency department on clinical, process and service use outcomes: a systematic review. BMJ Open. (2023) 13:e066030. doi: 10.1136/bmjopen-2022-066030
18. Green, RK, Nieser, KJ, Jacobsohn, GC, Cochran, AL, Caprio, TV, Cushman, JT, et al. Differential effects of an emergency department-to-home care transitions intervention in an older adult population: a latent class analysis. Med Care. (2023) 61:400–8. doi: 10.1097/MLR.0000000000001848
19. Labor Statistics Information Services. (2023). Available at: https://statfy.mol.gov.tw/statistic_DB.aspx (Accessed May 15, 2023).
20. Chen, CF, and Fu, TH. Policies and transformation of long-term care system in Taiwan. Ann Geriatr Med Res. (2020) 24:187–94. doi: 10.4235/agmr.20.0038
21. Social Welfare Gender Statistics Indicators. (2023). Available at: https://dep.mohw.gov.tw/DOS/cp-5342-59468-113.html (Accessed May 15, 2023).
Keywords: emergency department, nurse, older population, social, transitional care
Citation: Hsu H-L, Ho C-H, Lin Y-J, Tsai K-T, Yang P-C, Hsu S-L, Peng A-C, Hsu C-C, Ho SY-C and Huang C-C (2024) Developing a novel transitional care model for older emergency department patients and exploring the target population in Taiwan. Front. Med. 11:1444724. doi: 10.3389/fmed.2024.1444724
Edited by:
Esther-Lee Marcus, Herzog Hospital, IsraelReviewed by:
Pavel Weber, Masaryk University, CzechiaTheingi Maung Maung, AIMST University, Malaysia
Copyright © 2024 Hsu, Ho, Lin, Tsai, Yang, Hsu, Peng, Hsu, Ho and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chien-Cheng Huang, amFzb25odWFuZzA4MDNAZ21haWwuY29t
 Hung-Lin Hsu
Hung-Lin Hsu Chung-Han Ho
Chung-Han Ho Ying-Jia Lin
Ying-Jia Lin Kang-Ting Tsai4,5
Kang-Ting Tsai4,5 Chien-Cheng Huang
Chien-Cheng Huang