- Department of Nuclear Medicine, Peking University First Hospital, Beijing, China
Background: Prostate tuberculosis is a common form of urogenital tuberculosis that occurs in men. Clinical and imaging manifestations of prostate tuberculosis are atypical, which often need to be differentiated from benign prostatic hyperplasia, a prostate malignant tumor, and a urinary tract infection. Although prostate-specific membrane antigen (PSMA) is considered a specific biomarker for prostate cancer, it is also found within tuberculosis tissues that may be stimulated by angiogenic factors. An abnormal PSMA uptake on positron emission tomography combined with computed tomography (PET/CT) should eliminate the possibility of tuberculosis.
Case report: In this study, we reported a case of a 51-year-old man with an elevated erythrocyte sedimentation rate (ESR) but a normal prostate-specific antigen (PSA) value. 2-Deoxy-2-[fluorine-18]-fluoro-D-glucose (18F-FDG) and [fluorine-18]-prostate-specific membrane antigen (18F-PSMA) PET/CT scans were performed for further evaluation. The prostate showed a high fluoro-D-glucose (FDG) uptake but a slight PSMA uptake. Multiple osteolytic bone destruction and lymph nodes with an increased FDG uptake but a mild PSMA uptake were observed throughout the body. Systemic tuberculosis was diagnosed based on the prostate biopsy and the positive result of the T-cell spot test regarding tuberculosis infection. After 6 months of standard anti-tuberculosis treatment, the patient experienced symptom relief.
Conclusion: In the case of a urinary tract infection, where the prostate shows high FDG uptake lesions with perilesional abscess, a mildly increased PSMA uptake, a low PSA value, a high ESR, and relevant clinical symptoms, tuberculosis should be considered and laboratory tests are required, especially when symptoms are relieved after successful anti-tuberculosis therapy. The final confirmation of the diagnosis still relies on pathological examination.
Introduction
Among extrapulmonary tuberculosis (EPTB) forms, urogenital tuberculosis ranks third after lymph node involvement and tuberculosis pleural effusion (1). The incidence of prostate tuberculosis is 6.6% of urogenital tuberculosis (2). It is primarily caused by distant lesions that spread to the prostate via the bloodstream. Meanwhile, it may also spread from renal tuberculosis. Symptoms and imaging examinations of prostate tuberculosis are atypical, which often need to be differentiated from a prostate malignant tumor. Prostate-specific membrane antigen (PSMA) is an ideal diagnostic and therapeutic target for prostate cancer since it has low levels of expression in normal prostate tissues and non-prostate cancer tissues. In this study, we reported a case of a 51-year-old man with systemic tuberculosis involving the prostate, who had a high erythrocyte sedimentation rate (ESR) but a normal Prostate-specific antigen (PSA) value. His prostate showed a high fluoro-D-glucose (FDG) uptake but a slight PSMA uptake during positron emission tomography combined with computed tomography (PET/CT).
Case report
A 51-year-old male presented with night sweats, loss of appetite, and 10 kg weight loss over the past 6 months. He had difficulty urinating for more than 3 months. Therefore, he came to the hospital for laboratory tests and imaging investigations of the urinary system. Some important dates and times, as well as the magnetic resonance imaging (MRI), 2-Deoxy-2-[fluorine-18]-fluoro-D-glucose (18F-FDG), and [fluorine-18]-prostate-specific membrane antigen (18F-PSMA) of the patient, are shown in Supplementary Figure S1. The laboratory tests revealed a high ESR of 77 mm/h (normal range, 0-15 mm/h), normal free prostate-specific antigen (f-PSA) of 0.151 ng/mL and total prostate-specific antigen (t-PSA) of 1.900 ng/mL, and slightly high neuron-specific enolase (NSE) of 20.19 ng/mL (normal range, <16.3 ng/mL). The MRI showed prostate lesions with isointensity on T1-weighted imaging (T1WI), heterogeneous intensity on T2-weighted imaging (T2WI) (Figure 1A), heterogeneous hyperintensity on diffusion-weighted imaging (DWI) (Figure 1B), and an apparent diffusion coefficient (ADC) with hypointensity (Figure 1C). A lesion with hyperintensity on T2WI was observed around the right iliopsoas muscle (Figure 1D). Bilateral iliac bone destruction and multiple swollen lymph nodes adjacent to the right iliac vessels were also found (Figure 1E). The possibility of prostate cancer with bone metastasis was considered.

Figure 1. MRI imaging. The prostate lesions showed heterogeneous intensity on T2WI (A), heterogeneous hyperintensity on DWI (B), and an apparent diffusion coefficient (ADC) with hypointensity (C). A lesion with hyperintensity on T2WI around the right iliopsoas muscle (D). Bilateral iliac bone destruction on T1WI (E).
18F-FDG and 18F-PSMA PET/CT were performed to further evaluate the overall condition. 18F-PSMA was developed through the method of 18F-aluminum fluoride (Al18F) labeling in our hospital (3). The 3-dimensional maximum intensity projection (MIP) image of the 18F-FDG PET/CT showed multiple FDG-avid lesions (Figure 2A). The prostate displayed an unevenly increased FDG uptake, especially on the right side, with an SUVmax of 17.6 (Figure 2B). A low-density lesion on the right iliopsoas muscle showed a high FDG uptake with an SUVmax of 18.6 (Figure 2C). Multiple osteolytic bone destruction was observed in the spine, bilateral ribs, bilateral iliac bones, and the right acetabulum, with an elevated FDG uptake and an SUVmax of 10.3 (Figure 2D). In the abdomen, chest, left armpit, and bilateral neck, multiple lymph nodes showed an increased FDG uptake, with an SUVmax of 18.7 (Figure 2E). The 18F-PSMA PET/CT demonstrated multiple systemic PSMA-avid lesions on the MIP image (Figure 2F). A slightly unevenly increased PSMA uptake was noted in the prostate, with an SUVmax of 3.2 (Figure 2G). In the low-density lesion of the right iliopsoas muscle, the PSMA uptake was slightly unevenly increased and SUVmax was 3.1 (Figure 2H). There was a slightly increased PSMA uptake in the bones and lymph nodes (Figures 2I,J).
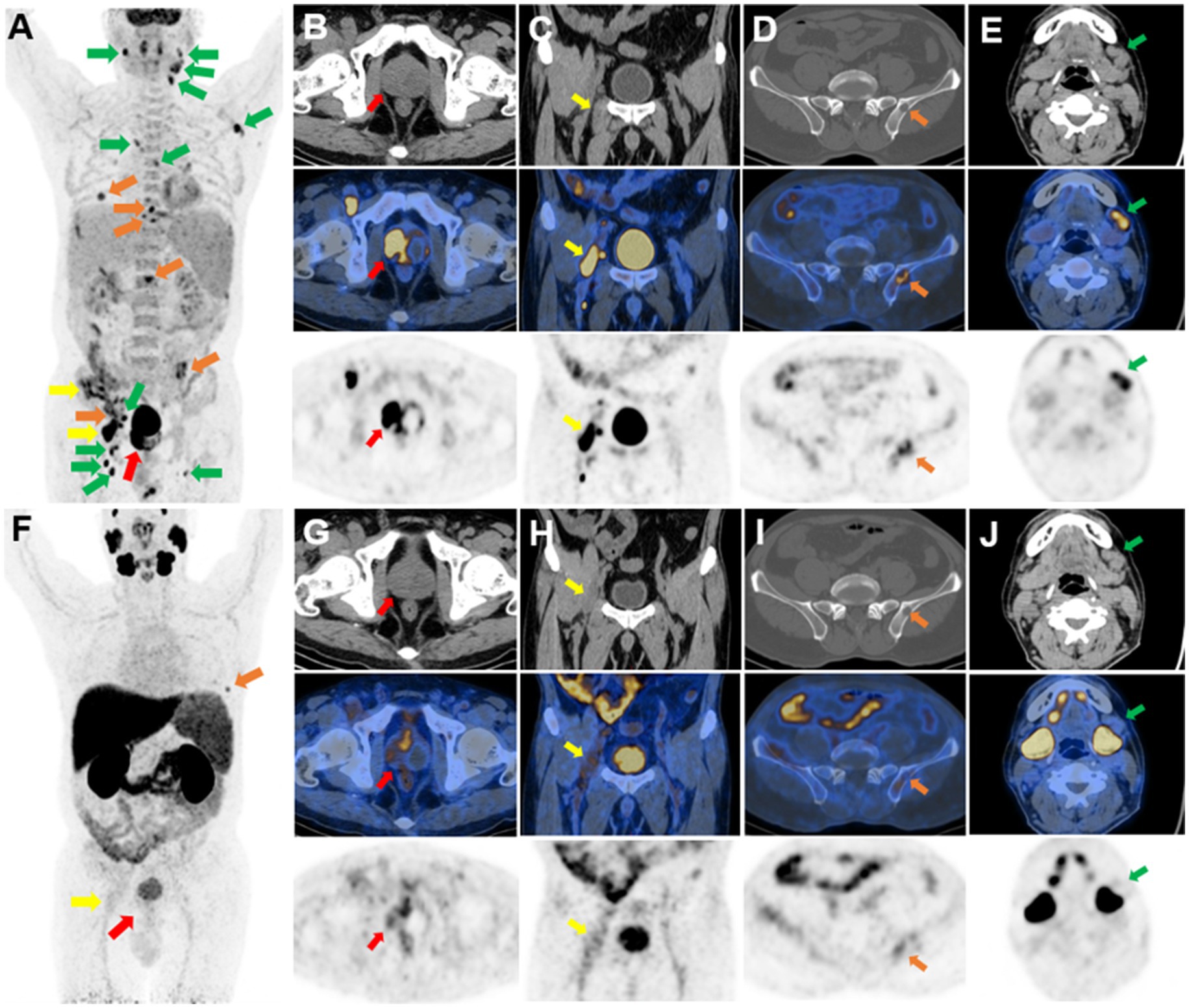
Figure 2. 18F-FDG and 18F-PSMA PET/CT imaging. Multiple FDG-avid lesions (A) on PET MIP images. An unevenly increased FDG uptake on the right side of the prostate, with an SUVmax of 17.6 (B). A high FDG uptake in a low-density lesion on the right iliopsoas muscle, with an SUVmax of 18.6 (C). Destruction of the left iliac bone with an increased FDG uptake (D). Multiple lymph nodes of the left neck with a high FDG uptake (E). Multiple PSMA-avid lesions (F) on PET MIP images. A slightly unevenly increased PSMA uptake in the prostate (G), the low-density lesion of the right iliopsoas muscle (H), bones (I), and lymph nodes (J).
A transperineal ultrasound-guided (TPUS) 12-core prostate biopsy revealed multifocal necrosis with granulomatous lesions (Figure 3A) and multinucleated giant cell reaction (Figure 3B). Immunohistochemistry of the bilateral internal lower puncture tissues showed CK34βE12 (+), P504S (−), and P63 (+). In addition, based on the positive result of tuberculosis infection of the T cell spot test, systemic tuberculosis was diagnosed. After 6 months of a standard anti-tuberculosis treatment with isoniazid 0.3 g, qd, the patient’s symptoms of dysuria, night sweats, and loss of appetite significantly improved. From the patient’s perspective, he experienced symptom relief, gained a better appetite, and felt less uncomfortable during urination. His overall quality of life had been greatly improved.
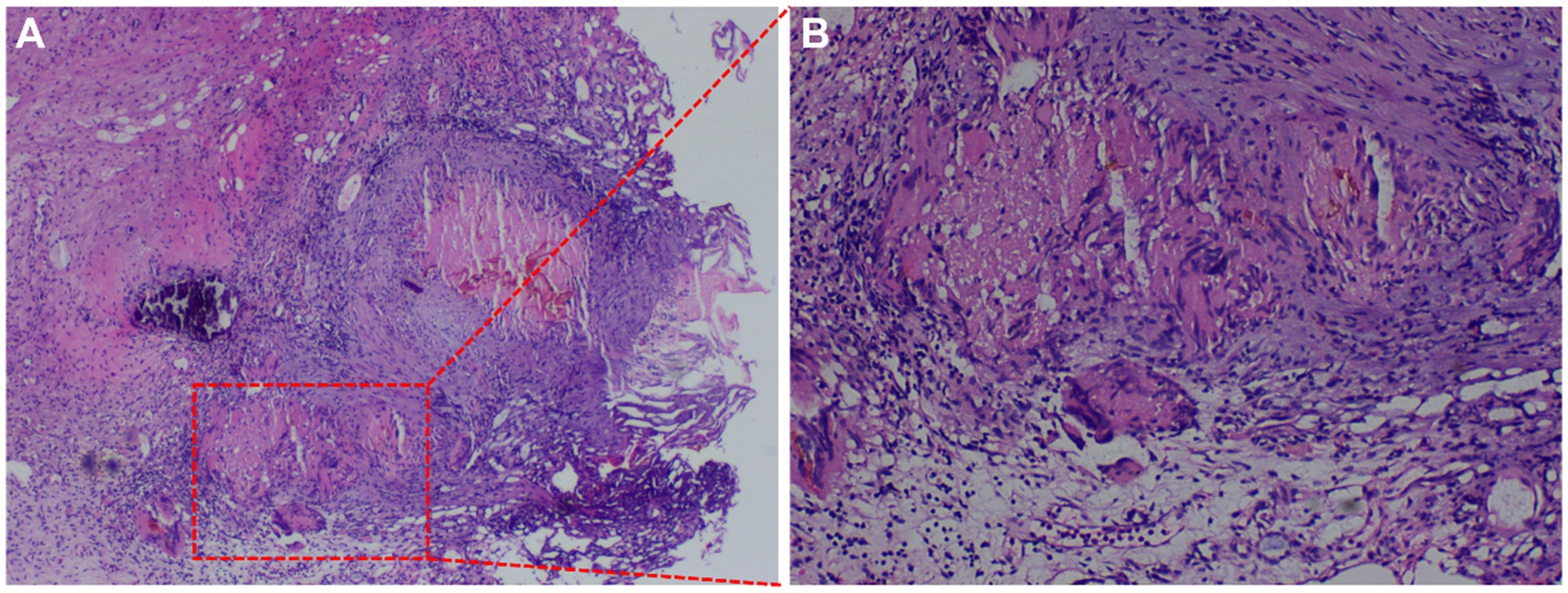
Figure 3. Acid-fast staining of prostate biopsy. (A) Multifocal necrosis with granulomatous lesions (×40). (B) Multinucleated giant cell reaction (×100).
Discussion
Tuberculosis remains a serious public health problem, especially in developing countries. The condition of prostate tuberculosis is an idiopathic infective granulomatous prostatitis, which is often accompanied by both seminal vesicle and epididymal tuberculosis. The prostate is more likely to be affected by hematogenous spread than through the urinary system (4, 5). Prostate tuberculosis is usually asymptomatic, but it can include symptoms such as urinary tract irritation and hematuria. Prostate nodules can be detected during digital rectal examination. At the same time, PSA levels may be normal or elevated, while urine analysis and urine culture are generally negative (6). Cancerous glands lack basal cells, which are found in benign glands. Thus, when confronted with an ambiguous lesion, markers of basal cells (CK34βE12 and P63) are usually used to identify the basal cells (7–9). CK34βE12 and P63 positivity argue against the diagnosis of invasive prostatic carcinoma (9, 10). P504S is a positive marker of prostate carcinoma with high sensitivity (11–13).
Imaging examination plays an important role in prostate tuberculosis. MRI findings of prostate tuberculosis typically show isointensity on T1WI and diffuse or focal hypointensity on T2WI. T2WI of prostate cancer also often shows hypointensity (6). DWI reflects the diffusion ability of water molecules. Due to tight intercellular connections and limited water, prostate cancer typically shows significant limited diffusion or no diffusion and low ADC values. Prostate tuberculosis can also show limited diffusion on DWI or low values on ADC, but the signal is higher than that of prostate cancer, showing significant differences (14). Transrectal ultrasound (TRUS) of prostate tuberculosis has no specific features according to previous literature (6). Hypoechoic lesions, prostate enlargement, and calcification caused by caseous necrosis can be seen. In our study, prostate enlargement with calcification was observed in the patient. Hence, it is often difficult to distinguish prostate tuberculosis from benign prostatic hyperplasia, a prostate malignant tumor, and a urinary tract infection because of their similar clinical and imaging changes. Therefore, we need to enhance the understanding of imaging manifestations of prostate tuberculosis for a better diagnosis in the early stage.
PET is a valuable tool for prognostication and treatment response assessment due to its high sensitivity capabilities for lesion detection at nanomolar concentrations and its quantification capabilities. The most common radiopharmaceutical used in research and clinical practice for PET imaging is FDG, a glucose analogue. However, one major limitation of using FDG is the high false-positive rate due to its poor specificity. Prostatic tissues physiologically express PSMA, a Type II transmembrane protein. However, it is significantly overexpressed by prostate cancer cells (15), and its expression increases with tumor aggressiveness (16). Although PSMA is considered a specific biomarker of prostate cancer, it has been reported that angiogenic factors may stimulate the production of PSMA in tuberculosis tissues. PSMA activity in prostate tuberculosis may partially be attributed to the inflammation caused by infection with Mycobacterium tuberculosis, which leads to increased capillary penetration. Physiological reparative reactions within the neovasculature may be another explanation (17). It has been reported that spinal (18), pulmonary (19), and cerebral tuberculosis (17) have an increased uptake of 68Ga-PSMA (SUVmax 2.3–9.6). Compared with latent infection, PSMA avidity may indicate a greater likelihood of active infection (17). In previous studies, PSMA-avid prostate mycobacterial infection has not been reported. In addition, a study by Vorster et al. demonstrated that 68Ga-citrate PET/CT is better than FDG PET/CT at imaging pulmonary tuberculosis (PTB) and brain parenchyma tuberculosis (20). Due to the formation of a dense fibrotic cuff around the tuberculosis lesions, radiolabeled inhibitors of fibroblast activation protein (68Ga-FAPI) targeting fibrosis have been synthesized for the PET imaging of tuberculosis. Several cases of PTB and extrapulmonary tuberculosis (EPTB), which have an incidental uptake of 68Ga-FAPI (21, 22), have been reported.
In this study, the patient had an elevated ESR but a normal PSA value. The prostate lesion manifested a significant increase in the FDG uptake and a slight increase in the PSMA uptake. Multiple osteolytic bone destruction, lymph nodes with an increased FDG uptake, and mildly increased PSMA expression were observed throughout the body. These should be distinguished from the neuroendocrine differentiation in prostate malignant tumors with systemic metastasis, lymphoma, or prostate sarcoma. However, distant lymph nodes are rarely metastatic sites of prostate malignant tumors, and the systemic disease should be considered. A high PSMA uptake in the prostate misled our diagnosis, but the pathological diagnosis was tuberculosis. Indeed, tuberculosis exhibits an increased PSMA uptake under certain circumstances.
Conclusion
Clinical and imaging manifestations of prostate tuberculosis are atypical. The possibility of tuberculosis should be taken into account in cases where prostate lesions exhibit a high FDG uptake with perilesional abscess, which is rarely observed in metastatic cancer, a mild PSMA uptake elevation, low PSA levels, and pertinent clinical symptoms with infection. Laboratory tests are imperative for further evaluation. However, the ultimate confirmation of the diagnosis still relies on pathological examination.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XS: Conceptualization, Writing – original draft, Writing – review & editing. YQ: Conceptualization, Data curation, Investigation, Writing – original draft. LS: Formal analysis, Methodology, Software, Writing – review & editing. LK: Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (82171970), the Beijing Science Foundation for Distinguished Young Scholars (JQ21025), the Beijing Municipal Science & Technology Commission (Z221100007422027), National High Level Hospital Clinical Research Funding (Interdisciplinary Research Project of Peking University First Hospital, 2023IR17).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1430300/full#supplementary-material
References
1. Figueiredo, AA, Lucon, AM, and Srougi, M. Urogenital tuberculosis. Microbiology. Spectrum. (2017) 5:1. doi: 10.1128/microbiolspec.TNMI7-0015-2016
2. Kadouri, Y, Zaoui, Y, and Bondil, P. Pauci-symptomatic disseminated tuberculosis revealed by an increase in the specific antigen of the prostate. Urol Case Rep. (2020) 33:101312. doi: 10.1016/j.eucr.2020.101312
3. Duan, X, Cao, Z, Zhu, H, Liu, C, Zhang, X, Zhang, J, et al. 68Ga-labeled ODAP-urea-based PSMA agents in prostate cancer: first-in-human imaging of an optimized agent. Eur J Nucl Med Mol Imaging. (2022) 49:1030–40. doi: 10.1007/s00259-021-05486-x
4. Sporer, A, and Auerbach, O. Tuberculosis of prostate. Urology. (1978) 11:362–5. doi: 10.1016/0090-4295(78)90232-7
5. Kundasamy, P, Kemp, B, Kearns, D, McCallum, A, Nazir, S, and Lyon, PC. A rare case of disseminated genitourinary tract tuberculosis complicated by emphysematous prostatitis and seminal vesicle abscess. BJR Case Rep. (2023) 9:20220101. doi: 10.1259/bjrcr.20220101
6. Li, Y, Dan, S, Yang, F, He, X, He, L, and Yue, W. Prostate tuberculosis mimicking prostate cancer: case report and literature review. Medicine. (2023) 102:e36172. doi: 10.1097/MD.0000000000036172
7. Wojno, KJ, and Epstein, JI. The utility of basal cell-specific anti-cytokeratin antibody (34 beta E12) in the diagnosis of prostate cancer. A review of 228 cases. Am J Surg Pathol. (1995) 19:251–60. doi: 10.1097/00000478-199503000-00002
8. Kahane, H, Sharp, JW, Shuman, GB, Dasilva, G, and Epstein, JI. Utilization of high molecular weight cytokeratin on prostate needle biopsies in an independent laboratory. Urology. (1995) 45:981–6. doi: 10.1016/S0090-4295(99)80118-6
9. Shah, RB, Zhou, M, LeBlanc, M, Snyder, M, and Rubin, MA. Comparison of the basal cell-specific markers, 34betaE12 and p63, in the diagnosis of prostate cancer. Am J Surg Pathol. (2002) 26:1161–8. doi: 10.1097/00000478-200209000-00006
10. Hasan, IA, Gaidan, HA, and Al-kaabi, MM. Diagnostic value of cytokeratin 34 beta E12 (Ck34βE12) and α-Methylacyl-CoA racemase (AMACR) Immunohistochemical expression in prostatic lesions. Iran J Pathol. (2020) 15:232–8. doi: 10.30699/ijp.2020.113544.2229
11. Varma, M, and Jasani, B. Diagnostic utility of immunohistochemistry in morphologically difficult prostate cancer: review of current literature. Histopathology. (2005) 47:1–16. doi: 10.1111/j.1365-2559.2005.02188.x
12. Jiang, Z, Wu, CL, Woda, BA, Iczkowski, KA, Chu, PG, Tretiakova, MS, et al. Alpha-methylacyl-CoA racemase: a multi-institutional study of a new prostate cancer marker. Histopathology. (2004) 45:218–25. doi: 10.1111/j.1365-2559.2004.01930.x
13. Kumaresan, K, Kakkar, N, Verma, A, Mandal, AK, Singh, SK, and Joshi, K. Diagnostic utility of α-methylacyl CoA racemase (P504S) & HMWCK in morphologically difficult prostate cancer. Diagn Pathol. (2010) 5:83. doi: 10.1186/1746-1596-5-83
14. Radwan, A, Menias, CO, El-Diasty, MT, Etchison, AR, Elshikh, M, Consul, N, et al. Multimodality imaging of genitourinary tuberculosis. Curr Probl Diagn Radiol. (2021) 50:867–83. doi: 10.1067/j.cpradiol.2020.10.005
15. Silver, DA, Pellicer, I, Fair, WR, Heston, WD, and Cordon-Cardo, C. Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res. (1997) 3:81–5.
16. Bostwick, DG, Pacelli, A, Blute, M, Roche, P, and Murphy, GP. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer. (1998) 82:2256–61. doi: 10.1002/(SICI)1097-0142(19980601)82:11<2256::AID-CNCR22>3.0.CO;2-S
17. Wong, VCK, Shen, L, Nasser, E, Adams, DN, and Mansberg, R. 68Ga-prostate-specific membrane antigen uptake in cerebral tuberculosis. Clin Nucl Med. (2020) 45:238–40. doi: 10.1097/RLU.0000000000002910
18. Gupta, N, Elumalai, RK, Verma, R, Belho, ES, and Dhawan, S. Spinal tuberculosis mimicking as prostate cancer metastases in Ga-68 prostate-specific membrane antigen positron-emission tomography/computed tomography. Indian J Nuclear Med. (2020) 35:271–3. doi: 10.4103/ijnm.IJNM_56_20
19. Liu, H, Liu, Y, Chen, Y, and Liu, H. 68Ga-PSMA uptake in pulmonary tuberculosis: a pitfall in prostate cancer PET imaging. Nuklearmedizin Nuclear Med. (2021) 60:252–3. doi: 10.1055/a-1312-6148
20. Vorster, M, Maes, A, van de Wiele, C, and Sathekge, M. 68Ga-citrate PET/CT in tuberculosis: a pilot study. Q J Nuclear Med Mol Imaging. (2019) 63:48–55. doi: 10.23736/S1824-4785.16.02680-7
21. Deng, Y, Wu, J, Xu, C, and Zhang, W. Primary solitary tuberculosis in the hepatic round ligament detected by 68Ga-FAPI PET/CT. Clin Nucl Med. (2022) 47:e414–6. doi: 10.1097/RLU.0000000000004122
Keywords: prostate, tuberculosis, 18F-FDG, 18F-PSMA, PET/CT
Citation: Sun X, Qiu Y, Song L and Kang L (2024) Case report: Systemic tuberculosis with prostate involvement mimicking prostate cancer with multiple metastases on 18F-FDG and 18F-PSMA PET/CT. Front. Med. 11:1430300. doi: 10.3389/fmed.2024.1430300
Edited by:
Domenico Albano, University of Brescia, ItalyReviewed by:
Edel Noriega-Álvarez, University Hospital of Guadalajara, SpainCarmelo Caldarella, Fondazione Policlinico Universitario A. Gemelli IRCCS, Italy
Copyright © 2024 Sun, Qiu, Song and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Kang, a2FuZ2xlaUBiam11LmVkdS5jbg==
 Xinyao Sun
Xinyao Sun Yongkang Qiu
Yongkang Qiu Lele Song
Lele Song Lei Kang
Lei Kang