- 1Department of Surgery, National Hospital, Abuja, Nigeria
- 2Department of Surgery, Lagos University Teaching Hospital, Lagos, Nigeria
- 3Department of Obstetrics and Gynaecology, Ahmadu Bello University Teaching Hospital, Zaria, Nigeria
- 4Department of Surgery, University College Hospital, Ibadan, Nigeria
- 5Department of Maxillofacial Surgery, University of Maiduguri Teaching Hospital, Maiduguri, Nigeria
- 6Department of Surgery, River State University Teaching Hospital, Port Harcourt, Nigeria
- 7Smile Train Africa, Lagos, Nigeria
- 8Department of Surgery, Federal Medical Centre, Umuahia, Abia, Nigeria
Background: Limited research capacity has contributed to the lack of high-quality research from low-and middle-income countries. This is compounded by limited research training opportunities. Research capacity scale-up training was deployed as part of the implementation of the National Surgical, Obstetrics, Anaesthesia, and Nursing Plan for Nigeria. We report the impact of this locally contextualized efforts to scale up research capacity in sub-Saharan Africa.
Methods: This is an evaluation of the training of 65 participants in research, grant writing and manuscript writing and publication. Pre- and post-training surveys using a 5-point Likert scale and open-ended questions were administered to evaluate the impact of the programme.
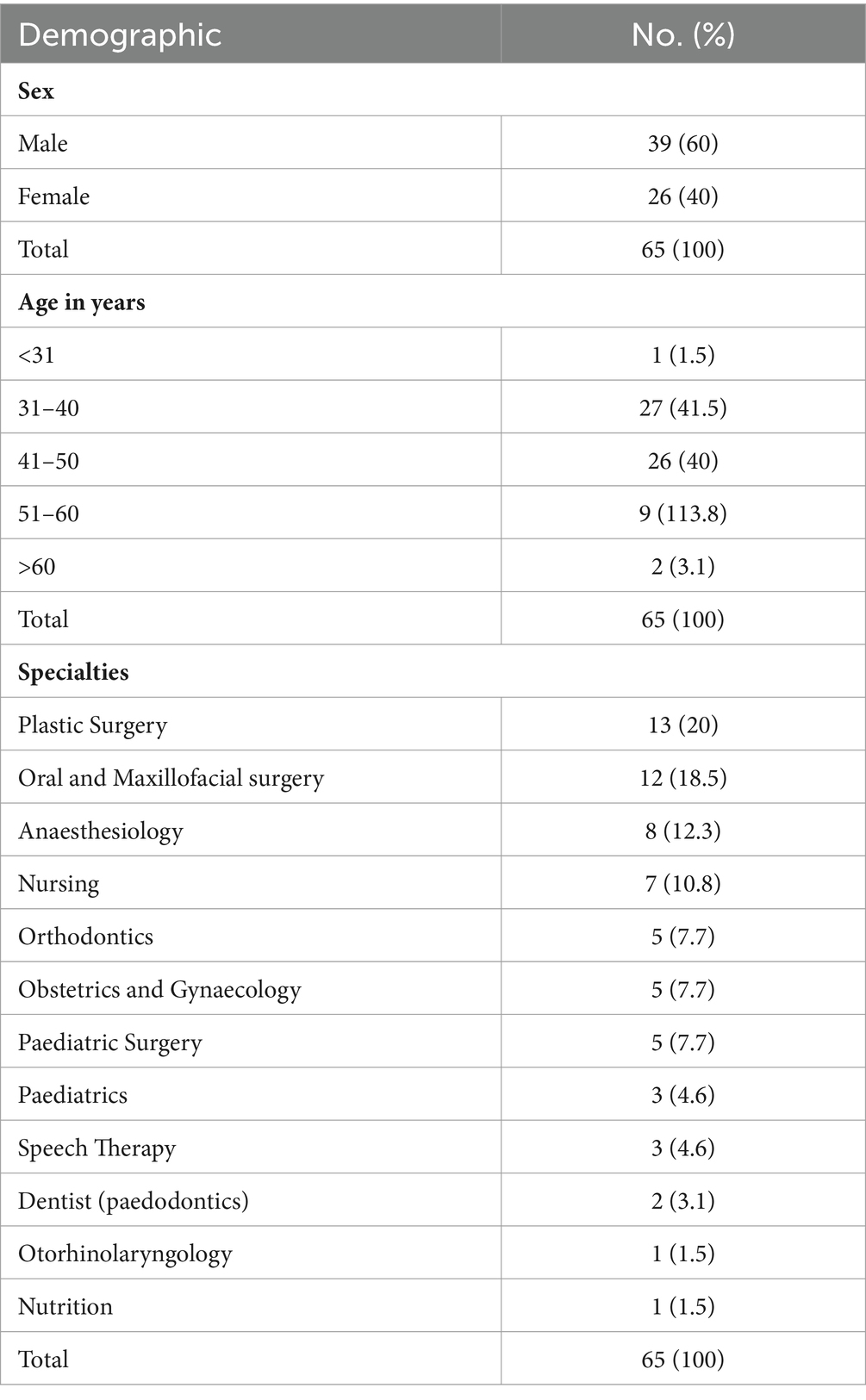
Results: There were 39 (60%) males and 26 (40%) females aged 26–62 years (median 42 years). Thirty-nine (60%) participants had previous training in research, but only 12 (18.5%) had previously received grant writing training, and 17 (26.2%) had previously received manuscript writing and publishing training. Following training, 45 (70.3%) participants agreed that the training was relevant. The research, grant writing and manuscript writing, and publication components of the training were rated high by the participants (45–59, 70.3–92.2%). However, 41.2% felt that there was not enough time, and 32.4% felt that the training was too comprehensive. Nearly all the participants agreed that the training had improved their skills in research, grant writing and manuscript writing and publication, and more than two-thirds subsequently engaged in informal mentoring of others. Overall, participants achieved success in designing their own research projects and publishing manuscripts and grants. Three (4.6%) of the participants had gone on to become faculty for the research training programme. The three top barriers encountered following training were time constraints (67.3%), lack of funding (36.5%) and not being able to find research collaborators (25%).
Conclusion: Outcome of this training programme is encouraging and highlights the feasibility and potential impact of deploying such programmes in low and middle income countries (LMICs). Despite the positive outcomes, barriers including time constraints, funding limitations, and difficulties in finding research collaborators remain to be addressed. Such training programmes need to be supported to strengthen the research capacity in this and similar settings.
Introduction
It is estimated that 30% of the global burden of disease is surgical (1). The contribution to this burden from low-and middle-income countries is at best estimated due to poor health information systems and research capacity (2). Research capacity is critical to development but has lagged in low-and middle-income countries compared to high-income countries, with sub-Saharan Africa contributing just 1.1% of global researches in 2013 (3).
Sub-Saharan Africa is currently experiencing significant challenges in surgical healthcare due to several factors, including limited resources, inadequate infrastructure, and a shortage of skilled personnel. Amidst these challenges, building research capacity becomes crucial to drive contextualized solutions and improve patient outcomes. Although progress is being made to address the burden of surgical diseases in the region, there remains a critical gap in research capacity (4). This deficit not only hampers the development and implementation of evidence-based practices but also limits the region’s ability to advocate for policy changes and secure funding for essential surgical services.
In low resource settings, research output is limited both in volume and quality. Much of this is due to limited training in research, poor research infrastructure, and very importantly, inadequate investments by countries in research. One report has noted that despite Africa making up 15% of the world’s population, it accounted for only 1.1% of global investments in research. In addition, sub-Saharan Africa invests 0.44% of GDP in research and development compared to 2.28–3.32% in North America and the European Union (5).
Nigeria’s Federal Ministry of Health prioritized scaling up research capacity as one of the key components of her National Surgical, Obstetrics, Anaesthesia and Nursing Plan (NSOANP) (6). The implementation of this plan has been made feasible through collaboration with nongovernmental organizations (7). North–south partnerships have hitherto contributed to improved research capacity in low-and middle-income countries (8–11). These efforts are rarely focused on the surgical healthcare workforce. In addition, the cost of such research capacity programmes is often not sustainable (11–13). For sustainability, the focus should now be more directed to encouraging locally led training programmes that have the potential to reach more participants at less cost. Nigeria’s NSOANP, therefore, deployed research training for the surgical healthcare workforce to teach the fundamentals of high-quality research, writing and publishing as well as research grants writing. This is a report on the outcome of this training and is intended to highlight the feasibility and impact of locally led and contextualized efforts to scale up research capacity in sub-Saharan Africa.
Materials and methods
This was a cross-sectional study of 65 participants who participated in research training in Nigeria from August 2021–April 2023. The training was funded by Smile Train Incorporated, New York, a cleft lip and palate focused organisation.
Participant selection
Participants were from surgical healthcare specialties and specialties involved in comprehensive cleft care in the 6 geopolitical zones of Nigeria. Invitations were sent to the cleft lip and palate team leads at institutions involved in comprehensive cleft care to nominate potential participants for training. In addition, NSOANP team lead asked institutions in areas without a cleft lip and palate team to nominate potential participants from surgical healthcare specialties. Nominated participants were requested to provide a statement on their interest in research and the training, if they had unanalysed research data, and at least two research ideas they would want to work on during the training. Participants who were able to provide this information were then selected for training, while ensuring representation across the 6 geopolitical zones.
Training programme
The 65 participants were in 6 different groups (10–12) and underwent in-person, intensive five-day interactive and hands-on training:
Training programme
The training programme consisted of a full 5-day schedule focusing on research design and conduct, grants writing and grants management, statistics and data analysis, as well as manuscript writing and publishing. The detailed schedule is provided in the attached Supplementary material S1. There was no pre-learning activity before the training. All the 6 groups had the same training schedule. However, based on feedback from earlier groups, later groups were given more examples and templates for Gant chart and grant budgeting. The first training was deployed in 2021.
Training faculty
The training faculty consisted of experienced and highly published biomedical researchers and an experienced biomedical statistician. The faculty all had previous experience in research mentoring. There were 5–6 faculty at each training session. The training faculty was composed of only local research experts in surgery and obstetrics and gynaecology, as well as trained biomedical statistician.
Training evaluation
Pre- and post-training evaluations were completed by the participants immediately before and after the training using a survey format. In addition, a follow-up survey was deployed 2 years after the first training session to evaluate the short-term impact of the training programme (3 months for the last group of participants). The survey consisted of questions structured on a five-point Likert scale as well as open-ended questions to evaluate participants’ knowledge, experience and perceived impact of the training. The surveys were deployed using the Survey Monkey® platform. The pre- and post-training surveys are presented in Supplementary material S2.
All participants who took part in the training were invited to participate in the surveys. Overall, 65 participants completed the pre-training evaluation, 64 completed the post-training evaluation and 52 completed the follow-up evaluation.
Data analysis
The data were analysed directly from the Survey Monkey® platform using the Statistical Package for the Social Sciences version 20. The 5-point Likert scale (strongly agree, agree, neutral, disagree, strongly disagree; and, very confident, confident, neither confident nor unconfident, unconfident, very unconfident) was compressed to a 3-point Likert scale (agree, neutral, disagree; and, confident, neutral, not confident) for the purpose of analysis. Descriptive data are expressed as percentages, medians, interquartile ranges, and qualitative data by creating themes from the open-ended responses.
Results
Demographics
There were 39 (60%) males and 26 (40%) females aged 26–62 years (median 42 years). Sixty-five participants were trained. The participants were from 11 different surgical healthcare and cleft care specialties (Table 1).
Pre-training evaluation
Thirty-nine (60%) participants had previous training in research, but only 12 (18.5%) had previously received grant writing training, and 17 (26.2%) had previously received manuscript writing and publishing training. In addition, 44 (67.7%) participants had presented a paper at a conference, 33 (50.8%) had a publication as a lead author, and three (4.6%) had received a research grant.
Post-training evaluation
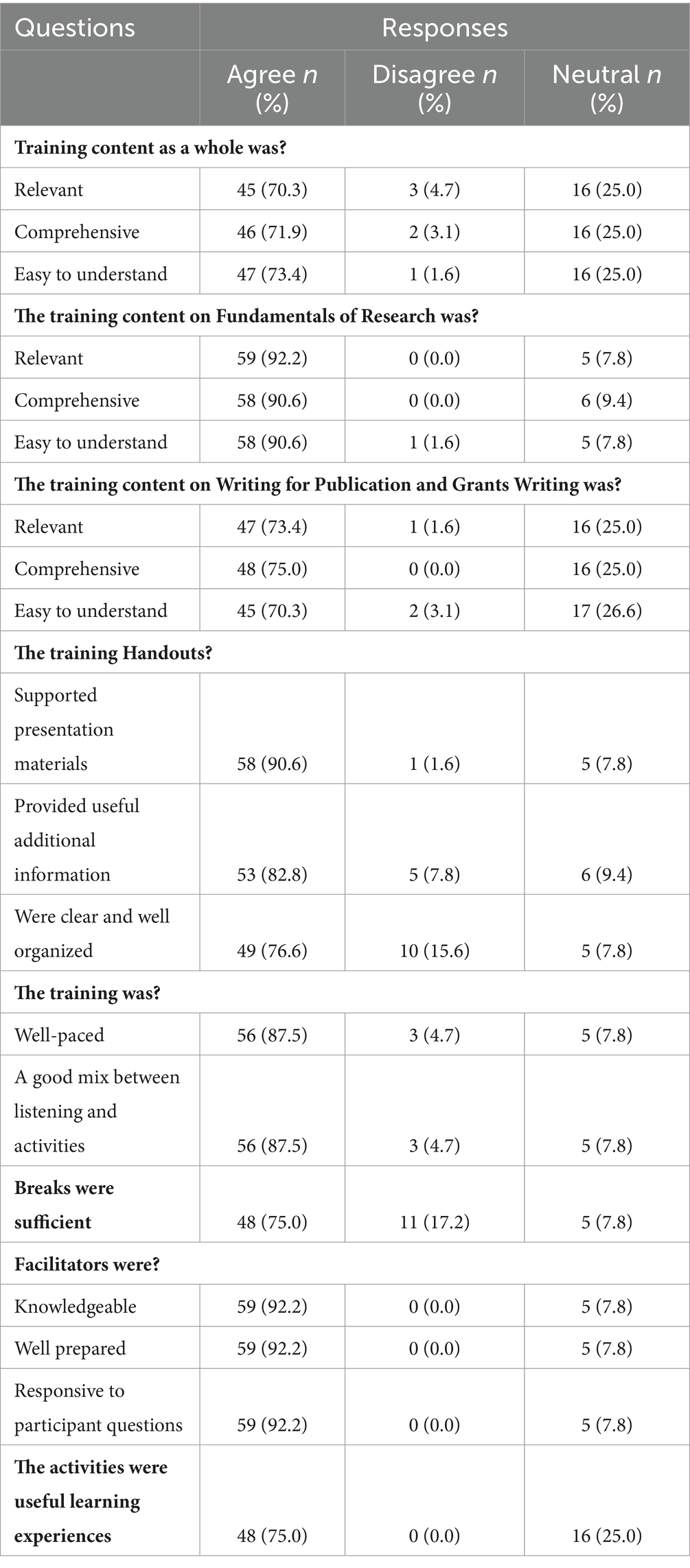
Following training, 45 (70.3%) participants agreed that the training was relevant, 46 (71.9%) agreed that it was comprehensive, and 47 (73.4%) agreed that it was easy to understand. The individual components of the training were also highly rated by the participants (45–59, 70.3–92.2%). Similarly, 53 (82.8%) participants agreed that the handouts for the training were useful, and 59 (92.2%) agreed that the faculty were knowledgeable and responsive to the participants’ training needs. Eleven (17.2%) participants disagreed that the breaks given during the training were sufficient (Table 2).
The thematic responses on what the participants liked best about the training showed that the faculty and learning structure had the highest response (57.9%). In addition, statistics (19.3%) and that they learned more about grants and manuscript writing (15.8%) were identified (Table 3). Regarding what they liked least about the training, 41.2% felt there was not enough time, and 32.4% felt the training was too comprehensive.
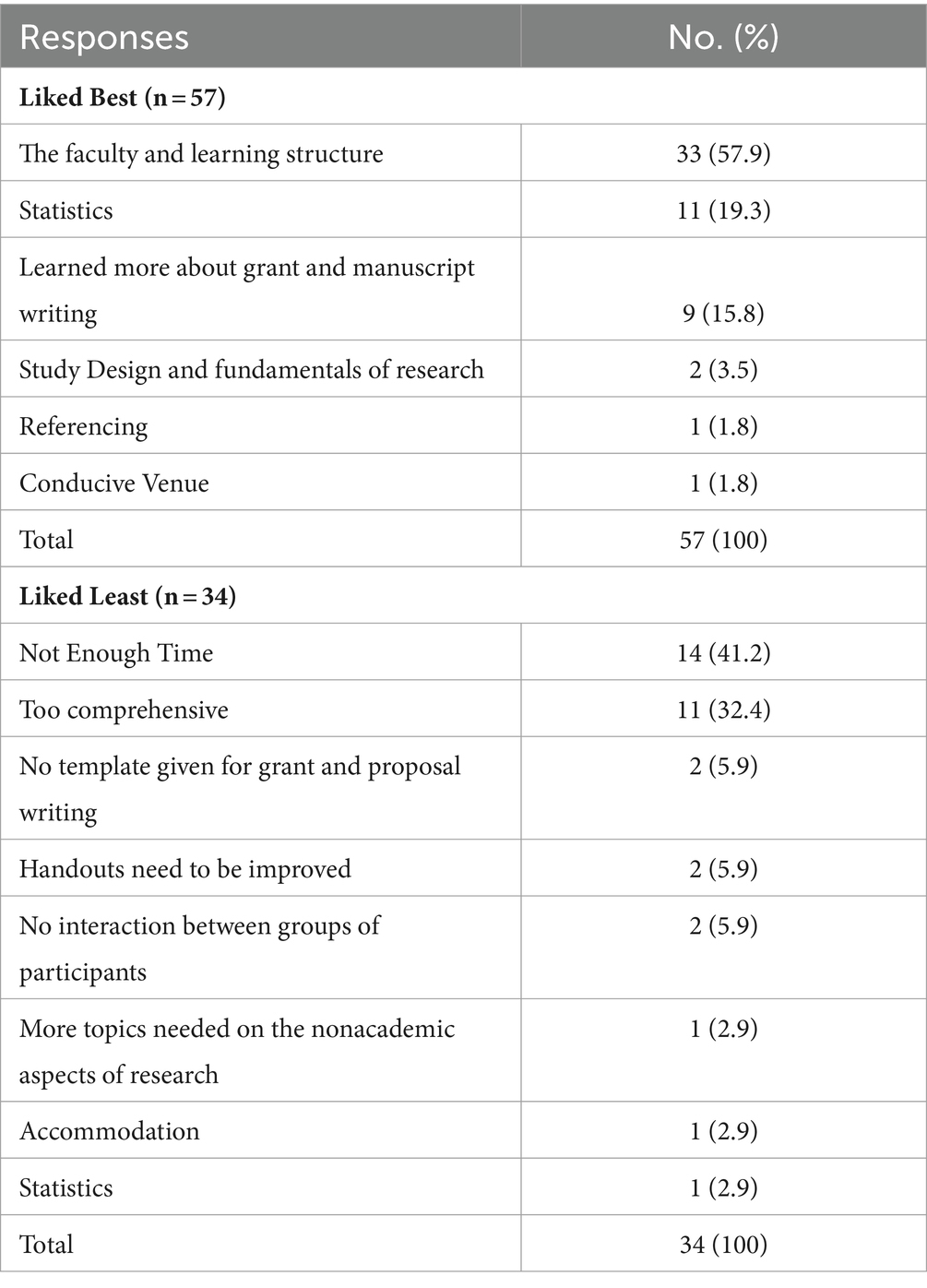
Table 3. Feedback from participants’ feedback on what they liked best and liked least about the training.
All 64 of the participants who responded to the post-training feedback said they would recommend the training to others. There was improvement in participants’ personal reflection on their skills and abilities after the training (Table 4). The participants rated their confidence in the process of conceiving and preparing research as well as writing a fundable research proposal that was mostly good and excellent after the training. They also reported that their confidence in writing a publishable scientific manuscript changed from poor to fair before the training to good and excellent after the training. One-third of the participants rated their ability to design and undertake a research project independently as good or excellent before the training. However, after the training, this ability was rated good to excellent by more than two-thirds of the participants.
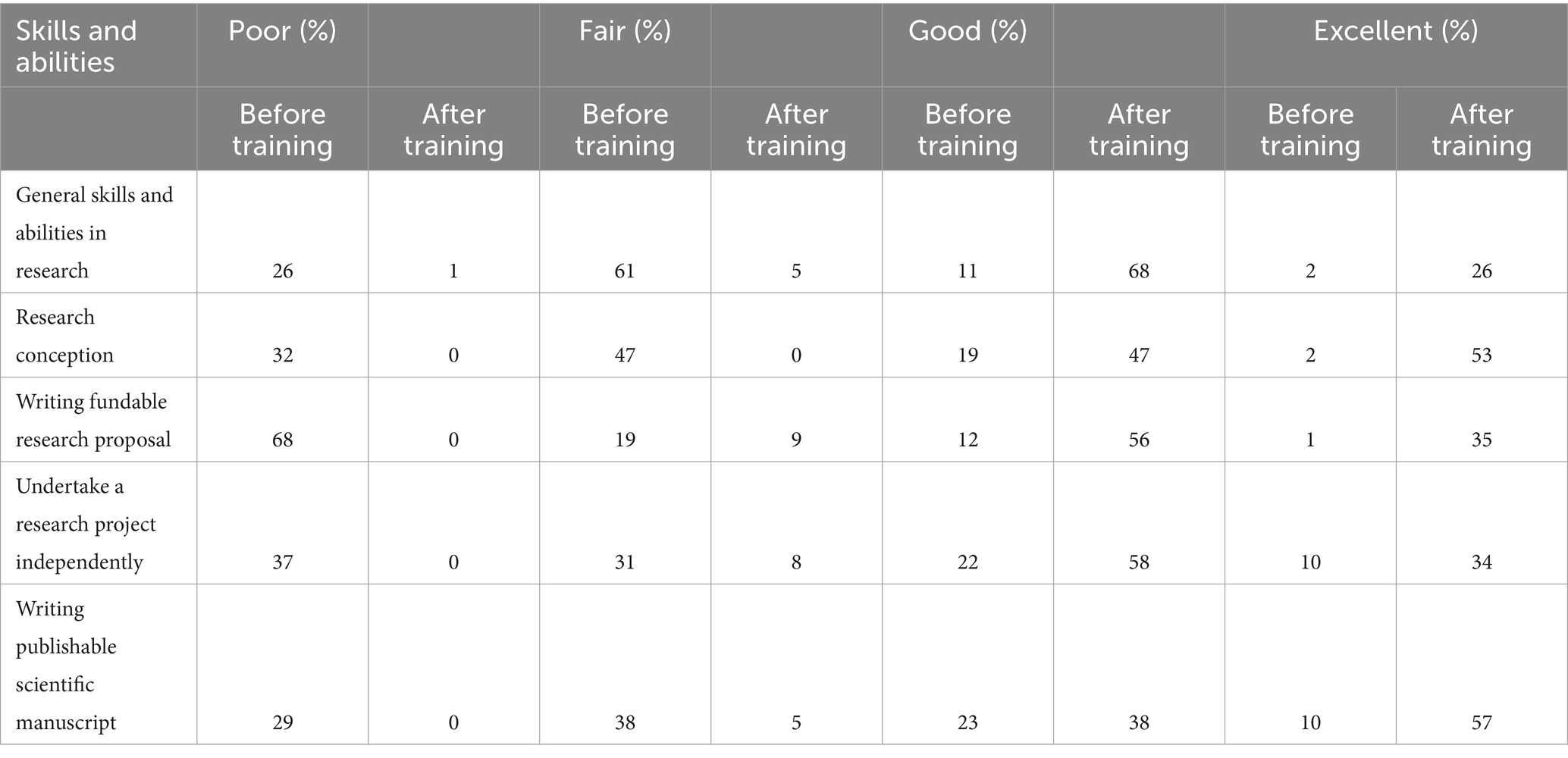
Table 4. Participants’ self-reported confidence in their skills and abilities in various aspects of research, grant writing and publishing.
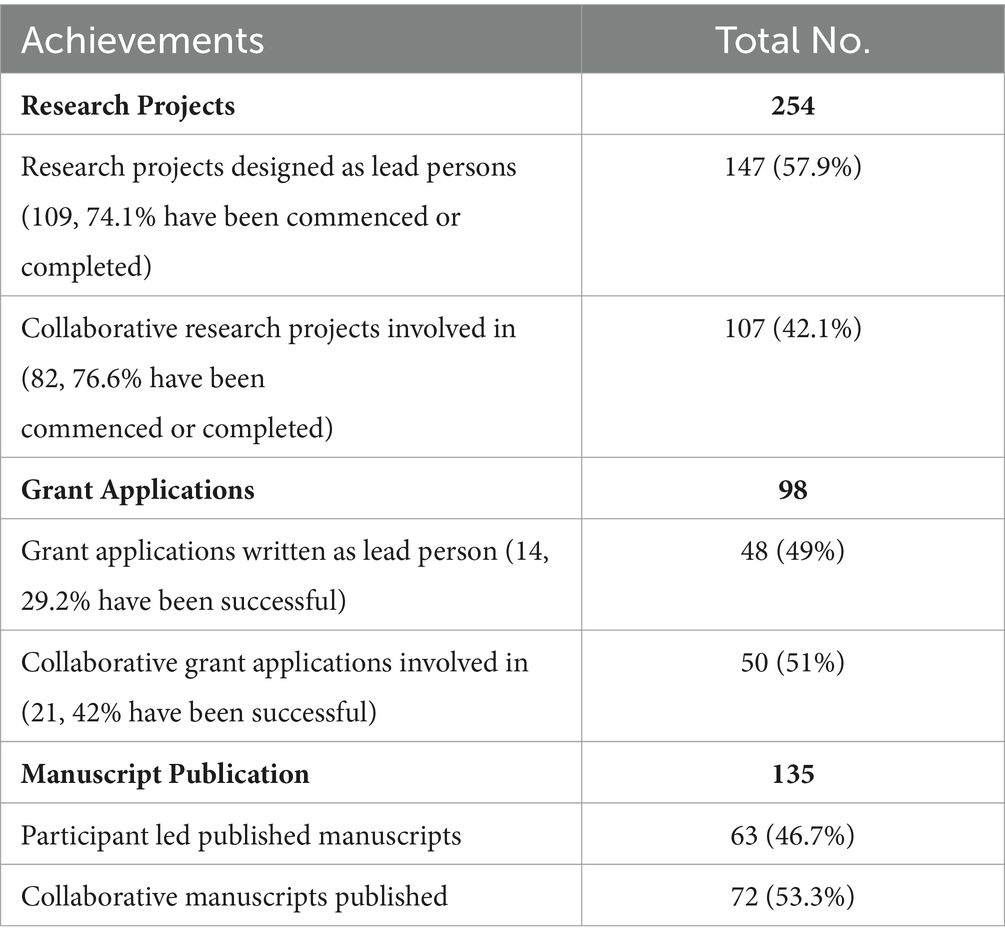
Impact of training on research output and grant application success
There was an 80% response to the follow-up evaluation to determine the impact of the training on research outputs and grant application success. The participants were asked to rate their level of agreement on the impact of the training on improvements in their skills in research conduct, grant writing and manuscript writing and publication. Nearly all the participants agreed that the training had improved their skills in these areas. In addition, 80% undertook informal mentoring of others in research, 69% in manuscript writing and publishing and 42% in grant writing. However, most (>50%) had not deployed any formal training or seminars in research, grant writing or manuscript writing and publishing (Figure 1). The majority of the participants felt that they were confident in research, manuscript writing and publication, and grant writing (Figure 2).
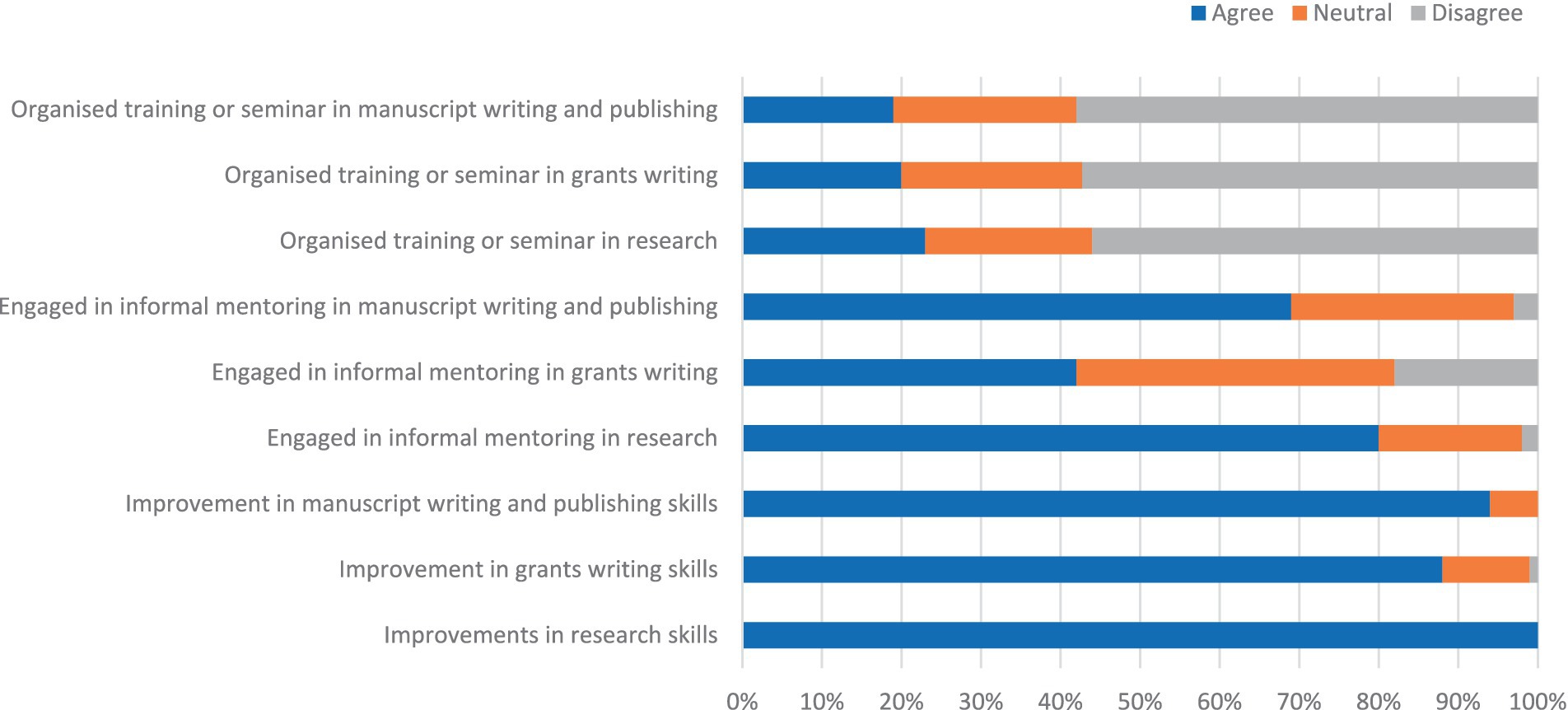
Figure 1. Improvements in participants’ skills and involvement in research, grant writing, and manuscript writing mentoring activities.
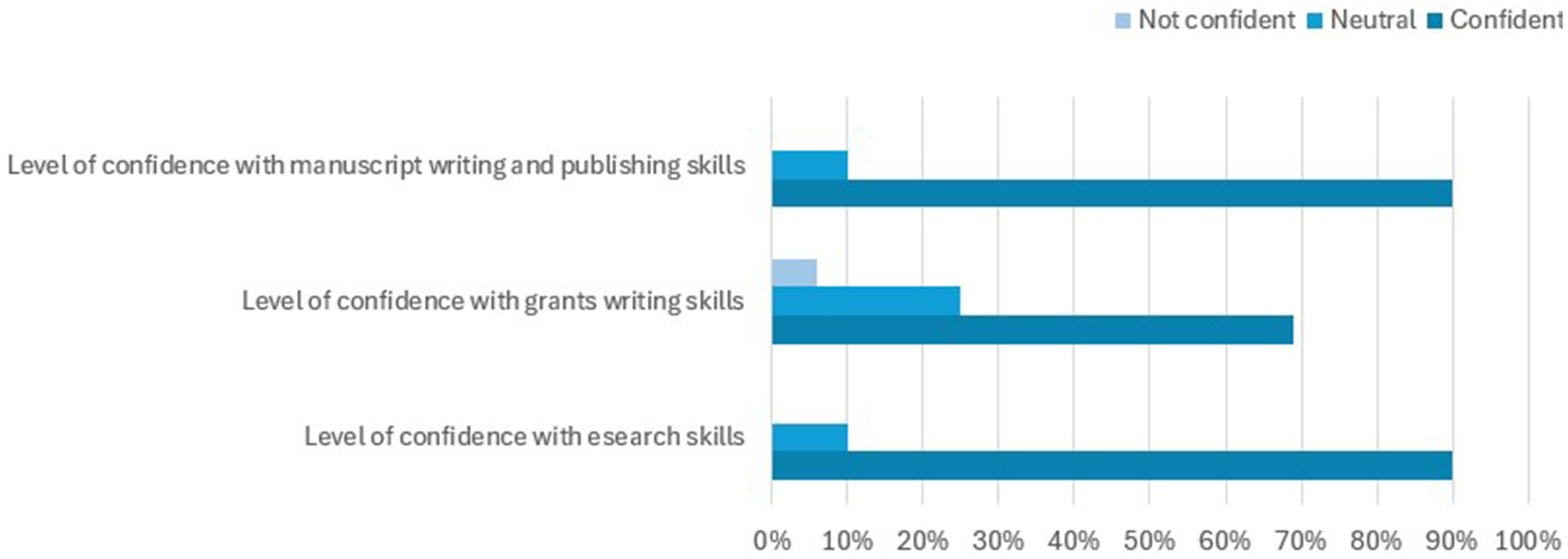
Figure 2. Participants’ level of confidence in their research, grant writing, and manuscript writing skills after training.
Overall, the 52 participants who completed the follow-up evaluation had 63 participant-led published manuscripts, 72 collaborative manuscripts, 14 successful participant-led grant applications and 21 successful collaborative grant applications. One hundred forty-seven research projects were designed by the participants as the lead persons (Table 5). In addition, 3 of the participants became faculty for subsequent NSOANP research training.
The three most common challenges and barriers encountered by the participants were time constraints (35, 67.3%), lack of funding (19, 36.5%) and not being able to find collaborators (13, 25%) (Table 6).
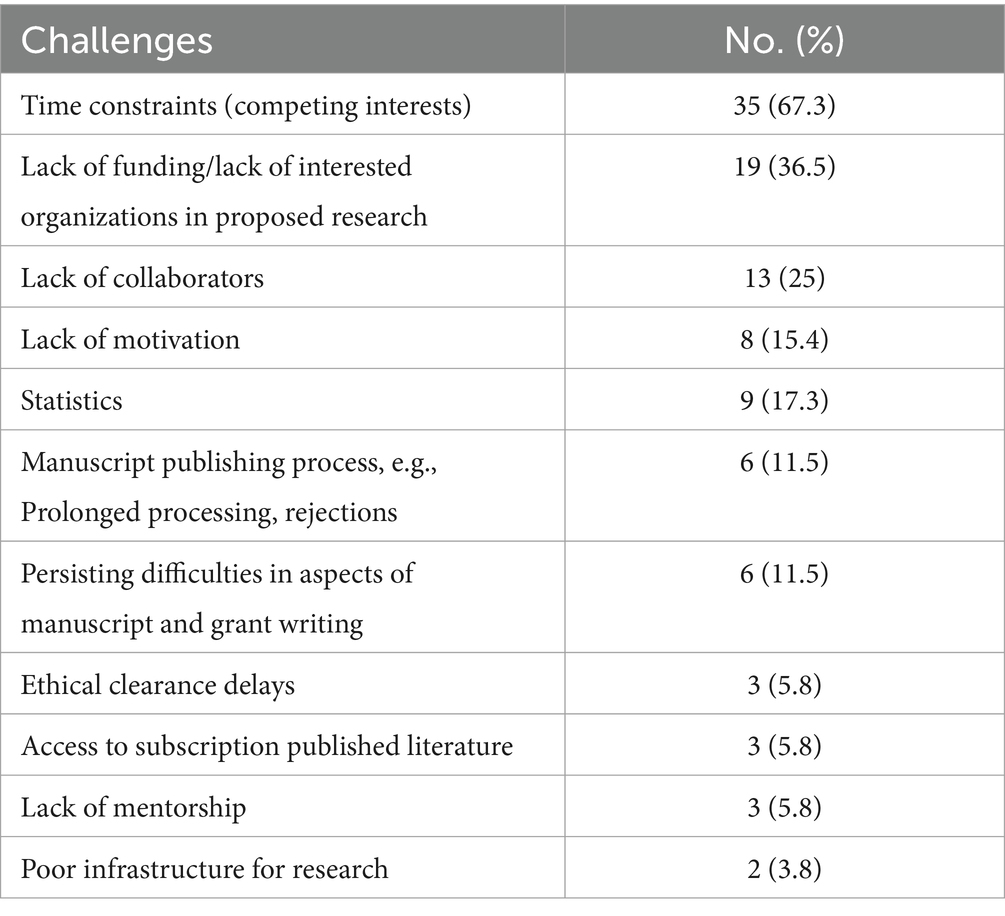
Table 6. Challenges and barriers encountered by 52 participants in research, grant writing and publication following training.
Discussion
The training model used in this study was in-person, intensive and hands-on. This approach enables the mentoring of participants to work on their own research ideas and data to immediately put into practice the knowledge and skills being acquired under onsite mentoring by faculty. In addition, this in-person model ensures protected time, avoids distractions, fosters learning, and is reported to facilitate research output (14, 15). Although the COVID-19 pandemic has resulted in the increasing use of online training programmes and engagements with obvious merits, in-person training has the advantages of encouraging protected time, removing distractions considerably and avoiding technical issues associated with internet connectivity (16, 17). Such technical internet connectivity issues are common in the setting and have the potential of losing valuable learning time. However, the virtual (online) platform could be deployed to support ongoing mentoring to strengthen the knowledge and skills acquired through in-person training.
Participants’ reception of training
The training was well received by the participants, as they particularly rated the faculty, learning structure and inclusion of statistics as the top three aspects of the training. The inclusion of grant writing was also rated as important. This is crucial, as success at grant applications has remained a challenge in LMICs, contributing to the perennial lack of research funding in the setting. Participants indicated a lack of enough time and an overly comprehensive nature of the training as what they liked least. This feedback created opportunities for improvements and restructuring for future courses.
Impact of training
The impact of research capacity strengthening programmes has been identified to be rather low compared to that of output and outcome measures (18). However, in our training programme, the participant-reported impact was encouraging, as skills in research, writing and publishing and grant writing improved. The finding that most participants were able to engage in informal mentoring of others is desirable and encouraging and would help to cascade the benefits of the training to reach a wider pool of researchers. However, the limited deployment of formal training seminars creates an opportunity for ongoing mentoring by faculty to support participants in this regard. This would potentially further extend the impact of the training.
The participants were successful at designing both individual and collaborative research, as well as publishing research manuscripts. This is an early indication that training is gradually impacting research capacity. A lack of access to grants has been previously identified as one of the barriers to surgical research in East Africa (19). In the present report, the participant-reported success at grant applications is encouraging. This was supported by the provision of competitive small grants by a funder. The provision of such competitive small funder-administered grants allows those trained in research to quickly put into practice the skills they have acquired. This has the potential to strengthen the acquired skills and success of the applications, gradually increasing their confidence and capacity for grant writing. This model should contribute to scaling up the capacity of LMIC practitioners to compete in the wider global research funding space. Unlike other training programmes that focus on the number of trainees reached (11, 20), our approach focuses on the impact of the training on immediate and short-term rated skills, abilities, and research output. Having shown the feasibility and encouraging impact of our approach, the next steps would be to begin to significantly increase the number of those trained and encourage their involvement in mentoring others to achieve a multiplier effect.
While the achievements of this training are encouraging, ongoing mentoring and tracking of impact and progress are crucial to ensuring continuous improvements and strengthening of research capacity in the setting. In addition, developing and strengthening the research infrastructure, which is presently weak in the setting, and incorporating graduated and appropriately structured research training into the curriculum of medical schools and surgical training would be necessary to strengthen overall research capacity in the setting.
Limitations
The main limitation of this report is that it includes a small number of participants mostly from healthcare specialties involved in cleft lip and palate care, and the findings may not be completely applicable to other healthcare specialties. However, it forms an important background to begin to build on for future training programmes.
Conclusion
Encouragingly, the participants expressed a willingness to recommend the training to others, and there was a notable increase in their confidence levels in research and manuscript writing. This was further supported by the observed improvements in research output and grant application success. Despite these positive outcomes, barriers such as time constraints, funding limitations, and difficulties in finding research collaborators remain. Addressing these barriers presents an opportunity for strengthening training programmes and fostering continued research productivity. Going forward, such training requires ongoing support and resources to sustain the gains and overcome the persistent challenges in research capacity in a low-resource setting. Our findings emphasise already acknowledged limitations in research capacity and highlight the need to urgently invest in scaling up surgical research capacity in the setting.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved as part of the implementation of NSOANP by Institutional Review Board (Health Research & Ethics Committee), National Hospital, Abuja, Nigeria. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because Pre-training and post-training evaluation were integral parts of the research training programme. Participants were informed that completion of the pre- and post-training evaluations were voluntary.
Author contributions
EA: Conceptualization, Formal analysis, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing, Resources. JS-O: Conceptualization, Formal analysis, Project administration, Writing – original draft, Writing – review & editing, Resources. NA: Conceptualization, Project administration, Writing – original draft, Writing – review & editing, Resources. AM: Writing – original draft, Writing – review & editing. MA: Writing – original draft, Writing – review & editing. OA: Writing – original draft, Writing – review & editing. NO: Funding acquisition, Writing – original draft, Writing – review & editing. IC: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The research training programme was funded by Smile Train Inc., New York, United States.
Acknowledgments
Smile Train, Inc., provided funding support for the research training programme. The Federal Ministry of Health in Nigeria provided oversight for the implementation of the NSOANP, of which scaling up research capacity is a key priority. We appreciate the suggestions from Dr. Chisom Udeigwe-Okeke, Dr. Aderonke Obisesan, and Mrs. Ngozi Opara, during the finalisation of the manuscript at the NSOANP technical review meeting.
Conflict of interest
NO is the Africa regional director for Smile Train.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: www.frontiersin.org/articles/10.3389/fmed.2024.1429168/full#supplementary-material
References
1. Shrime, MG, Bickler, SW, Alkire, BC, and Mock, C. Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health. (2015) 3:S8–9. doi: 10.1016/S2214-109X(14)70384-5
2. Meara, JG, Leather, AJM, Hagander, L, Alkire, BC, Alonso, N, Ameh, EA, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. (2015) 386:569–624. doi: 10.1016/S0140-6736(15)60160-X
3. United Nations Educational Scientific and Cultural, Organization. UNESCO Global Science Report: Towards 2030. UNESCO Publishing, Paris, (2015). Available at: https://uis.unesco.org/sites/default/files/documents/unesco-science-report-towards-2030-part1.pdf (Accessed April 27, 2024).
4. Bekele, A, Alayande, BT, Powell, BL, Obi, N, Seyi-Olajide, JO, Riviello, RR, et al. National Surgical Healthcare Policy Development and implementation: where do we stand in Africa? World J Surg. (2023) 47:3020–9. doi: 10.1007/s00268-023-07131-0
5. Seyi-Olajide, JO, Brindle, M, Faboya, O, Sleemi, A, Williams, O, and Ameh, EA. Is neocolonialism existing in global surgery practice? An analysis of a web-based survey amongst global surgery practitioners. J Glob Health Rep. (2024) 8:e2024016. doi: 10.29392/001c.117624
6. National surgical, obstetric and anaesthesia planning: Nigeria. Boston: Harvard Program in Global Surgery and Social Change; (2020). Available at: https://www.pgssc.org/national-surgical-planning (Accessed April 26, 2024).
7. Seyi-Olajide, JO, Anderson, JE, Williams, OM, Faboya, O, Amedu, JO, Anyanwu, SN, et al. National surgical, obstetric, anaesthesia and nursing plan, Nigeria. Bull World Health Organ. (2021) 99:883–91. doi: 10.2471/BLT.20.280297
8. Henschke, N, Mirny, A, Haafkens, JA, Ramroth, H, Padmawati, S, Bangha, M, et al. Strengthening capacity to research the social determinants of health in low-and middle-income countries: lessons from the INTREC programme. BMC Public Health. (2017) 17:514. doi: 10.1186/s12889-017-4399-0
9. Färnman, R, Diwan, V, Zwarenstein, M, and Atkins, SARCADE consortium. Successes and challenges of north–south partnerships – key lessons from the African/Asian regional capacity development projects. Glob Health Action. (2016) 9:30522. doi: 10.3402/gha.v9.30522
10. Olaleye, DO, Odaibo, GN, Carney, P, Agbaji, O, Sagay, AS, Muktar, H, et al. Enhancement of health research capacity in Nigeria through north–south and in-country partnerships. Acad Med. (2014) 89:S93–7. doi: 10.1097/ACM.0000000000000353
11. Jack, HE, Merritt, C, Medhin, G, Musesengwa, R, Mafuta, C, Gibson, LJ, et al. Developing sustainable capacity-building in mental health research: implementation outcomes of training of trainers in systematic reviewing. Glob Health Action. (2020) 13:1715325. doi: 10.1080/16549716.2020.1715325
12. Fonn, S, Hu, J, Igumbor, JO, Gatoto, D, Muula, A, and Ezeh, A. Quantifying the cost of in-kind contributions to a multidonor-funded health research capacity-building programme: the case of the consortium for advanced research training in Africa. BMJ Glob Health. (2020) 5:e002286. doi: 10.1136/bmjgh-2020-002286
13. Vicente-Crespo, M, Agunbiade, O, Eyers, J, Thorogood, M, and Fonn, S. Institutionalizing research capacity strengthening in LMICs: a systematic review and meta-synthesis. AAS Open Res. (2021) 3:43. doi: 10.12688/aasopenres.13116.3
14. Elkbuli, A, Zajd, S, Narvel, RI, Dowd, B, Hai, S, McKenney, M, et al. Factors affecting research productivity of trauma surgeons. Am Surg. (2020) 86:273–9. doi: 10.1177/000313482008600340
15. Etando, A, Amu, AA, Haque, M, Schellack, N, Kurdi, A, Alrasheedy, AA, et al. Challenges and innovations brought about by the COVID-19 pandemic regarding medical and pharmacy education especially in Africa and implications for the future. Healthcare (Basel). (2021) 9:1722. doi: 10.3390/healthcare9121722
16. Jadhav, HT, and Bamane, PD. Assessing the impact of an online training program on research performance of students and faculty members. J Eng Educ Transform. (2021) 34:312–8. doi: 10.16920/jeet/2021/v34i0/157161
17. Bickler, SW, Funzamo, C, Rose, J, Assane, A, Cassocera, P, Vaz, F, et al. Building surgical research capacity in Mozambique. Acad Med. (2014) 89:S107. doi: 10.1097/ACM.0000000000000339
18. Williams, JR, Schatz, EJ, Clark, BD, Collinson, MA, Clark, SJ, Menken, J, et al. Improving public health training and research capacity in Africa: a replicable model for linking training to health and sociodemographic surveillance data. Glob Health Action. (2010) 3:5287. doi: 10.3402/gha.v3i0.5287
19. Tijssen, R, and Kraemer-Mbula, E. Research excellence in Africa: policies, perceptions, and performance. Sci Public Policy. (2018) 45:392–403. doi: 10.1093/scipol/scx074
Keywords: research capacity, low-resource setting, structured training, impact, surgical plan
Citation: Ameh EA, Seyi-Olajide JO, Ameh N, Michael A, Abdullahi MA, Aria ON, Obi N and Chukwu I (2024) Strengthening surgical healthcare research capacity in sub-Saharan Africa: impact of a research training programme in Nigeria. Front. Med. 11:1429168. doi: 10.3389/fmed.2024.1429168
Edited by:
Sebastian Schnaubelt, Medical University of Vienna, AustriaReviewed by:
Margaret Tarpley, University of Botswana, BotswanaChristoph Veigl, Medical University of Vienna, Austria
Copyright © 2024 Ameh, Seyi-Olajide, Ameh, Michael, Abdullahi, Aria, Obi and Chukwu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emmanuel A. Ameh, ZWFhbWVoQHlhaG9vLmNvLnVr
 Emmanuel A. Ameh
Emmanuel A. Ameh Justina O. Seyi-Olajide
Justina O. Seyi-Olajide Nkeiruka Ameh3
Nkeiruka Ameh3 Afieharo Michael
Afieharo Michael Mohammed AS Abdullahi
Mohammed AS Abdullahi Nkeiruka Obi
Nkeiruka Obi Isaac Chukwu
Isaac Chukwu